Abstract
Our goal in this chapter is to demonstrate the operational benefits that can be gained by implementing real-time, big data analytics in a healthcare setting and the concomitant influence of organizational culture on adoption of the technology. Benefits include improving the quality and accuracy of clinical decisions, processing health records efficiently, streamlining workflow, and improving patient satisfaction. We demonstrate these benefits by investigating patient-physician interactions in a large medical practice at WellSpan Health, and we compare the observed workflow with a modified one made possible with a big data, real-time analytics platform. By comparing these two states, we illuminate the lost opportunity and the value left on the table by legacy behaviors and processes. In addition, we uncover organizational characteristics that create a climate for cultural modification and initial acceptance of big data, real-time analytics in a change-resistant organization. The combination of academic research and practitioner implementation shows that optimization of clinical operations is a key first step toward gaining user acceptance of big data technologies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Healthcare in the United States is undergoing a rapid transformation toward using data and analytics to provide improved patient care, evidence-based management, and outcome accountability (Kayyali, Knott, & Van Kuiken, 2013; Wang & Hajli, 2016). Data analytics is based on integrating information from payers, hospitals, laboratories, and physician offices, among others, as fundamental to this shift (Paradise et al., 2013). Such large datasets and the concomitant integration of multiple data types are often referred to as “big data.” Analytics associated with big data enables assessment of performance, cost, and utilization metrics and is essential to driving improvements in care management (Paradise, Gold, & Wang, 2013). The next wave of innovation in healthcare is expected to be in real-time health systems based on these data and “the transformation of the healthcare delivery organization into one that is more aware, collaborative and patient-centric” (Runyon, 2016). WellSpan Health, the case study for this paper, is an early adopter of healthcare analytics and is moving rapidly toward enabling and acquiring the underlying data for real-time systems. In this paper, we focus on process analysis and the illumination of workflow inefficiencies to guide the culture change necessary for successful adoption of a new electronic health record (EHR).
The objectives of this chapter are (1) to present management challenges in aligning business strategies and analytics in a complex healthcare organization, (2) to demonstrate operational benefits that can potentially be gained with real-time analytics, and (3) to suggest industry–academic collaboration to address alignment gaps.
WellSpan Health
WellSpan Health is a community-based integrated health system located in South Central Pennsylvania with more than 15,000 employees and 140 patient care locations (WellSpan, 2017). This not-for-profit organization includes a multispecialty medical group of more than 1200 physicians and advanced practice clinicians, a regional behavioral health organization with services for children and adults, and 6 hospitals. WellSpan’s hospitals include WellSpan York Hospital (a 580-bed community teaching hospital and trauma center with 7 residency programs, 5 allied health schools, and associated training programs), WellSpan Gettysburg Hospital (a 76-bed acute care hospital), WellSpan Good Samaritan Hospital (a 170-bed acute care hospital), WellSpan Ephrata Community Hospital (a 130-bed acute care hospital), WellSpan Philhaven (a behavioral health hospital), and the 70-bed WellSpan Surgery and Rehabilitation Hospital. WellSpan York Hospital’s Regional Resource/Level 1 Trauma Center is accredited by the Pennsylvania Trauma Systems Foundation and is the only accredited trauma center in York, Adams, and Franklin counties.
With a strong focus on the health of the community, WellSpan has been working to transform the delivery of care to meet the changing needs of its central Pennsylvania communities. For example, WellSpan has attempted to reduce hospital medication errors through double bar-code scanning and decision support technologies (Phillips-Wren & McKniff, 2012, 2015). As the healthcare organization has grown with the addition of new hospitals, physicians, and services, WellSpan has increasingly focused its efforts on helping individuals develop a relationship with a primary care physician who can partner with them and the health system to become healthy and stay that way (WellSpan, 2017). Each patient’s information is available to providers at any WellSpan location through a sophisticated EMR, and their care is coordinated by teams of physicians, health coaches, social workers, and other professionals.
Although adoption of these technologies offers many benefits, including operational efficiencies, physicians have been slow to adapt to the needed changes in workflow. In the following section, we provide background on big data analytics in healthcare and aligning organizational culture with adoption of the technology.
Background
“Big Data” Analytics
The healthcare industry is generating “big data” in the form of individual patient history due to the large uptake of electronic health records (EHRs) . In 2015, 96% of nonfederal acute care hospitals reported use of certified electronic health record (EHR) technology with similar usage at state levels (Henry, Pylypchuk, Searcy, & Patel, 2016). Functionality is also increasing, and efforts are now shifting to interoperability of health information and using technology to support reform of care delivery (Henry et al., 2016). These EHRs contain quantitative data such as laboratory tests, qualitative data such as physician observations, and transactional data such as healthcare delivery records. Although the healthcare industry has utilized scientific inquiry and rigorous analysis of experimental data such as randomized trials to inform practice, big data and associated analytics such as machine learning offer new ways to improve the quality and efficiency of healthcare delivery (Murdoch & Detsky, 2013).
Big data add new dimensions to analytics (Phillips-Wren et al., 2015). Big data can be described as data that have one or more of the characteristics of volume, velocity, and variety (Goes, 2014; SAS 2017), or the three V’s. In addition, these data can be generally represented as either structured or unstructured (Agarwal & Dhar, 2014). Volume indicates the huge and growing amount of data being generated, with more data often at higher granularity in EHRs . Velocity indicates the speed at which data are being generated from digital sources such as patient monitoring with wearable sensors, offering the potential for real-time analysis and response. Variety refers to the variation in types of data such as physician observations or X-ray imaging. Structured data reside in spreadsheets and relational databases that impose a structure for storage and access. Semi-structured data lack a strict and rigid format but have identifiable features such as images being tagged with type, date, and patient. Human language is unstructured data of growing importance to analytics using tools to perform activities such as text mining. Other characteristics are sometimes added to the three V’s such as variability and complexity (SAS, 2017) or value and veracity (Raghupathi & Raghupathi, 2014) to recognize additional difficulties that organizations encounter in implementing data-intensive applications.
Business intelligence and big data analytics refer to a set of analytical techniques that have been developed to obtain insights from large, complex datasets of varying types using advanced data storage, management, analysis, and visualization technologies (Chen, Chiang, & Storey, 2012). These approaches are based on mathematical models, statistical techniques, decision support methods, data science approaches, and computer science algorithms such as machine learning integrated to address the unique challenges in big data. Generally, analytics can be descriptive, predictive, or prescriptive. Descriptive analytics refers to a description of data and may use exploratory methods to attempt to understand data. Predictive analytics utilizes historical data to predict or forecast a future state. Prescriptive analytics is an emerging field that attempts to find the optimal course of action by examining various possibilities and decision options (Phillips-Wren, Iyer, Kulkarni, & Ariyachandra, 2015). Although many of these methodologies have been standard in data analysis for a long time, in the case of big data, there is a larger amount and variety of data under consideration, as well as the possibility of real-time data acquisition and analysis.
Specific to healthcare and based on analysis of 26 big data implementation cases, derived benefits from analytics were classified into five benefit categories: IT infrastructure, operational, organizational, managerial, and strategic (Wang, Kung, & Byrd, 2016). The two benefits noted most often were IT infrastructure (reduce system redundancy, avoid unnecessary IT costs, and transfer data quickly among healthcare IT systems) and operational benefits (improve the quality and accuracy of clinical decisions , process a large number of health records in seconds, and reduce the time of patient travel) (Wang et al., 2016). “This implies that big data analytics has a twofold potential as it implements in an organization. It not only improves IT effectiveness and efficiency, but also supports the optimization of clinical operations. In addition, [the] results also indicate that big data analytics is still at an early stage of development in healthcare due to the limited benefits of big data analytics at the organizational, managerial, and strategic levels” (Wang et al., 2016, p. 8).
In this paper, we focus on the optimization of clinical operations by investigating one service delivery area in WellSpan Health that can use big data analytics to streamline operations, improve patient safety, and enhance clinical decision-making . In this case, there is potential to impact all three levels of the system.
“Big Data” in Healthcare Practice
The healthcare industry appears to be repeating the trend of computerization and data management that has occurred in other industries (Sanders, Burton, & Protti, 2013). Sanders et al. (2013) describe three phases. Phase I consists of data collection and transaction-based processing and is reflected in EMR adoption. Phase II is information sharing, facilitated in healthcare by Healthcare Information Exchanges (HEI). Phase III is the data analysis phase characterized by enterprise data warehouses and analysis of “small” and “big” data. “Small” data are not necessarily small in volume – they may be huge datasets; they are simply able to be collected internally and analyzed using existing tools. In many organizations, analytics associated with even “small” data represents a significant step forward.
Moving to “big data” analytics presents even more challenges in healthcare settings. One way to overcome the challenges is to follow a generalized methodology consisting of four steps: (1) a concept statement to establish the need based on the three V’s; (2) a proposal development stage; (3) fleshing out of the methodology including data and platform identification, data acquisition and cleaning, data transformation , and data analysis; and (4) deployment including testing, evaluation, and validation (Raghupathi & Raghupathi, 2014). “This process differs from routine analytics only in that the techniques are scaled up to large data sets” (Raghupathi & Raghupathi, 2014, p. 7). As we will see later, the specific methodology utilized by WellSpan Health follows this general process.
A more specific Healthcare Analytics Adoption Model is shown in Fig. 8.1 and provides a way to assess expansion of analytics capabilities and maturity in data sources, complexity, data literacy, and data timeliness (Sanders et al., 2013). To progress through the steps, an organization must have standard ways of collecting data and assessing its validity, integrating data, automating reporting, reducing variability in processes, tailoring patient care, predicting outcomes to suggest interventions, and tailoring patient care. The nine levels shown in Fig. 8.1 move from inconsistent versions of the truth at Level 0 through standardization processes in Levels 1 and 2. Internal standardization can be obtained with an enterprise data warehouse that employs consistent language, norms, and governance.
Healthcare analytics adoption model. (Adapted from Sanders et al., 2013)
Analytics is employed on Level 3 to develop automated internal reports and new knowledge with internal data for executive decision-making, and it is extended to impact external reporting in Level 4 and clinical best practice in Level 5. Levels 6–8 require data beyond the organization and can be considered big data . Level 6 at the point-of-care uses population metrics to guide patient care, and those metrics are drawn by analysis of the larger world body of patients. Predictive risk models in Level 7 require external data to include in the analysis such as collaboration between physicians, hospitals, payers, and patients. Level 8 utilizes analytics toward patient health optimization and requires personalized data such as genetic data.
Organizations do not move through these phases linearly, and they may be working on multiple levels simultaneously. However, “the return on investment of EMRs … will not be realized … until the healthcare industry … commits culturally to the exploitation of analytics, − that is, to become a data-driven culture, incented economically to support optimal health at the lowest cost” (Sanders et al., 2013, p. 8).
Even with the advantages of these processes, there is resistance in healthcare. Evidence-based medicine (EBM) is “the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients” (Sackett, Rosenberg, Gray, Haynes, & Richardson, 1996). “EBM stands in contrast to anchoring decisions on personal habits, tangible and intangible incentives unrelated to care, or medical traditions that have little or no empirical validation” (Fichman, Kohli, & Krishnan, 2011). Barriers to widespread adoption of analytics include lack of knowledge and misconceptions about the actual effectiveness of treatment, the difficulty of diffusing that knowledge, and practitioner resistance that is often connected to a desire for autonomy, incentive conflicts, and fear of litigation (Fichman et al., 2011). Many of these issues of technology adoption and culture change have been faced and studied by the information systems community for decades (Karahanna, Straub, & Chervany, 1999), and the lessons learned can be applied to healthcare.
“In healthcare, the foremost concern for management is the people that compose it – the key stakeholders – be they patients, physicians, nurses, and other medical staff, referring providers, or representatives from the local community. Empowering these individuals and increasing the quality and transparency of decision-making are key goals for any business analytics initiative. Therefore, the organization needs to establish business analytics as an organizational and cultural objective, a component of its long-term strategy. However, to realize these benefits, clinicians, support staff, and leadership all need to understand and appreciate the importance of business analytics as tools and as a fundamental process within the organization. Otherwise, the organization will continue to underinvest and staff will be skeptical of the value of recording data as a matter of course” (Ward, Marsolo, & Froehle, 2014, p. 577).
Organizational Culture and Technology Adoption
Culture has been framed in various ways, for example, as ideologies, beliefs, assumptions, shared values, collective will, norms, practices, symbols, rituals, myths, ceremony, and tacit versus explicit components (Leidner & Kayworth, 2006). Organizational culture is an important factor in absorbing and implementing new technology in a healthcare setting (Caccia-Bava, Guimaraes, & Harrington, 2006). A review of the literature shows that there is a range of social, technical, and organizational characteristics that need to be managed to ensure that technology innovations are useful to healthcare organizations and individuals; however, these factors are interrelated and complex (Cresswell & Sheikh, 2013).
Information systems research has a rich history of investigating the influence of culture (e.g., national, organizational, group) and the adoption of IT in organizations (Leidner & Kayworth, 2006). In particular, technology acceptance and use has been studied at length in the information systems community (Phillips-Wren & McKniff, 2015). Perhaps the best-known theoretical model is the technology acceptance model (TAM) (Davis, 1989) and its extensions based on the theory of reasoned action (Fishbein & Ajzen 1975) that attitudes and norms (e.g., influenced by culture) predict behavioral intention which predicts actual behavior. TAM has been utilized to understand physician acceptance of telemedicine, decision support systems in primary care, physicians’ intention to accept innovation, adverse event reporting, technology within hospitals, and healthcare professionals’ intention to utilize healthcare information systems (Phillips-Wren & McKniff, 2012, 2015). Technology adoption is a necessary important first step toward a data-driven organization, and it is the aspect that we focus on in this paper.
In the following section, we apply these concepts to analyze a situation in a healthcare organization dedicated to moving toward real-time analytics and achieving the benefits of a data-driven culture for its organizational processes and patient care.
Methodology and Discussion of Results
Issues, Controversies, and Problems
As the WellSpan organization began preparations for the substantial undertaking of replacing multiple legacy systems with an enterprise-wide EHR , a variety of departments were identified as being high risk for adoption of the workflows necessary for successful EHR implementation. Direct observation of the service delivery processes within these departments reinforced these concerns. “Workflows must be designed in a way that assures the important data elements will be captured during a visit and that these tasks minimally disrupt workflow, particularly expensive resources such as nurses and physician” (Ward, Marsolo, & Froehle, C., 2014, p. 378).
In response to an invitation from leadership of orthopedic services at WellSpan, and with full disclosure of the intent to evaluate workflow as it pertained to the EHR, we observed various teams during regularly scheduled office hours . Our initial approach provoked a Hawthorne effect where the person being observed changes their behavior in response to observation. Thus, the care teams attempted to use the computer system in ways that further broke their processes and reinforced their beliefs of computer-generated process inefficiencies. On a few occasions, the orthopedic team used this opportunity of having a captive audience to share testimonials and demonstrate functionality flaws. These dialogues introduced additional distractions and delays to such an extreme that the observers chose to remove themselves, so throughput, for the day, might be restored.
To mitigate some of the difficulties with data acquisition, a different approach was introduced in attempt to increase the opportunities of capturing accurate workflow examples. Trusted in-house personnel with clinical workflow experience shadowed the clinical support staff. These individuals gained trust of the care team and provided value in real-time while simultaneously witnessing the work-arounds. More importantly, they gained awareness via uncensored remarks justifying the work-arounds. All management levels, including site directors and practice managers, were actively involved in this undertaking which became known to the process improvement team as “WOW” WellSpan Orthopedic Workgroup.
Physicians shared a common fear that any amount of time spent interacting with the EHR is time not spent with a patient and, thus, would increase patient visit times and ultimately decrease visit volume. This deep-seated cultural belief was the foremost obstruction to the project. A paradigm shift needed to occur. The belief that the EHR is just a slow electronic form of documentation is a perhaps a valid perception, albeit outdated. Value-added data served up just-in-time to provide guidance during the fast-paced delivery of orthopedic ambulatory care needed to be proven.
“Current State” Workflow Observed in Practice
Figure 8.2 shows a traditional cross-functional workflow diagram representing the findings of our observations on the “current state.” It shows the role-based activity steps and handoffs during a typical ambulatory office visit for orthopedic evaluation or postoperative visit. Despite having a functioning EHR , physicians and their support teams employed work-arounds designed to decrease the physician’s need to interact with the computer. As shown in the diagram, the physician verbally requests the room location of the next patient to be evaluated. The support staff pause, think, and respond verbally. Following the physician’s exam, orders are verbally communicated in the charting area hallway. The details necessary to complete the electronic orders frequently require additional clarification. Decision support systems and best practice advisories appear during the order placement, and resolution of the alert often requires the expertise of the physician. This creates a recurring situation of waiting and interrupting one another for task completion or perhaps a riskier practice of the alert being addressed by a non-physician.
Note writing is another area in which the support staff devised a work-around to alleviate some of the documentation burden for the physician. However, only one person can contribute to a note at a time. This created a situation of waiting between colleagues to finish and release the note. One enhancement recommended by the care team during our observations was to allow for multiple simultaneous contributors to a note. While this might seem to make documentation faster, it has obvious inherent safety concerns.
Clinical support staff can be inadvertently put in situations in which they are practicing above their certification/license in the name of physician efficiency. Lack of standard processes and physician preferences introduced process variation that challenges support staff to work effectively with different physicians and contributes to staff attrition and retention issues.
Workflow Process for “Future State”
We suggested that by using big data technologies and analytics with the EHR , the process could be significantly simplified to a “future state” with improvements as shown in Fig. 8.3. In this workflow, the physician uses technology associated with the EHR to locate the patient; capture observations and recommendations during the patient encounter; record heath strategies such as medication, treatment, follow-up, and referrals; and move to the next patient. We suggest that although cultural changes are required to implement the new workflow, the advantages will be significant. The physician’s expertise is captured accurately, decisions are documented, patient prior encounter information is available, patient history can be incorporated into treatment plans, best practice alerts can guide decision-making in real-time, and clinical staff contact with the patient is more effective. The support staff will become more available to effect office throughput because of the previous opportunity cost of their time waiting and doing nonsupport staff responsibilities. Support staff will not be waiting to clarify verbal orders and other rework that was out of the scope of their certification/license. In addition, the capture of structured and unstructured data can be incorporated into the EHR and used to inform real-time decision-making and reporting.
Technology Acceptance and Cultural Challenges
We used the traditional tool of a cross-functional diagram to illuminate what we thought were obvious risks and delays. We created a “current state” diagram (Fig. 8.2) based on our observations and a proposed “future state” diagram (Fig. 8.3). We presented these documents to a few of the orthopedic physicians . Our technique failed. We did not successfully persuade them that a workflow change was necessary for their efficiency or for their readiness to adapt to the impending implementation of a new EHR . The culture is so ingrained, along with the fact that diagrams were developed by non-orthopedics personnel, that the diagrams were considered an inaccurate representation of the current state. Physicians feared that the recommended process changes would be detrimental to their office efficiency and, subsequently, their livelihoods.
A different approach to overcome organizational resistance to technology was needed. After discussion with leaders, we presented the workflows at an orthopedic all-staff and all-provider meeting and asked them for help validating our findings. We used custom animation via PowerPoint to make the workflow advance one activity step at a time. We replaced some of the words and squares with clip art representing physicians and staff. We did this slowly and void of judgment. The energy in the room became palpable. The staff clapped and cheered as group consensus grew and the gaps and rework were illuminated . The interactive approach overcame initial resistance as the group participated in developing the process flow.
The approach used during the team meeting was a catalyst of multiple downstream efforts to change culture and affect efficiency. The orthopedic care team realized that ineffective processes had accidently evolved in the name of efficiency. The phrase “efficiency theater” was a light way for staff to refer to a situation where rework and reduced waiting time resulted when colleagues assisted each other in using the technology effectively.
Discussion of Results: Digital Transformation at WellSpan
Within WellSpan Health, an organizational goal is the use of technology to improve the delivery of patient care. WellSpan’s mission is “Working as one to improve health through exceptional care for all, lifelong wellness and healthy communities.” The executive leadership team at WellSpan Health has embraced the challenge to provide tools necessary to deliver exceptional care. A reliable EHR , accurate real-time analytics, and clinically led information technology initiatives have provided a foundation for success.
However, this technology adoption project was initially interpreted as risky while not adding value. Using technology was viewed as slowing down the number of patients that could be seen in a day, and time is critical since charges are accrued per patient. In addition, healthcare professionals prefer to interact with humans rather than a computer. They are trained to assess a situation and make decisions without technology, so introducing technology into the workflow was not clearly an advantage. Yet they rely on discrete patient-specific data and situational health information when applying their knowledge of medicine to safely formulate their care delivery decisions. The EHR will be considered a value-added tool when physicians and nurses experience value in real-time through data analytics such as decision support alerts that interrupt the ordering of an inappropriate medication, or a population health alert that recommends an appropriate diagnostic screening exam, or a timesaving alert indicating that a procedure will not be covered by the patient’s insurer. When providers experience the embeddedness of the EHR in the delivery of safe healthcare, then digital transformation will begin to occur.
Clinical stakeholders must be involved in all phases of technology development and implementation in order to incentivize physicians and clinical end users to adopt and embrace it. The collective experience of interacting with the EHR defines usability. Issues such as slow log-on times, number of clicks to perform a task, and nonintuitive design contribute to resistance and subsequently underutilization by the end user. Just-in-time support and at-the-elbow guidance may mitigate the steep learning curve that historically has contributed to the delegation of EHR responsibilities to residents and junior staff. Such delegation further delays the hands-on experience required for adoption and increases patient risk potential because decision support is being addressed by less experienced providers.
Another technique to positively affect the rate of digital transformation is to listen to the physicians’ concerns and mitigate them when possible. If the physician is incentivized for visit volume, they must be provided tools that do not impede their ability to function at an optimal capacity. In our case, it was important not to replicate bad processes or simply automate current paper records. Lean methodologies should be applied to the workflows surrounding the physician’s workload such as strategizing and standardizing tasking, formally delegating prescription refill responsibilities, or alleviating time burdens via upstream data collection such as documentation of the patient’s preferred pharmacy.
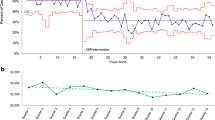
By clearly communicating organizational goals and subsequent anticipated results, members of an organization can collaborate to achieve a common goal. One example is to achieve a specific level/stage of EMR adoption model. In 2015, WellSpan Health’s hospitals were judged by a US organization, Healthcare Information and Management Systems Society (HIMSS), an American not-for-profit organization dedicated to improving healthcare in quality, safety, cost-effectiveness, and access through the best use of information technology and management systems. WellSpan received two Electronic Medical Record Adoption Model (EMRAM) certificates of achievements from HIMSS. Figure 8.4 shows the percent of hospitals achieving that level in 2015. WellSpan Surgery and Rehabilitation Hospital in York, Pennsylvania, achieved HIMSS EMRAM Level 7, and WellSpan Good Samaritan Hospital in Lebanon, Pennsylvania, achieved HIMSS EMRAM Level 6 designation in 2015.
The current HIMSS EMRAM is shown in Fig. 8.5 along with the percent of hospitals achieving each level in 2017. It differs somewhat from the Generalized Healthcare Analytics Adoption Model discussed earlier (Fig. 8.1) and the HIMSS EMRAM 2015 (Fig. 8.4). HIMSS EMRAM 2017 has seven stages and does not currently require the use of personalized data such as genetic markers as outlined in Level 8 of the Sanders et al.’s (2013) model. We discussed the generalized model in Fig. 8.1 as aspirational and applicable to all healthcare organizations, national and international, while the EMRAM 2017 model in Fig. 8.5 is an instance of a metric-driven evaluative model developed by a specific US organization (HIMSS, 2017). These standards continue to evolve.
In 2015, at the time WellSpan Surgery and Rehabilitation Hospital achieved stage 7, only 4.2% of the hospitals in the United States had achieved this designation, while 27.1% had achieved stage 6 with WellSpan Good Samaritan Hospital. In 2017 Q3, the percentage of US hospitals achieving stage 7 had risen to 6.1%, while the percentage in stage 6 was 32.7% (HIMSS, 2017). Thus, IT adoption is improving in US hospitals, although more slowly than proponents desire (Keller et al., 2017).
Bridging the Gap Between Research and Practice
A major issue in the implementation and effective use of big data analytics in an organization is convincing practitioners that the required changes are worth the effort. One way that the academic community can contribute to overcoming this perception is by theoretically researching benefits of big data analytics and documenting those benefits with real use cases.
In healthcare, academics can provide evidence that a larger population of data acquired by the EHR will improve evidence-based decision-making and lead to improved patient care. These new data enhance generalizability of medical decisions by including demographics and patient characteristics that cannot be captured in randomized trials that are necessarily limited by practicality. To be most effective, big data analytics should be delivered into the hands of the most experienced professional to affect decision-making, so the physician should personally see the data, the alerts, and best practices suggested by the data.
Academics can also apply process-flow methodologies to enhance operations using big data analytics and operational research techniques. The concept of having additional human resources to relieve physicians from tasks that do not require their expertise is logical at first glance. Physicians are trained professionals who should not be performing tasks such as record keeping. The authors agree with this premise when the task was simply transcription of notes into electronic format. However, the increasing capacity of computers to assist in complex human decision-making creates new opportunities. Using big data analytics such as that made possible with EMRs, computers can correlate patient outcomes with healthcare , identify trends and best practices in the larger population, provide individualized recommendations and alerts, and with greater precision provide information to mitigate patient harm. Thus, physicians need to interact directly with the technology as records are being created.
In the classroom, case studies such as WellSpan serve to illustrate the applicability of analytics methods to the real world and, especially for graduate students, provide an analogy to a student’s own organization. It is especially powerful to have business partners as speakers to instructional groups. This two-way dialogue between educators and members of the business community lends credence to pedagogy and relevance to the concomitant research.
Conclusion
This paper reports research on the environmental conditions needed to obtain value from big data analytics in a healthcare setting. We focused on an orthopedics unit at WellSpan Health and observed the workflow and the interaction of physician, staff, patient, and documentation processes. We found that simply having an electronic medical record available was not enough. Although real-time analytics has the potential to assist healthcare professionals with decision-making, underlying cultural processes can interfere with effective use of available data. In our case, optimization of clinical operations was a key first step toward utilizing electronic medical record systems effectively to improve patient safety and enhance clinical decision-making .
Big data analytics will continue to grow in the healthcare sector due to its proven ability to enhance medical decision-making and improve operational efficiency. Physicians and healthcare providers are becoming increasingly trusting and subsequently reliant on real-time, big data during the decision-making phases of the delivery of patient care. Not just the use of technology but the use of smart timely data will continue to be further embedded into the workflow of personnel caring for patients.
References
Agarwal, R., & Dhar, V. (2014). Editorial: Big data, data science, and analytics: The opportunity and challenge for IS Resesarch. Information Systems Research, 25(3), 443–448.
Caccia-Bava, M., Guimaraes, T., & Harrington, S. (2006). Hospital organization culture, capacity to innovate and success in technology adoption. Journal of Health Organization and Management, 20(3), 194–217.
Chen, H., Chiang, R., & Storey, V. (2012). Business intelligence and analytics: From big data to big impact. MIS Quarterly, 36(4), 1165–1189.
Cresswell, K., & Sheikh, A. (2013). Organizational issues in the implementation and adoption of health information technology innovations: An interpretative review. International Journal of Medical Informatics, 82, e73-e86.
Davis, F. D. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly, 13(3), 319–339.
Fichman, R., Kohli, R., & Krishnan, R. (2011). The role of information systems in healthcare: Current research and future trends. Information Systems Research, 22(3), 419–428.
Fishbein, M., & Ajzen, I. (1975). Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley Publishing Co.
Goes, P. (2014). Editor’s comments: Big data and IS research. MIS Quarterly, 38(3), iii–viii.
Henry, J., Pylypchuk, Y., Searcy, T., & Patel, V. (2016, May). Adoption of electronic health record systems among U.S. Non-Federal Acute Care Hospitals: 2008–2015. The Office of National Coordinator for Health Information Technology. Retrieved from https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-ehr-adoption-2008-2015.php
HIMSS Analytics. (2017). Electronic medical record adoption model. Retrieved from http://www.himssanalytics.org/emram
Karahanna, E., Straub, D., & Chervany, N. (1999). Information technology adoption across time: A cross-sectional comparison of pre-adoption and post-adoption beliefs. MIS Quarterly, 23(2), 183–213.
Kayyali, B., Knott, D., & Van Kuiken, S. (2013). The big-data revolution in US health care: Accelerating value and innovation (pp. 1–13, vol. 2(8)). Mc Kinsey & Company. Retrieved from http://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/the-big-data-revolution-in-us-health-care
Keller, E., Crowley-Matoka, M., Collins, J., Chrisman, H., Milad, M., & Vogelzang, R. (2017). Fostering better policy adoption and inter-disciplinary communication in healthcare: A qualitative analysis of practicing physicians’ common interests. PLoS One, 12(2), e0172865.
Leidner, D., & Kayworth, T. (2006). A review of culture in information systems research: Toward a theory of information technology culture conflict. MIS Quarterly, 30(2), 357–399.
Murdoch, T., & Detsky, A. (2013). The inevitable application of big data to health care. Journal of the American Medical Association, 309(13), 1351–1352. https://doi.org/10.1001/jama.2013.393
Paradise, J., Gold, M., & Wang, W. (2013, October 01). Data analytics in Medicaid: Spotlight on Colorado’s accountable care collaborative. The Kaiser Foundation. Retrieved from http://kff.org/medicaid/issue-brief/data-analytics-in-medicaid-spotlight-on-colorados-accountable-care-collaborative/
Phillips-Wren, G., Iyer, L. S., Kulkarni, U., & Ariyachandra, T. (2015). Business analytics in the context of big data: A roadmap for research. Communications of the Association for Information Systems, 37, 23.
Phillips-Wren, G., & McKniff, S. (2012). Fusing decision support into the fabric of healthcare to prevent medication errors. In DSS (pp. 27–36).
Phillips-Wren, G., & McKniff, S. (2015). Beyond technology adoption: An embeddedness approach to reduce medication errors. Journal of Organizational Computing and Electronic Commerce, 25(2), 1–20.
Raghupathi, W., & Raghupathi, V. (2014). Big data analytics in healthcare: Promise and potential. Health Information Science and Systems, 2(1), 3.
Runyon, B. (2016, May 11). Industry vision: The real-time health system (Gartner ID: G00308258.). Gartner.
Sackett, D. L., Rosenberg, W., Gray, J., Haynes, R., & Richardson, W. (1996). Evidence based medicine: What it is and what it isn’t. British Management Journal., 312(7023), 71–72.
Sanders, D., Burton, D., & Protti, D. (2013). The healthcare analytics adoption model: A framework and roadmap. HealthCatalyst. Retrieved from http://healthsystemcio.com/whitepapers/HC_analytics_adoption.pdf
SAS. (2017). Big data – What is it and why it matters. Retrieved from https://www.sas.com/en_us/insights/big-data/what-is-big-data.html
Wang, Y., & Hajli, N. (2016). Exploring the path to big data analytics success in healthcare. Journal of Business Research, 70, 287–299. Retrieved from https://doi.org/10.1016/j.jbusres.2016.08.002.
Wang, Y., Kung, L., & Byrd, T. (2016). Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological Forecasting and Social Change Retrieved from https://doi.org/10.1016/j.techfore.2015.12.019
Ward, M., Marsolo, K., & Froehle, C. (2014). Applications of business analytics in healthcare. Business Horizons, 57(5), 571–582.
WellSpan. (2017). Retrieved from https://www.wellspan.org/
Acknowledgments
We extend special thanks to Mark A Deitch, MD, MBA, Vice President, Orthopedic Service Line, WellSpan Health, for his guidance and support.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Phillips-Wren, G., McKniff, S. (2019). Aligning Operational Benefits of Big Data Analytics and Organizational Culture at WellSpan Health. In: Anandarajan, M., Harrison, T. (eds) Aligning Business Strategies and Analytics. Advances in Analytics and Data Science, vol 1. Springer, Cham. https://doi.org/10.1007/978-3-319-93299-6_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-93299-6_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-93298-9
Online ISBN: 978-3-319-93299-6
eBook Packages: Business and ManagementBusiness and Management (R0)