Abstract
Background
Achieving an optimal limb alignment is an important factor affecting the long-term survival of total knee arthroplasty (TKA). This is the first study to look at the limb alignment and orientation of components in TKA using a novel image-free handheld robotic sculpting system.
Methods
This case-controlled study retrospectively compared limb and component alignment of 77 TKAs performed with a robot (Robot-group) with a matched control group of patients who received conventional alignment with intramedular rods (Control group). Alignment and component positioning was measured on full-leg weight-bearing and standard lateral X-rays by two independent observers. The image-free handheld robotic sculpting system calculated the planned and achieved mechanical axis (MA). Outliers were defined as > 3° deviation from planned alignment.
Results
Mean MA was 180.1° (SD = 1.9) in the Robot-group, compared to the Control group with a mean MA of 179.1° (SD = 3.1, p = 0.028). We observed 5 outliers (6%) in the Robot-group and 14 outliers (18%, p = 0.051) in the Control group. Fraction of outliers of the frontal tibial component was 0% in the Robot-group versus 8% in the Control group (p = 0.038). There were no other statistical differences regarding the implant positioning between both groups.
Conclusion
The Robot-group showed significantly less outliers compared to the conventional technique. Whether these differences are clinically relevant is questionable and should be investigated on the long term. Randomized controlled trials with larger patient series will be needed in the future to confirm our preliminary results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is the gold standard for patients with end-stage knee osteoarthritis (OA), with excellent clinical results. It provides pain relief, enhanced mobility and improved quality of life in patients with OA [1]. In the literature, implant survival rates between 81% and 92% at 15-years follow-up were reported [2, 3]. Accurate implant alignment and soft tissue balancing is an important factor for a successful outcome [4, 5]. Well-known reasons for early failure are instability, implant malpositioning and limb malalignment [6]. The typical objective of TKA is to obtain a limb alignment within 2°–3° around a neutral mechanical axis (MA) of the leg in the coronal plane [7, 8]. Deviation of more than 3° from a neutral MA is associated with increased failure rates due to off-axis loading, polyethylene wear and subsequent implant loosening [4, 7,8,9].
As with most techniques in modern medicine, TKA has been developed significantly over the past decades with improvement of both implant survival and daily function. Computer-assisted surgery (CAS) for TKA was introduced in the late 1990s to improve alignment of TKA and reduce the incidence of outliers. Pins are placed on the femur and tibia and with help of a computer platform, tracking system and a rigid body marker, anatomical landmarks around the knee are registered and prosthetic sizing and bone resection level can be analyzed. Studies showed the percentage of outliers in the coronal plane was 9–13% with CAS and up to 32% with conventional instruments (CI) [10, 11].
A concern that arises with any new technique is whether it will achieve satisfactory outcome. Published results on CAS are contradictory. Despite improving mechanical alignment, CAS failed to improve functional results when compared to conventional techniques [12,13,14].
Recently, the next generation of robotics was introduced to further reduce the amount of outliers. An image-free handheld robotic sculpting system enables the surgeon to plan the implant position in six degrees of freedom peroperatively without the need for preoperative imaging. Intraoperative adjustments allow the surgeon to optimize soft tissue balancing and bony alignment. Implant placement accuracy of this image-free approach has been demonstrated in a cadaveric study [15]. Published clinical results on this image-free handheld robot system are scarce. To the best of our knowledge, no clinical studies have yet been published comparing the precision freehand robotic sculpting system with a matched cohort of conventional TKAs. This matched cohort study on robotics and conventional technique for the implantation of TKA was designed to address the following research question: Is there a difference in the alignment accuracy between robotic and conventional TKA? Does the robot achieve the desired MA as planned by the surgeon’s preference? We hypothesize that the robot will be more accurate when compared to conventional TKA and will achieve the desired MA with few outliers.
Methods
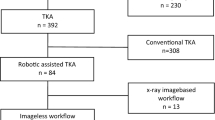
This retrospective case-controlled study included a consecutive series of patients operated with an image-free handheld robot system for TKA (NAVIO Surgical System, Smith & Nephew, Memphis, USA) between May 2018 and March 2019 in the St. Trudo Hospital (St. Truiden, Belgium). A total of 79 patients were operated by means of robotic-assisted TKA (Robot-group) for end-stage knee OA. Two patients were excluded because of technical difficulties with the robot system and were switched to conventional technique peroperatively. The remaining 77 patients were matched on gender, age, type of implant (Journey II/Genesis/Legion) and follow-up time with seventy-seven patients who had been operated with the conventional technique using intramedular rods (Control group), forming a total cohort of 154 patients. All TKA procedures were performed by 2 experienced knee surgeons (PB and JM), both performing a minimum of 150 TKA procedures annually. Six patients were excluded because of missing data. Baseline demographics and operative data are shown in Table 1.
Operating technique
In all procedures, a tourniquet and a standard medial parapatellar approach was used. In the Robot-group, two percutaneous bicortical partially threaded pins were placed with help of a pointer instrument into the proximal tibia and into the distal femur for the tracking arrays of the robot system. Standard exposure of both the femur and tibia was carried out with patella eversion. The anterior and posterior cruciate ligaments were sacrificed and osteophytes were excised before gathering data with the robot. Mechanical and rotational axes of the limb were determined peroperatively by establishing the hip, knee and ankle centers. The kinematic axis of the knee was identified and selected to determine the rotational position of the femoral component. The morphology of the knee was determined by mapping out the condylar anatomy by “painting” the surfaces with the probe. A software program of the robot creates a virtual 3D model of the knee. The implant size that best fits on the virtual model is then selected by the surgeon, including the position of the implant in coronal, sagittal and rotational planes.
Thereafter, valgus and varus stress was applied during full range of motion to tension the medial and lateral structures for balancing the dynamic soft tissue. The robot software creates a graphical gap space through the full range of motion by which the surgeon can adjust the desired MA and the planned position of the femoral and tibial components to optimize the soft tissue balancing. Adjustments of the implant size and position in all planes were made to optimize soft tissue balance and component tracking before bone preparation. After planning the components, the distal femur bone was prepared with a high-speed 5-mm burr by continuously moving a hand piece and switched on and off as the motorized burr moved in and out of the mapped cutting space. The pin holes for the saw guides were prepared with a 5-mm burr for the proximal tibia and with a 2-mm burr for the distal femur. The saw guides were then fixed, with the feedback of the robot, in an optimal position to make the bone cuts of the proximal tibia and anterior and posterior femur.
After putting in the trial components, balancing and component tracking was checked again with valgus and varus stress during full range of motion with graphical representation of gap spacing. TKA were cemented (Gentamicin Palacos, Heraeus Kulzer GmbH., Hanau, Germany) in all procedures.
The operative procedure in the Control group was identical to that in the Robot-group, except for pin placement for the cutting blocks, which was done using conventional intramedullary alignment rods. Soft tissue balancing and patella resurfacing were performed when deemed necessary.
Clinical outcome
All patients were seen on standard outpatient visits, and all information was obtained from the patient’s records. Standing, full weight-bearing, AP long-leg and lateral digital radiographs were taken preoperatively and 6 weeks postoperatively in both groups. Radiographic measurements were made with the use of a calibrated protocol on digital images using the Impax system for Windows (AGFA HealthCare). All radiographic evaluation was performed twice for each radiograph separately by 1 observer (AB) to obtain intra-observer reliability and once by an independent observer (SK) to calculate the inter-observer reliability.
The MA was determined according to Tigani et al. [16]. The position of the femoral (frontal femoral component, FFC) and tibial (frontal tibial component, FTC) components perpendicular to the MA was measured on the same standing, weight-bearing, AP long-leg radiographs. On the standard lateral radiographs, the flexion and slope for, respectively, the femoral (lateral femoral component, LFC) and tibial (lateral tibial component, LTC) components were measured according to Tigani et al. [16]. The LFC was measured as the anterior angle between the femoral component and the anterior cortex of the femur. The LTC was measured as the anterior angle between the tibial component and the posterior cortex of the tibia. Proportions of deviation > 3° were calculated for the MA and individual components. These were considered as outliers.
Further perioperative conditions including operating time (incision to closure in minutes) and type of implant (Journey II/Genesis/Legion) were assessed from the patients operative records.
The study was approved by the Local Review Board (Sint-Truiden, Belgium; approved on February 20th, 2019; IRB-Nr PEC-V-HJ2019-02-20) and conducted according to the principles of the Declaration of Helsinki (2008) and in accordance with the Medical Research Involving Human Subjects Act [17].
Statistical analysis
Statistical Package for the Social Sciences version 21.0 (SPSS, Inc., Chicago, IL) for Windows was used. All radiographic evaluation was performed by 2 independent assessors (AB and SK). Intra- and inter-class correlation coefficients (ICCs) were calculated to check for intra- and inter-observer reliabilities. An ICC ≥ 0.7 was considered as good correlation. Statistically significant differences for the baseline conditions and radiographs between the Robot-group and the matched Control group were analyzed with a Student’s t test. Fisher’s exact test was used to test differences of proportions. No a priori sample size or power was calculated for this retrospective case-controlled study. It was carried out in an attempt to predict an appropriate sample size to design a full-scale research project. Therefore, effect size (i.e., Cohen’s d) for the primary endpoint, the postoperative mechanical axis, was calculated as the standardized difference between two means divided by the standard deviation of both groups. An effect size of 1.0 is equivalent to a change of one SD in the sample and considered very large. An effect size of 0.8 is large, 0.5 is moderate and ≤ 0.3 is small [18]. For all analyses, a p-value was considered to be statistically significant at p ≤ 0.05. Results are presented as mean (SD), proportions (%) and 95% confidence interval (CI).
Results
Patients from the Control group were perfectly matched with patients from the Robot-group, and no differences in baseline characteristics were reported. Additional perioperative information shows a significant longer operation (OR) time (p = 0.000) in the Robot-group. Baseline and operative data are presented in Table 1.
The difference in the postoperative MA was statistically significant (p = 0.028) between the Robot-group and Control group with a mean of 180.1° (1.9°) and 179.1° (3.1°), respectively. The postoperative MA in the Robot-group improved significantly (p = 0.005) when compared to the preoperative MA. Difference between the pre- and postoperative MA for both the Robot-group and Control group is visualized in Fig. 1.
A moderate effect size of 0.4 was calculated for the MA. The frontal and lateral radiographic outcome for both the femur and tibia are summarized in Table 2.
The MA was restored accurately in all patients, but with accompanying numbers of outliers in the Robot-group and Control group. All radiographic measurements of both observers were reliable, and ICCs were excellent except for the inter-observer agreement (0.411) regarding the LFC. Only the number of outliers for the varus–valgus position of the tibial component showed a significant difference (p = 0.038) with more outliers in the Control group (n = 6, 8%) than in the Robot-group (0%). Outliers and corresponding percentage, including the intra- and inter-observer agreement, are summarized in Table 3.
Regarding the preoperative planned and postoperative achieved mechanical leg alignment as measured with the robot, data of 71 patients (92%) from the Robot-group were available. When compared with the postoperative standing, weight-bearing, AP long-leg radiographs, 6 (8%) and 11 (15%) outliers were found for the planned and achieved MA, respectively, as obtained with the robot.
Discussion
The most important finding of the present study is the ability of a novel image-free handheld robot sculpting system to accurately achieve the planned mechanical axis (MA) in TKA with few outliers. There were significant but no clinically relevant differences between the two groups regarding the radiographic outcome measures. The present study investigated the alignment and component positioning of TKA performed with an image-free handheld robotic sculpting system and compared these results with a matched control group of TKAs performed with conventional intramedullary technique, without focusing on learning curve, clinical outcome and complication rate of the robot.
Restoring a neutral MA within 3° of varus/valgus remains one of the most fundamental principles in TKA [8, 19, 20]. Recent studies have raised doubts about the benefits of a neutral MA. A study with a 20-year follow-up revealed that there was no difference in survival between TKA that were mechanically aligned or those outside the 3° of varus/valgus [21]. Furthermore, this objective to obtain a neutral MA has been questioned by the introduction of kinematic alignment (KA) in TKA [22]. The philosophy of KA is to restore the physiological kinematics by allowing a certain degree of constitutional varus/valgus in TKA. In the present study, KA robot TKA was compared with MA conventional TKA. Due to the retrospective nature of this study, we did not report the degree of the planned femoral cut in the Control group. In the Control group, bony cuts were measured on preoperative X-rays and made in order to achieve a neutral MA. In the Robotic-group, all TKAs’ were kinematically aligned to achieve optimal soft tissue balancing, and an alignment of ± 2° from neutral was tolerated. Despite the ongoing debate on optimal limb alignment, it remains clear that a well-balanced TKA is paramount to ensure long-term survival by avoiding off-axis loading, polyethylene wear and subsequent implant loosening [4, 7,8,9]. The robotic-assisted system provides a useful tool for the surgeon to peroperatively change implant positioning and alignment in order to achieve a well-balanced TKA.
In literature, conventional TKA have a risk of outliers of up to 30% [10, 23]. Thienpont et al. observed 20% outliers in a meta-analysis on patient-specific instrumentation (PSI) for TKA [23]. A meta-analysis studying computer-assisted surgery (CAS) for TKA showed that outliers occurred in 9% of the cases [10]. The most recent robotic-assisted TKA established outliers in just 3% of all cases [24]. The outliers (6%) found in the present study with the robotic system are in line with the other robotic systems.
Interestingly, study data reveals a difference in outliers between the achieved MA, as measured by the robotic-assisted system, and the postoperative MA, which was measured on long-leg standing X-rays. Based on our experience, we believe this is due to the extra amount of force of a weight-bearing radiograph in comparison with the robotic-assisted system measurements, where the patient is lying flat on the operating table. This has previously been shown in the literature too [25, 26]. Despite these preliminary data, we should therefore consider the possibility of inaccurate measurements of the robotic-assisted system.
In the present study, no outliers of the frontal tibia component were observed in the Robot-group, which was significantly better compared to the Control group with 8% outliers (p = 0.038). Tibial component malalignment had been shown to be a well-known cause of early failure in TKA [27]. The accuracy of the robotic-assisted system in implant positioning has been previously validated in unicondylar knee arthroplasty [15, 28, 29]. Casper et al. validated its accuracy in TKA in a recent cadaveric study [30]. Mason et al. previously reported frontal femoral and tibial malalignment in 5% and 4%, respectively, in CAS TKA [10]. We expected fractions of outliers to be comparable, or better, than CAS TKA, though a higher fraction of femoral outliers was found. We believe this is due to a learning curve. However, we should consider low accuracy of the planning software.
There may be some concerns regarding the radiological measurements in the sagittal plane. The present study observed 17% and 86% outliers in the Robot- group for, respectively, the tibia slope and flexion of the femoral component as measured on lateral X-rays. These large amounts of outliers were also observed in the Control group, without significant differences between both groups. This worse outcome can partly be explained by the suboptimal quality of the lateral X-ray measurements as found between both observers (inter-observer agreement: 0.411) and was therefore not reliable. This low inter-observer agreement was disappointing that it should be considered invalid. A wide variety of different analyses in the literature are used to objectively determine the postoperative position for both the femur and tibia implants. Most of the literature studying postoperative implant position use long-standing radiographs. Determining sagittal component alignment using plain radiographs is challenging due to the effects of difficulty in establishing a true sagittal axis using standard lateral X-rays [31, 32]. Despite a good ICC for the evaluation of the frontal position of both femur and tibia implants, rotational alignment was not examined. Postoperative evaluation on 3D-CT has shown to be a valuable tool to measure position and orientation of both the femur and tibia components, including the implant rotation [33, 34]. Unfortunately, a postoperative 3D-CT is not routinely performed in our clinic. Future studies on the accuracy of the robotic-assisted system are needed with accurate CT-based measurements, to assess this observation.
A valuable strength of this study was the well-described patient cohorts due to the extensive information available in the patient’s medical records. This allowed matching of patients from the Robot-group with suitable patients from the Control group. Another particular strength of this study was that both surgeons operated with the robot and conventional alignment tools and with use of the different designs of implants. These strengths provide less sensitivity for selection bias in this study.
In this study, 2 patients were excluded because of technical issues of the Navio tracking system. Both cases were switched to conventional instrumentation peroperatively. Here we report setup issues in the early experience with the Navio robot. As mentioned before, a learning curve is to be expected with the use of a novel technology.
Together with the retrospective design of the study, the most important limitation was the limited number of patients. The study was designed for radiographic analysis of the postoperative MA with the use of long-leg standing X-rays. Therefore, a type II error cannot be ruled out. A post hoc power analysis revealed a power of 0.669 (1− β). Based on these results, we performed a power analyses with effect size of 0.4, power (1− β) set at 0.80 and a = 0.05 (two-tailed). Approximately 105 patients in each group are needed to obtain statistical power at the recommended 0.80 level.
Finally, despite the retrospective nature of this study, with a limited number of patients, this is the first study comparing an image-free handheld robot with conventional alignment for TKA giving valuable insight about the use of a promising knee alignment tool addressing a relevant outcome. The results illustrate that an image-free handheld robot for TKA can help to restore the desired limb alignment and accurate tibial implant position.
Conclusion
The present study illustrates that this simplified surgical robot technique for TKA is effective with acceptable radiological outcome. The Robot-group showed significantly less mechanical axis outliers compared to the conventional technique. Whether these differences are clinically relevant is questionable and should be investigated on the long term. Randomized controlled trials with larger patient series will be needed in the future to confirm our preliminary results.
References
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63. https://doi.org/10.1007/s11999-009-1119-9
Gothesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, Hallan G, Furnes O (2013) Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994–2009. Bone Joint J. https://doi.org/10.1302/0301-620x.95b5.30271
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92(12):2143–2149. https://doi.org/10.2106/jbjs.i.01398
Lotke PA, Ecker ML (1977) Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am 59(1):77–79
Golladay GJ, Bradbury TL, Gordon AC, Fernandez-Madrid IJ, Krebs VE, Patel PD, Suarez JC, Higuera Rueda CA, Barsoum WK (2019) Are patients more satisfied with a balanced total knee arthroplasty? J Arthroplast 34(7s):S195–s200. https://doi.org/10.1016/j.arth.2019.03.036
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318. https://doi.org/10.1097/00003086-200111000-00041
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73(5):709–714
Bargren JH, Blaha JD, Freeman MA (1983) Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res 173:178–183
Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K (2007) Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplast 22(8):1097–1106. https://doi.org/10.1016/j.arth.2007.08.001
Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK (2012) Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplast 27(6):1177–1182. https://doi.org/10.1016/j.arth.2011.12.028
Cheng T, Pan XY, Mao X, Zhang GY, Zhang XL (2012) Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee 19(4):237–245. https://doi.org/10.1016/j.knee.2011.10.001
Gothesen O, Espehaug B, Havelin LI, Petursson G, Hallan G, Strom E, Dyrhovden G, Furnes O (2014) Functional outcome and alignment in computer-assisted and conventionally operated total knee replacements: a multicentre parallel-group randomised controlled trial. Bone Joint J. https://doi.org/10.1302/0301-620x.96b5.32516
Harvie P, Sloan K, Beaver RJ (2012) Computer navigation vs conventional total knee arthroplasty: five-year functional results of a prospective randomized trial. J Arthroplasty 27(5):667–672.e661. https://doi.org/10.1016/j.arth.2011.08.009
Lonner JH, John TK, Conditt MA (2010) Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res 468(1):141–146. https://doi.org/10.1007/s11999-009-0977-5
Tigani D, Busacca M, Moio A, Rimondi E, Del Piccolo N, Sabbioni G (2009) Preliminary experience with electromagnetic navigation system in TKA. Knee 16(1):33–38. https://doi.org/10.1016/j.knee.2008.09.004
(2013) World Medical Association Declaration of Helsinki. JAMA 310 (20):2191
Kazis LE, Anderson JJ, Meenan RF (1989) Effect sizes for interpreting changes in health status. Med Care 27(3 Suppl):S178–189
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty 24(4):570–578. https://doi.org/10.1016/j.arth.2008.03.002
Abdel MP, Ollivier M, Parratte S, Trousdale RT, Berry DJ, Pagnano MW (2018) Effect of postoperative mechanical axis alignment on survival and functional outcomes of modern total knee arthroplasties with cement: a concise follow-up at 20 years. J Bone Joint Surg Am 100(6):472–478. https://doi.org/10.2106/jbjs.16.01587
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53. https://doi.org/10.1007/s11999-011-1936-5
Thienpont E, Schwab PE, Fennema P (2017) Efficacy of patient-specific instruments in total knee arthroplasty: a systematic review and meta-analysis. J Bone Joint Surg Am 99(6):521–530. https://doi.org/10.2106/jbjs.16.00496
Ren Y, Cao S, Wu J, Weng X, Feng B (2019) Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J 95(1121):125–133. https://doi.org/10.1136/postgradmedj-2018-136190
Sabharwal S, Zhao C (2008) Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg Am 90(1):43–51. https://doi.org/10.2106/jbjs.f.01514
Jang KM, Lee JH, Cho IY, Park BK, Han SB (2017) Intraoperative Fluoroscopic assessment of limb alignment is a reliable predictor for postoperative limb alignment in biplanar medial opening-wedge high tibial osteotomy. J Arthroplasty 32(3):756–760. https://doi.org/10.1016/j.arth.2016.08.022
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34. https://doi.org/10.1097/01.blo.0000148578.22729.0e
Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE (2015) High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res 473(1):206–212. https://doi.org/10.1007/s11999-014-3764-x
Smith JR, Riches PE, Rowe PJ (2014) Accuracy of a freehand sculpting tool for unicondylar knee replacement. Int J Med Robot 10(2):162–169. https://doi.org/10.1002/rcs.1522
Casper M, Mitra R, Khare R, Jaramaz B, Hamlin B, McGinley B, Mayman D, Headrick J, Urish K, Gittins M, Incavo S, Neginhal V (2018) Accuracy assessment of a novel image-free handheld robot for total knee arthroplasty in a cadaveric study. Comput Assist Surg (Abingdon) 23(1):14–20. https://doi.org/10.1080/24699322.2018.1519038
Solayar GN, Chinappa J, Harris IA, Chen DB, Macdessi SJ (2017) A comparison of plain radiography with computer tomography in determining coronal and sagittal alignments following total knee arthroplasty. Malays Orthop J 11(2):45–52. https://doi.org/10.5704/moj.1707.006
Schmidt GL, Altman GT, Dougherty JT, DeMeo PJ (2004) Reproducibility and reliability of the anatomic axis of the lower extremity. J Knee Surg 17(3):141–143
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg Br 93(5):629–633. https://doi.org/10.1302/0301-620x.93b5.25893
Boonen B, Schotanus MGM, Kerens B, Hulsmans FJ, Tuinebreijer WE, Kort NP (2017) Patient-specific positioning guides for total knee arthroplasty: no significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg Sports Traumatol Arthrosc 25(9):2809–2817. https://doi.org/10.1007/s00167-015-3661-1
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
PB conceived, designed, coordinated the study and drafted the manuscript. AB coordinated the study, collected data and drafted the manuscript. JM conceived the study and critically reviewed the manuscript. SK analyzed the data and drafted the manuscript. MS participated in the design of the study, analyzed the data and critically reviewed the manuscript. DJ participated in the design of the study, coordinated the study and critically reviewed the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
PB and JM are consultants on the NAVIO Robotic technique for Smith & Nephew, Europe. The other authors certify that they have no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted abstract.
Ethical approval
Ethical approval by the local ethical committee was obtained for this study.
Informed consent
Informed consent was not necessary since it was a retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bollars, P., Boeckxstaens, A., Mievis, J. et al. Preliminary experience with an image-free handheld robot for total knee arthroplasty: 77 cases compared with a matched control group. Eur J Orthop Surg Traumatol 30, 723–729 (2020). https://doi.org/10.1007/s00590-020-02624-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02624-3