Abstract
This chapter summarizes a review of previous and current knowledge of diagnostic imaging modalities of head and neck cancer. A quick analysis of each modality will be presented. Recent modalities like positron emission tomography – computed tomography PET-CT, Magnetic resonance imaging (MRI) will be discussed with more details through case presentations. The role of imaging in treatment planning and post-treatment outcomes will also be highlighted.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
19.1 Introduction
Diagnostic imaging is of great significance in the management of head and neck cancer patients. Treatment planning and prognosis depend heavily on imaging findings in addition to clinical and histopathological findings. A multi-disciplinary team of oncologists, radiologists, and surgeons work together, to plan the best treatment choices that are available for the patient. Accurate localization of a suspected malignant tumor and early detection of metastatic lymph nodes has a great impact in predicting the prognosis as well as in the choice and extent of therapy. Therefore, radiology not only plays a primary role in detecting the tumor, but also it helps monitoring the response to therapy during and after treatment [1]. Imaging may also provide important clues to the diagnosis when representative biopsies are difficult to obtain in deeply located lesions or when located in close relation to vital structures. These findings can profoundly influence the staging and management of patients with head and neck cancer. Finally, imaging may be used to detect recurrent or persistent disease before it becomes clinically evident, possibly with a better chance for successful retreatment. The single most important factor in the optimal use of all this information is the joint co-operation between the radiologist and the physician/ surgeon team in charge of patient care [2].
19.2 Imaging Modalities
The sixth edition of the American Joint Committee, on Cancer staging manual specifically states that “any diagnostic information which contributes to the overall accuracy of the pretreatment assessment should be considered in clinical staging and treatment planning” [3]. Many radiographic modalities are available for evaluation of head and neck cancer. The most commonly used modalities include computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography- computed tomography (PET-CT). The information from cross-sectional imaging is an important component for initial staging and post-treatment evaluation of the patient with head and neck squamous cell carcinoma [4].
In the following text we will give a closer look on the available imaging modalities. Some of these modalities are no longer used in evaluation of head and neck cancer, but knowledge about them is important because it explains the development in technology in diagnostic imaging field.
19.2.1 Plain Radiography
There is a long history of the use of the conventional radiography back to 1895 when Conrad Roentgen made the first X-ray film image of his wife’s hand (Fig. 19.1a). X-rays are a form of radiant energy that is similar in many ways to visible light. The difference between it and visible light is that they have a very short wavelength and are able to penetrate many substances that are opaque to light. The X-ray beam is produced by attacking a tungsten target with an electron beam within an x-ray tube [5, 6].
Conventional film radiography uses a screen-film system within a film cassette as the x-ray detector. When X-rays pass through the human body, they get attenuated while passing through body tissues of different densities where absorption and scattering of the beam happens and produce an image pattern on film. The film is then removed from the cassette and developed by chemicals. The final product is an x-ray image of the patient’s anatomy on a film [7].
19.2.2 Computed Radiography (CR)
Computed radiography (CR) is a filmless system that eliminates the problem of chemical processing and provides digital radiographic images which is easier to use and store. The same X-ray tube, and exposure control systems used in conventional radiography are still utilized for CR. The only difference is just the use of a phosphor imaging plate for the film screen cassette. The phosphor-coated imaging plate interacts with x-rays transmitted through the patient to capture an image. The digital image is transferred to a computerized picture archiving and communication system (PACS). The PACS stores and sends out digital images via computer networks to give medical care providers in many locations simultaneous direct access to the diagnostic images.
19.2.3 Digital Radiography (DR)
Digital radiography (DR) is a film-free and cassette-free system for capturing X-ray images in digital format. DR substitutes a fixed electronic detector or charge-coupled device for the film screen cassette or phosphor imaging plate. Direct readout detectors produce an immediate DR image. Direct digital image capture is particularly useful for angiography, because it provides rapid digital image subtraction, and for fluoroscopy, because it captures video images with low, continuous levels of radiation [8].
19.2.4 Interpretation of Radiography
The body has different densities, therefore radiography was able to demonstrate these differences into five basic radiographic densities: air, fat, soft tissue, bone, metal, and radiographic contrast media (which are suspensions Iodine and Barium compounds highly attenuate the x-ray beam and are used to outline anatomic structures). The X-ray beam can pass with very little attenuation through air, allowing nearly the full force of the beam to blacken the image. Bone, metal, and radiographic contrast agents attenuate a large quantity of the x-ray beam, allowing very little radiation through to blacken the image. Thus, bone, metallic objects appear white on radiographs. Fat and soft tissues stand in the middle attenuating intermediate amounts of the x-ray beam, resulting in proportional degrees of image blackening (shades of gray). Thick structures attenuate more radiation than thin structures of the same composition. Anatomic structures are seen on radiographs when they are outlined in whole or in part by tissues of different x-ray attenuation (Fig. 19.1b, c) [9].
In diagnosis of suspicious lesions, plain radiography is considered as a classic or conventional method, which is no longer used particularly in diagnosis of head and neck cancer after the emergence of the modern modalities that provide more accurate anatomical details with high resolution capabilities. As the value of x-ray techniques was very limited to stage head and neck cancer, they are now replaced by cross-sectional imaging modalities. However, plain radiography is still widely used in radiotherapy. Also, a “barium swallow” is still in use after pharyngeal surgery to investigate the presence of fistulae and in evaluating other functional disorders after radiotherapy [2].
19.3 Cross Sectional Imaging
Ultrasonography (USG), Computed tomography (CT) and magnetic resonance imaging (MRI) are techniques that can provide cross-sectional images. These techniques cross-examine a three-dimensional volume or slice of patient tissue to produce a two-dimensional image. The digital images obtained by USG, CT, and MRI examinations are ideal for storage and access on PACS (a computerized picture archiving and communication system).
19.3.1 Ultrasonography
Ultrasound imaging is one of the most important and widely used diagnostic tools in modern medicine. Recently, it has been introduced to the head and neck region to investigate and assess soft tissue swellings. The potential of ultrasound as an imaging modality was discovered in the late 1940s and early 1950s when John Wild and John Reid developed an ultrasonic imaging instrument and were able to reveal the capability of ultrasound for imaging and characterizing cancerous tissues at frequencies as high as 15 MHz. Ultrasonography of the head and neck is mostly used to evaluate soft tissue lesions specially the thyroid gland, salivary glands, and cervical lymph nodes [10].
Ultrasonography in combination with fine needle aspiration cytology (FNAC) is the most accurate method for neck nodal staging in most head and neck cancers [11]. However, execution of this procedure is relatively time consuming, and the obtained results are operator dependent [12].
19.3.1.1 Basic Ultrasound Principles
Sound is a mechanical wave resulting from a vibrating source, such as tuning fork or a string musical instrument. When this source vibrates, adjacent particles in air are displaced. These particles in turn push against other adjacent particles. The constant pushing is known as particle vibration. Ultrasound refers to sound waves beyond the human audible range. Diagnostic applications of ultrasound in the medical field use frequencies of 1–12 MHz. In medical Ultrasound the vibrating source is a ceramic element that vibrates in response to an electrical signal. The vibrating motions of the ceramic element in the transducer cause the particles of the surrounding tissues to vibrate. As the source vibrates, it periodically presses against and pulls away from the adjacent medium with resultant particle compression and expansion (rarefaction) in the medium. This movement of energy through the anatomical structures is called a wave. Patients are examined with a transducer that converts electrical energy into mechanical energy. When the sound beam is directed into the body at various angles; reflection, absorption and scatter change the returning signal to be weaker than the initial impulse [13].
19.3.1.2 Doppler Ultrasound
The first applications of the Doppler principle were in astronomic studies. This principle is still playing a major tool for cosmologic research. Then, other applications started gradually to emerge. Paul Langevin from France developed the first sonar equipment for detecting submarines. He also used piezoelectric crystals for transmitting and receiving ultrasound waves. This technology was used to sense submarines, initially during World War I and more extensively during World War II. Then, development of diagnostic Doppler ultrasound technology emerged. First, it was used in obstetrics and gynecology. Doppler sonography has allowed exploration and understanding of human fetus hemodynamic, which was inaccessible before. The Doppler refers to a change in frequency of a sound wave when either the source or the listener is moving relative to one another. When the source moves toward the listener, the perceived frequency is higher than the emitted frequency. This creates a higher pitched sound. If the sound moves away from the listener, the perceived frequency is lower than the transmitted frequency, and the sound will have a lower pitch. In the medical application of the Doppler principle, the frequency of the reflected sound wave is the same as the frequency transmitted; only if the reflector is stationary. Color Doppler can be used to characterize the maxillofacial soft tissue vascular anomalies (Fig. 19.2) [13, 14, 15].
19.3.1.3 Advantages of Ultrasonography
Ultrasonography has an exclusive and valuable role in imaging the neck region. It can provide excellent and reproducible anatomic images that are safe, comfortable to the patient and inexpensive. The role of ultrasonography has evolved to provide important data in many clinical indications: to determine pathology, volumetric, vascular status, tumor size, and guided fine needle biopsy [16].
Ultrasonography also has some distinctive characteristics that are advantageous in comparison to other competing modalities such as computed tomography (CT) and Magnetic Resonance Imaging (MRI). It is portable, so it can be easily transported to the bedside of a patient. It is a form of a nonionizing radiation and is thought to be safe until now. It can produce images in real time. It has a resolution in the millimeter range, which may be improved if the frequency is increased. It can depict blood flow information by applying the Doppler principle.
19.3.1.4 Limitations of Ultrasonography
Although Ultrasonography has many unique characteristics, it still has some limitations.
-
Ultrasonic examination is only through a limited window.
-
Organs containing gases and bony structures are hard to be imaged adequately.
-
Special training for the radiologist is needed to perform and interpret it.
-
Inability to obtain good images from certain types of patients like obese patients.
In summary, air and dense anatomic structures such as bone obstruct evaluation of structures lying deep to them. Skeletal structures are barely accessible if at all with US, at least in the adult [17].
19.3.1.5 Ultrasonography and Cancer Screening
Cancer screening is an examination in subjects who are asymptomatic and generally healthy. It is a group of diagnostic procedures that are frequently done on asymptomatic subjects for early identification of a possible malignancy. Discovering the disease in its early stages can modify the natural history of the cancer and consequently improve the treatment outcomes. Cancer surveillance is usually done for asymptomatic individuals but at high risk to develop malignancy. Both screening and surveillance are considered preventive methods in oncology which can help decreasing the morbidity and mortality rates. Their goal is the prevention/delay, within reasonable costs and through early diagnosis and treatment. Malignancy development takes place in two phases the preclinical phase, which begins at the time of the biologic development of the disease itself which is followed by a clinical phase that begins with the onset of symptoms. So, Ultrasonography is better than other ionizing techniques such as CT because it is noninvasive and inexpensive [18].
19.3.1.6 Ultrasonography of Cervical Lymph Nodes
The number of lymph nodes in a normal neck is nearly 300 lymph nodes. The pharyngeal nodes tend to be very small in size, usually less than 0.5 cm in their short axis and flattened or oval in the transverse view of the neck. Enlarged lymph nodes are usually due to either inflammation or hyperplasia [19]. High-resolution Ultrasonography shows a white line of fat and intranodal blood vessels running through the center of the lymph node known as a hilar line. The hilar line is present in most benign lymph nodes greater than 0.5 cm and is also more prominent in older patients. A hilar line is hardly seen in malignant lymph nodes. Because lymph node hyperplasia is frequently common in the neck, only those lymph nodes >0.5 cm in the short axis are usually biopsied. Those with a short axis 0.5 cm in the pharyngeal region reaching 0.8 cm in their short axes should have their location marked and be reexamined in 6 months. Metastatic lymph node appearance is generally more rounded in the transverse view with a short/long axis ratio >0.5 cm. Postreatment ultrasound surveillance for cancer is done in the transverse view, since all lymph nodes may appear elongated in the longitudinal view (Fig. 19.3). Another finding of malignancy in addition to a rounded shape and the absence of a hilar line is the position of internal jagular vein which migrates anterior next to the carotid artery in the postoperative neck. Metastatic nodes are commonly located in proximity to the jugular vein or within the carotid sheath; any deviation of the jugular vein away from the carotid artery strongly suggests malignancy. In addition to causing deviation of the internal jugular vein, malignant lymph nodes tend to compress the vein and cause a partial obstruction to blood flow. Benign lymph nodes rarely do this until they become quite large [20].
19.3.1.7 Ultrasonography and Cancer Staging
Treatment planning is principally influenced by the pretreatment staging of the disease. Advanced stages most likely affect the prognosis of the disease which worsens by 50% with advanced stages. In most cases, the treatment of choice in the initial stages is surgical excision of the primary tumor which may be more conservative or more radical depending on the anatomic relation of the tumor to its surrounding structures. The anatomic- pathologic evaluation should involve a reasonable margin of healthy tissue around the excised lesion.
There are several phases of diagnosis that should be followed. This includes (1) the first or initial diagnosis (identification of the lesion and its topographical position), (2) characterization or differential diagnosis of the lesion, in the terms of non-tumor vs. tumor, benign vs. malignant and primary vs. metastatic, (3) staging (assessment of the spread of the disease, for diagnosis, treatment and prognosis), (4) treatment plan including surgery, radiotherapy, chemotherapy, combinations between different choices, (5) assessment of response of the tumor during and after therapy (both in the short term for cure and complication judgment and in the long term for follow up and assessment of recurrent lesions). Accurate staging is critical in the patient who will undergo surgical interaction. In early stages, surgical removal of the primary tumor is the treatment of choice. This choice can be more radical or more conservative according to the relation of the tumor to surrounding vital structures and lymph node involvement (metastases). In cases, with locally advanced tumors (locoregional infiltration), palliative surgery and/or cytoreductive surgery may be performed. Tumor debulking, i.e. the removal of more-or-less large parts of the tumor mass, can affect positively the response of systemic or radiation therapy (adjuvant). Sometime starting with chemotherapy and /or radiotherapy (neoadjuvant) before surgery can improve the surgical outcomes and reduce postsurgical complications. In this way curative surgery may be able to obtain a result similar to that of radical surgery but without adjuvant treatment, or it may be possible to eliminate (potential) micrometastases after surgical resection, or to re-evaluate a lesion not initially considered for radical surgery (debulking). In fact, the goal of neoadjuvant treatment is to obtain a downstaging of the tumour [18].
Another modality of Ultrasonography is the endoscopic ultrasound (EUS). It can be used for evaluation of pharyngeal lymph nodes which cannot be examined by external ultrasonographic examination. EUS was used in staging of esophageal cancer. It provided a detailed view of the esophageal wall, helping in determining tumor depth of infiltration, and characterizing lymph nodes as malignant or benign. It was the most accurate modality for regional staging of esophageal cancer and is more accurate than computed tomography and positron emission tomography scan for the characterization of nodal status [21].
19.3.2 Computed Tomography
In 1970, the CT technology was developed. This technology was initially used in brain imaging, and then it was rapidly extended to the whole body. When comparing the conventional radiograph with CT, the difference is that; radiograph capture a whole picture, while CT take several captures in the form of slices where each slice shows the anatomical contents of this section. CT images are produced by a combination of x-rays, computers, and detectors. In the CT unit, the x-ray tube rotates around the patient, and images are produced by exposure to a very thin beam of X-ray. A computer-controlled bed transfers the patient in short increments through the opening in the scanner housing. Each image or slice requires only a few seconds. The thickness of these axial images or slices ranges from 1 to 10 mm depending on the indications of each study. An average CT study takes approximately 10–20 min. As in a radiograph, the amount of the x-ray beam that passes through each slice or section of the patient will be attenuated according to the density of each tissue. However, in CT, the x-ray beam hits the detector instead of film, and the detectors subsequently convert it to an electron stream. This electron stream is digitized (i.e. converted to numbers known as CT units or Hounsfield units); then a computer software converts these numbers to corresponding shades of black, white, and gray which is printed on a film. Dense structures like bone allow only a small amount of x-rays to strike the detectors. The result is a white density on the film. On the other hand, air will absorb little of the x-ray beam, allowing a large number of x-rays to strike the detectors. The result is a black density on the image. Soft tissue structures appear gray on the image (Fig. 19.4a, b).
(a) Axial contrast-enhanced CT image showing outstanding anatomical details of bony structure and enhanced soft tissue details. (b) Coronal CT image showing the anatomical details of the neck in a patient with a T3 N2 right aryepiglottic fold (supraglottic) squamous cell carcinoma. (c) MidSagital contrast enhanced CT image showing the anatomical details of head and neck. (d) Axial CT image (with contrast agent enhancement) showing an artifact arising from metallic dental restoration fillings (amalgam) which causes rarefaction and inability to evaluate the obtained image
This CT digital information can be displayed on a video monitor, stored on magnetic tape, transmitted across computer networks, or printed on radiographic film via a format camera.
19.3.2.1 High-Resolution Computed Tomography
High-resolution computed tomography (HRCT) refers to CT studies that result in thin slices that are approximately 1.0–2.0 mm thick.
19.3.2.2 Spiral Computed Tomography
Spiral CT imaging is a relatively new development. This technology is similar to standard CT but with a few new twists. In helical or spiral CT, the patient continuously moves through the gantry while the x-ray tube continuously encircles the patient. This combination of the patient and x-ray tube continuous movement results in a spiral configuration. This technology can produce 1 slice per second, and the slice can vary in thickness from 1 to 10 mm. The resolution and contrast of these images are better than standard CT images. In the helical or spiral CT scanner, the x-ray tube continuously circles the patient while the patient couch moves continuously through the opening in the x-ray tube gantry. The combination of continuous patient and x-ray tube movement results in a spiral configuration; hence the name “helical.” In a standard CT or nonhelical scanner, the patient couch moves in short increments toward the gantry opening and stops intermittently to allow the x-ray tube to move around the patient. Thus, the x-ray tube moves around the patient only when the couch is stationary.
19.3.2.3 Multislice Computer Tomography
Conventional CT scanners have a single row of detectors; thus only one tomographic slice is generated for each rotation of the x-ray tube around the patient. In multislice CT there are multiple contiguous rows of detectors that yield multiple tomographic slices or images with each rotation of the x-ray tube. There can be as many as 16 detector rows in one CT machine, resulting in reduced acquisition time.
19.3.2.4 Computed Tomographic Angiography
This term refers to imaging of blood vessels using either a multislice or a helical CT scanner. The procedure produces 3-mm slices during the rapid injection of contrast media.
19.3.2.5 Three Dimensional CT Images (3D CT)
This format of CT is usually done to study and evaluate the bony structures of the maxillofacial skeleton. This technique does not show the adjacent soft tissues. In oncologic lesions with extensive bone destruction, 3D display can help the surgeon to determine the outlines the margins of bone resection in relation to the tumour and the normal adjacent tissues [22].
19.3.2.6 Requirements for Optimal CT Diagnostic Study
19.3.2.6.1 Patient Positioning
The patient should be comfortably positioned in a supine position during quite respiration. The supine position with slightly extended neck is needed in order to compare symmetric structures. Malposition may result in disease simulating appearance. The patient should be comfortable during the study; this will help the patient, dropping the shoulders to a position as low as possible which is applicable for all indications if multidetector spiral CT (MDCT) is used, as this modality allows retrospective high quality reformatting in every spatial plane.
19.3.2.6.2 Contrast Agent Injection
CT imaging is accomplished with and/or without intravenously injected contrast media. The intravenous contrast media enhance or increase the density of blood vessels, vascular soft tissues, organs, and tumors as in a radiograph. This enhancement assists in distinguishing between normal tissue and a pathologic process.
Injection of iodinated contrast agents is essential to obtain state of the art CT images. Optimal tissue enhancement allows correct differentiation between tumoral and normal tissue. For all practical purposes, a single bolus technique with an injection rate of 1 cc/s is appropriate on modern CT machines. A total amount of 100 ml is adequate. To some extent, a higher volume (up to 150 ml) may be required when an incremental or single slice spiral CT technique is used. It is essential to wait 60 s before starting the image acquisition, to give the contrast media a chance to diffuse throughout the body. A subsequent saline injection at the same injection rate is recommended [23]. Currently, in most patients computed tomography (CT) or magnetic resonance imaging (MRI) is performed for pre-therapeutic staging of a head and neck malignancy. Based on the information obtained from those techniques, treatment planning strategies are more clearly defined. A common question is which of these techniques should be used on a particular patient. The most widely used technique is CT, as it has a number of important advantages over MRI.
19.3.2.7 Advantages of CT
-
Wide availability
-
Relative low cost
-
Easy to execute
-
Rapid scan acquisition
-
Short examination time, less image quality degradation caused by motion, such as swallowing and respiration
-
Superior quality for bone details (Fig. 19.4c)
-
Demonstration of calcifications
-
High quality multiplanar imaging on multidetector CT systems
-
Easy extension of the study into the upper thoracic cavity or intracranial cavity, if needed
-
Easier interpretation
The new technological advances in CT have led to an increase of its use. However, there is a high radiation dose exposure while the examination is carried out. CT accounts for more than 40% of all radiation exposure to patients from diagnostic imaging. There may be as many as 65 million CT examinations performed each year in the United States and as many as 260 million CTs performed yearly worldwide. Many (up to 11%) of these examinations are performed on infants and children, who are more susceptible to the adverse effects of radiation. These considerations put a great responsibility on the radiologist and physicians to limit CT use to definitive indications; provide dose-efficient CT imaging protocols; suggest other imaging techniques, especially for young children, who are at the greatest risk from radiation; work with manufacturers to limit radiation dose; and educate patients and health care providers about the potential risks of radiation. In addition to that, CT also has a number of disadvantages compared to MRI.
19.3.2.8 Disadvantages of CT
-
Relatively low soft tissue contrast resolution.
-
Administration of iodinated contrast agent is necessary to enhance the resolution.
-
Severe image quality degradation by dental restorations or other metallic foreign objects (Fig. 19.4d) [6].
19.3.3 Magnetic Resonance Imaging (MRI)
After 10 years of the emergence of CT, Magnetic resonance imaging (MRI) applications in the medical field revolutionized diagnostic imaging and provided a great leap forward in diagnostic imaging of the whole body and specifically imaging of head and neck pathologies. MRI can provide critical information in detection of neoplastic lesions either clinically detected or not. It has added value in depiction of anatomical details of soft tissues, marrow involvement, and perineural spread (invasion of nerve tissue). The excellent tissue characterization and multiplanar imaging capability of MR imaging resulted in more accurate diagnosis of neoplastic and benign processes [24].
MR is a technique producing tomographic images by means of magnetic fields and radio waves. The physics of MRI is complicated and beyond the scope of this chapter. To make it simple, MR is based on the ability of a small number of protons within the body to absorb and emit radio wave energy when the body is placed within a strong magnetic field.
Different tissues absorb and release radio wave energy at different, visible, and characteristic rates. MR scans are acquired by placing the patient in a static magnetic field 0.02–4 tesla (T). Low field strength systems are less than 0.1 T, midfield systems range between 0.1 and 1.0 T, and high-field systems range between 1.5 and 3.0 T. MR analyzes multiple tissue characteristics, including hydrogen (proton) density, T1 and T2 relaxation times of tissue, and blood flow within tissue. A small number of tissue protons in the patient align with the main magnetic field and are subsequently displaced from their alignment by application of radiofrequency (RF) gradients. When the RF gradient is terminated, the displaced protons realign with the main magnetic field, releasing a small pulse of energy that is detected, localized, and then processed by a computer algorithm similar to that used in CT to produce a cross-sectional tomographic anatomic image.
Standard spin-echo sequences produce a batch of images in 10–20 min. Rather than obtaining data for each image one slice at a time, many spin-echo MR sequences obtain data for all slices in the imaged tissue volume throughout the entire imaging time. Consequently, patient motion caused by breathing, cardiac and vascular pulsation may degrade the image considerably. MR has advanced to rapid-imaging breath-hold techniques. Continuing technologic improvements are making MR acquisition times comparable to those for CT [25].
19.3.3.1 Advantages of MRI
One of the outstanding advantages of MR is its excellent soft tissue contrast resolution (Fig. 19.5a–c). Also, it has the ability of providing images in any anatomic plane without exposure to ionizing radiation. Image quality is not hindered by small metallic dental fillings like CT, but image artifacts can still result with big restorations.
(a) Axial T2- weighted MR image showing excellent anatomical details of soft tissues and demonstrate a mass in the left side. The lesion is clearly delineated from surrounding structures and extending under the masseter muscle which does not display intrinsic changes. (b) Axial T2- weighted MR image showing a mass in the nasal sinus area. (c) Coronal STIR MR image (with contrast enhancing agent) showing a mass the submandibular region appearing with higher signal intensity (arrow). (d) Axial MR image shows artifact hindering the ability to evaluate the obtained image caused by a large fixed metallic restoration in the oral cavity. (e) Axial MR image with artifact due to the movement of the patient during the examination study in the MRI unit leading to inability to evaluate the hazy obtained image
19.3.3.2 Disadvantages of MRI
MRI is relatively expensive, and therefore it is less available. MR is limited in its ability to demonstrate dense bone details or calcifications, it has long acquisition time, making this technique sensitive to motion artifacts. It is not easy with MRI to properly stage both primary tumor and neck nodal disease in a single study. Also, because of the physically limited space for the patient within the magnet, a number of patients may suffer from symptoms of claustrophobia and necessitate sedation or are simply unable to tolerate MR scanning. “Open” magnet design can be helpful in the MR imaging of obese and/or claustrophobic patients, but these units have lower field strength and lack the resolution of the high-field strength “tube” magnets.
There is no agreement regarding the use of CT or MRI as primary imaging tool, although most of radiologists prefer to use MRI because of its high ability in depicting anatomical structures without exposure to any radiation doses. It is quite hard to define the ideal imaging protocol depending upon the availability, cost, presence of prosthetic implants etc [2].
19.3.3.3 MR Artifacts
Artifacts in MRI may result from distortion of the magnetic field due to the presence of ferromagnetic objects such as orthopedic devices, surgical clips and wire, and metallic foreign bodies in the patient. The artifact is seen as areas of signal void (Fig. 19.5d) at the location of the metal implant with a rim of increased intensity and a distortion of the image in the surrounding area. Also, motion artifacts are common in MR because of the long image acquisition time which results in blurred images (Fig. 19.5e). So, patients are advised to hold his breath periodically to avoid the artifact [6].
19.3.3.4 Requirements for Optimal MRI Diagnostic Study
Magnetic resonance imaging (MRI) has been extensively used in the assessment of head and neck cancer. Accurate determination of tumor extent is of utmost importance in head and neck cancer because it has important consequences for staging of disease, choice of treatment, and prediction of prognosis. Magnetic resonance imaging is superb in detecting submucosal and perineural tumor spread, skull base invasion, and nodal metastases.
19.3.3.4.1 Patient Positioning
Similar to CT, image acquisition is performed with the patient in the supine position, and during quiet respiration. The head and neck should be aligned and symmetrically positioned. The patient should be instructed not to move, cough and swallow during the image acquisition.
19.3.3.4.2 Coils
The choice of the receiver coil depends on the localization of the disease process. If the tumor is localized in the oral cavity or the lower part of the neck (infrahyoid), the neck coil should be used. When the neoplasm is at the level of the base of the skull, sinonasal cavities, face, parotid glands, or nasopharynx, the head coil should be selected. However, when head and neck region needs to be covered in one exam, as in nasopharyngeal cancer where neck adenopathies are usually involved, the head and neck coil can be both used together, allowing detailed evaluation of the entire head and neck region. On the other hand, in the absence of a dedicated neck coil, one can choose to stage the primary tumor with MRI, using the head coil, and perform an additional CT or Ultrasonography of the neck to stage neck disease.
A standard examination of the head and neck should start with a T2-weighted spin echo. The high signal intensity of fat on a T2-weighted sequence can be a disadvantage because it may reduce the contrast between a tumor and the surrounding tissues. This low contrast can be enhanced by applying an additional “inversion recovery preparation pulse” (a short inversion time known as STIR) (Fig. 19.5a, b).
Repetition of this sequence after injection of gadolinium-DTPA (contrast media), and comparison with the pre-injection sequence helps to outline the areas of contrast enhancement and to differentiate these areas from fat. A fat-saturated T1-weighted SE sequence after injection of gadolinium-DTPA may be helpful, as the contrast media enhances resolution of tissues and fat. Yet, such a sequence has some drawbacks too. A fat-suppressed sequence is susceptible to artifacts, which is more observed in the head and neck region because of the presence of different types to tissues (soft tissue-bone and tissue-air interfaces). Furthermore, the depiction of anatomical structures is reduced, and the acquisition time is longer. The selection of the plain of imaging is selected according to the location of the lesion [25].
19.3.3.4.3 Contrast Agent
Most neoplasms will show increased signal intensity after contrast agent injection. In MR studies for head and neck neoplasms, acquiring sequences before and after injection of gadolinium-DTPA (at a dose of 0.1–0.2 mmol/kg body weight) is mandatory. This will usually increase the contrast between the tumor and the surrounding lesions. Tumor necrosis becomes more visible after injection of gadolinium which is important in staging the neck nodes. On the other hand, tumors infiltrating bone marrow may become less well visible after contrast injection, as their signal intensity may become similar to that of the surrounding bone marrow. Ultra-small super paramagnetic iron oxide (USPIO) particles are captured by macrophages in normally functioning lymph nodes. As a result, signal intensity reduction is observed in tissues accumulating these particles, because of the susceptibility effects of iron oxide. Metastatic lymph nodes show increased intensity on sequences weighted to these effects [6].
19.3.3.5 Additional MRI Techniques
The flexibility of MRI may provide each patient a tailored study that fits his condition. Although the standard sequences solve the diagnostic questions in most cases, in some instances additional sequences can further characterize pathological tissues. MRI is considered as a gold standard in structural imaging of the head and neck, particularly for the deeply located lesions as the skull base and related regions, oral cavity, larynx and hypopharynx. In addition to its excellent anatomical depiction, it has other functional imaging characteristics. MRI may investigate some functional aspects of disease using the recent developments in diffusion and perfusion MRI techniques.
19.3.3.5.1 Diffusion-Weighted (DW) MRI
Diffusion-weighted (DW) MRI is an imaging technique showing molecular diffusion, corresponding to the Brownian motion of the spins in biologic tissues. The apparent diffusion coefficient (ADC) is a parameter used to quantify DW-MRI. The ADC is in part determined by the molecular diffusion of water, the microcirculation of blood and the presence of structures on a microscopic scale (microvessels, tubules, and others) [26]. Cell size, cell density and cell integrity influence the signal intensity seen on DW images, as well as the value of the ADC. This technique shows potential to distinguish benign and malignant tumour. Volumetric interpolated breath-hold imaging (VIBE) is a 3D fat-saturated gradient-echo T1-weighted sequence that can be optimized for short acquisition times, providing high-quality MR angiograms if acquisition and contrast injection are properly synchronized. It can also be used to evaluate tumor perfusion, or as an alternative to T1-weighted SE sequences, as it combines excellent image contrast with minimal partial volume averaging [27]. These sequences provide high-resolution anatomical images of the cranial nerves; however, involvement of the nerves by neoplasms is often best detected on gadolinium enhanced images.
Recently, many reports have been published which investigated the capabilities of Diffusion-weighted imaging (DWI) as a functional diagnostic tool for detection and characterization of tumors. Technical improvements and higher magnetic fields (with wider use of 3 T systems) enhanced research in diffusion techniques. The principle of diffusion weighted imaging (DWI) is based on exploring the motion of the free water molecules in tissue, including intracellular and extracellular motion. Diffusion-weighted MRI in combination with size and morphological criteria of the tumor are a strong predictor of presence of malignant lymph nodes. It is also indicated to assess response to chemoradiotherapy as early as 1 week after beginning of treatment [6].
19.3.3.5.2 Perfusion Techniques
Perfusion techniques are mostly used for the assessment of the tumour response to treatment with antiangiogenic (prevention of formation of new blood supply to the tumour cells) and vascular-disrupting agents. Many chemotherapeutic agents and radiotherapy are targeting angiogenesis. Perfusion imaging estimates local blood volume variations and capillary permeability. Tissue characteristics such as blood flow, blood volume and transit time parameters have been related with tumour vascularization and microvascularization. It thus provides information for tumor classification and in T1-weighted dynamic contrast-enhanced Perfusion MRI is studied to measure the drug effects on tumour microvascularity and capillary permeability [28].
19.4 Nuclear Imaging
Nuclear radiology is a functional imaging technique that includes both therapeutic and diagnostic modalities. Many techniques are available for nuclear imaging diagnosis such as single photon emission computed tomography (SPECT) and positron emission tomography (PET) which is progressively being used in the evaluation of head and neck cancer. PET and PET-CT, using fluorine-18-labeled 2-fluoro-2-deoxy-D-glucose (18FDG) as a tracer, have received a lot of consideration recently. This modality can be used in pretreatment staging of the neoplasm, during therapy, and in the post treatment follow-up. Radiographic anatomic imaging depicts and measures the dimensions of a lesion, but functional imaging shows the activity related to malignant changes. PET-CT has greatly improved patient diagnosis, tumor staging, and post treatment evaluation of tumour therapy. Also PET-MRI is a new technology which is recently introduced and showed promising results in follow up and detection of recurrent disease.
Nuclear imaging studies provide high functional resolution, physiologic and functional information not otherwise obtainable by other modalities like Ultrasonography, CT, and MRI.
Although PET is considered the best modality in detection and staging of cancer, it still has some drawbacks. PET has a higher sensitivity but lower specificity in detecting tumors in comparison with CT and MRI. The low spatial resolution and lack of tracer uptake in some neoplasms can cause false-negative results. Also, tracer accumulation in inflamed tissues may cause false-positive results. The high cost of PET imaging is also an important drawback [29].
19.4.1 Imaging Principles of Nuclear Imaging
The basic principles of diagnostic nuclear imaging are simple. Comparing the normal patterns of uptake, distribution, and excretion with the abnormal patterns leads to diagnosis of presence or absence of disease. External detection and mapping (image formation) of the biodistribution of radiotracers that have been administered to a patient either orally or parentally is the basic foundation for nuclear imaging. Sometimes a radionuclide or radioisotope is used alone or in combination with other physiologically active compounds. Usually, a radioactive isotope is combined with a physiologically active compound to create a di-pharmaceutical.
19.4.2 Image Interpretation
In order to interpret the obtained nuclear images, a basic knowledge of anatomic, physiologic, and nuclear imaging principles is necessary to make accurate diagnosis based on nuclear medicine studies.
When preparing a case for nuclear imaging, determination of the radiopharmaceutical isotope is important. Also, age, gender, the site of injection, patient orientation during imaging, the type of study, and the type of images (planar or tomographic, static or dynamic) should be considered.
Therefore, a basic knowledge of the normal biodistribution of the radio-pharmaceutical and the usual indications for performing the study are needed. This information is critical to image interpretation. One approach to enhance and speed detection of abnormalities and asymmetries is to study the first frame (image) or two very closely and then move directly to the last frame. Direct comparison of early and late images will show changes between the two images.
19.4.3 Positron Emission Tomography (PET)
PET is considered the technique of choice for metabolic and molecular imaging of cancer (Fig. 19.6a–c) and is now widely available. PET scanning with 18fluorodeoxyglucose (18FDG) can be used for staging and evaluation of recurrence for primary head and neck tumors. 18F-FDG, is used as a marker of glycolysis. It has excellent intrinsic molecular sensitivity. For that reason, PET can be used for detection of nanomolar concentrations of molecules. This prospect of molecular applications (e.g. receptor expression, integrines and apoptosis) give it a lot of credit to be used in the future. PET has recently been improved by the combination of a CT scan, leading to the integration of morphological and anatomical information of CT with the metabolic and molecular information of PET [30].
Since 1970, Positron emission tomography (PET) started to be utilized for clinical imaging. It is more sensitive than CT or MRI for T1-staged lesions. The most recent advances in PET systems are the hybrid PET/CT scanners. The use of this modality was limited to specialized research institutions and was focused on the physiology and pathophysiology of the brain, heart, and then the use of PET in oncology has considerably increased [31].
Recently, several authors have shown the high negative predictive value and accuracy of PET for the follow-up after radiotherapy of head and neck tumors [32]. In case the PET scan is negative, further investigations are not needed according to most authors. PET may be performed within 4 weeks after the completion of chemotherapy, chemoimmunotherapy, or chemohormonal therapy. In contrast, PET is normally not performed until 2–3 months after radiation or chemoradiation or 1–2 months after surgery, because acute inflammatory changes that are commonly seen in the first few weeks after radiation or surgery can result in false positive PET scans.
However, PET evaluation of distant metastatic disease should be reliable even during this time. PET uses positron-emitting radioisotopes of natural elements, oxygen-15, carbon-11, nitrogen-13, and fluorine-18. These radioisotopes can keep their normal biologic function. So, they are used for the combination of many positron-emitting radiopharmaceuticals. 18fluoro-deoxyglucose- FDG-CT when used in combination with CT or MRI, the diagnostic efficacy increase to detect metastases. So it can be used for pre and post-treatment follow up. In addition, it may be used for cancer screening [33]. PET is a true whole-body imaging technique; modern scanners can acquire studies covering from head to knee area within 25 min or less (Fig. 19.7a–c). Therefore, PET is not limited to the depiction of one target lesion, but can be used to assess multiple tumor sites and to monitor their responses to different therapeutic choices. The spatial resolution of PET has improved during the recent years, and under optimal conditions, state-of-the-art PET scanners now provide a resolution of 3–4 mm. In routine clinical protocols, the spatial resolution is in the range of 5–6 mm. in consequence, PET is still limited in the detection and characterization of small lesions and in the evaluation of tumor heterogeneity in larger lesions [34, 35, 36].
19.4.4 Positron Emission Tomography-Computed Tomography PET-CT
Recently, PET-CT was introduced in oncology of head and neck. This modality allows direct image fusion between PET and CT and improves the ability to anatomically localize foci of fluorodeoxyglucose (FDG) uptake (Fig. 19.8a–c). The potential of PET-CT to evaluate malignancies of the head and neck, specifically squamous cell carcinoma is considerably high. It can be used for pretreatment staging, treatment monitoring, and post-treatment evaluation. It can identify lesions even 1 mm in volume. PET also has the ability to detect metastatic cervical lymph nodes, which may be both clinically occult and not detected by CT or MR. False-negative results may be obtained in patients treated with radiotherapy if the study is performed within 3 months of the completion of treatment. Also, false-positive results for treated oral and pharyngeal malignancies may be obtained due to artifact from tongue uptake after radiotracer administration, lingual tonsil uptake, retained salivary uptake in the oral cavity, or post treatment granulation tissue. Similar false-positive findings can be seen in laryngeal carcinomas treated with combined chemotherapy and radiotherapy, and may be due to evaluation in less than 3 months period after completion of chemoradiotherapy. Several studies have assessed the diagnostic accuracy of PET-FDG for detecting recurrent HNSCCA. PET-FDG has a higher diagnostic accuracy compared to cross-sectional imaging. It must be noted that the most accurate PET results will only be obtained if the information is interpreted in relation to clinical findings as part of a multidisciplinary head and neck oncology team.
Also, PET-CT was able to detect unknown primary tumors of the upper aerodigestive tract. PET-CT is mostly performed after confirming the presence of metastatic HNSCCA and following a negative endoscopy. PET is usually performed before endoscopic biopsies to help improve the yield of the speculative tissue sampling. The diagnostic findings will likely increase with PET-CT because this technique improves accurate anatomic localization of areas of abnormal FDG uptake [31].
PET-CT is currently under investigation in determining response to nonsurgical treatment modalities; either chemotherapy and/or Radiotherapy. Comparison of pretreatment standardized uptake values (SUVs) to SUVs 2 weeks into treatment can allow measurement of the speed of response and the sensitivity of the tumour to the treatment modality. Poorly responsive tumours can then be treated to higher doses of radiation or shift to perform surgery. PET-CT is very promising, and it will most likely be the modality of choice for both pre-treatment and post-treatment assessment in head and neck cancer in the future [33].
19.5 Molecular Imaging in Cancer
Molecular imaging in cancer has made great progress in the capabilities of conventional anatomical imaging methods. Molecular imaging will allow clinicians to not only localize tumors in the body, but also to depict the expression and activity of specific molecules (e.g. proteases and protein kinases) and biological processes (e.g. apoptosis, angiogenesis, and metastasis). Therefore, it can be used in monitoring the response to cancer therapy. This information is expected to have a major impact on cancer detection, individualized treatment, and drug development [37].
19.5.1 PET as a Biomarker
PET biomarkers allow noninvasive serial studies of the whole tumor mass. The most unique characteristic of PET-based biomarkers is that they are measuring a biologic process and not the concentration of a particular cellular protein. This differs in several ways from biomarkers derived from tumour biopsies or plasma samples. In biopsies, only small parts of the tumor can be evaluated [38].
The intratumoral heterogeneity can significantly affects the analysis of biomarkers derived from tumor biopsies which is really important in evaluating changes in a biomarker during treatment because it is difficult to ascertain that different parts of the tumor demonstrated the same expression of the biomarker before therapy. Serum biomarker studies are noninvasive and can easily be used to measure changes in multiple biomarkers over time. Yet, the results may be baffled by the metabolism and excretion of tumor derived biomarkers. Imaging of these biomarkers allows direct assessment of the tumor tissue without interfering with the metabolic processes in plasma or normal organs. The imaging signal in PET studies is the result of the functional interaction of multiple proteins. This is illustrated by studies that have correlated tumor FDG uptake with the expression of glucose transporters and hexokinase, the two classes of proteins involved in the intracellular uptake and trapping of FDG [39, 40].
19.6 Neoplasms of Head and Neck
In squamous cell carcinoma of the head and neck, CT, MRI and PET-CT play a critical role in pre-treatment staging of tumors.
19.6.1 Maxillary Sinus, Nasal Cavity, Nasopharynx
Determination of early stage disease (T1 and T2) is based on clinical assessment of disease spread. T3 disease is based on spread of the disease to involve the thin bony component that comprises the soft tissue structures immediately adjacent to the primary site. Early cortical erosion is better detected on CT and PET-CT compared to MR (Fig. 19.9a–g). However; MRI is still the imaging method of choice by most radiologists for bone marrow involvement, intracranial extension, and perineural extension (Fig. 19.10a–f) and should be performed when attempting to distinguish between T4a and T4b disease. For that reason, MRI is recommended for all sinonasal carcinomas if there is a doubt of intracranial spread of the tumor.
(a) Contrast enhanced axial CT image. (b) Coregistered PET-CT image at the level of the maxillary sinus of a recurrent nasopharyngeal squamous cell carcinoma with superior spread and bone erosion. (c), (d) Contrast enhanced sagittal CT and coregistered PET-CT of the recurrent tumor showing the recurrent tumor (outlined in purple color) and destruction of cortical bone (appears as black area in the skull anterior part). (e), (f), (g) Sagittal, coronal and axial PET images showing a high uptake of 18 F-FDG in the forehead area with close proximity of the tumor to brain tissues
(a) Axial T2-weighted contrast-enhanced MR image shows moderate enhancement in left maxillary sinus (b) Axial T2-weighted contrast-enhanced MR image shows dense enhancement in the left maxillary sinus (c) Axial T2-weighted contrast-enhanced MR image clearly identifies dense enhancement at the level of the frontal sinus crossing the midline. (d) STIR MRI image showing intracranial extension of the tumour, (e) STIR MRI image showing the recurrent tumor
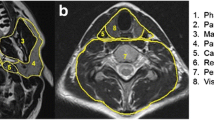
Cross-sectional imaging is critically essential for accurate staging of nasopharyngeal carcinoma. It is important to understand the anatomy of this region to be able to localize the neoplasm in fascial spaces of head and neck like parapharyngeal (PPS), masticator (MS), and retropharyngeal (RPS) spaces. When lesions are limited to the PPS, they are T2 lesions, but lesions that involve the masticator space are T4 lesions. For advanced staging, early cortical erosion (outer layer of compact bone) is better detected on CT compared to MR 2. However, MR is superior to CT for evaluation of bone marrow involvement. A noncontrast axial T1-weighted (T1 W) image is the most reliable sequence to determine if there is marrow involvement, looking for replacement of high-signal marrow by intermediate signal tumor in the untreated patient. MR is clearly superior to CT for detecting perineural extension (extension to nerve sheath). As a result, all patients with nasopharyngeal carcinoma should undergo thin-section contrast-enhanced MR of the skull base and cavernous sinus.
19.6.2 Laryngeal Carcinoma
Laryngoscopy plays a great role in diagnosis of laryngeal carcinomas and should be performed with clinical examination. It can detect any mucosal abnormalities. However, when these tumors spread submucosally which takes place with a high tendency, this extension into the deeply located tissue planes is frequently difficult to evaluate by clinical examination alone. In that condition MRI and CT play a role revealing the spread away from the mucosal lining. The site of the tumour is considered the first clinical criteria used for giving a tumor a particular T-classification. Involvement of different laryngeal anatomical subsites and limited vocal cord mobility in the larynx are important criteria of staging. About 65–70% of laryngeal cancers originate at the glottic level (Fig. 19.11a–d), and about 30% at the supraglottic level. Laryngeal cancer originating from the subglottic region is rare. Classification of laryngeal cancer based only on clinical findings alone is insufficient when compared with pathologic classification. Diagnostic accuracy is markedly improved when the results of CT or MRI are added to the clinical findings [41]. Findings from imaging studies frequently result in an upstaging of the disease. In order to evaluate the accuracy of the CT and MR imaging, many studies compared the findings of imaging with the whole organ sectioning after total or partial laryngectomy, which confirmed that both techniques are accurate methods to visualize laryngeal pathology [41]. Erosion or lysis has been found to be a specific criterion for neoplastic invasion in all cartilages. The positive diagnosis of neoplastic invasion of the thyroid cartilage should be made with extreme caution on MRI [42].
(a) Sagittal contrast enhanced CT image of a patient with supraglottic squamous cell carcinoma (arrow). (b) Axial contrast enhanced CT Image showing the tumor and metastatic lymph nodes on both sides of the neck (outlined in red). (c) Sagittal coregistered PET-CT image showing the tumor and its high uptake of 18 F-FDG (arrow). (d) Axial coregistered PET-CT image clearly depicting the primary tumor (high uptake of 18 F-FDG) and the metastatic lymph nodes (moderate uptake of 18 F-FDG) which are outlined in red color
19.6.3 Supraglottic and Subglottic Carcinomas
The site of involvement is the main criterion for Primary site staging in clinical diagnosis (Fig. 19.11a–d). Involvement of various subsites of the supraglottic larynx and vocal cord mobility should be carefully assessed. Imaging can aid to a great extent to identify occult submucosal transglottic extension. Imaging criteria that define T3 lesions are extensions into the pre-epiglottic space (paralaryngeal fat) or erosion of the inner cortex of the thyroid cartilage [6].
Tumors that erode through the outer cortex of the thyroid cartilage are defined as T4a tumors. Stage T4 (a&b) tumors are difficult to identify based on clinical examination alone because most of the criteria cannot be assessed by endoscopy and palpation. Tumor limited to one subsite of supraglottis with normal vocal cord mobility are classified as T1, Tumor invading the mucosa of more than one adjacent subsite of supraglottis, glottis or region outside of supraglottis, without fixation of the larynx are T2. Vocal cord fixation or invasion of postcricoid area, preepiglottic and/or paraglottic space, and/or minor thyroid cartilage erosion is classified as T3. T4 tumors are: extralaryngeal tumor spread T4a: tumor invading through thyroid cartilage, or tissues beyond the larynx (e.g. trachea, soft tissues of the neck, strap muscles, thyroid gland, and esophagus) andT4b: tumor invading prevertebral space, mediastinum, or encasing carotid artery.
19.6.4 Glottic Carcinoma
Clinical diagnosis can identify T1 and T2 tumors. To confirm the clinical diagnosis, cross-sectional imaging may be used to prove that the clinical diagnosis of early stage lesions is correct. Also, cases with submucosal extension is identified using the cross sectional Imaging. Imaging may also identify glottic carcinomas that have occult transglottic or subglottic spread. Tumor erosion limited to the inner cortex of the thyroid cartilage indicates a T3 lesion, whereas carcinomas which erode through the outer cortex of the thyroid cartilage describe a T4a tumor. To make such an accurate imaging diagnosis, High-resolution Computed Tomography (Fig. 19.12a–g) is used where the slice thickness does not exceeding 2.5 mm. Both MR and CT may be used to detect cartilage invasion. However, there will be cases that MR may detect cartilage invasion not seen on CT and vice versa. CT is preferred over MR due a shorter scan time and lower costs. Staging of glottic carcinoma is as following: T1 Tumor limited to vocal cord(s) with normal mobility (may involve anterior or posterior commissure), T1a: limited to one vocal cord, T1b: involving both vocal cords. T2 Extension into supra and/or subglottis, and/or with impaired vocal cord mobility. T3 Vocal cord fixation and/or invasion of paraglottic space, and/or minor thyroid cartilage erosion. T4 Extralaryngeal tumor spread T4a: tumor invading through thyroid cartilage or tissues beyond the larynx (e.g. trachea, soft tissues of the neck, strap muscles, thyroid gland, and esophagus) T4b: tumor invading prevertebral space, mediastinum, or encasing carotid artery [2].
(a), (b), (c) Axial, coronal, sagittal PET images showing a high uptake of 18 F-FDG by a mass in right side of the neck and the primary laryngeal tumor. (d), (e), (f) Coregistered PET-CT images clearly identifying in axial, coronal and sagittal planes the primary tumor and the metastatic lymph nodes (outlined by green color)
19.7 Assessment of Metastatic Spread of Head and Neck Cancers
Accurate assessment of tumor spread affect the staging, prognosis, and treatment options of the disease. It determines whether conservative surgery and/or radiation therapy can be performed or a more radical technique is necessary. It guides the physician and surgeon to choose the best treatment choice for the patient starting with radiotherapy, radiochemotherapy and/or surgery. The assessment of the extent of the lesion can also identify other factors that may prevent surgical resection. These factors include encasement of the carotid artery (invasion of the tumour to the carotid artery), fixation to the base of the skull, intracranial extension. Also, involvement of the prevertebral fascia or direct invasion of the prevertebral space eliminates the option of tumor resection and consequently predicts a poor prognosis. Therefore, in patients who are surgical candidates, it would be practically useful if preoperative imaging could reliably assess the absence of prevertebral compartment involvement. As a result, this would reduce the need for intraoperative assessment in these patients [43].
The improved soft-tissue resolution and multiplanar capabilities of MRI make it a more accepted diagnostic tool for detection of tumor spread into the deep spaces of the head and neck. In cases with large nasopharyngeal, large pharyngeal and laryngeal cancers, surgery is not a recommended option because it would be difficult to obtain tumor-free margins. For example, surgical resection of the prevertebral muscle or debulking of the tumor in cases of prevertebral space involvement is coupled with poor outcomes on both clinical and functional levels. Therefore, patients with prevertebral involvement can be treated with other treatment choices as radiotherapy and complementary chemotherapy [43, 44].
Enlarged lymph nodes are usually due to either inflammation or hyperplasia. In the assessment of cervical lymph nodes, imaging plays a major role. It is used mainly for (N staging). Also, imaging plays an increasing role in evaluating the degree of extension and spread of the disease. Most metastases originate from malignant neoplasms of the mucous membranes in head and neck, skin, thyroid and salivary glands follow certain pathway in spread. Metastatic adenopathies can be identified even when still in a subclinical stage or at places not accessible for clinical examination, such as the retropharyngeal or paratracheal lymph nodes. Imaging is needed in submucosal lesions, covered by an intact mucosa.
Assessment of the nodal status is an essential procedure in patients of head and neck cancer, not only for treatment planning but also for prediction of treatment outcomes. Malignancy involved lymph nodes from head and neck cancers usually follow a certain pattern of spread with respect to the location of the primary tumour. Consequently, that assessment of the distribution of metastatic nodes in patients with unidentified primary can indirectly help, revealing the site of the primary tumor [19, 45, 46].
Additionally, metastatic nodes in an unpredicted site may point to the fact that the primary tumor is biologically more aggressive [47, 48].
Together with metastases, lymphoma is also a common malignant disease and head and neck involvement is very common. Clinically, lymphoma of the cervical lymph nodes is difficult to differentiate from other causes of lymphadenopathy including metastatic nodes. Metastatic cervical lymph nodes from head and neck primaries are site specific [49].
The common nodal metastaic sites for head and neck primaries are:
-
Tumours of pharynx, larynx, oesophagous, and papillary carcinoma of thyroid metastasize along internal jugular chain.
-
Tumours in the oral cavity metastasize to the submandibular and upper cervical lymph nodes, although carcinoma of the tongue may give rise to skip metastases to the lower neck.
-
Infraclavicular primaries from breast and lung metastasize to supraclavicular fossa and posterior triangle nodes.
-
Nasopharyngeal carcinomas commonly spread to upper cervical nodes and posterior triangle nodes [50, 51].
19.7.1 Lymphadenopathy of the Neck
The causes of enlarged cervical lymph nodes are usually due to one of the following reasons:
19.7.1.1 Reactive Inflammatory Enlargement
The reactively enlarged lymph nodes are most often due to bacterial or viral infections (Fig. 19.13a–c) When a patient presents with enlarged lymph nodes, differential diagnosis should be done to determine the cause behind the adenopathy. History, clinical examination, and microbiological tests can confirm the differentiation that the adenopathy is due to exposure to an infection and not as a result of metastases of malignancy originating in the region of head and neck. Cat scratch disease (mycobacterial infection), suppurative bacterial lymphadenitis, Castleman’s disease, tuberculosis, mononucleosis, herpes, cytomegalovirus infection, rubella, or seldom HIV should be included in the differential diagnosis [6].
(a) sonogram showing the normal oval shaped elongated LN (normal appearance) (arrow) in the submandibular region. (b) Sonogram showing enlarged oval shaped lymph nodes (LN) (inflammatory) in the submandibular region. (c) Sonogram showing enlarged round shaped Lymph nodes (arrow heads) with internal enhancement) suspecting inflammatory reaction or neoplastic change
In suppurative bacterial lymphadenitis Ultrasonography can be used to determine inflammatory changes [52]. Ultrasound examination is helpful in diagnosis of enlarged lymph nodes [19]. Viral infections usually cause bilateral diffuse lymphadenopathy without necrosis of the central part. Sarcoidosis and toxoplasmosis, rarely cause diffuse, multiple nodal enlargement. In these cases, the salivary glands can be swollen as well as mediastinal lymph node enlargement. Carotid body paragangliomas can mimic lymphadenopathy. Imaging is helpful in these cases by showing the vascular nature and exact location of the lesion; however, Median (thyroglossal) or lateral (brachial) cervical cysts have a typical low-density center and sometimes rim enhancement appearance on enhanced CT. T2-weighted MR imaging shows the typical cystic appearance. However, squamous cell metastases rarely appear as cystic lesions (Fig. 19.14a–c). The exact localization and extent of a lesion is also critical when surgical treatment is considered in order to know the extension and the relation of vital structures to the neoplasm such as the carotid artery, the prevertebral fascia, and base of the skull [6].
(a) Axial PET showing high FDG uptake of cervical lymph nodes on both right and left sides. (b) Coregistered PET-CT showing the primary tumor and the metastatic spread to cervical lymph nodes (outlined in red color). (c) Coregistered coronal PET-CT showing the primary tumor and metastaic lymph nodes
19.7.1.2 Metastatic Lymphadenopathy
In 1932, Rouvière came up with a classification of the regional lymph nodes of the neck bases on the anatomical relation. Recently, the American Academy of Otolaryngology developed a new classification that most clinicians are using now based on both clinical and radiographic examination. One of the major reasons for using the new classification is that almost all of patients with head and neck malignancies undergo cross-sectional imaging before treatment.
According to this classification neck is divided into levels:
-
1.
Level 1A: it includes all submental nodes that are between the medial margins of the anterior bellies of the digastric muscles below the mylohyoid muscle.
Level 1B: it includes the submandibular nodes. These are above the hyoid bone, below the mylohyoid muscle, in front of the posterior belly of the digastrics muscles and around the submandibular glands.
-
2.
Level 2: it includes the upper internal jugular nodes. This level extends from the skull base to the level of the bottom of the body of the hyoid bone. Lymph nodes in this level are posterior to the back of the submandibular gland and anterior to the back of the sternocleidomastoid muscle. Level 2 nodes can be subclassified into levels 2A and 2B. Level 2A nodes are situated around the internal jugular vein; level 2B nodes are posterior to the internal jugular vein, separated from the vein by a fat plane. Nodes medial to the internal carotid artery are called retropharyngeal lymph nodes.
-
3.
Level 3: it includes the mid-jugular nodes. They extend from the level of the bottom of the hyoid bone to the level of the bottom of the cricoid cartilage. They lie anterior to the back of the sternocleidomastoid muscle. They are located lateral to the carotid arteries.
-
4.
Level 4: it includes the low-jugular nodes. They extend from the level of the bottom of the cricoid bone to the level of the clavicle. They lie anterior to a line connecting the back of the sternocleidomastoid muscle and the posterolateral margin of the anterior scalene muscle. They are also lateral to the carotid arteries.
-
5.
Level 5: it includes nodes in the posterior triangle. They are posterior to the back of the sternocleidomastoid muscle from the skull base to the clavicle. Level 5 is also divided into level 5A and 5B. Level 5A extends inferiorly toward the bottom of the cricoids bone whereas 5B extends from the bottom of the cricoids cartilage to the clavicle. They are also anterior to the anterior edge of the trapezius muscle.
-
6.
Level 6: it includes the visceral nodes which are inferior to the lower body of the hyoid bone, superior to the top of the manubrium sterni muscle, and between the left and right common carotid arteries or the internal carotid arteries.
-
7.
Level 7: it includes the superior mediastinal nodes. They are between the carotid arteries below the level of the top of the manubrium and above the level of the innominate vein [51].
For consistency with the prior classifications, the following nodal groups, as well as the other superficial nodes, are referred to by their anatomical names as retropharyngeal, parotid, facial, occipital, and postauricular. Most tumors originating from the mucosal lining of the upper aerodigestive tract have a well-defined and more predictable pattern of metastasis to the neck.
The classification of neck levels of lymph nodes of the neck depicts the map of surgical removal of the involved nodes in neck dissection according to the N staging. This clinical classification leads to improved management of patients which could be followed by radiation therapy depending on histological findings to confirm the presence of extra nodal spread or presence of multiple metastases. This line of treatment (surgery and radiation therapy) still has a considerable morbidity and mortality. Therefore, imaging assessment of the lymph node status is critically significant for the choice of treatment. So, making the decision for such a radical treatment should be fully supported by the obtained findings of a highly accurate radiographic modality. For example, ultrasonography (USG) that has the advantage of Ultrasound guided fine needle aspiration cytology (USgFNAC) which is considered highly accurate and has the best diagnostic value for the detection of cervical lymph node metastases. Ultrasound alone is also associated with high diagnostic odds ratio (DOR). The DOR is a single indicator of test performance. It varies between 0 and infinity [53]. Whereas computed tomography (CT) and magnetic resonance imaging (MRI) perform less well. The nature and internal structure of small lymph nodes (≤5 mm) may not be readily assessed by them. Also, MRI may not identify intranodal calcification which is a feature used in prediction of metastatic nodes from papillary carcinoma of the thyroid gland [54]. The main advantages of CT and MRI are the lower inter-observer variation (not highly dependent on the operator), and less time consuming compared to USgFNAC and USG. Furthermore, CT and MRI are relatively standardized techniques that can be interpreted by general radiologists, whereas USG and USgFNAC should be performed by a well experienced radiologist in Ultrasonography. Detection of occult lymph nodes by imaging can guide the treatment choices according to its findings in cancer patients. It has been proposed that a minimally invasive approach concerning management of the clinically negative neck could be allowed, if the risk of occult lymph node metastases is less than 20% [6].
Cross-sectional imaging has been shown to be superior to clinical examination for staging of cervical lymph nodes. The diagnostic accuracy of cross-sectional imaging is based on cross-sectional diameter and presence of internal abnormalities. The reader is referred to the prospective study of Curtin et al., which reports the diagnostic accuracy of CT and MR based on these criteria. The advent of multidetector imaging now permits rapid reconstruction on imaging studies in the sagittal and coronal planes. Curtin’s classic work only evaluated axial dimensions. There have been no large-scale randomized prospective trials that have been performed to determine if sagittal or coronal measurements will improve the diagnostic accuracy of CT for detecting metastatic lymph nodes. Extracapsular penetration can be detected on cross-sectional imaging and is defined by reticulation of the fat adjacent to the outer margin of a lymph node. These findings are not pathognomonic, as similar findings can be seen in inflamed lymph nodes due to adenitis. However, the presence of such findings in a patient with head and neck cancer, in the absence of an infection, should be considered highly suspicious for extracapsular penetration.
19.7.1.3 PET-CT and Lymph Nodes
With the development of new technologies, additional criteria are added that improved the diagnostic performance of existing techniques. Positron emission tomography-computed tomography (PET-CT) imaging is a valuable addition to the diagnostic armamentarium in the diagnosis of metastases to lymph nodes (Fig. 19.15a, b) [53].
(a), (b) Coregistered PET-CT images of a patient with multiple neck lymph node metastases at Level II under the sternocleidomastoid muscle. PET revealed high FDG uptake in the right side which was enlarged on CT images (outlined with red color) and moderate FDG uptake in the lymph node in the left side (outlined in purple)
One of the potential applications of PET-CT is using it in advanced stage head and neck squamous cell carcinoma to evaluate for occult distant metastases to the lungs or bones. The presence of pulmonary metastases upstages a patient from M0 to M1 and alters treatment plan. However if a solitary nodule is identified, it is often unclear if this is a separate primary, metastasis, or a granuloma. PET may help in this evaluation because an FDG-positive nodule will likely require biopsy, whereas an FDG-negative nodule (>8 mm) likely indicates a granuloma and a biopsy may be avoided. Knowledge of these patterns of metastases is important for radiologists and surgeons. The most frequent source for metastases to lymph nodes in the head and neck region is from squamous cell carcinomas of the mucous membranes of this region as it comprises more than 90% all head and neck tumors. The presence of one isolated lymph node metastases (stage N1) lowers the prognosis with 50%, where as multiple metastases worsen the prognosis even more. Therefore, prediction of prognosis in head and neck tumors is usually based on the lymph node staging [55, 56].
19.8 Imaging Accuracy of Diagnostic Modalities
Accurate staging of head and neck cancers represents a great challenge to radiologists because of the anatomical and functional complexity of this region of the human body. The introduction of CT and MRI has renovated head and neck radiology. Modern radiological modalities can provide a reliable image of the head and neck structures with extraordinary level of details. These techniques can provide a comprehensive evaluation of the location and extent of neoplastic lesions. The introduction of new developments like diffusion-weighted MRI, PET-CT, and PET-MRI has intensified the accuracy level of imaging in addition to monitoring tumor response to treatment [55]. The main tasks of imaging in management of patients with head and neck cancers are:
-
1.
Identification of the neoplasm and its extent in the initial or pre-treatment diagnosis in order to outline the possibility of complete surgical resection.
-
2.
Assessment of lymph nodes for metastatic spread.
-
3.
Monitoring tumour response to the appropriate therapy.
-
4.
Assessment of disease recurrence after treatment.
Positron Emission Tomography CT (PET-CT) is now competing with the CT and MRI and gaining more acceptance in imaging of head and neck neoplasms. PET-CT major advantage is the ability to provide information about both the anatomy and metabolism of examined area. It can identify metastatic cervical lymph nodes with a negative predictive value up to 90%. It can also detect the primary tumor in patients with metastatic squamous cell carcinoma of the head and neck with unknown primary lesion in 30–50% of cases. Further advances in the technology of PET-CT can promote its role to provide optimal diagnostic quality [55].
PET-CT provides high quality images which can be used to detect pathological lesions and differentiate between malignant and physiological uptake. There are many reports on the clinical usefulness of PET-CT system for head and neck cancer with promising diagnostic accuracy; on the other hand, there are some patients who do not tolerate iodine-based IV contrast media used in PET-CT [57, 58]. Nakamoto et al, 2009 tried to use MRI instead of CT because of the higher tissue contrast by MRI in head and neck cancers than with CT and because it could be used in patients allergic to contrast media used in PET-CT. They found that the fusion of MR and PET images resulted in some clinical advantages for head and neck cancers over PET/CT. However, the clinical application of MR and PET fusion imaging of the whole body is still limited [59].
Ultrasonography is also a strong player in the diagnosis of metastatic cervical lymph nodes. It has the highest accuracy among all modalities especially with the evolution of endoscopic Ultrasonography (EUS) which overcame the drawback of the inability to pass through dense structures. Ultrasonography guided needle biopsy enables identification of the nature of pathological processes. Ultrasonography can diagnose not only cervical metastatic lymph nodes but can also be used to evaluate treatment-induced changes in lymph node metastases after chemoradiotherapy. Ultrasonographic assessment of the presence or absence of metastases is directly associated with the decision of removal of the involved lymph nodes by neck dissection. Ultrasonography allows the evaluation of lymph nodes that are 10 mm diameter or more, which can be diagnosed as cervical lymph node metastasis-positive by computed tomography (CT) or magnetic resonance imaging (MRI). It also can evaluate lymph nodes of less than 10 mm diameter, based on sufficient image information. All lymph node metastases less than 10 mm in diameter are considered as “potential lymph node metastases” and radical dissection is recommended. Although radical neck dissection can decrease the rate of secondary lymph node metastases or relapse, it may induce various postoperative pain and disorders due to cervical dysfunction. Using combination therapy chemotherapy/ radiotherapy even in metastatic lymph nodes may lead to organ preservation. The number of patients in whom satisfactory efficacy has been obtained even with cervical lymph node metastases by combining chemotherapy with radiotherapy is continuously rising. Ultrasonographic evaluation of therapeutic effects on cervical lymph node metastases is significantly necessary to choose the patients who do not need additional neck therapy, to avoid shoulder dysfunction or swallowing disturbance caused by excess neck therapy. So, it is important to perform pretreatment ultrasonographic assessment of lymph nodes less than 10 mm in diameter which cannot be assessed by CT or MRI in diagnostic procedures for cervical lymph node metastases of head and neck cancer. This can lead to more conservative surgeries or even prevention of surgical treatment [60].
Tumor resectability is the major challenge that faces the surgeon. The translation of diagnostic images to the operative field is the key to obtain a successful treatment. The high accuracy of imaging modality helps the surgeon to adequately discriminate between tumor and normal tissue. This has a role in determining the healthy margins. However, the only way to do this during surgery is by visual appearance and palpation. Introduction of real-time imaging technologies into the operating room has the potential of cross the gap between radiology and surgery, resulting in intraoperative image-guided surgery. Optical imaging is currently considered the optimal technique for intraoperative image-guided surgery. In optical imaging, the properties of light are exploited to image anatomic or chemical characteristics of tissue. Imaging of optical contrast can be performed either using the properties intrinsic to the tissue, or, analogous to many radio-labeled agents, using antibodies or ligands conjugated to an optically active reporter to target a recognized disease biomarker [59, 61]. Accurate assessment of tumor spread leads to accurate staging; therefore the treatment outcomes and prognosis can be predicted more accurately. It determines whether conservative surgery and/or radiotherapy can be performed or whether more radical surgical intervention is necessary. In addition to guiding the surgeon, imaging has been used to recognize other reasons that may interfere with surgery and redirect the treatment plan to another choice. These reasons include encasement (involvement) of the carotid artery, fixation of the tumor to the base of the skull, intracranial (inside the skull) tumour extension, extension to the nasopharynx, or invasion of the brachial plexus (network of nerve fibers, running from the spine). Prevertebral space involvement defined as fixation to or direct invasion of the prevertebral fascia eliminates the option of surgical resection and predict very poor prognosis. The 2002 American Joint Commission on Cancer (AJCC) revised the T-stage classification of head and neck cancers recommending that advanced (T4) stage cancers to be subdivided into T4a and T4b categories. T4b tumors were categorized as surgically unresectable; T4a lesions are still classified resectable although they may require extensive surgery. The criteria of T4 according to the AJCC for most aerodigestive system locations are: (1) Vascular encasement and invasion, (2) Prevertebral space invasion and (3) Invasion of mediastinal structures [62].
MRI can be particularly helpful in assessing carotid encasement. If the vessel shows greater than 270° of circumferential encasement, it usually cannot be resected from the artery at surgery. Tumors that surround the artery by less than 180° can be readily resected; most tumors showing 180–270° encasement can also be resected [1, 62, 63].
Based on the previous discussion of different diagnostic modalities, each case is unique and needs a specific study to address it carefully. Once a lesion is identified, there are two questions needed to be answered: (1) where is it located? And (2) what is its nature? To answer these questions other factors should be included which are epidemiologies, clinical presentation, and pathological findings. The imaging findings consist primarily of CT and MRI because these are the most commonly used modalities for evaluating the extracranial head and neck lesions. So, in summary, each modality has its advantages and disadvantages. No modality can provide everything needed in every study; however some modalities can be more superior to another and provide more information. Also, combinations between these imaging modalities can provide a complementary evaluation by covering the drawbacks in each modality.
19.9 Role of Imaging in Treatment Planning of Head and Neck Cancer
Recent and continuing research is empowering the impact of imaging in health care of patients with cancer. Consequently, the radiologist is now considered to be an important member of the multidisciplinary team managing head and neck cancer patients.
Imaging of tumours and surrounding normal tissues is used for several purposes related to treatment, this includes:
-
Cancer screening and surveillance.
-
Initial or pre-treatment radiographic diagnosis which comprise detection, staging, location, relations, metastases and resectability.
-
Planning for therapy to determine the treatment of choice with consideration to the age or the patient and his general health.
-
Evaluation of treatment outcomes during the treatment period and that includes observation of changes in tumour size and shape in response to treatment and
-
Finally post-treatment follow up of the patient to examine the signs of the cure of the disease and /or recurrence of the tumour.
Although head and neck cancer can be successfully managed with a combination of surgical and chemoradiotherapeutic interventions, the disease should be well characterized both radiographically and histopathologically before carrying out surgical or medical management of the patient. Radiographic imaging is a fundamental part of the initial staging process for head and neck cancer and plays an important role in identifying the locoregional extent of the tumor, localization of an unknown primary site, and the presence of distant metastases which in turn guide the surgical planning.
Several imaging modalities are recommended for the pretreatment evaluation of head and neck tumors. The most commonly used are magnetic resonance imaging (MRI) and computed tomography (CT). Computed tomography is a well-established diagnostic tool in the initial staging and surgical planning for head and neck cancer since it provides structural information at a high spatial resolution. However, it does not always provide additional needed information. Suspicion for nodal disease is mainly based on size, which can be due to inflammatory reaction or due to metastases. Ultrasonography and Positron emission tomography (PET) using the radiolabeled glucose analogue fluorodeoxyglucose F 18 can be used in both the initial evaluation and in the detection of recurrent lesions after treatment. Positron emission tomography provides metabolic information of the tumor by showing the metabolically active tissues. PET can be used for initial staging, for detecting regional or distant nodal disease (metastases), for localizing unknown primary tumors, and for identifying recurrent disease. With all these advantages, it lacks of perfect anatomical resolution which is necessary for surgical and radio/chemo therapeutic planning. This limits its usefulness as a single diagnostic modality. So, combinations with other modalities like CT and MRI are now applied to improve the technology of PET imaging. A newer imaging modality, PET and CT fusion (PET-CT), allows for simultaneous image acquisition and co-registration of metabolic and anatomical data, expanding the benefits of PET or CT alone. This relatively new diagnostic imaging modality, PET-CT plays a valuable role in the initial staging and in the therapeutic management planning for untreated head and neck cancer patients in both early and advanced stages of the disease. Patients with early-stage disease can benefit from the detection of regional metastases, and those with advanced-stage disease can benefit from the detection of distant metastases. They can also benefit from a well defined extension of regional spread of the tumor and its relationship to the surrounding normal tissues [64, 65].
Treatment strategies of squamous cell carcinoma of the head and neck is planned with respect to many considerations that include: site, stage of the disease, age and general health of the patient. In most cases of early stages (stage I, II) the modality of choice is surgery or radiotherapy as initial treatment. Before 1980, the initial treatment of patients with locally advanced stage III or IV was also surgery and/or radiation therapy, a choice that also depended on the site of the disease, the resectability of the cancers. The obtained poor results in these advanced stages with the “traditional” therapy led to introduction of systemic chemotherapy in the mid 1970s as part of combined modality treatment. Later, chemotherapy was used in patients with earlier disease stages and with resectable disease for organ preservation and better cure rates. Advanced squamous cell cancers of the head and neck are usually associated with high rates of morbidity and mortality with predicted prognosis of less than 30% 5 year survival rates. The introduction of new active chemotherapeutic agents and combinations with radiotherapy, targeted treatments, and better sequencing of treatment options, it is expected to promote the improvements in treatment results. Organ preservation is more commonly achieved. Newer targeted therapies will also add to the progress that has already been achieved in the multimodality management of patients with head and neck cancers. New standards of care have been defined for patients with nasopharyngeal cancer and for those with advanced unresectable disease [59].
In head and neck cancer patients, it is essential to monitor the response of the tumor to radiotherapy, and to determine whether the chosen treatment regimen is effective so that an ineffective Treatment approach or drug regimen can be changed. After irradiation therapy, clinical examination of the head and neck is difficult and residual or recurrent tumor cannot be detected. Post-radiotherapy, residual tumor and post-radiation changes may show contrast enhancement. Post treatment MR imaging is inaccurate in the differentiation of residual tumor from post-radiation changes, as fibrous tissues may be enhanced, simulating a tumor, and residual tumors may show insignificant contrast enhancement and may be mistaken for post-treatment fibrosis. Diffusion-weighted MR imaging has been applied to differentiate residual or recurrent tumors from post-treatment changes in head and soft-tissue masses. Functional imaging like Diffusion-weighted MR and PET-CT could identify nonresponding tumours early, which allows for a switch in therapy [66, 67].
Abbreviations
- PET-CT:
-
Positron emission tomography – computed tomography
- MRI:
-
Magnetic resonance imaging
- USG:
-
Ultrasonography
- PACS:
-
Picture archiving and communication system
- FNAC:
-
Fine needle aspiration cytology
- LN:
-
Lymph node
- DW:
-
Diffusion weighted
- MIP:
-
Maximum intensity projection
- HNSCCA:
-
Head and neck squamous cell carcinoma
References
Di Martino E, Nowak B, Hassan HA, Hausmann R, Adam G, Buell U, Westhofen M (2000) Diagnosis and staging of head and neck cancer: a comparison of modern imaging modalities (positron emission tomography, computed tomography, color-coded duplex sonography) with panendoscopic and histopathologic findings. Arch Otolaryngol Head Neck Surg 126:1457–1461
Hermans R, De Keyzer F, Vandecaveye V (2006) Imaging techniques. In: Hermans R (ed) Head and neck cancer imaging. Springer, Berlin/Heidelberg/New York
Greene F (2002) American Joint Committee on Cancer (AJCC) cancer staging handbook. In: Greene F, Page D, Fleming I, Fritz A, Balch C, Haller D, Morrow M (eds) TNM classification of malignant tumors, 6th edn. Springer, New York
Mukherji S (2008) Special radiologic imaging considerations in the evaluation of sc cancer of the head and neck. In: Harrison L, Sessions R, Ki Hong W (eds) Head and neck cancer: multidisciplinary approach, 3rd edn. Lipppincott Williams & Wilkins, Philadelphia
Bushberg J, Seibert J, Leidholdt E, Boone J (2001) The essential physics of medical imaging, 2nd edn. Lippincott Williams & Wilkins, Baltimore
William E, Clide A, Smith W (2007) Fundamentals of diagnostic radiology. In: William E, Wilbur L (eds) Radiology 101: the basics and fundamentals of imaging, 3rd edn. Lipppincott Williams & Wilkins, Philadelphia
Seibert JA (2005) Considerations for selecting a digital radiography system. J Am Coll Radiol 2:287–290
Badawi R, Kroger L, Bushberg J (2007) Essential science of nuclear medicine. In: Brant W, Helmes C (eds) Fundamentals of diagnostic radiology, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Major N (2005) Practical approach to radiology. Elsevier, Philadelphia
Suk N, Songra A, Nayeem A, Lister B (2001) Ultrasound features of osteosarcoma of the mandible—a first report. Oral Med Oral Pathol Oral Radiol Endod 92:582–586
Van den Brekel M, Castelijns J, Stel H et al (1991) Occult metastatic neck disease: detection with US and US-guided fine needle aspiration cytology. Radiology 178:457–461
Van Overhagen H, Lameris JS, Berger MY et al (1991) Supraclavicular lymph node metastases in carcinoma of the esophagus and gastroesophageal junction: assessment with CT, US, and US-guided fine- needle aspiration biopsy. Radiology 179(1):155–158
Shung K (2005) Diagnostic ultrasound: imaging and blood flow measurements. CRC Press, Boca Raton
Astl J, Jabloniscky P, Lastuvka P, Taud M, Dubova J, Betka J (2003) Ultrasonography (b scan) in the head and neck region. Int Congr Ser 1240:1423–1427
Glod L, Nazarian L, Johar A, Rao V (2003) Characterization of maxillofacial soft tissue vascular anomalies by Ultrasound and color Doppler imaging: an adjuvant to computed tomography and magnetic resonance imaging. J Oral Maxillofac Surg 61:19–31
Goldberg B, Kimmelman B (1988) Medical diagnostic ultrasound: a retrospective on its 40th anniversary. Eastman Kodak, Rochester
Hagen-Ansert S (2006) Textbook of diagnostic ultrasonography, vol 1, 6th edn. Mosby Elsevier, St. Louis
Catalano O, Nunziata A, Siani A (2009) Fundamentals in oncologic ultrasound: sonographic imaging and intervention in the cancer patient. Springer, New York
Ahuja A, Ying M, Ho S, Antonio G, Lee Y, King A, Wong K (2008) Ultrasound of malignant cervical lymph nodes. Cancer Imaging 8:48–56
Ahuja A, Ying M, Phil M, King A, Yuen HY (2001) Lymph node hilus-gray scale and power Doppler sonography of cervical nodes. J Ultrasound Med 20:987–9927
Shami V, Kahaleh M (2010) Clinical gastroenterology. Endoscopic ultrasound. Springer, New York
Jun BC, Song SW, Cho JE et al (2005) Three-dimensional reconstruction based on images from spiral high-resolution computed tomography of the temporal bone: anatomy and clinical application. J Laryngol Otol 119(9):693–698
Keberle M, Tschammler A, Hahn D (2002) Single-bolus technique for spiral CT of laryngopharyngeal squamous cell carcinoma: comparison of different contrast material volumes. Flow Rates Start Delays Radiol 224:171–176
Shah G, Wesolowski J, Ansari S, Mukherji S (2008) New directions in head and neck imaging. J Surg Oncol 97:644–648
Hashemi R, Bradley W, Lisanto C (2004) MRI: the basics. Williams & Wilkins, Baltimore
Le Bihan D, Breton E, Lallemand D et al (1988) Separation of diffusion and perfusion in intravoxel incoherent motion. MRI imaging. Radiology 168:497–505
Farina D, Borghesi A (2005) Techniques of radiological examination. In: Maroldi R, Nicolai P (eds) Imaging in treatment planning for sinonasal diseases. Springer, Secaucus
Koh DM, Collins DJ (2007) Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol 188:1622–1635
Hillner B, Siegel B, Liu D, Shields A, Gareen I, Hanna L, Stine S, Coleman R (2008) Impact of positron emission tomography/computed tomography and positron emission tomography (PET) alone on expected management of patients with cancer: initial results from the National Oncologic PET Registry. J Clin Oncol 26(13):2155–2161
Wong W, Chevretton E, McGruck M, Hussain K et al (1997) A prospective study of PET-FDG imaging for the assessment of head and neck squamous cell carcinoma. Clin Otolaryngol 22:209–214
Paul S, Stoeckli S, Von Schulthess G, Goerres G (2007) FDG PET and PET/CT for the detection of the primary tumour in patients with cervical non-squamous cell carcinoma metastasis of an unknown primary. Eur Arch Otorhinolaryngol 264:189–195
Liao C et al (2009) Preoperative [18 F] Flourodeoxyglucose positron emission tomography standardized uptake value of neck lymph nodes predicts neck cancer control and survival rates in patients with oral cavity squamous cell carcinoma and pathologically positive lymph nodes. Int J Radiat Oncol Biol Phys 74(4):1054–1061
Nakamoto Y, Tamai K, Saga T, Higashi T et al (2009) Clinical value of image fusion from MR and PET in patients with head and neck cancer. Mol Imaging Biol 11:46–53
Matsumoto K, Kitamura K, Mizuta T et al (2006) Performance characteristics of a new 3-dimensional continuous-emission and spiral-transmission high-sensitivity and high-resolution PET camera evaluated with the NEMA NU 2-2001 standard. J Nucl Med 47:83–90
Brambilla M, Secco C, Dominietto M et al (2005) Performance characteristics obtained for a new 3-dimensional lutetium oxyorthosilicate-based wholebody PET/CT scanner with the national electrical manufacturers association NU 2-2001 standard. J Nucl Med 46:2083–2091
Juweid M, Cheson B (2006) Positron-emission tomography and assessment of cancer therapy. N Engl J Med 354:496–507
Weissleder R (2006) Molecular imaging in cancer. Science 312:1168–1171
Weber W (2006) Positron emission tomography as an imaging biomarker. J Clin Oncol 24(20):3282–3292
Beyer T, Townsend D, Brun T et al (2004) A combined PET/CT scanner for clinical oncology. J Nucl Med 41:1369–1379
Tian M, Zhang H, Higuchi T et al (2001) Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther 69:89–95
Zbaren P, Becker m, Lang H (1996) Pretheraputic staging of laryngeal carcinoma. Clinical findings, computed tomography, and magnetic resonance imaging compared with histopathology. Cancer 77:1263–1273
Zbaren P, Becker M, Lang H (1997) Staging of laryngeal cancer: endoscopy, computed tomography and magnetic resonance versus histopathology. Eur Arch Otolaryngeol 245(Supl 1):5117–5122
Mukherji S, Bradford CR (2006) Is there a role for PET-CT in the initial staging of head & neck squamous cell carcinoma? AJNR Am J Neuroradiol 27:239–245
Bruschini P, Giorgetti A, Bruschini L et al (2003) Positron emission tomography (PET) in the staging of head neck cancer: comparison between PET and CT. Acta Otorhinolaryngol Ital 23(6):446–453
Ishiii J, Amagasa T, Tachibana T, Shinozuka K, Shioda S (1993) US and CT evaluation of Cervical Lymph node metastases from oral cancer. J Cranio-Max-Fac Surg 1991:19–123
Vassallo P, Edel G, Roos N, Nagaib A, Peters P (1993) In- vitro high resolution ultrasonography of benign and malignant lymph nodes. A sonographic-pathologic correlation. Invest Radiol 28(8):698–705
Som P (1992) Detection of metastases in cervical lymph nodes: CT and MRI criteria and differential diagnosis. Am J Roentgenol 158:961–969
Som P (1987) Lymph nodes of the neck. Radiology 165:593–600
Ahuja A, Ying M (2000) Grey scale sonography in assessment of cervical lymphadenopathy: review of sonograophic appearances and features that may help a beginner. Br J Oral Maxillofac Surg 38(5):451–459
Ahuja A, Ying M, Yang WT, Evans R, King W, Metreweli C (1996) The use of sonography in differentiating cervical lymphomatous lymph nodes from cervical metastatic lymph nodes. Clin Radiol 51(3):186–190
Harnesberger H et al (2011) Diagnostic imaging: head and neck, 2nd edn. Amirsys, Altona
Bassiony M, Yang J et al (2009) Exploration of ultrasonography in assessment of fascial space spread of odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 107(6):861–869
De Bondt R, Nelemans P, Hofman P, Casselman J, Kremer B, van Engelshoven J, Beets-Tan R (2007) Detection of lymph node metastases in head and neck cancer: a meta-analysis comparing US, USgFNAC, CT and MR imaging. Eur J Radiol 64:266–272
Som P, Brandwein M, Lidov M, Lawson W, Biller H (1994) The varied presentations of papillary thyroid carcinoma cervical nodal disease: CT and MRI findings. Am J Nueroradiol 15:1123–1128
Schwartz DL, Ford E, Rajendran J et al (2005) FDG-PET/CT imaging for preradiotherapy staging of head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys 61:129–136
Mack M et al (2008) Cervical lymph nodes. Eur J Radiol 66(3):493–500
Nakamoto Y, Tamai K, Saga T, Higashi T, Hara T, Suga T, Koyama T, Togashi K (2009) Clinical value of image fusion from MR and PET in patients with head and neck cancer. Mol Imaging Biol 11:46–53
Furukawa M, Furukawa M (2010) Diagnosis of lymph node metastases of head and neck cancer and evaluation of effects of chemoradiotherapy using ultrasonography. Int J Clin Oncol 15:23–32
Frangioni J (2008) New technologies for human cancer imaging. J Clin Oncol 26:4012–4021
Schmid D, Stoeckli S, Bandhauer F et al (2003) Impact of positron emission tomography on the initial staging and therapy in locoregional advanced squamous cell carcinoma of the head and neck. Laryngoscope 113:888–891
Benchaou M, Lehmann W, Slosman D et al (1996) The role of FDGPET in the preoperative assessment of N-staging in head and neck cancer. Acta Otolaryngol 116:332–335
Hunter K, Parkinson E, Harrison P (2005) Profiling early head and neck cancer. Nat Rev Cancer 5:127–135
Mao L, Hong W, Papadimitrakopoulou V (2004) Focus on head and neck cancer. Cancer Cell 5:311–316
Keereweer S, Sterenborg H, Kerrebijn J, Van Driel P, de Jong R, Löwik C (2011) Image-guided surgery in head and neck cancer: current practice and future directions of optical imaging. Head Neck 34(1):120–126
Abdel Razek A, Soliman N, Elkhamary S et al (2006) Role of diffusion weighted MR imaging in cervical lymphadenopathy. Eur Radiol 16:1468–1477
Razek AA, Megahed AS, Denewer A, Motamed A, Tawfik A, Nada N (2008) Role of diffusion-weighted magnetic resonance imaging in differentiation between the viable and necrotic parts of head and neck tumors. Acta Radiol 49(3):364–370
McCabe K, Rubinstein D (2005) Advances in head and neck imaging. Otolaryngologic Clin N Am 38:307–319
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Bassiony, M., Aydogan, B., Radosevich, J.A. (2013). Diagnostic Imaging Considerations. In: Radosevich, J. (eds) Head & Neck Cancer: Current Perspectives, Advances, and Challenges. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-5827-8_19
Download citation
DOI: https://doi.org/10.1007/978-94-007-5827-8_19
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-5826-1
Online ISBN: 978-94-007-5827-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)