Abstract
Robot-assisted THA for femoral side is one of the oldest appreciations of robotics in orthopedic surgery. The first active robotic system, ROBODOC, has been used in many countries. Originally, it utilized pin-based registration system and required locator pin implantation in the patient femur before THA. Subsequently, non-pin-based surface registration technique was developed, which eliminated the need for pin implantation and pin-related complications. Besides the function of femoral milling during primary THA, this system can also selectively remove bone cement from the femoral canal during revision THA. Although one study shows a higher revision rate of robotic femoral surgery than a conventional technique, many studies show accurate femoral preparation, same or slightly better postoperative function, better alignment of the stem, less fat embolism, less stress shielding, and a lower incidence of femoral fracture by using the robot than conventional techniques.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Historically, there were two robotically assisted systems for femoral milling during total hip arthroplasty (THA): ROBODOC (Think Surgical, Fremont, CA, USA) and CASPAR (URS Ortho, Rastatt, Germany). ROBODOC was the first active robotic system designed to improve outcomes on the femoral side of cementless total hip arthroplasty (THA) by reducing technical errors [1]. During the 1980s, the clinical results using cementless THA were not stable because of bone ingrowth failure and persistent thigh pain. Manual preparation of the femoral cavity was thought to be one of the major causes of the problem [2]. Initial pilot studies were performed in dogs, and clinical use of this system was initiated in 1992 [2].
The US Food and Drug Administration (FDA) authorized a multicenter study that started in 1994. Although the robotic system used in that study required insertion of three locator pins, and the average operative time was more than 240 min, the study demonstrated better fit and positioning of the femoral component in the robot-assisted group [1]. Later, there were further system improvements that included reduction in the number of locator pins used (from three to two) and improved milling speed and cutting paths to reduce surgical invasiveness and robot milling time [1].
The European Union approved the system in 1994 [3], although the early trials in Germany led to multiple lawsuits and negative media coverage because of the high complications rate [4]. In Japan, we initiated a multicenter clinical trial in 2000 to acquire approval by our Ministry of Health, Labour, and Welfare. Subsequently, a “pinless” registration system was developed that utilized the bone surface for registration. In 2008, it received FDA approval for its use in THA. The ROBODOC system has now been used for more than 28,000 joint arthroplasties, including those in the knee.
CASPAR was the other image-based active robotic system. Although preliminary in vitro studies showed better bone-implant contact than manual implantation [5] and accuracy comparable to that of the ROBODOC system [6], the CASPAR system has been shown to have low accuracy regarding the postoperative stem anteversion angle compared with that in the original plan [7]. In addition, in a prospective trial, the CASPAR system had worse outcomes in terms of blood loss, dislocation, revision rate, and heterotopic ossification than the conventional group at the average 18 months of follow-up [8]. This system is no longer available for clinical use [4]. In this chapter, therefore, we address the ROBODOC system.
2 Techniques
2.1 Primary THA Using a Pin-Based System
ROBODOC is a fiducially based registration system. It consists of three units: a robotic arm with a high-speed end-milling device, a control cabinet, and a preoperative planning workstation (ORTHODOC; Think Surgical) (Fig. 11.1). Additional disposable equipment (e.g., sterilized drill bits and drapes) are needed for each robotic operation.
Using this pin-based system, each procedure consists of locator pin implantation, computed tomography (CT) scanning, preoperative planning using the workstation, robotic diagnostics and preparation, exposure and registration of pins, and robotic milling of the femur. For femoral registration, two locator pins are implanted: one in the greater trochanter and the other in the lateral condyle of the femur (Fig. 11.2). After pin implantation, which is performed with the patient under local anesthesia prior to THA, a CT scan is obtained according to the manufacturer’s specified protocol.
At the workstation, using the CT image data for the patient, the surgeon can create a three-dimensional (3D) preoperative plan to select the size of the prosthesis and its position in the femur (Fig. 11.3a). As the workstation shows the cutting paths three-dimensionally, the surgeon can identify any risk of abductor tendon injury and/or damage to the greater trochanter (Fig. 11.3b). When the implant is optimally positioned (virtually, at the workstation), the preoperative planning data are recorded on a compact disk (CD). Prior to the surgical procedure, the surgeon loads the patient data on the CD into the robot-assisted system and performs self-start-up diagnostics of the robot.
During the operation, the surgeon exposes the pins and secures the patient’s lower extremity to the robot with a femoral positioning clamp (Fig. 11.4). The surgeon then moves the robot arm by guiding its probe into contact with the pins (Fig. 11.5). The robot-assisted system computer records the pin locations and automatically performs registration and verification of its accuracy.
Surgical exposure of the left hip via a posterior approach. Femoral head and neck are elevated by an abdominal spatula (a). Gluteus maximus is retracted with a Charnley retractor (b). Gluteus medius and minimus muscles are retracted with a Hohmann retractor (c). A femoral positioning clamp (d) is then applied to the proximal femur (just below the lesser trochanter) to connect it with the robot (e). Finally, a bone motion monitor (f) is placed on the bone surface. (g) Greater trochanter; (h) femoral head
The surgeon then installs a drill bit and guides the robotic arm in front of the bone to begin milling the femur (Fig. 11.6a). While the robot mills the femoral canal, the monitor shows the milling process (Fig. 11.6b). The surgeon can stop the machine at any time by pressing a “pause” button. We prefer a posterior approach so the gluteus medius and minimus muscles are easily retracted anteriorly to avoid damage (Fig. 11.6a). After the milling is complete, the surgeon inserts the implant in the usual fashion. It is easy to determine the osteotomy level of the femoral neck because the medial cortex of this level has already been milled by the robot.
2.2 Primary THA Using a Pinless System
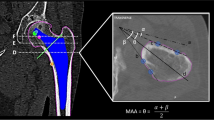
To eliminate the need for locator pin implantation and its potential pin-related complications (e.g., postoperative pain at the site of pin implantation [9]), a proprietary non-pin-based surface registration technique was developed by the manufacturer in 2000. First, a CT scan of the femur is performed according to the manufacturer’s specified protocol. The CT data are then imported into the workstation, and surface models of the proximal and distal femur are created for surface registration (Fig. 11.7). A preoperative plan is created in the same manner as with the pin-based registration system (Fig. 11.3). Once the surface bone model is successfully created and the optimal surgical plan completed, the surgeon transfers the data to a CD.
Prior to the surgical procedure, the surgeon loads the CD’s information into the robotic system and performs routine setup and diagnostic checks. During surgery, the surgeon secures the patient’s leg in the femoral fixator of the robot and then locates the bone surface points on the femur using a digitizer (Think Surgical) (Fig. 11.8a). In the present study, 14 points from the proximal femur and three points from the distal femur were digitized (Fig. 11.8b). The robotic computer recorded the spatial information of surface points and matched them to the coordinate surface model that was created preoperatively on the workstation. This procedure is called surface registration. When the registration has been completed, the surgeon verifies its accuracy by touching bone surfaces with the digitizer. If the difference between the digitization-based surface contour and the CT-derived surface contour is within 1 mm, the registration is considered acceptable (Fig. 11.8c). A drill bit is then installed, and the milling of the femur begins.
Pinless registration technique. (a) During the operation, the surgeon oriented the robot by selecting points on the femoral surface using a “digitizer.” (b) Registration of the proximal femur. Fourteen points were chosen, as shown on the monitor. The surgeon verified the registration accuracy by touching the bone surfaces with the digitizer. (c) If the locations coincided with the bone surface points on the monitor, the surgeon accepted the registration
2.3 Cement Removal During Revision THA Using a Pin-Based System
The pin-based registration system can also selectively remove bone cement from the femoral canal during revision THA. Prior to the surgery, two locater pins are implanted into the affected femur under local anesthesia. CT scans are obtained, and their data are imported into a preoperative planning workstation. The long axis of the femur is aligned. At least eight cross sections are defined, and the surgeon demarcates a perimeter around the bone cement on axial views of the femur. From these data, the workstation program automatically creates a 3D cutting path for cement removal (Fig. 11.9). At this point, the surgeon can check and modify the cutting path. These preoperative planning data are recorded on a CD. During the operation, the femur is exposed and the femoral component removed using a conventional procedure. After the patient’s leg is fixed to the robot and surgical table, registration is performed using the two locater pins. After soft tissues are firmly retracted, the robot mills the femoral canal to remove the bone cement. Finally, the surgeon manually reams the femoral canal and inserts the stem.
At the planning workstation, multiplanar reconstruction view of the proximal femur is used to plan robotic cement removal. A minimum of eight cross sections are defined on a coronal view. A perimeter around the bone cement is demarcated on each section (blue lines). The cutting path (purple) is then created automatically
3 Clinical Outcomes
3.1 Primary THA Using the Pin-Based System
The clinical accuracy (75 hips) of the pin-based system using postoperative CT images was <5% for the canal fill, <1 mm for the gap, and <1° for the mediolateral and anteroposterior alignment [10]. In our prospective, randomized study (78 hips underwent robotic milling, 78 underwent hand rasping) using a posterolateral approach, the robotic milling group showed significantly superior Merle d’Aubigne hip scores at 2 years. Compared with the robotic milling group, the hand rasping group had more intraoperative femoral fractures (0 vs. 5), more stem undersizing, higher vertical seating, and more femoral anteversion causing inferior fit of the implant [11]. At the 5-year follow-up (71 hips with robotic milling, 75 with hand rasping), there was significantly less variance in limb-length inequality and less stress shielding of the proximal femur in the robotic milling group, although differences in the clinical scores were not significant [12]. This tendency was also true at the 10-year follow-up [13]. At 2 years postoperatively, a dual energy X-ray absorptiometry study suggested that robotic milling was effective in facilitating proximal load transfer around the femoral component and minimizing bone loss after cementless THA [14].
The robotic femoral milling system reportedly reduces the development of intraoperative pulmonary embolisms. Using transesophageal echocardiography (46 hips with robotic milling, 25 with hand rasping), Hagio et al. found that the incidence of severe embolic events was lower in the robotic-milling group than in the hand-rasping group [15]. In contrast, Honl et al., who conducted a prospective, randomized study with 2 years of follow-up (74 hips with robotic milling, 80 with hand rasping using an anterolateral approach), found that 18% of the attempted robotic implantation procedures required conversion to manual implantation because the robotic system failed. They also found more complications in the robotic milling group, including nerve palsy (7%), dislocation (18%), and abductor dysfunction requiring reoperation (15%) [16].
One reason for the difference could be the surgical approach. It is possible that the posterolateral approach allows better retraction of the abductor muscles and thus better access for robotic milling than the anterolateral approach. However, Bach et al. reported that, when the insertion of the hip abductor muscles was protected appropriately, gait analysis showed no functional impairment after robotic procedures, even with an anterolateral approach [17]. Another reason could be the surgeons’ learning curve with this system. The preoperative planning workstation shows the cutting paths three-dimensionally, and the well-trained surgeon can then make the appropriate decisions preoperatively and intraoperatively to avoid abductor tendon injury by choosing the appropriate implant and/or approach for each patient [12].
3.2 Primary THA Using a Pinless System
We have reported a comparison study of the pinless system (40 hips) versus the pin-based system (78 hips). The average duration of the surgery was 25 min longer with the pinless system because more time was required for registration, including verification. Differences in the average blood loss and complications (e.g., nerve palsy, femoral fissure, dislocation, thigh pain) were not significant. At an average of 38 months postoperatively, Japanese Orthopaedic Association hip scores were significantly better in the pinless group than in the pin-based group, probably because patients with the pinless system had no pin-related knee pain. The accuracy of postoperative stem alignment of the pinless system was comparable to that of the pin-based method [18].
The pinless system received FDA approval in 2008. The advantages of this system are that there is no need for prior pin implantation surgery and no concern about pin-related knee pain.
3.3 Revision THA
Yamamura et al. reported 19 cases that required robotic bone cement removal from the femoral canal. The mean robotic milling time was 34 min (range 17–51 min). None of the patients suffered perforation or fracture of the femur during surgery or follow-up. No patients displayed nerve palsy or infection. Dislocation was seen in one patient. Radiographically, the bone cement was completely removed in all cases. Stem subsidence was seen in two cases. At final follow-up (76–150 months), all stems were considered stable. Early weight bearing was possible because of circumferential preservation of the femoral cortex. In nine cases, full weight bearing was achieved within 1 week postoperatively, which was better than that achieved with extended trochanteric osteotomy. Robotic bone cement removal thus seems safe and effective [19].
4 Discussion
There are several advantages of a robotic milling system. It enables precise preoperative 3D planning and execution of the plan. It enables better fit and increased bony ingrowth between the implant and the host bone. It reduces the incidence of complications, such as intraoperative pulmonary embolism, femoral fractures, and limb-length inequality. Its disadvantages are increased surgical invasiveness, longer operation time, an extended learning curve, and higher cost. In addition, surgeons cannot modify the surgical plan intraoperatively [4].
There have also been several reports of technical complications, such as having to halt a procedure because of bone motion during cutting, thereby requiring reregistration, femoral shaft fissures requiring wire cerclage, acetabular rim damage during milling, milling of a defect of the greater trochanter, and registration failures [20, 21]. To avoid these errors and complications, surgeons and staff must be fully educated regarding the use of the robotic milling system. Being familiar with the equipment and its use can minimize negative occurrences and optimize the safety and usefulness of the robot. Surgeons should keep in mind that, with this system, preoperative planning is part of the surgery, and an inappropriate plan results in failure. During surgery, the surgeon needs to understand the workspace and appropriate positioning of the patient and robot, carefully watch the moving path of the cutter, and listen to the sound of the milling to detect any abnormalities [22].
Future designs of the robotic system should include fail-safe mechanisms and tracking to prevent inadvertent injuries. For example, combining it with a navigation system would help avoid the need for reregistration as a result of bone motion. An improved user–machine interface could reduce the incidence of registration failure and subsequent incorrect execution of the surgery.
References
Bargar WL, Bauer A, Borner M. Primary and revision total hip replacement using the Robodoc system. Clin Orthop. 1998:82–91.
Paul HA, Bargar WL, Mittlestadt B, Musits B, Taylor RH, Kazanzides P, Zuhars J, Williamson B, Hanson W. Development of a surgical robot for cementless total hip arthroplasty. Clin Orthop. 1992:57–66.
Bargar WL. Robots in orthopaedic surgery: past, present, and future. Clin Orthop Relat Res. 2007;463:31–6.
Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31:2353. https://doi.org/10.1016/j.arth.2016.05.026.
Wu LD, Hahne HJ, Hassenpflug J. The dimensional accuracy of preparation of femoral cavity in cementless total hip arthroplasty. J Zhejiang Univ Sci. 2004;5:1270–8. https://doi.org/10.1631/jzus.2004.1270.
Schneider J, Kalender W. Geometric accuracy in robot-assisted total hip replacement surgery. Comput Aided Surg. 2003;8:135–45.
Mazoochian F, Pellengahr C, Huber A, Kircher J, Refior HJ, Jansson V. Low accuracy of stem implantation in THR using the CASPAR-system: anteversion measurements in 10 hips. Acta Orthop Scand. 2004;75:261–4. https://doi.org/10.1080/00016470410001178.
Siebel T, Kafer W. Clinical outcome following robotic assisted versus conventional total hip arthroplasty: a controlled and prospective study of seventy-one patients. Z Orthop Ihre Grenzgeb. 2005;143:391–8. https://doi.org/10.1055/s-2005-836776.
Nogler M, Maurer H, Wimmer C, Gegenhuber C, Bach C, Krismer M. Knee pain caused by a fiducial marker in the medial femoral condyle: a clinical and anatomic study of 20 cases. Acta Orthop Scand. 2001;72:477–80.
Nishihara S, Sugano N, Nishii T, Tanaka H, Nakamura N, Yoshikawa H, Ochi T. Clinical accuracy evaluation of femoral canal preparation using the ROBODOC system. J Orthop Sci. 2004;9:452–61.
Nishihara S, Sugano N, Nishii T, Miki H, Nakamura N, Yoshikawa H. Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplasty. 2006;21:957–66.
Nakamura N, Sugano N, Nishii T, Kakimoto A, Miki H. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res. 2010;468:1072–81.
Nakamura N, Sugano N. Sakai T. Nakahara I. Comparison between robotic-assisted and manual implantation of primary cementless total hip arthroplasty; minimum ten years follow-up results. Proceedings of International CAOS meeting, 2014. 2014.
Hananouchi T, Sugano N, Nishii T, Nakamura N, Miki H, Kakimoto A, Yamamura M, Yoshikawa H. Effect of robotic milling on periprosthetic bone remodeling. J Orthop Res. 2007;25:1062–9.
Hagio K, Sugano N, Takashina M, Nishii T, Yoshikawa H, Ochi T. Effectiveness of the ROBODOC system in preventing intraoperative pulmonary embolism. Acta Orthop Scand. 2003;74:264–9.
Honl M, Dierk O, Gauck C, Carrero V, Lampe F, Dries S, Quante M, Schwieger K, Hille E, Morlock MM. Comparison of robotic-assisted and manual implantation of a primary total hip replacement. A prospective study. J Bone Joint Surg Am. 2003;85:1470–8.
Bach CM, Winter P, Nogler M, Gobel G, Wimmer C, Ogon M. No functional impairment after Robodoc total hip arthroplasty: gait analysis in 25 patients. Acta Orthop Scand. 2002;73:386–91.
Nakamura N, Sugano N, Nishii T, Miki H, Kakimoto A, Yamamura M. Robot-assisted primary cementless total hip arthroplasty using surface registration techniques: a short-term clinical report. Int J Comput Assist Radiol Surg. 2009;4:157–62.
Yamamura M, Nakamura N, Miki H, Nishii T, Sugano N. Cement removal from the femur using the ROBODOC system in revision total hip arthroplasty. Adv Orthop. 2013;2013:347–58. https://doi.org/10.1155/2013/347358.
Schulz AP, Seide K, Queitsch C, von Haugwitz A, Meiners J, Kienast B, Tarabolsi M, Kammal M, Jurgens C. Results of total hip replacement using the Robodoc surgical assistant system: clinical outcome and evaluation of complications for 97 procedures. Int J Med Robot. 2007;3:301–6.
Chun YS, Kim KI, Cho YJ, Kim YH, Yoo MC, Rhyu KH. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty. 2011;26:621–5. https://doi.org/10.1016/j.arth.2010.05.017.
Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg. 2013;5:1–9. https://doi.org/10.4055/cios.2013.5.1.1.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Nakamura, N. (2018). Robotic Primary and Revision THA for the Femoral Side. In: Sugano, N. (eds) Computer Assisted Orthopaedic Surgery for Hip and Knee. Springer, Singapore. https://doi.org/10.1007/978-981-10-5245-3_11
Download citation
DOI: https://doi.org/10.1007/978-981-10-5245-3_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-5244-6
Online ISBN: 978-981-10-5245-3
eBook Packages: MedicineMedicine (R0)