Abstract
Objectives
To estimate the number of patients who receive a cumulative effective dose (CED) of ≥ 100 mSv from computed tomography (CT) in a single day or episode of care.
Methods
We examined 28,870 patients who underwent 49,834 CT examinations in a tertiary care centre in Italy in 2.5 years. Radiation exposures were retrieved from the hospital’s automatic exposure monitoring system. Two cohorts were identified as those who received a CED of ≥ 100 mSv in a single day and within a month starting from the first examination. Organ doses were estimated for the first cohort.
Results
Among the 1765 (6.1%) patients who received CED ≥ 100 mSv in the observation period, 427 received a CED of ≥ 100 mSv within a month (and 70 patients in a single day). This group represented 1.5% of all patients who underwent CT exams and 24% of those who received CED ≥ 100 mSv in the observation period. The clinical indication for referral included cancer in 132 patients (31%) and non-oncological indications in 295 patients (69%). In 68/70 patients with CED > 100 mSv in a single day, at least one organ/tissue received a dose of ≥ 100 mGy.
Conclusions
The finding of a sizeable percentage of patients undergoing CT exams and receiving CED ≥ 100 mSv in a single episode of care points toward the need of imaging appropriateness criteria, to revise the routine protocols, to replace older machines, and to provide to the radiologist the patient’s prior radiation history to facilitate an appropriate decision-making process.
Key Points
• Patients can receive effective doses greater than 100 mSv in a single CT or in multiple CT examinations performed in a single episode of care in 1.5% of patients in a 2.5-year period.
• In this study, the clinical indication for CT referral was non-oncological in 69% of patients.
• The patient’s prior radiation history should be provided to the referring physicians and the radiological medical practitioner to facilitate an appropriate decision-making process.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A cumulative effective dose (CED) of ≥ 100 mSv for patients undergoing radiological imaging has been recently the focus of several publications. According to ICRP [1], effective dose (ED) should not be used for individual risk assessment and 100 mSv of ED should not be interpreted as a threshold for radiation effects. Nonetheless, at this level of ED, many organs are susceptible to receive doses of 100 mGy or more and the recent review undertaken by the United Nations Scientific Committee on Effects of Atomic Radiation (UNSCEAR) evidenced radiation-related adverse effects (particularly cancer) at or above the absorbed organ dose greater than 100 mGy for certain cancers like of the bone marrow, thyroid, breast, and colon [2]. Moreover, a recent review shows that there is now convincing evidence of excess cancer risk at organ doses even below 100 mGy [3].
The widespread diffusion of automatic exposure monitoring systems has prompted the recollection of retrospective data aimed at identifying patients with different clinical condition who are likely to reach a high CED [4,5,6,7] or to assess percent of patients undergoing multiple computed tomography (CT) exams [8,9,10] or interventional radiology procedures [11] that lead to a CED of ≥ 100 mSv, in a set period of time.
Most of the published studies reporting patients with a CED of ≥ 100 extended their period of observation to years or even decades in which the doses were accrued. It is not clear if such high CED can be accrued in a single episode of care.
In this study, by retrospectively searching in our exposure monitoring system, we investigated the clinical condition of patients susceptible to receive a CED at or above 100 mSv from CT examinations in a single day (in those cases, also organ/tissue doses of ≥ 100 mGy were assessed) and within a month, since such a delay would embrace the usual duration of patient management for a usual “single-shot” disease or an episode of chronic disease.
Materials and methods
Source of data
Data was collected between 13 June 2017 and 18 November 2019 using the exposure monitoring system Gray Detector (Ver 2.0 EL.CO Healthcare Solutions) which stored data of all patients undergoing CT exams since 2017. Patient data were imported in the CT through the radiological information systems, and no examinations were performed to subsequent patients, without the required data entry. A single visit for a CT study (one accession number) was counted as single CT “exam,” and thus, if multiple phases (CT scan acquisitions) were performed during the study, it was still counted as one CT exam. The CT scanners employed during the observation period were as follows: Brilliance 16, Ingenuity Core 64, Ingenuity Elite 128, Brilliance ICT Elite 256 (Philips Healthcare), LightSpeed VCT 64, Optima 540 (GE Healthcare), and an intraoperative CT scanner (AIRO, Brainlab).
Inclusion criteria
The CT machines provide volumetric computed tomography dose index (CTDIvol) and dose-length product (DLP) values for each patient along with the patient’s unique ID, which are automatically stored in the hospital picture archiving and communication system (PACS) and retrieved by the exposure monitoring system, by accession to the PACS.
DLP data indicate the total amount of radiation (i.e. intensity × scan length) used to perform the CT examination and are quantified in a cylindrical phantom of a specified size (i.e. 16 cm “head” or 32 cm “body” in diameter). Using the reference dose quantities provided by machines, the system then calculates ED using conversion factors ED/DLP: 0.0023 and 0.017 mSv mGy−1 cm−1 for the head and body phantom, respectively, as published in radiation protection publication 154 of the European Commission [12].
This method for estimating ED is a well-established one and has been used in many previous publications [9, 13]. A CED of ≥ 100 mSv accrued in single day or within a month was chosen as the criterion for inclusion in the study. The medical condition of each patient leading to referral for CT was identified in the medical record.
Organ dose estimates
CTDIvol and DLP are common methods to estimate a patient’s radiation exposure from a CT procedure. The exposures are the same regardless of patient size, but the size of the patients is a factor in the absorbed organ doses (HT). Therefore, after inclusion in the study, the software VirtualDose (ver.2017, Virtual Phantoms Inc.), in conjunction with body mass index (BMI) of the single patient, was used to compute HT based on Monte Carlo simulations of radiation transport in virtual anthropomorphic phantoms (CEDMC) [14] in the cohort of patients with > 100 mSv in a single day. This code has been validated as an accurate tool to provide HT from CT in both adults and paediatric patients [15, 16] and has been used in many publications [17, 18].
Statistical analysis
Data were described using mean and standard deviation or median, interquartile ranges, and percentiles. Box and whisker plots were used to provide a graphical representation of the organ doses. Outliers are points higher than the value of the 75th percentile plus 1.5 times the interquartile distance, or lower than the value of the 25th percentile minus 1.5 times the interquartile distance.
Results
Number of CT exams
In the database, there were 28,780 patients who underwent 49,834 CT exams. The average number of CT exams per patients was 1.73 ± 1.41. The 75th percentile in the distribution of CT examinations was 2 and the 95th percentile was 4.
Patients with a CED of ≥ 100 mSv
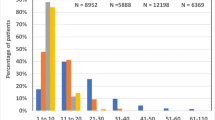
The study identified a cohort of 1765 patients who received CEDCC ≥ 100 mSv in the observation period of 2.4 years, based on the ED/DLP conversion coefficient method. This represents 6.1% of all patients who underwent CT exams. The frequency distribution of patients reaching the threshold of 100 mSv in a set period starting from the first recorded examination is represented in Fig. 1. Since the follow-up period was not the same for each patient, the percentages of patients likely to overpass the threshold of 100 mSv in 3 months, 6 months, and 1 year might be seen as an underestimation since the ones having the first examination in the last year of the observation period might not have their doses recorded for the entire year (or semester, or trimester).
Patients with a CED of ≥ 100 mSv in a single day and in a month
The demographic characteristics of the patients are reported in Table 1. This study identified a subgroup of 70 patients who received CED ≥ 100 mSv in a single examination (66) or in multiple examinations performed on the same day (4). This group represented 0.25% of all patients who underwent CT exams and 4% of those who received CED ≥ 100 mSv in the observation period. The mean number of sequences per examination was 5.9 ± 1.8 with a maximum of 10 sequences in two exams performed in the same day in a polytrauma patient submitted first to a whole-body CT (1 head, 1 neck, 1 lumbar spine, 2 chest with and without contrast and a three-phase abdominal CT) and to a CT-guided intervention for vertebroplasty on the same day (2 sequences).
The study identified another subgroup of 427 patients who received CED ≥ 100 mSv within a month from the first examination. This group represented 1.5% of all patients who underwent CT exams and 24% of those who received CED ≥ 100 mSv in the observation period. The mean number of CT exams per patient was 2.5 ± 1.5 with a maximum of 12, and the mean number of sequences per patient in the period was 9.4 ± 3.5.
The patient’s clinical indication for referral together with the estimated CED values is reported in Table 2 and included cancer in 132 patients (31%): among them, 33 were referred for cancer diagnosis, 15 for cancer follow-up, and 84 for cancer staging. The remaining 295 patients (69%) had non-oncological indications which were grouped in renal evaluation (22) including renal cysts, colic, and transplant; polytrauma (97); thoracic and abdominal evaluations (130) including aortic dissection, bowel obstruction, ischemia or diverticulitis, abdominal colic, and evaluation of liver cirrhosis; CT-guided interventions (7) for biliary drainage or vertebroplasty; and other indications (30).
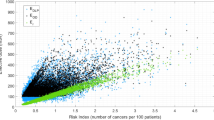
An insight in the potential dependence of high doses from CT equipment is available in Fig. 2 in which the frequency distribution of patients with CED ≥ 100 mSv in a month depending on CT equipment is presented. For each type of scanner, also the mean CED is reported.
A better insight into the dose optimisation is available through Table 3 in which the median value of dose-length product (DLP) in mGy cm is presented overall and for different CT scanners. It indicates that on average radiation doses of CT patients were lower than the European Diagnostic reference levels as published in EC publication Radiation Protection n.180 [19] but higher than the US national benchmark as obtained through the American College of Radiology Dose index registry [9].
Organ doses
Table 4 and Fig. 3 show summary statistics for HT estimated with the Monte Carlo simulation in the subset of 70 patients with CED ≥ 100 mSv in a single day. Noteworthy, in all but two patients, there was at least organ/tissue receiving an HT ≥ 100 mGy. The percentage of patients receiving HT ≥ 100 mGy ranged from 21% for the brain to 87% for the liver.
Discussion
CT imaging provided immense benefits in the diagnosis and management of many health conditions, which far outweigh radiation risk when the procedure is justified and optimised to achieve the required diagnostic objective. Nevertheless, attention has been raised recently to patients who require repeated imaging for both diagnostic and therapeutic purposes. Information has become available that the number of patients who accumulate an effective dose of 100 mSv and higher in a few years from recurrent CT procedures is greater than previously known and might concern nearly half million patients per year in OECD (Organization for Economic Co-operation and Development) countries [10] and one out of five such patients is likely to be below 50 years of age [9].
Data analysed in this study show that overall, 6.1% of patients undergoing CT exams in a tertiary care centre received doses from CT exams with CED ≥ 100 mSv in an observation period of 2.4 years and that a sizeable percentage of them (1.5%) accrued such CED in a single day, due to a single CT examination or in a single episode of care involving multiple CT examinations within a month starting from the first examination.
Although the finding of patients receiving CED > 100 mSv in a set period of time has been recently the topic of several publications [8,9,10,11], the existence of a sizeable subgroup of patients susceptible to receive such value in a single episode of care is unprecedented and add information on the current framework of CT usage.
There is a need to develop models for predicting patients with clinical indications that are likely to accumulate relatively high doses due to recurrent CT imaging. Noteworthy, in our study, 69% of such patients were referred to CT for non-oncologic indications and, among them, the polytrauma subgroup, showing a mean age of 53 years, was on average 13 years younger of the subgroup of patients referred for diagnosis, follow-up, or staging of a suspected or already-known cancer.
The current study was not aimed at examining the CT acquisition parameters like voltage, current, rotation time, tube current modulation, and iterative image reconstruction. Nonetheless, the impact of CT techniques can be indirectly assessed from the DLP values for individual exams reported in Table 3. Among the CT devices, there were significant differences in terms of average DLP values. The LightSpeed VCT and the Brilliance CT exhibited the highest median values for DLP in body examinations (1107 and 835 mGy cm, respectively), well above the European DRLs and accounted for nearly 70% to the number of patients with high CED (126 and 169 patients, respectively). Both CTs were not equipped with iterative reconstruction methods and were eventually dismissed from routine clinical practice at the end of 2018–beginning of 2019. This provides, although only “a posteriori”, a reason why older machines should be replaced with modern equipment and points toward the role that industry plays in dose reduction, by improving hardware and software.
Concerning the protocols, it must be underlined the high number of acquisitions per examination: while the median number of CT exams needed to overpass 100 mSv was in the range of 1–4, the median number of acquisitions was in the range 6–11 demonstrating the high prevalence of multiphase examinations. This finding emphasises the need of customising imaging protocols for clinical situations that require repeated imaging in order to minimise the cumulated radiation dose, since such imaging situations might often need fewer doses than other exams for the same anatomical region.
Our study has some limitations. Due to the retrospective collection of data, patients were followed for different time periods. This will likely affect the percentage of patients with CED ≥ 100 mSv in a set period of time, but should have only a limited impact on the assessment of patients who overpassed the same threshold in a single episode of care, defined arbitrarily as 1 month after the first examination. Although, as a rule in our hospital, care is taken to repeat successive examinations on the same patient with the same CT machine, not always this was the case. Therefore, the distribution of patients with CED ≥ 100 mSv with respect to different CT equipment should be interpreted with caution. We did not include radiation dose from other exams such as interventional procedures and nuclear medicine studies, both of which involve significant radiation doses. This is expected to result in an underestimation of the number of patients with CED ≥ 100 mSv in the period. The conversion factors used to calculate E are not standardised and there can be significant differences in values of E derived with different methods, and the uncertainties associated might be high. However, the estimation of ED by “simpler” methods based on easily measurable dose metrics and the application of conversion factors that have been determined through scientific research have been promoted by UNSCEAR in 2015 [20].
Despite these limitations, our results are the first assessment of the number of patients receiving relatively high doses from repeated CT examinations in a single episode of care that should prompt actions from the different stakeholders involved in patient’s radiation protection including the need for medical societies to develop imaging strategies for clinical conditions that require repeated imaging, for industry to further development of lower dose CT including sub-millisievert CT, for developers of exposure monitoring systems to make patient’s prior radiation history available to the referring physicians, and for radiological medical practitioners to facilitate a decision-making process based upon weighing benefits and risks.
Conclusions
This study showed that 1.5% of the patients submitted to CT in a 2.5-year period can receive a CED greater than 100 mSv in a single episode. The clinical indication for CT referral was non-oncological in 69% of patients. Actions are needed from various stakeholders to ensure that the patient’s prior radiation history is taken into consideration as a factor to re-evaluate current radiation risk management policies.
Abbreviations
- CED:
-
Cumulative effective dose
- CT:
-
Computed tomography
- CTDIvol :
-
Volumetric computed tomography dose index
- DLP:
-
Dose-length product
- ED:
-
Effective dose
- H T :
-
Organ doses
- PACS:
-
Picture archiving and communication system
References
(2007) The 2007 recommendations of the International Commission on Radiological Protection. Ann ICRP 103(37):1–332
United Nations Scientific Committee on the Effects of Atomic Radiation (2018) Sources, effects and risks of ionizing radiation. Available via https://www.unscear.org/docs/publications/2017/UNSCEAR_2017_Report.pdf. Published March 2018. Last accessed on 17/07/2020
Hauptmann M, Daniels RD, Cardis E et al (2020) Epidemiological studies of low-dose ionizing radiation and cancer: summary bias assessment and meta-analysis. J Natl Cancer Inst Monogr 56:188–200
Einstein AJ, Weiner SD, Berheim A et al (2010) Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA 304:2137–2144
Stein EG, Haramati LB, Bellin E et al (2010) Radiation exposure form medical imaging in patients with chronic and recurrent conditions. J Am Coll Radiol 7:351–359
De Mauri A, Brambilla M, Chiarinotti D, Matheoud R, Carriero A, De Leo M (2011) Estimated radiation exposure from medical imaging in hemodialysis patients. J Am Soc Nephrol 22:571–578
De Mauri A, Brambilla M, Izzo C et al (2012) Cumulative radiation dose from medical imaging in kidney transplant patients. Nephrol Dial Transplant 27:3645–3651
Brambilla M, Vassileva J, Kuchcinska A, Rehani MM (2020) Multinational data on cumulative radiation exposure of patients from recurrent radiological procedures: call for action. Eur Radiol 305:2493–2501
Rehani MM, Yang K, Melick ER et al (2020) Patients undergoing recurrent CT scans: assessing the magnitude. Eur Radiol 304:1828–1836
Rehani MM, Hauptmann M (2020) Estimates of the number of patients with high cumulative doses through recurrent CT exams in 35 OECD countries. Phys Med 76:173–176
Li X, Hirsch JA, Rehani MM, Ganguli S, Yang K, Liu B (2020) Radiation effective dose above 100 mSv from fluoroscopically guided intervention: frequency and patient medical condition. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.19.22227
European Commission (2008) European guidance on estimating population doses from medical X-ray procedures. Radiation protection No 154. EC Brussels. Accessed July 17, 2020
Masjedi H, Zare MH, Keshavarz Siahpoush N, Razavi-Ratki SK, Alavi F, Shabani M (2020) European trends in radiology: investigating factors affecting the number of examinations and the effective dose. Radiol Med 125:296–305
Ding A, Gao Y, Liu H et al (2015) VirtualDose: a software for reporting organ doses from CT for adult and pediatric patients. Phys Med Biol 60:5601–5625
Liu T, Du X, Su L et al (2014) Monte Carlo CT dose calculation: a comparison between experiment and simulation using ARCHER-CT. Med Phys 41:424
Zhang D, Li X, Gao Y, Xu XG, Liu B (2013) A method to acquire CT organ dose map using OSL dosimeters and ATOM anthropomorphic phantoms. Med Phys 40:081918
Peng Z, Fang X, Yan P et al (2020) A method of rapid quantification of patient-specific organ doses for CT using deep-learning-based multi-organ segmentation and GPU-accelerated Monte Carlo dose computing. Med Phys 47:2526–2536
Mahmood U, Horvat N, Horvat JV et al (2018) Rapid switching kVp dual energy CT: value of reconstructed dual energy CT images and organ dose assessment in multiphasic liver CT exams. Eur J Radiol 102:102–108
European Commission RP 180 Medical Radiation Exposure of the European Population, Part 1 & Part 2. 2014. https://ec.europa.eu/energy/content/rp-180-medical-radiation-exposure-european-population-part-1-part-2_en. Accessed on 12 November 2020
UNSCEAR Global Survey on Medical Exposure. A user manual. Draft Version May 2015. http://www.survey.unscear.org/lib/exe/fetch.php?media=unscear_user_manual_version_may2015.pdf. Accessed on 9 January 2020
Funding
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Marco Brambilla.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
The expert in statistics is Marco Brambilla, who is among the authors of the paper.
Informed consent
Written informed consent was not required for this study because no change of intervention in patient management was part of the work that involved data analysis retrospectively.
Ethical approval
Institutional Review Board approval was not required because only summary data (total numbers) were needed for the analysis.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brambilla, M., Cannillo, B., D’Alessio, A. et al. Patients undergoing multiphase CT scans and receiving a cumulative effective dose of ≥ 100 mSv in a single episode of care. Eur Radiol 31, 4452–4458 (2021). https://doi.org/10.1007/s00330-020-07665-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07665-0