Abstract
Atlantooccipital dislocation (AOD) or occipitoatlantal dislocation (OAD) is a rare but serious injury of the upper c-spine caused by a traumatic ligamentous disruption of the craniocervical junction. This injury usually occurs after high-energy/-velocity accidents and is associated with a high morbidity and a mortality rate of 20–30% amongst all traumatic c-spine injuries. It can be easily overlooked but needs to be considered especially after high-impact trauma and in field resuscitation. Once deemed fatal (in earlier days only 1/3 of patients reached the hospital alive), better emergency management and the widespread availability of CTs led to better on site survival and more frequent recognition and more timely diagnosis of this injury improving mortality rates and neurological outcome. This has in consequence led to an increasing incidence of this injury.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
1.1 Objective 1: OC Luxation (Difficulties in Assessment and Treatment, Prognosis)
Atlantooccipital dislocation (AOD) or occipitoatlantal dislocation (OAD) is a rare but serious injury of the upper c-spine caused by a traumatic ligamentous disruption of the craniocervical junction. This injury usually occurs after high-energy/-velocity accidents and is associated with a high morbidity and a mortality rate of 20–30% amongst all traumatic c-spine injuries. It can be easily overlooked but needs to be considered especially after high-impact trauma and in field resuscitation. Once deemed fatal (in earlier days only 1/3 of patients reached the hospital alive), better emergency management and the widespread availability of CTs led to better on site survival and more frequent recognition and more timely diagnosis of this injury improving mortality rates and neurological outcome. This has in consequence led to an increasing incidence of this injury [1].
This chapter will show a case of AOD with a typical trauma mechanism and typical clinical signs and symptoms. Aim of this case is to raise the sensitivity for this rare traumatic injury. Recognition of AOD requires experience and the awareness of the existence of this often times overlooked serious injury.
This case will detail the following problems such as:
-
recognition of this rare and potentially fatal injury
-
choice of imaging
-
management of this injury
At the end of this chapter the reader should be aware of the problems and pitfalls in recognition and treatment of AOD.
These injuries are classified according to Harris into three types:
-
Type I: Anterior dislocation of the occiput
-
Type II: Posterior dislocation of the occiput
-
Type III: Axial dislocation of the occiput
1.1.1 Case Description
A 53 y/o male construction worker fell headway from a scaffold of 3 m height. He was awake initially with no neurological deficit and referred to a tertiary peripheral hospital. There he soon developed respiratory insufficiency and a bilateral N. VI palsy. He was intubated on site and transferred to the ER of a level I trauma center.
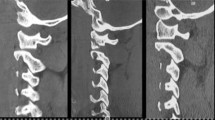
On presentation in the ER the patient was intubated, sedated and ventilated. Pupils were miotic and reactive to light. The cranial CT showed no signs of trauma, except for a traumatic subarachnoid hemorrhage in the craniocervical junction (Fig. 32.1). Sagittal reconstructions of the CT-angiogram revealed extension of the tSAH around the spinal cord of the entire c-spine (Fig. 32.2). Trauma mechanism and neurological deterioration of the patient with respiratory insufficiency and bilateral N. VI palsy raised the suspicion of an injury of the occipitocervical junction. On closer inspection of the CT-scan revealed the AOD (Fig. 32.3). MRI was performed immediately confirming AOD (Fig. 32.4).
Harris classification [2]
The patient received surgery with posterior occipitocervical fixation from the occiput with an occiput plate to C2–3 with C2 isthmic and C3 lateral mass screws the same day (postop CT-scan Fig. 32.5).
After surgery the patient was weaned from the ventilator and could be extubated within the next days. He had no new neurological deficit. The N. VI palsy was remitting over the next few weeks. Two weeks after admission the patient experienced a sudden onset of severe dyspnea and cardiac arrest needing CPR and emergency intubation. Pulmonary CT showed a fulminant pulmonary embolism leading to the subsequent death of the patient (Fig. 32.6).
1.1.2 Discussion of the Case
1.1.2.1 Clinical and Radiological Assessment
The greatest difficulty in AOD is the timely recognition and treatment of this traumatic c-spine injury. This is necessary, because it is a purely ligamentous lesion with subtotal or total rupture of the occipitocervical ligaments which is highly unstable and therefore life-threatening. Clinical assessment of these patients usually is difficult or impossible since the majority lose consciousness, are cardiopulmonary unstable and need intubation at the trauma site. In field resuscitation or a comatous patient are therefore highly suggestive for AOD, especially after high impact trauma and a patient of younger age. Visible signs of hyperflexion or -extension injuries such as lacerations of the back of the head or forehead are more signs suggesting AOD.
When suspecting AOD it is imperative to avoid any unnecessary movement of the patient, especially any extension manoeuvre that can cause neurological deterioration in up to 10%. We recommend performing early CT and MRI of the cranium and the c-spine with CTA and / or MRA especially of the carotid arteries to rule out dissections.
1.1.2.2 Indication
Since AOD must be considered a highly unstable ligamentous injury, early fixation is necessary.
1.1.2.3 Choice of Treatment
These injuries need to be fixed immediately. Treatment with internal fixation and fusion is recommended.
1.1.2.4 Accordance with the Literature Guidelines
Our treatment is accordance with the treatment guidelines of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons.
1.1.2.5 How Strong is the Level of Evidence Available to Date
Current recommendations in adults are based on level III evidence with regard to diagnostics and treatment.
For pediatric patients there is a level I recommendation for CT imaging to determine the condyle-C1-interval.
Pearls and Pitfalls
-
Early and timely recognition and surgery are crucial for this potentially fatal injury.
-
Look out for indirect signs of AOD such as:
-
Trauma mechanism (hyperextension/flexion injury)
-
High energy trauma
-
Patient age (ligamentous injuries predominant in younger patients)
-
tSAH in the craniocervical junction on CT as an indirect sign of ligamentous disruption of the craniocervical junction
-
In field resuscitation as an indirect sign of a high-energy trauma and traumatic lesion of the craniocervical junction with affection of the brainstem.
-
-
Not only look for osseous lesions, but also look for ligamentous lesions, which are hard to detect on CT or x-ray.
-
Always check alignment, i.e. check for pathological condyle-C1-interval (CCI), atlanto-dental interval (ADI)
-
Traction is not recommended in AOD. Be careful with cervical orthosis or any other cervical immobilization device. They might exert traction leading to neurological deterioration with a potentially fatal outcome.
1.2 Objective 2: C2 Fracture (Treatment Options Surgical/Problems with Halo)
C2 injuries comprise of fractures of the odontoid, traumatic spondylolisthesis and atypical axis fractures.
In this chapter we will discuss a case of a traumatic odontoid fracture (tOF) since these are the most frequent injuries of the c-spine (10–15%). The frequency of tOFs increases with age.
They are classified into three types according to Anderson and D’Alonzo [3]:
- Type I: :
-
Fracture through the tip; unstable
- Type II: :
-
Fracture through the base of neck; usually unstable
- Type IIA: :
-
Comminuted type II fracture; usually unstable
- Type III: :
-
Fracture through body of C2; usually stable
or according to Grauer (Fig. 32.7):
- Type I: :
-
Fracture through odontoid tip
- Type IIA: :
-
Transverse fracture line through base of neck, non-displaced
- Type IIB: :
-
Anterior-superior to posterior-inferior fracture line or displaced type II fracture
- Type IIC: :
-
Anterior-inferior to posterior-superior fracture line or comminuted type II fracture
- Type III: :
-
Fracture including at least one of the superior articular C2 facets
Type I fractures with avulsion of the alar ligaments are very rare. Type II fractures are the most frequent tOF.
In younger patients the trauma mechanism usually is a high impact/velocity trauma after a fall from great height or after a motor vehicle accident. In contrast the trauma mechanism in elderly patients usually is a low energy trauma, such as a simple fall in a domestic environment.
Therefore the fatality at the time of accident in younger patients is reported to range between 25% and 40%, whereas there is basically no reported mortality in elderly patients. Eighty percent of patients with type II fractures are neurologically intact, 10% have a minor and 10% a significant neurological deficit. The main complaint usually is neck pain.
This case will detail the following problems concerning the treatment modality (conservative vs. surgical management) with regard to:
-
age and bone quality
-
fracture type and anatomical conditions
-
surgical technique
-
factors affecting outcome and morbidity and mortality
At the end of this chapter the reader should be aware of the problems and pitfalls in the treatment of tOF, especially with regard to age (young vs old patient).
1.2.1 Case Description
A 45-year old male patient fell from a ladder from approximately 4 m height. He was uncconscious shortly and complained of severe neck pain on regaining consciousness. He was brought to the ER awake and without neurological deficit. A CT scan of the cervical spine showed a non-dislocated traumatic odontoid fracture type IIB (Fig. 32.7). An MRI confirmed the acute type IIB tOF (STIR weighted MRI) and ruled out any further discoligamentous injuries (Fig. 32.8).
The patient was immobilized in a hard collar and received surgery with an anterior odontoid screw fixation in Böhler technique using biplanar c-arm fluoroscopy within 7 days after trauma (Figs. 32.9 and 32.10). Surgery was uneventful. The hard collar was removed and the patient was mobilized the next day. The postoperative CT scan showed correct fracture alignment and a correct position of the anterior odontoid lag screw (Fig. 32.11). The patient was discharged on the second postoperative day with improved neck pain (VAS 3/10) and without neurological deficit.
1.2.2 Discussion of the Case
1.2.2.1 Indication
Type II fractures are the most common tOF. Since these fractures are usually unstable they need to be immobilized. There is still an ongoing debate concerning the treatment modality especially in elderly patients, which is being investigated in an ongoing prospective European multicentre trial (INNOVATE Trial). Treatment options vary from conservative treatment with a hard collar or halo vest to surgical treatment via anterior approaches such as anterior transarticular C1/2 fixation, an anterior odontoid screw fixation or a combination of both techniques with one or two odontoid screws to posterior fixations such as posterior transarticular C1-C2 fixation in Magerl technique [11] (Fig. 32.12a) or posterior C1 lateral mass-C2 isthmic or pedicle screw fixation in Harms-Goel technique with a polyaxial screw rod system [9, 10] (Fig. 32.12b).
Posterior transarticular C1-C2 fixation technique after Magerl (a, left); posterior C1-C2 fixation technique after Harms-Goel (b, right). (Courtesy of AOSpine) (Source: AO Surgery Reference, www.aosurgery.org) (© Copyright by AO Foundation, Switzerland)
1.2.2.2 Choice of Treatment
There is no class I evidence on how to treat tOF. Class II evidence recommends surgery for type II tOF in elderly patients ≥50 years of age. A prospective multicenter trial was able to significantly improve functional outcome, increase fusion rate and reduce mortality in surgically treated elderly patients. Also the nonunion rate is reported to be 21-times higher in patients ≥50 years of age compared to younger patients if treated conservatively [5, 6]. Therefore for these patients surgery is recommended with a strong recommendation for posterior fixation [7]. Class III evidence indicates that factors such as patient age, fracture type/displacement, secondary loss of reduction and delayed treatment are associated with nonunion [5]. Immobilization in a halo vest can be administered in non-displaced type II fractures. However, it is associated with a high mortality rate of up to 40% in elderly patients [8]. Surgery should be considered in displaced fractures of ≥5 mm, comminuted fractures or inability to achieve or maintain fracture alignment with external immobilization [5]. Fusion rates are reported to be >90% for anterior and posterior surgical fixations alike. However, there are some contraindications concerning some surgical techniques. Whereas the Harms-Goel technique is universally applicable for any kind of tOF in any patient even in displaced fractures, which can be openly reduced during surgery, the Magerl technique is unsuitable in displaced fractures or patients with a kyphotic thoracic spine since the entry point for the drill is approximately at the level of Th1. Also the rate of vertebral artery injuries is reported to be higher than with the Harms-Goel technique.
Anterior odontoid screw fixation (AOSF) is a relatively easy and minimally-invasive technique. However, it is not suitable in patients with barrel chest, thoracic kyphosis or patients with a very short neck, in osteoporosis or reduced bone mineral density and in type IIC fractures. If these factors are not taken into account prior to surgery, the failure rate can be as high as 36% (loss of correction, non-union, delayed fusion, pseudarthrosis) and is associated with an increased risk of postoperative dysphagia and pneumonia in elderly patients. Therefore we recommend using this technique only in patients <50 years of age with good bone quality and non-displaced type IIA and IIB fractures.
1.2.2.3 Why Were Things Done this Way
This patient had a non-displaced type IIB fracture and his age was below 50 years of age. Therefore we decided to treat him surgically with an anterior odontoid screw fixation (AOSF).
Our treatment recommendation for tOF is:
Type I: External immobilization |
Type II: Younger patient with type IIA or non-displaced type IIB: |
Anterior odontoid screw fixation |
Older patient or type IIC: |
Posterior atlantoaxial fixation |
Type III: Stable: External immobilization |
Unstable: Atlantoaxial fixation |
1.2.2.4 Accordance with the Literature Guidelines
Our treatment is accordance with the treatment guidelines of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons.
1.2.2.5 How Strong is the Level of Evidence Available to Date
Current recommendations are based on level II and III evidence.
2 Conclusions and Take Home Message
Surgery should be considered in unstable type II and III odontoid fractures. AOSF should be restricted to younger patients with normal bone mineral density and non-displaced type IIA + B fractures. There is growing evidence that elderly patients benefit from surgery compared to conservative treatment with a strong recommendation for posterior C1-C2 fixation.
Pearls and Pitfalls
-
Type II odontoid fractures are the most common c-spine fractures
-
Elderly patients seem to benefit from surgery compared to conservative management with regard to functional outcome, quality of life, mortality and fusion rate
-
There is a strong recommendation for posterior C1-C2 fixation in elderly patients
-
The Harms-Goel technique is universally applicable in any odontoid fracture type
-
The Magerl technique is unsuitable in displaced fractures and certain anatomical conditions (thoracic kyphosis, high riding vertebral artery)
-
AOSF should preferably applied in younger patients with non-displaced fractures (type IIA and IIB) and good bone quality
-
AOSF is contraindicated in osteoporosis and comminuted fractures or fracture lines ascending from anterior-inferior to posterior-superior
-
Osteoporosis is the most important risk factor for tOF in the elderly [12]
-
tOF in the elderly are associated with higher failure and higher morbidity and mortality rates irrespective of the treatment modality
2.1 Objective 3: Isolated C1 Ring Fracture
Atlas fractures account for approx. 3–13% of c-spine fractures. About 56% are isolated C1 ring fractures, 44% are combined C1-C2 fractures. Typical Jefferson fractures with combined fractures of the anterior and posterior C1 ring are found in one third of patients.
Approx. 9% have additional other c-spine fractures and 21% have associated head injuries.
The typical trauma mechanism is axial loading by jumping headfirst into shallow water or falls directly on the cranial vertex. Patients are usually neurologically intact.
C1 ring fractures are classified after Gehweiler et al. [13] (Fig. 32.13):
-
Type 1: Isolated anterior ring fracture
-
Type 2: Isolated posterior ring fracture
-
Type 3: Combined anterior and posterior ring fracture “Jefferson fracture”
-
3a: Intact transverse atlantal ligament (TAL) (stable)
-
3b: Disrupted TAL (unstable)
-
-
Type 4: Isolated lateral mass fracture (rare)
-
Type 5: Isolated transverse process fracture (very rare)
Gehweiler classification of atlas fractures. Gehweiler type 3a = stable Jefferson fracture; Gehweiler type 3b = unstable Jefferson fracture (from [17])
The most relevant fractures are the combined anterior and posterior C1 ring fractures type 3b better known as Jefferson fractures. It is crucial to assess the integrity of the transverse atlantal ligament (TAL) because its integrity determines whether a type 3 fracture is stable (type 3a, TAL intact) or unstable (type 3b, TAL disrupted).
Type 3b fractures are further classified after Dickmann et al. [14] (Fig. 32.14):
-
Type IA: Interligamentous central TAL lesion
-
Type IB: Interligamentous TAL lesion near the lateral mass
-
Type IIA: Isolated osseous TAL avulsion
-
Type IIB: Osseous TAL avulsion with lateral mass fracture (Gehweiler type 4)
Dickmann classification of transverse atlantal ligament (TAL) lesions (from [17])
Treatment of isolated C1-ring fractures therefore mainly depends on the integrity of the transverse atlantal ligament (TAL). A non-displaced atlas fracture with an intact TAL might be treated by immobilization alone, while all other atlas fractures should be treated surgically. C1-ring osteosynthesis should be considered in dislocated atlas fractures with intact or non-displaced osseous avulsion of the TAL. In displaced and/or intraligamentous TAL rupture an atlantoaxial fusion should be performed (see flowchart Fig. 32.19).
In combined C1-C2 fractures the C2 fracture type dictates the treatment modality (s. C2 fractures).
The purpose of this case is to delineate the importance and difficulties to adequately diagnose and treat C1 fractures with regard to:
-
adequate diagnostic imaging
-
correct classification
-
treatment options
-
the importance of the integrity of the transverse atlantal ligament (TAL)
Adequate diagnostic clinical and imaging work-up is essential to assess potentially unstable C1 fractures which are solely determined by the integrity of the transverse atlantal ligament (TAL). TAL integrity is also the main factor in decision-making as to which treatment modality should be applied.
At the end of this chapter the reader should be aware of the problems and pitfalls in the correct classification and treatment of isolated C1 fractures.
2.1.1 Case Description
A 25 y/o female fell on her head while tussling with her 5 y/o son. She presented to her GP for neck pain (VAS 7/10) who prescribed oral pain medication. Due to persisting neck pain despite oral analgesics she admitted herself to the ER 1 week after trauma. Because of her young age it was decided to perform plain as well as flexion/extension radiographs instead of a CT scan to minimize radiation exposure. Radiographs revealed an atlantoaxial instability with an increased atlanto-dental interval (ADI) of >3 mm (Fig. 32.15). On presentation she fortunately was neurologically intact and provided with a cervical orthosis. To properly assess the extent of osseous and ligamentous injury to the atlantoaxial complex a CT scan and MRI with STIR-weighted images were necessary which confirmed a right-sided Jefferson burst fracture (anterior and posterior ring) with osseous avulsion of the transverse atlantal ligament (TAL) (Gehweiler type 3b/Dickmann type IIB) and slight displacement of the odontoid peg (Figs. 32.16 and 32.17). A posterior C1-ring osteosynthesis was performed. Surgery was uneventful and the patient could be discharged from hospital without a cervical orthosis with improved neck pain (VAS 3/10) on the second postoperative day. Postoperative a.p. and lateral radiographs showed correct alignment of the atlantoaxial complex and correct positioning of the osteosynthesis material (Figs. 32.18 and 32.19).
2.1.2 Discussion of the Case
2.1.2.1 Why Were Things Done this Way
This patient had a C1-ring fracture Gehweiler type 3b, Dickmann type IIB equalling an unstable fracture with an osseous TAL avulsion. Therefore she was treated with a C1-ring osteosynthesis.
2.1.2.2 Were they in Accordance with the Literature Guidelines
Our treatment is accordance with the treatment guidelines of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons.
2.1.2.3 How Strong is the Level of Evidence Available to Date
3 Conclusions and Take Home Message
Assessment of the integrity of the transverse atlantal ligament (TAL) is crucial in the decision making for treatment of isolated C1-ring fractures. MRI imaging with STIR-sequences is essential to properly assess TAL and other ligamentous injuries. Flexion/extension radiographs might be helpful to confirm instability in cases with indistinct MRI findings.
Pearls and Pitfalls
-
Integrity assessment of the TAL is crucial for treatment decision
-
MRI and if needed flexion/extension radiographs should be performed to assess TAL integrity and other discoligamentous injuries
-
An atlanto-dental interval (ADI) of >3 mm is an indirect sign of atlantoaxial instability
-
C1 fractures Gehweiler type 3a with an intact TAL can usually be treated with external immobilization
-
C1 fractures Gehweiler type 3b with a disrupted TAL can be treated with a halo orthosis. However, the reported morbidity and mortality especially in the elderly is considerably high, therefore surgical fixation might be the superior treatment option
Editorial Comment
This is highly recommended reading regarding modern concepts of upper cervical spine trauma. Especially the motion-preserving osteosynthesis of unstable isolated C1-ring fractures and the fact that a posterior Harms/Goel construct is the surgical treatment of choice for odontoid fractures in the elderly.
References
Level of Evidence II (Diagnosis)/III (Treatment)
Theodore N, Aarabi B, Dhall SS, et al. The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery. 2013;72(Suppl 2):114–26.
Kandziora F, Schnake K, Hoffmann R. Injuries to the upper cervical spine. Part 1: Ligamentous injuries. Unfallchirurg. 2010;113:931–43.
Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74.
Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5(2):123–9.
Ryken TC, Hadley MN, Aarabi B, et al. Management of acute combination fractures of the atlas and axis in adults. Neurosurgery. 2013;72(Suppl 2):151–8.
Vaccaro AR, Kepler CK, Kopjar B, et al. Functional and quality-of-life outcomes in geriatric patients with type-II dens fracture. J Bone Joint Surg Am. 2013;95(8):729–35.
Harrop JS, Hart R, Anderson PA. Optimal treatment for odontoid fractures in the elderly. Spine (Phila Pa 1976). 2010;35(21 Suppl):S219–27.
Majercik S, Tashjian RZ, Biffl WL, et al. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59(2):350–6; discussion 356–8.
Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001;26:2467–71.
Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir. 1994;129:47–53.
Magerl F. Spondylodesis of the upper cervical spine. Acta Chir Austriaca. 1982;43(Suppl):69.
Käsmacher J, Schweizer C, Valentinitsch A, et al. Osteoporosis is the most important risk factor in traumatic odontoid fractures in the elderly. J Bone Miner Res. 2017;32(7):1582–8.
Level of Evidence III
Gehweiler JA, Osborne RH, Becker RF. The radiology of vertebral trauma. Philadelphia: Saunders; 1983.
Dickmann CA, Greene KA, Sonntag VK. Injuries involving the transverse atlantal ligament: classification and treatment guidelines based upon experience with 39 injuries. Neurosurgery. 1996;38:44–50.
Hadley MN, Walter PC, Grabb PA, et al. Isolated fractures of the atlas in adults. In: guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery. 2002;50(3 suppl):S120–4.
Ryken TC, Aarabi B, Dhall SS, et al. Management of isolated fractures of the atlas in adults. Neurosurgery. 2013;72(Suppl 2):127–31.
Kandziora F, Schnake K, Hoffmann R. Injuries to the upper cervical spine. Part 2: Osseous injuries. Unfallchirurg. 2010;113:1023–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ryang, YM. (2019). Upper Cervical Spine Trauma. In: Meyer, B., Rauschmann, M. (eds) Spine Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-98875-7_32
Download citation
DOI: https://doi.org/10.1007/978-3-319-98875-7_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98874-0
Online ISBN: 978-3-319-98875-7
eBook Packages: MedicineMedicine (R0)