Abstract
The aim of our study was to compare the applicability of the conventional echocardiography and a novel method, tissue Doppler imaging (TDI) in detection of late or subclinical cardiotoxicity following anthracycline chemotherapy in long-term follow up. Forty women (31 to 65 years) were enrolled, who had not received anthracyclines previously and had normal cardiac function. The control group consisted of 20 healthy persons of similar age range. In addition to standard echocardiographic measurements, each patient underwent specific measurements (E-septum separation, pulmonary venous flow) as well. Furthermore, the myocardial velocity of numerous segments of the mitral anulus obtained with pulsed wave TDI was also detected over a two-year-long period. Systolic left ventricular function did not change significantly either in the study or in the control group. After one year, diastolic left ventricular function was impaired in 39 patients (97.5%), and 29 (72.5%) of these showed clear changes by means of the traditional E/A ratio and TDI. However, in ten patients (25%) the diastolic dysfunction could only be detected with TDI. At the end of the study diastolic dysfunction was detected in each patient, but in 13 patients (32.5%) the relaxation disorder could be revealed only with TDI. Detectable myocardial damage occurred in the study group as a result of anthracycline therapy. Our results confirmed our assumptions that TDI is a more precise and useful examination method than the traditional ones (E/A ratio or deceleration time) to demonstrate isolated diastolic dysfunction. TDI may become a regularly and more widely used noninvasive method to detect subclinical cardiotoxicity emerging after chemotherapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiotoxicity is a well known side effect of numerous chemotherapeutic drug treatments. The first issue published in 1967 referring to this topic described cardiac complications and cardiovascular failures following daunomycin treatment of children with leukemia [30]. Anthracyclines have been in the lime-light since then due to their cardiotoxicity. Mechanisms of the harmful effect and the clinical outcome are probably different. Direct myocardial impairment might lead to acute heart failure or to the development of later chronic cardiotoxicity. The main point of this cardiotoxicity is the diastolic dysfunction, possibly leading to heart failure or death years or decades after the therapy [27]. Antitumor drugs induce direct myocyte injury through free-radical mechanism [3]. This process may play a role in the later deteriorative effect of the anthracyclines. The importance of the late cardiotoxicity is that the administration of modern chemotherapeutical protocols has improved the survival rates of patients with tumors, and life expectancy has become longer.
Numerous protocols, therapeutic instructions and guidelines prescribe preliminary measurement of physiological functions and cardiovascular state before the planned therapy [6]. Standard Doppler measurement has to be part of the basic investigation, because under ideal circumstances it describes the left ventricular diastolic function appropriately. However, besides the diastolic functions of the left ventricle, the conventional E/A inflow curve is influenced by the preload, afterload, frequency, atrioventricular delay, ventricular interaction, viscoelastic properties and pericardial limiting factors. The mitral inflow curve is easy to drawn, but the evaluation requires consideration of the factors mentioned above. Regarding this question, a novel, noninvasive echocardiographic method, tissue Doppler imaging (TDI) increases the informative value of the examinations. This method can be used in the analysis of longitudinal and radial movement of the myocardium in each segment, including its direction and real-time velocity. Its role and benefits have been confirmed in numerous diseases, like coronary diseases [1], hypertension [22], hypertrophic cardiomyopathy [29], arrhythmias [18, 20] and in acute allograft rejection of transplanted patients [7]. It proved to be useful for selection of certain therapies e.g. indication of resynchronization treatment [25]. For the detection of myocardial impairment in children it has been described as a safe examination and easy to carry out [9]. In our previous study [19] we showed that cardiotoxicity can be detected earlier with TDI than with conventional methods. The aim of our investigation was to verify the applicability of a novel method, tissue Doppler imaging in long-term measurements besides the conventional echocardiographic assessments (mitral inflow curve, pulmonary venous curve) of early subclinical cardiotoxicity following chemotherapy, particularly when chemicals of the anthracycline group are used. Our additional purpose was to confirm whether TDI is a more sensitive method in the detection of diastolic dysfunction.
Patients and Methods
To verify our hypothesis we analyzed the information about cardiotoxicity collected with the two methods about the patient and the control group at the same time with the same methods during the two years of follow-up. For easier comparability diastolic dysfunction was examined at all time with both methods.
Study Population
The prospectively collected and selected database of oncology of Uzsoki hospital from April 2003 to August 2005 was analyzed. Forty female patients (31 to 65 years, mean 49 ± 10 years) were recruited for the study, who were operated on malignant breast cancer, were chemotherapy-naive and did not have any cardiovascular risk factors. Exclusion criteria were the following: hypertension (severe or mild), anemia, diabetes mellitus, coronary heart disease, left ventricular hypertrophy, severe aortic stenosis, mitral valve disease, cardiomyopathy or irradiation of the left side of the thorax or thoracic cavity.
The cancer was in the right breast of the patients, thus no patient underwent mediastinal or left sided thoracic irradiation. Patients with lower or medium risk of invasive breast cancer underwent postoperative chemotherapy, consisting of four series of EC or AC infusions. The cumulative dose of doxorubicin was 240 mg/m2, and the cumulative dose of epirubicin was 360 mg/m2. The control group consisted of twenty healthy women aged between 33 and 62 years (mean 50 ± 9 years) without any cardiovascular risk factors, who were observed with the same protocol.
Supportive therapy was not an exclusion criterion (e.g. palliative irradiation in other localization, painkillers, antiemetics and bisphosphonates).
Study Method
Cardiologic monitoring was performed at the following stages: before initiation of chemotherapy (T0); 3 months after the second chemotherapy, which is nearly in the middle of the total treatment (T1); immediately after the fourth chemotherapy, which means the end of the total therapy (6 months) (T2); 1 year and 2 years after the start of chemotherapy (T3 and T4). At all times, cardiologic examination, standard echocardiographic measurement and TDI were performed, as described below.
Cardiologic Examination
Besides the cardiological history, findings of physical examinations, especially the cardiovascular conditions were recorded. A standard 12-lead electrocardiogram (ECG) was recorded and blood pressure was measured at rest. In order to reproduce data adequately, both the study and the control group were examined by the same cardiologist. ECG was simultaneously recorded during echocardiography.
Echocardiographic Study
The echocardiograms were performed with a commercially available echocardiographic device (Vivid 3, GE Medical System, Horten, Norway) in the echolaboratory of the cardiology department of the Uzsoki hospital. For purposes of comparability and further processing the images were recorded digitally.
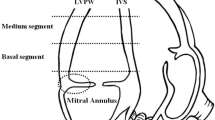
M-mode recordings were performed in parasternal long-axis view at the level under the apex of the mitral valves. The aortic root, LV end-diastolic dimension (LVEDd) and end-systolic dimension (LVEDs); the thickness of the left ventricular septum and posterior wall in systole (IVSs and LVPWs) and in diastole (IVSd and LVPWd); and the atrial dimension were measured. Left ventricular end-diastolic and end-systolic volumes as well as the ejection fraction (EF) were calculated according to the modified Simpson rule.
Doppler gain and filters were adjusted to obtain the best spectral recordings. Mitral flow velocities were recorded from an apical four-chamber view by placing the pulsed-wave Doppler sample volume between the tips of the mitral valves in the centre of the flow stream. The following parameters were derived: peak early (mitral E velocity) and atrial (mitral A velocity) flow velocities, E/A ratio and deceleration time of the E wave. From the apical four-chamber view the pulmonary venous flow velocities were recorded by placing the pulsed-wave Doppler sample volume approximately 1 cm into the right upper pulmonary vein. The pulmonary venous peak systolic (pulmonary S) and peak diastolic (pulmonary D) flow velocities, S/D ratio, peak reverse flow velocity and duration due to left atrial systole were recorded.
In all views, wall motion, valve disorders, and the occurrence of accidental pericardial effusion were examined.
Tissue Doppler Imaging (TDI)
By activating the TDI function in the same echocardiographic machine, recordings of the mitral annular velocities were made with pulsed-wave TDI. To obtain the best quality recordings, filter settings and gains were adjusted to the minimal optimal level to minimize artifact and eliminate the signals produced by the transmitral flow. From the apical four-chamber view, four different sites of the mitral annulus were selected. By placing the TDI cursor on the septal side of the mitral annulus and having the movement of the mitral annulus align with the sample volume line, the recordings of annular velocity at the interventricular septum were obtained along the long axis of the left ventricle. From the apical four-chamber view, the mitral annular velocities of the LV lateral wall were also recorded by moving the sample volume at the lateral site of the mitral annulus. The velocities at the anterior and inferior sites of the mitral annulus were also recorded from the apical two-chamber view in a similar way. Three major velocities were recorded from all four mitral annular sites, one of them being the positive systolic velocity (S velocity) when the mitral ring moved toward the cardiac apex. The other two negative diastolic velocities, the early phase (Ea diast. vel.) and the late phase of diastole (Aa diast. vel.) were recorded when the mitral annulus moved toward the base away from the apex.
In chemotherapy-related cardiomyopathy besides the global systolic and diastolic function the regional wall motion also deteriorates and has to be monitored. In the pulsed TDI the sample has to be placed in the middle of the septal and posterior wall in parasternal long axis view.
A mean of three consecutive cycles was used to calculate all tissue Doppler echocardiography parameters.
Statistics
Data were analyzed with Kolmogorov–Smirnov normality and the different statistical tests were performed accordingly. Data are presented as mean value ± SD. Comparisons of baseline characteristics between the groups were assessed using an independent t test. For the analysis of the changes in heart rate, blood pressure and standard echo parameters like mitral inflow and annulus velocity parameters in each time point paired t test was used in each group. The SPSS Version 10.0 software (SPSS Inc., Chicago, IL) was used for the statistical analysis and a p value of 0.05 or less was considered as statistically significant.
Results
Before the start of chemotherapy (T0) there was no difference between the two groups in mean age, risk factors, general physical parameters, blood pressure and pulse. Similarly, there was no significant difference in the standard echocardiographic parameters and tissue Doppler imaging measurements in either segment. The two groups could be compared with these parameters. After administrations of drugs there were slight changes in basic circulation parameters at the different times of measurements (Table 1).
Pulse rate increased in the cancer group after the first (T1) and second chemotherapy cycle (T2) however, it became significant only after one year of follow-up (T3), but even then it was not clinically relevant. Pulse got back to normal at the end of the two years (T4) of follow-up.
Blood pressure in the cancer group showed a slight, statistically significant, but clinically still not relevant drop after the second cycle (T2) and it normalized at the end. In the control group neither the pulse nor the blood pressure changed during the two-year period of follow-up. Symptoms of circulation disorder were observed with particular attention. Chest pain or any signs of circulation disorder could not be detected in either group. There were no ECG abnormalities in the cancer group over the 2 years of follow-up.
Mild enlargement of the left atrium after the second therapy (T2) and after 1 year (T3) enlargement of the left ventricle could be measured with echocardiography in the cancer group, which were significant changes compared with the previous measurements. Regarding the ejection fraction correlating with the clinical status there was no considerable change.
Conventional echo parameters of diastolic function indicated the relaxation disorder soon after the first treatment (T1). The first peak of the mitral inflow wave (mitral E wave velocity) gradually decreased while the peak of the second wave (mitral A wave velocity) showed a rising tendency. Their quotient (E/A) decreased accordingly and showed a significant change already at T1, the reduction remaining significant during the whole follow-up period. The other parameters of diastolic function, e.g. the two waves of pulmonary venous curve (pulmonary venous S and D wave) and their quotient (S/D) also described the diastolic dysfunction properly.
The Ea and Aa diastolic velocities and their ratio (Ea/Aa) measured with TDI showed a change at T1 similar to the measurements with the conventional method, which remained significant until the end of the study (Table 2). We mention that the systolic fiber-shortening velocity of the segments (S wave) also changed and they showed a decreasing tendency from T1 to T3 however, the values were higher at T4.
Besides the mean values above, the multiple analysis of patients showed that 22 patients (55%) had normal diastolic function at T1, in 18 patients (45%) diastolic dysfunction could be detected with Tissue Doppler Imaging, in 16 patients (40%) with both methods (the conventional and the TDI method; Fig. 1). At the end of the study (T4) these data changed, because late myocardial lesion could be demonstrated with either method in all patients. At this point diastolic dysfunction was detected in 27 patients (67.5%) upon the conventional mitral inflow curve and the pulmonary venous curve, but in 13 patients (32.5%) only with TDI.
Analysis of E/Ea representing the left ventricular loading pressure showed that after the second administration of chemotherapy (T2) the loading pressure significantly increased (Fig. 2).
Discussion
Anthracyclines are widely used as adjuvant chemotherapy for breast cancer patients. The risk of developing cardiac dysfunction after administration of chemotherapy for the treatment of aggressive malignancies, both solid and hematologic, was published four decades ago [14, 30]. Congestive heart failure, malignant arrhythmias, stimuli and propagation disorders and sudden death are the clinically relevant side effects, which may appear years or decades after the treatment [12, 15–17, 27].
Early detection of subclinical cardiotoxicity and prevention of the consequential heart failure have permanently been a great challenge for oncology. The rate of subclinical cardiotoxicity detected with traditional methods is estimated between 20–75% in different studies [4, 15, 19, 21, 27, 28, 32]. The goal is to minimize the myocardial damage through limitation of doses of anthracyclines and changes in therapeutical protocol with routine cardiologic monitoring, proper cardiovascular risk assessment and follow-up. The rate of heart failure related to anthracycline therapy among patients with risk factors is estimated between 15–20%, the rate among patients without any risk factors is 2% [8]. This fact emphasizes not only the importance of cardiovascular risk stratification and follow-up, but requires a method for early detection of cardiotoxicity. As written in the introduction, the traditional Doppler mitral inflow measurement for cardiotoxicity is influenced by several factors.
An advantage of tissue Doppler imaging over the conventional method is that it can measure the myocardial velocity in both systolic and diastolic periods independent of any factors [2]. It is a new finding that TDI can detect the regional abnormalities before any changes in global function. Myocardial relaxation properties are complex, determined by the internal processes and structure (e.g. active and passive elasticity) of the heart and by external factors (right ventricular pressure, preload, afterload, heart rate, pericardial and pleural pressure). In contrast to the standard Doppler echocardiography, TDI can measure the myocardial tissue velocity during systole and diastole, which directly determinates the myocardial contractility and relaxation [24]. A number of studies have been performed on the applicability of TDI and on detecting early myocardial impairment induced by cardiotoxic chemotherapy [9, 10, 31]. Our study has confirmed the feasibility of TDI in early detection of cardiotoxicity, as well [19].
In our present study we investigated whether the previously detected diastolic dysfunction caused by chemotherapy changed during the first two years after initiation, and whether systolic dysfunction deteriorated after this period of time. In cases of patients after treatment with anthracyclines Tassan-Mangina and collaborators found that TDI can be used for detecting the early diastolic dysfunction, which in some cases may be followed by systolic dysfunction years after the therapy [31].
In our actual study, the initial similarity between the treated and the healthy group regarding heart rate disappeared; the pulse in the treated group was significantly higher after one year. Higher frequency is likely linked to cardiotoxicity. While in the acute period the background of tachycardia is known [26], after a year the myocardial impairment, cardiomyopathy, remodelling [28] and the consequent sympathicotonia are responsible for arrhythmias. Since this difference disappeared again at the end of the 2-year period, it is assumed to be a reversible process.
There was no clinically relevant difference in blood pressure between the two groups, and as an independent risk factor this did not lead to diastolic dysfunction.
We found a significant difference in size of the left atrium and ventricle after the first year of follow-up, which persisted until the end of the study. However, it was a mild enlargement, which lead neither to clinical deterioration of circulation nor to notable change in the pump function. Similarly to our results, several authors described this non-significant enlargement [9, 13] without remarkable deterioration of the ejection fraction.
Comparing the traditional and novel method we confirm that both of them are feasible to detect the late, subclinical cardiotoxicity following anthracycline chemotherapy in young female patients without any risk factors. Both methods indicate the significant change of diastolic dysfunction parameters (E, A, E/A, S/D, Ea/Aa) soon after the first treatment (T1). Serial analysis of patients confirmed the obvious benefit of modern TDI. TDI is a more sensitive method because the diastolic dysfunction could be confirmed very soon, at T1 in 18 (45%) patients in contrast to the 16 (40%) patients examined with the traditional method. The difference in sensitivity was larger at T4 (40 vs. 27 patients). Regarding the fact that TDI is independent of numerous factors and easy to carry out, it has a place in routine diagnostic.
Our present study verified the applicability of TDI in early detection of late cardiotoxicity in accordance with literature data. On one hand, we established that the detection of diastolic dysfunction with TDI is more accurate as compared to standard noninvasive echocardiographic methods. On the other hand, we pointed out that cardiotoxic chemotherapy might result in manifest cardiomyopathy even in young female patients without risk factors. According to existing data, the rate of clinically relevant cardiac decompensation in patients with breast cancer treated with standard anthracycline is 0.5–1%, with the elderly people and those who had previous heart disease are being more susceptible [5]. Former studies barely emerged that this problem occurs in patients with previous heart disease. In contrast, our results indicate that the commercial medium dose of anthracycline may lead to cardiac injury even in patients with intact heart.
In our study we examined a young group with low risk, who were healthy in other respects. Presently, there are no established methods for cardiologic screening or proper follow-up for the detection of early or late cardiotoxicity in patients who need invasive oncological therapy and have more risk or a cardiovascular disease.
Further investigations are worthwhile to follow cardiomyopathy after more aggressive protocols and new therapeutical schemas (Herceptin, taxanes, etc).
Limitations of the Study
Diastolic dysfunction may occur without any inclination with age. The incidence among population over 60–65 years without any risk factors is 35–40% [11, 23]. There was a younger population in the treated and control groups (mean age 49 and 50 years, respectively). Therefore, patients in the control group had no risk factors, were in the same age and we did not detect diastolic dysfunction in the members.
The limitations of pulsed wave Doppler technique are: (1) necessity of manual settings; (2) it gives a limited disintegration, making impossible to separate subendocardial and subepicardial myocardium velocity; (3) it is not possible to have a picture of different ventricular segments at the same time; (4) different equipments operate in different frequency ranges with different sensitivity and filters. As a result, comparisons are not reliable.
Abbreviations
- AC:
-
doxorubicin and cyclophosphamide
- EC:
-
epirubicin and cyclophosphamide
- ECG:
-
electrocardiography
- EF:
-
ejection fraction
- IVSs and IVSd:
-
thicknesses of the left ventricular septum in systole and in diastole
- LVPWs and LVPWd:
-
thicknesses of the left ventricular posterior wall in systole and in diastole
- LVEDs and LVEDd:
-
left ventricular end-diastolic dimension in systole and in diastole
- TDI:
-
tissue Doppler imaging
References
Alam M, Wardell J, Andersson E, Samad BA, Nordlander R (2000) Effects of first myocardial infarction on left ventricular systolic and diastolic function with the use of mitral annular velocity determined by pulsed wave Doppler tissue imaging. J Am Soc Echocardiogr 13:343–352
Aranda JM Jr, Weston MW, Puleo JA, Fontanet HL (1998) Effect of loading conditions on myocardial relaxation velocities determined by Doppler tissue imaging in heart transplant recipients. J Heart Lung Transplant 17:693–697
Billingham ME (1984) Evaluation of anthracycline cardiotoxicity: predictive ability and functional correlation of endomyocardial biopsy. Cancer Treat Symp 3:71–76
Bu’Lock FA, Mott MG, Oakhill A, Martin RP (1995) Left ventricular diastolic function after anthracycline chemotherapy in childhood: relation with systolic function, symptoms, and pathophysiology. Br Heart J 73:340–350
Burstein H, Winer E (2000) Primary care for survivors of breast cancer. N Engl J Med 343:1086–1094
Canal P, Gamelin E, Vassal G, Robert J (1998) Benefits of pharmacological knowledge in the design and monitoring of cancer chemotherapy. Pathol Oncol Res 4:171–178
Dandel M, Hummel M, Muller J, Wellnhofer E, Meyer R, Solowjowa N, Ewert R, Hetzer R (2001) Reliability of tissue Doppler wall motion monitoring after heart transplantation for replacement of invasive routine screenings by optimally timed cardiac biopsies and catheterizations. Circulation 104(Suppl 1):I184–I191
Kantrowitz NE, Bristow MR (1984) Cardiotoxicity of antitumor agents. Prog Cardiovasc Dis 27:195–200
Kapusta L, Thijssen JM, Groot-Loonen J, Antonius T, Mulder J, Daniels O (2000) Tissue Doppler imaging in detection of myocardial dysfunction in survivors of childhood cancer treated with anthracyclines. Ultrasound Med Biol 26:1099–1108
Kapusta L, Thijssen JM, Groot-Loonen J, van Druten JA, Daniels O (2001) Discriminative ability of conventional echocardiography and tissue Doppler imaging techniques for the detection of subclinical cardiotoxic effects of treatment with anthracyclines. Ultrasound Med Biol 27:1605–1614
Klein AL, Burstow DJ, Tajik AJ, Zachariah PK, Bailey KR, Seward JB (1994) Effects of Age on left ventricular dimensions and filling dynamics in 117 normal persons. Mayo Clin Proc 69:212–224
Krischer JP, Epstein S, Cuthbertson DD, Goorin AM, Epstein ML, Lipshultz SE (1997) Clinical cardiotoxicity following anthracycline treatment for childhood cancer: the Pediatric Oncology Group experience. J Clin Oncol 15:1544–1552
Krupicka J, Markova J, Pohlreich D, Kozak T, Linkova H, Diehl V (2002) German Hodgkin's Lymphoma Study Group. Echocardiographic evaluation of acute cardiotoxicity in the treatment of Hodgkin disease according to the German Hodgkin's Lymphoma Study Group. Leuk Lymphoma 43:2325–2329
Lefrak EA, Pitha J, Rosenheim S, Gottlieb JA (1973) A clinico-pathologic analysis of adriamycin cardiotoxicity. Cancer 32:302–314
Lipshultz SE, Colan SD, Gelber RD, Perez-Atayde AR, Sallan SE, Sanders SP (1991) Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Eng J Med 324:808–815
Lipshultz SE, Colan SD, Walsh EP, Sanders SP, Sallan SP (1990) Ventricular tachycardia and sudden unexplained death in late survivors of childhood malignancy treated with doxorubicin. Pediatr Res 27:145A
Lipshultz SE, Lipsitz SR, Mone SM, Goorin AM, Sallan SE, Sanders SP, Orav EJ, Gelber RD, Colan SD (1995) Female sex and drug dose as risk factors for late cardiotoxic effects of doxorubicin therapy for childhood cancer. N Eng J Med 333:1359–1360
Nagueh SF, Mikati I, Kopelen HA, Middleton KJ, Quinones MA, Zoghbi WA (1998) Doppler estimation of left ventricular filling pressure in sinus tachycardia. A new application of tissue doppler imaging. Circulation 98:1644–1650
Nagy AC, Tolnay E, Nagykalnai T, Forster T (2006) Cardiotoxicity of anthracycline in young breast cancer female patients: the possibility of detection of early cardiotoxicity by TDI. Neoplasma 53:511–517
Nakayama K, Miyatake K, Uematsu M, Tanaka N, Kamakura S, Nakatani S, Yamazaki N, Yamagishi M (1998) Application of tissue Doppler imaging technique in evaluating early ventricular contraction associated with accessory atrioventricular pathways in Wolff–Parkinson–White syndrome. Am Heart J 135:99–106
Nysom K, Colan SD, Lipshultz SR (1998) Late cardiotoxicity following anthracycline therapy for childhood cancer. Prog Pediatr Cardiol 8:121–128
Pela G, Bruschi G, Cavatorta A, Manca C, Cabassi A, Borghetti A (2001) Doppler tissue echocardiography: myocardial wall motion velocities in essential hypertension. Eur J Echocardiogr 2:108–117
Rakowski H, Appleton C, Chan KL, Dumesnil JG, Honos G, Jue J, Koilpillai C, Lepage S, Martin RP, Mercier LA, O’Kelly B, Prieur T, Sanfilippo A, Sasson Z, Alvarez N, Pruitt R, Thompson C, Tomlinson C (1996) Canadian consensus recommendation for the measurement and reporting of diastolic dysfunction by echocardiography. J Am Soc Echocardiol 9:736–760
Shimizu Y, Uematsu M, Shimizu H, Nakamura K, Yamagishi M, Miyatake K (1998) Peak negative myocardial velocity gradient in early diastole as a noninvasive indicator of left ventricular diastolic function: comparison with transmitral flow velocity indices. J Am Coll Cardiol 32:1418–1425
Sogaard P, Hassager C (2004) Tissue Doppler imaging as a guide to resynchronization therapy in patients with congestive heart failure. Curr Opin Cardiol 19:447–451
Steinberg JS, Cohen AJ, Wasserman AG, Cohen P, Ross AM (1987) Acute arrhythmogenicity of doxorubicin administration. Cancer 60:1213–1218
Steinherz LJ, Steinherz PG, Tan C (1995) Cardiac failure and dysrhythmias 6–19 years after anthracycline therapy: a series of 15 patients. Med Pediatr Oncol 24:352–361
Steinherz LJ, Steinherz PG, Tan CT, Heller G, Murphy ML (1991) Cardiac toxicity 4 to 20 years after completing anthracycline therapy. JAMA 266:1672–1677
Tabata T, Oki T, Yamada H, Abe M, Onose Y, Thomas JD (2000) Subendocardial motion in hypertrophic cardiomyopathy: assessment from long- and short-axis views by pulsed tissue Doppler imaging. J Am Soc Echocardiogr 13:108–115
Tan C, Tasaka H, Yu KP, Murphy ML, Karnofsky DA (1967) Daunomycin, an antitumor antibiotic, in the treatment of neoplastic disease: clinical evaluation with special reference to childhood leukemia. Cancer 20:333–353
Tassan-Mangina S, Codorean D, Metivier M, Costa B, Himberlin C, Jouannaud C, Blaise AM, Elaerts J, Nazeyrollas P (2006) Tissue Doppler imaging and conventional echocardiography after anthracycline treatment in adults: early and late alterations of left ventricular function during a prospective study. Eur J Echocardiogr 7:141–146
Uematsu M, Nakatani S, Yamagishi M, Matsuda H, Miyatake K (1997) Usefulness of myocardial velocity gradient derived from two-dimensional tissue Doppler imaging as an indicator of regional myocardial contraction independent of translational motion assessed in atrial septal defect. Am J Cardiol 79:237–241
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagy, A.C., Cserép, Z., Tolnay, E. et al. Early Diagnosis of Chemotherapy-induced Cardiomyopathy: a Prospective Tissue Doppler Imaging Study. Pathol. Oncol. Res. 14, 69–77 (2008). https://doi.org/10.1007/s12253-008-9013-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-008-9013-4




