Abstract
Since its first introduction by Hounsfield and Cormack in 1972, computed tomography (CT) has become one of the most important imaging modalities in diagnostic imaging, because of its strong impact on patient outcome. As a result, CT utilization has risen 10% per year during the last 15 years in the USA [1] and 142% between 1998 and 2008 in Switzerland [2]. In 2008, CT was responsible for 68% of the yearly Swiss medical radiation exposure while accounting for only 6% of the ionizing radiation examinations [2]. Current knowledge on the attributable risk of cancer induction by low level medical imaging radiation exposure (<100 submillisiev-ert, mSv) is largely based on longitudinal studies of atomic bomb survivors [3]. These data were recently augmented by two large, retrospective, epidemiologic cohort studies that showed a correlation between CT radiation exposure and a slightly increased cancer risk in children and young adults [4, 5]. However, the disease status of these patients represents a confounding factor in the interpretation of these data.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Iterative Reconstruction
- Tube Current Modulation
- Pulmonary Compute Tomography Angiography
- Lung Cancer Screening
- Increase Radiation Dose
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Since its first introduction by Hounsfield and Cormack in 1972, computed tomography (CT) has become one of the most important imaging modalities in diagnostic imaging, because of its strong impact on patient outcome. As a result, CT utilization has risen 10% per year during the last 15 years in the USA [1] and 142% between 1998 and 2008 in Switzerland [2]. In 2008, CT was responsible for 68% of the yearly Swiss medical radiation exposure while accounting for only 6% of the ionizing radiation examinations [2]. Current knowledge on the attributable risk of cancer induction by low level medical imaging radiation exposure (<100 submillisiev-ert, mSv) is largely based on longitudinal studies of atomic bomb survivors [3]. These data were recently augmented by two large, retrospective, epidemiologic cohort studies that showed a correlation between CT radiation exposure and a slightly increased cancer risk in children and young adults [4, 5]. However, the disease status of these patients represents a confounding factor in the interpretation of these data.
Given the rapid rise in CT frequency and the potential risk of cancer induction, it is the responsibility of the radiologic community (radiologists, technologists, medical physicists, CT manufacturers) to optimize radiation dose. In addition to ensuring CT examination justification, supervising radiologists are responsible for using the lowest diagnostic CT radiation dose, in accordance with the ALARA (as low as reasonable achievable) principle. In chest examinations, the reasons for rigorous dose optimization include highly radiosensitive organs (breast tissue, bone marrow, lung) within the scanned volume and the frequent scanning of radiosensitive young adults (e.g., to query pulmonary embolism).
The radiation dose in a chest CT can be reduced without degradation of the diagnostic accuracy by taking advantage of the large differences in attenuation between air and soft tissue. The intrinsic high subject contrast allows the acceptance of higher image noise. In addition, CT technical advances have facilitated dose reduction while maintaining image quality. This chapter summarizes the currently available methods for dose reduction/optimization in cardiothoracic CT.
Practical Methods for Dose Reduction
Practical methods for dose reduction are independent of the CT scanner and are controlled by the operator.
Limitation of the Enhancement Phases
A first and simple step in dose reduction is the limitation of the number of acquisition phases dependent on the clinical question. An additional pre-contrast phase in a chest CT is indicated only in a few clinical situations; e.g., to assess an intramural aortic hematoma or an aortic stent graft endoleak. Two-phase scanning for these indications may be eliminated by the use of dual-energy CT, which derives a virtual non-contrast image from a contrast-enhanced dual energy acquisition [6]. However, to realize a reduction in the radiation dose, the dual-energy CT protocol needs to be optimized.
Reduction of Scan Length
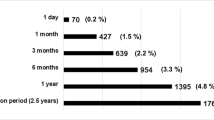
In general, the scanned volume should be adapted to the clinical question. For example, in suspected pulmonary embolism, the radiation dose in CT pulmonary angiography can be reduced by up to 30% by only scanning to the level of the subsegmental pulmonary arteries and excluding the lung apex and base [7] (Fig. 1), which harbor distal vessels that will not impact clinical treatment in most cases. The negative impact of this dose reduction strategy is the potential to miss a clinically significant alternative diagnosis, such as a malignant lung nodule.
Simulation of reduced scan length and estimated organ doses in pulmonary CT angiography to rule out pulmonary embolism, in which the lung apex and base are excluded. A reduction of the effective dose by about one third compared with the original scan volume is estimated by the dose management software (Radimetrics, Bayer, Germany)
Positioning of the Arms
In thoracic CT, the patient’s arms should be raised over his or her head to achieve a dose-efficient thoracic CT scan with acceptable image quality. The increased attenuation by the arms in the x-axis forces the automatic tube current modulation to increase the radiation dose to maintain constant image quality thus increasing the radiation dose to most organs. Furthermore, with the arms next to the thorax, beam-hardening artifacts are increased degrading image quality (Fig. 2). Compared to arm-down positioning, placing the arms above the head increases subjective and objective image quality [8] and leads to a dose reduction of up to 45% in CT of the thorax and abdomen [9]. If a patient is unable to lift one arm, the technician should still position the other arm above the head.
Localizer radiograph and transverse CT slice of the lung base in a patient who underwent two CT examinations, one in which the arms were raised over the head (a) and the other with the arms placed next to the thorax due to immobility (b). The second CT scan resulted in an increase of beam hardening artifacts and reduced image quality in the lung bases
Patient Positioning in the Isocenter of the CT Scanner
The detrimental radiation dose effect of mis-centering patients within the scanner gantry is often not appreciated by technicians and radiologists. The increased radiation dose associated with mis-centering arises from the pre-patient X-ray beam bowtie filters installed in all modern CT scanners. These filters modify beam strength by strongly attenuating the peripheral projections and weakly attenuating central ones. This evens the X-ray fluence at the detector and reduces the radiation dose to less-attenuating peripheral structures. Incorrect centering defeats the purpose of the bowtie filter, leading to an increased radiation dose to peripheral structures and a decreased image quality [10]. Clinical studies have found that up to 95% of patients receiving a thoracic or abdominal CT scan are not centered properly in the vertical plane [10], with an average error of 2.6 cm. Li et al. quantified this effect, thereby demonstrating that a vertical mis-centering of 3 cm results in an increase in the peripheral radiation dose of up to 18%, with a 6% increase in image noise [10]. Thus, technicians should be trained to meticulously center patients such that the bowtie filters are utilized optimally.
Technical Advances for Dose Reduction
In the last 10 years, CT manufacturers have introduced a number of effective tools that reduce the radiation dose while maintaining or improving image quality. The clinical consequence of impaired image quality associated with dose reduction has been demonstrated in experimental studies using computer-simulated low-dose scans [11]. In the experimental design, intra-observer agreement was lower when noisy, low-dose rather than higher dose exams were interpreted [12]. The authors concluded that optimal dose reduction should be achieved without sacrificing image quality. Since CT manufacturers use diverse technical approaches for dose reduction, there are some differences in the technical implementations and their resultant effectiveness.
Automatic Tube Current Modulation
Since radiation dose is linearly related to tube current at constant kVp, a decrease in the tube current results in dose reduction. Although image noise is impacted by dose reduction, there is no impact on the CT numbers (Hounsfield units) of the body tissues scanned. The aim of automatic tube current modulation (ATCM) is to maintain operator-selected image quality throughout the scan while reducing the radiation dose to the patient. State-of-the-art ATCM modulates the tube current in three dimensions (x-,y-, and z-axes) for every slice of the scan, based on the X-ray attenuation within the slice. Tube current modulation is implemented based on either: 1. attenuation measurements obtained from the topogram or scout views: This approach is used by all manufacturers for z-axis (longitudinal) ATCM modulation, but is used by GE and Toshiba for the x- and y-axes (transverse or angular) [13, 14]; 2. tube current adjustment “on the fly” using the measured attenuation of the previous one-half gantry rotation: This approach is used by Siemens for x, y (transverse or angular) ATCM modulation [15].
The noise level or desired image quality is user-programmable and typically adjusted according to the clinical task specified on the clinical requisition. Therefore, the effectiveness of ATCM dose reduction is dependent on the radiologist. Each manufacturer uses a proprietary method to define the desired image quality (e.g., reference mA by Siemens, noise index by GE, standard deviation by Toshiba, reference images by Philips). In chest CT, a dose reduction of 20–26% can be achieved in average-size patients using ATCM rather than fixed tube current [16]. However, in very large patients, ATCM can result in increased radiation doses [17] because the system attempts to maintain uniform image quality almost independently of body size. Thus, the operator needs to be aware of this important caveat and to adjust the image quality level in obese patients.
A few years ago, organ-based tube current modulation was introduced by one manufacturer with the goal of reducing the tube current (x–y plane) when the X-ray tube was positioned over radiosensitive organs, including the female breast, the thyroid gland, and the lens of the eye. Long term follow-up data from the Life Span Study have shown that the radiation sensitivity of female breast tissue is higher than previously thought. Consequently, in the 2007 ICRP (International Commission on Radiological Protection) publication [18], the tissue weighting factor of the female breast was increased. Because in chest CT the breasts are included in the scan range but are not the target organ of the imaging procedure, it is important to decrease the radiation dose to these radiosensitive tissues. Organ-based tube current modulation reduces the tube current in the anterior 120° arc of the rotation by up to 25% of the tube current, while increasing the tube current to 125% over the remaining 240° of the rotation to maintain constant image quality in the center of the patient [19] (Fig. 3). In phantom studies, an average reduction of the breast dose up to 37% was achieved [20]. Nevertheless, recent clinical studies showed that in a majority of women (up to 99%) parts of the glandular breast tissue are located outside the dose-reduced sector and therefore might be at increased risk of overexposure when organ-based tube current modulation is used [20, 21]. Further refinement of this technique will be required to better protect radiosensitive breast tissue.
Principle of organ-based tube current modulation: to protect radiosensitive organs such as the female breasts, the tube current is reduced during the anterior 120° of the gantry rotation. To maintain image quality in the center of the image, the tube current is augmented for the remaining 240° of rotation
Adjustment of the Tube Voltage for Pulmonary CT Angiography
Increasing attention is being paid to the use of lower tube voltages (80–100 kVp) in contrast-enhanced CT. In the chest, pulmonary CT angiography to rule out an embolism is well suited for a low tube voltage technique for two reasons (Fig. 4): while the radiation dose decreases at a more than linear rate, the iodine contrast enhancement increases substantially (by a factor of 2, for example, when the tube voltage is decreased from 140 to 80 kVp). The increased attenuation of contrast medium at reduced kVp (70–100) is secondary to the enhanced photoelectric effect at a lower kVp. Two publications demonstrated that image quality did not decrease when the peak tube voltage for pulmonary CT angiography was lowered to 100 kVp, while resulting in a dose reduction of up to 50% [22, 23]. Furthermore, Schueller-Weidekamm et al. reported an increase in analyzable segmental pulmonary arteries at 100 kVp compared to 140 kVp [23]. The first large-scale prospectively randomized study (REDOPED) investigating the accuracy of low-dose pulmonary CT angiography provided clear evidence that, in patients up to 100 kg body weight, an 80-kVp protocol yields very similar accuracy, diagnostic confidence, and image quality but with a dose that is 30% lower than in a 100-kVp protocol [24]. The estimated effective dose was only 2.25 mSv at 80 kVp. The study also suggested the potential for further dose reduction since it employed a dated CT technology using slow scan times and no iterative reconstruction.
Examples of lowering the tube voltage in pulmonary CT angiography to rule out pulmonary embolism. a A transverse slice in a male patient (95 kg body weight) who was scanned with 80 kVp [150 mA; volume CT dose index (CTDIvol) of 4.2 mGy]. b An obese male patient (150 kg body weight) scanned with 100 kVp (100 mA, CTDIvol of 9.3 mGy). Both images were acquired on a 16-slice MDCT scanner and reconstructed with filtered back projection. The images clearly demonstrate that, even with dated CT technology, lowering of the tube voltage in pulmonary angiography is possible without impairing diagnostic accuracy
Reduced tube voltage can be implemented either manually or using an automated technique. We employ a manual technique based on clinical observation and measurements; specifically, an 80-kVp protocol is applied for patients with a body weight up to 100 kg and a 100-kVp protocol for patients with a body weight >100 kg (Fig. 4). At least two manufacturers offer automatic tube voltage selection, which selects an optimal tube voltage based on patient size, selected CT protocol, and operator-defined image quality [25]. In a prospective study, Niemann et al. demonstrated a dose reduction of 39% in pulmonary CT angiography using automatic tube voltage selection [25]. Instead of the standard tube voltage of 120 kVp, in 28% of the cases a tube voltage of 100 kVp and in 69% of the cases a tube voltage of 80 kVp were automatically selected.
Iterative Reconstruction Technique
While the commonly used filtered back-projection image reconstruction technique is computationally efficient, it suffers from noise and artifact limitations. Despite their availability over 20 years ago, iterative reconstruction (IR) techniques never gained acceptance due to their computational intensity and slow image reconstruction speed. The advent of faster computer platforms and the demand for a reduction of the radiation dose without an increase in image noise has spurred research into IR. The nomenclature of IR techniques is not yet standard. Manufacturers have developed a number of proprietary techniques involving different strengths and varying in reconstruction speed spatial resolution, and image noise. In general, in IR an initial image is formed that is then used to generate simulated raw scan data, which are compared to the acquired scan data. A new image is then generated based on the difference. This process is repeated, or iterated to further improve the image. IR can operate either with image and raw scan data space (Adaptive Statistical Iterative Reconstruction, ASIR, GE Healthcare; Adaptive Iterative Dose Reduction 3D, AIDR 3D, Toshiba, Sinogram Affirmed Iterative Reconstruction, SAFIRE, Siemens Healthcare; and iDose, Philips Healthcare) or raw scan data space alone (MBIR or Veo, GE Healthcare; Advanced Modeled Iterative Reconstruction, ADMIRE, Siemens Healthcare). IR is a powerful tool to either improve image quality in large patients or to maintain diag-nostically adequate noise while decreasing radiation dose in small or intermediate sized patients.
There are numerous reports of substantial dose reductions using IR rather than standard filtered back projection while maintaining image quality [26, 27]. However, radiologist applying IR techniques have to be aware of the fact that images thus reconstructed tend have a blotchier and more pixilated appearance, impacting the evaluation of normal anatomic lung structure such as the interlobular fissures, subsegmental bronchial walls, and small peripheral blood vessels [27]. This occurs particularly with very aggressive noise reduction in order to achieve sub-mSv chest CT scans. Moreover, the image quality of sub-mSv chest CT is suboptimal for diagnosing mediastinal structures such as lymph nodes [27]. In the use of IR techniques for dose reduction in general, radiologists are advised to pay extra attention to the diagnostic accuracy with respect to the detection of small pulmonary nodules on the IR images. This advice is given against the background of the substantially decreased image noise achieved with IR but no impact of improved lesion detectability [28].
Special Indications
Pulmonary CT Angiography in Pregnancy
Low-dose pulmonary CT angiography is a valuable alternative for a ventilation/perfusion scan to exclude pulmonary embolism in a pregnant woman with elevated D-dimer level and negative compression sonography of the veins of the lower extremities. The use of tube voltages of 80 or 100 kVp and limiting the scan range from the aortic arch to the diaphragm will effectively reduce the radiation dose. The increased radiosensitivity of the glandular breast tissue during pregnancy deserves particular attention. Although the impact of using breast shields in preventing higher absorbed breast dose is controversial [29, 30], a reduction of tube current in the anterior part of the thorax with organ-based tube current modulation might offer a partial solution, as mentioned earlier.
Lung Cancer Screening
Recent US and Japanese lung cancer screening trial data have shown a statistically significant (p<0.05) reduction in lung cancer mortality when lung cancers are diagnosed at an early stage [31, 32]. Ultra low dose lung cancer screening is possible because the large contrast differences between the pulmonary nodules and surrounding air-filled lung allows the use of images with very high noise levels; however, mediastinal images will have reduced diagnostic accuracy with these techniques. The image quality and diagnostic accuracy for the lung parenchyma using low mA values have been investigated [12, 33]. Results from phantom studies showed that 80 or 100 kVp can be combined with 25 mA with no deterioration in the detection of small lung nodules [33]. A recent phantom study achieved high image quality and sensitivity in pulmonary nodule detection at an effective dose of 0.06 mSv using a novel IR technique and tin filtration for spectral shaping [34].
Cardiac CT Dose Reduction
In cardiac CT, the requirement for scan acquisition to be synchronized to the phase of the cardiac cycle leads to specialized dose reduction strategies [35]. The initial approach to cardiac gating was retrospectively gated helical acquisitions that used low pitch values (approximately 0.2–0.5 depending on heart rate and single vs. dual tube gantry configuration) to provide raw scan data at all spatial locations in all phases of the cardiac cycle. Initial retrospective helical acquisition allowed the reconstruction of low-noise images at multiple cardiac phases. The images were typically reconstructed at 5 or 10% increments of the R to R interval. These image sets provided visualization of the coronary arteries and the motion of the ventricular walls and valves but at the cost of a high radiation dose (9–32 mSv). Moreover, this acquisition technique was radiation dose wasteful for pure coronary artery imaging, as the arteries are only motion free at 60–80% of the R to R interval for heart rates below 80 beats per minute.
The dose efficiency of retrospective helical acquisition was improved by >50% with the implementation of EKG tube current modulation, which reduces tube current by 50–90% during high-motion portions of the cardiac cycle. This provides low-noise coronary artery images in diastole and noisier wall and valve motion images at selected increments through the remaining cardiac cycle. The use of tube current modulation is recommended for all retrospective cardiac-gated acquisitions.
Prospective cardiac gating provides further dose reductions for coronary artery imaging by acquiring raw scan data only at 60–80% of the cardiac cycle. This scan acquisition mode is a modification of “step and shoot,” with the scanner table stationary while a full detector width (e.g., 40 mm) of raw scan data are acquired. The scan table is then moved (e.g., 35 mm) and raw data are acquired at another position of the heart during the next heart beat. Thus, the detector steps through the entire cardiac volume, while the 5-mm overlap ensures there are no gaps in the coronary artery anatomy due to minor variations in heart positions between acquisitions. This results in a pitch factor of 0.875. Depending on the size of the heart and the width of the detector, three to five table steps are used. The result is a 77% dose reduction compared to retrospective helical acquisition without tube current modulation. Wide-area detectors capable of covering the entire z-axis length of the heart (e.g., 16 cm) can perform this acquisition without table movement. This allows a pitch factor of 1 but requires cone beam corrections in the image reconstruction.
A further modification of prospective gating is provided in dual tube CT scanners operating in helical mode. This technique is known as high-pitch or flash imaging. Using two CT tubes, complete raw scan data sets can be obtained using a pitch factor of 3.2. The high table speed allows coverage of the entire heart during diastole in patients with a heart rate below 65 beats per minute. This mode is not useful secondary to motion artifact in patients with higher heart rates.
In all prospective acquisitions, transient elevation in heart rate or arrhythmias can seriously degrade image quality. With the exception of high-pitch acquisitions, this source of image degradation can be partially mitigated by acquiring redundant projections. This modification is referred to as padding and allows movement of the acquisition window within the diastolic interval to search for the most motion-free time point for the coronary arteries. In some cases, motion-free visualization of different parts of the vessels (e.g., proximal vs. distal portion of the right coronary artery) occurs at different time points. However, these additional projections are associated with an increased radiation dose such that some authors recommend against the routine use of padding [36].
Conclusion
This review has outlined a number of practical methods for dose reduction that are independent of the CT scanner make and model. Other very effective scanner-specific technical innovations are also available on current-generation scanners. They require that radiologists are aware of the benefits and limitations of their use. When all current dose reduction strategies are utilized sub-mSv cardiothoracic CT is achievable in non-obese patients.
References
Mettler FA, Jr., Bhargavan M, Faulkner K et al (2009) Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources 1950–2007. Radiology 253:520–531.
Aroua A, Samara ET, Bochud FO et al (2013) Exposure of the Swiss population to computed tomography. BMC Medical Imaging 13:22.
Preston DL, Ron E, Tokuoka S et al (2007) Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiation Res 168:1–64.
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505.
Mathews JD, Forsythe AV, Brady Z et al (2013) Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 346:f2360.
Flors L, Leiva-Salinas C, Norton PT et al (2013) Endoleak detection after endovascular repair of thoracic aortic aneurysm using dual-source dual-energy CT: suitable scanning protocols and potential radiation dose reduction. AJR Am J Roentgenol 200:451–460.
Prokop M (2008) [Radiation dose in computed tomography. Risks and challenges]. Der Radiologe 48:229–242.
Karlo C, Gnannt R, Frauenfelder T et al (2011) Whole-body CT in polytrauma patients: effect of arm positioning on thoracic and abdominal image quality. Emerg Radiol 18:285–293.
Brink M, de Lange F, Oostveen LJ et al (2008) Arm raising at exposure-controlled multidetector trauma CT of thoracoabdominal region: higher image quality, lower radiation dose. Radiology 249:661–670.
Li J, Udayasankar UK, Toth TL et al (2007) Automatic patient centering for MDCT: effect on radiation dose. AJR Am J Roentgenol 188:547–552.
Mayo JR, Whittall KP, Leung AN et al (1997) Simulated dose reduction in conventional chest CT: validation study. Radiology 202:453–457.
Mayo JR, Kim KI, MacDonald SL et al (2004) Reduced radiation dose helical chest CT: effect on reader evaluation of structures and lung findings. Radiology 232:749–756.
Kalra MK, Maher MM, Toth TL (2004) Comparison of Z-axis automatic tube current modulation technique with fixed tube current CT scanning of abdomen and pelvis. Radiology 232:347–353.
Kalra MK, Maher MM, Kamath RS et al (2004) Sixteen-detector row CT of abdomen and pelvis: study for optimization of Z-axis modulation technique performed in 153 patients. Radiology 233:241–249.
Greess H, Lutze J, Nomayr A et al (2004) Dose reduction in subsecond multislice spiral CT examination of children by online tube current modulation. Eur Radiol 14:995–999.
Kalra MK, Rizzo S, Maher MM et al (2005) Chest CT performed with z-axis modulation: scanning protocol and radiation dose. Radiology 237:303–308.
Schindera ST, Nelson RC, Toth TL et al (2008) Effect of patient size on radiation dose for abdominal MDCT with automatic tube current modulation: phantom study. AJR Am J Roentgenol 190:W100–W105.
The 2007 Recommendations of the International Commission on Radiological Protection (2007) ICRP publication 103. Annals of the ICRP 37:1–332.
Duan X, Wang J, Christner JA et al (2011) Dose reduction to anterior surfaces with organ-based tube-current modulation: evaluation of performance in a phantom study. AJR Am J Roentgenol 197:689–695.
Lungren MP, Yoshizumi TT, Brady SM et al (2012) Radiation dose estimations to the thorax using organ-based dose modulation. AJR Am J Roentgenol 199:W65–73.
Taylor S, Litmanovich DE, Shahrzad M (2014) Organ-based tube current modulation: are women’s breasts positioned in the reduced-dose zone? Radiology 140694[Epub ahead of print].
Heyer CM, Mohr PS, Lemburg SP et al (2007) Image quality and radiation exposure at pulmonary CT angiography with 100- or 120-kVp protocol: prospective randomized study. Radiology 245:577–583.
Schueller-Weidekamm C, Schaefer-Prokop CM, Weber M et al (2006) CT angiography of pulmonary arteries to detect pulmonary embolism: improvement of vascular enhancement with low kilovoltage settings. Radiology 241:899–907.
Szucs-Farkas Z, Christe A, Megyeri B et al (2014) Diagnostic accuracy of computed tomography pulmonary angiography with reduced radiation and contrast material dose: a prospective randomized clinical trial. Invest Radiol 49:201–208.
Niemann T, Henry S, Faivre JB et al (2013) Clinical evaluation of automatic tube voltage selection in chest CT angiography. Eur Radiol 23:2643–2651.
Kalra MK, Woisetschlager M, Dahlstrom N et al (2013) Sinogram-affirmed iterative reconstruction of low-dose chest CT: effect on image quality and radiation dose. AJR Am J Roentgenol 201:W235–244.
Padole A, Singh S, Ackman JB et al (2014) Submillisievert chest CT with filtered back projection and iterative reconstruction techniques. AJR Am J Roentgenol 203:772–781.
Schindera ST, Odedra D, Raza SA et al (2013) Iterative reconstruction algorithm for CT: can radiation dose be decreased while low-contrast detectability is preserved? Radiology 269:511–518.
Vollmar SV, Kalender WA (2008) Reduction of dose to the female breast in thoracic CT: a comparison of standard-protocol, bismuth-shielded, partial and tube-current-modulated CT examinations. Eur Radiol 18:1674–1682.
Hurwitz LM, Yoshizumi TT, Goodman PC et al (2009) Radiation dose savings for adult pulmonary embolus 64-MDCT using bismuth breast shields, lower peak kilovoltage, and automatic tube current modulation. AJR Am J Roentgenol 192:244–253.
Aberle DR, DeMello S, Berg CD et al (2013) Results of the two incidence screenings in the National Lung Screening Trial. New England J Med 369:920–931.
Nawa T, Nakagawa T, Mizoue T et al (2012) A decrease in lung cancer mortality following the introduction of low-dose chest CT screening in Hitachi, Japan. Lung Cancer 78:225–228.
Christe A, Charimo-Torrente J, Roychoudhury K et al (2013) Accuracy of low-dose computed tomography (CT) for detecting and characterizing the most common CT-patterns of pulmonary disease. Eur J Radiol 82:e142–150.
Gordic S, Morsbach F, Schmidt B et al (2014) Ultralow-dose chest computed tomography for pulmonary nodule detection: first performance evaluation of single energy scanning with spectral shaping. Invest Radiol 49:465–473.
Mayo JR, Leipsic JA (2009) Radiation dose in cardiac CT. AJR Am J Roentgenol 192:646–653.
Leipsic J, LaBounty TM, Ajlan AM et al (2013) A prospective randomized trial comparing image quality, study interpretability, and radiation dose of narrow acquisition window with widened acquisition window protocols in prospectively ECG-triggered coronary computed tomography angiography. J Cardiovasc Comput Tomogr 7:18–24.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Italia
About this chapter
Cite this chapter
Euler, A., Szucs-Farkas, Z., Mayo, J.R., Schindera, S.T. (2015). Dose-Lowering Strategies in Computed Tomography Imaging of the Lung and Heart. In: Hodler, J., von Schulthess, G.K., Kubik-Huch, R.A., Zollikofer, C.L. (eds) Diseases of the Chest and Heart 2015–2018. Springer, Milano. https://doi.org/10.1007/978-88-470-5752-4_22
Download citation
DOI: https://doi.org/10.1007/978-88-470-5752-4_22
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-5751-7
Online ISBN: 978-88-470-5752-4
eBook Packages: MedicineMedicine (R0)