Abstract
A scan of any cancer, diabetes, cardiovascular disease or kidney health guideline underscores the importance of preventive strategies to offset the risk of developing chronic conditions. It also highlights the commonalities amongst preventive strategies for these conditions. In this chapter, we focus on the lifestyle practices that increase or reduce the risk of developing common chronic conditions. We examine how modifying individual-level determinants of health, such as exercise and dietary habits, environmental exposures, and alcohol and medication intake could help prevent them. Throughout this chapter we will discuss how these determinants of health can also work in synergy to influence risk. We will particularly focus on the complementary roles of diet and exercise in reducing body fatness and subsequently in reducing many of the risks associated with chronic disease. This chapter concludes with sections on pharmacoprevention and potential approaches to enhance the uptake of, and adherence to, health-promoting behaviours that can prevent the development of chronic conditions and cancer.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Risk reduction
- Lifestyle practices
- Body fatness
- Nutrition
- Exercise
- Pharmacoprevention
- Environmental exposures
-
Research increasingly indicates that cancer and other chronic conditions tend to share common risk factors.
-
While many drugs have the potential to limit the risk of chronic disease and cancer, the most feasible and economic determinants of health to target are often lifestyle-related.
-
The risks associated with cancer and chronic conditions are often amenable to lifestyle modifications that reduce body fatness, maximise physical activity, promote good nutrition that emphasises plant-based sources, and minimise alcohol intake.
-
Many health-promoting lifestyle practices have numerous benefits, operating in synergy to modify risk. In particular, good nutrition and optimum physical activity tend to work in a complementary way to reduce body fatness, which, along with tobacco smoking and high alcohol consumption, embodies an enormous risk to health.
-
Adherence to diet, exercise and pharmacotherapy is complex, and remains problematic in the context of preventing chronic disease.
7.1 Introduction: Why Prevention Matters
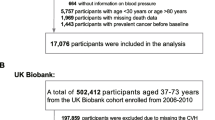
The incidence of chronic conditions such as cardiovascular and kidney disease, diabetes and cancer is rising. The World Health Organisation argues that these chronic conditions affect not only individual quality of life; they are also an under-appreciated cause of poverty and a significant impediment to the economic development of many countries [1]. The WHO Global Report on chronic diseases and health promotion estimated that preventive strategies could result in an additional 2 % reduction in chronic disease death rates worldwide each year, with the potential to prevent 36 million premature deaths by 2015 [1]. The substantial personal and societal costs of chronic disease and cancer have prompted governments to recognise that systemic collaborative action is needed to target chronic disease prevention [2, 3]. Fortunately, there are solutions to the problem that are both efficacious and highly cost-effective [1]. These solutions are the focus of this chapter.
7.2 Defining Prevention
Prevention in the context of chronic conditions and cancer is broadly defined as “approaches and activities aimed at reducing the likelihood that a disease or disorder will affect an individual, interrupting or slowing the progress of the disorder or reducing disability” [4]. Given that many chronic conditions can take decades to become fully established and tend to occur for a long time once they appear, strategies to prevent them are classified into three stages [2]:
-
Primary prevention, which reduces the likelihood of developing a disease or disorder
-
Secondary prevention, which interrupts, prevents or minimises the progress of a disease or disorder at an early stage
-
Tertiary prevention, which halts the progression of damage already done [2].
The good news is that most of the strategies discussed in this chapter are beneficial irrespective of the individual’s position on this continuum of prevention.
7.3 Modifying Individual-Level Determinants of Health to Prevent Chronic Disease and Cancer
The elements that influence whether and how an individual develops a chronic condition, and which are often the target of preventive strategies, are known as the determinants of health. Determinants comprise a range of factors: the broader features of the society in which the individual is situated, their socioeconomic characteristics, their individual knowledge and practise of health behaviours, and their biomedical characteristics, such as birth weight, immune status and genetic inheritance.
There are many inter-relationships between the determinants of health. That is, many determinants such as diet, physical activity and genetic inheritance tend to co-exist, working synergistically to potentiate or modify the risk of developing a chronic condition. Adding to this complexity, a single adverse determinant of health can be implicated in the development of several different chronic conditions, which increases the likelihood that comorbidities will develop. Tobacco smoking for example is implicated in the development of type 2 diabetes, ischaemic heart disease, stroke, kidney disease, arthritis, osteoporosis, lung and colorectal cancer, chronic obstructive pulmonary disease, asthma, depression and compromised oral health [5]. Existing disease states are also determinants of health, as they can compound the risk of multiple chronic diseases. For example, diabetes is linked to the subsequent development of cardiovascular, eye and kidney disease [1], while women previously treated for breast cancer are more likely to develop cardiovascular disease or osteoporosis.
To account for this complexity, the World Health Organisation classifies strategies to modify determinants of health into twelve broad areas that range from the universal to the individual: laws and regulations, tax and price interventions, improving the built environment, advocacy, community-based interventions, school-based interventions, workplace interventions, screening, clinical prevention, disease management, rehabilitation, and palliative care [1]. Prevention strategies often work best when they simultaneously target universal-, intermediate- and individual-level determinants of health [3]. Successfully reducing lung cancer rates, for example, commonly involves widespread regulations to restrict the sale of tobacco complemented by confronting anti-tobacco marketing, increased tobacco excise, public health education, individual support via Quit programs and systemic screening programs for those at risk [3]. Given the clinical focus of this book, however, in this chapter we concentrate on the preventive strategies that are most amenable to health professional intervention at the individual level.
Tables 7.1, 7.2 and 7.3 highlight that most of the rigorous evidence related to the individual determinants of chronic disease pertain to cancer, although research increasingly indicates that cancer and other chronic conditions tend to share common risk factors. The three “focus” health determinants for individual-level chronic disease and cancer prevention are risky alcohol consumption, tobacco smoking, and unhealthy diet coupled with excessive energy intake [1, 3]. These determinants are often expressed through the intermediate risk factors of hypertension, abnormal blood lipids and body fatness [1].
In the next sections, we tease out how the individual risk factors presented in these tables operate in the primary, secondary and tertiary continuum of chronic disease and cancer prevention. We discuss the modification of exercise, nutrition, environmental exposures and medications in light of compelling recent evidence that explains the pathophysiology of risk, and how lifestyle modifications work to reduce risk. We also discuss the evidence underpinning strategies to modify the risk of developing chronic diseases and cancer.
7.4 Exercise, Chronic Disease and Cancer
7.4.1 Primary Prevention
In the context of chronic disease, physical activity should be considered as potent a medicine as many preventative drugs [6]. Physical activity is defined as movement that increases metabolic rate and can be categorised in relation to the energy cost of the activity (termed metabolic equivalent, MET, which is the ratio of the work metabolic rate to the resting metabolic rate). There is ‘convincing grade’ evidence for the beneficial role of physical activity in the primary prevention of dementia [7], type 2 diabetes [8, 9], cardiovascular disease [10, 11] and colorectal cancer [12], and ‘probable’-grade evidence in postmenopausal breast cancer and endometrial cancer [13] (Table 7.1).
For the primary prevention of breast cancer in postmenopausal women, a 3 % decreased risk is observed per 7 MET-hours (METs used per hour) of recreational activity/week [13]. Every 5 MET-hours/day is associated with a decreased risk of developing colorectal cancer and colon cancer by 3 and 8 %, respectively [14]. Interestingly, the same relationship does not appear to exist in rectal cancer [14]. While it is not yet possible to determine the dose-response relationship of exercise in endometrial cancer due to differences in physical activity assessment across studies, individuals engaging in the greatest amount of recreational, occupational and/or incidental physical activity demonstrate a reduced risk of cancer of the endometrium compared to those engaging in the lowest levels of activity [15].
The effects of physical activity on the primary prevention of colorectal, endometrial and postmenopausal breast cancers are likely pleiotropic (i.e. have multiple, seemingly unrelated effects) and involve a combination of host pathways [16]. Research suggests that physical activity could reduce the risk of these cancers through a number of pathways, including the modulation of body composition, metabolic hormones, sex-steroid hormones, alterations in immune function, levels of oxidative stress as well as the balance of markers of inflammation and cytokines [17].
The most widely investigated pathway linking physical activity to cancer risk is the effect of exercise on circulating metabolic factors. Changes in metabolic status mediated through the insulin-like growth factor (IGF) axis represent one of the most plausible host pathways through which physical activity is linked to colorectal cancer [17–19]. For example, Chi and colleagues [20] reported a positive association between the risk of colorectal cancer incidence and circulating levels of IGF-1 (OR = 1.25; p = 0.003) and IGF-2 (OR = 1.52; p = 0.003). Exercise has a likely hormetic (“U” shaped) effect on the IGF axis, and possibly reduces IGF concentrations in states of systemic overabundance, effectively reducing IGF-1 receptor-mediated signalling; cancer outcomes are subsequently improved with exercise through ablation of this mitotic signalling pathway [21]. Moreover, muscle contraction during exercise induces molecular signalling and involves a variety of signalling molecules, including adenosine monophosphate-activated protein kinase (AMPK; a master regulator of cellular energy homeostasis) [22]. In response to increased energy demands during exercise, AMPK conserves adenosine triphosphate via inhibition of the biosynthetic and anabolic pathways, directly contributing to control of cancer cell growth [23]. Indeed, AMPK is reported to be differentially up-regulated following exercise in tumour-bearing mice [24].
Cytokines, which are proteins vital for immune system regulation, also have anti-tumour properties [25]. Deregulation of cytokine production or activity can lead to detrimental acceleration of inflammation, angiogenesis and cell proliferation; hence cytokines can be cancer-promoting factors [25–27]. In pre-existing cancer cells, an abundance of cytokines can stimulate tumour growth and cell proliferation [25]. As such, chronically elevated serum cytokines could potentiate tumour development and progression.
The effects of acute versus chronic exercise on plasma cytokine responses are seemingly paradoxical. Acute exercise results in a transient increase in circulating levels of cytokines produced by myoblasts [28–31]. The underlying mechanism behind this acute increase is the development of a hypoxic microenvironment within the muscle cells [32, 33]. Hypoxia results in the production of reactive oxygen species [32, 33] that stimulate the AP-1 and NF-κB pathways, the primary sources of cytokine production, such as interleukin-8 (IL-8) [34–36]. It is postulated that IL-8 acts locally to stimulate angiogenesis within the muscle, a known adaptation to exercise [37]. An increase in IL-8 is accompanied by a concomitant increase in CXCR2 (a protein coding gene) expression following exercise in the proximate endothelial cells resulting in angiogenesis in the muscle microvasculature [38]. In contrast to the increase in cytokine response to acute exercise, chronic exposure to exercise can normalise circulating cytokine concentrations [39, 40], reducing the perturbations in homeostasis following acute exercise [41]. Given that hypoxia is the primary trigger of cytokine production during exercise, it is reasonable to assume that following regular exercise training, improved delivery of oxygen to the exercising muscles coupled with greater mitochondrial volume results in less hypoxic stress, plus reduced production of cytokine from the muscles. This is supported by numerous studies showing that athletic populations characterised by greater levels of aerobic fitness have dampened immune responses to exercise than their sedentary counterparts [41–44].
Physical activity also plays a role in the prevention of weight gain, which is associated with independent, ‘probable’ level evidence for the primary prevention of postmenopausal breast cancer. Indeed, the reduced risk of endometrial and postmenopausal breast cancers associated with physical activity can be explained, at least in part, by the enhanced balance of circulating oestrogens, progesterone and androgens that are either a direct result of exercise, or secondary to improvements in body composition that accompany exercise [45, 46]. The modulation of body composition, in particular the reduction of visceral adipose tissue, with regular exercise can also lead to reductions in circulating cytokine levels. Indeed, obesity is associated with higher levels of circulating IL-8 [47, 48] and the reductions in IL-8 found by Troseid and colleagues [40] were associated with reductions in body mass index and waist circumference.
7.4.2 Secondary and Tertiary Prevention
Exercise (planned and structured physical activity) has been touted as a ‘polypill’ for chronic disease management [49] due to its ability to concomitantly improve the modifiable risk factors associated with the development of type 2 diabetes, cardiovascular disease and some cancers [16]. This includes improvements in atherogenic dyslipidemia [50], insulin resistance [51], hypertension [52], low-grade systemic inflammation [53], central obesity [54], and intrahepatic lipids [55].
Patients with cancer have an increased risk of developing co-morbid chronic diseases including chronic kidney disease (CKD) [56] and coronary heart disease [57], and can also have more cardiovascular disease risk factors than the general population [58]. Indeed, most exercise oncology research has focussed on secondary prevention of chronic conditions, and the modification of the disease- and treatment-related side effects of cancer. Level 1 evidence for the benefits of exercise for cancer patients and survivors indicates it improves psychological wellbeing and quality of life [59], cancer-related fatigue [60], physical functioning [61], body weight and composition [62], muscle strength and endurance [61, 62], immune function [63], and cardiovascular fitness [64].
Treatments for certain cancers, such as selective estrogen receptor modulators (SERMs) for breast cancer and androgen deprivation therapy for prostate cancer, can promote abnormal body composition by increasing fat mass and reducing lean muscle mass [65]. Observational studies have associated abnormal body composition with a poorer prognosis of cancer [66], including hepatocellular carcinoma [67]. Sarcopenia (age-associated loss of skeletal muscle mass and function) is also an independent predictor of mortality after controlling for body mass index, age and tumour stage (HR: 5.19; 95 % CI: 2.58, 10.43) [67]. Regular aerobic exercise training increases energy expenditure and induces lipolysis, which can reduce fat mass, while progressive resistance training induces muscular hypertrophy and prevents the loss of muscle mass commonly associated with hypo-caloric diets [68, 69].
Evidence for ‘exercise as medicine’ is emerging for a range of secondary sequelae from cancer and its treatments, such as cardiovascular disease [70]. For example, both cellular (e.g. mitigation of mitochondrial dysfunction [71] and reactive oxygen species emission from cardiac mitochondria [72]) and functional (e.g. attenuation of decrements in left ventricular function [73]) mechanisms are implicated in animal models to explain the protection from anthracycline-induced cardiotoxicity afforded by exercise.
Strong associations are also reported between type 2 diabetes and the incidence and prognosis of cancer, especially of the colon, liver and pancreas [74, 75]. Increases in plasma IGF-1 and IGF-2 as a result of hyperinsulinemia activate their respective receptors and initiate mitogenic behaviour within cancerous cells [76, 77]. Exercise training improves peripheral insulin sensitivity [76] and is the most potent stimulus to increase skeletal muscle glucose transporter 4 (GLUT4) expression and subsequent improvement of insulin action, glucose disposal and muscle glycogen storage [22]. In combination with nutritional and pharmacological interventions, exercise training can prevent the progression of impaired glucose tolerance and impaired fasting glucose (conditions indicative of pre-diabetes) to type 2 diabetes. For patients with type 2 diabetes, exercise training can decrease HbA1c levels [8, 78] and prevent further complications associated with poor glycaemic control such as renal and ophthalmic diseases [79].
The improvements in insulin sensitivity and body composition linked with exercise training further reduce the delivery of free fatty acids and glucose to the liver and are associated with improvement of non-alcoholic fatty liver disease (NAFLD). The benefits of exercise on NAFLD arise through numerous mechanisms involving the liver, muscle and adipose tissue, including the abovementioned activation of AMPK. For example, exercise-induced activation of AMPK reduces intrahepatic lipid content by inhibiting lipid synthesis and increasing fatty acid oxidation within the liver [80]. Insulin resistance is a hallmark feature of non-alcoholic steatohepatitis (NASH), a progressive form of NAFLD, characterised by inflammatory changes, hepatocyte ballooning and a variable degree of fibrosis. While there is no evidence demonstrating the reversal of NASH with exercise alone, exercise could prevent the progression of simple steatosis to NASH [81].
There are several other chronic diseases that can arise secondary to the disease- and treatment-related effects of cancer, such as chronic kidney disease CKD, osteoporosis and cognitive impairment. For example, there is a bidirectional relationship between the incidence of CKD and cancer [82]. Physical inactivity is a major risk factor for the development of CKD [83] and there is ‘probable’-grade evidence to suggest that exercise improves estimated glomerular filtration rate (eGFR) indicating an improvement in kidney function [84]. Initiation of androgen deprivation therapy (ADT) in men with prostate cancer is reported to result in a 5- to 10-fold increased loss of bone mineral density in multiple skeletal sites [85, 86]. This bone loss and accompanying decrease in muscle mass increases the risk of osteoporosis, falls, and fractures. Indeed, a fracture risk of up to 20 % is reported after 5 years on ADT, nearly twice the risk of healthy men or men with prostate cancer not receiving ADT [87]. This ADT-related increased risk of osteoporosis and osteoporotic fractures arises from the suppression of testosterone and oestrogen, two hormones that have vital direct and indirect roles in the regulation of bone metabolism [88] and microarchitectural decay [89]. Exercise training, specifically resistance training and impact-loading exercises that involve mechanical loading of the skeleton from ground reaction forces and muscle pull, can positively influence bone health [90]. However, while early results are encouraging [91], further research is needed to confirm the skeletal benefits of exercise during or after cancer treatment. Similarly, there is growing evidence to suggest that aromatase inhibitor therapy may be associated with long-term cognitive impairment in some cancer patients, especially in breast cancer survivors [92–94]. Exercise is well-known to improve cognitive function and prevent age- and disease-related cognitive decline, with recent evidence suggesting this may include oestrogen deficiency-induced cognitive impairment [95, 96].
7.4.3 Physical Activity Recommendations
Given that physical inactivity is the fourth leading cause of death due to non-communicable diseases (contributing to over three million preventable deaths per year [97]), it is an important target for the prevention of chronic diseases. Indeed, yielding a physical activity energy expenditure of 1000 kcal/week (a level considered ‘minimal adherence’ to physical activity guidelines as outlined below) is associated with a 20–30 % reduction in risk of all-cause mortality, with greater energy expenditures yielding further reductions [98–100]. Poor cardiorespiratory fitness is suggested to be a potent risk factor for all-cause mortality, cardiovascular disease [99] and the incidence of metabolic syndrome [100]. Importantly, improving cardiorespiratory fitness by just one MET is associated with 13 and 15 % reductions in all-cause mortality and risk of cardiovascular events, respectively [101], and these associations are independent of body mass [102].
Cancer survivors are advised to undertake 150 min per week of moderate or 75 min per week of vigorous aerobic exercise or an equivalent combination; and perform resistance exercise of moderate or high intensity on two or more days per week [103, 104]. Exercise prescription guidelines for a range of chronic conditions are available as position statements and reports from a variety of sources, including the American College of Sports Medicine and Exercise and Sports Science Australia. Consistent across all exercise guidelines for health and fitness is the recommendation for adults to undertake both aerobic exercise and progressive resistance training. Emerging evidence suggests that higher intensity exercise may achieve comparable or even superior benefits for a range of cardio-metabolic risk variables including cardiorespiratory fitness and glycaemic control [105] with less time commitment. Progressive resistance training is important for improvements in lean muscle mass, muscle strength and function [79] and may optimise insulin sensitivity; thus the current Australian guidelines for the prevention or management of type 2 diabetes advocate that at least 60 min of the recommended 210 min of moderate, or 125 min of vigorous intensity exercise be performed as progressive resistance training each week [79]. For more specific exercise prescriptions and for complex conditions where there are competing demands, referral to an exercise specialist is recommended to ensure the prioritisation of key components pertinent to the individual’s specific needs [e.g. Accredited Exercise Physiologists (Australia), Certified Exercise Physiologists (Canada) or Clinical Exercise Physiologists (United States of America)].
Despite the evidence for the effectiveness of physical activity in enhancing wellness irrespective of health status, people with chronic disease appear to be even less likely than the general population to meet physical activity guidelines e.g. only 12 % of prostate cancer survivors [106] meet contemporary exercise recommendations. Multi-faceted cognitive behavioural strategies to promote the uptake of lifestyle, environmental exposure, diet, exercise and medication recommendations are essential to successful behaviour change. These strategies enable people to modify their lifestyle by changing the way that they think about themselves, their behaviours and their circumstances [107]. While a detailed discussion of these is beyond scope, interventions that use the cognitive behavioural approach generally incorporate two or more of the following processes: mutual goal setting; increasing self-awareness through self-monitoring of enablers and barriers to change; frequent and prolonged contact through scheduled follow-up; feedback and reinforcement by health professionals to guide behaviour; enhancement of self-efficacy; exposure to credible role-modelling; mutual problem solving; and motivational interviewing comprising goal-oriented and individualised counselling [107]. Research demonstrates that when two or more of these strategies are used, particularly favourable results are attained [107].
The following recommendations are provided to encourage increased physical activity of individuals, including those with chronic disease:
-
1.
Referral to exercise professionals specialising in disease-related exercise e.g. clinical exercise physiologists, is recommended to ensure safe, individualised, supervised exercise programs are prescribed to cancer patients and survivors.
-
2.
If individuals are currently sedentary or have low levels of physical activity, build gradually towards the physical activity guidelines.
-
3.
Encourage the incorporation of active transport into the daily routine, such as walking or cycling rather than driving a car.
-
4.
The use of activity trackers can be recommended as an objective tool to enable self-monitoring and gradual improvements in physical activity e.g. 10 % in average steps per week.
-
5.
Encourage individuals to break up long periods of sitting as often as possible and be aware of time spent in front of the computer screen.
At the community level, the following environmental changes and policy-related activities are suggested to increase physical activity, prevent disease or promote health in groups of people [108]:
-
1.
Using the media to deliver community-wide, large-scale, multicomponent physical activity campaigns.
-
2.
Implementing point-of-decision prompts (e.g. signs posted by elevators and escalators) to encourage use of stairs.
-
3.
Focus on building, strengthening, and maintaining social networks to enhance social support interventions in community settings.
-
4.
Creation of or enhanced access to places for physical activity combined with informational outreach activities.
-
5.
Street- or community-scale urban design (e.g. ensuring sidewalk continuity) and land-use policies (e.g. mixed land-use zoning) and practices to support physical activity participation.
-
6.
Transportation and travel policies and practices to encourage active transport by facilitating walking, bicycling, and public transportation use.
7.5 Nutrition, Cancer and Chronic Disease
Nutrition can have a profound impact on both cancer and chronic diseases because the same nutritional deficiencies or excesses that increase the risk of cancer can also initiate or enhance susceptibility to the chronic degenerative diseases of ageing such as diabetes, cardiovascular disease and dementia [109]. An example at the micronutrient level is folate deficiency, which increases the risk of colorectal, breast, ovary, pancreas, brain, lung and cervical cancers [110] as well as neural tube defects and anaemia [111]. The reason folate deficiency is associated with cancer is because it causes a high level of DNA damage (e.g. DNA strand breaks, chromosome aberrations, micronuclei), chromosomal instability and DNA hypomethylation, which accelerates the number of cells with abnormal genomes and/or epigenomes from which cancers can evolve [110, 112]. In addition, folate deficiency causes an elevation in homocysteine concentration, which is a risk factor for diabetic retinopathy and nephropathy in type 1 diabetes, cardiovascular disease and dementia [111, 113–115]. At the macronutrient level, the available evidence suggests that excess caloric intake leading to obesity could increase the risk for several cancers (e.g. oesophagus, breast, prostate, pancreas and colorectum), as well as the propensity to develop diabetes, cardiovascular disease and cognitive impairment [12, 116–118]. The mechanism by which obesity increases the risk of cancer, diabetes cardiovascular disease and cognitive decline is not clear but obesity and all of the above chronic conditions are associated with increased DNA damage at the chromosomal, telomere, and mitochondrial DNA level. This suggests a common DNA damage mechanism, which is most likely to be a combination of increased oxidative stress due to inflammation, excessive intake of dietary genotoxins and perhaps deficiency in the micronutrients needed for DNA replication and/or repair [98, 112, 119–121]. Furthermore, as indicated above, obesity increases IGF-1 and IGF-2, which may promote the growth of initiated cancer cells.
A significant cause of cancer is damage to the genome leading to abnormal gene expression [122–127]. DNA damage can occur at the chromosomal, gene sequence, telomere and mitochondrial DNA level and could also involve alterations in DNA methylation, which accelerate the evolution of the genomically unstable cells that can more easily transform into cancers and divide abnormally. In this regard, from a cancer prevention perspective, nutrition is important in ensuring healthy cell function and reproduction with respect to the supply of:
-
1.
Co-factors required for DNA synthesis (e.g. folate, vitamin B12, vitamin B6)
-
2.
Co-factors required for DNA repair (e.g. niacin, zinc, magnesium)
-
3.
Antioxidants to prevent oxidation of DNA (e.g. vitamin C, lycopene, polyphenols)
-
4.
Methyl donors to maintain epigenetic control of gene expression (e.g. folate, choline)
-
5.
Natural or man-made genotoxins that damage DNA (e.g. hetrocyclic amines, alcohol)
-
6.
Excess calories that promote obesity and oxidative stress
-
7.
Phytonutrients that promote apoptosis of cells with damaged DNA (e.g. retinoids, polyphenols)
-
8.
Nutrients that may promote the growth of initiated cancers (e.g. methionine, folic acid).
Figure 7.1 summarises the impact of key nutrient deficiencies that can affect genome integrity via multiple mechanisms. These include the defective maintenance of methylated DNA, causation of damage to DNA bases, and impairment of DNA repair leading to chromosomal instability and aberrant karyotypes which fuel the evolution of malignant cancers [112, 127].
The 2014 World Cancer Research Fund report provides the most comprehensive assessment of the level of evidence for the impact of nutrition on reducing or increasing cancer risk [13]. Tables 7.1 and 7.2 provide a summary of the key outcomes of the meta-analyses that were performed with regards to food and beverage groups and some of the minor dietary components that also affect the risk of other degenerative diseases (e.g. salt, which also affects cardiovascular disease risk and mortality). Based on current evidence, there is (i) convincing evidence that increased intake of foods contaminated with aflatoxins, red meat and processed meat, water contaminated with arsenic, alcoholic drinks, and high dose beta-carotene supplements increase the risk of cancer and (ii) evidence of a probable decreased risk for cancer with increased intake of plant foods including those rich in fibre (cereals, grains, roots, tubers, plantains) and non-starchy vegetables, fruits, pulses, legumes, nuts, seeds, herbs, spices. In addition, breastfeeding (lactation) is convincingly associated with reduced breast cancer risk of the mother and more recently evidence has emerged that childhood leukaemia incidence could be reduced by breastfeeding for 6 months or more [128, 129].
Although there is some evidence that certain dietary patterns (e.g. Mediterranean diet [130]) protect against cardiovascular disease, dementia and cancer there are too few robustly-designed epidemiological prospective studies to provide convincing evidence that a specific dietary pattern aggravates cancer risk to a significantly different extent, relative to another dietary pattern. The main difficulty is that even within a single dietary pattern there can be large differences in micronutrient composition and caloric intake, depending on the food items within the same food group that are included in the pattern. For example, in the case of vegetables one would have to consume 2.5 kg per day if choosing roots, tubers and ‘fruit’ vegetables but only 0.4 kg per day if one consumed pulses, legumes, leafy and cruciferous vegetables to achieve the recommend intake of folate [131]. Therefore it is plausible that the choice of vegetables influences micronutrient intake and possibly cancer risk. With regards to flesh foods, in October 2015, based on robust epidemiological evidence and strong mechanistic plausibility, the WHO International Agency for Research on Cancer (IARC) classified consumption of processed meat as “carcinogenic to humans” (Group 1 carcinogen) and consumption of red meat as “probably carcinogenic to humans” (Group 2A carcinogen) [132]. This provides an important indication for choosing dietary patterns that are mainly plant-based and low in processed meat and/or red meat. The consumption of alcoholic drinks varies between cultures and has one of the most profound impacts on cancer risk, particularly amongst those with genetic defects in detoxifying acetaldehyde [133, 134], a genotoxic metabolite generated directly from alcohol in the body, which has been classified as a Group 1 carcinogen by IARC [135, 136].
Intake of alcoholic drinks is convincingly associated with cancers of the mouth, pharynx, larynx, oesophagus, colorectum (in men), breast (pre- and post-menopausal) and probably with liver and colorectum (women) [132]. The consumption of alcoholic drinks varies between cultures and has one of the most profound impacts on cancer risk, particularly amongst those with genetic defects in the ALDH2 enzyme required to detoxify acetaldehyde, a genotoxic metabolite generated directly from alcohol in the body. Acetaldehyde has been classified as a Group 1 carcinogen by IARC [133, 135, 136]. Acetaldehyde exerts its carcinogenic effects via a genotoxicity mechanism which causes DNA adducts, DNA-protein cross-links, chromosome aberrations and micronuclei and these effects are stronger in those with defective capacity in detoxifying acetaldehyde to acetate or if cells are deficient in folate [133, 134, 137–139].
To date, there is no conclusive direct evidence to support the association of caloric intake with human cancer risk, even though it is evident from several studies that caloric restriction appears to increase life-span and postpone the onset of degenerative diseases across mammalian species [140, 141]. Therefore, current guidelines suggest that irrespective of whether an individual is at the primary, secondary or tertiary stage of chronic disease prevention, all individuals should eat a diet consistent with the relevant national guidelines and avoid physical inactivity. Table 7.3, which is adapted from the World Cancer Research Fund guidelines, outlines lifestyle recommendations germane to most chronic conditions.
7.6 Reducing Body Fatness: The Synergy of Diet and Exercise in Preventing Chronic Disease Risk
Obesity, the excessive accumulation of body fat, is associated with the development of many chronic diseases. The central distribution of excess body fat (i.e., increased levels of visceral adipose tissue) and the ectopic storage of excess fat (e.g., within the liver, pancreas and muscle) are particularly linked to an increased risk of cardiometabolic disease [142–144]. As pharmacological agents do not specifically reduce fat from these regions, or are unsuitable for the long-term treatment of obesity, the synergy of diet and exercise is the cornerstone of obesity management.
7.6.1 Dietary Interventions to Prevention of Body Fat Gain and Promote Body Fat Loss
The most successful dietary interventions to prevent weight gain or promote weight loss are generally based on dietary patterns that meet nutritional requirements for health without excess calories, or marginally fewer calories (in the case of weight loss) than what is needed to meet energy requirements or achieve energy balance [145–147]. Good examples are the Mediterranean diet and the Dietary Approaches to Stop Hypertension [DASH] program. Weight loss in those who are overweight or obese can be achieved by reducing the portion sizes of habitual foods or by replacing high caloric density foods that are poor in micronutrients with foods containing less calories, but which are richer in vitamins and other essential micronutrients [148, 149].
A higher intake of plant foods is usually associated with leaner body mass [150, 151]. Evidence is also accumulating in support of novel higher-protein (>20 % of energy) diets for successful weight loss maintenance and the prevention of type 2 diabetes [152, 153]. Higher protein and plant-based diets have the advantage of having relatively low energy density and aiding longer-term appetite suppression [150, 151, 153]. Success in caloric restriction is improved by selecting foods that are most effective with respect to satiety. A recent systematic review found ‘probable’ evidence for high intake of dietary fibre and nuts predicting less weight gain, and for high intakes of meat in predicting more weight gain [154].
Low calorie meal replacements provide a practical approach to achieving and maintaining successful control of body weight and preventing weight regain in the longer term [155, 156]. Although there are concerns about weight cycling due to difficulty in maintaining a lower or healthier body weight, Level 1 evidence indicates that the risks related to weight cycling, cancer or cardiometabolic disease and mortality is small, if not non-existent [157, 158].
The WHO recommendations to prevent weight gain are as follows [159]:
-
Energy intake (calories) should be in balance with energy expenditure. Total fat should not exceed 30 % of total energy intake to avoid unhealthy weight gain, with a shift in fat consumption away from saturated fats to unsaturated fats, and towards the elimination of industrial transfats.
-
Limiting intake of free sugars to less than 10 % of total energy intake is part of a healthy diet. A further reduction to less than 5 % of total energy intake is suggested for additional health benefits.
7.6.2 Physical Activity Recommendations for Reducing and Preventing Increases in Body Fatness
Physical activity can also prevent an increase in body fatness, in particular visceral adipose tissue, which is linked with numerous chronic health conditions including type 2 diabetes [160, 161], non-alcoholic fatty liver disease [162], and cardiovascular disease [163], as well as several cancers (Table 7.2). Increased levels of physical activity independently predict lower waist circumference (a clinical indicator of central fat distribution, which includes both subcutaneous and visceral adipose tissue) [164]. Moreover, epidemiological data indicate that for individuals with the same body mass index, those with moderate levels of cardiorespiratory fitness have lower levels of total and visceral adipose tissue than their less fit counterparts [165].
Evidence indicates that 150–250 min/week of moderate intensity physical activity effectively prevents weight gain in adults [69]; however, while physical activity alone can lead to small reductions in weight [166], the volume required to lose weight with exercise alone is much larger in the absence of concomitant caloric restriction. The current recommendation for weight loss and the maintenance of weight reduction recommend 60 min per day of low-moderate intensity exercise, totalling ~470 min per week [69].
While caloric restriction is the most effective method for achieving weight reduction [167], epidemiological evidence indicates that physical activity plays an important role in the prevention of weight regain, with 90 % of individuals who have successfully maintained weight loss for over 5 years reporting an average of 60 min of exercise per day (mostly walking) [168]. Furthermore, Level 1 evidence indicates that the benefits of aerobic exercise aerobic on visceral adipose tissue reduction [54, 169] can occur at levels below those currently recommended for weight reduction [54]. While the evidence for resistance training for the reduction of visceral adipose tissue is less clear [54, 62], resistance training is the only antidote for muscle loss associated with caloric restriction [170]. Therefore, the combination of caloric restriction and increased physical activity is undoubtedly the most effective method for weight loss and body fat reduction.
7.7 Pharmacoprevention
Pharmacoprevention is the use of drugs to reduce the risk of chronic diseases and cancer [171]. In this section, we begin with a discussion of drugs known to prevent cancer or its recurrence. This is followed by an exploration of the drugs used to prevent or manage the chronic diseases that can develop in cancer patients as a result of their cancer treatment, and drugs that offset the impact of cancer treatments on comorbid chronic conditions.
7.7.1 Prevention of Primary Cancer and Cancer Recurrence
In terms of cancer prevention, the most rigorous evidence for prevention applies only to the primary prevention of breast cancer, where risk is high in the following circumstances [171]:
-
Multiple relatives affected by breast cancer or ovarian cancer on the same side of the family
-
Younger age (i.e. under 40 years) at cancer diagnosis
-
Relative with an identified mutation in a high-risk breast cancer gene, e.g. BRAC1 or BRAC2
-
Relatives affected by bilateral breast cancer
-
Breast and ovarian cancer in the same relative
-
Ashkenazi Jewish ancestry.
The selective oestrogen receptor modulators (SERMS) tamoxifen and raloxifene are the most common pharmacopreventatives. Both drugs interfere with the carcinogenic actions of oestrogen on breast tissue. Tamoxifen reduces the risk of pre- and post-menopausal women developing oestrogen receptor-positive breast cancer where there is a family history of the disease [171]. Raloxifene is used only in post-menopausal women [172], and has the incidental benefit of reducing the risk of osteoporotic fractures. While they do reduce risk by up to 40 % [171] in the target population, SERMS ultimately have no effect on mortality [172] and are not useful in the case of oestrogen receptor-negative breast cancers.
Aromatase inhibitors: Drugs could also have a role in reducing the risk of cancer recurrence in women previously treated for breast cancer. Aromatase inhibitors such as exemestane, letrozole and anastrozole are currently used to treat hormone receptor–positive breast cancers in postmenopausal women. These drugs decrease oestrogen levels by interfering with the ability of the aromatase enzyme produced by body fat to change naturally circulating androgen into oestrogen. Hence aromatase inhibitors are only useful in post-menopausal women, whose ovaries no longer produce oestrogen. The National Cancer Institute guidelines recommend [172] the use of aromatase inhibitors to reduce the incidence of breast cancer in postmenopausal women with an increased risk (i.e., aged over 60 years, previous ductal carcinoma in situ with mastectomy, or a Gail 5-year risk score >1.66) [172]. The Australian guidelines, on the basis of Level 2 evidence, also recommend their use [173].
Metformin: The literature often states, based on the results of some epidemiological studies, that individuals with type 2 diabetes or insulin resistance are not only at risk of type 1 diabetes and its attendant comorbidities, they are also at risk of developing a range of cancers (primarily cancer of the pancreas, colon and liver) [174]. At this stage, however, the evidence of a causal association between diabetes and cancer is poor [175], as the findings of these studies are predominantly retrospective and non-randomised [176]. If there is a definite association, it could be the result of a common risk factor: body fatness. High levels of body fat, cancer and type 2 diabetes are all associated with increased production of insulin-like growth factor, a hormone critical to cell growth, proliferation and death. This has led to further suggestion that metformin, most commonly used as an anti-hyperglycaemic and insulin sensitiser in type 2 diabetes, could also inhibit the growth and metabolic processes of cancer cells [174]. It therefore is considered a potentially viable agent to prevent cancer, with many clinical trials currently underway [176].
As with all medications, cancer preventives do not come without chronic disease risks of their own. Tamoxifen is associated with the development of endometrial cancer and both drugs are implicated in thromboembolic events [171, 172]. Fortunately both side effects are relatively rare. Aromatase inhibitors accelerate osteoporosis and affect lipid metabolism [173]. More importantly, hormone modulation induces symptoms of menopause, which are often more sudden and more severe than in natural menopause [177]. These side effects influence adherence to the therapy [173], which in turn influences risk reduction, because to achieve their effect these drugs must be taken for 5 years. 46 % of women prescribed tamoxifen do not complete their 5-year course [173].
7.7.2 Drugs to Prevent Development of Other Chronic Diseases After Cancer Treatment
Table 7.2 outlines the chemotherapy drugs most strongly associated with the subsequent development of cardiotoxicity, especially heart failure, after cancer treatment. Anthracyclines and trastuzamab are the agents most commonly associated with cardiotoxicity. Anthracycline chemotherapy is thought to disrupt the normal catalytic cycle of topoisomerase 2β, resulting in mitochondrial dysfunction, the generation of free radicals and DNA disruption. Because it results in cardiomyocyte death, it is largely irreversible [178, 179]. Trastuzamab cardiotoxicity is thought to result from the disruption of the cellular repair pathways the enable cardiomyocyte contractility, causing reversible cell dysfunction rather than cell death [180]. Radiotherapy, if incidentally delivered in the cardiac field, is associated with coronary arteritis and atherosclerosis up to 15 years from treatment completion [180]. Underlining the synergistic nature of cancer, cancer treatments and other chronic diseases, many of the known risk factors for developing chemotherapy-induced cardiotoxicity are remarkably similar to those for developing cardiovascular disease; namely pre-existing cardiovascular symptoms, family history, diabetes, dyslipidaemia and obesity [178].
Dexrazoxane, an iron-chelating agent, is thought to be cardioprotective during chemotherapy in two ways. The first is by interfering with the iron-mediated generation of free radicals associated with the administration of anthracycline chemotherapy [178, 180]; the second involves interference with anthracycline’s ability to inhibit topoisomerase 2β, which results in cell death. A meta-analysis of cardioprotective agents for anthracycline chemotherapy published in 2011 [181] reported ambiguous results for dexrazoxane. While the analysis demonstrated a statistically significant benefit in favour of dexrazoxane for the occurrence of subsequent heart failure, it could not determine differences in survival between the intervention and control groups [181]. A subsequent meta-analysis by Kalem and Marwick [182], however, demonstrated that dexrazoxane given prophylactically to asymptomatic patients receiving chemotherapy could usefully lessen the burden of subsequent cardiotoxicity.
Beta blockers and ACE inhibitors: Based on good evidence, for many years diabetes [183], cardiovascular disease [184, 185] and kidney [186] guidelines have recommended the use of anti-hypertensives to mitigate the risk of renal or cardiovascular comorbidities. More recently, these drugs have played a role in some cancer treatments. The European Guidelines for Medical Oncology (ESMO) note that patients receiving potentially cardiotoxic chemotherapy have a high risk of developing heart failure and could be considered ‘Stage A’ or asymptomatic heart failure patients [180]. There is therefore a potential role for heart failure drugs during and after cancer treatment, especially angiotensin agonists (ACE-I) and beta blockers. This role was confirmed by a meta-analysis reporting the efficacy of ACE-Is and beta blockers in reducing the incidence of anthracycline-induced cardiotoxicity in patients who were asymptomatic during chemotherapy [182].
Statins have had a long-standing role in reducing the risk of hypertension in individuals pre-disposed to high cholesterol levels, but they are also increasingly used in the primary prevention of cardiovascular disease after cancer treatment. A recent meta-analysis confirmed the potential for statins to prevent cardiotoxicity in asymptomatic patients receiving cardiotoxic cancer treatments [182]. The cardioprotective action of statins in this context is attributed to their capacity to reduce the oxidative stress and cellular inflammation that result from chemo- and radiotherapy, and to delay myocyte apoptosis [182]. It is sometimes argued that cholesterol-lowering drugs, which coincidentally antagonise the cellular processes that control the initiation, growth and metastasis of tumours, could also help prevent melanoma [187], and colorectal [187] and prostate [188] cancers. However this argument is not supported by rigorous evidence, with some experts arguing that the results of animal studies imply that statins are in fact “carcinogenic” [189], and that case-control [189] and placebo-controlled studies [190] in humans indicate that statin therapy is actually associated with a higher incidence of cancer.
7.7.3 Drugs that Offset the Impact of Cancer Drugs on Co-existing Chronic Conditions
Beta blockers and ACE inhibitors: There is strong evidence that beta blockade and ACE-I therapy initiated within 2 months of chemotherapy completion in patients with confirmed anthracycline-induced cardiomyopathy can reverse left ventricular dysfunction [180]. The same recommendations apply to trastuzamab- and radiotherapy-induced cardiac dysfunction [180]. The precise mechanism of action is unknown, but could be because both drugs reduce cardiac afterload [182]. Angiotensin inhibitors also have complex beneficial interactions with cardiomyocyte angiotensin 2 receptors and epidermal growth factors; whilst beta blockers have potential antioxidant effects [182].
Aspirin: Antiplatelet therapy, in conjunction with a healthy lifestyle, can diminish the risk of cardiovascular disease [191, 192]. Mostly recommended in the form of low-dose aspirin, like all drugs it is not without side effects and these must be weighed against its benefits. Low-dose aspirin is recommended for individuals with established cardiovascular disease, or those who have known cardiovascular risk factors (such as previous anthracycline therapy for cancer), to reduce the risk of non-fatal myocardial infarction and non-fatal stroke [193]. This recommendation is made only where an overall benefit exists and clearly outweighs the harm of gastrointestinal bleeding and haemorrhagic stroke. There is no evidence to support the prophylactic use of aspirin in individuals who do not have cardiovascular risk factors [193]. Some studies raise the possibility of aspirin providing protection against colon cancer after five years of use; however the many methodological limitations of these studies mean that the evidence for this use of aspirin is poor.
7.8 Environmental Risk Reduction
7.8.1 Radiation Exposure
Radiation risks fall into two categories: those associated with ionising radiation and those associated with solar and ultraviolet radiation (sun) exposure. Ionising radiation is particularly associated with the development of many malignancies of the blood and solid tissue, and with the DNA damage that leads to a variety of other genetically-based chronic conditions. Exposure to ionising radiation apart from radiotherapy is beyond the lifestyle focus of this chapter. More amenable to lifestyle modification is sun exposure, which is limited to cancer risk.
Solar radiation and ultraviolet (UV) radiation from UV-emitting tanning devices are considered Class 1 carcinogens [194], which are particularly implicated in the development of primary cutaneous malignant melanomas and non-melanocytic skin cancers [195]. Radiotherapy is also innately carcinogenic and is routinely associated with the development of second primary cancers such as melanoma [196]. Although a recent systematic review determined that only a relatively small proportion of second cancer is associated with radiotherapy [197], nonetheless, radiotherapy and some common chemotherapy treatments such as 5-fluorouracil, methotrexate and doxorubicin tend to increase sun sensitivity in the treatment period, and for some time after treatment. Hence the standard preventive approaches of limiting exposure to intense sunlight, regular use of broad spectrum sunscreen, wearing wide-brimmed hats, sunglasses and loose clothing, and avoidance of solarium beds are as critical during treatment as they are before and after cancer treatment [195].
7.8.2 Viral Infections
Many infectious agents induce chronic diseases such as tuberculosis, malaria, some cancers and HIV-AIDS. For example, between 3.3 and 16 % of all cancers are attributed to viral infections [198]. Infectious agents induce long-term conditions in three ways [199]. The first is through progressive tissue pathology or organ decompensation, e.g. when the hepatitis B virus induces chronic liver disease. The second is a result of the initial infection causing permanent lifestyle deficits or disabilities, e.g. poliomyelitis-induced paralysis. The third is by predisposing individuals to chronic outcomes. This is a complex pathway exemplified by maternal infection during pregnancy, which in turn leads to pre-term delivery, that, even when the infant is not infected, increases the child’s subsequent risk of respiratory and neurological disabilities [199].
As O’Connor et al. [199] argue, understanding these viral pathways and their synergies affords many opportunities to reduce the impact of chronic disease before its outcomes are irreversible. For example, some forms of the sexually-transmitted human papillomavirus (HPV) are classified as Class I carcinogens, implicated in the development of cancers of the genital organs and the oropharyngeal and anal regions [198]. Infection with the hepatitis B (HBV) and hepatitis C (HCV) viruses, which involve sexual and/or blood-to-blood contact, not only induces chronic liver disease but substantially increases the risk of developing liver cancer, with 80 % of all primary liver cancers associated with hepatitis infection [200]. Gastric cancers are strongly associated with helicobacter pylori infection [201].
Inevitably, lifestyle factors working in synergy with these biological agents potentiate risk; hence lifestyle modification again has the potential to positively affect global health outcomes, especially where these cancers are concerned. Safe sexual and drug injection practices substantially modify the risks of HBC and HPV infection [198]; vaccination helps protect against HBV and HPV [198]; while studies indicate that a high salt intake could work in synergy with helicobacter to potentiate the risk of gastric cancer [201].
7.9 Encouraging Uptake of Preventive Strategies
Much of the information presented in this chapter is not novel. We know intuitively and from rigorous evidence that lifestyle behaviours affect health. We understand that people have the highest risk of chronic disease when they have several adverse determinants of health. It is equally clear that lifestyle modification and medications can help prevent and modify the risk of chronic disease. But we also know that these factors interact in complex ways. The problem is that there are many desirable behaviour targets: exercise, diet, smoking behaviours, sun avoidance, medication adherence, and sexual practices. Targeting a single behaviour in a time- and resource-poor clinical environment could exclude other, equally important lifestyle variables. The World Health Organisation emphasise that a combination of interventions is often needed to realise the full potential of risk reduction strategies in the context of chronic disease [1]. Moreover, strategies that account for several risk factors at once tend to be more cost-effective than those that only address a single risk factor [1, 3].
The other problem is that making the necessary lifestyle changes is not easy, nor even particularly attractive in a societal context that values novel, highly technical interventions; where 60 % of the population have low levels of health literacy [202]; and when the most socially-disadvantaged are at highest risk because they have less access to health education and services, less opportunity to exercise, and fewer healthy food options [203]. The difficulties in instilling behaviour changes are underscored by the latest Australian census data, which are typical of developed countries. For example, 63 % of men and 73 % of Australian women are either sedentary or engage in the lowest levels of exercise [204]. These levels are incompatible with health. There is also a clear trend in the Australian population to the heavier end of the body mass index, with 70 % of men and 56 % of women now classed as overweight or obese [204]. The Australian Bureau of Statistics (2015) attributes this to “an imbalance between energy consumed and energy expended”, a situation not helped by the high Australian rates of alcohol consumption. The census data for 2011–2012 reveal that 29 % of Australian men and 10 % of Australian women have self-reported ‘risky’ alcohol intakes, which indicates a small but significant increase from previous years [204]. Fortunately, the incidence of tobacco smoking has decreased, but given it is considered the largest single preventable cause of cancer and chronic disease [204], the current rates of 20 % for men and 16 % for women remain problematic [204]. In addition, while medications are therapeutic, they often come with a range of unpleasant or undesirable side effects that individuals might consider outweigh any benefits they confer. How to select which of the many determinants and behaviours to target, how to promote the uptake of those behaviours, and how to ensure adherence, are discussed in the remainder of this chapter.
7.9.1 Adherence
The factors that affect sustained uptake of preventive interventions are remarkably similar to those that determine health status. These are socio-economic, health system, therapy-related, patient-related and condition-related factors [205]. Hence strategies to enhance adherence to medication, lifestyle and other changes need to be equally multifaceted. Despite this complexity, the American College of Preventive Medicine [205] argues that interventions to promote adherence can and should be simple, and that simple interventions are often the most cost-effective. The College recommends the “SIMPLE” approach to improve adherence to medication, but this approach is equally useful in sustaining all of the behaviour changes discussed in Table 7.4.
7.10 Conclusion
Human behaviours are powerful factors that increase or reduce the risk of developing common chronic conditions and cancer at the primary, secondary and tertiary levels. While many drugs have the potential to limit the risk of chronic disease and cancer, the most feasible and economic determinants of health to target are often lifestyle-related. Although it can be difficult to persuade people to change their lifestyles and to sustain that change, it is worth the effort. Many health-promoting lifestyle practices have numerous benefits, operating in synergy to modify risk. In particular, good nutrition and optimum physical activity tend to work in a complementary way to reduce body fatness, which along with tobacco smoking and high alcohol intakes, embodies an enormous risk to health.
References
World Health Organisation (WHO) (2005) Preventing chronic diseases: a vital investment. WHO, Geneva
Australian Institute of Health and Welfare (AIHW) (2014) Preventing and treating ill health. AIHW, Canberra
Australian Institute of Health and Welfare (AIHW) (2015) Health behaviours and their role in the prevention of chronic disease. http://www.aihw.gov.au/chronic-disease/risk-factors/ch1/. Accessed 20 Jan 2016
World Health Organisation (WHO) (2004) Global Forum on chronic disease prevention and control. WHO, Geneva
World Cancer Research Fund International (2016) Continuous update project. http://www.wcrf.org/int/research-we-fund/continuous-update-project-cup. Accessed 20 Feb 2016
Naci H, Ioannidis JPA (2013) Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ Brit Med J. 347:f5577 (10/0108/22/accepted 2013)
Aarsland D, Sardahaee FS, Anderssen S, Ballard C (2010) Is physical activity a potential preventive factor for vascular dementia? A systematic review. Aging Ment Health 14(4):386–395
Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ (2001) Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA 286(10):1218–1227
Thomas DE, Elliott EJ, Naughton GA (2006) Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev 3:Cd002968
Pearson TA, Blair SN, Daniels SR et al (2002) AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 106(3):388–391
Fletcher GF, Balady G, Blair SN et al (1996) Statement on exercise: benefits and recommendations for physical activity programs for all Americans. A statement for health professionals by the Committee on Exercise and Cardiac Rehabilitation of the Council on Clinical Cardiology, American Heart Association. Circulation 94(4):857–862
Eheman C, Henley SJ, Ballard-Barbash R et al (2012) Annual Report to the Nation on the status of cancer, 1975–2008, featuring cancers associated with excess weight and lack of sufficient physical activity. Cancer 118(9):2338–2366
World Cancer Research Fund and American Institute for Cancer Research (WCRF/AICR) (2010) Continuous update project report summary: food, nutrition and physical activity and the prevention of breast cancer. 2014
World Cancer Research Fund/American Institute for Cancer Research (2011) Continuous update project report. Food, nutrition, physical activity, and the prevention of colorectal cancer. http://www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports/colorectal-bowel-cancer. Accessed 22 Feb 2016
World Cancer Research Fund International (2013) Continuous update project report. Food, nutrition, physical activity, and the prevention of endometrial cancer. http://www.dietandcancerreport.org
Pedersen L, Christensen JF, Hojman P (2015) Effects of exercise on tumor physiology and metabolism. Cancer J 21(2):111–116
Betof AS, Dewhirst MW, Jones LW (2013) Effects and potential mechanisms of exercise training on cancer progression: a translational perspective. Brain Behav Immun 30(Suppl):S75–S87
Ballard-Barbash R, Friedenreich CM, Courneya KS, Siddiqi SM, McTiernan A, Alfano CM (2012) Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst 104(11):815–840
Buffart LM, Galvao DA, Brug J, Chinapaw MJ, Newton RU (2014) Evidence-based physical activity guidelines for cancer survivors: current guidelines, knowledge gaps and future research directions. Cancer Treat Rev 40(2):327–340
Chi F, Wu R, Zeng YC, Xing R, Liu Y (2013) Circulation insulin-like growth factor peptides and colorectal cancer risk: an updated systematic review and meta-analysis. Mol Biol Rep 40(5):3583–3590
Devin JL, Bolam KA, Jenkins DG, Skinner TL (2015) The influence of exercise on the insulin-like growth factor axis in oncology: physiological basis, current, and future perspectives. Cancer Epidemiol Biomarkers Prev
Richter EA, Hargreaves M (2013) Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev 93(3):993–1017
Hardie DG, Ross FA, Hawley SA (2012) AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol Cell Biol 13(4):251–262
Jiang W, Zhu Z, Thompson HJ (2009) Effects of physical activity and restricted energy intake on chemically induced mammary carcinogenesis. Cancer Prev Res (Phila) 2(4):338–344
Dranoff G (2004) Cytokines in cancer pathogenesis and cancer therapy. Nat Rev Cancer 4(1):11–22
Hiscott J, Ware C (2011) Cytokines. Curr Opin Immunol 23(5):561–563 (10)
Lippitz BE (2013) Cytokine patterns in patients with cancer: a systematic review. Lancet Oncol 14(6):e218–e228
Chan MH, Carey AL, Watt MJ, Febbraio MA (2004) Cytokine gene expression in human skeletal muscle during concentric contraction: evidence that IL-8, like IL-6, is influenced by glycogen availability. Am J Physiol Regul Integr Comp Physiol 287(2):R322–R327
Louis E, Raue U, Yang Y, Jemiolo B, Trappe S (2007) Time course of proteolytic, cytokine, and myostatin gene expression after acute exercise in human skeletal muscle. J Appl Physiol (1985) 103(5):1744–1751
Akerstrom T, Steensberg A, Keller P, Keller C, Penkowa M, Pedersen BK (2005) Exercise induces interleukin-8 expression in human skeletal muscle. J Physiol 563(Pt 2):507–516
Nieman DC, Davis JM, Henson DA et al (2003) Carbohydrate ingestion influences skeletal muscle cytokine mRNA and plasma cytokine levels after a 3-h run. J Appl Physiol (1985) 94(5):1917–1925
Ali MH, Schlidt SA, Chandel NS, Hynes KL, Schumacker PT, Gewertz BL (1999) Endothelial permeability and IL-6 production during hypoxia: role of ROS in signal transduction. Am J Physiol 277(5 Pt 1):L1057–L1065
Ito K, Hanazawa T, Tomita K, Barnes PJ, Adcock IM (2004) Oxidative stress reduces histone deacetylase 2 activity and enhances IL-8 gene expression: role of tyrosine nitration. Biochem Biophys Res Commun 315(1):240–245
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82(1):47–95
Kim YM, Reed W, Wu W, Bromberg PA, Graves LM, Samet JM (2006) Zn2+-induced IL-8 expression involves AP-1, JNK, and ERK activities in human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol 290(5):L1028–L1035
Yamamoto S, Shimizu S, Kiyonaka S et al (2008) TRPM2-mediated Ca2+ influx induces chemokine production in monocytes that aggravates inflammatory neutrophil infiltration. Nat Med 14(7):738–747
Pedersen BK, Akerstrom TC, Nielsen AR, Fischer CP (2007) Role of myokines in exercise and metabolism. J Appl Physiol (1985) 103(3):1093–1098
Frydelund-Larsen L, Penkowa M, Akerstrom T, Zankari A, Nielsen S, Pedersen BK (2007) Exercise induces interleukin-8 receptor (CXCR2) expression in human skeletal muscle. Exp Physiol 92(1):233–240
Della Gatta PA, Garnham AP, Peake JM, Cameron-Smith D (2014) Effect of exercise training on skeletal muscle cytokine expression in the elderly. Brain Behav Immun 39:80–86 (7)
Troseid M, Lappegard KT, Claudi T et al (2004) Exercise reduces plasma levels of the chemokines MCP-1 and IL-8 in subjects with the metabolic syndrome. Eur Heart J 25(4):349–355
Croft L, Bartlett JD, MacLaren DP et al (2009) High-intensity interval training attenuates the exercise-induced increase in plasma IL-6 in response to acute exercise. Appl Physiol Nutr Metab 34(6):1098–1107
Ambarish V, Chandrashekara S, Suresh KP (2012) Moderate regular exercises reduce inflammatory response for physical stress. Indian J Physiol Pharmacol 56(1):7–14
Fischer CP, Plomgaard P, Hansen AK, Pilegaard H, Saltin B, Pedersen BK (2004) Endurance training reduces the contraction-induced interleukin-6 mRNA expression in human skeletal muscle. Am J Physiol Endocrinol Metab 287(6):E1189–E1194
Gokhale R, Chandrashekara S, Vasanthakumar KC (2007) Cytokine response to strenuous exercise in athletes and non-athletes–an adaptive response. Cytokine 40(2):123–127
McTiernan A, Tworoger SS, Ulrich CM et al (2004) Effect of exercise on serum estrogens in postmenopausal women: a 12-month randomized clinical trial. Cancer Res 64(8):2923–2928
McTiernan A (2008) Mechanisms linking physical activity with cancer. Nat Rev Cancer 8(3):205–211
Bruun JM, Verdich C, Toubro S, Astrup A, Richelsen B (2003) Association between measures of insulin sensitivity and circulating levels of interleukin-8, interleukin-6 and tumor necrosis factor-alpha. Effect of weight loss in obese men. Eur J Endocrinol 148(5):535–542
Straczkowski M, Dzienis-Straczkowska S, Stepien A, Kowalska I, Szelachowska M, Kinalska I (2002) Plasma interleukin-8 concentrations are increased in obese subjects and related to fat mass and tumor necrosis factor-alpha system. J Clin Endocrinol Metab 87(10):4602–4606
Fiuza-Luces C, Garatachea N, Berger NA, Lucia A (2013) Exercise is the real polypill. Physiology (Bethesda) 28(5):330–358
Mann S, Beedie C, Jiminez A (2014) Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Medicine 44(2):211–221
Hawley JA (2004) Exercise as a therapeutic intervention for the prevention and treatment of insulin resistance. Diabetes Metab Res Rev 20(5):383–393
Sharman JE, Stowasser M (2009) Australian association for exercise and sports science position statement on exercise and hypertension. J Sci Med Sport. 12(2):252–257
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA (2011) The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 11(9):607–615
Ismail I, Keating SE, Baker MK, Johnson NA (2012) A systematic review and meta-analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Obes Rev 13(1):68–91
Keating SE, Hackett DA, George J, Johnson NA (2012) Exercise and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol 57(1):157–166
Shin HY, Linton JA, Shim JY, Kang HT (2015) Cancer survivors aged 40 years or elder are associated with high risk of chronic kidney disease: the 2010–2012 Korean National Health and Nutrition Examination Survey. Asian Pac J Cancer Prev 16(4):1355–1360
Fairley TL, Hawk H, Pierre S (2010) Health behaviors and quality of life of cancer survivors in Massachusetts, 2006: data use for comprehensive cancer control. Prev Chronic Dis 7(1):A09
Weaver KE, Foraker RE, Alfano CM et al (2013) Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal, and gynecologic cancers: a gap in survivorship care? J Cancer Surviv 7(2):253–261
Mishra SI, Scherer RW, Snyder C, Geigle P, Gotay C (2014) Are exercise programs effective for improving health-related quality of life among cancer survivors? A systematic review and meta-analysis. Oncol Nurs Forum 41(6):E326–E342
Meneses-Echavez JF, Gonzalez-Jimenez E, Correa-Bautista JE, Valle JS, Ramirez-Velez R (2015) Effectiveness of physical exercise on fatigue in cancer patients during active treatment: a systematic review and meta-analysis. Cad Saude Publica 31(4):667–681
Cheema BS, Kilbreath SL, Fahey PP, Delaney GP, Atlantis E (2014) Safety and efficacy of progressive resistance training in breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 148(2):249–268
Strasser B, Steindorf K, Wiskemann J, Ulrich CM (2013) Impact of resistance training in cancer survivors: a meta-analysis. Med Sci Sports Exerc 45(11):2080–2090
Kruijsen-Jaarsma M, Revesz D, Bierings MB, Buffart LM, Takken T (2013) Effects of exercise on immune function in patients with cancer: a systematic review. Exerc Immunol Rev 19:120–143
Schmitz KH, Holtzman J, Courneya KS, Masse LC, Duval S, Kane R (2005) Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 14(7):1588–1595
Haseen F, Murray LJ, Cardwell CR, O’Sullivan JM, Cantwell MM (2010) The effect of androgen deprivation therapy on body composition in men with prostate cancer: systematic review and meta-analysis. J Cancer Surviv 4(2):128–139
Gonzalez MC, Pastore CA, Orlandi SP, Heymsfield SB (2014) Obesity paradox in cancer: new insights provided by body composition. Am J Clin Nutr 99(5):999–1005
Fujiwara N, Nakagawa H, Kudo Y et al (2015) Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J Hepatol 63(1):131–140
Pines A (2012) Weight loss, weight regain and bone health. Climacteric 15(4):317–319
Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK (2009) American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41(2):459–471
Sturgeon KM, Ky B, Libonati JR, Schmitz KH (2014) The effects of exercise on cardiovascular outcomes before, during, and after treatment for breast cancer. Breast Cancer Res Treat 143(2):219–226
Ascensao A, Lumini-Oliveira J, Machado NG et al (2011) Acute exercise protects against calcium-induced cardiac mitochondrial permeability transition pore opening in doxorubicin-treated rats. Clin Sci (Lond) 120(1):37–49
Kavazis AN, Smuder AJ, Min K, Tumer N, Powers SK (2010) Short-term exercise training protects against doxorubicin-induced cardiac mitochondrial damage independent of HSP72. Am J Physiol Heart Circ Physiol 299(5):H1515–H1524
Chicco AJ, Schneider CM, Hayward R (2005) Voluntary exercise protects against acute doxorubicin cardiotoxicity in the isolated perfused rat heart. Am J Physiol Regul Integr Comp Physiol 289(2):R424–R431
Giovannucci E, Harlan DM, Archer MC et al (2010) Diabetes and cancer: a consensus report. CA Cancer J Clin 60(4):207–221
Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R (2009) Diabetes and cancer. Endocr Relat Cancer 16(4):1103–1123
Sandhu MS, Dunger DB, Giovannucci EL (2002) Insulin, insulin-like growth factor-I (IGF-I), IGF binding proteins, their biologic interactions, and colorectal cancer. J Natl Cancer Inst 94(13):972–980
Ahmed RL, Thomas W, Schmitz KH (2007) Interactions between insulin, body fat, and insulin-like growth factor axis proteins. Cancer Epidemiol Biomarkers Prev 16(3):593–597
Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C (2004) Physical activity/exercise and type 2 diabetes. Diabetes Care 27(10):2518–2539
Hordern MD, Dunstan DW, Prins JB, Baker MK, Singh MA, Coombes JS (2012) Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. J Sci Med Sport 15(1):25–31
Rector RS, Uptergrove GM, Morris EM et al (2011) Daily exercise vs. caloric restriction for prevention of nonalcoholic fatty liver disease in the OLETF rat model. Am J Physiol Gastrointest Liver Physiol 300(5):G874–G883
Berzigotti A, Saran U, Dufour JF (2015) Physical activity and liver diseases. Hepatology
Stengel B (2010) Chronic kidney disease and cancer: a troubling connection. J Nephrol 23(3):253–262
White SL, Dunstan DW, Polkinghorne KR, Atkins RC, Cass A, Chadban SJ (2011) Physical inactivity and chronic kidney disease in Australian adults: the AusDiab study. Nutr Metab Cardiovasc Dis 21(2):104–112
Heiwe S, Jacobson SH (2011) Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev 10:Cd003236
Israeli RS, Ryan CW, Jung LL (2008) Managing bone loss in men with locally advanced prostate cancer receiving androgen deprivation therapy. J Urol 179(2):414–423
Greenspan SL, Coates P, Sereika SM, Nelson JB, Trump DL, Resnick NM (2005) Bone loss after initiation of androgen deprivation therapy in patients with prostate cancer. J Clin Endocrinol Metab 90(12):6410–6417
Lattouf JB, Saad F (2010) Bone complications of androgen deprivation therapy: screening, prevention, and treatment. Curr Opin Urol 20(3):247–252
Clarke BL, Khosla S (2009) Androgens and Bone. Steroids 74(3):296–305 (10/17)
Hamilton EJ, Ghasem-Zadeh A, Gianatti E et al (2010) Structural decay of bone microarchitecture in men with prostate cancer treated with androgen deprivation therapy. J Clin Endocrinol Metab 95(12):E456–E463
Guadalupe-Grau A, Fuentes T, Guerra B, Calbet JA (2009) Exercise and bone mass in adults. Sports Med 39(6):439–468
Winters-Stone KM, Schwartz A, Nail LM (2010) A review of exercise interventions to improve bone health in adult cancer survivors. J Cancer Surviv 4(3):187–201
Schilder CM, Eggens PC, Seynaeve C et al (2009) Neuropsychological functioning in postmenopausal breast cancer patients treated with tamoxifen or exemestane after AC-chemotherapy: cross-sectional findings from the neuropsychological TEAM-side study. Acta Oncol 48(1):76–85
Jenkins V, Shilling V, Fallowfield L, Howell A, Hutton S (2004) Does hormone therapy for the treatment of breast cancer have a detrimental effect on memory and cognition? A pilot study. Psychooncology 13(1):61–66
Collins B, Mackenzie J, Stewart A, Bielajew C, Verma S (2009) Cognitive effects of hormonal therapy in early stage breast cancer patients: a prospective study. Psychooncology 18(8):811–821
Gomez-Pinilla F, Hillman C (2013) The influence of exercise on cognitive abilities. Compr Physiol 3(1):403–428
Li C, Zhou C, Li R (2015) Can exercise ameliorate aromatase inhibitor-induced cognitive decline in breast cancer patients? Mol Neurobiol
World Health Organisation (WHO) (2009) Mortality and burden of disease attributable to selected major risks. Global health risks. WHO, Geneva
Lee IM, Skerrett PJ (2001) Physical activity and all-cause mortality: what is the dose-response relation? Med Sci Sports Exerc 33(6 Suppl):S459–S471 (discussion S493–454)
Haapanen-Niemi N, Miilunpalo S, Pasanen M, Vuori I, Oja P, Malmberg J (2000) Body mass index, physical inactivity and low level of physical fitness as determinants of all-cause and cardiovascular disease mortality–16 y follow-up of middle-aged and elderly men and women. Int J Obes Relat Metab Disord 24(11):1465–1474
LaMonte MJ, Barlow CE, Jurca R, Kampert JB, Church TS, Blair SN (2005) Cardiorespiratory fitness is inversely associated with the incidence of metabolic syndrome: a prospective study of men and women. Circulation 112(4):505–512
Kodama S, Saito K, Tanaka S et al (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301(19):2024–2035
Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN (2014) Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis 56(4):382–390 (1)
Rock CL, Doyle C, Demark-Wahnefried W et al (2012) Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin 62(4):242–274
Schmitz KH, Courneya KS, Matthews C et al (2010) American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc 42(7):1409–1426
Ross R, Hudson R, Stotz PJ, Lam M (2015) Effects of exercise amount and intensity on abdominal obesity and glucose tolerance in obese adults: a randomized trial. Ann Intern Med 162(5):325–334
Galvao DA, Newton RU, Gardiner RA et al (2015) Compliance to exercise-oncology guidelines in prostate cancer survivors and associations with psychological distress, unmet supportive care needs, and quality of life. Psychooncology
Artinian NT, Fletcher GF, Mozaffarian D et al (2010) Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation 122(4):406–441
Centers for Disease Control and Prevention (2011) The CDC Guide to Strategies to Increase Physical Activity in the Community. In: Services DoHaH (ed) Atlanta, US
Kiefte-de Jong JC, Mathers JC, Franco OH (2014) Nutrition and healthy ageing: the key ingredients. Proc Nutr Soc 73(2):249–259
Duthie SJ (2011) Folate and cancer: how DNA damage, repair and methylation impact on colon carcinogenesis. J Inherit Metab Dis 34(1):101–109
McKay JA, Mathers JC (2016) Maternal folate deficiency and metabolic dysfunction in offspring. Proc Nutr Soc 75(1):90–95
Fenech MF (2010) Dietary reference values of individual micronutrients and nutriomes for genome damage prevention: current status and a road map to the future. Am J Clin Nutr 91(5):1438s–1454s
Xu C, Wu Y, Liu G, Liu X, Wang F, Yu J (2014) Relationship between homocysteine level and diabetic retinopathy: a systematic review and meta-analysis. Diagnostic Pathology. 9:167 (09/26 06/26/received 08/16/accepted 2014)
Douaud G, Refsum H, de Jager CA et al (2013) Preventing Alzheimer’s disease-related gray matter atrophy by B-vitamin treatment. Proceedings of the National Academy of Sciences. 110(23):9523–9528
Oulhaj A, Refsum H, Beaumont H et al (2010) Homocysteine as a predictor of cognitive decline in Alzheimer’s disease. Int J Geriatr Psychiatry 25(1):82–90
Nguyen JCD, Killcross AS, Jenkins TA (2015) Obesity and cognitive decline: role of inflammation and vascular changes. Frontiers in Neuroscience 8:375 (11/1910/06/received 10/31/accepted 2014)
Dufouil C, Seshadri S, Chene G (2014) Cardiovascular risk profile in women and dementia. J Alzheimers Dis 42(Suppl 4):S353–S363
Anderson AS, Key TJ, Norat T et al (2015) European Code against Cancer 4th Edition: Obesity, body fatness and cancer. Cancer Epidemiol 39(Suppl 1):S34–S45
Matyszewski A, Czarnecka AM, Solarek W et al (2015) Molecular basis of carcinogenesis in diabetic patients (review). Int J Oncol 46(4):1435–1443
Cerda C, Sanchez C, Climent B et al (2014) Oxidative stress and DNA damage in obesity-related tumorigenesis. Adv Exp Med Biol 824:5–17
Armani C, Botto N, Andreassi MG, Centaro E (2013) Molecular markers of cardiovascular damage in hypertension. Curr Pharm Des 19(13):2341–2350
Benayoun BA, Pollina EA, Brunet A (2015) Epigenetic regulation of ageing: linking environmental inputs to genomic stability. Nat Rev Mol Cell Biol 16(10):593–610
Macheret M, Halazonetis TD (2015) DNA replication stress as a hallmark of cancer. Annu Rev Pathol 10:425–448
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G (2013) The Hallmarks of Aging. Cell.153(6):1194–1217
Hanahan D, Weinberg Robert A (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Maslov AY, Vijg J (2009) Genome instability, cancer and aging. Biochim Biophys Acta 1790(10):963–969
Fenech M (2002) Chromosomal biomarkers of genomic instability relevant to cancer. Drug Discov Today 7(22):1128–1137
World Cancer Research Fund/American Institute for Cancer Research (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, Washington DC
Amitay EL, Keinan-Boker L (2015) Breastfeeding and childhood leukemia incidence: A meta-analysis and systematic review. JAMA Pediatrics 169(6):e151025
Sofi F, Cesari F, Abbate R, Gensini GF, Casini A (2008) Adherence to Mediterranean diet and health status: meta-analysis. BMJ 337 (2008-09-11 23:05:19 2008)
Fenech MF (2014) Nutriomes and personalised nutrition for DNA damage prevention, telomere integrity maintenance and cancer growth control. Cancer Treat Res 159:427–441
World Health Organisation/International Agency for Research on Cancer (2015) Continuous Update. http://www.iarc.fr/en/media-centre/iarcnews/pdf/Monographs-Q&A_Vol114.pdf. Accessed 18 Feb 2016
Brooks PJ, Zakhari S (2014) Acetaldehyde and the genome: beyond nuclear DNA adducts and carcinogenesis. Environ Mol Mutagen 55(2):77–91
Brooks PJ, Theruvathu JA (2005) DNA adducts from acetaldehyde: implications for alcohol-related carcinogenesis. Alcohol 35(3):187–193
International Agency for Research on Cancer (IARC) (2010) Alcohol consumption and ethyl carbamate. IARC, Lyon
International Agency for Research on Cancer (IARC) (2012) IARC Monographs on the Evaluation of Carcinogenic Risk to Humans. IARC, Lyon
Yu HS, Oyama T, Isse T et al (2010) Formation of acetaldehyde-derived DNA adducts due to alcohol exposure. Chem Biol Interact 188(3):367–375
Iarmarcovai G, Bonassi S, Botta A, Baan RA, Orsiere T (2008) Genetic polymorphisms and micronucleus formation: a review of the literature. Mutat Res 658(3):215–233
Teo T, Fenech M (2008) The interactive effect of alcohol and folic acid on genome stability in human WIL2-NS cells measured using the cytokinesis-block micronucleus cytome assay. Mutat Res 657(1):32–38
Fontana L, Partridge L (2015) Promoting health and longevity through diet: from model organisms to humans. Cell 161(1):106–118
Rizza W, Veronese N, Fontana L (2014) What are the roles of calorie restriction and diet quality in promoting healthy longevity? Ageing Res Rev 13:38–45
Tchernof A, Despres JP (2013) Pathophysiology of human visceral obesity: an update. Physiol Rev 93(1):359–404
Snel M, Jonker JT, Schoones J et al (2012) Ectopic Fat and Insulin Resistance: Pathophysiology and Effect of Diet and Lifestyle Interventions. Int J Endocrinol 2012:18
Hocking S, Samocha-Bonet D, Milner KL, Greenfield JR, Chisholm DJ (2013) Adiposity and insulin resistance in humans: the role of the different tissue and cellular lipid depots. Endocr Rev 34(4):463–500
Mancini JG, Filion KB, Atallah R, Eisenberg MU (2015) Systematic review of the Mediterranean diet for long-term weight loss. Am J Med S0002-9343(15):3027–3029
Hill AM, Harris Jackson KA, Roussell MA, West SG, Kris-Etherton PM (2015) Type and amount of dietary protein in the treatment of metabolic syndrome: a randomized controlled trial. Am J Clin Nutr 102(4):757–770
Razavi ZM, Telkabadi MH, Bahmani F, Salehi B, Farshbaf S, Asemi Z (2015) The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: a randomized clinical trial. Liver Int. doi:10.1111/liv.12990 [Epub ahead of print]
Ello-Martin JA, Ledikwe JH, Rolls BJ (2005) The influence of food portion size and energy density on energy intake: implications for weight management. Am J Clin Nutr 82(Suppl. 1):S236–S241
Rolls BJ (2014) What is the role of portion control in weight management? Int J Obes 38(Suppl. 1):S1–S8
Barnard ND, Levin SM, Yokoyama Y (2015) A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J Acad Nutr Diet 115(6):954–969
Sabate J, Wien M (2010) Vegetarian diets and childhood obesity prevention. Am J Clin Nutr 91(5):S1525–S1529
Tay J, Luscombe-Marsh ND, Thompson CH et al (2015) Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial. Am J Clin Nutr 102(4):780–790
Neacsu M, Fyfe C, Horgan G, Johnstone AM (2014) Appetite control and biomarkers of satiety with vegetarian (soy) and meat-based high-protein diets for weight loss in obese men: a randomized crossover trial. Am J Clin Nutr 100(2):548–558
Fogelholm M, Anderssen S, Gunnarsdottir I, Lahti-Koski M (2012) Dietary macronutrients and food consumption as determinants of long-term weight change in adult populations: a systematic literature review. Food Nutr Res 56. doi:10.3402/fnr.v56i0.19103 (Epub 2012 Aug 13)
Keogh JB, Clifton PM (2012) Meal replacements for weight loss in type 2 diabetes in a community setting. J Nutr Metab. doi:10.1155/2012/918571
Carney D, Schultz S, Lim J, Walters W (2015) Successful medical weight loss in a community setting. J Obes Weightloss Ther 5(1):pii:248
Mehta T, Smith DL, Muhammad J, Casazza K (2014) Impact of weight cycling on risk of morbidity and mortality. Obes Rev 15(11):870–881
Stevens VL, Jacobs EJ, Patel AV et al (2015) Weight cycling and cancer incidence in a large prospective US cohort. Am J Epidemiol 182(5):394–404
World Health Organisation (WHO) (2003) Population nutrient intake goals for preventing diet-related chronic diseases. Accessed 29 Feb 2016
Despres JP (1993) Abdominal obesity as important component of insulin-resistance syndrome. Nutrition 9(5):452–459
Goodpaster BH, Krishnaswami S, Resnick H et al (2003) Association between regional adipose tissue distribution and both type 2 diabetes and impaired glucose tolerance in elderly men and women. Diabetes Care 26(2):372–379
Park BJ, Kim YJ, Kim DH et al (2008) Visceral adipose tissue area is an independent risk factor for hepatic steatosis. J Gastroenterol Hepatol 23(6):900–907
Yusuf S, Hawken S, Ounpuu S et al (2005) Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet 366(9497):1640–1649
Ekelund U, Besson H, Luan J et al (2011) Physical activity and gain in abdominal adiposity and body weight: prospective cohort study in 288,498 men and women. Am J Clin Nutr 93(4):826–835
Janssen I, Katzmarzyk PT, Ross R et al (2004) Fitness alters the associations of BMI and waist circumference with total and abdominal fat. Obes Res 12(3):525–537
Shaw K, Gennat H, O’Rourke P, Del Mar C (2006) Exercise for overweight or obesity. Cochrane Database Syst Rev 4:Cd003817
Franz MJ, VanWormer JJ, Crain AL et al (2007) Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 107(10):1755–1767
Brown Medical School/The Miriam Hospital Weight Control, Diabetes Research Center (2016) The National Weight Control Registry. http://www.nwcr.ws/Research/default.htm. Accessed 22 Feb 2016
Vissers D, Hens W, Taeymans J, Baeyens J-P, Poortmans J, Van Gaal L (2013) The effect of exercise on visceral adipose tissue in overweight adults: a systematic review and meta-analysis. PLoS ONE 8(2):e56415
Bryner RW, Ullrich IH, Sauers J et al (1999) Effects of resistance vs. aerobic training combined with an 800 calorie liquid diet on lean body mass and resting metabolic rate. J Am Coll Nutr 18(2):115–121
Cancer Australia (2011) Risk-reducing Medication for Women at Increased Risk of Breast Cancer Due to Family History. In: Australia C (ed) Australian Government
National Cancer Institute (2015) Breast cancer prevention for health professionals. http://www.cancer.gov/types/breast/hp/breast-prevention-pdq#section/_1. Accessed 19 Oct 2015
Australia Cancer (2011) Recommendations for aromatase inhibitors as adjuvant endocrine therapy for post-menopausal women with hormone receptor-positive early breast cancer. National Breast Cancer Centre, Camperdown
Morales D, Morris AD (2015) Metformin in cancer treatment and prevention. Annu Rev Med 66(1):17–29
Vestergaard P, Starup-Linde J (2013) Diabetes, cancer and treatment—A mini-review. Curr Drug Saf 8(5):292–295
Pollak MN (2012) Investigating metformin for cancer prevention and treatment: the end of the beginning. Cancer Discov 2(9):778–790
McCarthy AL, Tramm R, Shaban RZ, Yates P (2013) Factors influencing health behaviors of younger women after menopause-inducing cancer treatment. Public Health Nurs 30(2):106–116
Vejpongsa P, Yeh ETH (2014) Prevention of Anthracycline-Induced Cardiotoxicity: Challenges and Opportunities. J Am Coll Cardiol 64(9):938–945
Todaro MC, Oreto L, Qamar R, Paterick TE, Carerj S, Khandheria BK (2013) Cardioncology: state of the heart. Int J Cardiol 168(2):680–687
Curigliano G, Cardinale D, Suter T et al (2012) Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO Clinical Practice Guidelines. Ann Oncol 23(Suppl 7):vii155–vii166
van Dalen EC, Caron HN, Dickinson HO, Kremer LC (2008) Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev 2:Cd003917
Kalam K, Marwick T (2013) Role of cardioprotective therapy for prevention of cardiotoxicity with chemotherapy: a systematic review and meta-analysis. Eur J Cancer 49:2900–2909
Colagiuri B, Roscoe JA, Morrow GR, Atkins JN, Giguere JK, Colman LK (2008) How do patient expectancies, quality of life, and postchemotherapy nausea interrelate? Cancer 113(3):654–661
National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand (2012) An expert guide to clinical practice for secondary prevention of coronary heart disease. Reducing risk in heart disease. National Heart Foundation of Australia, Melbourne
National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand (Chronic Heart Failure Guidelines Expert Writing Panel) (2011) Guidelines for the prevention, detection and management of chronic heart failure in Australia. National Heart Foundation of Australia
Kidney Health Australia (2015) Prevention. http://www.kidney.org.au/KidneyDisease/Prevention/tabid/820/Default.aspx. Accessed 21 Oct 2015
Demierre MF, Higgins PD, Gruber SB, Hawk E, Lippman SM (2005) Statins and cancer prevention. Nat Rev Cancer 5(12):930–942
Lustman A, Nakar S, Cohen AD, Vinker S (2014) Statin use and incident prostate cancer risk: does the statin brand matter? A population-based cohort study. Prostate Cancer Prostatic Dis 17(1):6–9
Ravnskov U, Rosch PJ, McCully KS (2015) Statins do not protect against cancer: quite the opposite. J Clin Oncol
Goldstein MR, Mascitelli L, Pezzetta F (2008) Do statins prevent or promote cancer? Curr Oncol 15(2):76–77
Heart Foundation (2009) Aspirin. http://www.heartfoundation.org.au/SiteCollectionDocuments/Aspirin.pdf. Accessed 20 Oct 2015
American Heart Foundation (2015) Aspirin and heart disease. American Heart Foundation, Dallas
Hung J (2003) Aspirin for cardiovascular disease prevention. Med J Aust 179(3):147–152
International Agency for Research on Cancer (1992) (IARC). IARC monographs on the evaluation of carcinogenic risks to humans. Solar and ultraviolet radiation. IARC Monogr Eval Carcinog Risks Hum 55:1–316
CancerAustralia (2015) UV radiation. Cancer Australia, Sydney
Morton LM, Onel K, Curtis RE, Hungate EA, Armstrong GT (2014) The rising incidence of second cancers: patterns of occurrence and identification of risk factors for children and adults. Am Soc Clin Oncol Educ Book e57–e67
Berrington DGA, Curtis RE, Kry SF et al (2011) Proportion of second cancers attributable to radiotherapy in adults: a cohort study in the US SEER cancer registries. Lancet Oncol 12(4):353–360
Cancer Australia (2015) Infections. Cancer Australia, Sydney
O’Connor SM, Taylor CE, Hughes JM (2006) Emerging infectious determinants of chronic diseases. Emerg Infect Dis 12(7):1051–1057
Hepatitis B Foundation (2014) Hepatitis B and Primary Liver Cancer. http://www.hepb.org/professionals/hepb_and_liver_cancer.htm. Accessed 20 Oct 2015
Wroblewski LE, Peek RM Jr, Wilson KT (2010) Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbiol Rev 23(4):713–739
Australian Commission on Saftey and Quality in Health Care (ACSQHC) (2015) Health literacy: a summary for clinicians. ACSQHC, Sydney
Australian Bureau of Statistics (2010) Health and socioeconomic disadvantage. Australian Social Trends, cat. no. 4102.0. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4102.0Main+Features30Mar+2010. Accessed 21 Oct 2015
Australian Bureau of Statistics (ABS) (2015) Health risk factors. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.001Chapter4002011-12. Accessed 18 Feb 2016
American College of Preventative Medicine (2011) Medication adherence time tool: medication adhereance—Improving health outcomes. http://www.acpm.org/?MedAdhereTTProviders. Accessed 8 Feb 2016
Colagiuri R, Girgis S, Gomez M, Walker K, Colagiuri S, O’Dea K (2009) National evidence based guideline for the primary prevention of type 2 diabetes. Diabetes Australia and the NHMRC, Canberra
Kohl HW, 3rd (2001) Physical activity and cardiovascular disease: evidence for a dose response. Med Sci Sports Exerc 33(6 Suppl):S472–S483 (discussion S493–474)
Whelton SP, Chin A, Xin X, He J (2002) Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 136(7):493–503
Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R et al (2008) Role of leisure-time physical activity in nonalcoholic fatty liver disease: a population-based study. Hepatology 48(6):1791–1798
Marques EA, Mota J, Carvalho J (2012) Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Age (Dordr) 34(6):1493–1515
Barcellos FC, Santos IS, Umpierre D, Bohlke M, Hallal PC (2015) Effects of exercise in the whole spectrum of chronic kidney disease: a systematic review. Clin Kidney J 8(6):753–765
World Cancer Research Fund International (2015) Kidney cancer 2015 report. http://www.wcrf.org/int/researche-we-find/continuous-update-project-findings-reports/kidney-cancer. Accessed 21 Sep 2015
World Cancer Research Fund International (2015) Prostate cancer report 2014 report. http://www.wcrf.org/int/researche-we-find/continuous-update-project-findings-reports/prostate-cancer. Accessed 29 Sep 2015
Goss PE, Ingle JN, Alés-Martínez JE et al (2011) Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med 364(25):2381–2391
Chadban S, Howell M, Twigg S et al (2010) The CARI guidelines. Prevention and management of chronic kidney disease in type 2 diabetes. Nephrology (Carlton) 15(Suppl 1):S162–S194
World Cancer Research Fund International (2015) Liver cancer 2015 report. http://www.wcrf.org/int/researche-we-find/continuous-update-project-findings-reports/liver-cancer. Accessed 29 Sep 2015
Australia Cancer (2015) Tobacco. Cancer Australia, Sydney
Campbell PT, Patel AV, Newton CC, Jacobs EJ, Gapstur SM (2013) Associations of recreational physical activity and leisure time spent sitting with colorectal cancer survival. J Clin Oncol 31(7):876–885
Biswas A, Oh PI, Faulkner GE et al (2015) Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 162(2):123–132
Bauman AE, Chau JY, Ding D, Bennie J (2013) Too much sitting and cardio-metabolic risk: an update of epidemiological evidence. Curr Cardiovasc Risk Rep 7(4):293–298
Further Reading
American college of sports medicine. http://www.acsm.org/public-information/position-stands
Exercise and sports science Australia. https://www.essa.org.au/for-media/position-statements/
World cancer research fund international. http://www.wcrf.org/int/research-we-fund/our-cancer-prevention-recommendations
World cancer research fund international. http://www.wcrf.org/int/research-we-fund/continuous-update-project-cup
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
McCarthy, A., Skinner, T., Fenech, M., Keating, S. (2016). Prevention of Chronic Conditions and Cancer. In: Koczwara, B. (eds) Cancer and Chronic Conditions. Springer, Singapore. https://doi.org/10.1007/978-981-10-1844-2_7
Download citation
DOI: https://doi.org/10.1007/978-981-10-1844-2_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-1843-5
Online ISBN: 978-981-10-1844-2
eBook Packages: MedicineMedicine (R0)