Abstract
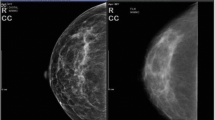
Nowadays, cancer is a major cause of women death, especially breast cancer which is most seen on ladies older than 40 years. As we know, several techniques have been developed to fight breast cancer, like a mammography, which is the preferred screening examination for breast cancer. However, despite mammography test showing negative result, there are still patients with breast cancer diagnostic, found by other tests like ultrasound test. It can be explained by potential side effect of using mammography, which can push patients and doctors to look for other diagnostic technique. In this literature review, we will explore the digital infrared imaging which is based on the principle that metabolic activity and vascular circulation, in both pre-cancerous tissue and the area surrounding a developing breast cancer, is almost always higher than in normal breast tissue. In the same way, an automated infrared image processing of patient cannot be done without a model like the hemispheric model, which is very well known. As novelty, we will give a comparative study of breast cancer detection using modern visual IT techniques view by the perspective of computer scientist.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
In a healthy body, natural systems control the creation, growth and death of cells. We can see the apparition of cancer cells when these systems don’t work right and cells don’t die at the normal rate, this results to more cell growth than cell death. In addition, breast cancer occurs when cells in the breast divide and grow without their normal control. It is a world problem which is present in every country, for example, in USA one in eight women will be diagnosed with breast cancer in her lifetime and more than 40,000 will die [1]. A reduction of this rate can be achieved with a better screening and early detection, also with an increased in awareness, and continuous improvement in treatment options. In this literature review, we will explore the Digital Infrared Imaging which is based on the principle that metabolic activity and vascular circulation, in both pre-cancerous tissue and the area surrounding a developing breast cancer, is almost always higher than in normal breast tissue. As we know, several techniques have been developed to fight breast cancer, like a mammography, which is the preferred screening examination for breast cancer [2]. Our duty is to give a clear picture of what has been done so far and what we esteemed to be the most convenient way among the state-of-the-art techniques. Later on, we will give the elements that will enhance our ideas.
2 Previous Techniques and Comments
Authors in [3] did a review, based on several articles from 2002 to 2010, which reveals Screen-film mammography (SFM) limitations, which are illustrated by its false-negative rate ranges from 4 to 34%. Even if, mammography has been considered for long time as the gold standard for breast cancer screening and detection, the need of new techniques to overcome those limitations came in evidence. Also publication [4] has presented near-infrared fluorescent (NIRF) as key roles in clinical diagnosis, as well as evaluation of disease status and treatment of tumour. However, it is very important for the image processing to have a Clair strong NIRF signal, so that the image taken, can content a lot of information very near to the real state of the breast. As we know, as early is the detection of the tumor, as better and successful is the treatment. In addition, authors [5] talked about the difficulty to obtain tumor parameters such as: metabolic heat, tumor depth and diameter from a thermogram, Furthermore, another paper [6] mentioned the limitations of computed tomography (CT) and magnetic resonance imaging (MRI), which have a low sensitivity for sub-centimetre lesions due to their limited spatial resolution. In addition, [7] mentioned another bad point of a successive mammography test for a period of 10 years, according to his study paper, the rate of false positive diagnosis for women after doing a mammogram every year for 10 years is 49.1%. Other aspect has been explored in [8], where he advised to do (Sentinel Lymph Node) SLN biopsy, in order to reduce the a higher risk of disease (breast cancer) progression, in addition authors [9] has advised, to not take breast cancer’s thermography result like sufficient information for decision taking.
2.1 Related Works
2.1.1 A Doubt for Infrared Base Techniques
Article [9] illustrates the limitation of the thermography image as important tool in decision taking technique due to its high number of false positive observe by conducting, for example a test on 126 breasts of 63 patients (58 females and five males). An assumption has been taken so that the mean age of the patients was 47.6 years (range 26–82 years). After processing the thermal image, cancerous lesions were finally diagnosed in 20 breasts and there were no bilateral cancers. The outcome of the study was that the thermal diagnosis as non-sufficient for the primary evaluation of symptomatic patients.
2.1.2 Infrared Thermal Imaging
Paper [3] deal with pre-digital mammography (FFDM) and digital infrared thermal imaging (DITI) as imaging modalities that would overcome mammography limitations. Due to its ability to selectively optimize contrast in areas of dense parenchyma, Digital mammography is superior to screen-film mammography in younger women with dense breasts, however we observe due to the density of their breast tissue, a lower sensitivity of mammography. In Other hand, the utilization of Digital Infrared Imaging is based on the principle that, metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing cancer, is almost always higher than in normal tissue, also it is reported that the results of thermography can be correct 8–10 years before mammography can detect a mass in the patient’s body. In addition of that, a shortage of qualified radiologists, also causes an urgent demand for the development of computer technologies as computerized thermal imaging (CTI).
Furthermore, paper [6] discussed about thermal diagnosis, which is still improving every year, furthermore, several thermal diagnosis show that breast cancer patients with abnormal thermograms have fast growing tumours. For achieved a better test results, a protocol must be follow before a patient undergoes an examination, for the testing procedure and environment during the examination and for the post processing of the obtained thermograms. In addition, thermal diagnosis can be further optimize by the help of Artificial Neural Network (ANNs) where many images both with cancer and without breast cancer must be provided, to feed the input layer and then processed in the hidden layers. The output from the last hidden layer serves as input to the neurons in the output layer and a decision is taken. A better improvement can be to combine ANNs, genetic algorithms, and computer simulations, so that they relate the skin surface temperature with the tumor depth, diameter, and heat generation, all of these, by considering the computational domain as layered semi-spherical breast (Fig. 1a). Furthermore, it is good to notice that ANN showed good agreement with the numerical simulation and surface temperatures (Fig. 1c). For better understanding of the breast cancer several geometric models have been propose so far, among them, we have: Rectangular domain (Fig. 2) which provided a first insight on predictive models that relate the surface temperature with the tumor size and location, however it does not represent the real shape of the breast; hemispherical computational domains (Fig. 3) gave results in better agreement with experimental data. Also, the temperature distribution illustrated the effect of the different layers in the surface temperature.
Thermal diffusion in a conventional breast representation [10]
Rectangular domain which provided a first insight on predictive models that relate the surface temperature with the tumor size and location [11]
Hemispherical domain with non-concentric layers, which is a very popular model due to its ability of reproducing surface temperatures [12]
In our context of breast tumor detection, the surface temperature of the breast is the solution the bio-heat transfer equation, so we just need to determine the value of the parameters of this equation. An application of the inverse modelling method requires however a model for the breast. Furthermore, in our context the bio-heat transfer equation is solved for a set of initial values of the thermos physical properties of the breast tissues.
We need also optimization techniques such as the Gradient Descent Method, the Levenberg-Marquardt algorithm, or Genetic Algorithms so to estimate the value of the Thermal physical properties. However, as temperature can only be measured at the surface of the breast and the temperature profile inside the breast remains unknown, the inverse modelling problem remain an ill posed with no unique solution. In the other side, paper [13] elaborate on the IR radiation of human body which is most often in the range of 2–20 μm wavelength, it can be detected very precisely with our nowadays infrared camera [14, 15]. Two factor must be keep for achieved a success rate of computer diagnosis: higher quality of the sensing element (infrared camera) and Improvement of the image processing algorithms throughout the whole process. In the same way, Independent component analysis (ICA) is a subspace projection technique that projects data from a high-dimensional space to a lower-dimensional space. The ICA’s tumor analysis method is composed of 3 concatenated phases: separation of the original image in two chrominance (Cb, Cr) and luminance components (Y), obtaining the independent components (ICA) of the image and post-processing for segmentation of the tumorous areas. This analysis brings out features that are inappreciable in the original image which are associated with areas of high risk tumor, because of their high body temperature link to an extreme tone within the original image. However, ICA is to solve problem which consists in considering the observation data matrix X (digital image) as a linear combination of independent components, i.e. X = A · S where S contains the independent components and the mixing matrix, and its coefficients describe uniquely the mixed source regions and can be used as extracted features. In short, ICA attempts to ‘un-mix’ the data by estimating a Demixing matrix W where Y = W · X, so the goal of ICA is to recover A and Y using the information contained in X. One possible algorithm for obtaining the matrix W = A power (−1) (the demixing matrix). The different outputs of ICA will be given as input of automated post processed, which by the help of several internal computation will proceed each input and compare the result so that the output is with a best accuracy as possible.
2.1.3 Near-Infrared Fluorescent (NIRF) and Agent
Article [2] introduced the concept of agent which represents in this context, a composition of molecule which when uptake, can envelop the tumor and produce a stronger near-infrared fluorescent (NIRF) signal suitable for a good localization in the brain. The IR780-phospholipid micelle (Fig. 1) is suitable for this purpose, as it has the ability to pass through the natural barrier of brain, localize and attach itself to tumour cells (Fig. 2).
2.1.4 The Diameter and Depth of the Tumor
Paper [3] shows the diameter and depth of the tumor as a problem to be solve using thermal techniques, the full width at half maximum (FWHM), to estimate the depth of a small heat source from the isothermal distribution of hot spots at the surface. Furthermore, due to the complex structure of the breast heat transfer, the application of a vascular model requires a detailed knowledge of the microvasculature network.
In order to determine the relationship between depth and heat transfer during cooling, it is helpful to define the thermal penetration depth which is not yet precise due to the complex structure of the breast. However an assumption can be made by considering hemispherical domaine. Furthermore, it appears that after cooling of the breast, the response time (the considerable among of heat detect at the surface the breast) increases with tumor depth. In addition, we have observe that the tumor diameter have no significant effect on the response time for shallow tumors. We have also observe that the smaller the tumor is, the longer is the response time. During our experience, we have observe certain principle in order to measure a correct values or make our thermal sensor more accurate. One of the important procedure was to keep the room’s temperature stable within the range of 18–22 °C.
2.2 Economical Aspects of Breast Cancer
Breast cancer is the most common cancer in women, making up 23% of all newly diagnosed oncology cases. 85% of families in which one of the parents will suffer from cancer without the help of family, friends, nonprofit organizations or even debt. Caring for patients with breast cancer has a major impact on the budget, so it is a priority of public health to support effective preventive programs that could be cost-saving in the long run by reducing the incidence of cancer or offering therapeutic interventions that would increase patients’ survival chances, thus reducing the indirect costs of morbidity and mortality [16]. The reality of the cost burden is evidenced by many studies, for example authors [10] show that loss of productivity associated with breast cancer in Poland were €583.7 million in 2010 and €699.7 million in 2014. During this period, costs accrued for 0.162–0.171% of GDP. Public finance expenditure for social insurance benefits to BC sufferers ranged from €50.2 million (2010) to €56.6 million (2014), an equivalent of 0.72–0.79% of expenditures for all diseases. Lost opportunities costs in public finance revenues accounted for €173.9 million in 2010 and €211.0 million in 2014 [10].
Authors at [12] estimated that $245 million USD in cohort of Mexican women in medical costs and income losses owing to breast cancer could be saved over a cohort’s lifetime. Medical costs account for 80% of the economic burden; income losses and opportunity costs for caregivers account for 15 and 5%, respectively [12].
Paper [17] evaluated cost utility of Breast Cancer Index (BCI) from a US third-party payer perspective. Use of BCI was projected to be cost saving. In the newly diagnosed population, net cost savings were $3803 per patient tested. In the 5 years post diagnosis population, BCI was projected to yield a net cost savings of $1803 per patient tested.
Authors at [18] estimated the socioeconomic cost and burden for breast cancer patients in Korea between 2007 and 2010. The prevalence of treated breast cancer increased from 7.9 to 20.4%. The total socioeconomic costs incurred by breast cancer increased by approximately 40.7% from US $668.49 million in 2007 to US $940.75 million in 2010. Medical care costs for 2010 were 1.4 times greater (US $399.22 million) than for 2007 (US $278.71 million. The direct non-medical costs rose from US $50.69 million in 2007 to US $75.83 million in 2010, a 49.6% increase. Regarding the economic burden of breast cancer, the total indirect costs were US $339.09 million in 2007 and increased by 37.3% to US $465.70 million in 2010.
However, cost growth may not always be linked to rising prevalence but also to the development of new healing methods. For example, standard chemotherapy in the Czech Republic for breast cancer costs around 200 EUR. Biological treatment, which is suitable for one fifth of patients, costs roughly 30,000 EUR. Hormonal standard treatment comes to 200 EUR, while other hormonal preparations are worth 9,000 EUR. The cost of radiotherapy [14, 15, 19] is between 1,700 and 2,600 EUR. At present, emerging gene or epigenetic therapy that directly influences genetic information responsible for tumor growth will be even more expensive [11]. Oncology cost growth is expected in the 7.5–10.5% range annually through 2020, when global oncology costs will exceed $150 billion (Fig. 4).
Global oncology costs and growth, 2010–2020 [20]
Based on all mentioned facts, the reason to find any new detection method or even small improvement of current ones is more than evident.
3 Discussion of Findings
3.1 Differences Between no Touch BreastScan and Sentinel BreastScan Techniques
The study of the breast cancer base on modern techniques gives us a better view of the issue relate to the accurate detection of the tumor. Base on the previous paper discussed in “related works section”, we have considered some features that we judge relevant enough to show us, a general difference between the sentinel BreastScan and the no Touch BreastScan (Table 1). It appears that, most of techniques nowadays use Neural network to reduce the number of false positive.
We have also observe an important improvement in breast cancer detection for the women with age < 50, with a sensibility ≥ 78% using No Touch software.
3.2 Proposed Model
Through the reviews of the different papers discussed in this Literature review, we have noticed the importance of the image processing which is well done by a human been but still not well achieve by Artificial intelligent. We attend in this discussion to emphasize on the need of Computer Aid Device (CAD) which will help us to better understand the thermal images, capture by our different thermal camera. CAD will be a new neural network SVM model (Fig. 5) (assuming already trained) which will take Thermal images as input and as output will classifier images as cancer or not.
It is good to mention that each neuron will apply Super vector Machine classification so that for any incoming image having a close similarity with an image of a breast cancer, the model will be powerful enough to differentiate both images.
Our propose architecture (Fig. 5) can be assimilate to a flow chart where each module represent a specific component. We can explant each as follow:
-
Pre-processing of breast Thermal images: here, each images are converted to a matrix of features which will be submit as input to the next module.
-
Region of Interest: the areas with more gradient colour will be localize as they are more susceptible to have a Cancer. They will be transfer as input to the next component.
-
Features Extract and Formalize: the localize area will be extract and convert to the appropriate format suitable for the input of the Neural Network SVM model.
-
Neural Network SVM model: Through several computations base on SVM at each layer of the neural network, the system will classify the input and will output the given status of the thermal image (Normal or Cancerous).
4 Conclusion
During presented literature review, it was question to present some works done on breast cancer in the point of view of a computer scientist [21]. In that thought, we have presented the different most common techniques used to detect the breast Cancer, their strengths and dear weaknesses. We came out however, with one among them which present a good future, due to its non-immersive property and its big number of data which needs to be process with more efficient techniques. Infrared imaging couple with an agent prior administrate to a patient can lead to a very precise detector of tumor. We will use in our future study a camera with 0.5 thermal sensitivity and we will propose a model of breast which can help us to achieve a more precise diagnostic.
References
Breast Cancer Facts, National Breast Cancer Foundation (2016)
Dongola, N.: Mammography in Breast Cancer. Medscape Logo (2016)
Köşüş, N., Köşüş, A., Duran, M., Simavlı, S., Turhan, N.: Comparison of standard mammography with digital mammography and digital infrared thermal imaging for breast cancer screening. J. Turk. Ger. Gynecol. Assoc. (2010)
Li, S., Johnson, J., Peck, A., Xie, Q.: Near infrared fluorescent imaging of brain tumor with IR780 dye incorporated phospholipid nanoparticles. J. Trans. Med. (2017)
Amria, A., Pulko, S.H., Wilk, A.J.: Potentialities of steady-state and transient thermography in breast tumour depth detection: a numerical study. Comput. Methods Programs Biomed. (2016)
Boogerd, L.S.F., Handgraaf, H.J.M., Lam, H.-D., Huurman, V.A.L., Farina-Sarasqueta, A., Frangioni, J.V., van de Velde, C.J.H., Braat, A.E., Vahrmeijer, A.L.: Laparoscopic detection and resection of occult liver tumors of multiple cancer types using real-time near-infrared fluorescence guidance. Surg. Endosc. (2017)
Kandlikar, S.G., Perez-Raya, I., Raghupathi, P.A., Gonzalez-Hernandez, J.L., Dabydeen, D., Medeiros, L., Phatak, P.: Infrared imaging technology for breast cancer detection—Current status, protocols and new directions. Int. J. Heat Mass Trans. (2017)
Tsutomu Namikawa, T.S.: Recent advances in near-infrared fluorescence-guided imaging surgery using indocyanine green. Surg. Today (2015)
Kontos, M., Wilson, R., Fentiman, I.: Digital infrared thermal imaging (DITI) of breast lesions: sensitivity and specificity of detection of primary breast cancers. Clin. Radiol. (2011)
Łyszczarz, B., Nojszewska, E.: Productivity losses and public finance burden attributable to breast cancer in Poland, 2010–2014. BMC Cancer 17(1), 676 (2017)
National Oncology Program. Czech Oncological Society (2011)
Unar-Munguía, M., Meza, R., Colchero, M.A., et al.: Economic and disease burden of breast cancer associated with suboptimal breastfeeding practices in Mexico. Cancer Causes Control (2017)
Boquete, L., Ortega, S., Miguel-Jiménez, J.M., Rodríguez-Ascariz, J.M.: Automated detection of breast cancer in thermal infrared images, based on independent component analysis. J. Med. Syst. (2012)
Kubicek, J., Bryjova, I., Faltynova, K., Penhaker, M., Augustynek, M., Maresova, P.: Evaluation of gama analysis results significance within verification of radiation IMRT plans in radiotherapy. Lecture Notes in Computer Science, vol. 10449, pp. 541–548 (2017). https://doi.org/10.1007/978-3-319-67077-5_52
Augustynek, M., Korpas, D., Penhaker, M., Cvek, J., Binarova, A.: Monitoring of CRT-D devices during radiation therapy in vitro. BioMedical Engineering Online, 15 (1), article no. 29 (2016). https://doi.org/10.1186/s12938-016-0144-7
Smidova, I.: Alcohol and breast cancer—economic costs. Hygiena 51(1), 17–21 (2012)
Gustavsen, G., Schroeder, B., Kennedy, P., et al.: Health economic analysis of breast cancer index in patients with ER+, LN− breast cancer. Am. J. Manag. Care 20(8), 1 (2014)
Kim, Y.A., Oh, I.H., Yoon, S.J., et al.: The economic burden of breast cancer in Korea from 2007–2010. Cancer Res. Treat. 47(4), 583–590 (2015)
Bryjova, I., Kubicek, J., Molnarova, K., Peter, L., Penhaker, M., Kuca, K.: Multiregional segmentation modeling in medical ultrasonography: extraction, modeling and quantification of skin layers and hypertrophic scars. Lecture Notes in Computer Science, vol. 10449, LNAI, pp. 182–192 (2017). https://doi.org/10.1007/978-3-319-67077-5_18
IMS Health, MIDAS, Dec 2015; Market Prognosis, Mar 2016. IMS Institute for Healthcare Informatics, May 2016
Cardoso, F., Harbeck, N., Bergh, J., Cortés, J.: Research needs in breast cancer. Ann. Oncol. (2016)
Acknowledgements
This work was supported by internal students project at FIM, University of Hradec Kralove, Czech Republic (under ID: UHK-FIM-SP-2018).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Mambou, S., Maresova, P., Krejcar, O., Selamat, A., Kuca, K. (2018). Breast Cancer Detection Using Modern Visual IT Techniques. In: Sieminski, A., Kozierkiewicz, A., Nunez, M., Ha, Q. (eds) Modern Approaches for Intelligent Information and Database Systems. Studies in Computational Intelligence, vol 769. Springer, Cham. https://doi.org/10.1007/978-3-319-76081-0_34
Download citation
DOI: https://doi.org/10.1007/978-3-319-76081-0_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-76080-3
Online ISBN: 978-3-319-76081-0
eBook Packages: EngineeringEngineering (R0)