Abstract
c-Jun N-terminal kinase (JNK), a member of stress-induced mitogen-activated protein (MAP) kinase family, has been shown to modulate a variety of biological processes associated with neurodegenerative pathology of the retina. In particular, various retinal cell culture and animal models related to glaucoma, age-related macular degeneration (AMD), and retinitis pigmentosa indicate that JNK signaling may contribute to disease pathogenesis. This mini-review discusses the impact of JNK signaling in retinal disease, with a focus on retinal ganglion cells (RGCs), photoreceptor cells, retinal pigment epithelial (RPE) cells, and animal studies, with particular attention to modulation of JNK signaling as a potential therapeutic target for the treatment of retinal disease.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
- c-Jun N-terminal Kinase (JNK)
- Retinal degeneration
- Retinal ganglion cell (RGC)
- Optic neuropathy
- Retinal pigmented epithelial (RPE) cell
- Age-related macular degeneration (AMD)
- Photoreceptor cells
- Retinitis pigmentosa
- Therapeutic target
1 Introduction
The activation of mitogen-activated protein (MAP) kinase family, including extracellular signal-regulated kinase (ERK) , p38, and c-Jun N-terminal kinase (JNK), is often observed, playing a critical role in fate-determining process of neuronal cells (Kyosseva 2004). Together with p38, JNK is known as a stress-induced MAP kinase, which is involved in neuronal development as well as degenerative diseases such as Alzheimer’s disease and Parkinson’s disease (Ries et al. 2008; Sclip et al. 2014). The intracellular signaling cascade of JNK is initiated by many stressors followed by subsequent activation of downstream signaling molecules (Barr and Bogoyevitch 2001; Weston and Davis 2002). These molecular events result in various gene transcription and following diverse biological outcomes, which promote the next step of disease progression (Mizuno et al. 2005; Morishima et al. 2001; Podkowa et al. 2010). The retina is comprised of several types of neurons, glial, and other supporting cells. The retina receives visual information, converts it into a neurochemical signal by phototransduction , initiates signal processing, and transmits the signal information to the brain via the optic nerve (Heavner and Pevny 2012). Dysfunction and/or death of many of the cells involved in this complex process, whether due to abnormalities in development or due to later disease processes, can result in vision loss and even blindness. To both better understand and develop improved methods to prevent and treat visual loss, numerous studies have been directed at understanding the molecular mechanisms of injury in the visual system. In this review, we will summarize current knowledge on the role of the c-JNK signaling pathway on retinal degeneration .
2 JNK Signaling and Axonal Degeneration of RGC Related to Glaucoma and Other Diseases
Retinal ganglion cells (RGCs) transmit visual information from bipolar cells to vision relay centers in the brain, such as the lateral geniculate nucleus (LGN) and superior colliculus (SC) , and ultimately to the visual cortex (Yu et al. 2013). Injury and death of RGCs, which together constitute the so-called optic neuropathies , are a major cause of vision loss and blindness worldwide (Quigley 1999). The impact of JNK and its upstream/downstream pathways in RGC death has been actively investigated using various in vivo models of optic nerve disease, such as neuronal excitotoxicity by NMDA (Bessero et al. 2010), experimental optic nerve crush (ONC) (Fernandes et al. 2012; Welsbie et al. 2013), and retinal ischemic injury (Kim et al. 2016; Roth et al. 2003). In particular, Fernandez and colleagues demonstrated that combined deletion of JNK2 and JNK3 inhibited RGC death with long-term protection after ONC injury, and a similar effect was shown by conditional deletion of JUN, a downstream signaling molecule of JNK (Fernandes et al. 2012). In addition, blocking upstream signaling of JNK led to significantly decreased JNK activation that was associated with enhanced RGC survival following ONC (Welsbie et al. 2013). Similar results have been reported with cell death caused by ischemic injury (Biousse and Newman 2014), a disorder of the inner retinal blood supply which results in a temporary or persistent ischemic environment for RGCs, resulting in cell death.(Havens and Gulati 2016; Sugawara et al. 2004). As with the other conditions described above, ischemic injury also upregulates JNK activation in inner retinal layer cells , including RGCs (Roth et al. 2003), and results in RGC death accompanied with progressive inner retinal remodeling (Kim et al. 2013). Importantly, several studies suggest that pharmacological inhibition of JNK activation can significantly increase RGC viability and prevented inner retinal degeneration (Kim et al. 2016). In particular, Kim et al. demonstrated that ischemia/reperfusion (I/R) triggered JNK activation in various cells in the inner retinal layers and RGC axonal loss were significantly inhibited by administration of SP600125. This finding suggested that activation of JNK plays a pivotal role in RGC death (Kim et al. 2016). In this study, Kim and colleagues also showed that ischemic injury initiated early JNK activation in RGC as well as non-RGC cells in the NFL/RGC layer at later post-injury time, which suggests that RGCs may be the most susceptible cell type for ischemic injury. In addition, this finding also suggested that ischemic injury possibly triggers JNK activation in non-RGCs in the NFL/RGC layer such as displaced amacrine cells and astrocytes. One interesting observation related to this finding is that the role of JNK may be different in different retinal cell types treated with the same pathological impact. For example, Dvoriantchikova and Ivanov showed that RGCs treated with the proinflammatory cytokine tumor necrosis factor (TNF) did not demonstrate NF-kB activation but showed sustained JNK activation (Dvoriantchikova and Ivanov 2014). In contrast, TNF-treated astrocytes showed induced NF-kB activation with transient JNK activation, which was associated with prolonged astrocyte survival. Taken together, these findings indicate that JNK inhibitors may be an interesting class of pharmacological molecules for promoting RGC survival through inhibiting JNK activation to prevent RGC death and simultaneously inhibiting proinflammatory responses in glial cells.
3 JNK Signaling and Retinal Pigment Epithelium Cells: Possible Relationship with Age-Related Macular Degeneration
Retinal pigment epithelial (RPE) cells are a retinal cell type underlying and supporting photoreceptor cells through various functions to maintain functional and structural integrity (Boulton and Dayhaw-Barker 2001; Strauss 2005). The biological aspects RPE cells in human diseases have been actively investigated, particularly in age-related macular degeneration (AMD) (Young 1987). AMD is a leading cause of vision loss in the elderly in the United States and other developed Western countries (Gehrs et al. 2006), associated with multiple mechanisms and risk factors of AMD (Gehrs et al. 2006; Tan et al. 2016). AMD can be categorized into two broad types in late stage, a non-neovascular (dry) form and a neovascular (wet) form (Gehrs et al. 2006). The non-neovascular form is more common, but the neovascular form is generally associated with more severe vision loss. Neovascular AMD is characterized by aberrant choroidal neovascularization mediated, at least in part, by the angiogenic growth factor vascular endothelial growth factor (VEGF) . In the retina, VEGF both stimulates neovascularization and increases vascular permeability, resulting in abnormalities in the macular region that are associated with central vision loss (Gehrs et al. 2006). Among other important roles that the RPE plays in AMD pathogenesis, RPE cells constitutively produce VEGF, and they show increased production in response to pathologic conditions (Blaauwgeers et al. 1999; Holtkamp et al. 2001). Importantly, JNK has been suggested as a key signaling molecule promoting VEGF expression through phosphorylation of c-Jun and binding to the VEGF promotor mediating neovascularization (Du et al. 2013; Guma et al. 2009). Dry AMD, characterized by regional loss of RPE cells followed by photoreceptor cell dysfunction and cell loss, is currently untreatable (Ambati and Fowler 2012; Gehrs et al. 2006). To better understand RPE cell death mechanisms, in vitro studies of primary human RPE cells and cell lines have been widely used to define JNK-associated RPE cell death under various pathologic conditions (Cao et al. 2012; Roduit and Schorderet 2008; Westlund et al. 2009). Despite these many studies, the role of JNK in RPE viability remains controversial. Cao and colleagues showed that ultraviolet B radiation induced apoptotic cell death of the ARPE-19 RPE cell line. Surprisingly, inhibition of JNK exacerbated apoptosis, whereas activation of JNK attenuated ARPE-19 cell death, suggesting an anti-apoptotic role of JNK (Cao et al. 2012). In contrast, Roduit et al. reported enhanced RPE cell survival upon JNK inhibition under UV irradiation (Roduit and Schorderet 2008). However, this issue is not resolved and warrants further research.
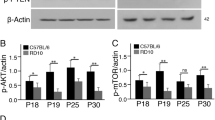
4 JNK Signaling and Photoreceptor Degeneration
Many vision diseases associated with photoreceptor loss have been reported, which are briefly categorized into inherited degeneration, such as retinitis pigmentosa, and adaptive degenerations caused by age and other multiple factors, such as AMD (Wright et al. 2010). Notably, nonsyndromic retinitis pigmentosa is highly polygenic, associated with mutation of more than 50 genes (Bowne et al. 2011; Nishiguchi et al. 2013; https://sph.uth.edu/Retnet/). The association of JNK with photoreceptor cell death is relatively less known compared to other retinal cell types. Nonetheless, several in vitro and animal models have suggested a role of JNK as a mediator of photoreceptor cell death, initiated by various genetic and environmental factors. Using the photoreceptor cell line 661 W, Choudhury showed that reprogramming of the unfolded protein response (UPR) by genetic deletion of caspase 7 resulted in a decrease of JNK-induced apoptosis (Choudhury et al. 2013). This finding suggested that JNK is an important apoptotic mediator of UPR, which is known as a major causative process of photoreceptor cell death in some forms of retinitis pigmentosa (Galy et al. 2005; Kang et al. 2012). These findings indicate that JNK may play an important role in photoreceptor cell death.
5 Conclusions: JNK Signaling Pathway as a Potential Therapeutic Target in Retinal Degenerative Disease?
In summary, as described above, apoptosis of a variety of retinal cells is associated with activation of the JNK pathway. In addition, in a number of different retinal degeneration models, genetic and pharmacological inhibition of JNK signaling results in protection from cell death and reduced pathologic progression . As a common mediator of retinal cell death, pharmacological inhibition of JNK, or associated family members, may provide a pathway for a “generic” treatment strategy that is relatively independent of the specific genetic mutation causing the disease. Additionally, JNK inhibition strategies may provide a complementary treatment approach to gene-specific therapies. For these reasons, it seems reasonable to pursue the JNK pathway as a promising target for the development of novel therapeutic strategies for treatment of the photoreceptor degenerative diseases .
References
Ambati J, Fowler BJ (2012) Mechanisms of age-related macular degeneration. Neuron 75(1):26–39
Barr RK, Bogoyevitch MA (2001) The c-Jun N-terminal protein kinase family of mitogen-activated protein kinases (JNK MAPKs). Int J Biochem Cell Biol 33(11):1047–1063
Bessero AC, Chiodini F, Rungger-Brandle E et al (2010) Role of the c-Jun N-terminal kinase pathway in retinal excitotoxicity, and neuroprotection by its inhibition. J Neurochem 113(5):1307–1318
Biousse V, Newman N (2014) Retinal and optic nerve ischemia. Continuum (Minneap Minn) 20(4 Neuro-ophthalmology):838–856
Blaauwgeers HG, Holtkamp GM, Rutten H et al (1999) Polarized vascular endothelial growth factor secretion by human retinal pigment epithelium and localization of vascular endothelial growth factor receptors on the inner choriocapillaris. Evidence for a trophic paracrine relation. Am J Pathol 155(2):421–428
Boulton M, Dayhaw-Barker P (2001) The role of the retinal pigment epithelium: topographical variation and ageing changes. Eye (Lond) 15(Pt 3):384–389
Bowne SJ, Sullivan LS, Koboldt DC et al (2011) Identification of disease-causing mutations in autosomal dominant retinitis pigmentosa (adRP) using next-generation DNA sequencing. Invest Ophthalmol Vis Sci 52(1):494–503
Cao G, Chen M, Song Q et al (2012) EGCG protects against UVB-induced apoptosis via oxidative stress and the JNK1/c-Jun pathway in ARPE19 cells. Mol Med Rep 5(1):54–59
Choudhury S, Bhootada Y, Gorbatyuk O et al (2013) Caspase-7 ablation modulates UPR, reprograms TRAF2-JNK apoptosis and protects T17M rhodopsin mice from severe retinal degeneration. Cell Death Dis 4:e528
Du H, Sun X, Guma M et al (2013) JNK inhibition reduces apoptosis and neovascularization in a murine model of age-related macular degeneration. Proc Natl Acad Sci U S A 110(6):2377–2382
Dvoriantchikova G, Ivanov D (2014) Tumor necrosis factor-alpha mediates activation of NF-κB and JNK signaling cascades in retinal ganglion cells and astrocytes in opposite ways. Eur J Neurosci 40(8):3171–3178
Fernandes KA, Harder JM, Fornarola LB et al (2012) JNK2 and JNK3 are major regulators of axonal injury-induced retinal ganglion cell death. Neurobiol Dis 46(2):393–401
Galy A, Roux MJ, Sahel JA et al (2005) Rhodopsin maturation defects induce photoreceptor death by apoptosis: a fly model for RhodopsinPro23His human retinitis pigmentosa. Hum Mol Genet 14(17):2547–2557
Gehrs KM, Anderson DH, Johnson LV et al (2006) Age-related macular degeneration--emerging pathogenetic and therapeutic concepts. Ann Med 38(7):450–471
Guma M, Rius J, Duong-Polk KX et al (2009) Genetic and pharmacological inhibition of JNK ameliorates hypoxia-induced retinopathy through interference with VEGF expression. Proc Natl Acad Sci U S A 106(21):8760–8765
Havens SJ, Gulati V (2016) Neovascular Glaucoma. Dev Ophthalmol 55:196–204
Heavner W, Pevny L (2012) Eye development and retinogenesis. Cold Spring Harb Perspect Biol 4(12):a008391
Holtkamp GM, Kijlstra A, Peek R et al (2001) Retinal pigment epithelium-immune system interactions: cytokine production and cytokine-induced changes. Prog Retin Eye Res 20:29–48
Kang MJ, Chung J, Ryoo HD (2012) CDK5 and MEKK1 mediate pro-apoptotic signalling following endoplasmic reticulum stress in an autosomal dominant retinitis pigmentosa model. Nat Cell Biol 14(4):409–415
Kim BJ, Braun TA, Wordinger RJ et al (2013) Progressive morphological changes and impaired retinal function associated with temporal regulation of gene expression after retinal ischemia/reperfusion injury in mice. Mol Neurodegener 8:21
Kim BJ, Silverman SM, Liu Y et al (2016) In vitro and in vivo neuroprotective effects of cJun N-terminal kinase inhibitors on retinal ganglion cells. Mol Neurodegener 11:30
Kyosseva SV (2004) Mitogen-activated protein kinase signaling. Int Rev Neurobiol 59:201–220
Mizuno N, Kokubu H, Sato M et al (2005) G protein-coupled receptor signaling through Gq and JNK negatively regulates neural progenitor cell migration. Proc Natl Acad Sci U S A 102(35):12365–12370
Morishima Y, Gotoh Y, Zieg J et al (2001) Beta-amyloid induces neuronal apoptosis via a mechanism that involves the c-Jun N-terminal kinase pathway and the induction of Fas ligand. J Neurosci 21(19):7551–7560
Nishiguchi KM, Tearle RG, Liu YP et al (2013) Whole genome sequencing in patients with retinitis pigmentosa reveals pathogenic DNA structural changes and NEK2 as a new disease gene. Proc Natl Acad Sci U S A 110(40):16139–16144
Podkowa M, Zhao X, Chow CW et al (2010) Microtubule stabilization by bone morphogenetic protein receptor-mediated scaffolding of c-Jun N-terminal kinase promotes dendrite formation. Mol Cell Biol 30(9):2241–2250
Quigley HA (1999) Neuronal death in glaucoma. Prog Retin Eye Res 18(1):39–57
Ries V, Silva RM, Oo TF et al (2008) JNK2 and JNK3 combined are essential for apoptosis in dopamine neurons of the substantia nigra, but are not required for axon degeneration. J Neurochem 107(6):1578–1588
Roduit R, Schorderet DF (2008) MAP kinase pathways in UV-induced apoptosis of retinal pigment epithelium ARPE19 cells. Apoptosis 13(3):343–353
Roth S, Shaikh AR, Hennelly MM et al (2003) Mitogen activated protein kinases and retinal ischemia. Invest Ophthalmol Vis Sci 44(12):5383–5395
Sclip A, Tozzi A, Abaza A et al (2014) c-Jun N-terminal kinase has a key role in Alzheimer disease synaptic dysfunction in vivo. Cell Death Dis 5:e1019
Strauss O (2005) The retinal pigment epithelium in visual function. Physiol Rev 85(3):845–881
Sugawara T, Fujimura M, Noshita N et al (2004) Neuronal death/survival signaling pathways in cerebral ischemia. NeuroRx 1(1):17–25
Tan PL, Bowes Rickman C, Katsanis N (2016) AMD and the alternative complement pathway: genetics and functional implications. Hum Genomics 10(1):23
Welsbie DS, Yang Z, Ge Y et al (2013) Functional genomic screening identifies dual leucine zipper kinase as a key mediator of retinal ganglion cell death. Proc Natl Acad Sci U S A 110(10):4045–4050
Westlund BS, Cai B, Zhou J et al (2009) Involvement of c-Abl, p53 and the MAP kinase JNK in the cell death program initiated in A2E-laden ARPE-19 cells by exposure to blue light. Apoptosis 14(1):31–41
Weston CR, Davis RJ (2002) The JNK signal transduction pathway. Curr Opin Genet 12(1):14–21
Wright AF, Chakarova CF, Abd El-Aziz MM et al (2010) Photoreceptor degeneration: genetic and mechanistic dissection of a complex trait. Nat Rev Genet 11(4):273–284
Young RW (1987) Pathophysiology of age-related macular degeneration. Surv Ophthalmol 31(5):291–306
Yu DY, Cringle SJ, Balaratnasingam C et al (2013) Retinal ganglion cells: energetics, compartmentation, axonal transport, cytoskeletons and vulnerability. Prog Retin Eye Res 36:217–246
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this paper
Cite this paper
Kim, BJ., Zack, D.J. (2018). The Role of c-Jun N-Terminal Kinase (JNK) in Retinal Degeneration and Vision Loss. In: Ash, J., Anderson, R., LaVail, M., Bowes Rickman, C., Hollyfield, J., Grimm, C. (eds) Retinal Degenerative Diseases. Advances in Experimental Medicine and Biology, vol 1074. Springer, Cham. https://doi.org/10.1007/978-3-319-75402-4_43
Download citation
DOI: https://doi.org/10.1007/978-3-319-75402-4_43
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-75401-7
Online ISBN: 978-3-319-75402-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)