Abstract
Early detection and quantification of cardiac damage in cancer patients are essential to readily intervene with cardioprotective strategies and avoid the need of the discontinuation of antineoplastic treatment.
Many strategies are available to monitor cardiac function during or after chemotherapy including cardiac imaging (echocardiography, nuclear imaging, cardiac magnetic resonance) and measurement of biomarkers (troponin, natriuretic peptides).
Systematic and repeated monitoring of left ventricle ejection fraction (LVEF) remains the most used technique to diagnose cardiotoxicity in clinical practice. Among the new techniques that evaluate cardiac function, GLS derived by 2D-STE is the best validated technique with a considerable amount of evidences supporting its role in the early detection of cardiotoxicity. Regarding CMR, its low availability and the high cost limit its use to particular subsets of patients.
Measuring biomarkers (troponin and NT-proBNP) also appear to be effective in the prediction of cardiotoxicity; their elevations identify high-risk cohort of cancer patients who may benefit from early cardioprotective medication.
A multimodality approach in selected individuals may provide incremental value in predicting cardiotoxicity and prove to be useful in clinical practice; however further studies are needed for wider validation in the clinical setting.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Early detection
- Cardiotoxicity
- Echocardiography
- Biomarkers
- Multimodality approach
- Global longitudinal strain
Introduction
Advances in the early diagnosis, staging, and therapy have significantly reduced the mortality and increased longevity in cancer patients. An estimated 14.5 million people are currently living with a history of cancer in the USA. This number is projected to rise to 19 million over the next 10 years [1]. A significant proportion of cancer survivors are living with long-term adverse effects of cancer therapy, involving multiple organ systems. Cardiovascular toxicity of cancer therapy is a major concern in this regard.
Cancer therapies, especially anthracyclines and monoclonal antibodies, have been linked with increased rates of cardiotoxicity (CTX). The clinical manifestations of cardiotoxicity are broad and can include heart failure, cardiomyopathies, arrhythmias, ischaemia, valves heart disease, pericardial disease, hypertension, or thrombosis. Cancer therapeutics-related cardiac dysfunction (CTRCD) is reported in 2–3% in randomized trials on breast cancer women treated with anthracyclines and trastuzumab but can reach up to 26% in observational studies [2].
It is clear that symptom-based monitoring is ineffective because when they occur, damage is already advanced, and therefore it is recommended after a baseline evaluation to monitor cardiac function to promptly detect any variation. Early detection and quantification of cardiac damage is required to readily intervene with cardioprotective therapy and to allow the prosecution of antineoplastic treatment and avoid the need of its discontinuation. Therefore, cardio-oncology is a newly emerging subspecialty of cardiology with the aim of monitoring, early diagnosis, prevention, and treatment of cardiotoxicity related to cancer therapies and careful planning of chemotherapy in patients with pre-existing cardiovascular disease to avoid overt cardiotoxicity and heart failure.
Many strategies are available to monitor cardiac function during or after chemotherapy including cardiac imaging (echocardiography, nuclear imaging, cardiac magnetic resonance) and biomarkers (troponin, natriuretic peptides). The choice of different modalities depends upon local expertise and availability [3]. Table 16.1 summarizes the main techniques available and current diagnostic criteria.
Echocardiography
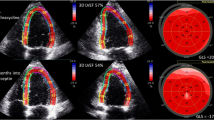
Monitoring with 2D echocardiography is the most frequently used technique in clinical practice because of its safety, wide availability, repeatability, and low cost (Fig. 16.1). Echocardiographic technology has been continuously evolving, with two major developments being real-time three-dimensional echocardiography (3DE) and myocardial deformation imaging.
Echocardiography vs. other modalities for detection of cancer therapeutics-related cardiac dysfunction. (Adapted from Zito et al. [4])
For conventional analysis, left ventricular volumes and left ventricular ejection fraction (LVEF) are the most widely used parameters to detect CTX [5, 6]. The method for 2D echocardiographic volume calculations recommended by the European Association of Cardiovascular Imaging (EACVI) and American Society of Echocardiography (ASE) is the biplane method of disc summation (modified Simpson’s rule). Volume measurements are based on tracings of the blood tissue interface in the apical four- and two-chamber views. At the mitral valve level, the contour is closed by connecting the two opposite sections of the mitral ring with a straight line. Left ventricle (LV) length is defined as the distance between the middle of this line and the most distant point of the LV contour (Fig. 16.2, left panel). The LVEF is then calculated using the following formula: LVEF = (LVEDV − LVESV)/LVEDV; (LVED LV end-diastolic volume, LVESV LV end-systolic volume). Normal LVEF using biplane method of discs is 63% ± 5%, and LVEF in the range of 53–73% is classified as normal [7].
CRTCD is defined as a 10% decrease of left ventricle ejection fraction to a value below the normal limit of normal confirmed in repeated studies (at 2–3 weeks).
Newer echocardiography techniques, using contrast echocardiography or 3D technology, have resulted in significant improvement in the accuracy of LVEF assessment. Contrast agents should be used to improve endocardial delineation when two or more contiguous left ventricle endocardial segments are poorly visualized in apical views [7, 8]. Contrast-enhanced images may provide larger volumes than unenhanced images that are closer to those obtained with cardiac magnetic resonance (CMR) [9].
In patients with good image quality, 3D echocardiographic measurements are accurate and reproducible and should therefore be used if available [7]. One of the advantages of 3D echocardiographic volume measurements is that they do not rely on geometric assumptions.
A small study of 50 patients with breast cancer undergoing serial LVEF assessments demonstrated that 3D echocardiography was feasible and reproducible for assessing changes in LV volumes and LVEF compared with the gold standard cardiac MRI [10]. Thavendiranathan et al. showed that non-contrast 3D echocardiography was the most reproducible technique for LVEF assessment, capable of detecting smaller changes in LVEF (~5%) [11].
Unfortunately, impairment of LVEF is detectable only after that a considerable cell loss has taken place [12, 13] and thus too late to allow effective prevention. For this reason, new markers of systolic dysfunction have been investigated to earlier detect damage and predict cardiotoxicity. Deformation analysis seems to be a promising tool to detect myocardial dysfunction at an earlier stage [14].
Besides monitoring systolic function, it is recommend in cancer patients to perform a comprehensive echocardiographic evaluation measuring diastolic function and evaluating cardiac valves and pericardium [15].
Diastolic function is frequently impaired in cancer studies [4, 16]. Several studies demonstrated an early reduction in the e′ velocity of the mitral annulus using tissue Doppler imaging (TDI), which remained reduced during and for several years after treatment [17, 18]. However, the use of the E/e′ ratio remains questionable in the oncological setting because E and e′ velocity fluctuations in these patients may be the consequence of changes in loading conditions associated with chemotherapy (e.g. nausea, vomiting, and diarrhoea) more than the result of a real change in left ventricle diastolic performance [4].
Chemotherapeutic agents do not directly affect cardiac valves, but valve heart disease may manifest in oncological patients for different reasons such as:
-
(a)
Pre-existing valve disease
-
(b)
Concomitant radiation therapy that causes calcification and fibrosis of the aortic root, aortic cusps, mitral valve annulus, tips, and commissures [19]
-
(c)
Infective endocarditis favoured pancytopenia associated with chemotherapy
-
(d)
Mitral regurgitation secondary to annular dilatation or apical tethering due to CRDT and tricuspid regurgitation as consequence of right ventricle dysfunction and pulmonary hypertension [3, 15].
Echocardiography is the assessment method of choice, and 3D echocardiography may be useful, particularly for the evaluation of mitral valve commissures. CMR and computed tomography (CT) may be used to assess the severity of the valve disease but usually are not required in routine clinical practice [15].
According to the current EACVI/ASE recommendations [15], patients with baseline or changing valve findings should undergo careful evaluation of valve structure and function during and after cancer treatment.
Pericardial disease is also common in oncologic patients, as consequence of cancer therapies or metastasis, and usually occurs as pericarditis and pericardial effusion and sometimes as constrictive pericarditis especially after radiotherapy or high-dose chemotherapy. Acute pericarditis may occur predominantly with the use of anthracyclines, cyclophosphamide, cytarabine, and bleomycin. Transthoracic echocardiography is the method of choice for the evaluation of patients with suspected pericardial disease due to chemotherapy, but CT can be helpful to identify calcification, and CMR should be considered in the evaluation of primary tumours of the heart. Pericardial effusion should be quantified and graded according to standard methods [20], and it is important to evaluate the presence of echocardiographic and Doppler signs of cardiac tamponade in this setting of patients.
Myocardial Deformation Imaging
LVEF reflects the volumetric variation of the ventricle during the cardiac cycle, which depends on the size and shape of the left ventricle, the contraction of the global myocardium, the integrity of the mitral and aortic valve, and the preload and post-load. In contrast, myocardial deformation analysis reflects the length variation of the myocardial fibres, and thus it is a measure of intrinsic contractility (Fig. 16.2, right panel) [14].
By the analysis of the motion of speckles in the two-dimensional ultrasonic image, this technique allows a non-Doppler angle-independent objective analysis of myocardial deformation, with the possibility to quantify longitudinal, circumferential, radial function and torsion. The best validated strain measure is global longitudinal strain (GLS). Speckle-tracking echocardiography (STE) has recently demonstrated to be an accurate, feasible, and reproducible measure of cardiac function [21].
The maximum extent of systolic myocardial deformation (i.e. peak systolic strain) and its peak rate (i.e. peak systolic strain rate) were used regionally and globally [4]. One of the first studies using 2D-STE strain was performed in 2008 and demonstrated that this technique recognized early damage caused by anthracyclines [22].
Many authors subsequently focused their efforts on this topic to identify CTX in patients previously treated with oncologic therapies to predict CTX development.
2D-STE was more sensitive than LVEF reduction for the early recognition of asymptomatic left ventricle systolic dysfunction caused by chemotherapy in children and adults [4, 23,24,25].
Other studies [26, 27] provided information on serial evaluations of cardiac function before and after chemotherapy by comparing GLS with LVEF . They found that GLS was the most sensitive and specific measurement for the detection of subclinical myocardial injury early after anthracycline exposure (from 1 day to 3 months after the treatment in the different studies) because GLS decreased significantly without any reduction in LVEF.
A prospective study of 81 patients with breast cancer evaluated the use of longitudinal strain assessed at baseline, after completion of anthracycline-based therapy, and every 3 months during trastuzumab. A longitudinal strain value lower than −19% (less negative or a lower negative number) after the completion of anthracyclines was predictive of CTX [28]. The accuracy of the prediction increased when cardiac troponin was also measured [28]. Measuring the percentage variation of GLS between follow-up and baseline seems to be a specific approach to early detect CTX. Negishi K et al. demonstrated that an 11% reduction of GLS (95% confidence interval, 8.3–14.6%) was the optimal cut-off, with sensitivity of 65% and specificity of 94% for detecting CTX [29].
The European Society of Cardiology (ESC) recently provided a document [3] containing a practical approach for monitoring patients undergoing cancer therapy with GLS. Measurements of GLS during chemotherapy should ideally be compared with baseline value, and a relative percentage reduction of GLS of less than 15% from baseline is very likely to predict future CRTD (Table 12.1). The same vendor-specific ultrasound machine should be used when monitoring STE for longitudinal follow-up of patients with cancer.
A small study demonstrated that early therapeutic intervention with beta-blocker based on strain reduction alone allowed a normalization of strain values during follow-up; however evidences demonstrating a clinical impact of this approach are still lacking [30]. The multicentre, randomized SUCCOUR (Strain Surveillance During Chemotherapy for Improving Cardiovascular Outcomes) trial is designed to determine if a strain-based strategy for initiation of cardioprotective therapy is superior to one based on LVEF .
Three-dimensional speckle-tracking echocardiography (3D-STE) is a promising techniques in the evaluation of myocardial function. The possibility of evaluating the deformation on a full-volume model avoids the errors derived from the use of two-dimensional images [31].
Recent studies demonstrated that childhood cancer survivors evaluated by 3D-STE had significantly reduced GLS and torsion and greater systolic dyssynchrony index in comparison to healthy controls [32]. Mornoş et al. found that GLS evaluated by 3D-STE was superior to biomarkers and to LVEF in predicting future development of cardiotoxicity [33].
Although 3D-STE is a promising method, there are few studies on small populations that compared this technique to the other standard methods. Moreover, 3D-STE is not widely available in the echo-labs; thus its use has still to be considered reserved to research purpose.
Nuclear Imaging and Cardiac Magnetic Resonance
Radionuclide angiography (MUGA) was referred as the gold standard to evaluate left ventricle systolic function in patients undergoing chemotherapy for many years [34]. MUGA makes use of 99mTC-erythrocyte labelling enabling the visualization of the cardiac blood pool by γ-camera with electrocardiogram-triggered acquisitions. The final result provides a highly reproducible and precise quantification of LV volumes and dyssynchrony independently of geometrical assumption [35]. The main disadvantage of MUGA is radiation exposure, which reduces its use given the increasing availability of other radiation-free imaging techniques (Table 12.1).
MUGA also provides limited structural and functional information on other cardiac structures (right ventricle, left and right atrium, valves, and pericardium). Therefore, it is frequently used as an adjunct and complementary technique to echocardiography.
The need of a reliable and accurate detection method for early CTX has encouraged the introduction of second-line advanced imaging modality into the evaluation of chemotherapy-treated patients, such as cardiac magnetic resonance (CMR) (Table 16.1). CMR is an ionizing radiation-free imaging method recently accepted as the gold standard for quantifying biventricular volumes, function, and mass [36, 37].
The standard CMR approach for quantifying biventricular function parameters uses contiguous short-axis slices covering the entire ventricles acquired from a cine steady-state free precession (SSFP) sequence (Fig. 16.3) [36]. In the evaluation of CTX, the incremental value of CMR is represented by its capability for providing information on tissue characterization, such as oedema, hyperaemia, fibrosis, and iron overload. It also serves to evaluate the pericardium, especially in patients with chest irradiation.
Neilan et al. [38] showed that myocardial scar by late gadolinium enhancement CMR is infrequent in patients with anthracycline cardiomyopathy despite a reduced ejection fraction, and indexed LV mass by CMR imaging is a predictor of adverse cardiovascular events.
A new CMR parameter was recently proposed, the LV global function index, that combines left ventricular stroke volume, end-systolic and end-diastolic volumes, and mass, and a value less than 37% has been shown to be associated with the occurrence of cardiovascular events [39]. However, no data are available on this promising index in monitoring CTX [36].
Myocardial deformation can be evaluated by tagging techniques and, more recently, by using phase-contrast imaging. In the technique most frequently used, the myocardium is tagged with a grid of magnetic saturation lines at end diastole, allowing the analysis of deformation by tracking the distortion of the grid during systole.
In a recent study [40], measures of left ventricular systolic performance (LVEF and mean mid-wall circumferential strain) deteriorated early and remained abnormal 6 months after initiation of low to moderate doses of anthracycline-based chemotherapy. Authors did not appreciate new infarcts or fibrosis by late gadolinium enhancement.
Few studies evaluated the presence of oedema and fibrosis in patients treated with chemotherapy. Regarding the detection of myocardial oedema as early marker of cardiac damage, in this setting of patients, results are contrasting, and no prognostic data are available [41, 42].
The prevalence of non-ischaemic areas of LGE was reported between 6% and 100% [43, 44]. However, the role of the LGE in the prognostic stratification of these patients is not yet well defined [38, 44, 45].
LGE is able to detect only macroscopic fibrosis. However, oncologic patients can develop diffuse myocardial fibrosis that can be detected by T1 mapping with the evaluation of the extracellular volume (ECV). Small studies showed encouraging results on the use of T1 mapping in the detection of myocardial damage during and after chemotherapy [46,47,48].
Based on these evidences, T1 mapping seems to be a very useful technique in oncologic patients in order to detect changes in the molecular features of the myocardium prior to the occurrence of functional alterations. However, its prognostic role is still under investigation.
Cardiac damage induced by anthracyclines appears to be partially dependent on the alteration of intracellular iron metabolism. Unfortunately, evaluations of myocardial iron overload in patients treated with anticancer drugs have not yet been performed [36].
Actually, CMR is recommended for the quantification of LVEF when the quality of echocardiogram is suboptimal. In follow-up assessments, CMR is recommended for the quantification of LVEF in cases of possible discontinuation of chemotherapeutic regimens as a result of CTX or when LVEF estimation by echocardiography is controversial or unreliable due to technical constrains. Diastolic function by CMR is not usually recommended in current practice [15].
Biomarkers
The use of cardiac biomarkers during cardiotoxic chemotherapy may be considered in order to detect early cardiac injury. Currently, the most studied biomarkers for the early detection of cardiac damage induced by anticancer drugs are cardiac troponins (cTns) and natriuretic peptides (Table 16.1).
Cardiac troponins are sensitive and specific markers of myocardial injury and are widely used in cardiovascular medicine. Troponin I is a serum marker that detects damage of myofibrils and cardiomyocytes. It identifies acute injury due to ischaemia but also to other causes such as drugs.
Among troponins, TnI is the most widely studied serum biomarker of cardiotoxicity, its elevation can predict the future decline of myocardial function, and the amount of its elevation is correlated with patients’ prognosis [49]. Particularly, it has been shown that in patients with cancer, treated with high doses of anthracyclines, the increase in cTn allows discrimination between patients with a low risk of developing chemotherapy-induced CTX and who do not need strict follow-up and those at high risk, which require a more rigorous cardiac monitoring [50].
In particular, patients with a persistent (early and late) increase in cTn show a greater reduction in LVEF at follow-up [51]. In patients treated with trastuzumab, the elevation of cTnI identified patients who developed CTX and who did not recover after interruption of treatment [52]. Less established is the role of troponin in predicting cardiotoxicity in patients treated with conventional doses of anthracyclines; in this setting high-sensitivity troponin (hsTn) is probably more useful (Table 16.2).
In patients with breast cancer, a recent study demonstrated that the combination of high-sensitivity troponin with GLS might provide the greatest sensitivity (93% when both are altered) and sensitivity (87%, when one of two parameters is altered) to predict future cardiotoxicity [28].
Main advantages of cTn use include wide availability, accuracy, reproducibility, and lower cost than imaging. Nevertheless, there are some uncertainties that still remain unresolved, including the optimal timing of assessing, frequency of cTn evaluations, optimal cut-off point for positivity with the highest level of specificity, and comparison of different assays of troponin [49]. Table 12.2 reports main studies which demonstrated usefulness of TnI for predicting CTX.
Natriuretic peptides are hormones released during haemodynamic stress when ventricles dilate, undergo hypertrophy, or is subject to increased wall tension. Use of BNP and NT-proBNP to detect subclinical cardiac dysfunction is under investigation, and results of published studies are controversial [54, 62, 63].
BNP levels were increased during chemotherapy treatment and correlated with diastolic dysfunction [55] and progressive development of cardiac dysfunction [56, 64].
In some studies, BNP anomalies were observed in the absence of changes in cTn [57, 65, 66], which suggested that in patients receiving anticancer drugs at low or medium doses and with a predictable reduced myocardial suffering, BNP monitoring could be more useful than cTn [49]. In other studies, BNP was not predictive of EF change [28].
Other circulating biomarkers tested include C-reactive protein, cytokines, and parameters of oxidative stress.
Due to the mechanisms of anthracycline-mediated toxicity, measurement of inflammatory markers and parameters of oxidative stress are also reasonable [49, 58]. C-reactive protein is a nonspecific marker of inflammation, and the utility of its evaluation in the setting of anticancer drug-related CTX is controversial.
Recently, galectin-3 (gal-3) has been considered as a potential biomarker for predicting early or late onset of CTX. However, increases of gal-3 were found to be insignificant and not predictive of CTX as defined by echo-derived LVEF reduction [53].
Finally, potential CTX markers under investigation in oncology are heart-type fatty acid-binding protein (H-FABP), glycogen phosphorylase BB (GPBB), and circulating microRNAs, but they are not yet validated [59,60,61].
Multimodality Approach
As demonstrated by recent studies, a combined multimodality approach in selected individuals may provide incremental value in predicting cardiotoxicity and prove to be useful in clinical practice [28, 53, 67,68,69]. However, only a few studies have explored the utility of a multimarker approach in monitoring patients undergoing antineoplastic drugs at high baseline risk.
Fallah-Rad et al. [43] conducted the first multimodality surveillance strategy, combining biomarkers (troponin T, CRP, and BNP) with imaging (echocardiography and CMR) in breast cancer patients treated in the adjuvant setting by anthracyclines and trastuzumab. Biomarkers were not associated with any prognostic value, along with LVEF assessment, but Doppler measurement of s′, GLS, and radial strain parameters were able to identify, at 3 months’ follow-up, the patients who developed CTRCD at 6 months. In this study, CMR, performed at baseline and at 12 months, documented an increase in LV volumes, a decrease in LVEF, and a late gadolinium enhancement in the LV lateral wall in the CTRCD group.
Similarly, Sawaya et al. [18] observed that NT-proBNP was not associated with any predictive value, while high-sensitive TnI at 3 months appeared as an independent predictor of cardiotoxicity at 6 months. Furthermore, a combination of GLS and hsTnI allowed with a better accuracy the early identification of myocardial damage and was predictive of subsequent CRTCD during the surveillance in patients receiving trastuzumab after anthracyclines.
The troponin levels added prognostic value to GLS: if both were abnormal, the specificity for the prediction of CTRCD increased from 73% to 93%. If both were normal, the negative predictive value increases to 91% [28].
Given these scientific evidences, the recent EACVI/ASE consensus document [15] encourages an integrated approach to early detect cardiotoxicity. Particularly a strategy that includes, in addition to LVEF assessment, the calculation of GLS and the measurement of troponin at baseline and during follow-up in order to compare changes during time is proposed. (Fig. 16.4).
Multimodality approach to monitor patients undergoing antineoplastic treatment. 2DE, 2D echocardiography; 3DE, 3D echocardiography; GLS, global longitudinal strain; LLN, lower limit of normal; LVEF, left ventricular ejection fraction. (Reprinted from Plana et al. [15]. With permission from Elsevier)
Conclusions
Systematic and repeated monitoring of LVEF remains the most used technique to diagnose cardiotoxicity in clinical practice. 2DE is the most used method; however, 3DE has proved to be more accurate and reproducible, and this is preferable if available. Regarding CMR, it is very accurate, but its low availability and the high cost limit its use to particular subsets of patients.
Decrease of LVEF is detectable when damage is considerable and possibility of recovery reduced; therefore it is not suitable as an early indicator of cardiotoxicity.
Among the new techniques that evaluate cardiac function, GLS derived by 2D-STE is the best validated technique with a considerable amount of evidences supporting its role in the detection of cardiotoxicity. Baseline evaluation of GLS and periodical monitoring during treatment is recommended. Promising techniques such as 3D-STE and tissue characterization performed by CMR are under investigation and could provide new insights into the future for the evaluation of chemotherapy-treated patients.
Monitoring troponin levels also appears to be effective in the prediction of cardiotoxicity, and its elevations identify high-risk cohort of cancer patients who may benefit from early cardioprotective medication. According to some evidences, the persistence of NT-proBNP elevation seems to identify patients at higher risk of LVEF decline.
A multimodality approach using troponin and GLS seems to increase the accuracy in the detection of cardiotoxicity especially in patients at high baseline risk; however further studies are needed for wider validation in the clinical setting.
Cardiotoxicity is likely to be a continuous phenomenon characterized by progressive left ventricular ejection fraction decline that, if disregarded and not treated, may progressively lead to overt heart failure. On the other side, if we catch this process in the early phases, overt damage can be prevented and the dysfunction avoided. For this reason, it is extremely important to monitor patients undergoing antineoplastic drugs and to apply sensitive technique to early detect damage.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics 2016. CA Cancer J Clin. 2016;66:7–30.
Thavendiranathan P, Abdel-Qadir H, Fischer HD, Camacho X, Amir E, Austin PC, et al. Breast cancer therapy-related cardiac dysfunction in adult women treated in routine clinical practice: a population-based cohort study. J Clin Oncol. 2016;34(19):2239–46.
Zamorano JL, Lancellotti P, Rodriguez Muñoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines. The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur J Heart Fail. 2017;19:9–42.
Zito C, Longobardo L, Cadeddu C, Monte I, Novo G, Dell’Oglio S, et al. Cardiovascular imaging in the diagnosis and monitoring of cardiotoxicity: role of echocardiography. J Cardiovasc Med (Hagerstown). 2016;17(Suppl 1):e35–44.
Tan TC, Scherrer-Crosbie M. Assessing the cardiac toxicity of chemotherapeutic agents: role of echocardiography. Curr Cardiovasc Imaging Rep. 2012;5(6):403–9.
Altena R, Perik PJ, van Veldhuisen DJ, de Vries EG, Gietema JA. Cardiovascular toxicity caused by cancer treatment: strategies for early detection. Lancet Oncol. 2009;10:391–9.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–53.
Mulvagh SL, Rakowski H, Vannan MA, Abdelmoneim SS, Becher H, Bierig SM, et al. American Society of Echocardiography consensus statement on the clinical applications of ultrasonic contrast agents in echocardiography. J Am Soc Echocardiogr. 2008;21:1179–201.
Hoffmann R, von Bardeleben S, Kasprzak JD, Borges AC, ten Cate F, Firschke C, et al. Analysis of regional left ventricular function by cineventriculography, cardiac magnetic resonance imaging, and unenhanced and contrast-enhanced echocardiography: a multicenter comparison of methods. J Am Coll Cardiol. 2006;47:121–8.
Walker J, Bhullar N, Fallah-Rad N, Lytwyn M, Golian M, Fang T, et al. Role of three-dimensional echocardiography in breast cancer: comparison with two-dimensional echocardiography, multiple-gated acquisition scans, and cardiac magnetic resonance imaging. J Clin Oncol. 2010;28(21):3429–36.
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013;61(1):77–84.
Monsuez JJ. Detection and prevention of cardiac complications of cancer chemotherapy. Arch Cardiovasc Dis. 2012;105(11):593–604.
Banchs J, Jefferies JL, Plana JC, Hundley WG. Imaging for cardiotoxicity in cancer patients. Tex Heart Inst J. 2011;38:268–9.
Tarr A, Stoebe S. Early detection of cardiotoxicity by 2D and 3D deformation imaging in patients receiving chemotherapy. Echo Res Pract. 2015;2(3):81–8.
Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2014;15:1063–93.
Di Lisi D, Bonura F, Macaione F, Peritore A, Meschisi M, Cuttitta F, et al. Chemotherapy-induced cardiotoxicity: role of the tissue Doppler in the early diagnosis of left ventricular dysfunction. Anti-Cancer Drugs. 2011;22(5):468–72.
Nagy AC, Cserép Z, Tolnay E, Nagykálnai T, Forster T. Early diagnosis of chemotherapy induced cardiomyopathy: a prospective tissue Doppler imaging study. Pathol Oncol Res. 2008;14:69–77.
Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Cohen V, et al. Early detection and prediction of cardiotoxicity in chemotherapy-treated patients. Am J Cardiol. 2011;107:1375–80.
Lancellotti P, Nkomo VT, Badano LP, Bergler-Klein J, Bogaert J, Davin L, European Society of Cardiology Working Groups on Nuclear Cardiology and Cardiac Computed Tomography and Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, Society of Cardiovascular Computed Tomography, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2013;14:721–40.
Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587–610.
Cameli M, Mondillo S, Galderisi M, Mandoli GE, Ballo P, Nistri S, et al. Speckle tracking echocardiography: a practical guide. G Ital Cardiol (Rome). 2017;18(4):253–69.
Migrino RQ, Aggarwal D, Konorev E, Brahmbhatt T, Bright M, Kalyanaraman B. Early detection of doxorubicin cardiomyopathy using two-dimensional strain echocardiography. Ultrasound Med Biol. 2008;34:208–14.
Cheung YF, Hong WJ, Chan GC, Wong SJ, Ha SY. Left ventricular myocardial deformation and mechanical dyssynchrony in children with normal ventricular shortening fraction after anthracycline therapy. Heart. 2010;96:1137–41.
Bi X, Deng Y, Zeng F, Zhu Y, Wu Y, Zhao C, et al. Evaluation of epirubicin-induced cardiotoxicity by two-dimensional strain echocardiography in breast cancer patients. J Huazhong Univ Sci Technolog Med Sci. 2009;29:391–4.
Ho E, Brown A, Barrett P, Morgan RB, King G, Kennedy MJ, et al. Subclinical anthracycline- and trastuzumab-induced cardiotoxicity in the long-term follow-up of asymptomatic breast cancer survivors: a speckle tracking echocardiographic study. Heart. 2010;96:701–7.
Kang Y, Cheng L, Li L, Chen H, Sun M, Wei Z, et al. Early detection of anthracycline-induced cardiotoxicity using two dimensional speckle tracking echocardiography. Cardiol J. 2013;20:592–9.
Stoodley PW, Richards DA, Hui R, Boyd A, Harnett PR, Meikle SR, et al. Two-dimensional myocardial strain imaging detects changes in left ventricular systolic function immediately after anthracycline chemotherapy. Eur J Echocardiogr. 2011;12:945–52.
Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Tan TC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging. 2012;5:596–603.
Negishi K, Negishi T, Hare JL, Haluska BA, Plana JC, Marwick TH. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr. 2013;26:493–8.
Negishi K, Negishi T, Haluska BA, Hare JL, Plana JC, Marwick TH. Use of speckle strain to assess left ventricular responses to cardiotoxic chemotherapy and cardioprotection. Eur Heart J Cardiovasc Imaging. 2014;15(3):324–31.
Pizzino F, Vizzari G, Qamar R, Bomzer C, Carerj S, Zito C, et al. Multimodality imaging in cardiooncology. J Oncol. 2015;2015:263950.
Yu HK, Yu W, Cheuk DK, Wong SJ, Chan GC, Cheung YF. New three-dimensional speckle-tracking echocardiography identifies global impairment of left ventricular mechanics with a high sensitivity in childhood cancer survivors. J Am Soc Echocardiogr. 2013;26(8):846–52.
Mornoş C, Manolis AJ, Cozma D. The value of left ventricular global longitudinal strain assessed by three-dimensional strain imaging in the early detection of anthracycline-mediated cardiotoxicity. Hell J Cardiol. 2014;55(3):235–44.
Gottdiener JS, Mathisen DJ, Borer JS, Bonow RO, Myers CE, Barr LH, et al. Doxorubicin cardiotoxicity: assessment of late left ventricular dysfunction by radionuclide cineangiography. Ann Intern Med. 1981;94:430–5.
Takuma S, Ota T, Muro T, Hozumi T, Sciacca R, Di Tullio MR, et al. Assessment of left ventricular function by real-time 3-dimensional echocardiography compared with conventional noninvasive methods. J Am Soc Echocardiogr. 2001;14(4):275–84.
Pepe A, Pizzino F, Gargiulo P, Perrone-Filardi P, Cadeddu C, Mele D, et al. Cardiovascular imaging in the diagnosis and monitoring of cardiotoxicity: cardiovascular magnetic resonance and nuclear cardiology. J Cardiovasc Med (Hagerstown). 2016;17(Suppl 1):e45–54.
Goenka AH, Flamm SD. Cardiac magnetic resonance imaging for the investigation of cardiovascular disorders. Part 1: current applications. Tex Heart Inst J. 2014;41:7–20.
Neilan TG, Coelho-Filho OR, Pena-Herrera D, Shah RV, Jerosch-Herold M, Francis SA, et al. Left ventricular mass in patients with a cardiomyopathy after treatment with anthracyclines. Am J Cardiol. 2012;110:1679–86.
Mewton N, Opdahl A, Choi EY, Almeida AL, Kawel N, Wu CO, et al. Left ventricular global function index by magnetic resonance imaging–a novel marker for assessment of cardiac performance for the prediction of cardiovascular events: the multi-ethnic study of atherosclerosis. Hypertension. 2013;61:770–8.
Drafts BC, Twomley KM, D’Agostino R Jr, Lawrence J, Avis N, Ellis LR, et al. Low to moderate dose anthracycline-based chemotherapy is associated with early noninvasive imaging evidence of subclinical cardiovascular disease. JACC Cardiovasc Imaging. 2013;6:877–85.
Grover S, Leong DP, Chakrabarty A, Joerg L, Kotasek D, Cheong K, et al. Left and right ventricular effects of anthracycline and trastuzumab chemotherapy: a prospective study using novel cardiac imaging and biochemical markers. Int J Cardiol. 2013;168:5465–7.
Jordan JH, D’Agostino RB Jr, Hamilton CA, Vasu S, Hall ME, Kitzman DW, et al. Longitudinal assessment of concurrent changes in left ventricular ejection fraction and left ventricular myocardial tissue characteristics after administration of cardiotoxic chemotherapies using T1-weighted and T2-weighted cardiovascular magnetic resonance. Circ Cardiovasc Imaging. 2014;7:872–9.
Fallah-Rad N, Walker JR, Wassef A, Lytwyn M, Bohonis S, Fang T, et al. The utility of cardiac biomarkers, tissue velocity and strain imaging, and cardiac magnetic resonance imaging in predicting early left ventricular dysfunction in patients with human epidermal growth factor receptor II-positive breast cancer treated with adjuvant trastuzumab therapy. J Am Coll Cardiol. 2011;57:2263–70.
Fallah-Rad N, Lytwyn M, Fang T, Kirkpatrick I, Jassal DS. Delayed contrast enhancement cardiac magnetic resonance imaging in trastuzumab induced cardiomyopathy. J Cardiovasc Magn Reson. 2008;10:5.
Wadhwa D, Fallah-Rad N, Grenier D, Krahn M, Fang T, Ahmadie R, et al. Trastuzumab mediated cardiotoxicity in the setting of adjuvant chemotherapy for breast cancer: a retrospective study. Breast Cancer Res Treat. 2009;117:357–64.
Toro-Salazar OH, Gillan E, O’Loughlin MT, Burke GS, Ferranti J, Stainsby J, et al. Occult cardiotoxicity in childhood cancer survivors exposed to anthracycline therapy. Circ Cardiovasc Imaging. 2013;6:873–80.
Tham EB, Haykowsky MJ, Chow K, Spavor M, Kaneko S, Khoo NS, et al. Diffuse myocardial fibrosis by T1-mapping in children with subclinical anthracycline cardiotoxicity: relationship to exercise capacity, cumulative dose and remodeling. J Cardiovasc Magn Reson. 2013;15:48.
Neilan TG, Coelho-Filho OR, Shah RV, Feng JH, Pena-Herrera D, Mandry D, et al. Myocardial extracellular volume by cardiac magnetic resonance imaging in patients treated with anthracycline-based chemotherapy. Am J Cardiol. 2013;111:717–22.
Novo G, Cadeddu C, Sucato V, Pagliaro P, Romano S, Tocchetti CG, et al. Role of biomarkers in monitoring antiblastic cardiotoxicity. J Cardiovasc Med (Hagerstown). 2016;17(Suppl 1 Special issue on Cardiotoxicity from Antiblastic Drugs and Cardioprotection):e27–34.
Cardinale D, Sandri MT, Martinoni A, Tricca A, Civelli M, Lamantia G, et al. Left ventricular dysfunction predicted by early troponin I release after high-dose chemotherapy. J Am Coll Cardiol. 2000;36(2):517–22.
Cardinale D, Sandri MT, Colombo A, Colombo N, Boeri M, Lamantia G, et al. Prognostic value of troponin I in cardiac risk stratification of cancer patients undergoing high-dose chemotherapy. Circulation. 2004;109:2749–54.
Cardinale D, Colombo A, Torrisi R, Sandri MT, Civelli M, Salvatici M, et al. Trastuzumab-induced cardiotoxicity: clinical and prognostic implications of troponin I evaluation. J Clin Oncol. 2010;28:3910–6.
Ky B, Putt M, Sawaya H, French B, Januzzi JL Jr, Sebag IA, et al. Early increases in multiple biomarkers predict subsequent cardiotoxicity in patients with breast cancer treated with doxorubicin, taxanes, and trastuzumab. J Am Coll Cardiol. 2014;63:809–16.
Feola M, Garrone O, Occelli M, Francini A, Biggi A, Visconti G, et al. Cardiotoxicity after anthracycline chemotherapy in breast carcinoma: effects on left ventricular ejection fraction, troponin I and brain natriuretic peptide. Int J Cardiol. 2011;148:194–8.
Suzuki T, Hayashi D, Yamazaki T, Mizuno T, Kanda Y, Komuro I, et al. Elevated B-type natriuretic peptide levels after anthracycline administration. Am Heart J. 1998;136:362–3.
Sandri MT, Salvatici M, Cardinale D, Zorzino L, Passerini R, Lentati P, et al. N-terminal pro-B-type natriuretic peptide after high-dose chemotherapy: a marker predictive of cardiac dysfunction? Clin Chem. 2005;51:1405–10.
Romano S, Fratini S, Ricevuto E, Procaccini V, Stifano G, Mancini M, et al. Serial measurements of NT-proBNP are predictive of not high-dose anthracycline cardiotoxicity in breast cancer patients. Br J Cancer. 2011;105:1663–8.
Lagoa R, Gañán C, López-Sánchez C, García-Martínez V, Gutierrez-Merino C. The decrease of NAD(P)H:quinone oxidoreductase 1 activity and increase of ROS production by NADPH oxidases are early biomarkers in doxorubicin cardiotoxicity. Biomarkers. 2014;19:142–53.
El Ghandour AH, El Sorady M, Azab S, El Rahman M. Human heart-type fatty acid-binding protein as an early diagnostic marker of doxorubicin cardiac toxicity. Hematol Rev. 2009;1:29–32.
Horacek JM, Tichy M, Pudil R, Jebavy L. Glycogen phosphorylase BB could be a new circulating biomarker for detection of anthracycline cardiotoxicity. Ann Oncol. 2008;19:1656–7.
Horie T, Ono K, Nishi H, Nagao K, Kinoshita M, Watanabe S, et al. Acute doxorubicin cardiotoxicity is associated with miR-146a-induced inhibition of the neuregulin-ErbB pathway. Cardiovasc Res. 2010;87:656–64.
Levis EB, Binkley BF, Shapiro CL. Cardiotoxic effects of anthracycline-based therapy: what is the evidence and what are the potential harms? Lancet Oncol. 2017;18:e445–56.
Pistillucci G, Ciorra AA, Sciacca V, Raponi M, Rossi R, Veltri E. [Troponin I and B-type Natriuretic Peptide (BNP) as biomarkers for the prediction of cardiotoxicity in patients with breast cancer treated with adjuvant anthracyclines and trastuzumab]. Clin Ter. 2015;166:e67–71. [Article in Italian.]
Meinardi MT, van Veldhuisen DJ, Gietema JA, Dolsma WV, Boomsma F, van den Berg MP, et al. Prospective evaluation of early cardiac damage induced by epirubicin-containing adjuvant chemotherapy and locoregional radiotherapy in breast cancer patients. J Clin Oncol. 2001;19:2746–53.
Lee HS, Son CB, Shin SH, Kim YS. Clinical correlation between brain natriutetic peptide and anthracyclin-induced cardiac toxicity. Cancer Res Treat. 2008;40:121–6.
Urun Y, Utkan G, Yalcin B, Akbulut H, Onur H, Oztuna DG, et al. The role of cardiac biomarkers as predictors of trastuzumab cardiotoxicity in patients with breast cancer. Exp Oncol. 2015;37:53–7.
Yu AF, Ky B. Roadmap for biomarkers of cancer therapy cardiotoxicity. Heart. 2016;102(6):425–30.
Moonen M, Oury C, Lancellotti P. Cardiac imaging: multimodality advances and surveillance strategies in detection of cardiotoxicity. Curr Oncol Rep. 2017;19:63.
Putt M, Hahn VS, Januzzi JL, Sawaya H, Sebag IA, Plana JC, et al. Longitudinal changes in multiple biomarkers are associated with cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. Clin Chem. 2015;61(9):1164–72.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Novo, G., Nugara, C., Lancellotti, P. (2019). Early Detection of Cardiac Damage. In: Russo, A., Novo, G., Lancellotti, P., Giordano, A., Pinto, F. (eds) Cardiovascular Complications in Cancer Therapy. Current Clinical Pathology. Humana Press, Cham. https://doi.org/10.1007/978-3-319-93402-0_16
Download citation
DOI: https://doi.org/10.1007/978-3-319-93402-0_16
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-93401-3
Online ISBN: 978-3-319-93402-0
eBook Packages: MedicineMedicine (R0)