Abstract
Background
This investigation aims to assess morbidity, mortality and postoperative outcomes of cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) in recurrent epithelial ovarian cancer (REOC) with peritoneal metastases (PM).
Methods
Consecutive patients with radiographic evidence of REOC with PM were scheduled for CRS and HIPEC at the Comprehensive Cancer Center, University Hospital Tübingen, Germany. Clinical data were retrospectively analyzed.
Results
In total, 90 patients were analyzed. Complete cytoreduction and HIPEC could be performed in 69 % of patients. When categorizing patients with respect to the completeness of cytoreduction (CC-0/1 vs CC-2/3), there was no difference considering baseline demographic characteristics. Cumulative morbidity was 42 %. Morbidity rates did not statistically differ between CC-0/1 patients with HIPEC and CC-2/3 patients without HIPEC. No surgery-related and 90-day postoperative mortality was observed. In CC-0/1 patients, median overall survival was 35 months as opposed to 14 months in CC-2/3 patients. There was no difference in survival with respect to the peritoneal carcinomatosis index (PCI) as long as complete cytoreduction could be achieved.
Conclusions
CRS and HIPEC can be performed with acceptable morbidity and low mortality in specialized centres. Our data do not suggest that HIPEC necessarily increases the risk of postoperative adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recurrent epithelial ovarian cancer (REOC) occurs in about 70 % after primary treatment consisting of radical surgical resection and platin-based systemic chemotherapy. Treatment protocols at this point of the disease are mainly based on palliative chemotherapy [1–3].
An alternative approach is repetitive surgery which is up to now restricted to clinically symptomatic patients. In patients with REOC and peritoneal metastases (PM), secondary radical surgery, however, provided a similar outcome compared with patients suffering from recurrent disease without PM as long as complete cytoreduction could be achieved. Moreover, in this particular patient population, survival was mainly dependent on the completeness of cytoreduction [4, 5] supporting again the pivotal role of radical surgery in the treatment of REOC.
It remains unclear, however, whether simultaneous hyperthermic intraperitoneal chemotherapy as adjunct to radical surgery could further improve prognosis in REOC. In prospective trials, normothermic intraperitoneal chemotherapy has already shown promising results prolonging overall survival in primary advanced ovarian cancer [6–8].
Radical cytoreductive surgery (CRS) along with hyperthermic intraperitoneal chemotherapy (HIPEC) revolutionized treatment in various stage IV cancers [9, 10]. There is a growing body of retrospective data favourizing this multimodal strategy [11–17] also in epithelial ovarian cancer even though it is still discussed controversially. At least in Germany, many gynaecological oncologists discourage from using CRS and HIPEC outside of well-designed, prospective and controlled clinical trials claiming this multimodal procedure to be associated with increased morbidity in particular due to the HIPEC itself [18]. Recently, several prospective trials in primary and recurrent ovarian cancer have been set up to evaluate the beneficial effect of HIPEC (www.clinicaltrials.gov).
The objective of our retrospective analysis was to evaluate morbidity, mortality and postoperative outcomes of CRS and HIPEC in REOC with PM.
Patients and methods
Patient selection
Between February 2007 and June 2012, 90 consecutive patients with REOC and PM were enrolled in the Peritoneal Surface Malignancy Program at the University of Tübingen, Germany. Preoperative diagnostics consisted of a clinical examination, blood test and CT scan and laparoscopy in some cases to rule out distant metastases and local irresectability, i.e. infiltration of the mesenteric axis, retroperitoneum or diffuse extensive tumour growth on the entire small bowel surface. Eligibility for CRS and HIPEC was assessed by a surgical oncologist, a gynaecological oncologist, a radiologist and a clinical pathologist attending a weekly interdisciplinary oncologic team meeting presenting patient demographics and imaging results.
Patients were retrospectively categorized into two groups with respect to the completeness of cytoreduction (CC-0/1 vs CC-2/3).
Surgical procedure
After laparotomy through a midline incision, complete adhesiolysis and exploration of the entire abdominal cavity, the peritoneal carcinomatosis index (PCI) was determined following the criteria described by Sugarbaker et al. [19, 20].
If PM were interpreted to be potentially resectable, cytoreductive surgery was started aiming for complete cytoreduction (CC-0, CC-1; CC-0 meaning no visible disease; CC-1 meaning nodules smaller than 0.25 cm).
After complete cytoreduction and fashioning of intestinal anastomoses, if necessary, HIPEC with cisplatin 50 mg/m2 for 90 min at 42 °C using the open coliseum technique was administered.
Postoperative morbidity and mortality
Adverse events were categorized according to the Clavien-Dindo (CD) complication score [21]. Grade 1 was defined as any deviation from the normal postoperative course, and grade 2 required pharmacological treatment. In grade 3 complications, there was a need for radiological, endoscopic or surgical intervention. Life-threatening complications were classified as grade 4 and death as grade 5. Surgery-related mortality was defined as death within 30 days of surgery. Overall complication rate was defined as the percentage of patients developing as least one CD I-V adverse event within the postoperative period.
Statistics
Data are presented as median (min-max) or n (%) unless otherwise stated. Qualitative differences were compared using Χ 2 test and quantitative differences using Mann-Whitney U test. Survival analysis was performed by the Kaplan-Meier method. For overall survival (OS), time to event was calculated as time from cytoreductive surgery until death or time to last contact, if the patient was alive. Recurrence was calculated from the date of surgery to disease relapse or to the last known date of follow-up evaluation or date of death using the Kaplan-Meier method. A p value less than 0.05 was considered significant. SPSS version 13.0 software (SPSS, Chicago, Illinois, USA) was used for all statistical analysis.
Results
Operative outcomes
A total of 90 patients were scheduled to cytoreductive surgery and HIPEC when there was evidence of peritoneal disease without signs of irresectability. Complete cytoreduction and HIPEC could be performed in 62 patients (69 %) (CC-0 47 patients (52 %), CC-1 15 patients (17 %)), whereas in 5 patients (6 %), residual tumour volume was greater than 0.25 cm (CC-2) located either in the hepatoduodenal ligament or the mesenteric axis. Twenty-three patients (25 %) only underwent explorative laparotomy or tumour debulking either due to retraction of the mesenteric axis or diffuse extensive tumour growth on the entire small bowel surface. Eight of these 23 patients (35 %) have been operated on for symptomatic bowel obstruction or to prevent mechanical ileus.
Patients were retrospectively categorized with respect to the completeness of cytoreduction (CC-0/1 vs CC-2/3). Both groups were comparable for baseline demographic characteristics except intra-abdominal tumour load (PCI), time in operating room and postoperative hospital stay (Table 1).
Types of visceral resections are shown in Table 2. Patients with complete cytoreduction received more visceral resections as opposed to patients with incomplete cytoreductive surgery. In particular, there was a higher incidence of rectosigmoid resection, greater omentectomy, diaphragma resection and splenectomy. In total, an ostomy had to be created in seven patients.
Morbidity and mortality
Thirty-eight patients suffered from postoperative adverse events resulting in an overall complication rate (Clavien-Dindo I-V) of 42 %. There was no significant difference in morbidity rates between CC-0/1 and CC-2/3 patients (28 patients (45 %) vs 10 patients (36 %); p = 0,254) even though there was a trend to a higher frequency of CD ≥3 adverse events in the CC-0/1 group (p = 0.086). Re-laparotomy had to be performed in nine patients (15 %) in the CC-0/1 as opposed to one patient (4 %) in the CC-2/3 group. Following complete cytoreduction and HIPEC, four patients (6 %) suffered from postoperative pneumonia and seven patients (11 %) from pulmonary embolism, whereas these adverse events were not observed after exploratory laparotomy (Table 3).
There was no surgery-related and 90-day postoperative mortality.
Survival
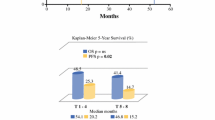
Median follow-up was 19 months [2–62]. In patients with complete cytoreduction (CC-0/1), median overall survival was calculated to 35 months (95 % CI 23–46) as opposed to 14 months (95 % CI 4–25) in patients with incomplete cytoreduction (CC-2/3) (Fig. 1a). In addition, there was no difference in survival with respect to PCI as long as complete cytoreduction could be achieved (Fig. 1b).
Discussion
CRS and HIPEC are a multimodal treatment strategy for intra-abdominal tumour spread without organ metastases or extra-abdominal seedings currently utilized for various gastrointestinal cancers especially colorectal cancer [9, 10]. This therapy protocol is based on the rationale that the peritoneal surface compartment is considered a natural barrier against systemic tumour spread limiting tumour growth to the peritoneal cavity. While radical surgery is intended for eliminating macroscopic disease, HIPEC is supposed to erase non-visible remaining tumour or free tumour cells.
Standard of care for recurrent ovarian cancer with PM, so far, is palliative systemic chemotherapy, whereas surgery is only considered in case of mechanical bowel obstruction. The multicentre DESKTOP I trial for recurrent ovarian cancer, however, suggested radical debulking surgery as preferable treatment strategy as long as complete cytoreduction can be achieved [4, 5].
Since phase III trials are not available, HIPEC is still considered as “experimental” in ovarian cancer and is restricted to selected individual cases or interventional institutional studies [11–17]. Some gynaecological oncologists argue that HIPEC itself causes major morbidity postponing systemic chemotherapy in case of severe postoperative adverse events. In our series, overall morbidity was 42 % which is accordance to the current literature where morbidity ranges between 20 and 66 %, mainly due to the extent of surgery [11, 12, 14, 22]. Even though our re-operation rate was 15 %, there was neither surgery-related death nor any patient died within 90 days from surgery. Interestingly, there was no significant difference in the overall cumulative complication rate between patients who underwent radical cytoreductive surgery plus HIPEC compared with those who did not even though visceral resections were much more frequent in the CC-0/1 group. The trend to a higher frequency of Clavien-Dindo ≥3 adverse events is more likely related to the extent of surgery rather than the HIPEC procedure itself. Despite of numerous visceral resections, ostomy had to be created in only six patients (10 %).
Four patients (6 %) developed transient leucopenia (<2,000/μl) following HIPEC which resolved spontaneously with no need for granulocyte colony-stimulating factors. In addition, we did not find more infectious complications such as surgical site infections following HIPEC. HIPEC itself—at least according to our data—does not seem to necessarily increase morbidity not allowing early postoperative chemotherapy.
We found a median overall survival of 35 months (95 % CI 23–46) in patients with complete cytoreduction plus HIPEC as opposed to 14 months (95 % CI 4–25) in patients with incomplete cytoreduction (CC-2/3). Recently, Bakrin et al. demonstrated a 45.7-month overall survival in a French retrospective multicentre cohort study [11]. Median overall survival for chemotherapy alone in EORC was reported to be as high as 29 months [1] or 18 months [2]. It remains unclear, however, how many patients suffered from PM in these particular investigations. In the DESKTOP I trial, Harter et al. reported a median overall survival of 19.9 months following cytoreductive surgery without additional HIPEC in patients suffering from REOC with PM. In this study, however, complete cytoreduction could only be achieved in 26 % of patients [4, 5]. Those particular patients showed a significant increase in overall survival with a 2-year survival rate of 77 % even without additional HIPEC. Compared with our study, however, PM were defined as present according to the surgical report [5] without any quantification by PCI, and the extent of surgery for achieving complete cytoreduction was not reported. In addition, approximately 90 % of patients received postoperative chemotherapy which has been proven by the authors as an independent prognostic factor by multivariate analysis [4].
In summary, complete cytoreduction seems to be the major prognostic factor in REOC for long-term outcome [4, 5]. Even in primary ovarian cancer, progression-free and overall survivals were dependent on surgical radicalness and could be prolonged by more radical surgery exploring the entire abdominal cavity [23].
In our series, we were able to achieve complete cytoreduction in 69 % of the patients. However, we did not find appropriate clinical selection criteria to anticipate the probability of complete cytoreduction. Selecting these particular patients in whom complete cytoreduction is likely to be achieved remains a major challenge for the future.
Interestingly, PCI did not impact survival in our series as long as complete cytoreduction could be achieved. This is in discordance to a recently published multicentre paper where Bakrin et al. observed that patients with a PCI ≤8 had a significant better survival than patients with a PCI >8. However, the percentage of “incomplete cytoreduction” in the PCI >8 group is not documented and may lead to bias in this study. Therefore, at least in our opinion, we should not a priori exclude patients with high intra-abdominal tumour load from the opportunity of radical cytoreductive surgery.
Most importantly, patients should be treated by surgeons and gynaecological oncologists who are familiar with cytoreductive/visceral surgery in specialized centres. In order to reduce morbidity, we prefer an organ-preserving approach rather than radical organ resections. Recently, our group was able to demonstrate that colon-preserving surgery along with meticulous “cleaning” of the bowel instead of colectomy in REOC can keep morbidity down at an acceptable level [24].
Due to the retrospective evaluation of our experience, however, our results have to be interpreted with caution, and as previously mentioned, the beneficial effect of HIPEC remains to be proven. However, our series is one of the largest single centre reports on REOC showing again that this multimodal option can be offered in patients with acceptable morbidity.
Pushing surgical efforts seem to result in favourable survival data, and organ-preserving surgery may diminish morbidity. The impact of HIPEC on non-visible disease remains to be evaluated in prospective trials. We are urgently awaiting the results of the CHIPOR study [25]. This randomized controlled phase III compares cytoreductive surgery and HIPEC to cytoreductive surgery alone with respect to overall survival. In addition, preoperative neoadjuvant chemotherapy using either carboplatin-paclitaxel or carboplatin-caelyx is performed in both arms testing the hypothesis that adjunction of HIPEC in REOC is able to improve the median overall survival by 12 months.
References
Parmar MK, Ledermann JA, Colombo N, du Bois A, Delaloye JF, Kristensen GB, Wheeler S, Swart AM, Qian W, Torri V, Floriani I, Jayson G, Lamont A, Tropé C, CON, AGO Collaborators (2003) Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: the ICON4/AGO-OVAR-2.2 trial. Lancet 361:2099–2106
Pfisterer J, Plante M, Vergote I, du Bois A, Hirte H, Lacave AJ, Wagner U, Stähle A, Stuart G, Kimmig R, Olbricht S, Le T, Emerich J, Kuhn W, Bentley J, Jackisch C, Lück HJ, Rochon J, Zimmermann AH, Eisenhauer E (2006) Gemcitabine plus carboplatin compared with carboplatin in patients with platinum-sensitive recurrent ovarian cancer: an intergroup trial of the AGO-OVAR, the NCIC CTG, and the EORTC GCG. J Clin Oncol 24:4699–4707
Hennessy BT, Coleman RL, Markman M (2009) Ovarian cancer. Lancet 374:1371–1382
Harter P, du Bois A, Hahmann M, Hasenburg A, Burges A, Loibl S et al (2006) Surgery in recurrent ovarian cancer: the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) DESKTOP OVAR trial. Ann Surg Oncol 13:1702–1710
Harter P, Hahmann M, Lueck HJ, Poelcher M, Wimberger P, Ortmann O et al (2009) Surgery for recurrent ovarian cancer: role of peritoneal carcinomatosis: exploratory analysis of the DESKTOP I trial about risk factors, surgical implications, and prognostic value of peritoneal carcinomatosis. Ann Surg Oncol 16:1324–1330
Alberts DS, Liu PY, Hannigan EV, O’Toole R, Williams SD, Young JA et al (1996) Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus inrtavenous cyclophosphamide for stage III ovarian cancer. N Engl J Med 335:1950–1955
Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S et al (2006) Intraperitoneal cisplatin and paclitaxel in ovarian cancer. N Engl J Med 354:34–43
Jaaback K, Johnson N, Lawrie TA (2011) Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer. Cochrane Database Syst Rev.; 9;(11)
Verwaal VJ, van Ruth S, de Bree E, van Sloothen GW, van Tinteren H, Boot H et al (2003) Randomized trial of cytoreduction and hyperthermic intraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. J Clin Oncol 21:3737–3743
Elias D, Gilly F, Boutitie F, Quenet F, Bereder JM, Mansvelt B et al (2010) Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy: retrospective analysis of 523 patients from a multicentric french study. J Clin Oncol 28:63–68
Bakrin N, Bereder JM, Decullier E et al (2013) Peritoneal carcinomatosis treated with cytoreductive surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) for advanced ovarian carcinoma: a French multicentre retrospective cohort study of 566 patients. Eur J Surg Oncol 39:1435–1443
Helm CW (2009) The role of hyperthermic intraperitoneal chemotherapy (HIPEC) in ovarian cancer. Oncologist 14:683–694
Piso P, Dahlke MH, Loss M, Schlitt HJ (2004) Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in peritoneal carcinomatosis from ovarian cancer. World J Surg Oncol 2:21
Di Giorgio A, Naticchioni E, Biacchi D, Sibio S, Accarpio F, Rocco M et al (2008) Cytoreductive surgery (peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in the treatment of diffuse peritoneal carcinomatosis from ovarian cancer. Cancer 113:315–325
Helm CW, Randall-Whitis L, Martin RS III, Metzinger DS, Gordinier ME, Parker LP et al (2007) Hyperthermic intraperitoneal chemotherapy in conjunction with surgery for the treatment of recurrent ovarian carcinoma. Gynecol Oncol 105:90–96
Spiliotis J, Vaxevanidou A, Sergouniotis F, Lambropoulou E, Datsis A, Christopoulou A (2011) The role of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in the management of recurrent advanced ovarian cancer: a prospective study. J BUON 16:74–79
Chua TC, Liauw W, Robertson G, Chia WK, Soo KC, Alobaid A et al (2009) Towards randomized trials of cytoreductive surgery using peritonectomy and hyperthermic intraperitoneal chemotherapy for ovarian cancer peritoneal carcinomatosis. Gynecol Oncol 114:137–139
Harter P, Mahner S, Hilpert F, Runnebaum I, Ortmann O, Mustea A, Sehouli J, du Bois A, Wagner U (2013) Statement by the Kommission OVAR of the AGO study group on the use of HIPEC to treat primary and recurrent ovarian cancer. Geburtsh Frauenheilk 73:221–223
Jaquet P, Sugarbaker PH (1996) Current methodologies for clinical assessment of patients with peritoneal carcinomatosis. J Exp Clin Cancer Res 15:49–58
Sugarbaker PH (1995) Peritonectomy procedures. Ann Surg 221:29–42
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Raspagliesi F, Kusamura S, Campos Torres JC, de Souza GA, Ditto A, Zanaboni F et al (2006) Cytoreduction combined with intraperitoneal hyperthermic perfusion chemotherapy in advanced/recurrent ovarian cancer patients: the experience of National Cancer Institute of Milan. Eur J Surg Oncol 32:671–675
Chi DS, Eisenhauer EL, Zivanovic O, Sonoda Y, Abu-Rustum NR, Levine DA et al (2009) Improved progression-free and overall survival in advanced ovarian cancer as a result of a change in surgical paradigm. Gynecol Oncol 114:26–31
Königsrainer I, Beckert S, Becker S, Zieker D, Fehm T, Grischke EM, Lauk O, Glatzle J, Brücher B, Wallwiener D, Königsrainer A (2011) Cytoreductive surgery and HIPEC in peritoneal recurrent ovarian cancer: experience and lessons learned. Langenbecks Arch Surg 396:1077–1081
Hyperthermic intra-peritoneal chemotherapy (hipec) in relapse ovarian cancer treatment (CHIPOR); http://clinicaltrials.gov/show/NCT01376752
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This manuscript contains original material that has not been previously published.
Rights and permissions
About this article
Cite this article
Königsrainer, I., Horvath, P., Struller, F. et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in recurrent epithelial ovarian cancer with peritoneal metastases: a single centre experience. Langenbecks Arch Surg 399, 589–594 (2014). https://doi.org/10.1007/s00423-014-1207-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1207-5