Abstract
Conducting a literature review on contrast-enhanced digital mammography (CEDM) is not easy due to the variety of abbreviations and acronyms referring to this procedure and due to the limited articles available in international biomedical databases (less than 100 to date). Among the most notable limitations of CEDM studies are their heterogeneity and sampling design, as well as their small sample population sizes. We focused on the dual-energy technique, as the temporal subtraction technique has become obsolete. The majority of studies conducted were concerned with assessing sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV); the key focus of many studies was comparison among CEDM, full-field digital mammography (FFDM) and magnetic resonance imaging (MRI) in terms of accuracy and diagnostic performance in breast imaging. CEDM showed an increase in diagnostic performance over FFDM alone, was comparable to MRI in terms of sensitivity and NPV and had a higher specificity and higher PPV. In addition, CEDM was examined as an additional imaging tool for problem-solving associated with suspicious lesions detected by conventional imaging techniques, such as microcalcifications, architectural distortions and the evaluation of dense breasts, with very promising results. Finally, we analysed the average glandular dose (AGD), and all results obtained were below the limits set by the regulations of the Mammography Quality Standards Act, thus positioning CEDM as a new valuable diagnostic technique in breast imaging.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Sensitivity
- Specificity
- PPV
- Problem-solving
- Dual energy
- LE CEDM
- Average glandular dose (AGD)
- MRI
- FFDM
- Microcalcifications
- Architectural distortions (AD)
1 Introduction
The first bibliographical approach to contrast-enhanced mammography may be complicated by the variety of abbreviations and acronyms referring to this procedure, such as CESM (contrast-enhanced spectral mammography), CEDM (contrast-enhanced digital mammography), dual-energy mammography, TCEM (temporal contrast-enhanced mammography) and CEM (contrast-enhanced mammography).
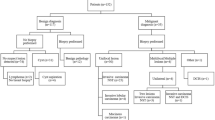
To date, there are fewer than 100 CEDM studies published in medical journals in the most important international biomedical databases. These studies are very heterogeneous in terms of their different methodologies, few being prospective studies, while the majority were retrospective and were performed on small population samples.
The sampling design in CEDM leads to an increased risk of bias, because it is a diagnostic examination given to an ultra-selected population with a high prevalence of disease, thus misrepresenting the pretest probability of suffering from breast cancer.
From the beginning, two procedures have been described: one approach involving temporal subtraction known as temporal contrast-enhanced mammography (TCEM) and a new approach, which has replaced the first, based on dual-energy subtraction known as contrast-enhanced digital mammography (CEDM).
In TCEM, the temporal subtraction technique consists of the acquisition of high-energy single images in a single projection before and after contrast medium injection, at an interval of 1 minutes. The pre-contrast image is then subtracted from the post-contrast image, offering the possibility of kinetic analysis of the enhancement pattern of breast lesions, similar to breast MRI. Unfortunately, many studies demonstrated that this first technical approach had a variety of issues, one of the most important being the long duration of breast compression, which led to patient discomfort and to altered perfusion of the contrast medium for vascular stasis, which did not permit the enhancement of some hyper-vascularized lesions. Another disadvantage was the ability to study only one breast at a time in a unilateral manner with each single projection.
Currently, TCEM has been replaced by CEDM. The dual-energy technique consists of the acquisition of a pair of low-energy images (25–33 peak kilovoltage; kVp) with silver (Ag) or rhodium (Rh) filters and high-energy images (45–49 kVp) with copper filters (Cu) only after contrast medium injection. The recombined image, which contains information on the iodine distribution, is produced from the spectral subtraction of these images. The acquisition of CEDM images starts 2 minutes after the intravenous administration of iodinated contrast medium and is completed within 8 minutes. During these 6 minutes, the high-energy (HE) and low-energy (LE) coupled images are obtained with craniocaudal (CC) and mediolateral oblique (MLO) projections of each breast. The main advantage of the dual-energy technique is the ability to study bilateral breasts in all the four mammographic projections; this also allows better visualization of contrast enhancement because breast compression occurs just 2 minutes after injection of the iodinated agent, thus reducing patient discomfort.
2 Literature Review of the Diagnostic Accuracy of CEDM
From a “historical” point of view, although it may appear to be a relatively new technique in breast imaging, CEDM was first studied and performed more than 10 years ago. Lewin et al. published the first introductory study of the feasibility in 2003; the authors performed CEDM on 26 patients with suspected breast lesions detected by full-field digital mammography (FFDM), acquiring images from just a single MLO projection. They identified 13 invasive carcinomas, 11 of which demonstrated intense contrast enhancement. After this study, CEDM was defined as a promising and research-worthy new tool for breast imaging [1].
It has been 15 years since the introduction of this technique, and many more studies investigating CEDM have been published since then, evaluating both the sensitivity and specificity. According to an accurate literature analysis, the sensitivity of CEDM varies from 86 to 100%, which are very high values with elevated agreement and homogeneity between studies (Table 5.1, Fig. 5.1).
The results concerning the specificity of CEDM are discordant, with variable values. This may be attributed to the intrinsic features of different studies, which are very heterogeneous with small population samples and insufficient initial familiarity of radiologists with this new technique (Table 5.1, Fig.5.2).
3 CEDM in Comparison with FFDM Alone and FFDM + US
Lobbes et al. [2] demonstrated that CEDM is an excellent tool for problem-solving. In this study, two radiologists examined 113 patients referred for CEDM from screening, due to suspicious lesions identified by FFDM. They observed that the diagnostic performance was higher with CEDM than with FFDM. When CEDM was compared with FFDM, CEDM was found to have 100% (+3%) sensitivity, 88% (+46%) specificity, 76% (+37%) positive predictive value (PPV) and 100% (+3%) negative predictive value (NPV). In particular, CEDM was demonstrated to be very useful for improving specificity, thus reducing the number of false-positive cases.
Another very interesting result was the high NPV, suggesting that the absence of contrast enhancement excluded breast malignancies.
In a follow-up study, Lalji et al. [3] obtained similar results where 10 radiologists with different levels of experience in CEDM retrospectively examined 199 patients referred from screening. CEDM presented, in comparison to FFDM, a sensitivity of 97% (+4%) and a specificity of 70% (+34%). These data confirmed Lobbes’ first observations, and they also demonstrated that CEDM has hardly any learning curve, making its implementation into daily clinical practice safe and feasible.
In a meta-analysis, Tagliafico et al. [4] reviewed all studies on CEDM sensitivity and specificity using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) system [5], which consists of a checklist of 27 items that act as eligibility criteria.
Out of 643 studies inspected, only eight studies met the 27 criteria and were included in the review. Of these eight studies, four were prospective and four were retrospective studies.
The authors obtained values of 98% for sensitivity and approximately 58% for specificity, including three studies with values below 40%, which is not acceptable in clinical practice.
The limitations and pitfalls of this review were the heterogeneity (prospective and retrospective) of the eight studies, which included the fact that three of the studies were from the same working group (Luczynska) and that specificity was evaluated in only six of the studies, while sensitivity was evaluated in all eight studies.
Another limitation was the risk of bias in the population sampling, as stated above. However, the study by Lobbes et al. [2] was considered to have a reasonably low risk of bias because it was a prospective study, which included patients from screening programmes.
Since low-energy CEDM images present the same physical characteristics (same KVp) as FFDM, some studies [6,7,8] have focused on comparing the CEDM low energy and FFDM images to demonstrate their equivalence in terms of diagnostic accuracy.
These studies agreed that there are no statistically significant differences between low-energy images and FFDM.
In particular, the aim of the study by Lalji et al. [6] was to evaluate the quality of low-energy (LE) CEDM images and compare them with FFDM, following the 20 EUREF criteria.
Two independent expert radiologists observed 147 cases of FFDM and LE CEDM images. No statistically significant differences were observed in the quality scores of the two images for 17 out of 20 criteria, thus indicating that the LE CEDM images were just as accurate as FFDM images.
In a study by Fallenberg et al. [7], CEDM alone had the same sensitivity as CEDM + FFDM with just a 6.2% increase in average glandular dose (AGD). The author suggests that when CEDM is available, FFDM can be avoided, resulting in 61% reduction of the radiation dose, particularly in women with dense breasts.
Based on these results, Tennant et al. [9], proposed have proposed to use LE CEDM images as the first line of examination in patients with palpable masses to reduce radiation exposure.
Five radiologists retrospectively evaluated 100 CEDM exams, initially analysing just the LE images and then the recombined images 3 weeks after the full exam.
ROC analysis showed an improved overall performance of CEDM over LE CEDM alone, with an area under the curve of 0.93 versus 0.83. CEDM showed increased sensitivity (95% versus 84%) and specificity (81% versus 63) compared to LE CEDM alone, with all five readers showing improved accuracy.
Tumour size estimation with CEDM was significantly more accurate than with LE CEDM alone, the latter tending to undersize lesions. In 75% of cases, CEDM was regarded as a useful or significant aid in diagnosis.
Although this study was run as a double-blinded experiment, all five readers knew that patients were symptomatic and that lesions were large in size, thus leading to a minimum risk of bias.
Regarding the indications for CEDM, EUSOBI [10] (European Society of Breast Imaging) states that “On the basis of still preliminary results, CEDM can be considered as an alternative to contrast-enhanced MRI in the case of contraindications to MRI (including the presence of MRI-unsafe devices in the patient’s body, claustrophobia and obesity preventing the patient from entering the magnet) or to gadolinium-based contrast injection as well as local conditions of difficult MRI availability due to interesting results obtained by comparing CESM and MRI in the same patients”. Therefore, CEDM shares the same potential clinical indications as MRI.
In a study by Cheung et al. [11], they inferred that CEDM might be used as a valid device for the evaluation of calcifications. In this study, 59 women with suspicious microcalcifications (BI-RADS 4) without an associated mass, referred from screening, were analysed to verify the potential correlation between the type of suspicious microcalcification and contrast enhancement.
In total, 37 microcalcifications (amorphous microcalcifications) were classified as low concern and 22 as intermediate (20 pleomorphic microcalcifications) or high concern (two linear microcalcifications).
Of the 59 microcalcifications, 22 were diagnosed as cancers, 19 were atypical lesions, and 18 were benign lesions (Table 5.2).
When microcalcifications were classified as high concern, they were more likely to demonstrate enhancement in CEDM. However, the presence of enhancement was not inevitably suggestive of malignancy, because benign microcalcifications may also show contrast enhancement.
Ten of the 37 amorphous microcalcifications had associated enhancement; five were diagnosed as cancerous and five as non-cancerous. Of the 22 intermediate- and high-risk microcalcifications, 16 (15 cancerous, 1 non-cancerous lesion) showed enhancement (Fig. 5.3).
Of the 22 pleomorphic microcalcifications, 16 showed brilliant enhancement in CEDM, out of which 15 were histologically proven to be malignant lesions. Of the 37 amorphous microcalcifications, only 10 showed enhancement, out of which 5 were histologically proven to be malignant lesions. This result shows a strong correlation between pleomorphic calcifications and malignancy, especially if the lesions present as enhancement on CEDM
The true positive rate of intermediate- and high-concern microcalcifications was significantly higher than that of low-concern lesions (93.75% vs. 50%). Overall, the diagnostic sensitivity of enhancement was 90.9%, with 83.78% specificity, 76.92% positive predictive value, 93.94% negative predictive value and 86.4% accuracy.
The potential bias of this study is based on the small number of cases and patient sample size. Subsequently, Cheung and colleagues [12] conducted a study with a larger cohort, enrolling 94 patients, thus confirming their previous results.
CEDM can also be used as an efficient diagnostic tool for the evaluation of architectural distortions detected by FFDM or tomosynthesis. Suspicious mammographic distortions with contrast enhancement in CEDM are worthy of further histological characterization, whereas the absence of enhancement may prevent unnecessary biopsies.
The retrospective study done by Bhavika Patel et al. on 45 women with 49 distortions [13] was among the most significant study to date for this indication, despite its limitation of a small sample population size.
The authors observed that architectural distortions (AD) detected by tomosynthesis and showed contrast enhancement on CEDM were more often associated with the presence of malignant lesions; thus, contrast media allows us to better characterize suspicious findings, increasing the sensitivity and specificity.
Thirty-seven (75.5%) ADs exhibited associated enhancement, with a resulting PPV of 78.4% (29/37), sensitivity of 96.7% (29/30), specificity of 57.9% (11/19) and NPV of 91.7% (11/12). The false-positive rate was 21.6% (8/37), and the false-negative rate was 8.3% (1/12). The accuracy was 81.6% (40/49) (Fig. 5.4).
The high sensitivity and NPV of CEDM in patients with AD are very promising for the diagnosis of malignancy and thereby avoiding unnecessary biopsies, respectively.
4 CEDM in Dense Breasts
As already discussed in chapter 2 by Vincenzo Lattanzio, it is a well-known fact that increased breast parenchymal density is the main limitation of FFDM as a diagnostic test. To solve this problem, we compared FFDM findings with other imaging modalities such as ultrasonography, tomosynthesis and MRI. CEDM is a promising additional tool for radiologists to overcome the difficulties associated with interpretation of very dense breasts.
Fallenberg et al., conducted a study on this topic [7], in which they compared the sensitivity of FFDM, CEDM and the combination of FFDM + CEDM.
The final outcome showed a better sensitivity for CEDM than FFDM in dense breasts (93% vs. 72%), and similar values were obtained for CEDM in the comparison with the combined examination of FFDM + CEDM (94%). CEDM was proposed as an alternative, first-line examination to study dense breasts (Table 5.3).
Since then, there are other studies that have verified Fallenberg’s results. In a study by Mori et al. [14], the authors suggested that CEDM offers better clinical performance than FFDM. The use of CEDM may decrease false-negative cases, especially for women with dense breasts. A total of 143 breasts on 72 women who underwent CEDM and FFDM were analysed, and 58 (40.6%) of 143 breasts were diagnosed with breast cancer based on histopathology.
CEDM revealed eight false-negative cases among 58 breast cancer cases (sensitivity of 86%) and five false-positive cases (specificity of 94%). The accuracy of CEDM was 91%.
FFDM was found to detect 31 true-positives among 58 breast cancer cases (sensitivity of 53%) and false-positives in 12 cases (specificity of 86%). FFDM missed malignancies in 27 breasts. Of these 27 cases missed on FFDM, 25 of them were dense breasts, in which 20 (80.0%) were found to be positive on CEDM (Table 5.4).
Cheung et al. [15] analysed 100 lesions (72 breast malignancies and 28 benign lesions) in 89 females. The use of CEDM in their study improved cancer diagnosis compared to FFDM in terms of sensitivity (71.5–92.7%) and specificity (51.8–67.9%) (Table 5.4).
CEDM is also a valuable tool for problem-solving in cases of inconclusive findings on conventional imaging. Tardivel et al. [16] retrospectively subjected 195 patients with inconclusive lesions detected by conventional imaging to undergo a CEDM examination. Contrast agent allowed the authors to identify and characterize new lesions. Out of the 195 cases, 41 patients (21%) modified their therapeutic plan with more extensive surgery (n = 21) or neoadjuvant chemotherapy (n = 1), while unnecessary biopsy was avoided in the 20 patients with negative CEDM findings. The use of CEDM improved cancer diagnosis compared with conventional imaging based on the higher sensitivity (94%) and specificity (74%), with the PPV and NPV being at 91% and 81%, respectively. CEDM can easily be performed as a clinical assessment after positive breast cancer screening and may significantly change the diagnostic and treatment strategy through breast cancer staging.
Another important factor evaluated in the literature is the average glandular dose (AGD) absorbed in CEDM. Fallenberg et al. [7] obtained rather interesting results, where they observed that in very dense breasts (ACR4), the AGD of CEDM was significantly lower than that of FFDM (Table 5.5).
Fallenberg’s explanation of this result was “At equal thickness under compression, a dense breast will absorb more in the upper parts (closer to the tube) and ‘shields’ the lower parts in a way. To still have a reasonable number of photons at the detector level, one way is to compensate by increasing kVp, which lowers the absorbed dose. AGD for a 100% glandular breast is estimated to be 20% lower than for a 50/50 glandular breast; the latter absorbs 20% less than a 0% glandular breast”.
Conversely, James et al. [17] demonstrated how AGD increases with very dense breasts in phantoms and patients with varying breast thickness and density. Non-dense phantoms had a mean AGD of 1.0 mGy with 2D FFDM and 1.6 mGy with CEDM, while dense breast phantoms had a mean AGD of 1.3 mGy with 2D FFDM and 2.1 mGy with CEDM. At a compressed thickness of 4.5 cm, radiation exposure from CEDM was approximately 25% higher in dense breast phantoms than in non-dense breast phantoms.
The dose in dense phantoms at a compressed thickness of 6 cm was approximately 42% higher than the dose in non-dense phantoms at a compressed thickness of 4.5 cm (Table 5.6). Therefore, these findings were in contrast with the study done by Fallenberg and colleagues.
Many studies have evaluated AGD, with variable and noncomparable results. Some studies have been performed with a CEDM prototype unit in which exposure settings were manually set, while others were performed with automatic control of exposition, and additional studies were dependent on breast thickness and glandularity.
Despite this high variability between the studies, all the results obtained were under the radiation dose limits set by the Mammography Quality Standards Act (MSQA).
5 CEDM in Comparison with MRI
CEDM has proven to be an effective alternative to MRI for functional imaging of the breast, to assess hyper-vascularized tissues that may be related to tumour angiogenesis. Many experts have focused on comparing these two examinations.
The sensitivity is the same for both CEDM and MRI, but there is still limited available data on the specificity. Fallenberg’s study was the only one, which compared the specificity between these two modalities, and they observed a specificity of 94% in CEDM in comparison to 88% in MRI [18] (Table 5.7).
The first study to compare CEDM and MRI was performed by Jochelson et al. [19]. Each technique identified 50 out of 52 lesions with the same sensitivity (96%), but CEDM had a lower sensitivity for detecting ipsilateral additional lesions than MRI; specifically, CEDM identified 14 lesions out of 25 (56%), and MRI identified 22 (88%).
CEDM showed a higher PPV (97% vs. 85%), thus increasing the specificity: there were just two false-positives with CEDM and 13 false-positives with MRI. These results may be explained by the differential timing of acquisition between the two techniques and the differing molecular composition of the contrast media (iodinate in CEDM and paramagnetic in MRI). Iodinated contrast in CEDM persists for more than 10-minutes in breast glandularity, allowing better visualization of lesions with slow enhancement.
Subsequently, Luczynska et al. [20] enrolled 102 patients (identified by conventional mammography) into a CEDM/MRI study, and 118 lesions were identified by the combination of CEDM and breast MRI. The sensitivity was 100% with CEDM and 93% with breast MRI. The accuracy was 79% with CEDM and 73% with breast MRI. ROC curve areas based on BI-RADS were 0.83 for CEDM and 0.84 for breast MRI. These results showed that CEDM has a high NPV and false-positive rate similar to that of breast MRI.
Li et al. [21] retrospectively compared the diagnostic performance of CEDM and MRI for breast cancer detection. This study enrolled 48 women who underwent both CEDM and MRI exams, performed within 30 days. The parameters of the study were to determine the sensitivity, PPV, lesion size, morphology (using the breast MRI BI-RADS lexicon), index lesion and background enhancement (from 0, no enhancement, to 3, marked/moderate enhancement, according to the guidelines from ACR BI-RADS 5th edition).
In this study, CEDM identified 64 lesions, all visible by MRI as well, of which 62 were malignant findings and two were benign lesions. MRI identified 66 lesions, two more than CEDM, which were found to be benign lesions upon pathology. The sensitivity was 100% for both techniques, but CEDM had a better PPV (97% vs. 94%) and a lower false-positive rate (2/64 vs. 4/66). The morphology of the malignant findings was 100% consistent between CEDM and MRI. The authors concluded that CEDM had a higher PPV and a lower BPE than MRI and potentially represents a new innovative alternative to MRI.
Another important two-centre study performed by Fallenberg et al. [18] aimed to demonstrate that CEDM alone is not inferior to MRI and is superior to FFDM for breast cancer detection. Six independent breast radiologists examined the FFDM, CEDM and MRI images of 187 patients.
Twenty-three of 187 were ineligible, and the remaining 155 were included. The authors found that the sensitivity of FFDM alone (0.81) was significantly lower than that of CEDM (0.94) and MRI (0.95), and the MRI sensitivity was higher than that of CEDM alone and CEDM + FFDM; the MRI specificity (0.88) was lower than that of other modalities (CEDM, 0.94, and FFDM 0.95). The benefits of CEDM alone and MRI alone were particularly evident in dense breast. CEDM alone and with MRI showed no significant differences in ROC curves, demonstrating that it is an accurate alternative to MRI.
In another study by Fallenberg [22], the measurements of the size of the index cancer were compared between FFDM, CEDM, MRI and postoperative histology in 59 cases for which the index cancer was depicted with all three imaging techniques and final histology findings were available.
There was a slight underestimation of the tumour size using FFDM and MRI compared to CEDM and pathology (Table 5.8).
These results confirmed that CEDM has a good correlation with postoperative histology for size assessment.
Lobbes et al. also concluded that CEDM is not inferior to MRI for tumour size assessment. Using the surgical specimen as a gold standard, the authors evaluated 57 CEDM examinations and compared them with MRI exams. They found that Pearson’s correlation coefficient was >0.9 for CEDM vs. histopathology with p < 0.0001, which was the same value calculated for MRI, with a mean difference of 0.03 mm (vs. 2.12 mm for MRI), and there was no additional benefit to performing MRI after CEDM in any case [23].
6 Review of the Literature on New Potential Clinical Indications
Based on the available literature, the efficiency and accuracy of CEDM, which are comparable to those of MRI, have already been proven; therefore researchers are now focussing on expanding its clinical indications. Currently, EUSOBI guidelines have concluded that CEDM should be performed when there are contraindications to MRI [10].
Beyond the diagnostic efficiency of CEDM, Patel et al. defined new potential clinical indications [24]. The authors focused on two potential indications, which are monitoring the response of neoadjuvant chemotherapy (NAC) and “personalized” screening. The authors demonstrate not only the efficiency of CEDM in comparison to MRI for evaluating the perioperative chemotherapy (ChT) but also the usefulness of CEDM as an alternative tool in patients with pacemakers, severe claustrophobia and other MRI contraindications.
We also analysed the study by El Said et al., which included 21 patients undergoing NAC [25]; this study reported six false-negative cases, but the authors suggested that this was due to residual small tumour foci receiving nutrients by diffusion instead of new angiogenic vessels and not due to a lack of CEDM sensitivity.
Other studies have been performed to evaluate CEDM efficacy in evaluating residual tumour post-NAC. One important retrospective study by Barra FR et al. [26] involved the analysis of eight lesions in eight patients who received NAC as part of their treatment before undergoing surgery. Three radiologists assessed the size of the residual tumour by CEDM and FFDM separately and then correlated the residual tumour size with the pathological response in surgical specimens.
The authors used low-energy CEDM images (for FFDM) and recombined images to measure suspicious findings. The results indicated a higher sensitivity (83.3% vs. 50%), specificity (100% vs. 50%), PPV (100% vs. 50%) and NPP (66% vs. 25%) for CEDM.
The correlation between CEDM and surgical specimens was statistically significant and differed from FFDM, with an underestimation of lesion size in 37.5% vs. 50% of cases, an overestimation by both techniques in 37.5% of cases and correct assessment in 25% vs. 12.5% of cases. Additionally, the interobserver agreement was slightly better for CEDM, increasing the diagnostic performance of all readers.
A second, larger study sought to compare CEDM and MRI for the evaluation of tumour response to NAC. This prospective study enlisted 54 women with breast cancer who were indicated for NAC. CEDM and MRI were performed three times: before NAC, after 3 months and after 6 months, just before surgery. To evaluate tumour response, seven independent radiologists measured the size of the residual lesion by both CEDM and MRI and compared it to the surgical specimen (gold standard). Response to therapy was assessed according to the parameters set in the RECIST criteria: complete response (CR, no residual lesion), partial response (PR, reduction ≥30% of largest dimension), stable disease (SD, <30% reduction, <20% increase) and progressive disease (PD ≥ 20% increase). Forty-six patients of 54 completed the study. CEDM better predicted pCR than MRI (Lin’s coefficient of 0.81 vs. 0.59). Both methods underestimated the residual size (4.1 mm in CEDM vs. 7.5 mm in MRI). For the evaluation of CR, CEDM sensitivity and sensibility were 100% and 84% vs. 87% and 60% for MRI, respectively.
This study confirms that CEDM is as reliable as MRI for monitoring the response to NAC [27].
The second diagnostic potential indication was to use CEDM to perform a personalized individual screening programme for each woman [23]. Since dense breast has a higher risk of developing cancer than fatty breast parenchyma, and CEDM alone or CEDM + FFDM has better diagnostic accuracy than FFDM alone, many women with dense breast parenchyma may benefit from this additional screening [7, 14].
Additionally, in a recent study by Convington et al., the authors discussed the possibility of personalizing screening procedures for each patient depending on breast density and the potential lifetime risk of developing cancer [28]. MRI is the standard screening modality in high-risk women, such as BRCA1 and BRCA2 mutation carriers [29]. However, supplemental screening with MRI is only cost-effective if the risk is more than 20%. Since CEDM is approximately 25% cheaper than the cost of an MRI, it may be an important tool in those women with intermediate lifetime risk, such as women with dense breasts [30].
There is still no commercially available system to obtain biopsies under CEDM guidance at present. However, to our knowledge it should be available in due time. For now, researchers have tried placing a clip at the site of a suspicious enhancement with CEDM guidance and then performed a stereotactic core needle biopsy targeting the clip [28].
Potentially greater cost savings than MRI also supports the implementation of CEDM. A study by Bhavika Patel and colleagues in Mayo Clinic, Arizona, stated that the total cost of MRI screening was $954, encompassing contrast administration, contrast medium costs and computer-assisted detection with prior FFDM, whereas the cost for a CEDM examination was $196 because it was not necessary to conduct a separate FFDM study given the equivalency of the low-energy CEDM image. Therefore, with CEDM implementation, the savings amount would be $750 per examination and $1.1 billion annually, a cost that is 80% cheaper than MRI with comparable performance [30]. In our experience, at our centre at AOU Careggi, a breast MRI costs approximately €245, whereas CEDM costs only €95 and thus a CEDM examination is approximately 60% cheaper.
In conclusion, based on the review of the available literature, results have shown that CEDM is more sensitive and specific than conventional mammography for the detection of breast cancer. Additionally, it has a sensitivity that is comparable to MRI for the detection of primary breast cancers. Given its low cost, potential broad availability and ability to be used in women who cannot undergo MRI, CEDM has proven to be a promising addition to current breast imaging techniques.
References
Lewin JM, Isaacs PK, Vance V, Larke FJ. Dual-energy contrast-enhanced digital subtraction mammography: feasibility. Radiology. 2003;229(1):261–8.
Lobbes MB, Lalji U, Houwers J, Nijssen EC, Nelemans PJ, van Roozendaal L, Smidt ML, Heuts E, Wildberger JE. Contrast-enhanced spectral mammography in patients referred from the breast cancer screening programme. Eur Radiol. 2014;24(7):1668–76.
Lalji UC, Houben IP, Prevos R, Gommers S, van Goethem M, Vanwetswinkel S, Pijnappel R, Steeman R, Frotscher C, Mok W, Nelemans P, Smidt ML, Beets-Tan RG, Wildberger JE, Lobbes MB. Contrast-enhanced spectral mammography in recalls from the Dutch breast cancer screening program: validation of results in a large multireader, multicase study. Eur Radiol. 2016;26(12):4371–9.
Tagliafico AS, Bignotti B, Rossi F, Signori A, Sormani MP, Valdora F, Calabrese M, Houssami N. Diagnostic performance of contrast-enhanced spectral mammography: systematic review and meta-analysis. Breast. 2016;28:13–9. https://doi.org/10.1016/j.breast.2016.04.008. Epub 2016 May 7.
Libera A, Altman DG, Tetzla J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. PRISMA Statement per il reporting di revisioni sistematiche e meta-analisi degli studi che valutano gli interventi sanitari: spiegazione ed elaborazione. Evidence. 2015;7(6):e1000115.
Lalji UC, Jeukens CR, Houben I, Nelemans PJ, van Engen RE, van Wylick E, Beets-Tan RG, Wildberger JE, Paulis LE, Lobbes MB. Evaluation of low-energy contrast-enhanced spectral mammography images by comparing them to full-field digital mammography using EUREF image quality criteria. Eur Radiol. 2015;25(10):2813–20.
Fallenberg EM, Dromain C, Diekmann F, Renz DM, Amer H, Ingold-Heppner B, Neumann AU, Winzer KJ, Bick U, Hamm B, Engelken F. Contrast-enhanced spectral mammography: does mammography provide additional clinical benefits or can some radiation exposure be avoided? Breast Cancer Res Treat. 2014;146(2):371–81.
Francescone MA, Jochelson MS, Dershaw DD, Sung JS, Hughes MC, Zheng J, Moskowitz C, Morris EA. Low energy mammogram obtained in contrast-enhanced digital mammography (CEDM) is comparable to routine full-field digital mammography (FFDM). Eur J Radiol. 2014;83(8):1350–5.
Tennant SL, James JJ, Cornford EJ, Chen Y, Burrell HC, Hamilton LJ, Girio-Fragkoulakis C. Contrast-enhanced spectral mammography improves diagnostic accuracy in the symptomatic setting. Clin Radiol. 2016;71(11):1148–55.
Sardanelli F, Fallenberg EM, Clauser P, Trimboli RM, Camps-Herrero J, Helbich TH, Forrai G, European Society of Breast Imaging (EUSOBI), with language review by Europa Donna–The European Breast Cancer Coalition. Mammography: an update of the EUSOBI recommendations on information for women. Insights Imaging. 2017;8(1):11–8.
Cheung YC, Tsai HP, Lo YF, Ueng SH, Huang PC, Chen SC. Clinical utility of dual-energy contrast-enhanced spectral mammography for breast microcalcifications without associated mass: a preliminary analysis. Eur Radiol. 2016;26(4):1082–9.
Cheung YC, Juan YH, Lin YC, Lo YF, Tsai HP, Ueng SH, Chen SC. Dual-energy contrast-enhanced spectral mammography: enhancement analysis on BI-RADS 4 non-mass microcalcifications in screened women. PLoS One. 2016;11(9):e0162740.
Patel BK, Naylor ME, Kosiorek HE, Lopez-Alvarez YM, Miller AM, Pizzitola VJ, Pockaj BA. Clinical utility of contrast-enhanced spectral mammography as an adjunct for tomosynthesis-detected architectural distortion. Clin Imaging. 2017;46:44–52.
Mori M, Akashi-Tanaka S, Suzuki S, Daniels MI, Watanabe C, Hirose M, Nakamura S. Diagnostic accuracy of contrast-enhanced spectral mammography in comparison to conventional full-field digital mammography in a population of women with dense breasts. Breast Cancer. 2017;24(1):104–10.
Cheung YC, Lin YC, Wan YL, Yeow KM, Huang PC, Lo YF, Tsai HP, Ueng SH, Chang CJ. Diagnostic performance of dual-energy contrast-enhanced subtracted mammography in dense breasts compared to mammography alone: interobserver blind-reading analysis. Eur Radiol. 2014;24(10):2394–403.
Tardivel AM, Balleyguier C, Dunant A, Delaloge S, Mazouni C, Mathieu MC, Dromain C. Added value of contrast-enhanced spectral mammography in Postscreening assessment. Breast J. 2016;22(5):520–8.
James JR, Pavlicek W, Hanson JA, Boltz TF, Patel BK. Breast radiation dose with CESM compared with 2D FFDM and 3D Tomosynthesis mammography. AJR Am J Roentgenol. 2017;208(2):362–72.
Fallenberg EM, et al. Contrast-enhanced spectral mammography vs. mammography and MRI—clinical performance in a multi-reader evaluation. Eur Radiol. 2017;27(7):2752–64.
Jochelson MS, Dershaw DD, Sung JS, Heerdt AS, Thornton C, Moskowitz CS, Ferrara J, Morris EA. Bilateral contrast-enhanced dual-energy digital mammography: feasibility and comparison with conventional digital mammography and MR imaging in women with known breast carcinoma. Radiology. 2013;266(3):743–51.
Łuczyńska E, Heinze-Paluchowska S, Hendrick E, Dyczek S, Ryś J, Herman K, Blecharz P, Jakubowi J. Comparison between breast MRI and contrast-enhanced spectral mammography. Med Sci Monit. 2015;21:1358–67.
Li L, et al. Contrast-enhanced spectral mammography (CESM) versus breast magnetic resonance imaging (MRI): a retrospective comparison in 66 breast lesions. Diagn Interv Imaging. 2017;98(2):113–23.
Fallenberg EM, Dromain C, Diekmann F, Engelken F, Krohn M, Singh JM, Ingold-Heppner B, Winzer KJ, Bick U, Renz DM. Contrast-enhanced spectral mammography versus MRI: initial results in the detection of breast cancer and assessment of tumour size. Eur Radiol. 2014;24(1):256–64.
Lobbes MBI, et al. The quality of tumor size assessment by contrast-enhanced spectral mammography and the benefit of additional breast MRI. J Cancer. 2015;6(2):144–50.
Patel BK, Lobbes MB, Lewin J. Contrast enhanced spectral mammography: a review. Semin Ultrasound CT MRI. 2018;39:70–9.
ElSaid NAE, Mahmoud HGM, Salama A, et al. Role of contrast enhanced spectral mammography in predicting pathological response of locally advanced breast cancer post neo-adjuvant chemotherapy. Egypt J Radiol Nucl Med. 2017;48(2):519–27.
Barra FR, et al. Accuracy of contrast-enhanced spectral mammography for estimating residual tumor size after neoadjuvant chemotherapy in patients with breast cancer: a feasibility study. Radiol Bras. 2017;50(4):224–30.
Iotti V, et al. Contrast-enhanced spectral mammography in neoadjuvant chemotherapy monitoring: a comparison with breast magnetic resonance imaging. Breast Cancer Res. 2017;19:106.
Covington MF, et al. The future of contrast-enhanced mammography. AJR. 2018;210:292–300.
Pataky R, et al. Cost-effectiveness of MRI of breast cancer screening in BRCA1/2 mutation carriers. BMC Cancer. 2013;13:339.
Patel BK, et al. Potential cost savings of contrast-enhanced digital mammography. AJR. 2017;208:W231–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
De Benedetto, D., Bellini, C. (2018). An Overview of the Literature on CEDM. In: Nori, J., Kaur, M. (eds) Contrast-Enhanced Digital Mammography (CEDM). Springer, Cham. https://doi.org/10.1007/978-3-319-94553-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-94553-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-94552-1
Online ISBN: 978-3-319-94553-8
eBook Packages: MedicineMedicine (R0)