Abstract
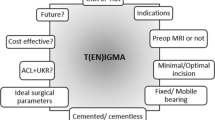
Unicompartmental knee arthroplasty (UKA) is now a well-established procedure in the armamentarium of an orthopaedic surgeon whose practice deals with managing the degenerating knee. Total knee arthroplasty (TKA) predominates in the management of knee osteoarthritis because it lies within the skills and competence of the generalist orthopaedic surgeon, has well-designed instrumentation, and the outcomes are reasonably predictable. The cost-effectiveness of UKA over TKA depends on the revision rates of the former, which tend to be higher than TKA [1]. UKA requires a different philosophical approach [2]. There are no soft tissue corrections permitted. Only the missing bearing surface is being replaced. The key is to restore the joint line accurately in all planes, which means matching the position of the meniscus. All the soft tissue ligaments are preserved, although Cartier allows the absence of an ACL when using a fixed-bearing implant [3, 4]. The underlying principle of UKA is that by restoring the native alignment of the knee, the remaining articular cartilage in the contralateral compartment of the knee becomes normally loaded and so stays healthy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
14.1 Introduction
Unicompartmental knee arthroplasty (UKA) is now a well-established procedure in the armamentarium of an orthopaedic surgeon whose practice deals with managing the degenerating knee. Total knee arthroplasty (TKA) predominates in the management of knee osteoarthritis because it lies within the skills and competence of the generalist orthopaedic surgeon, has well-designed instrumentation, and the outcomes are reasonably predictable. The cost-effectiveness of UKA over TKA depends on the revision rates of the former, which tend to be higher than TKA [1]. UKA requires a different philosophical approach [2]. There are no soft tissue corrections permitted. Only the missing bearing surface is being replaced. The key is to restore the joint line accurately in all planes, which means matching the position of the meniscus. All the soft tissue ligaments are preserved, although Cartier allows the absence of an ACL when using a fixed-bearing implant [3, 4]. The underlying principle of UKA is that by restoring the native alignment of the knee, the remaining articular cartilage in the contralateral compartment of the knee becomes normally loaded and so stays healthy.
Medial UKA is classically indicated in the presence of three conditions:
-
Advanced isolated pain at the medial knee joint space
-
Marked isolated medial knee joint surface destruction, (bone-on-bone)
-
Failure of conservative therapy
The classic definition of indications and contraindications for UKA was reported in 1989 by Kozinn and Scott [5]. Deschamps and Chol [6] reported good and excellent results if UKA was indicated for:
-
Isolated medial or lateral osteoarthrosis (OA) or osteonecrosis of the knee
-
Age over 60 years
-
Weight under 82 kg
-
Lower leg deformity <15° of coronal knee deformity which needs to be correctable to neutral during surgery
-
Extension loss <5°
-
Total knee range of motion (ROM) at least 90°
Contraindications are high activity and systemic inflammatory joint disease.
14.2 Indications for UKA
14.2.1 Biological Factors
14.2.1.1 Age
Thompson et al. [7] analysed 229 UKAs performed at their institution for factors associated with poor outcome. They found that patients younger than 60 years did significantly better than older patients at 2 years follow-up (Knee score KSS 93 vs 77). Pennington et al. [8] reported a series of 46 consecutive UKAs under the age of 60 years at implantation; 93% of these UKAs had excellent results at mean of 11 years of follow-up. Other case series showed similar results [3, 9]. Thus, age under 60 years is no longer thought to be a contraindication for UKA. In a recent review about indications for UKA, Zuiderbaan et al. [10] proposed under age 40 years old as the new threshold.
14.2.1.2 Advanced Disease
-
Rheumatoid arthritis (RA) is a systemic disease affecting all joints and therefore considered to be a contraindication for UKA. However, during the past two decades, the treatment of RA patients has changed considerably. The goal of therapy is no longer only symptom relief but rather the full prevention of structural joint damage and functional decline [11]. Today, no data exist in the literature reporting on the outcome of UKA in RA patients. However, further improvements in medical therapy may lead to an extended lifespan of these joints, eventually becoming candidates for partial knee arthroplasty. Today, progression of inflammatory joint disease is still believed to be less dependent on mechanical factors than on biological ones; therefore these patients are not suitable for UKA.
-
Patellofemoral osteoarthritis (PFOA) visible on radiographs was thought to be a contraindication for UKA. Berger et al. [12] reported a series of 62 consecutive patients with medial UKA at minimum of 10 years of follow-up. Only two patients had to be revised but both for progressive PFOA. However, Berend et al. [13] reported on 638 consecutive knees with medial UKA and compared patients with no radiological evidence of PFOA with patients with such evidence. They found no patient was revised for advanced PFOA during follow-up. As well, they found no difference in outcome or revision rates for medial or lateral PFOA. In addition, Ma et al. [14] compared 100 consecutive medial UKAs with symptomatic anterior knee pain (AKP) in 43% of cases before surgery and looked for the location of PFOA. They found no significant difference between groups with or without preoperative AKP after a minimum of 50 months of follow-up. Patients with preoperative radiological medial PFOA had no significant difference in outcome to patients without PFOA. However, patients with lateral PFOA had a significantly poorer outcome compared to medial or no PFOA. A reason may be that UKA straightens the varus angle of the knee unloading the medial patellofemoral joint, whereas lateral PFOA is loaded more and may become more symptomatic. Thein et al. [15] studied the patellofemoral congruence angle before and after UKA. They found improved congruence after UKA suggesting that the medial PFOA is unloaded by the limb alignment correction. In conclusion, radiological PFOA with or without AKP is not a strong contraindication for UKA. However, severe degenerative PFOA with advanced patellar bone deformity and destruction is still widely held to be a contraindication because these patients have not been included in the above-mentioned series.
-
Lateral tibiofemoral TFOA visible on radiographs was thought to be a contraindication for medial UKA in varus OA. However, both UKA series of Berger et al. [12] and Pennington et al. [8] implanted UKA in the presence of asymptomatic lateral TFOA. They found little or slow progression of the disease over 10–15 years of follow-up without significant worsening of symptoms. Their patients had no progressive lateral joint pain and no revision for lateral TFOA. The key to this result may be the subtotal correction of the weight-bearing axis achieved. The mean femorotibial angle was 5°, which is a mild varus resulting in limited loading of the lateral TF joint space [8]. Marya and Thukral [16] took this concept to the limit by implanting a medial UKA in tricompartmental varus knee OA with symptoms confined to the medial tibiofemoral joint. In 45 low-demand older patients, medial UKA resulted in 96% survival and 95% good and excellent outcomes after 6 years mean follow-up. Therefore, candidates with isolated medial joint space symptoms for medial UKA that have visible early radiological signs of OA at the lateral tibiofemoral joint may still be treated successfully by isolated medial UKA.
-
Minimal disease at the medial TF joint is a contraindication for medial UKA despite the presence of adequate symptoms. Niinimäki et al. [17], in their series of 113 consecutive medial UKAs, analysed the reoperation rate which was found to be independent of age, gender, obesity or arthroscopic degree of cartilage damage in the medial TF joint. However, if the medial knee compartment was thicker than 2 mm on standing anteroposterior radiographs, or more than 40% thickness of the unaffected lateral compartment, the reoperation rate was six times higher. Therefore, even in the presence of arthroscopically proven advanced cartilage loss at the medial compartment, if the medial joint space is radiologically intact, medial UKA must be avoided.
14.2.1.3 Physical Activity
Although Kozinn and Scott [5] recommended low activity and sedentary lifestyle in UKA, current practice changed. Pietschmann et al. [18] studied the preoperative activity level in relation to complications and outcome in their series of 131 consecutive patients. They found that higher preoperative activity was associated with higher postoperative activity with better overall outcome. In contrast, revision rates and complications were equal to the low-activity group after 4.2 years mean follow-up. Despite this encouraging comparative trials, van der List et al. [19] performed a recent large systematic review of 3967 UKA failures. They identified aseptic loosening and polyethylene wear as accounting for 50% of failure after UKA. Knowing that activity causes polyethylene wear and wear causes aseptic loosening, high-impact activity after UKA is still not recommended today.
14.2.1.4 Obesity
Obesity , defined as weighing more than 180 pounds (82 kg), was suggested as a contraindication for UKA in the past [5]. However, Cavaignac et al. [20] performed a retrospective study of 212 UKAs at mean follow-up of 12 years and found no significant influence of weight on revision rate or clinical outcome. Neither comparing patients up to 82 kg nor up to a BMI of 30 kg/m2 revealed a significant difference. Thompson et al. [7] looked at even higher weight. They found that a BMI <35 kg/m2 had no significant difference in revision rate but a significant better outcome score at 1 year follow-up. However, after 2 years of follow-up, this difference in outcome became insignificant, indicating slower recovery for patients with BMI >35. Therefore, currently there is no evidence-based threshold to deny UKA in obese patients.
14.2.2 Mechanical Factors
14.2.2.1 Anterior Cruciate Ligament Deficiency
Anterior cruciate ligament (ACL) deficiency in UKA has been reported to cause early failure and disappointing long-term results [21]. Therefore, in the absence of a functional ACL, combined procedures including UKA and ACL reconstruction have been conducted with success in 15 consecutive cases with excellent results [22]. However, recently, Boissonneault et al. [23] compared medial UKA in the ACL intact and not intact state and found no difference at mean follow-up of 5 years comparing 46 cases of each. Despite this, a recent systematic review looked at complications of UKA in ACL deficiency [24]. The revision rate of UKA in the presence of ACL deficiency was twice as high as in the group with UKA and combined ACL reconstruction. UKA with ACL reconstruction revealed lower outcome than UKA with intact ACL, but this difference was not significant. In conclusion, as for the native knee, if the patient has symptomatic knee instability, the ACL should be reconstructed, whereas the ACL rupture can be ignored in the medial arthritic knee with pain as the main complaint and no instability [25].
14.2.2.2 Mediolateral Subluxation
Mediolateral subluxation of the knee visible on weight-bearing radiographs has been described as a contraindication for medial UKA. This situation was defined either as advanced deformity or as mediolateral ligament insufficiency [6]. However, in a recent series reported by Khamaisy et al. [26] reporting on 174 medial UKAs, mediolateral subluxation could be reduced, and congruence of the lateral knee compartment was effectively restored by UKA. Thus, mild mediolateral ligament insufficiency caused by cartilage wear rather than by ligament insufficiency is not a contraindication for UKA.
14.2.2.3 Deformity and Restricted Range of Motion
Most authors agree that patients with knee varus deformity of more than 10–15° and restricted range of motion of less than 90° with combined extension—flexion or lack of extension of 5°—should not be treated by UKA [5, 19]. However, adequate studies comparing patient outcomes according to these preoperative variables are missing. Therefore, the influence of preoperative limb alignment may be questioned. However, the effect of postoperative limb alignment on UKA outcome has been studied in several case series and systematic reviews. Hernigou and Deschamps [27] analysed their series of 58 medial UKAs at 10–20 years follow-up and found overcorrection into valgus (hip-knee-ankle angle of more than 180°) associated with advanced degeneration of the uninvolved lateral knee compartment, and undercorrection with a hip-knee-ankle angle under 170° was associated with high wear. UKAs between 171° and 180° had better outcomes and lower revision rates. Vasso et al. analysed [28] their series and compared UKA alignment of mild varus (5–7°) with normal -2° to 1° and next to normal 2–4° of varus in 125 consecutive medial UKAs at mean 7.6 years. Mild varus limb alignment resulted in better outcome and no more complications than normal or next normal group. However, Zuiderbaan et al. [10], in their series of 104 consecutive medial UKAs, found better WOMAC scores in patients with a postoperative varus alignment of UKAs between 1° and 4° compared to UKAs with less than 1° or more than 4° of varus. In conclusion, over- and undercorrection with the UKA procedure should be avoided. Consequently, patients with medial compartment OA and valgus knee alignment are not ideal candidates for medial UKA.
14.2.3 Influence of Alternatives on UKA Indications
14.2.3.1 Total Knee Arthroplasty
Several advantages have been listed in case series and randomised controlled trials comparing outcome of UKA and TKA patients. Less perioperative morbidity, reduced blood loss, shorter postoperative rehabilitation, higher postoperative range of motion and reduced surgical costs favour UKA over TKA [29, 30]. In addition, patient-based outcome including the “forgotten knee joint score” is superior for UKA compared to TKA in limited medial knee OA [31]. However, in a recent meta-analysis, the revision rates of partial versus TKA have been compared. Medial UKA showed to have a 2.18-fold annual revision rate compared to TKA [32]. However, despite higher revision rates, UKA has shown to be more cost effective than TKA in a large study comparing 15.437 primary TKAs with 10.624 UKAs [33].
14.2.3.2 High Tibial Osteotomy
HTO was the established treatment for medial unicompartmental knee OA before UKA was available. The most obvious advantage of HTO is that it preserves the natural knee joint. Regarding the indications for UKA versus HTO, overlap exists in the current literature. Both surgical techniques have improved tremendously in accuracy, outcome and longevity. Some relatively clear cut-off variables can be defined in literature. Trieb et al. [34] compared HTO in 27 patients older than 65 years with 67 patients younger and found a 1.5-fold increased risk of failure at mean 13 years follow-up. In addition, the outcome was significantly worse in the older patients group. In two studies (BMI >27.5 kg/m2 and >30 kg/m2), HTO was associated with worse outcome and higher failure rate at 10–20 years follow-up after HTO [35, 36]. In conclusion, patients older than 65 years and obese should be candidates for UKA rather than HTO.
However, regarding deformity and ligament instability, in a recent systematic review, HTO showed superior survival comparing HTO and combined ACL reconstruction with UKA and combined ACL reconstruction [25]. In addition, HTO can stabilise a certain degree of medial collateral ligament insufficiency and can correct varus deformities above 15° or which cannot be corrected by manual reposition. Thus, HTO can be an option when UKA is contraindicated.
A recent meta-analysis of comparative trials between HTO and UKA by Fu et al. [37] comparing HTO and UKA for the treatment of unicompartmental knee OA found 8 studies including 461 patients. There was no overall difference in knee scores, but the postoperative functional subscore favoured UKA, but range of motion favoured HTO. However, HTO had a longer rehabilitation time with initially partial weight-bearing making UKA more attractive for the older and less active patients. Even though most studies showed a difference in complication rates between HTO and UKA, this meta-analysis including 4 studies with 301 patients found no significant difference.
14.2.3.3 Outcome of UKA and HTO Revision to TKA
Seven studies with 5641 patients compared the revision rates after HTO and UKA [37]. The reason for revision after HTO was mainly progressive OA. UKA was revised for loosening or breaking of the components, chronic pain and less frequently for progressive OA. After HTO, there was difficulty achieving correct tibial component position and adequate exposure of the knee. In UKA the most common difficulty was to manage bone defects in the tibia and femur. Compared to primary TKA or TKA after HTO, a significantly bigger polyethylene insert was needed after revision of UKA to TKA [38]. In another meta-analysis, Spahn et al. [39] compared time to TKA revision for patients with UKA and HTO. They found a significantly sooner time to revision of UKA at mean 8.2 years compared to 9.7 years for HTO. In contrast to HTO, the risk of revision of a UKA to TKA decreases with age. UKA patients under age 55 have a 3 times higher revision rate than above 55 years in the Swedish registry [40]. A possible reason was the higher activity and higher wear rate. It may also be that revising a UKA to a TKA is considered easier by general orthopaedic surgeons compared to TKA to TKA, and therefore a revision is more likely to be offered to a patient with an unsatisfactory UKA. Having said that the evidence suggests that in patients under 55 years old, one should favour treatment with an HTO rather than a UKA.
14.2.3.3.1 Summary of Indications
Medial UKA is indicated in symptomatic medial unicompartmental knee OA, with or without radiological signs of patellofemoral OA, in patients age over 55 years and with weight over 30 kg/m2, a varus deformity no greater than 15° or loss of extension over 10°, no need for ACL or other ligament reconstructions and no interest in jumping and pivoting activities. Otherwise, HTO should be considered.
Medial UKA may be considered as well in patients with symptomatic medial knee OA and radiological evidence of OA at the patellofemoral or lateral compartment but without pain and limited bone destruction or deformity in the other compartments, plus a knee range of motion of more than 90°. Otherwise TKA should be considered.
In valgus knee alignment and medial knee OA, or limited medial knee OA with more than 2 mm preserved joint space, other treatment options besides UKA should be considered.
14.3 State-of-the-Art Treatment
Leaving aside the argument about the relevance of the state of the patellofemoral joint, UKA is suitable on radiological grounds when there is bone-on-bone arthritis in either the medial or lateral compartment. It should be noted that this is most likely to be demonstrated on the medial side with the knee flexed and weight-bearing at 30° flexion, whereas on the lateral side, the wear occurs on the posterior condyle. Therefore, lateral tibiofemoral wear may not be shown on an anteroposterior (AP) weight-bearing radiograph, since the knee would have to be flexed at 90°. Therefore, in lateral unicompartmental OA, the standing AP radiograph may appear normal. A provocation test with the knee in valgus flexed beyond 90° elicits pain and crepitus on the lateral tibiofemoral joint line confirms the diagnosis. In this instance, an MRI scan may be useful. It has been argued that the presence of bone marrow lesions aids the decision for UKA [40], but this has been disputed for medial compartment disease [41].
A minimal incision surgery (MIS) approach is justified in UKA and allows full visualisation of the compartment. Placing the incision correctly is important. If too close to the midline, it can be difficult exposing the tibia for its resection. Too far from the midline and the tibial sagittal cut may be impossible. Exposure can be improved by partially excising the infrapatellar fat pad and any patellar and notch osteophytes. The patella can have a sliver removed along its medial or lateral borders to help expose the femoral condyle and avoid excessive retraction. Removing the femoral-rim osteophytes improves exposure since it also relaxes the soft tissues. Evaluating the PFJ, ACL and lateral compartment provides reassurance, although should not lead to a change in the surgical plan as the preoperative workup should have excluded significant damage in the other compartments. Having said that, one should always have a TKA system available if there is a surprise, and a UKA is found to be contraindicated (Fig. 14.1).
As stated earlier, the mobile-bearing UKA has a number of theoretical advantages over the fixed-bearing design. These include better conformity through the flexion arc and therefore potential lower wear rates. The National Joint Registry of England and Wales (NJR) [42] shows that 70% of tibiofemoral UKA are mobile-bearing in the UK. Revision rates (all causes) are consistently greater than for TKA, and fixed-bearing designs have lower revision rates than mobile ones (Table 14.1.)
It should be noted that the confidence intervals between mobile- and fixed-bearing UKAs do not cross. Mobile-bearings have theoretical advantages with respect to wear that should occur between 10 and 20 years post-operation, and the NJR only covers 10 years. The best performing implant in the NJR with 10 years follow-up is the fixed-bearing UKA (Fig. 14.2) with 6.31 revisions per 1000 patient-years (CI 95%, 5.16–7.70). The dominant UKA in the NJR (mobile-bearing UKA) has 12.02 revisions per 1000 patient-years (CI 95%, 11.51–12.54) reported. This may reflect the number of surgeons involved performing small numbers per year in the latter. The modes of failure appear similar, with the addition of bearing dislocation in mobile-bearing designs.
14.3.1 Technical Aspects of Medial Compartment Mobile-Bearing UKA
The degree of pre-existing laxity in the MCL should be evaluated to inform on the depth of tibial resection. The MCL should be normal, and therefore any laxity indicates the degree of articular cartilage and bone loss; the more lax the MCL, the less the resection.
After elevating the capsule from the most proximal part of the medial tibia, care must be taken to avoid damaging the deep MCL. Therefore, the soft tissue elevation medially should only be to the depth of the tibial resection. It must be remembered that the medial meniscus is attached to the MCL, so excision of the body of the meniscus should be undertaken with care, and a 1 mm rim should be left. Pulling hard on the anterior horn of the meniscus and then blindly sectioning the body with a scalpel can remove the deep MCL. If this happens, when the bearing size is assessed, it will be found to be much larger than expected. In this circumstance, either an MCL reconstruction will need to be performed or conversion to a constrained TKA. The MCL also has to be protected during the tibial bone resection. The posterior capsular attachment is the most difficult to elevate; the posteromedial corner can be mobilised safely with a small curved periosteal elevator. The tibial resection is critical. The alignment needs to be correct in the sagittal plane as well as the correct depth and slope. If the tibial resection is perfect, the rest of the operation is technically easy, including gap balancing and femoral component insertion. The tibial cut alignment can be improved through several key steps. The slope should be matched to the patient’s own anatomy in both planes. The depth should be sufficient to allow a 7 mm feeler gauge (or the minimum depth to allow for the thickness of the tibial implant plus 1 mm laxity) to be inserted into the joint without gripping the gauge. The key is to get the new joint line back to the native joint line in all planes. Since the posterior femoral condyle has the full thickness of articular cartilage in medial compartment OA, then when the knee is flexed to 90°, this acts as the marker for the true joint line. Therefore, if the feeler gauge is at the right tension after the tibial resection, then one should be confident that the correct level has been achieved. This also means that achieving the correct posterior femoral cut is easy, since this is now just the thickness of the implant’s posterior condyle, and is achieved using the relevant implant jig. The gap is now balanced in flexion. The MCL must be carefully protected during posterior femoral resection.
To achieve gap balance in extension, all tension must be removed from the soft tissues (i.e. the soft tissue retractors removed). The knee is then opened medially by a gentle valgus force to tension the MCL slightly. The extension gap can then be measured with feeler gauges where the tibial resection is the reference surface. The amount of distal femoral resection then allows for the thickness of the tibial implant and the distal femoral component thickness. Often this is 0 mm but more typically 2–3 mm. Femoral alignment may be improved with modern guides. Extramedullary rods avoid some of the pitfalls of incorrectly placed intramedullary rods. The pin guide must be flush against the condyle to provide accurate assessment of flexion-extension.
Uncemented implants may be used, but cemented implants are perhaps more forgiving. Tibial cement technique is critical and aims to produce 2–3 mm of bone penetration.
14.3.2 Technical Aspects of Medial Compartment Fixed-Bearing UKA
Fixed-bearing UKAs have a number of technical considerations to achieve a successful outcome [43]. Figure 14.3 shows an example which has an all-polyethylene tibial component. An all-polyethylene bearing allows for less bone resection and is easier to revise than a metal-backed one. Theoretically, the metal-back allows greater load transference and therefore may be more appropriate for younger, active patients.
The fixed-bearing surface needs to be flat to allow the curve of the femoral component to find its position on the insert after the wound has been closed; at this point the soft tissues will all be in a stable position and under their final tension. Any restraint caused by dishing the plastic risks overloading and early polyethylene wear. With a flat insert, the poly deforms by creep and so becomes dished and conforming without wear. It follows that it is important that the new implant is not inserted tight; slight laxity mimics the native knee.
Exposure is the same as for a mobile-bearing. Again, the key is to get the tibial cut right. Gap balancing is essentially the same. A key difference is that the femoral component needs to lie aligned with the tibial component in both flexion and extension. This means that the alignment on the femur does not match the femoral obliquity but is at right angles to the tibial alignment. If the tibial component has a varus slope, then the femoral component must match this (Fig. 14.4). It then follows that care must be taken that there is no overhang of the femoral component on the medial retinaculum at its most anterior point.
Finally the femoral component should be inserted flexed. This allows for greater knee flexion than if aligned with the femoral anatomical axis. With insertion with the knee at 90° flexion, impingement occurs between the posterior condyle of the femoral component and the posterior margin of the tibial component. Likewise, the posterior slope of the tibial component helps to avoid this conflict.
There is some evidence, including personal experience, that patients with fixed-bearing UKAs have less postoperative pain and more rapid recovery than mobile-bearings. This may possibly be due to soft tissue impingement by the mobile-bearing during knee motion. The 10-year follow-up data show no difference between the two types; however, the theoretical advantages of the mobile-bearing with respect to polyethylene wear are expected to be shown only after a longer time frame.
14.3.3 Technical Aspects of Lateral Compartment UKA
In the 1990s, lateral UKA was initially criticised by the proponents of the mobile-bearing UKA, mainly because it is difficult to balance the gaps as the lateral compartment is lax in flexion. Therefore, mobile-bearings tend to dislocate. Although the Oxford group have produced a domed-tibial mobile-bearing with some success in the designer hands, most surgeons favour a fixed-bearing design in the lateral compartment. Excellent long-term survival rates of 95–98% survival at 10-year follow-up have changed this perception [44, 45]. There are no differences between medial and lateral UKA when it comes to survival rates [46], if anything lateral fixed-bearing UKA is better as long as the different technical challenges are understood:
-
In the MIS lateral parapatellar approach, removing the lateral patellar osteophytes along with a small partial lateral patellar facetectomy facilitates the exposure of the lateral tibiofemoral compartment and avoids the need for significant medial displacement of the patella. Like on the medial side, the tibial cut should reproduce the native slope. On the medial side, the tibia is dish-shaped but is domed on the lateral. It therefore does not have an obvious posterior slope. The rim should be exposed to the posterior edge. This is easier than medially as the LCL is extracapsular. The resection is usually less than the thickness of the tibial implant to allow for the lateral femoral hypoplasia that is present. The tibia typically has a neutral mechanical axis.
-
The tibial sagittal cut should allow the tibial component to be positioned in internal rotation in order to compensate for the internal rotation of the external femoral condyle in extension (screw home mechanism). This may need to be achieved by creating the sagittal tibial cut with the saw blade passed through a separate stab incision through the patellar ligament. A malaligned tibial cut may induce impingement between the femoral component and the lateral tibial spine.
-
The lateral femoral marginal osteophytes should be preserved in order to position the femoral implant condyle as lateral as possible. However, the notch osteophytes should be removed (to avoid continuing impingement on the ACL and the risk of later rupture).
-
The posterior femoral condyle is worn, and so, if using standard medial UKA jigs for the posterior femoral cut, a suitable sized osteotome needs to be inserted between the bone and the jig to avoid an excessive flexion gap.
-
Strict gap balancing is usually impossible; the lateral compartment opens up if the knee is placed in the Fig. 14.4 position. Resection of the distal femoral condyle needs to be minimal because of the hypoplasia. The tibial and femoral resections need to be such that on insertion of the implant, the knee valgus is less than normal. This reduces overload of the implant and early polyethylene wear [47].
Using these technical tips, the long-term results of the lateral fixed-bearing UKAs are extremely encouraging. The indications can now be extended to include young patients, the overweight and in some cases of posttraumatic OA, e.g. after fracture of the lateral tibial plateau [48].
14.3.4 Custom-Made UKA
Compared to TKA, MIS-UKA leads to faster recovery, lower complications, more “forgotten” joints and higher satisfaction but also, as shown above, has higher revision rates [49]. Reducing the number of revisions is an important goal considering the increasing need for artificial joints. Revision of a UKA in the first 3 years is usually due to surgical error; component malalignment and poor gap balancing being the commonest problems. These manifest as pain, stiffness and, in mobile-bearing designs, bearing dislocation. Poor tibial component fit can result in loosening and subsidence. Femoral component malposition can result in soft tissue impingement as well as poor gap balancing. It is therefore logical to consider whether this can be improved using patient-specific knee implants which are custom-made [50]. This is particularly apparent as the lateral compartment of the knee is biomechanically and anatomically completely different from the medial compartment. Most commercially available unicompartmental implants are not designed specifically for the lateral compartment. Patient-specific implants and the instruments needed for correct alignment and fitting are manufactured by virtual 3D reconstruction and 3D printing based on computed tomography (CT) scans. For the first time, implants are now matched to the individual knee and not vice versa. The aim is to achieve the best possible individual situation and geometry that includes coverage/fit, tibial slope and flexion gap balance.
However, this is currently in its infancy where the literature is sparse, and no long-term data are available.
14.3.5 Robotic Surgery
Many UKA instrument systems rely on manual placement of cutting blocks and extramedullary alignment rods. Open blocks use flexible saw blades; slotted blocks use rigid blades. One system places pins through the block, which is then removed, and the blade cuts on the pins. Accurate positioning is more difficult with MIS as less of the knee is visualised. Since the accuracy of the bone cuts is essential for a favourable outcome from UKA, it is logical to consider whether this would be improved by navigation aids. Computer-assisted navigation and tactile-robot assistance have been increasingly tried. Originally static referencing was used, which still had some implant placement variation between 1 and 2 mm and 2° and 5°, although overall alignment variance was less than 2° [51]. More recently, a dynamic referencing tactile-guidance robotic system has been trialled, which reduces set-up time and complexity [52]. These gave similar results. A retrospective comparative review of robot-assisted implantation versus standard techniques showed no difference in postoperative implant position or short-term outcomes [53]. Robot assistance added 20 min on average to the operation.
Robotic assistance is still experimental. The companies have not made a robot that is independent of the surgeon on the grounds that this would be unacceptable. The current systems are not suitable for normal clinical practice; cost-effectiveness as well as clinical effectiveness still needs to be confirmed, on top of surgeon acceptance. Experienced surgeons have similar outcomes with standard techniques.
14.4 Future Treatment Options
Although not new, there is a vogue for bicompartmental UKA in those patients with an intact ACL and bicompartmental (or even tricompartmental [54]) OA. The problem with bicompartmental tibiofemoral knee arthroplasty is that the medial and lateral tibial plateaux are not in the same orientation. Access is via a standard open access incision, unless the two sides are performed at different times. Navigation and robotics have a role. Cartier has been an enthusiast for bicompartmental UKA for many years [3].
Another extension is to combine an ACL reconstruction with a UKA in the younger patient. The problem is that to perform an excellent ACL reconstruction, the tibiofemoral joint needs to be intact, and to gap balance a UKA needs an intact ACL. Care needs to be taken to ensure that the ACL tibial tunnel does not pass through the UKA tibial cut; the tunnel is placed closer to the midline. Bioabsorbable screws are better than metal ones, as there is a risk of fretting corrosion against the tibial metal (and galvanic corrosion with dissimilar metals). One method is to make the ACL tunnels first arthroscopically. The posterior horn of the meniscus can also be removed. The ACL graft (ideally hamstrings) is then passed and anchored on the femoral end. The UKA is then cemented. Finally, the ACL graft is tensioned and fixed at the tibial end. Since ACL graft rupture is a risk, it is advisable to consider a fixed-bearing UKA. In addition, for medial UKA plus ACL reconstruction, lowering the tibial slope protects the graft. In fact, a medial tibial slope set at 0° using a fixed-bearing UKA without ACL reconstruction is another method for managing the ACL ruptured knee and unicompartmental disease [2]. A point to consider with lateral UKA plus ACL reconstruction is that the femoral tunnel can act as a stress riser; care must be taken not to fracture the lateral condyle, especially with a patellar retractor.
It should be emphasised that these treatments may fail, and the patient runs the risk of needing to undergo revision to a TKA. The objective is to keep the knee as mobile and functional as possible.
14.5 Take-Home Message
Unicompartmental knee replacement is a procedure for the dedicated knee specialist. To obtain good results, the surgeon and the surgical team need to be performing the operation routinely. Patient selection is the most important factor for a good outcome. As Cartier has stated that after a UKA, you will see “a forgotten knee” in an enthusiastic patient [4].
References
Chawla H, Ghomrawi HM, van der List JP, Eggman AA, Zuiderbaan HA, Pearle AD. Establishing age-specific cost-effective annual revision rates for unicompartmental knee Arthroplasty: a meta-analysis. J Arthroplast. 2017;32:326–35.
Donell ST. Unicompartmental knee arthroplasty. In: Bentley G, editor. European instructional lectures, vol. 10. Berlin: Springer; 2010. pp. 159–165.
Heyse TJ, Khefacha A, Peersman G, Cartier P. Survivorship of UKA in the middle-aged. Knee. 2012;19:585–91.
Cartier P. Story of my passion. Knee. 2014;21:349–50.
Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71:145–50.
Deschamps G, Chol C. Fixed-bearing unicompartmental knee arthroplasty. Patients’ selection and operative technique. Orthop Traumatol Surg Res. 2011;97:648–61.
Thompson SA, Liabaud B, Nellans KW, Geller JA. Factors associated with poor outcomes following unicompartmental knee arthroplasty: redefining the “classic” indications for surgery. J Arthroplast. 2013;28:1561–4.
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2003;85:1968–73.
Price AJ, Dodd CA, Svard UG, Murray DW. Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br. 2005;87:1488–92.
Zuiderbaan HA, van der List JP, Chawla H, Khamaisy S, Thein R, Pearle AD. Predictors of subjective outcome after medial unicompartmental knee arthroplasty. J Arthroplast. 2016;31:1453–8.
Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Allaart CF, van Zeben D, Kerstens PJHazes JM, Zwinderman AH, Ronday HK, Han KH, Westedt ML, Gerards AH, van Groenendael JH, Lems WF, van Krugten MV, Breedveld FC, Dijkmans BA. Clinical and radiographic outcomes of four different treatment strategies in patients with early rheumatoid arthritis (the BeSt study): a randomized, controlled trial. Arthritis Rheum. 2005;52:3381–90.
Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87:999–1006.
Berend KR, Lombardi AV Jr, Morris MJ, Hurst JM, Kavolus JJ. Does preoperative patellofemoral joint state affect medial unicompartmental arthroplasty survival? Orthopedics. 2011;34:e494–6.
Ma T, Cai MW, Xue HM, Liu XD, Tu YH. Pre-operative assessment of the patellofemoral joint in unicompartmental knee replacement using Oxford phase III and its influence on outcome. Zhonghua Wai Ke Za Zhi. 2013;51:1010–5.
Thein R, Zuiderbaan HA, Khamaisy S, Nawabi DH, Poultsides LA, Pearle AD. Medial unicondylar knee arthroplasty improves patellofemoral congruence: a possible mechanistic explanation for poor association between patellofemoral degeneration and clinical outcome. J Arthroplast. 2015;30:1917–22.
Marya SK, Thukral R. Outcome of unicompartmental knee arthroplasty in octogenarians with tricompartmental osteoarthritis: a longer followup of previously published report. Indian J Orthop. 2013;47:459–68.
Niinimäki TT, Murray DW, Partanen J, Pajala A, Leppilahti JI. Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee. 2011;18:432–5.
Pietschmann MF, Wohlleb L, Weber P, Schmidutz F, Ficklscherer A, Gulecyuz MF, Safi E, Niethammer TR, Jansson V, Muller PE. Sports activities after medial unicompartmental knee arthroplasty Oxford III-what can we expect? Int Orthop. 2013;37:31–7.
van der List JP, Zuiderbaan HA, Pearle AD. Why do medial unicompartmental knee arthroplasties fail today? J Arthroplast. 2016;31:1016–21.
Cavaignac E, Lafontan V, Reina N, Pailhe R, Wargny M, Laffosse JM, Chiron P. Obesity has no adverse effect on the outcome of unicompartmental knee replacement at a minimum follow-up of seven years. Bone Joint J. 2013;95:1064–8.
Goodfellow J, O’Connor J. The anterior cruciate ligament in knee arthroplasty. A risk-factor with unconstrained meniscal prostheses. Clin Orthop Relat Res. 1992;276:245–52.
Pandit H, Beard DJ, Jenkins C, Kimstra Y, Thomas NP, Dodd CA, Murray DW. Combined anterior cruciate reconstruction and Oxford unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2006;88:887–92.
Boissonneault A, Pandit H, Pegg E, Jenkins C, Gill HS, Dodd CA, Gibbons CL, Murray DW. No difference in survivorship after unicompartmental knee arthroplasty with or without an intact anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2013;21:2480–6.
Mancuso F, Dodd CA, Murray DW, Pandit H. Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J Orthop Traumatol. 2016;17:267–75.
Mancuso F, Hamilton TW, Kumar V, Murray DW, Pandit H. Clinical outcome after UKA and HTO in ACL deficiency: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:112–22.
Khamaisy S, Zuiderbaan HA, van der List JP, Nam D, Pearle AD. Medial unicompartmental knee arthroplasty improves congruence and restores joint space width of the lateral compartment. Knee. 2016;23:501–5.
Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2004;423:161–5.
Vasso M, Del Regno C, D’Amelio A, Viggiano D, Corona K, Schiavone Panni A. Minor varus alignment provides better results than neutral alignment in medial UKA. Knee. 2015;22:117–21.
Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998;80:862–5.
Noticewala MS, Geller JA, Lee JH, Macaulay W. Unicompartmental knee arthroplasty relieves pain and improves function more than total knee arthroplasty. J Arthroplast. 2012;27(8 Suppl):99–105.
Zuiderbaan HA, van der List JP, Khamaisy S, Nawabi DH, Thein R, Ishmael C, Paul S, Pearle AD. Unicompartmental knee arthroplasty versus total knee arthroplasty: which type of artificial joint do patients forget? Knee Surg Sports Traumatol Arthrosc. 2017;25:681–6.
Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD. Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee. 2017;24:179–90.
Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L. Use of unicompartmental instead of tricompartmental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative. 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthop Scand. 1999;70:170–5.
Trieb K, Grohs J, Hanslik-Schnabel B, Stulnig T, Panotopoulos J, Wanivenhaus A. Age predicts outcome of high-tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2006;14:149–52.
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H. The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg Br. 2008;90:592–6.
Howells N, Salmon L, Waller A, Scanelli J, Pinczewski LA. The outcome at ten years of lateral closing-wedge high tibial osteotomy: determinants of survival and functional outcome. Bone Joint J. 2014;96:1491–7.
Fu D, Li G, Chen K, Zhao Y, Hua Y, Cai Z. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: a meta-analysis. J Arthroplast. 2013;28:759–65.
Gill T, Schemitsch EH, Brick GW, Thornhill TS. Revision total knee arthroplasty after failed unicompartmental knee arthroplasty or high tibial osteotomy. Clin Orthop Relat Res. 1995;321:10–8.
Spahn G, Hofmann GO, von Engelhardt LV, Li M, Neubauer H, Klinger HM. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:96–112.
Park CN, Zuiderbaan HA, Chang A, Khamaisy S, Pearle AD, Ranawat AS. Role of magnetic resonance imaging in the diagnosis of the painful unicompartmental knee arthroplasty. Knee. 2015;22:341–6.
Jacobs CA, Berend KR, Lombardi AV, Christensen CP. The location and severity of preoperative subchondral bone marrow lesions were not associated with inferior postoperative outcomes after medial unicompartmental knee arthroplasty or total knee arthroplasty. J Arthroplast. 2016;31:2476–80.
13th Annual Report of the National Joint Registry for England. Wales: Northern Ireland and the Isle of Man. 2016.
Deschamps G, Bussière C, Donell S. Fixed bearing unicompartmental knee prosthesis: results, complications, and technical considerations. In: Bonnin M, Amendola NA, Bellemans J, et al., editors. The knee joint: surgical techniques and strategies. Paris: Springer Verlag; 2012, pp. 669–684.
Lustig S, Elguindy A, Servien E, Fary C, Munini E, Demey G, Neyret P. 5- to 16-year follow-up of 54 consecutive lateral unicondylar knee arthroplasties with a fixed-all polyethylene bearing. J Arthroplast. 2011;26:1318–25.
Argenson JN, Parratte S, Bertani A, Flecher X, Aubaniac JM. Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res. 2008;466:2686–93.
van der List JP, McDonald LS, Pearle AD. Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee. 2015;22:454–60.
Lustig S, Lording T, Frank F, Debette C, Servien E, Neyret P. Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee. 2014;21(Suppl 1):S26–32.
Lustig S, Parratte S, Magnussen RA, Argenson JN, Neyret P. Lateral unicompartmental knee arthroplasty relieves pain and improves function in posttraumatic osteoarthritis. Clin Orthop Relat Res. 2012;470:69–76.
Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384:1437–45.
Beckmann J, Steinert A, Zilkens C, Zeh A, Schnurr C, Schmitt-Sody M. Patientenspezifische Instrumente und Implantate beim teilgelenkersatz des kniegelenkes (ConforMIS iUni, iDuo). Orthopade. 2016;45:322–30.
Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, Barrett A, Davies B. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88:188–97.
Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplast. 2012;27:803–8.
Hansen DC, Kusuma SK, Palmer RM, Harris KB. Robotic guidance does not improve component position or short-term outcome in medial unicompartmental knee arthroplasty. J Arthroplast. 2014;29:1784–9.
Thienpont E, Cartier P. Tricompartmental resurfacing arthroplasty with a follow-up of more than 30 years. Knee. 2014;21:875–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 ESSKA
About this chapter
Cite this chapter
Lustig, S. et al. (2018). Unicompartmental Knee Arthroplasty. In: Kerkhoffs, G.M.M.J., Haddad, F., Hirschmann, M.T., Karlsson, J., Seil, R. (eds) ESSKA Instructional Course Lecture Book. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-56127-0_14
Download citation
DOI: https://doi.org/10.1007/978-3-662-56127-0_14
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-56126-3
Online ISBN: 978-3-662-56127-0
eBook Packages: MedicineMedicine (R0)