Abstract
Recurrent ovarian cancer has a propensity for peritoneal spread, and it remains confined to the peritoneal cavity for prolonged periods. An aggressive locoregional therapy comprising of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) in addition to systemic chemotherapy has produced promising results in the treatment of this condition for which there is no standard therapy and cure is almost impossible. This treatment has shown an improvement in survival in patients with platinum-resistant recurrent ovarian cancer as well which has an extremely poor prognosis. There is substantial evidence to warrant the use of CRS, but the role of HIPEC needs to be defined further. The results of randomized controlled trials evaluating its benefit are awaited. The extent of disease determined by the peritoneal cancer index (PCI) and complete removal of all visible disease are the two most significant prognostic factors affecting the outcomes of CRS and HIPEC. With the availability of new chemotherapeutic agents and targeted therapies, treatment strategies, which integrate all these treatments to provide maximal gain in survival to patients while preserving the quality of life, are needed.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
A large proportion of the patients with advanced ovarian cancer develop disease recurrence within few years [1, 2]. Most of the patients who recur die within 5 years since recurrent disease is usually incurable [3]. Second-line therapy includes either chemotherapy or surgery or both chemotherapy and surgery but the outcomes remain poor.
Although most of the initial recurrences are frequently platinum sensitive, patients eventually develop resistance to platinum-based chemotherapy [3]. Resistance to chemotherapy, which is either intrinsic (primary) or acquired (secondary), is a major problem in the treatment of ovarian cancer and the main contributing factor in cancer-associated mortality. An aggressive locoregional therapy comprising of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) in addition to systemic chemotherapy has produced promising results. The optimal use of this combined modality treatment in addition to systemic therapy has the potential to provide a significant prolongation of the disease-free survival (DFS) and overall survival (OS) both in these patients.
2 Appropriate Terminology for Recurrent Disease
The time to recurrence after completion of first-line chemotherapy, i.e. the platinum-free interval (PFI) , has been used to classify recurrent ovarian cancer into two broad groups—platinum sensitive or platinum resistant.
This division is arbitrary and was done for the purpose of study design and interpretation by the Gynecologic Oncology Group (GOG) [4]. The platinum-sensitive group comprises of patients who recur 6 months or more after cessation of platinum-based chemotherapy . The clinically resistant group consists of those patients who actually progress while receiving platinum-based therapy, whose best response to platinum-based therapy is stable disease, and who recur within 6 months of cessation of platinum-based treatment [5]. Within this group are patients who have progressed on chemotherapy or had a less than partial response (stable disease) and could be termed as ‘platinum refractory’. This is seen in 20% of the cases, and these patients have the lowest probability of responding to second-line therapy. Among the other platinum-resistant patients are those that have a complete clinical response after surgery and chemotherapy and recur within 6 months of cessation of therapy. This would include patients who had optimal and suboptimal cytoreductive surgery (CRS) both [5]. Subsequent recurrences are classified according to the PFI from the last treatment.
The PFI has been widely used as a clinical surrogate for predicting the response to chemotherapy and determining the prognosis [6]. However, there are several caveats in using this division. There is a variability in the use and timing of investigations used to diagnose a recurrence. This influences the time at which the relapse is diagnosed and hence the categorization of the patients as platinum sensitive or platinum resistant. Moreover, in the platinum-sensitive group, the ‘platinum-free interval’ affects the response to further systemic therapy, with patients who are platinum-free for more than 12 months having better outcomes than those with a shorter PFI [6].
At the fourth Ovarian Cancer Consensus Conference (fourth OCCC) in Vancouver in 2010, there was an agreement that future clinical trials should evaluate outcomes based on four subsets of patients [7]. This division is also based on the PFI and is as shown in Table 11.1.
With the increasing use of non-platinum and biological agents like poly-ADP-ribose polymerase (PARP) inhibitors and angiogenesis inhibitors that may have an impact on disease biology and response to subsequent therapy, the PFI may not be the only prognostic factor affecting outcomes. At Fifth Ovarian Cancer Consensus Conference of the Gynecologic Cancer InterGroup, the PFI was replaced by a broader term, i.e. treatment-free interval (TFI), which was further divided into the TFI from last platinum dose (TFIp) , the TFI from last non-platinum therapy (TFInp) as well as last biological agent (TFIb) [8]. These classifications are being used to stratify patients for clinical trials that evaluate various systemic therapies.
An additional prognostic factor that has been overlooked in these classifications is the completeness of the first surgery. Some patients who did not have an attempt at complete CRS by a surgical/gynecologic oncologist may or may not have a complete response after chemotherapy. They may be inappropriately classified as platinum resistant/platinum refractory. Classe et al. suggested that to distinguish patients with a true early relapse refractory to platinum, other criteria such as the completeness of primary surgery performed in an expert centre need to be added to the disease-free interval [9].
3 Pattern of Recurrence
The commonest site of recurrence in epithelial ovarian cancer is the peritoneum. Seventy five percent of recurrences occur in the peritoneum, and in almost 50% of these cases, the peritoneum is the only site of recurrence [10]. Nodal recurrence is the second most common and is usually associated with peritoneal disease. Distant metastases are a rare site of disease recurrence [10].
Disease can recur in both treated and non-treated areas of the peritoneum. Pelvic recurrences are more common than upper abdominal recurrences [11, 12].
A retrospective study of 104 patients showed that in comparison to patients receiving systemic chemotherapy alone, patients who received intraperitoneal chemotherapy were more likely to recur in the upper abdomen or in extra-abdominal nodes [13]. Most of the recurrences from ovarian cancer are diffuse. In a study of 270 patients, reported by Ferrandina et al., ‘diffuse peritoneal carcinomatosis’ was seen in 62.1% of cases, while recurrences presented as a single lesion or multiple nodules occurred in 9.9 and 26.7% of cases, respectively [14]. Peritoneal carcinomatosis was defined as 20 or more peritoneal nodules by Chi et al. [15]. Isolated recurrence has been reported in patients with platinum-resistant disease as well [16]. It has been shown that the pattern of recurrence is dependent neither on the initial stage nor the completeness of CRS. A complete CRS does not affect the timing or pattern of recurrence though it reduces the absolute number of recurrences [17]. However, most of these studies consider <1 cm residual disease as a cut-off for complete cytoreduction though current evidence has shown that outcomes are better in patients with no residual disease as compared to any size of visible residual tumour [18].
4 Treatment of Recurrence
The treatment of recurrence essentially depends on the prior course of disease. It is important to review the prior treatment that has been administered—the surgical details and its completeness, the chemotherapy regimen, the time interval to recurrence—if complete remission was achieved or not.
The cornerstone of second-line therapy has been chemotherapy, and surgery is conventionally reserved for isolated localized recurrences. However, despite subjective and objective responses to second-line therapy and a prolonged disease-free and overall survival that is obtained in certain patients who have platinum-sensitive disease, the outcome of these patients is poor and cure is almost impossible [5]. The intent of treatment needs to be defined before starting any kind of therapy.
The tendency of recurrent disease to remain confined to the peritoneal cavity for prolonged periods forms a strong rationale for an aggressive locoregional approach comprising of CRS with or without hyperthermic intraperitoneal chemotherapy (HIPEC).
4.1 Evidence for Cytoreductive Surgery for Recurrent Ovarian Cancer
CRS can be performed as a second look following previous suboptimal surgery (secondary CRS) or for disease recurrence after complete response to first-line therapy (salvage CRS). The term ‘secondary CRS’ is broadly used for both situations. The completeness of surgery is defined according to the maximum diameter of the residual disease nodules. Complete cytoreduction is generally used for cases where there is no visible residual disease according to the completeness of cytoreduction score (Table 11.2) by Sugarbaker et al. [19]. The other commonly used term is ‘optimal cytoreduction’ which as defined by the Gynecologic Oncologic Group (GOG) as residual disease measuring <1 cm in maximal diameter [20].
Most of the evidence to support the use of CRS for recurrent ovarian cancer comes from retrospective studies [21,22,23,24]. These studies had a complete cytoreduction rate ranging from 50 to 87%. The median overall survival (OS) in patients undergoing complete cytoreduction ranged from 29 to 60 months. The criteria for complete CRS varied from no visible macroscopic residual disease to residual disease measuring <2 cm. Most of these studies have a short follow-up (1–4 years) and do not stratify patients according to PCI.
In a population-based study from the Netherlands, 408 patients who underwent secondary CRS at 38 centres experienced a median survival of 51 months [25]. Complete cytoreduction was achieved in 295 (72.3%) patients, with an OS of 57 months compared with 28 months in patients with incomplete cytoreduction (p = 0.001). Non-serous histology, a long progression-free interval (hazard ratio [HR], 0.29; 95% CI, 0.07–1.18), a good performance status (HR, 0.68; 95% CI, 0.49–0.94), secondary CRS without preoperative chemotherapy (HR, 0.72; 95% CI, 0.51–1.01) and complete CRS (HR, 0.46; 95% CI, 0.33–0.64) were prognostic factors for survival [25].
In a retrospective review of secondary CRS, Munkarah et al. found that patients with no gross residual disease after CRS had a survival of 44–60 months as compared to 35 months in those receiving chemotherapy alone [26]. Optimal cytoreduction was achievable in 38–87% of the study populations reviewed with acceptable perioperative complications and mortality. However, the impact of secondary CRS on survival could not be analysed due to (1) the inter-investigator differences in defining optimal cytoreduction, (2) the heterogeneity of the patients included (3) and the lack of information on postoperative therapy. Though most of these studies have drawbacks like small numbers, retrospective nature and lack of proper stratification based on prognostic variables, the survival reported is higher than that shown by modern multi-agent chemotherapy alone, especially in patients who had complete tumour removal (44–60 months) [26].
Bristow et al. published a meta-analysis of 40 studies, including 2019 patients, 13 studies were published between 1983 and 2000 and 27 (67.5%) were published between 2001 and 2007 [27]. Twelve of the 40 reports utilized prospective non-randomized data collection methodology; there were 27 retrospective analyses and one retrospective case-control study. The mean weighted median disease-free interval (DFS) prior to CRS for recurrent ovarian cancer was 20.2 months reflecting a tendency to select patients with platinum-sensitive disease for surgery. The parameter significantly associated with survival was the size of the residual disease. Each 10% increase in the proportion of patients left with optimal residual disease was associated with a 2.69-month increase in median survival time (95% CI 0.90 months to 4.49 months, p = 0.004). Similarly, each 10% increase in the proportion of patients undergoing complete surgical resection was associated with an increase in median cohort survival time of 2.84 months (95% CI 1.29 months to 4.38 months, p = 0.0008). The various limitations of this study pointed out by the authors were selection bias in selecting studies for the meta-analysis as well as patient selection in each study, the data collection interval was 25 years leading to heterogeneity in the chemotherapy regimens and other prognostic factors like tumour size, the number of lesions and performance status were not analysed [27].
In a Cochrane Database review of nine studies comprising of 1194 patients, there was a prolongation in overall survival in women who had a complete cytoreduction (no visible residual disease) and optimal cytoreduction (<1 cm residual disease) compared to those who had suboptimal cytoreduction (>1 cm residual disease) [28]. This meta-analysis included only those studies that has >50 women and had compared outcomes between optimal and suboptimal cytoreduction. There were no randomized controlled trials in this study. The authors concluded that though suggestive, this could not be taken as conclusive evidence, and the survival benefit could be due to a more favourable disease biology rather than the surgical effort alone. According to them, a randomized controlled trial was needed to further define the role of secondary CRS [29].
Bickell et al. used the Surveillance, Epidemiology and End Results Medicare database to assess the benefit of CRS in women who developed recurrence after first-line therapy for ovarian cancer [29]. Women who developed recurrence within 6 months of completion of first-line therapy were excluded from the analysis. Of the 1635 (80%) women who experienced recurrence, 265 (16%) were treated with secondary CRS and chemotherapy, 1171 (72%) with chemotherapy alone and 199 (12%) received hospice care. Propensity score adjusted log-logistic analyses showed that women undergoing surgery with chemotherapy had significantly greater survival compared with those receiving chemotherapy alone (hazard ratio [HR] = 1.33; 95% confidence interval [CI], 1.20–1.47). The estimated median survival of women treated with chemotherapy was 4.1 years from time of diagnosis; those treated with secondary surgery and chemotherapy survived a median of 5.4 years; 67% of those receiving hospice survived an average of 2.2 years. The 403 women who received no secondary treatments were classified as nonrecurrent and had a median survival of 9.3 years. The authors concluded that secondary CRS with chemotherapy to treat recurrent ovarian cancer increases survival by 1.3 years compared with chemotherapy alone and pending ongoing randomized trial results may be considered a standard of care [29].
There is a clear benefit of secondary CRS in selected patients with recurrent ovarian cancer who have a complete cytoreduction. They experience a significantly greater DFS and OS compared to patients undergoing chemotherapy alone. However, the chemotherapy group also comprises of patients with poor prognostic factors like platinum-resistant disease, extensive disease not amenable to complete cytoreduction and those with a poor performance status. Currently, three clinical trials are underway which will define the role of secondary CRS further.
The DESKTOP III is a phase 3 randomized controlled trial evaluating the role of cytoreductive surgery for first recurrence that has completed accrual. The results are expected in 2019. Patients with a positive AGO score (described below) are randomized to chemotherapy alone or CRS and chemotherapy (ClinicalTrials.gov identifier: NCT01166737).
Another randomized controlled multicentric trial is currently underway in the Netherlands (Netherlands Trial Register number: NTR3337; the Dutch SOCceR trial) that randomizes women with platinum-sensitive recurrence to undergo secondary CRS followed by platinum-based chemotherapy or platinum-based chemotherapy alone. Inclusion criteria are FIGO stage IC-IV (FIGO system 1988), first-line treatment consisted of complete or optimal (≤ 1 cm) cytoreductive surgery and (neoadjuvant) platinum-taxol-based chemotherapy, ascites <500 mL (pocket <8 cm on ultrasound examination), complete resection seems possible (estimated by a gynaecologic oncologist), good performance status (ECOG 0–1) and administration of platinum-based chemotherapy is possible [30].
The GOG 213 is a phase 3 randomized controlled trial that will determine the impact of secondary CRS in addition to chemotherapy in recurrent platinum-sensitive ovarian, fallopian tube and primary peritoneal cancer patients (NCT00565851).
The results of these trials will be available only after a few years. Meanwhile, CRS continues to be incorporated into second-line therapy as there is strong evidence showing a survival benefit.
The issues that need to be dealt with while incorporating CRS into second-line therapy are:
-
Criteria for selecting patients
-
Role of CRS in patients with platinum-resistant/platinum-refractory disease
-
Sequencing systemic chemotherapy with CRS, before or after
4.1.1 Selection of Patients
Selection of patients is important for attaining optimal results. Most studies report a favourable outcome in patients who recur more than 12 months after completion of first-line therapy and those who have complete/optimal cytoreduction [21,22,23,24, 31].
Other factors like a solitary site or limited number of sites of recurrence, complete response to first-line therapy and small maximum tumour diameter have also been associated with better survival outcomes [21,22,23,24, 31]. Only patients with minimal (<500 cc) or no ascites are subjected to surgery [32]. Women with symptomatic ascites, carcinomatosis, early relapse (i.e. less than 6 months) and poor general health are not likely to benefit from secondary CRS [33,34,35].
The AGO-DESKTOP study retrospectively analysed 267 patients who had undergone CRS for recurrent ovarian cancer and concluded that only those patients who had a complete CRS experienced a prolonged survival. A combination of performance status, early FIGO stage at the first surgery or no residual tumour after first surgery and absence of ascites could predict complete resection in 79% of patients. However, in patients with a negative score, a complete cytoreduction was achieved in 58%. The authors proposed a two-step model—patients with a negative score should undergo a laparoscopic evaluation and those without carcinomatosis be taken up for secondary CRS. With this strategy, a complete cytoreduction was possible in 63% of the patients with a negative score [36]. The DESKTOP II study prospectively analysed the predictive value of three of these criteria also known as the AGO score (complete resection at first surgery, good performance status and absence of ascites) and found that when all three are met with, a complete cytoreduction can be achieved in 76% of the patients with a morbidity of 11% [37]. This score is the first prospectively validated instrument to positively predict surgical outcome in recurrent ovarian cancer. It can aid in the selection of patients who might benefit from secondary cytoreductive surgery. However, in a retrospective study of 192 patients, a large proportion of patients with a negative AGO score also had complete removal of macroscopic disease at the time of secondary CRS, and the authors concluded that a refinement in the score was needed to exclude women who were unlikely to benefit from surgery [38].
Once again, these criteria exclude a subgroup of patients who never had surgery by a gynecologic oncologist/surgical oncologist leading to residual/recurrent disease and could benefit from secondary CRS.
It is prudent to undertake only those patients for surgery in whom there is probability of achieving a complete CRS. The survival in patients undergoing incomplete cytoreduction is similar to those receiving chemotherapy alone. This makes it important for such treatment to be carried out at expert centres by surgeons experienced in performing such procedures.
Despite the large body of evidence in favour of secondary CRS, the selection criteria need to be more clearly defined.
4.1.2 Platinum-Resistant Disease
The platinum-resistant group includes patients who are platinum refractory (progression on chemotherapy or stable disease after first-line therapy) and those who are platinum resistant (recurrence within 6 months of complete response to first-line therapy).
For patients with platinum-refractory disease who have had an attempt at complete cytoreduction at an expert centre, the treatment is chemotherapy. However, if the primary cytoreduction was not performed by an expert surgical/gynaecologic oncologist, a secondary CRS can be attempted.
Most studies use recurrence within 6 months as an exclusion criteria for secondary CRS; hence, evidence to support the use of surgery in these patients is scarce. Moreover, patients are not stratified as platinum refractory and platinum resistant which makes it difficult to determine the exact benefit or the selection criteria.
In a retrospective review of 18 patients by Musella et al., the 5-year overall survival was significantly longer in CRS group (57%) when compared with the control group of patients who received only systemic therapy (23.5%; p = 0.035). However, the peritoneum was the site of relapse in only 33% of these patients [39]. In another study of six patients with isolated peritoneal relapse and isolated lymph nodal recurrence treated with secondary cytoreductive surgery, secondary CRS significantly prolonged median time to first progression (12 vs 3 months; p-value = 0.016), median time to second progression (8 vs 3 months; p-value = 0.037) and post-relapse survival (PRS) (32 vs 8 months; p-value = 0.002). Residual tumour at the first surgery (p = 0.017), the PFI (p = 0.020) and complete cytoreduction (p = 0.039) were the independent prognostic factors on multivariate analysis [16]. In selected patients with platinum-resistant disease, secondary CRS could be attempted after second-line chemotherapy provided a complete cytoreduction can be attained. Such procedures are performed in patients with a good performance status and after controlling the disease with systemic chemotherapy.
4.2 Detection of Recurrence
In patients who have had a complete remission, an elevated CA 125 level is usually the first indication of disease recurrence. Some of these patients may have no clinical symptoms (pelvic pain, bloating, obstruction) or evidence of disease on imaging studies. The tumour marker elevation usually precedes the clinical manifestation of recurrence. A patient with platinum-refractory disease may have persistent marker elevation after completion of frontline therapy and/or radiological evidence of residual disease.
According to the Gynecologic Cancer InterGroup definition, CA 125 progression is defined by a progressive serial increase in serum CA 125 level as follows: patients with pretreatment CA 125 elevation normalizing during or after therapy or patients with pretreatment normal CA 125 who show a CA 125 value of at least two times the upper limit of the normal level on two measurements taken at least 1 week apart [40]. Patients with increased pretreatment CA 125 who never normalize must have a CA 125 value of at least two times the nadir value on two measurements at least 1 week apart [40]. This definition is now used in many clinical trials, together with Response Evaluation Criteria in Solid Tumors (RECIST) criteria .
4.3 Early Versus Delayed Treatment of Recurrence
Since recurrent ovarian cancer is not curable in most cases, the role of early treatment based on tumour marker elevation alone has been questioned. In a randomized trial (MRC OV05/EORTC 55955), 529 of the 1442 registered patients were randomized to either receive immediate chemotherapy or chemotherapy at clinical progression following a rise in CA 125 levels [41].
In all, 94% of the patients randomized to immediate treatment received salvage therapy versus 88% of the patients in the delayed treatment arm. The median time to starting salvage therapy was significantly shorter in the immediate treatment arm (0.8 vs 5.6 months; HR: 0.29; p < 0.00001). At a median follow-up of 49 months, no differences in survival were observed between the two groups (HR: 1.0; p = 0.98). However, the evaluation of quality of life, which is of paramount importance given the palliative role of second-line therapy for the majority of relapsing patients, showed that it was significantly better in the delayed treatment arm. Median time spent with a good global health score was 7.2 months in the early versus 9.2 months in the delayed treatment arm, and time from randomization to first deterioration in global health score or death was shorter in the early compared with delayed group (3.2 vs 5.8 months; p = 0.002). The authors concluded that there was no role of starting second-line therapy in asymptomatic patients based on a rise in CA 125 alone [41]. The limitations of this trial which would preclude the use of such a strategy in clinical practice are the use of nonuniform salvage therapy across the participating centres, the diversity in the study population in terms of the PFI, the role of secondary CRS that was not explored and, in particular, the differences between optimal and suboptimal primary CRS in the two arms that were not evaluated [40]. Some of the patients who have resectable recurrences and could benefit from early treatment may be denied the benefit if such a strategy is applied uniformly.
Tanner et al. retrospectively evaluated outcomes in 121 patients who had a complete clinical response after first-line therapy and developed recurrent disease [42]. Twenty two (18.2%) were diagnosed with a symptomatic recurrence. Though the median time to first recurrence was similar for asymptomatic and symptomatic patients (24.8 vs 22.6 months, p = 0.36), the post-recurrence survival was significantly longer in asymptomatic patients (45.0 vs 29.4 months, p = 0.006). Though secondary CRS was attempted equally in both groups (41% vs 32%, p = NS), the rate of complete CRS (optimal residual disease (<or = 5 mm)) was higher in patients with asymptomatic disease (90 vs 57%, p = 0.053). On multivariate analysis, detection of asymptomatic recurrence was a significant and independent predictor of improved overall survival (p = 0.001). Median OS was significantly greater for asymptomatic patients (71.9 vs 50.7 months, p = 0.004). This difference did not appear to be attributable to a discrepancy in the timing of diagnosis as a lead time bias would suggest, but, rather, to the location of these recurrences, to their earlier amenability to salvage chemotherapy and to more successful secondary CRS due to decreased volume of disease [42].
The authors pointed out several limitations in the study—small size, retrospective nature, and exclusion of a large number of patients during the study period due to either inadequate follow-up information or transfer of the patient care to another provider.
In another retrospective review by Gadducci et al., no difference in survival was observed in asymptomatic patients versus symptomatic patients although the rate of attempted secondary CRS (15%) was significantly lower than the current series. However, patients undergoing secondary CRS and chemotherapy experienced a significantly better overall survival than those who did not undergo surgery [43].
Thus, there seems to be a clear benefit of detection and early treatment of asymptomatic recurrence though it may need further evaluation in randomized trials.
4.4 Investigations: Evaluation of Disease Extent
4.4.1 CT Scan
The most commonly performed investigation is a contrast enhanced CT scan of the thorax, abdomen and pelvis [44]. The typical CT findings in recurrent ovarian cancer are similar to that of peritoneal metastases arising from other primary sites:
-
Thickened peritoneum
-
Ascites
-
Pelvic mass
-
Pelvic/retroperitoneal lymphadenopathy
-
Bowel surface/mesenteric deposits
-
Omental involvement
-
Pelvic sidewall involvement and/or hydroureter
-
Diaphragmatic involvement
A CT scan determines not only the extent of the disease but also the involvement of certain areas that would preclude a complete CRS—like involvement of the porta hepatis, extensive involvement of the small bowel/mesentery, extensive diaphragmatic involvement and upper abdominal lymphadenopathy (suprarenal) [44]. Several CT-based scores and algorithms have been developed to predict the probability of complete CRS in advanced ovarian cancer, and the same can be used to predict the probability in case of recurrent disease [45,46,47]. The sensitivity of CT for peritoneal tumours less than 1 cm was found to be only 25–50% compared with 85–95% for larger tumour deposits [48]. A CT scan has been shown to underestimate the extent of carcinomatosis in 33% of patients [49].
4.4.2 PET Scan/PET-CT Scan
Several studies demonstrated a benefit of fluorine-18-fluorodeoxyglucose positive emission tomography (FDG-PET) and FDG-PET/computed tomography (FDG-PET/CT) in the early detection of recurrent disease in ovarian cancer [50,51,52,53]. In a prospective multicentric study, Fulham et al. found a higher rate of detection of nodal, peritoneal and subcapsular liver disease as well as the total number of sites of disease with PET-CT as compared to CT [54]. They found that FDG-PET/CT altered the management in about 60% of the patients. In another study the accuracy of PET-CT for predicting optimal cytoreduction was found to be 78.6%. Like CT scan the main limitation is in the inability to detect small tumour nodules [55].
4.4.3 Staging Laparoscopy
Laparoscopy allows direct visualization of the peritoneal surfaces, the small bowel and its mesentery and can pick up small nodules that are missed on imaging. The disadvantages are its inability to evaluate retroperitoneal structures like the ureters and pancreas, the omental bursa near the celiac axis and the depth of involvement of the hepatic pedicle and the diaphragm [56]. Fagotti et al. evaluated the role of staging laparoscopy for selecting patients for secondary CRS. The negative predictive value, specificity, positive predictive value, sensitivity and accuracy rate of staging laparoscopy were 88.9, 64.0, 80.8, 95.0 and 83.1%, respectively [57]. A combined radiological (PET-CT) and laparoscopic evaluation showed a negative predictive value of 88.9%, a specificity of 59.3%, a positive predictive value of 78.8%, a sensitivity of 95.3% and an accuracy rate of 81.4%. The authors suggested that a combination of these two modalities could optimize patient selection [57].
4.5 Surgical Strategies for Secondary Cytoreductive Surgery
The goal of secondary CRS should be to attain a complete/optimal cytoreduction. Many surgeons/institutions still use cut-offs of residual tumour measuring <0.5 or <1 cm as the criteria for optimal CRS though there is evidence that complete removal of macroscopic disease (completeness of cytoreduction score, 0, i.e. CC-0) results in superior outcomes as compared to leaving behind any amount of residual disease [15, 19, 27].
To attain a complete cytoreduction, a combination of peritonectomy procedures and visceral resections needs to be performed as for peritoneal metastases from other tumours [58]. The visceral resections include small and large bowel resection, cholecystectomy, partial gastrectomy, full-thickness diaphragm resection, splenectomy, distal pancreatectomy, partial ureteric resection, partial cystectomy and resection of pelvic sidewall [59,60,61]. A detailed description is provided elsewhere [62]. Such procedures have a survival benefit if complete CRS can be obtained [63]. Though the goal is complete removal of macroscopic disease, it should not impair the gastrointestinal and urinary function to the extent that the quality of life is significantly impaired. Extensive intestinal resections that impair digestion and nutrition and lead to dependence of parenteral nutrition (extensive small bowel resection with or without total gastrectomy or colectomy) should not be performed. Posterior pelvic exenteration is often necessary; however, the vesical trigone must be left intact because, in this context, a total cystectomy should never be performed [64].
If a pelvic and/or retroperitoneal lymphadenectomy was not performed during primary CRS, it should be performed irrespective of the presence or absence of nodal metastases in patients undergoing complete CRS. This is performed even in patients with no evidence of lymph node involvement on preoperative imaging. Nodal recurrence can be isolated or present with peritoneal disease [65, 66]. Retroperitoneal lymphadenectomy is performed till the level of the renal veins. There is a survival benefit of surgery for nodal recurrence even if it is bulky (>2 cm maximum diameter of the largest lymph node is considered bulky nodal disease) [67,68,69]. In case of disease involving the suprarenal nodes, lymphadenectomy can be performed in this region also if the disease is not bulky and limited [63].
Hepatic resection can be performed synchronously with secondary CRS for solitary or multiple parenchymal liver metastases. The goal of such resections should be to resect the liver lesions with a negative margin. Several retrospective studies have reported an acceptable morbidity and mortality for such combined resections [70]. The common prognostic factors reported in these studies were optimal CRS <1 cm residual disease, negative resection margins, disease-free interval >12 months, fewer number of liver metastases and fewer sites of disease. The surgical and oncological outcomes from various studies on resection of hepatic metastases in recurrent ovarian cancer are described in Table 11.3.
4.6 Minimally Invasive Secondary CRS
Several studies have reported the feasibility of a minimally invasive approach for secondary CRS [78,79,80,81]. These studies include patients with localized recurrence (1–3 nodules), good performance status and long platinum-free interval. The reported morbidity and mortality is similar to that of open surgery and conversion rates are low (Table 11.4). One series reported the use of loop electrosurgical excision and argon beam coagulator to ablate the metastases [79]. Such methods cannot replace a formal peritonectomy and/or resection of the viscera where indicated. Though there is no head to head comparison, it has been suggested that such an approach could shorten the postoperative recovery times, leading to a better psychological state and quality of life [78]. The minimally invasive approach has an important limitation. A preoperative CT scan combined with a staging laparoscopy should be used to determine the extent of disease, though the extent of disease is usually underestimated. Moreover, the laparoscopic assessment is often limited by the presence of adhesions, and this should be kept in mind when taking up patients for such procedures.
4.7 Prognostic Factors
In a retrospective review of 153 patients with platinum-sensitive disease undergoing secondary cytoreductive surgery, Chi et al. reported that those with carcinomatosis had a poorer outcome compared to those patients with isolated disease or multiple nodules (<20) [15]. Similarly, patients recurring within 6–12 months of completion of frontline therapy fared worse than those recurring from 13 to 30 months or >30 months [15]. It is important to have a reproducible quantification of the disease extent—the disease extent is one of the strongest prognostic factors determining the outcome of second-line surgical therapy—and having a uniform method of quantifying it enables comparison of treatment outcomes. The most commonly used score for this is the ‘peritoneal cancer index’ (PCI) developed by Paul Sugarbaker [19]. Other poor prognostic factors are mucinous or clear cell histology and more than one route of metastasis (e.g. peritoneal metastases with haematogenous or lymphatic spread) [15]. In a meta-analysis that included 2019 patients, Bristow et al. evaluated the impact of residual tumour size ranging from 0 to 2 cm on overall survival. The only statistically significant clinical variable independently associated with post-recurrence survival was the proportion of patients undergoing complete CRS (p = 0.019). When each study was analysed individually also, there was a survival benefit that was significant in patients who had complete CRS as compared to those who had any size of residual disease. The presence of any size of residual disease was associated with a greater risk of dying due to disease. After controlling for all other factors, each 10% increase in the proportion of patients undergoing complete CRS was associated with a 3.0-month increase in median cohort survival time [27].
4.8 Systemic Chemotherapy in Addition to Secondary Cytoreductive Surgery
The role of systemic chemotherapy in addition to secondary CRS has not been evaluated. Most studies have used systemic chemotherapy either before or after secondary CRS. All ongoing clinical trials have incorporated chemotherapy in the surgical arm as well. Though the best treatment strategy for such patients is not known, a logical approach is as follows. In patients with disease resectable upfront, secondary surgery could be performed first followed by chemotherapy. It is important in such cases that postoperative chemotherapy is not delayed due to complications. In patients who recur within 6 months of first-line therapy or have disease not amenable to a complete cytoreduction, second-line chemotherapy can be administered before secondary/salvage CRS.
5 Rational for Intraperitoneal Chemotherapy for Recurrent Ovarian Cancer
Recurrent ovarian cancer remains confined to the peritoneal cavity for prolonged periods which is the basis of using intraperitoneal chemotherapy as part of locoregional therapy. Intraperitoneal (IP) drug therapy offers the potential to increase the therapeutic index by enhanced local drug concentration and at the same time limiting systemic absorption and toxicity [82]. It exposes the poorly vascularized tumour tissue to high concentrations of cytotoxic agents. The efficacy of IP drug therapy depends on the extent of drug penetration in tumour tissue, which is driven by diffusion and convection [82]. Obstacles to drug transport include elevated interstitial fluid pressure and the density of the interstitial matrix which are characteristic of tumour stroma [82]. In optimally resected stage III ovarian cancer, large randomized trials have shown that the addition of IP chemotherapy to adjuvant regimens significantly improved survival [83,84,85,86]. This type of chemotherapy is repeatedly administered through an implanted catheter and access port. Adverse events and catheter-related problems were more common in the IP chemotherapy group and often led to discontinuation of therapy [87, 88]. IP chemotherapy can be administered by direct abdominal wall puncture as well [89]. Benedetti-Panici reported the use of ultrasound-guided direct puncture and administration of chemotherapy in 38 patients with recurrent ovarian cancer. A total of 402 IP procedures were performed, with a mean of 10.5 procedures per patient. The feasibility rate was 97.4% [90]. In a retrospective study of 33 patients, Nicoletto et al. used IP chemotherapy administered in this manner for recurrent ovarian cancer [91]. This treatment was used as an alternative to systemic chemotherapy in patients who had received multiple lines of chemotherapy and no CRS was performed. IP cisplatin was administered on day 1 and paclitaxel on day 8 every 21–28 days for a total of 3–4 cycles. Twenty-seven patients had ascites and 14 patients had peritoneal carcinomatosis only. Fourteen (51.8%) out of 27 patients had a clinical response, with disappearance or significant reduction of ascites for more than 45 days after IP chemotherapy. These patients were compared to matched controls who received only systemic chemotherapy. In patients with less than three previous lines of treatment, IP chemotherapy conferred a survival advantage of about 2.2 months (IP = 10.0 vs IV = 7.8 months, p = 0.011). However, the survival advantage in heavily pretreated patients (with three or more previous treatments) was not significant [91]. There is not much evidence for this type of intraperitoneal chemotherapy in recurrent ovarian cancer. Hyperthermic intraperitoneal chemotherapy (HIPEC) is more commonly used in combination with CRS for recurrent ovarian cancer.
6 Rationale for Hyperthermic Intraperitoneal Chemotherapy (HIPEC)
The rationale for using HIPEC as part of second-line therapy for ovarian cancer is the same as that for CRS—recurrent ovarian cancer remains confined to the peritoneal cavity for a prolonged period. This is further supported by the benefit CRS and HIPEC have shown in the treatment of gastrointestinal peritoneal metastases. CRS and HIPEC are now the standard of care of pseudomyxoma peritonei and peritoneal mesothelioma and for colorectal peritoneal metastases with a limited peritoneal spread [92,93,94,95]. It is still the only treatment modality that has shown to prolong survival in patients with peritoneal metastases from gastric cancer [96, 97].
HIPEC is administered immediately after CRS which reduces tumour cell entrapment that is common after surgery. HIPEC has the added advantage of using heat which itself is cytotoxic to cancer cells and enhances the cytotoxicity of various chemotherapeutic drugs like platinum compounds, alkylating agents, mitomycin C and doxorubicin that is enhanced by hyperthermia [98,99,100,101]. Hyperthermia enhances tissue perfusion and oxygenation and may improve drug penetration [102].
7 HIPEC Methodology and Drugs
HIPEC can be performed by the open (coliseum) or closed technique maintaining an intra-abdominal temperature of 41–43° C throughout the procedure. HIPEC is performed only in those patients in whom complete cytoreduction is attained (CC-0 or CC-1) since the treatment is ineffective on residual disease more than 2–3 mm in size [103]. Any drug that is used for HIPEC should be retained in the peritoneal cavity with a limited systemic absorption [104].
One of the most commonly used drugs in this setting is cisplatin. Cisplatin is a drug that is retained in the peritoneal cavity, and its penetration into the adjacent tissues is potentiated by heat in both platinum-sensitive and platinum-resistant cell lines [105].
Hyperthermia can modify the cellular resistance to cisplatin as demonstrated by Hettinga et al. [106]. Relatively high doses of heat 43° for 60 min can interfere with cisplatin resistance by several mechanisms like drug penetration, adduct formation and repair [105]. These are further elaborated in Table 11.5. Hyperthermia can increase the cytotoxicity of cisplatin in both platinum-sensitive and platinum-resistant cell lines [107].
Van de Vaart et al. showed that cisplatin in combination with hyperthermia in vitro leads to a higher cisplatin ± DNA adduct formation which was a good predictor of the cytotoxic effect. The level of cisplatin-DNA adduct formation which is needed for a cytotoxic effect was observed in tumour nodules up to a depth of 5 mm. Hence, the effect HIPEC is useful for patients who are cytoreduced to minimal residual disease (CC-0/1) [108].
The ideal dose of cisplatin has been evaluated in the CHIPASTIN trial . This phase 1–2 escalating dose trial established that 70 mg/m2 of cisplatin for 1 h at 42 °C was the most appropriate protocol [109]. However, another phase 1 study concluded that a 100 mg/m2 dose of cisplatin for HIPEC in recurrent platinum-sensitive ovarian cancer has an acceptable safety profile [110].
Oxaliplatin that is commonly used for HIPEC in colorectal and appendiceal tumours has been used in recurrent ovarian cancer as well [111,112,113]. There is no direct comparison of oxaliplatin with platinum agents or taxols though preclinical data have shown a role in recurrent and platinum-resistant ovarian cancer [114]. Oxaliplatin has only moderate cross-resistance with cisplatin or carboplatin [115].
Carboplatin has a favourable toxicity profile compared to cisplatin and has replaced it in many of the intravenous regimens [102]. When nephrotoxicity is a concern, it can be administered in full dose for HIPEC as opposed to cisplatin which requires a dose reduction [116]. When a high dose of carboplatin is used for HIPEC, the drug concentration achieved in the tumour tissue is similar or superior to that achieved by an equitoxic dose of cisplatin [117]. Carboplatin undergoes hyperthermic enhancement of cytotoxicity and has been shown to have a more homogenous distribution of platinum as compared to cisplatin [117, 118]. Phase 1 trials for HIPEC as first-line and second-line therapy found that carboplatin doses up to 800–1000 mg/m2 were tolerable and did not preclude additional systemic therapy [119,120,121]. The duration of treatment is 90 min.
Paclitaxel (175 mg/m2) alone or in combination with cisplatin (100 mg/m2) at 41–43° C for 90 min has been used by some investigators for HIPEC in patients with platinum-sensitive recurrent ovarian cancer [122, 123]. The morbidity was acceptable and the drugs achieved high concentrations in the peritoneal tissue with low systemic absorption. The tissue penetration of paclitaxel was only 0.5 mm, compared to 2–3 mm for cisplatin [122, 124, 125]. The numbers in these studies are small, and further evaluation of toxicity and efficacy of such a regimen is needed. Unlike cisplatin, hyperthermia does not augment the cytotoxicity of paclitaxel [126].
Melphalan has been used for HIPEC in patients with recurrent tumours arising from various primary sites including recurrent and platinum-resistant ovarian cancer [127, 128]. The use of melphalan has been prompted by responses produced in regional chemoperfusion in soft tissue sarcomas and extremity melanomas [129, 130]. Melphalan undergoes cytotoxic enhancement with hyperthermia and has a favourable peritoneal fluid to plasma ratio [131,132,133,134]. Bijelic et al. first reported the use of 50–70 mg/m2 of melphalan at 41–43° C for 60–90 min in 34 patients [127]. The grade 3–4 morbidity was 43% and there was no mortality in this series. They recommended the use of 60 mg/m2 for 60 min for future evaluation of the role of melphalan.
The other agents that have been used are mitomycin C, doxorubicin, gemcitabine and irinotecan.
There is no study that has performed a head to head comparison between various agents/regimens.
Helm et al. analysed the effect of chemotherapy agents on survival in relation to the time point at which they were used. In patients with platinum-sensitive recurrence, the OS was superior with carboplatin as compared to cisplatin (p = 0.012) and mitomycin (p = 0.011), but there was no significant difference between agents in platinum-resistant disease. However, the numbers in the carboplatin group were small [135].
Some of the common regimens for HIPEC are listed in Table 11.6.
8 Evidence for HIPEC in Recurrent Ovarian Cancer
Salvage CRS and HIPEC is performed in patients who have recurred after an initial complete response to first-line therapy, and secondary CRS and HIPEC is performed in patients who have had an incomplete CRS with chemotherapy resulting in a partial response or stable disease [139]. Investigators have compared outcomes in patients who received HIPEC during secondary CRS with those who only received SCS and postoperative chemotherapy and those who only received IV chemotherapy without SCS [140]. Most of the available evidence comes from retrospective single and multi-institutional studies (Table 11.7). These studies have reported a median DFS ranging from 10 to 7 months, median OS ranging from 24 to 51 months and a 5 year OS ranging from 15 to 63%.
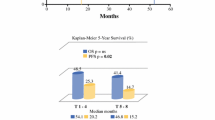
Petrillo et al. in a study of 70 patients treated with secondary CRS and HIPEC reported a longer second remission than the first in 52% of the patients. This is higher than that reported by most chemotherapy trials in a similar patient population as the second and subsequent remissions are usually shorter than the first [159, 160]. In a French retrospective multicentric study of 474 patients, the median OS was 45.7 months, and in patients who had complete CRS, it was 47.2 months in patients with platinum-sensitive disease and 51.6 months in those with platinum-resistant disease [152]. This difference was not statistically significant and showed that patients with platinum-resistant disease could have a survival similar to those with platinum-sensitive disease (Fig. 11.1).
Overall survival in platinum-sensitive (chemosensitive) and platinum-resistant (chemoresistant) recurrent epithelial ovarian cancer treated with cytoreductive surgery and HIPEC (log rank p-value = 0.799) (From ref. [152] with permission)
A PCI of >8 was found to be a significant factor affecting both disease-free and overall survival. The patients in this series included those with second and third recurrences as well. In 2015, the same group published the outcomes of secondary CRS and HIPEC in patients with first recurrence comprising of 314 patients from 13 institutions [9]. The CRS performed during first-line therapy was complete in 33.8% (101/314) patients, there was macroscopic residual disease in 66.2% (98/314) patients and this information was unknown for 15 patients. Treatment strategy was secondary chemotherapy followed by secondary surgery and HIPEC for 85.6% (269/314) of patients; the remaining patients were treated with secondary surgery and HIPEC before secondary chemotherapy. At a median follow-up of 50 months, the 5-year overall survival was 38.0%, with no difference between platinum-sensitive (n = 148) and platinum-resistant (n = 161) patients, and 5-year disease-free survival was 14%. Considering patients treated with second-line chemotherapy followed by secondary surgery and HIPEC, patients who had a pathological complete response to chemotherapy experienced a better DFS and OS both (Fig. 11.2). Median OS was not reached for patients with no pathological residual disease, while for patients with microscopic residual disease it was 56 months and for patients with a macroscopic residual disease 39 months (p = 0.073). The median DFS was 41 months for patients with no pathological residual disease, 13 months for patients with microscopic residual disease and 10 months for those with a macroscopic residual disease (p = 0.0019). The residual disease distribution was similar in the platinum-sensitive and platinum-resistant cases [9].
Overall (a) and disease-free survival (b) according to pathological residual disease at the time of secondary CRS and HIPEC (From ref. [9] with permission)
Four other studies treated patients with platinum-resistant disease with CRS and HIPEC, two of these did not report the outcomes in patients with platinum-resistant disease separately. In a single institution series of 81 patients, the OS and DFS in patients with platinum-sensitive and platinum-resistant disease were similar. However, 58% of the patients had more than two disease recurrences and more than two surgical explorations leading to an inaccurate assessment of the PFI [146]. In another multi-institutional series of 83 patients, those with platinum-sensitive recurrence experienced a significantly better OS compared to patients with platinum-resistant disease [135]. However, patients with advanced and recurrent ovarian cancer were pooled together in this analysis due to which the impact of secondary CRS and HIPEC in platinum-resistant disease cannot be determined from this series.
In a meta-analysis of 9 comparative and 28 other studies evaluating the role of CRS and HIPEC in advanced and recurrent ovarian cancer, CRS and HIPEC with systemic chemotherapy appeared to significantly improve 1- and 3-year overall survival compared with CRS + chemotherapy alone (OR 3.48, 95% CI 1.44–8.44, p = 0.006; OR 7.39, 95% CI 2.29–23.86, p < 0.001, respectively). However, the 2-, 4- and 5-year overall survival benefit was not statistically significant (OR 2.84, 95% CI 1.01–7.89, p = 0.05; OR 2.82, 95% CI 0.71–11.2, p = 0.14; OR 2.37, 95% CI 0.4–14.12, p = 0.34, respectively) [161]. The first published randomized controlled trial for HIPEC in recurrent ovarian cancer randomized 120 women undergoing secondary CRS to receive HIPEC or not. They included both platinum-sensitive and platinum-resistant cases, using cisplatin and paclitaxel for the platinum-sensitive patients and a doxorubicin/paclitaxel regimen for the platinum-resistant cohort. The OS for the HIPEC group was significantly longer than that of the control group (26.7 vs 13.4 months). Patients with a complete cytoreduction experienced a better survival compared to those with residual disease, and a PCI > 15 had a negative impact on survival. There was no difference in the OS in patients with platinum-sensitive and platinum-resistant disease. Chi et al. pointed out several weaknesses in the reporting of this trial—lack of information on the DFS, median follow-up, postoperative first-line treatment and complication rates [140].
Several case-control studies have compared secondary CRS and HIPEC with CRS alone [123, 162,163,164,165,166]. In four of these, there was a statistically significant benefit of CRS and HIPEC over CRS alone. These studies are listed in Table 11.8. One case-control study showed a survival benefit of secondary CRS and HIPEC over systemic chemotherapy alone in patients with platinum-sensitive recurrence [167]. Most of these studies have a small number of patients.
Thus, CRS and HIPEC appear to be a beneficial option for patients with recurrent ovarian cancer where currently there is no standard therapy. Though there are case-control studies demonstrating its benefit over CRS alone, the numbers in these studies are small, and further evaluation is needed in randomized controlled trials. Selecting patients is the key—patients with a limited PCI derive the maximum benefit from this procedure [152]. Other important variables are the completeness of cytoreduction and time to recurrence.
9 Clinical Trials Evaluating the Role of HIPEC in Recurrent Ovarian Cancer
Four clinical trials are underway to evaluate the role of HIPEC in recurrent ovarian cancer (Table 11.9). The HORSE trial (NCT01539785)—CRS with or without HIPEC in Ovarian cancer recurrence—is underway in Italy and is expected to complete accrual in 2018. Patients with platinum-sensitive ovarian cancer (PFI > 6 months) are randomized to secondary CRS with or without HIPEC followed by systemic chemotherapy in both arms. The primary end point is progression-free survival, and the secondary end points are post-recurrence overall survival, quality of life, morbidity and mortality and pattern of recurrence. Patients will be stratified according to PCI and PFI. HIPEC is expected to result in a >6 months benefit in the PFI. A similar trial CHIPOR (NCT01376752) is underway in Europe. At the first recurrence (PFI > 6 months), all patient receive three cycles of second-line chemotherapy followed by CRS with or without HIPEC. HIPEC is performed by the open or closed method using 75 mg/m2 of cisplatin for 60 min. The primary end point is overall survival (HIPEC should provide a 12-month benefit in overall survival), and the secondary objectives are improvement in DFS post-recurrence, morbidity and mortality, quality of life and cost-effectiveness. In addition, the pathological response to chemotherapy will be assessed, and a pharmacokinetic study comparing the open and closed methods will be performed. A similar phase 2 multi-institutional trial is being carried out in the United States using HIPEC with carboplatin for 90 min. The primary end point is progression-free survival. The fourth trial is being carried out at the Loma Linda University in the United States (NCT02672098). This is a phase 1 prospective study with the primary objective of comparing the efficacy and safety of CRS and HIPEC in treatment of recurrent ovarian, primary peritoneal or fallopian tube cancers. All patients with residual disease ≤2.5 mm after CRS will receive HIPEC for 90 min with carboplatin (800 mg/m2) using the closed abdomen technique. The primary objective is progression-free survival. Historical controls will be used for comparison.
Most of these trials are lagging behind in recruiting the expected number of patients over a given time period. The probable reasons for this as mentioned by the investigators are patients wanting treatment with HIPEC and to not undergo randomization and physician preference for newer systemic therapies instead of HIPEC. None of these trials evaluate the role of CRS and HIPEC in platinum-resistant patients.
These trials will help in clarifying the role of HIPEC in recurrent ovarian cancer. The drug regimens used have been validated in phase 1–2 trials [109, 110, 168]. However, given the multitude of regimens in use in clinical practice and in absence of a head to head comparison, future evaluation will continue to determine the best drugs and protocols.
Preclinical studies provide a strong basis for applying this therapy in clinical practice [169]. HIPEC in addition to secondary CRS has shown promising results in the data available so far. The challenge is to optimize HIPEC methodology and drug regimens and integrate CRS and HIPEC with systemic therapies to provide a meaningful benefit of this treatment to patients—in terms of survival, cost-effectiveness and quality of life.
10 Morbidity and Mortality
Reported mortality rates of secondary CRS and HIPEC range from 0 to 4.2%. Large series have reported a major morbidity (grade 3–4 complications) in 30–34.8% and a reoperation rate of 8% [9, 152, 157]. The meta-analysis by Huo et al. reported a pooled median 30-day post-HIPEC mortality rate in 1.8% (range, 0–13.6%) and major (grade 3–4) morbidities in 26.2% (1.8–55.6%) of the patients. The pooled rate of minor (grade 1–2) morbidities was 27.5% (16–60.2%) [161]. These reports are similar to the morbidity and mortality rates reported in patients undergoing CRS alone for advanced ovarian cancer [18, 170]. Major complications include anastomotic leakage, bowel perforation, intraperitoneal haemorrhage, acute renal failure and wound dehiscence. Complication specific to the administration of chemotherapy is neutropenia which is caused by systemic absorption of the drug. Over the years there has been a decline in the morbidity and mortality from this procedure which is due to the increase in experience of high volume centres [171]. In these expert centres, the reduction in mortality is not just due to lower complication rates but also due to their ability to rescue patients with complications [172]. Morbidity and mortality should no longer preclude the use of this treatment where it is indicated.
11 Management of Subsequent Recurrences
Recurrent ovarian cancer that has been rendered disease-free after second-line therapy will recur in almost all cases. Ovarian cancer can be considered a chronic disease with majority of the patients developing multiple recurrences that can be induced into a remission with surgery and or chemotherapy [173]. The second, third and subsequent recurrences have been treated with a combination of CRS with or without HIPEC and systemic chemotherapy. In one of the first reports on tertiary CRS, Leitao et al. reported a median disease-specific survival (DSS) of 34.4 months (range 20.4–46.4 months) in 26 patients. The outcome was better in patients who had optimal cytoreduction (residual disease <0.5 cm) and a long disease-free interval >12 months (median DSS-60 months). Patients with platinum-resistant disease also experience a prolonged survival after optimal CRS [173]. In another series of 77 patients, the same authors reported a median DSS of 47.7 months [174]. Residual disease after surgery remained the only independent prognostic factor. The survival in both these series was similar to that reported for secondary CRS and was superior to that reported with chemotherapy alone [173, 174]. Similar results have been reported by other investigators [175, 176]. In another series of 159 patients, the platinum-free interval after second-line therapy, presence of mesenteric lymph node metastases at secondary CRS and tertiary CRS (as opposed to systemic chemotherapy) were predictors of survival [177]. However, the strongest predictor of survival was complete tumour removal, and patients with residual disease had a survival similar to those receiving chemotherapy alone. Patients with ascites and disease and recurrence outside the pelvis have a poor outcome [177, 178].
HIPEC has been used along with tertiary and subsequent cytoreductive procedures. Most of these studies have a mixture of patients with first, second and subsequent relapses, and its role in third- and fourth-line therapy has not been evaluated separately [112, 146, 152].
Cytoreductive surgery with or without HIPEC can provide a survival benefit in selected patients with recurrence after second-line therapy. There are no randomized trials comparing surgical treatment with chemotherapy.
Conclusion
Recurrent ovarian cancer is a chronic disease. Secondary/salvage cytoreductive surgery can be considered the standard of care for first recurrence in platinum-sensitive disease though the results of randomized controlled trials are awaited. Early detection and treatment of recurrence has a survival benefit. HIPEC in addition to CRS and systemic chemotherapy has shown promising results in retrospective and case-control studies in both platinum-sensitive and platinum-resistant disease and has acceptable rates of morbidity and mortality. The results of randomized controlled trials are awaited which will clarify its role in this situation. The patient selection for CRS and HIPEC, drugs and protocols need standardization. An optimization of clinical strategies is needed to provide the maximal benefit of CRS and HIPEC to patients—in terms of survival, cost-effectiveness and quality of life. Such treatment requires multidisciplinary management and should be carried out at expert centres.
References
Pfisterer J, Plante M, Vergote I, du Bois A, Hirte H, Lacave AJ, et al. Gemcitabine plus carboplatin compared with carboplatin in patients with platinum-sensitive recurrent ovarian cancer: an intergroup trial of the AGO- OVAR, the NCICCTG, and the EORTCGCG. J Clin Oncol. 2006;24:4699–707. https://doi.org/10.1200/JCO.2006.06.0913.
Parmar MK, Ledermann JA, Colombo N, du Bois A, Delaloye JF, Kristensen GB, et al. Paclitaxel plus platinum-based chemotherapy versus conventional platinum- based chemotherapy in women with relapsed ovarian cancer: the ICON4/AGO-OVAR-2.2trial. Lancet. 2003;361:2099–106. https://doi.org/10.1016/S0140-6736(03)13718-X.
Pfisterer J, Ledermann JA. Management of platinum-sensitive recurrent ovarian cancer. Semin Oncol. 2006;33:S12–6. https://doi.org/10.1053/j.seminoncol.2006.03.012.
Thigpen JT, Blessing JA, Ball H, et al. Phase II trial of paclitaxel in patients with progressive ovarian carcinoma after platinum-based chemotherapy: a gynecologic oncology group study. J Clin Oncol. 1994;12:1748–53.
Markman M, Bookman M. Second-line treatment of ovarian cancer. Oncologist. 2000;5(1):26–35.
Friedlander M, Trimble E, Tinker A, et al. Clinical trials in recurrent ovarian cancer. Int J Gynecol Cancer. 2011;21:771–5.
Stuart GC, Kitchener H, Bacon M, et al. 2010 Gynecologic Cancer InterGroup (GCIG) consensus statement on clinical trials in ovarian cancer: report from the fourth ovarian cancer consensus conference. Int J Gynecol Cancer. 2011;21:750–5.
Wilson MK, Pujade-Lauraine E, Aoki D, Mirza MR, Lorusso D, Oza AM, du Bois A, Vergote I, Reuss A, Bacon M, Friedlander M, Rincon D, Joly F, Chang SJ, Ferrero AM, Edmondson RJ, Wimberger P, Maenpaa J, Gaffney D, Zhang R, Okamoto A, Stuart G, Ochiai K, on behalf of the participants of the 5th Ovarian Cancer Consensus Conference. 5th ovarian cancer consensus conference of the gynecologic cancer InterGroup: recurrent disease. Ann Oncol. 2016;28(4):727–732. mdw663. https://doi.org/10.1093/annonc/mdw663.
Classe JM, Glehen O, Decullier E, et al. Cytoreductive surgery and Hyperthermic Intraperitoneal chemotherapy for first relapse of ovarian cancer. Anticancer Res. 2015;35(9):4997–5005.
Amate P, Huchon C, Dessapt AL, Bensaid C, Medioni J, Le Frère Belda MA, Bats AS, Lécuru FR. Ovarian cancer: sites of recurrence. Int J Gynecol Cancer. 2013;23(9):1590–6. https://doi.org/10.1097/IGC.0000000000000007.
Gadducci A, Cosio S. Surveillance of patients after initial treatment of ovarian cancer. Crit Rev Oncol Hematol. 2009;71:43–52.
Vaidya AP, Curtin JP. The follow-up of ovarian cancer. Semin Oncol. 2003;30:401–12.
Tanner EJ, Black DR, Zivanovic O, Kehoe SM, Dao F, Konner JA, Barakat RR, Lichtman SM, Levine DA. Patterns of first recurrence following adjuvant intraperitoneal chemotherapy for stage IIIC ovarian cancer. Gynecol Oncol. 2012;124(1):59–62. https://doi.org/10.1016/j.ygyno.2011.09.011. Epub 2011 Oct 7.
Ferrandina G, Legge F, Salutari V, Paglia A, Testa A, Scambia G. Impact of pattern of recurrence on clinical outcome of ovarian cancer patients: clinical considerations. Eur J Cancer. 2006;42(14):2296–302.
Chi DS, McCaughty K, Diaz JP, et al. Guidelines and selection criteria for secondary cytoreductive surgery in patients with recurrent, platinum-sensitive epithelial ovarian carcinoma. Cancer. 2006;106(9):1933.
Petrillo M, Pedone Anchora L, Tortorella L, Fanfani F, Gallotta V, Pacciani M, Scambia G, Fagotti A. Secondary cytoreductive surgery in patients with isolated platinum-resistant recurrent ovarian cancer: a retrospective analysis. Gynecol Oncol. 2014;134(2):257–61. https://doi.org/10.1016/j.ygyno.2014.05.029. Epub 2014 Jun 5.
Paik ES, Lee YY, Shim M, Choi HJ, Kim TJ, Choi CH, Lee JW, Kim BG, Bae DS. Timing and patterns of recurrence in epithelial ovarian cancer patients with no gross residual disease after primary debulking surgery. Aust N Z J Obstet Gynaecol. 2016;56(6):639–47. https://doi.org/10.1111/ajo.12529. Epub 2016 Sep 9.
Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol. 2002;20(5):1248–59.
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res. 1996;82:359–74.
Hoskins WJ, McGuire WP, Brady MF, et al. The effect of diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol. 1994;170:974–80.
Jänicke F, Hölscher M, Kuhn W, et al. Radical surgical procedure improves survival time in patients with recurrent ovarian cancer. Cancer. 1992;70(8):2129–36.
Segna RA, Dottino PR, Mandeli JP, Konsker K, Cohen CJ. Secondary cytoreduction for ovarian cancer following cisplatin therapy. J Clin Oncol. 1993;11(3):434–9.
Eisenkop SM, Friedman RL, Wang HJ. Secondary cytoreductive surgery for recurrent ovarian cancer. A prospective study. Cancer. 1995;76(9):1606–14.
Vaccarello L, Rubin SC, Vlamis V, et al. Cytoreductive surgery in ovarian carcinoma patients with a documented previously complete surgical response. Gynecol Oncol. 1995;57(1):61–5.
van de Laar R, Kruitwagen RF, IntHout J, Zusterzeel PL, Van Gorp T, Massuger LF. Surgery for recurrent epithelial ovarian cancer in the Netherlands: a population-based cohort study. Int J Gynecol Cancer. 2016;26(2):268–75.
Munkarah AR, Coleman RL. Critical evaluation of secondary cytoreduction in recurrent ovarian cancer. Gynecol Oncol. 2004;95:273–80.
Bristow RE, Puri I, Chi DS. Cytoreductive surgery for recurrent ovarian cancer: a meta-analysis. Gynecol Oncol. 2009;112:265–74.
Al Rawahi T, Lopes AD, Bristow RE, Bryant A, Elattar A, Chattopadhyay S, Galaal K. Surgical cytoreduction for recurrent epithelial ovarian cancer. Cochrane Database Syst Rev. 2013;2:CD008765. https://doi.org/10.1002/14651858.CD008765.pub3.
Bickell NA, Egorova N, Prasad-Hayes M, Franco R, Howell EA, Wisnivesky J, Deb P. Secondary surgery versus chemotherapy for recurrent ovarian cancer. Am J Clin Oncol. 2016.
Van De Laar R, Zusterzeel PLM, Van Gorp T, et al. Cytoreductive surgery followed by chemotherapy versus chemotherapy alone for recurrent platinum-sensitive epithelial ovarian cancer (SOCceR trial): a multicenter randomised controlled study. BMC Cancer. 2014;14:22. https://doi.org/10.1186/1471-2407-14-22.
Zang RY, Zhang ZY, Li ZT, et al. Effect of cytoreductive surgery on survival of patients with recurrent epithelial ovarian cancer. J Surg Oncol. 2000;75(1):24–30.
Onda T, Yoshikawa H, Yasugi T, Yamada M, Matsumoto K, Taketani Y. Secondary cytoreductive surgery for recurrent epithelial ovarian carcinoma: proposal for patient selection. Br J Cancer. 2005;92:1026–32.
Schorge J, McCann C, Del Carmen M. Surgical debulking of ovarian cancer: what difference does it make? Rev Obstet Gynecol. 2010;3(3):111–7.
Fotiou S, Aliki T, Petros Z, et al. Secondary cytoreductive surgery in patients presenting with isolated nodal recurrence of epithelial ovarian cancer. Gynecol Oncol. 2009;114:178–82.
Schorge JO, Wingo SN, Bhore R, et al. Secondary cytoreductive surgery for recurrent platinum-sensitive ovarian cancer. Int J Gynaecol Obstet. 2010;108:123–7.
Harter P, du Bois A, Hahmann M, et al. Surgery in recurrent ovarian cancer: the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) DESKTOP OVAR trial. Ann Surg Oncol. 2006;13:1702–10.
Harter P, Sehouli J, Reuss A, Hasenburg A, Scambia G, Cibula D, Mahner S, Vergote I, Reinthaller A, Burges A, Hanker L, Pölcher M, Kurzeder C, Canzler U, Petry KU, Obermair A, Petru E, Schmalfeldt B, Lorusso D, du Bois A. Prospective validation study of a predictive score for operability of recurrent ovarian cancer: the multicenter intergroup study DESKTOP II. A project of the AGO Kommission OVAR, AGO study group, NOGGO, AGO-Austria, and MITO. Int J Gynecol Cancer. 2011;21(2):289–95.
Janco JM, Kumar A, Weaver AL, McGree ME, Cliby WA. Performance of AGO score for secondary cytoreduction in a high-volume U.S. center. Gynecol Oncol. 2016;141(1):140–7. https://doi.org/10.1016/j.ygyno.2016.01.027. Epub 2016 Feb 2.
Musella A, Marchetti C, Palaia I, Perniola G, Giorgini M, Lecce F, Vertechy L, Iadarola R, De Felice F, Monti M, Muzii L, Angioli R, Panici PB. Secondary cytoreduction in platinum-resistant recurrent ovarian cancer: a single-institution experience. Ann Surg Oncol. 2015;22(13):4211–6. https://doi.org/10.1245/s10434-015-4523-2. Epub 2015 Mar 24.
Guarneri V, Barbieri E, Dieci MV, Piacentini F, Conte P. Timing for starting second-line therapy in recurrent ovarian cancer. Expert Rev Anticancer Ther. 2011;11(1):49–55. https://doi.org/10.1586/era.10.204.
Rustin GJ, van der Burg ME, Griffin CL. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): a randomised trial. Lancet. 2010;376:1155–63.
Tanner EJ, Chi DS, Eisenhauer EL, Diaz-Montes TP, Santillan A, Bristow RE. Surveillance for the detection of recurrent ovarian cancer: survival impact or lead-time bias? Gynecol Oncol. 2010;117(2):336–40. https://doi.org/10.1016/j.ygyno.2010.01.014. Epub 2010 Feb 12.
Gadducci A, Fuso L, Cosio S, Landoni F, Maggino T, Perotto S, et al. Are surveillance procedures of clinical benefit for patients treated for ovarian cancer? A retrospective Italian multicentric study. Int J Gynecol Cancer. 2009;19(3):367–74.
Ferrandina G, Sallustio G, Fagotti A, et al. Role of CT scan-based and clinical evaluation in the preoperative prediction of optimal cytoreduction in advanced ovarian cancer: a prospective trial. Br J Cancer. 2009;101(7):1066–73. https://doi.org/10.1038/sj.bjc.6605292.
Funt SA, Hricak H, Abu-Rustum N, Mazumdar M, Felderman H, Chi DS. Role of CT in the management of recurrent ovarian cancer. AJR Am J Roentgenol. 2004;182:393–8.
Eisenkop SM, Spirtos NM. What are the current surgical objectives, strategies, and technical capabilities of gynecologic oncologists treating advanced epithelial ovarian cancer. Gynecol Oncol. 2001;82:489–97.
Bristow RE, Duska LR, Lambrou NC, Fishman EK. A model for predicting surgical outcome in patients with advanced ovarian carcinoma using computed tomography. Cancer. 2000;89:1532–40.
Coakley FV, Choi PH, Gougoutas CA, et al. Peritoneal metastases: detection with spiral CT in patients with ovarian cancer. Radiology. 2002;223:495–9.
Esquivel J, Chua TC, Stojadinovic A, et al. Accuracy and clinical relevance of computed tomography scan interpretation of peritoneal cancer index in colorectal cancer peritoneal carcinomatosis: a multi-institutional study. J Surg Oncol. 2010;102:565–70.
Bristow RE, del Carmen MG, Pannu HK, et al. Clinically occult recurrent ovarian cancer: patient selection for secondary cytoreductive surgery using combined PET/CT. Gynecol Oncol. 2003;90(3):519–28.
Takekuma M, Maeda M, Ozawa T, Yasumi K, Torizuka T. Positron emission tomography with 18Fluoro-2-deoxyglucose for the detection of recurrent ovarian cancer. Int J Clin Oncol. 2005;10(3):177–81.
Simcock B, Neesham D, Quinn M, Drummond E, Milner A, Hicks RJ. The impact of PET/CT in the management of recurrent ovarian cancer. Gynecol Oncol. 2006;103:271–6.
Thrall MM, DeLoia JA, Gallion H, Avril N. Clinical use of combined positron emission tomography and computed tomography (FDG-PET/CT) in recurrent ovarian cancer. Gynecol Oncol. 2007;105:17–22.
Fulham MJ, Carter J, Baldey A, Hicks RJ, Ramshaw JE, Gibson M. The impact of PET-CT in suspected recurrent ovarian cancer: a prospective multi-centre study as part of the Australian PET data collection project. Gynecol Oncol. 2009;112(3):462–8.
Fagotti A, Fanfani F, Rossitto C, et al. A treatment selection protocol for recurrent ovarian cancer patients: the role of FDG-PET/CT and staging laparoscopy. Oncology. 2008;75(3–4):152–8.
Seshadri RA, Hemanth Raj E. Diagnostic laparoscopy in the pre-operative assessment of patients undergoing cytoreductive surgery and HIPEC for peritoneal surface malignancies. Ind J Surg Oncol. 2016;7:230. https://doi.org/10.1007/s13193-015-0486-9.
Fagotti A, Ferrandina G, Fanfani F, Ercoli A, Lorusso D, Rossi M, Scambia G. A laparoscopy-based score to predict surgical outcome in patients with advanced ovarian carcinoma: a pilot study. Ann Surg Oncol. 2006;13(8):1156–61.
Sugarbaker PH. Cytoreductive surgery and perioperative chemotherapy: textbook and video atlas. Connecticut: Cine-Med Publishing; 2013.
Magtibay PM, Adams PB, Silverman MB, Cha SS, Podratz KC. Splenectomy as part of cytoreductive surgery in ovarian cancer. Gynecol Oncol. 2006;102(2):369–74.
Bristow RE, Peiretti M, Gerardi M, et al. Secondary cytoreductive surgery including rectosigmoid colectomy for recurrent ovarian cancer: operative technique and clinical outcome. Gynecol Oncol. 2009;114(2):173–7.
Tamussino KF, Lim PC, Webb MJ, Lee RA, Lesnick TG. Gastrointestinal surgery in patients with ovarian cancer. Gynecol Oncol. 2001;80(1):79–84.
Mehta SS, Bhatt A, Glehen O. Cytoreductive surgery and peritonectomy procedures. Ind J Surg Oncol. 2016;7:139–51.
Burton E, Chase D, Yamamoto M, de Guzman J, Imagawa D, Berman ML. Surgical management of recurrent ovarian cancer: the advantage of collaborative surgical management and a multidisciplinary approach. Gynecol Oncol. 2011;120(1):29–32. https://doi.org/10.1016/j.ygyno.2010.10.008.
Bakrin N, Classe JM, Pomel C, et al. Hyperthermic intraperitoneal chemotherapy (HIPEC) in ovarian cancer. J Visc Surg. 2014;151(5):347–53. https://doi.org/10.1016/j.jviscsurg.2014.07.005.
Tay EH, Grant PT, Gebski V, Hacker NF. Secondary cytoreductive surgery for recurrent epithelial ovarian cancer. Obstet Gynecol. 2002;99(6):1008–13.
Raymond E, Drolet Y, Marpeau L, et al. Long-term follow-up after adjuvant chemotherapy in completely resected early stage ovarian carcinoma. Eur J Obstet Gynecol Reprod Biol. 1997;72:181–90.
Bristow RE, Zahurak ML, Alexander CJ, Zellars RC, Montz FJ. FIGO stage IIIC endometrial carcinoma: resection of macroscopic nodal disease and other determinants of survival. Int J Gynecol Cancer. 2003;13:664–72.
Uzan C, Morice P, Rey A, et al. Outcomes after combined therapy including surgical resection in patients with epithelial ovarian cancer recurrence(s) exclusively in lymph nodes. Ann Surg Oncol. 2004;11:658–64.
Benedetti Panici P, Perniola G, Angioli R, Zullo MA, Manci N, Palaia I, Bellati F, Plotti F, Calcagno M, Basile S. Bulky lymph node resection in patients with recurrent epithelial ovarian cancer: impact of surgery. Int J Gynecol Cancer. 2007;17(6):1245–51. Epub 2007 Apr 8.
Gasparri ML, Grandi G, Bolla D, Gloor B, Imboden S, Panici PB, Mueller MD, Papadia A. Hepatic resection during cytoreductive surgery for primary or recurrent epithelial ovarian cancer. J Cancer Res Clin Oncol. 2016;142(7):1509–20. https://doi.org/10.1007/s00432-015-2090-3.
Meredith MA, Cliby WA, Keeney GL, Lesnick TG, Nagorney DM, Podratz KC. Hepatic resection for metachronous metastases from ovarian carcinoma. Gynecol Oncol. 2003;89:16–21.
Yoon SS, Jarnagin WR, Fong Y, DeMatteo RP, Barakat RR, Blum- gart LH, Chi DS. Resection of recurrent ovarian or fallopian tube carcinoma involving the liver. Gynecol Oncol. 2003;91(2):383–8.
Loizzi V, Rossi C, Cormio G, Cazzolla A, Altomare D, Selvaggi L. Clinical features of hepatic metastasis in patients with ovarian cancer. Int J Gynecol Cancer. 2005;15(1):26–31.
Abood G, Bowen M, Potkul R, Aranha G, Shoup M. Hepatic resection for recurrent metastatic ovarian cancer. Am J Surg. 2008;195:370–3.
Pekmezci S, Saribeyoglu K, Aytac E, Arvas M, Demirkiran F, Ozguroglu M. Surgery for isolated liver metastasis of ovarian cancer. Asian J Surg. 2010;30(2):83–8.
Niu G, Shen C, Cui W, Li Q. Hepatic resection is safe for metachronous hepatic metastases from ovarian cancer. Cancer Biol Med. 2012;9:182–7.
Roh HJ, Kim DY, Joo WD, Yoo HJ, Kim JH, Kim YM, Kim YT, Nam JH. Hepatic resection as part of secondary cytoreductive surgery for recurrent ovarian cancer involving the liver. Arch Gynecol Obstet. 2011;284(5):1223–9.
Gallotta V, Fagotti A, Fanfani F, Ferrandina G, Nero C, Costantini B, Gueli Alletti S, Chiantera V, Ercoli A, Scambia G. Laparoscopic surgical management of localized recurrent ovarian cancer: a single-institution experience. Surg Endosc. 2014;28(6):1808–15. https://doi.org/10.1007/s00464-013-3390-9.
Trinh H, Ott C, Fanning J. Feasibility of laparoscopic debulking with electrosurgical loop excision procedure and argon beam coagulator at recurrence in patients with previous laparotomy debulking. Am J Obstet Gynecol. 2004;190:1394–7.
Nezhat FR, Denoble SM, Cho JE, Brown DN, Soto E, Chuang L, Gretz H, Saharia P. Safety and efficacy of video laparoscopic surgical debulking of recurrent ovarian, fallopian tube, and primary peritoneal cancers. J Soc Laparoendosc Surg. 2012;16:511–8.
Magrina JF, Cetta RL, Chang YH, Guevara G, Magtibay PM. Analysis of secondary cytoreduction for recurrent ovarian cancer by robotics, laparoscopy, and laparotomy. Gynecol Oncol. 2013;129:336–40.
Ceelen W. Intraperitoneal drug therapy for peritoneal carcinomatosis: state of the art. Proc Belg R Acad Med. 2014;3:61–88.
Alberts DS, Liu PY, Hannigan EV, et al. Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus intravenous cyclophosphamide for stage III ovarian cancer. N Engl J Med. 1996;335:1950–5.
Markman M, Bundy BN, Alberts DS, et al. Phase III trial of standard-dose intravenous cisplatin plus paclitaxel versus moderately high-dose carboplatin followed by intravenous paclitaxel and intraperitoneal cisplatin in small-volume stage III ovarian carcinoma: an intergroup study of the gynecologic oncology group, southwestern oncology group, and eastern cooperative oncology group. J Clin Oncol. 2001;19:1001–7.
Armstrong DK, Bundy B, Wenzel L, et al. Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med. 2006;354:34–43.
Elit L, Oliver TK, Covens A, Kwon J, Fung MK, Hirte HW, Oza AM. Intraperitoneal chemotherapy in the first-line treatment of women with stage III epithelial ovarian cancer: a systematic review with meta analyses. Cancer. 2007;109:692–702.
Yamamoto R, Fujimoto S. Complications relating to intraperitoneal administration of cisplatin or carboplatin for ovarian carcinoma. Gynecol Oncol. 2000;79:420–3.
Landrum LM, Gold MA, Moore KN, Myers TK, McMeekin DS, Walker JL. Intraperitoneal chemotherapy for patients with advanced epithelial ovarian cancer: a review of complications and completion rates. Gynecol Oncol. 2008;108:342–7.
Lan C, Li Y, Liu J. Intraperitoneal access via direct puncture is an alternative way to deliver intraperitoneal chemotherapy in ovarian, fallopian tube and primary peritoneal cancer. Gynecol Oncol. 2009;114:42–7.
Benedetti-Panici P, Perniola G, Marchetti C, Pernice M, Donfrancesco C, Di Donato V, Tomao F, Palaia I, Graziano M, Basile S, Bellati F. Intraperitoneal chemotherapy by ultrasound- guided direct puncture in recurrent ovarian cancer: feasibility, compliance, and complications. Int J Gynecol Cancer. 2012;22:1069–74.
Nicoletto MO, Casarin A, Baldoni A, et al. Intraperitoneal chemotherapy in patients pretreated for ovarian cancer matched with patients treated with parenteral chemotherapy. Anticancer Res. 2016;36(12):6541–6.
Chua TC, Moran BJ, Sugarbaker PH, et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol. 2012;30(11):2449–56.
Yan TD, Deraco M, Baratti D, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for malignant peritoneal mesothelioma: multi-institutional experience. J Clin Oncol. 2009;27:6237–42.
Elias D, Gilly F, Boutitie F, et al. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric French study. J Clin Oncol. 2010;28:63–8.
Verwaal VJ, Bruin S, Boot H, van Slooten G, van Tinteren H. 8-year follow-up of randomized trial: cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann Surg Oncol. 2008;15:2426–32.
Glehen O, Gilly FN, Arvieux C, et al. Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2010;17(9):2370–7.
Glehen O, Passot G, Villeneuve L, et al. GASTRICHIP: D2resection and hyperthermic intraperitoneal chemotherapy in locally advanced gastric carcinoma: a randomized and multi-center phase III study. BMC Cancer. 2014;14:183.
Hildebrandt B, Wust P, Ahlers O, Dieing A, Sreenivasa G, Kerner T, Felix R, Riess H. The cellular and molecular basis of hyperthermia. Crit Rev Oncol Hematol. 2002;43(1):33–56.
Raaphorst GP, Yang DP. The evaluation of thermal cisplatin sensitization in normal and XP human cells using mild hyperthermia at 40 and 41 degrees C. Anticancer Res. 2005;25(4):2649–53.
Pestieau SR, Belliveau JF, Griffin H, Stuart OA, Sugarbaker PH. Pharmacokinetics of intraperitoneal oxaliplatin: experimental studies. J Surg Oncol. 2001;76(2):106–14.
Jacquet P, Averbach A, Stuart OA, Chang D, Sugarbaker PH. Hyperthermic intraperitoneal doxorubicin: pharmacokinetics, metabolism, and tissue distribution in a rat model. Cancer Chemother Pharmacol. 1998;41(2):147–54.
Los G, Sminia P, Wondergem J, Mutsaers PHA, Havemen J, Huinink DT, Smals O, Gonzalezgonzalez D, Mcvie JG. Optimization of intraperitoneal cisplatin therapy with regional hyperthermia in rats. Eur J Cancer. 1991;27(4):472–7.
Elias DM, Ouellet JF. Intraperitoneal chemohyperthermia: rationale, technique, indications, and results. Surg Oncol Clin N Am. 2001;10(xi):915–33.
Cotte E, Colomban O, Guitton J, et al. Population pharmacokinetics and pharmacodynamics of cisplatinum during hyperthermic intraperitoneal chemotherapy using a closed abdominal procedure. J Clin Pharmacol. 2011;51(1):9–18.
Hetting VE, Lemstra W, Meijer C, et al. Mechanism of hyperthermic potentiation of cisplatin action in cisplatin sensitive and -resistant tumor cells. Br J Cancer. 1997;75:1735–43.
Hettinga VE. Reduction of cisplatin resistance by hyperthermia (PhD Thesis, Univ. of Groningen, ISBN 90-367-0648-3) (Printpartners Ipskamp bv, Enschede), 1996.
Hettinga JV, Konings AW, Kampinga HH. Reduction of cellular cisplatin resistance by hyperthermia — a review. Int J Hyperth. 1997;13:439–57.
van de Vaart PJ, van der Vange N, Zoetmulder FA, van Goethem AR, van Tellingen O, ten Bokkel Huinink WW, Beijnen JH, Bartelink H, Begg AC. Intraperitoneal cisplatin with regional hyperthermia in advanced ovarian cancer: pharmacokinetics and cisplatin-DNA adduct formation in patients and ovarian cancer cell lines. Eur J Cancer. 1998;34(1):148–54.
Gouy S, Ferron G, Glehen O, Bayar A, Marchal F, Pomel C, Quenet F, Bereder JM, Le Deley MC, Morice P. Results of a multicenter phase I dose-finding trial of hyperthermic intraperitoneal cisplatin after neoadjuvant chemotherapy and complete cytoreductive surgery and followed by maintenance bevacizumab in initially unresectable ovarian cancer. Gynecol Oncol. 2016;142(2):237–42. https://doi.org/10.1016/j.ygyno.2016.05.032. Epub 2016 Jun 2.
Zivanovic O, Abramian A, Kullmann M, Fuhrmann C, Coch C, Hoeller T, Ruehs H, Keyver-Paik MD, Rudlowski C, Weber S, Kiefer N, Poelcher ML, Thiesler T, Rostamzadeh B, Mallmann M, Schaefer N, Permantier M, Latten S, Kalff J, Thomale J, Jaehde U, Kuhn WC. HIPEC ROC I: a phase 1 study of cisplatin administered as hyperthermic intraoperative intraperitoneal chemoperfusion followed by postoperative intravenous platinum-based chemotherapy in patients with platinum-sensitive recurrent epithelial ovarian cancer. Int J Cancer. 2015;136:699–708. https://doi.org/10.1002/ijc.29011.
Fagotti A, Paris I, Grimolizzi F, et al. Secondary cytoreduction plus oxaliplatin-based HIPEC in platinum-sensitive recurrent ovarian cancer patients: a pilot study. Gynecol Oncol. 2009;113:335–40.
Ceelen WP, Van Nieuwenhove Y, Van Belle S, et al. Cytoreduction and hyperthermic intraperitoneal chemoperfusion in women with heavily pretreated recurrent ovarian cancer. Ann Surg Oncol. 2009;19(7):2352–9.
Frenel JS, Leux C, Pouplin L, Ferron G, Berton Rigaud D, Bourbouloux E, Dravet F, Jaffre I, Classe JM. Oxaliplatin-based hyperthermic intraperitoneal chemotherapy in primary or recurrent epithelial ovarian cancer: a pilot study of 31 patients. J Surg Oncol. 2011;103(1):10–6.
Elkas JC, Winter WE III, Chernofsky MR, et al. A phase I trial of oxaliplatin and topotecan in recurrent ovarian carcinoma. Gynecol Oncol. 2007;104:422–7.
Piccart MJ, Lacave AJ, Reed N, et al. Oxaliplatin or paclitaxel in patients with platinum-pretreated advanced ovarian cancer: a randomized phase II study of the European Organization for Research and Treatment of Cancer Gynecology Group. J Clin Oncol. 2000;18:1193–202.
Los G, van Vugt MJ, Pinedo HM. Response of peritoneal solid tumors after intraperitoneal chemohyperthermia treatment with cisplatin or carboplatin. Br J Cancer. 1994;69(2):235–41.
Jandial DD, Messer K, Farshchi-Heydari S, Pu M, Howell SB. Tumor platinum concentration following intraperitoneal administration of cisplatin versus carboplatin in an ovarian cancer model. Gynecol Oncol. 2009;115(3):362–6.
Xu MJ, Alberts DS. Potentiation of platinum analogue cytotoxicity by hyperthermia. Cancer Chemother Pharmacol. 1988;21:191–6.
Lentz SS, Miller BE, Kucera GL, Levine EA. Intraperitoneal hyperthermic chemotherapy using carboplatin: a phase I analysis in ovarian carcinoma. Gynecol Oncol. 2007;106(1):207–10. [21].
Steller MA, Egorin MJ, Trimble EL, Bartlett DL, Zuhowski EG, Alexander HR, et al. A pilot phase I trial of continuous hyperthermic peritoneal perfusion with high-dose carboplatin as primary treatment of patients with small-volume residual ovarian cancer. Cancer Chemother Pharmacol. 1999;43(2):106–14.
Argenta PA, Sueblinvong T, Geller MA, Jonson AL, Downs LS Jr, Carson LF, Ivy JJ, Judson PL. Hyperthermic intraperitoneal chemotherapy with carboplatin for optimally-cytoreduced, recurrent, platinum-sensitive ovarian carcinoma: a pilot study. Gynecol Oncol. 2013;129(1):81–5. https://doi.org/10.1016/j.ygyno.2013.01.010.
Ansaloni L, Coccolini F, Morosi L, et al. Pharmacokinetics of concomitant cisplatin and paclitaxel administered by hyperthermic intraperitoneal chemotherapy to patients with peritoneal carcinomatosis from epithelial ovarian cancer. Br J Cancer. 2015;112(2):306–12. https://doi.org/10.1038/bjc.2014.602.
Cascales-Campos PA, Gil J, Feliciangeli E, Gil E, González-Gil A, López V, Ruiz-Pardo J, Nieto A, Parrilla JJ, Parrilla P. The role of hyperthermic intraperitoneal chemotherapy using paclitaxel in platinum-sensitive recurrent epithelial ovarian cancer patients with microscopic residual disease after cytoreduction. Ann Surg Oncol. 2015;22(3):987–93. https://doi.org/10.1245/s10434-014-4049-z. Epub 2014 Sep 12.
de Bree E, Rosing H, Filis D, Romanos J, Melisssourgaki M, Daskalakis M, Pilatou M, Sanidas E, Taflampas P, Kalbakis K, Beijnen JH, Tsiftsis DD. Cytoreductive surgery and intraoperative hyperthermic intraperitoneal chemotherapy with paclitaxel: a clinical and pharmacokinetic study. Ann Surg Oncol. 2008;15:1183–92.
Cashin PH, Ehrsson H, Wallin I, Nygren P, Mahteme H. Pharmacokinetics of cisplatin during hyperthermic intraperitoneal treatment of peritoneal carcinomatosis. Eur J Clin Pharmacol. 2013;69:533–40.
Muller M, Chérel M, Dupré PF, Gouard S, Collet M, Classe JM. The cytotoxic effect of combined hyperthermia and taxane chemotherapy on ovarian cancer cells: results of an in vitro study. Eur Surg Res. 2012;48(2):55–63. https://doi.org/10.1159/000333393. Epub 2011 Dec 23.
Bijelic L, Sugarbaker PH, Stuarte O. Hyperthermic intraperitoneal chemotherapy with melphalan: a summary of clinical and pharmacological data in 34 patients. Gastroenterol Res Pract. 2012;2012:827534.
Sardi A, Jimenez W, Nieroda C, Sittig M, Shankar S, Gushchin V. Melphalan: a promising agent in patients undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2014;21(3):908–14. https://doi.org/10.1245/s10434-013-3407-6. Epub 2013 Nov 26.
Bhangu A, Broom L, Nepogodiev D, Gourevitch D, Desai A. Outcomes of isolated limb perfusion in the treatment of extremity soft tissue sarcoma: a systematic review. Eur J Surg Oncol. 2013;39(4):311–9.
Raymond AK, Beasley GM, Broadwater G, et al. Current trends in regional therapy for melanoma: lessons learned from 225 regional chemotherapy treatments between 1995 and 2010 at a single institution. J Am Coll Surg. 2011;213(2):306–16.
Urano M, Ling CC. Thermal enhancement of melphalan and oxaliplatin cytotoxicity in vitro. Int J Hyperth. 2002;18(4):307–15.
Sugarbaker PH, Stuart OA. Pharmacokinetic and phase II study of heated intraoperative intraperitoneal melphalan. Cancer Chemother Pharmacol. 2007;59(2):151–5.
Mohamed F, Stuart OA, Glehen O, Urano M, Sugarbaker PH. Optimizing the factors which modify thermal enhancement of melphalan in a spontaneous murine tumor. Cancer Chemother Pharmacol. 2006;58(6):719–24.
Glehen O, Stuart OA, Mohamed F, Sugarbaker PH. Hyperthermia modifies pharmacokinetics and tissue distribution of intraperitoneal melphalan in a rat model. Cancer Chemother Pharmacol. 2004;54(1):79–84.
Helm CW, Richard SD, Pan J, Bartlett D, Goodman MD, Hoefer R, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer first report of the HYPER-O registry. Int J Gynecol Cancer. 2010;20:61–9.
Van der Speeten K, Stuart OA, Mahteme H, Sugarbaker PH. Pharmacokinetic study of perioperative intravenous Ifosfamide. Int J Surg Oncol. 2011;2011:185092. https://doi.org/10.1155/2011/185092. Epub 2011 Sep 21.
Deraco M, Baratti D, Cabras AD, et al. Experience with peritoneal mesothelioma at the Milan National Cancer Institute. World J Gastrointest Oncol. 2010;2(2):76–84. https://doi.org/10.4251/wjgo.v2.i2.76.
Sugarbaker PH, Stuart OA, Bijelic L. Intraperitoneal gemcitabine chemotherapy treatment for patients with resected pancreatic cancer: rationale and report of early data. Int J Surg Oncol. 2011;2011:161862. https://doi.org/10.1155/2011/161862.
Mulier S, Claes JP, Dierieck V, Amiel JO, Pahaut JP, Marcelis L, Bastin F. Survival benefit of adding hyperthermic IntraPEritoneal chemotherapy (HIPEC) at the different time-points of treatment of ovarian cancer: review of evidence. Curr Pharm Des. 2012;18:3793–803.
Cowan RA, O’Cearbhaill RE, Zivanovic O, Chi DS. Current status and future prospects of Hyperthermic Intraoperative Intraperitoneal Chemotherapy (HIPEC) clinical trials in ovarian cancer. Int J Hyperth. 2017;16:1–21. https://doi.org/10.1080/02656736.2017.1283066.
Bhatt A, Glehen O. The role of cytoreductive surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) in ovarian cancer: a review. Ind J Surg Oncol. 2016;7(2):188–97. https://doi.org/10.1007/s13193-016-0501-9. Epub 2016 Feb 16.
van der Vange N, van Goethem AR, Zoetmulder FAN, et al. Extensive cytoreductive surgery combined with cisplatin under hyperthermic conditions (OVHIPEC) in patients with recurrent ovarian cancer: a feasibility pilot. Eur J Surg Oncol. 2000;26:663–8.
Zanon C, Clara R, Chiappino I, et al. Cytoreductive surgery and intraperitoneal chemohyperthermia for recurrent peritoneal carcinomatosis from ovarian cancer. World J Surg. 2004;28:1040–5.
Piso P, Dahlke MH, Loss M, Schlitt HJ. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in peritoneal carcinomatosis from ovarian cancer. World J Surg Oncol. 2004;2:21.
Rufián S, Muñoz-Casares FC, Briceño J, et al. Radical surgery peritonectomy and intraoperative intraperitoneal chemotherapy for the treatment of peritoneal carcinomatosis in recurrent or primary ovarian cancer. J Surg Oncol. 2006;94:316–24.
Cotte E, Glehen O, Mohamed F, et al. Cytoreductive surgery and intraperitoneal chemohyperthermia for chemoresistant and recurrent advanced epithelial ovarian cancer: prospective study of 81 patients. World J Surg. 2007;31:1813–20.
Di Giorgio A, Naticchioni E, Biacchi D, et al. Cytoreductive surgery (peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of diffuse peritoneal carcinomatosis from ovarian cancer. Cancer. 2008;113(2):315–25.
Pavlov MJ, Kovacevic PA, Ceranic MS, Stamenkovic AB, Ivanovic AM, Kecmanovic DM. Cytoreductive surgery and modified heated intraoperative intraperitoneal chemotherapy (HIPEC) for advanced and recurrent ovarian cancer - 12-year single center experience. Eur J Surg Oncol. 2009;35(11):1186–91.
Carrabin N, Mithieux F, Meeus P, et al. Hyperthermic intraperitoneal chemotherapy with oxaliplatin and without adjuvant chemotherapy in stage IIIC ovarian cancer. Bull Cancer. 2010;97(4):E23–32.
Roviello F, Pinto E, Corso G, et al. Safety and potential benefit of hyperthermic intraperitoneal chemotherapy (HIPEC) in peritoneal carcinomatosis from primary or recurrent ovarian cancer. J Surg Oncol. 2010;102(6):663–70.
Königsrainer I, Beckert S, Becker S, et al. Cytoreductive surgery and HIPEC in peritoneal recurrent ovarian cancer: experience and lessons learned. Langenbeck’s Arch Surg. 2011;396(7):1077–81.
Bakrin N, Bereder JM, Decullier E, et al. Peritoneal carcinomatosis treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) for advanced ovarian carcinoma: a French multicentre retrospective cohort study of566 patients. Eur J Surg Oncol. 2013;39:1435–43.
Königsrainer I, Horvath P, Struller F, Grischke EM, Wallwiener D, Königsrainer A, Beckert S. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in recurrent epithelial ovarian cancer with peritoneal metastases: a single centre experience. Langenbeck’s Arch Surg. 2014;399(5):589–94. https://doi.org/10.1007/s00423-014-1207-5.
Massari R, Barone M, Basilico R, Carella C, Colasante A, De Tursi M, Filippone A, Guetti L, Mani A. Peritonectomy and hyperthermic chemotherapy in patients with advanced or recurrent epithelial ovarian cancer: a single center cohort study. Minerva Chir. 2014;69(1):17–26.
Coccolini F, Campanati L, Catena F, et al. Hyperthermic intraperitoneal chemotherapy with cisplatin and paclitaxel in advanced ovarian cancer: a multicenter prospective observational study. J Gynecol Oncol. 2015;26(1):54–61. https://doi.org/10.3802/jgo.2015.26.1.54.
Boisen MM, Richard SD, Holtzman MP, et al. Hyperthermic intraperitoneal chemotherapy for epithelial ovarian cancers: is there a role? J Gastrointest Oncol. 2016;7(1):10–7. https://doi.org/10.3978/j.issn.2078-6891.2015.103.
Petrillo M, De Iaco P, Cianci S, Perrone M, Costantini B, Ronsini C, Scambia G, Fagotti A. Long-term survival for platinum-sensitive recurrent ovarian cancer patients treated with secondary cytoreductive surgery plus Hyperthermic Intraperitoneal Chemotherapy (HIPEC). Ann Surg Oncol. 2016;23(5):1660–5. https://doi.org/10.1245/s10434-015-5050-x. Epub 2015 Dec 29.
Cripe J, Tseng J, Eskander R, Fader AN, Tanner E, Bristow R. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for recurrent ovarian carcinoma: analysis of 30-day morbidity and mortality. Ann Surg Oncol. 2015;22(2):655–61. https://doi.org/10.1245/s10434-014-4026-6. Epub 2014 Aug 26.
Armstrong DK, White AJ, Weil SC, Phillips M, Coleman RL. Farletuzumab (a monoclonal antibody against folate receptor alpha) in relapsed platinum-sensitive ovarian cancer. Gynecol Oncol. 2013;129:452–8.
Harrison ML, Gore ME, Spriggs D, Kaye S, Iasonos A, Hensley M, et al. Duration of second or greater complete clinical remission in ovarian cancer: exploring potential endpoints for clinical trials. Gynecol Oncol. 2007;106:469–75.
Huo YR, Richards A, Liauw W, Morris DL. Hyperthermic intraperitoneal chemotherapy (HIPEC) and cytoreductive surgery (CRS) in ovarian cancer: a systematic review and meta-analysis. Eur J Surg Oncol. 2015;41(12):1578–89. https://doi.org/10.1016/j.ejso.2015.08.172.
Munoz-Casares FC, Rufian S, Rubio MJ, et al. The role of hyper-thermic intraoperative intraperitoneal chemotherapy (HIPEC) in the treatment of peritoneal carcinomatosis in recurrent ovarian cancer. Clin Transl Oncol. 2009;11:753–9.
Spiliotis J, Vaxevanidou A, Sergouniotis F, Lambropoulou E, Datsis A, Christopoulou A. The role of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in the management of recurrent advanced ovarian cancer: a prospective study. J BUON. 2011;16:74–9.
Fagotti A, Costantini B, Petrillo M, et al. Cytoreductive surgery plus HIPEC in platinum-sensitive recurrent ovarian cancer patients: a case-control study on survival in patients with two-year follow-up. Gynecol Oncol. 2012;127:502–5.
Le Brun JF, Campion L, Berton-Rigaud D, Lorimier G, Marchal F, Ferron G, Oger AS, Dravet F, Jaffre I, Classe JM. Survival benefit of hyperthermic intraperitoneal chemotherapy for recurrent ovarian cancer: a multi-institutional case control study. Ann Surg Oncol. 2014;21(11):3621–7. https://doi.org/10.1245/s10434-014-3693-7.
Baiocchi G, Ferreira FO, Mantoan H, da Costa AA, Faloppa CC, Kumagai LY, de Mello CA, Takahashi RM, Nakagawa WT, Aguiar S Jr, Lopes A. Hyperthermic intraperitoneal chemotherapy after secondary cytoreduction in epithelial ovarian cancer: a single-center comparative analysis. Ann Surg Oncol. 2016;23(4):1294–301. https://doi.org/10.1245/s10434-015-4991-4. Epub 2015 Dec 1.
Safra T, Grisaru D, Inbar M, Abu-Abeid S, Dayan D, Matceyevsky D, Weizman A, Klausner JM. Cytoreduction surgery with hyperthermic intraperitoneal chemotherapy in recurrent ovarian cancer improves progression-free survival, especially in BRCA-positive patients- a case-control study. J Surg Oncol. 2014;110(6):661–5. https://doi.org/10.1002/jso.23688. Epub 2014 Jun 24.
Lim MC, Kang S, Choi J, Song YJ, Park S, Seo SS, Park SY. Hyperthermic intraperitoneal chemotherapy after extensive cytoreductive surgery in patients with primary advanced epithelial ovarian cancer: interim analysis of a phase II study. Ann Surg Oncol. 2009;16(4):993–1000. https://doi.org/10.1245/s10434-008-0299-y. Epub 2009 Jan 24.
Gremonprez F, Willaert W, Ceelen W. Intraperitoneal chemotherapy (IPC) for peritoneal carcinomatosis: review of animal models. J Surg Oncol. 2014;109(2):110–6. https://doi.org/10.1002/jso.23464. Review.
Gerestein CG, Damhuis RA, de Vries M, Reedijk A, Burger CW, Kooi GS. Causes of postoperative mortality after surgery for ovarian cancer. Eur J Cancer. 2009;45:2799–803.
Chua TC, Yan TD, Saxena A, Morris DL. Should the treatment of peritoneal carcinomatosis by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy still be regarded as a highly morbid procedure? A systematic review of morbidity and mortality. Ann Surg. 2009;249:900–7.
Wright JD, Ananth CV, Ojalvo L, Herzog TJ, Lewin SN, Lu YS, Neugut AI, Hershman DL. Failure to rescue after major gynecologic surgery. Am J Obstet Gynecol. 2013;209(420):e1–8.
Leitao MM Jr, Kardos S, Barakat RR, Chi DS. Tertiary cytoreduction in patients with recurrent ovarian carcinoma. Gynecol Oncol. 2004;95:181–8.
Shih KK, Chi DS, Barakat RR, Leitao MM Jr. Tertiary cytoreduction in patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer: an updated series. Gynecol Oncol. 2010;117:330–5.
Karam AK, Santillan A, Bristow RE, et al. Tertiary cytoreductive surgery in recurrent ovarian cancer: selection criteria and survival outcome. Gynecol Oncol. 2007;104:377–80.
Gultekin M, Velipaşaoğlu M, Aksan G, et al. A third evaluation of tertiary cytoreduction. J Surg Oncol. 2008;98:530–4.
Tang J, Liu DL, Shu S, Tian WJ, Liu Y, Zang RY. Outcomes and patterns of secondary relapse in platinum-sensitive ovarian cancer: implications for tertiary cytoreductive surgery. Eur J Surg Oncol. 2013;39(7):786–91. https://doi.org/10.1016/j.ejso.2013.02.006. Epub 2013 Mar 13.
Fotopoulou C, Richter R, Braicu IE, et al. Clinical outcome of tertiary surgical cytoreduction in patients with recurrent epithelial ovarian cancer. Ann Surg Oncol. 2011;18:49–57.A.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Bhatt, A., Bakrin, N., Glehen, O. (2018). Surgical Management of Recurrent Epithelial Ovarian Cancer. In: Bhatt, A. (eds) Management of Peritoneal Metastases- Cytoreductive Surgery, HIPEC and Beyond. Springer, Singapore. https://doi.org/10.1007/978-981-10-7053-2_11
Download citation
DOI: https://doi.org/10.1007/978-981-10-7053-2_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-7052-5
Online ISBN: 978-981-10-7053-2
eBook Packages: MedicineMedicine (R0)