Abstract
Sedentary behavior, as distinct from a lack of moderate-to-vigorous physical activity, is an emerging health risk behavior for the development of chronic diseases. Examples of sedentary behavior include sitting, watching television, using a computer, and driving a car. In this article, we define sedentary behavior; outline key concepts related to the physiology of sedentary behavior, review the recent evidence on the effects of prolonged sedentary behavior (or sitting) on the risk of cardio-metabolic disease and all cause mortality, and discuss the implications for current clinical practice. We found that most large scale studies on sedentary behavior were published in the last 5 years. There is moderately consistent evidence for an association between total sitting time and all-cause mortality, even when adjusted for or stratified by leisure time physical activity. Overall, we identified a compelling case for sitting reduction to be included in clinical preventive advice as a key component of ‘active living,’ where adults and children are encouraged to ‘move more and sit less’ across different settings and locations throughout the day.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction: Definition and Prevalence of Sedentary Behavior
The benefits of physical activity for chronic disease prevention are well established with the latest estimates that physical inactivity accounts for 9 % of premature mortality worldwide [1•]. Current public health guidelines recommend that adults engage in at least 150 min/wk of moderate-to-vigorous physical activity for good health [2]. Recently, increasing attention has been given to sedentary behavior, which appears to be associated with adverse health outcomes independent of moderate-to-vigorous physical activity [3•, 4, 5, 6•].
Sedentary behaviors are defined as any waking behavior characterized by an energy expenditure ≤1.5 METs while in a sitting or reclining posture [7, 8•]. Common examples of sedentary behaviors include:, sitting at work, driving a car, and watching television, and as such are a ubiquitous part of modern day living.
Studies that have objectively assessed population movement patterns (via accelerometry) have shown that adults in developed countries spend typically 55 % to 70 % of their waking time in sedentary behaviors (about 8.8–11.2 h/d assuming 8 h/d of sleep) [9–12]. In a multinational study, over 20 % of respondents from half of the 20 participating countries self-reported overall sitting time of 9 or more hours per day [13]. Population time use surveys have found that adults are sedentary for 7.6 h/d in their nonworking time, and that the majority of leisure time is sedentary, mostly spent in screen time (watching TV and using computers) [14, 15]. The prevalence of people with sedentary occupations has also increased steadily over the last 50 years [16].
The aims of this paper are first, to present the key concepts related to the physiology of prolonged sitting; second, to review the recent evidence on the effects of prolonged sedentary behavior (or sitting) on the risk of cardio-metabolic disease; and third, to discuss the implications for current clinical practice.
Physiology of Sedentary Behavior : Key Concepts
Central to the current thinking on sedentary behavior physiology is that chronic engagement in this behavior results in low muscle energy turn over [17], or muscular unloading [18], within the large skeletal muscles groups of the legs, back and trunk regions. The ‘switching off’ of these skeletal muscles is thought to initiate a cascade of cellular events culminating in metabolic deregulation, hyperglycaemia, and hyperlipidemia [18].
Recent evidence supporting the biological plausibility for sitting and health has been generated from 2 experimental conditions: (1) bed-rest in healthy human subjects; and (2) hind limb suspension in rodents [17, 19]. In brief, experiments have consistently shown that prolonged muscle inactivity (eg, typically 1–3 weeks in bed-rest studies) initiates a series of pathophysiological responses, including; glucose intolerance, hyper-insulinemia, and impaired lipid metabolism [17]. While the underlying physiological mechanisms remain unclear, evidence from biochemical analysis of skeletal muscle samples biopsied pre- and post-exposure to prolonged sedentary behavior suggest a downregulation of key enzymes involved in glucose and lipid metabolism. In particular, a reduced activity and content of the glucose transporter 4 protein (GLUT4) [20, 21], and the lipoprotein lipase enzyme (LPL) [22, 23] may be contributory factors. While these experiments provide important insights into the health consequences of muscular inactivity, there are limitations for the generalizability to human physiology and health. It is likely that the quantity of sedentary time encountered during bed-rest trials and animal hind limb suspension experiments far exceed that of healthy free-living ambulatory adults [17].
Recent experimental studies investigated the health consequences of sitting behaviors in settings more accurately replicate free-living ambulatory adults [24]. Stephens and colleagues investigated the effects of about of 1-day sitting (~17 h/d objectively assessed) on whole-body insulin sensitivity in a controlled setting, with strict dietary control [24]. Among healthy, young participants, an acute bout of prolonged sitting resulted in a 31 % reduced insulin sensitivity. This impaired insulin sensitivity was attenuated when participants undertook a subsequent experimental condition, in which sitting time was purposefully reduced (6 h/d vs 17 h/d), and displaced with light-intensity walking (2.2 h/d vs 0.1 h/d) and standing (9.8 h/d vs 0.1 h/d). Despite the small sample size and short duration, these results suggest that displacing prolonged sitting with light-intensity walking and standing may attenuate the relationship between sedentary behavior and cardio-metabolic risk [24].
Dunstan and colleagues [25•] further examined the acute cardio-metabolic effects of breaking up prolonged sitting. In a cross-over design, 19 middle-aged healthy, but overweight/obese adults undertook 3 experimental conditions; (1) uninterrupted sitting (~7 hours), (2) sitting interrupted with light-intensity walking (3.2 km/h) every 20 mins, and (3) sitting interrupted with moderate-intensity walking (5.8–6.4 km/h) every 20 minutes. For all 3 conditions, plasma glucose and serum insulin were monitored after participants consumed a standardized test meal (200 mL, 75 g carbohydrate, 50 g fat). Compared with uninterrupted sitting, plasma glucose was reduced by ~23 % in activity-break conditions. Notably, there were no differences in plasma glucose concentrations between the moderate-intensity and light-intensity walking groups. Although this study was limited by a small sample and short duration, these findings suggest that independent of activity intensity, breaking up prolonged sitting blunts postprandial plasma glucose responses. Therefore, frequent breaks may reduce the detrimental cardio-metabolic outcomes associated with this prolonged sitting.
Overall, the available physiological and experimental evidence suggests that the relationship between prolonged sedentary behavior and cardio-metabolic risk is biologically plausible.
Epidemiology of Sedentary Behavior: an Update of Recent Evidence
In the past year, there have been a large number of published studies expanding the evidence base on sitting and cardio-metabolic health. We used the recent systematic review and meta-analysis by Wilmot et al. [26] (which includes studies published between 1980 and January 2012) as the baseline for literature search, and additionally searched for publications up to January 2013.
Diabetes
Wilmot and colleagues reviewed 10 studies that examined the association between sitting and diabetes, of which 5 were cross-sectional and 5 were prospective. Evidence from these studies showed a consistent positive association between prolonged sitting and diabetes. One recent study examined self-reported sitting and diabetes and found that more sitting time was significantly associated with diabetes independent of physical activity in a large population-representative sample in Australia [27]. Using biomarkers for insulin resistance, Yates et al. [28] found that reported sitting time was positively associated with fasting insulin among women but not men after adjustment for physical activity. Among adults newly diagnosed with type 2 diabetes, Cooper and colleagues [29] found that objectively measured sitting time at baseline was associated with higher insulin at both baseline and 6 months follow-up. However, in this study, there was no association between objectively measured breaks in sitting time and insulin at baseline or follow-up.
Cardiovascular Diseases (CVD)
Wilmot et al’s systematic review and meta-analysis [26] included 3 studies on CVD and 8 studies on cardiovascular mortality. All 3 studies found positive and significant associations between sedentary behavior and CVD. Seven of the 8 studies found significant associations between sedentary behavior and cardiovascular mortality. In addition, Ford and Caspersen [30] published a review of sedentary behavior and CVD. In this review, the authors examined 4 population-based cohort studies on sitting time and CVD events and death; each study found an increased risk for incident or fatal CVD among those who spent more time sitting. Ford and Caspersen also reviewed 6 prospective studies on television viewing time and CVD events and cardiovascular mortality, of which only 3 studies noted significant positive associations.
In addition to the 2 reviews, we identified several studies on sedentary behavior and cardiovascular biomarkers from 2012. For example, in a British cross-sectional study, Pinto and colleagues [31] identified significant cross-sectional associations between specific sitting behavior and CVD biomarkers (HDL, LDL, triglycerides, and blood pressure). The relationships were stronger for television viewing, but weaker associations were observed for occupational sitting and CVD biomarkers. Based on a Danish sample, Frydenlund and colleagues [32] found significant and positive cross-sectional associations between leisure-time sitting and CVD biomarkers, including non-HDL cholesterol, triglycerides waist circumference, and waist-hip ratio.
Obesity and Weight Gain
Conceptually, prolonged sedentary time should be related to reduced total energy expenditure, and hence might contribute to obesity. Two large cohort studies have shown significant increases in weight among those at the highest levels of sitting, independent of leisure time physical activity participation [33, 34]. More recent longitudinal studies have shown a mixed pattern, with a recent British paper suggesting that obesity was associated with subsequent sedentary behavior (TV watching), but that sitting did not show a prospective association with weight gain [35]. Nonetheless, many cross-sectional studies still show associations between sedentary behaviors and obesity in low income US adults [36] and in a sample of older Spanish adults [37]. A Mexican study [38] showed that sitting was associated with obesity, which in turn was associated with diabetes and hypertension; this study considered obesity as a mediator of the relationship between sitting and cardio-metabolic health, but was limited by the cross-sectional design. Sitting at work was associated with obesity among Australian adults [39]. In a large sample of 70,000 Thai adults, sedentary behaviors, especially screen time, was associated with obesity, more strongly among males [40].
All-Cause Mortality
Wilmot’s review and meta-analyses included 8 studies on all-cause mortality, all of which were prospective studies. All these studies reported positive associations between sitting time and all-cause mortality. We have identified a few more recent studies that examined sedentary behavior and all-cause mortality.
Evidence from recent prospective cohort studies suggest that higher amounts of sitting are associated with greater risk of all-cause mortality after adjusting for physical activity. In an American cohort of adults aged 50–71 years followed for 8.5 years, those who reported daily sitting time of 9 or more h/d had 1.19 times greater risk of all-cause mortality than those who sat less than 3 h/d; adults who reported TV-viewing of 3–4, 5–6, and 7 or more h/d had 1.14, 1.31, and 1.61 times higher risk of dying, respectively, than those who watched less than 1 h/d of TV [41]. Pavey et al. [42] followed an Australian cohort of women for 9 years and found that women who sat for 8–11 h/d had 1.45 times higher risk of death compared with those who sat less than 4 h/d; those who sat more than 11 h/d had a 1.65 times higher risk of death. Using objective assessment of sedentary time with accelerometers in the US National Health and Nutrition Examination Survey (NHANES) 2003–2004 cohort, adults in the highest and second highest quartile of sedentary time, had 2.74 and 3.26 times, respectively, increased risk of death compared with those in the lowest quartile, after 2.8 years of follow-up [43]. Campbell and colleagues [44] studied survival among adult participants who were diagnosed with invasive, nonmetastatic colorectal cancer. They found that cancer patients who spent 6 hours or more a day in leisure sitting were more likely to die than those with 3 hours or less of leisure sitting (HR: 1.27–1.36). Based on the NHANES data, American adults could gain 2 years of life by reducing their daily sitting time to less than 3 hours and could gain 1.4 years of life by reducing their daily television viewing time to less than 2 hours [6•]. Using data from the Australian 45 years and up cohort, van der Ploeg and colleagues [45] estimated that daily sitting time independently accounted for 7 % of mortality from all causes.
Summary and Implications for Clinical Practice
The evidence base for sitting and health is at an early stage, as most large scale studies in this area were published in the past 5 years. The evidence is moderately consistent for total sitting time and all–cause mortality, even when adjusted for or stratified by leisure time physical activity. This adds to previous research that identified screen-time as the sitting domain leading to increased mortality risk, and suggests conceptually that prolonged sitting in workplaces, in cars and in other aspects of daily life may pose similar risks.
The physiological evidence for diabetes prevention and for associations with biomarker risks is also becoming more consistent, but the evidence is not yet clear whether reducing total sitting time, or just interrupting sitting regularly confers the most benefit. Larger laboratory and clinical studies are needed in this area, before definitive public health recommendations are possible.
For obesity prevention, the theoretical impact of prolonged sitting on lower levels of total energy expended is compelling. However, more longitudinal data in diverse populations are required to support a stronger causal assertion that “not sitting” prevents weight gain.
For clinical practice, the evidence is not yet specific enough for guidelines, although Canadian national recommendations for children and adolescents do suggest limiting screen time to under 2 h/d [46]. Recent physical activity guidelines from the UK [47] and US [48] have specifically states that adults should reduce the amount of time they spend sitting, even if they are already physically active.
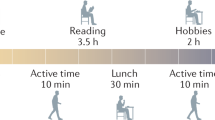
A conceptual summary of the effects of prolonged sitting, compared to reduced or interrupted sitting time is shown in Fig. 1. Not all the physiological pathways are fully understood, and the net energy balance relationship is still theoretical, but is likely to contribute independently to weight gain. Further, the biological mechanisms for (the observed epidemiological observations of) reductions in all cause mortality are only partly understood, but require further research. Nonetheless, Fig. 1 shows the potential for reducing sitting to improve health, even in a person who meets the physical activity recommendations [Fig. 1].
Thus, for clinical recommendations, should ‘reduced sitting’ be part of routine preventive advice? The case is increasingly compelling, but as part of an ‘active living’ approach to recommending that all adults and children ‘move more and sit less’, across the different settings and locations throughout the day. As generic recommendations, there is sufficient evidence for action, and given the ‘primum non nocere’ principle, reduced sitting is unlikely to have adverse effects. For this reason, as well as for the likely cardio-metabolic benefits, it is prudent to recommend reducing sitting time. The potential opportunities for reducing daily sitting time are abundant, and may include; reducing sitting at work, screen time at home, and possibly sitting in transport (through increased active travel). This recommended reduction of sitting may also lead to more total daily physical activity, providing increased benefits from that health-enhancing behavior as well [49]. Advice to reduce sitting can be universal, as it will likely benefit those with and without current chronic health problems. The only sub-groups for whom this advice is not recommended are those with serious comorbidity or physical disabilities, for whom standing or moving may be difficult or not possible. For all others, it is adding the ‘sit less’ to the ‘move more’ advice in clinical encounters that may lead to further health benefits.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major noncommunicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–29. This paper was a recent summary of the epidemiological evidence for physical inactivity and health using a burden of disease approach. It is slightly outside the remit of ‘sitting and health’ research, but is an important recent distillation of the health impact of not being physically active, with an estimated 9% of premature mortality across the world attributed to physical inactivity ( not meeting moderate intensity physical activity recommendations). This is around 5 million deaths per year that could be prevented if physical inactivity were abolished, and is a similar attributable number for tobacco smoking globally, and substantially larger to that attributed to obesity. For this reason, physical inactivity remains an important and under-recognized issue in preventive health.
WHO. Global recommendations on physical activity for health. Geneva: World Health Organization; 2010.
• Proper KI, Singh AS, van Mechelen W, Chinapaw MJM. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med. 2011;40:174–82. This systematic review explored the relationship between sedentary behaviors and health outcomes in adults, and identified 19 studies. The evidence was mixed for some outcomes, but a moderate evidence for sitting behavior and diabetes was evident, and a strong relationship between sitting behavior and all cause and cardiovascular disease mortality was noted. This type of summary is starting to synthesize the evidence that enables us to move towards public health recommendations.
Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–15.
Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality. JAMA. 2011;305:2448–55.
• Katzmarzyk PT, Lee IM. Sedentary behavior and life expectancy in the USA: a cause-deleted life table analysis. BMJ Open. 2012;2:4. This meta-analysis reviewed studies of sitting and mortality, and estimated increased life expectancy amongst USA adults if sitting time was reduced. The authors estimated that life expectancy would increase by 2 years if sitting were reduced to less than 3 hours per day, and an increase of 1.38 years in life expectancy would accrue if television viewing was restricted to less than 2 hours per day. Whilst the former may be a difficult goal to achieve in sedentary workplaces, the latter is a population health goal that might be achievable if alternate ways of spending time in domestic setting, became culturally normative. This is a long term approach, but is an important idea in thinking about the beneficial effects of reducing sitting time.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–504.
• Sedentary Behavior Research Network. Standardized use of the terms "sedentary" and "sedentary behaviors". Appl Physiol Nutr Metab. 2012;37:540–2. This methodological note describes the difference between not meeting physical activity recommendations (being inactive) and the specific sedentary behaviors, defined as “waking time behavior with an energy expenditure of less than 1.5 METS, whilst in a sitting or reclining position”. This definition is important because light physical activity might not meet recommendations, and includes standing or walking around, but is not classified as ‘sedentary behavior’ time. This distinction is important physiologically, epidemiologically, and for characterizing people’s lifestyle behaviors.
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81.
Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Reports, Statistics Canada, Catalogue no. 82-003-XPE. 2011;22.
Hagströmer M, Troiano RP, Sjöström M, Berrigan D. Levels and patterns of objectively assessed physical activity - a comparison between Sweden and the United States. Am J Epidemiol. 2010;171:1055–64.
Aresu M, Bécares L, Brage S, Chaudhury M, Doyle-Francis M, Esliger D, et al. Health survey for England 2008 Volume 1. Physical activity and fitness. UK: the NHS Information Centre for health and social care, 2009.
Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, et al. The descriptive epidemiology of sitting–a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41:228–35.
Chau JY, Merom D, Grunseit A, Rissel C, Bauman AE, van der Ploeg HP. Temporal trends in nonoccupational sedentary behaviors from Australian Time Use Surveys 1992, 1997, and 2006. IJBNPA. 2012;9:76.
van der Ploeg HP, Venugopal K, Chau JY, van Poppel MNM, Breedveld K, Merom D, et al. Population changes in nonoccupational sedentary behaviors in The Netherlands between 1975 and 2005. Am J Prev Med. 2013;44:382–7.
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6:e19657.
Bergouignan A, Rudwill F, Simon C, Blanc S. Physical inactivity as the culprit of metabolic inflexibility: evidence from bed-rest studies. J Appl Physiol. 2011;111:1201–10.
Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–67.
Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35:725–40.
Henriksen EJ, Bourey RE, Rodnick KJ, Koranyi L, Permutt MA, Holloszy JO. Glucose transporter protein content and glucose transport capacity in rat skeletal muscles. Am J Physiol. 1990;259(4 Pt 1):E593–8.
Kawanaka K, Tabata I, Katsuta S, Higuchi M. Changes in insulin-stimulated glucose transport and GLUT-4 protein in rat skeletal muscle after training. J Appl Physiol. 1997;83:2043–7.
Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551:673–82.
Hamilton MT, Etienne J, McClure WC, Pavey BS, Holloway AK. Role of local contractile activity and muscle fiber type on LPL regulation during exercise. Am J Physiol. 1998;275(6 Pt 1):E1016–22.
Stephens BR, Granados K, Zderic TW, Hamilton MT, Braun B. Effects of 1 day of inactivity on insulin action in healthy men and women: interaction with energy intake. Metabolism. 2011;60:941–9.
• Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–83. This experimental study examines physiological responses to sitting and compares a small number of mid aged adults in a randomized trial, with subjects allocated uninterrupted sitting, 2 minutes of light intensity every 20 minutes, and 2 minutes of moderate intensity every 20 minutes. This tests the question whether interrupting sitting with just standing or with moderate intensity activity improves physiological parameters. Objectively measured glucose uptake was examined, and the area under the curve was reduced in both the standing and moderate intensity categories compared with uninterrupted sitting. The insulin ‘area under the curve’ was similarly reduced in both intervention groups, suggesting post prandial responses to sitting are ameliorated by interrupting sitting time. This has implications for normalizing sitting related physiological responses.
Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55:2895–905.
George ES, Rosenkranz RR, Kolt GS. Chronic disease and sitting time in middle-aged Australian males: findings from the 45 and up Study. Int J Behav Nutr Phys Act. 2013;10:20.
Yates T, Khunti K, Wilmot EG, Brady E, Webb D, Srinivasan B, et al. Self-reported sitting time and markers of inflammation, insulin resistance, and adiposity. Am J Prev Med. 2012;42:1–7.
Cooper A, Sebire S, Montgomery A, Peters T, Sharp D, Jackson N, et al. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia. 2011;55:589–99.
Ford ES, Caspersen CJ. Sedentary behavior and cardiovascular disease: a review of prospective studies. Int J Epidemiol. 2012;41:1338–53.
Pinto Pereira SM, Ki M, Power C. Sedentary behavior and biomarkers for cardiovascular disease and diabetes in mid-life: the role of television-viewing and sitting at work. PLoS One. 2012;7:e31132. doi:10.1371/journal.pone.0031132.
Frydenlund G, Jorgensen T, Toft U, Pisinger C, Aadahl M. Sedentary leisure time behavior, snacking habits and cardiovascular biomarkers: the Inter99 Study. Eur J Prev Cardiol. 2012;19:1111–9.
Brown WJ, Williams L, Ford JH, Ball K, Dobson AJ. Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res. 2005;13:1431–41.
Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ. Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr. 2008;88:612–7.
Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon MM. Sitting behavior and obesity evidence from the Whitehall II study. Am J Prev Med. 2013;44:132–8.
Shuval K, Leonard T, Murdoch J, Caughy MO, Kohl HW, Skinner CS. Sedentary behaviors and obesity in a low-income, ethnic-minority population. J Phys Act Health. 2013;10:132–6.
Gomez-Cabello A, Pedrero-Chamizo R, Olivares PR, Hernandez-Perera R, Rodriguez-Marroyo JA, Mata E, et al. Sitting time increases the overweight and obesity risk independently of walking time in elderly people from Spain. Maturitas. 2012;73:337–43.
de Heer HD, Wilkinson AV, Strong LL, Bondy ML, Koehly LM. Sitting time and health outcomes among Mexican origin adults: obesity as a mediator. BMC Public Health. 2012;12.
Chau JY, van der Ploeg HP, Merom D, Chey T, Bauman AE. Cross-sectional associations between occupational and leisure-time sitting, physical activity and obesity in working adults. Prev Med. 2012;54:195–200.
Banks E, Lim L, Seubsman SA, Bain C, Sleigh A. Relationship of obesity to physical activity, domestic activities, and sedentary behaviors: cross-sectional findings from a national cohort of over 70,000 Thai adults. BMC Public Health. 2011;11.
Matthews CE, George SM, Moore SC, Bowles HR, Blair A, Park Y, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–45.
Pavey TG, Peeters GG, Brown WJ. Sitting-time and 9-year all-cause mortality in older women. Br J Sports Med. 2012;10. Accesible on: 1136/bjsports-2012-091676.
Koster A, Caserotti P, Patel KV, Matthews CE, Berrigan D, Van Domelen DR, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7:e37696.
Campbell PT, Patel AV, Newton CC, Jacobs EJ, Gapstur SM. Associations of recreational physical activity and leisure time spent sitting with colorectal cancer survival. J Clin Oncol. 2013;31:876–85.
van der Ploeg HP, Chey T, Korda R, Banks E, Bauman AE. Sitting time and all-cause mortality risk in 222,497 Australian adults. Arch Intern Med. 2012;172:494–500.
Tremblay MS, Leblanc AG, Janssen I, Kho ME, Hicks A, Murumets K, et al. Canadian sedentary behavior guidelines for children and youth. Appl Physiol Nutr Metab. 2011;36(59–64):65–71.
Department of Health, Physical Activity, Health Improvement and Protection. Start active, stay active: a report on physical activity for health from the four home countries’ Chief Medical Officers. UK: Department of Health, 2011.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59.
Bellew B, Bauman A, Martin B, Bull F, Matsudo V. Public policy actions needed to promote physical activity. Curr Cardiovasc Risk. 2011;5:340–9.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Adrian E Bauman declares that she has no conflict of interest. Josephine Y Chau declares that she has no conflict of interest. Ding Ding declares that he has no conflict of interest. Jason Bennie declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauman, A.E., Chau, J.Y., Ding, D. et al. Too Much Sitting and Cardio-Metabolic Risk: An Update of Epidemiological Evidence. Curr Cardiovasc Risk Rep 7, 293–298 (2013). https://doi.org/10.1007/s12170-013-0316-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12170-013-0316-y