Abstract
For over three decades, stents have been used in congenital heart disease with increasing experience and application in more diverse lesions at all ages. Stent implantation enables overcoming of several limitations of isolated balloon dilation leading to a superior relief of stenosis both acutely and in the long term. Especially elastic lesions, long-segment stenoses, hypoplastic vessels, stenoses related to kinking or tension on a vessel respond better to stent implantation. However, several issues unique to the paediatric population like small vessel access, difficulty in advancing the rigid stent through a tortuous vascular route or somatic growth requiring stent redilation warrant careful selection of stent and implementation of modified interventional techniques.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
For over three decades, stents have been used in congenital heart disease with increasing experience and application in more diverse lesions at all ages. Stent implantation enables overcoming of several limitations of isolated balloon dilation leading to a superior relief of stenosis both acutely and in the long term. Especially elastic lesions, long-segment stenoses, hypoplastic vessels, stenoses related to kinking or tension on a vessel respond better to stent implantation. However, several issues unique to the paediatric population like small vessel access, difficulty in advancing the rigid stent through a tortuous vascular route or somatic growth requiring stent redilation warrant careful selection of stent and implementation of modified interventional techniques.
Given the diversity of lesions and patient size range, a single type of stent does not suit all situations. Technological advances have led to availability of a wide range of stents to match particular lesions. Modern stents (Figs. 4.1, 4.2 and 4.3) can be classified in several groups according to:
-
Stent size:
-
Small size (up to 5–6 mm)
-
Medium size (6–12 mm)
-
Large size (12–20 mm)
-
Extra large (more than 20 mm)
-
-
Cell design:
-
Closed-cell design
-
Open-cell design
-
Hybrid design
-
-
Mounting:
-
Unmounted
-
Premounted
-
-
Mode of implantation:
-
Self-expanding stents
-
Balloon-expandable stents
-
-
Covering:
-
Uncovered stents
-
Covered stents
-
-
Other types:
-
Growth and biodegradable stents
-
Stent grafts
-
Examples of selected small size stents. (a) Balloon-expandable stainless steel coronary stent implanted in a systemic-to-pulmonary artery shunt. (b) Hybrid deployment of a self-expanding, nitinol sinus-SuperFlex-DS to the ductus arteriosus. (c) Percutaneous three-dimensional guided implantation of a self-expanding, nitinol Zilver Flex to the ductus arteriosus. (d) The latter stent after deployment. Radiopaque markers at both ends of the sent align with marking rings indicating pulmonary and aortic insertions of the duct
Examples of selected medium size stents. (a) Stainless steel, closed cell Palmaz Genesis stent implanted in the right ventricular outflow tract. (b) Stainless steel, open-cell Valeo Lifestent, placed in fenestration in a patient after Fontan completion. (c) Stainless steel, open-cell Visi-Pro is being positioned in the right pulmonary artery. (d) Stainless steel, open-cell Formula stent after hybrid implantation to restrictive interatrial communication
Examples of selected medium to large size stents. (a) Balloon-expandable platinum-iridium closed-cell design Cheatham-Platinum stent is being deployed on two balloons to the extracardiac tunnel in a patient after Fontan completion. (b) Angiography after reconnection of the superior caval vein to the right atrium with implantation of two covered Cheatham-Platinum stents. (c) A stainless steel, open-cell design, covered Advanta V12 stent was implanted to the extracardiac tunnel in a patient after fenestrated Fontan operation. (d) A chromium cobalt, hybrid cell design AndraStent was implanted to aortic coarctation
The basic principles of stent implantation are common to most lesions (Fig. 4.4). These include:
-
Obtaining access
-
Haemodynamic assessment and angiography
-
Predilation (optional)
-
Stent choice
-
Guide wire and sheath placement
-
Mounting (for unmounted stents)
-
Stent introduction
-
Stent positioning
-
Stent deployment
-
Final haemodynamic assessment and angiography
Step-by-step stent implantation. (a) A patient with hypoplastic left heart syndrome after hemi-Fontan operation. Angiography from SVC shows hypoplastic left pulmonary artery with poor contrast flow to the upper lobe. (b) The pulmonary artery was predilated for evaluation of compliance and potential compression on the left main bronchus. Simultaneous bronchoscopy was performed to assess consequence of balloon inflation on the bronchus. (c) An open-cell Valeo Lifestent was delivered through a long sheath introduced distally to the lesion. (d) Check angiography during positioning of the stent shows the implant placed between the origin of the left upper lobe branch artery and proximally the hemi-Fontan anastomosis. (e) The dedicated balloon was fully inflated with nominal pressure. (f) Angiography shows improved diameter of the left pulmonary artery with proximal end of the stent “hanging” in the hemi-Fontan connection. The distal end of the stent is placed just proximal to the first branching of the left pulmonary artery. (g) The proximal end of the stent was flared with a compliant oversized balloon. (h) Final angiography shows satisfactory result
The larger sheaths and stiffer guide wires used may increase the frequency and severity of complications associated with cardiac catheterisation though they are in general low. Complications after stent implantation include:
-
Stent malposition or migration (Fig. 4.5)
-
Side-branch compromise
-
Vessel dissection and rupture (Fig. 4.5)
-
Balloon rupture
-
Stent fracture (Fig. 4.6)
-
Restenosis (Fig. 4.7)
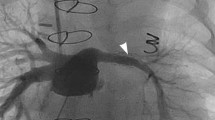
Step-by-step stent implantation. Complications— stent malposition and vessel dissection. (a) Initial angiography shows severely hypoplastic left pulmonary artery with discrete stenosis just proximal to the first branch. (b) A balloon-expandable Valeo Lifestent stent was introduced through a long vascular sheath placed in the main pulmonary artery. The nasogastric tube was used as a marking point for the distal end of the stent. (c) During balloon inflation, the stent milked back towards the main pulmonary artery. (d) Final angiography shows significant improvement of the left pulmonary artery diameter with dissection of the bottom wall and contrast extravasation
Complications—stent fracture. (a) A patient with hypoplastic left heart syndrome early after Fontan operation. Angiography shows fractured and fragmented previously implanted Palmaz Genesis stent in the left pulmonary artery. Additional tubular stenosis of the proximal right pulmonary artery may be seen. (b) A covered Advanta V12 stent was introduced through a long sheath placed in the extracardiac tunnel. Contrast injection was performed to position the stent so as to cover the proximal right pulmonary artery. (c) Both stents were postdilated with a high-pressure balloon to achieve larger final diameter. On full balloon inflation, a residual narrowing at the site of the first stent fracture may be seen. (d) Final angiography shows stabilised segments of the Palmaz Genesis stent, improved diameter of the proximal right pulmonary artery and residual stenosis at the level of the previous stent fracture
Complications—restenosis. (a) Patient with interrupted aortic arch after first-stage hybrid palliation. Angiography shows a self-expanding sinus-SuperFlex-DS stent in the arterial duct with significant stenosis due to neointimal hyperplasia. (b) Balloon-expandable Palmaz Blue stent was chosen to treat the stenosis. The stent was delivered through a long sheath from femoral vein access. (c) Still frame shows the stainless steel Palmaz Blue stent implanted inside the nitinol sinus-SuperFlex-DS stent. (d) Final angiography shows unobstructed flow through the stents placed in the arterial duct
The vast majority of acute stent-related complications can be prevented by meticulous step-by-step approach with attention to details. When they occur, however, it is vital to maintain guide-wire position for remedial action with the stent and vessel still accessible.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Goreczny, S., Rosenthal, E. (2019). Stents. In: Butera, G., Chessa, M., Eicken, A., Thomson, J.D. (eds) Atlas of Cardiac Catheterization for Congenital Heart Disease. Springer, Cham. https://doi.org/10.1007/978-3-319-72443-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-72443-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-72442-3
Online ISBN: 978-3-319-72443-0
eBook Packages: MedicineMedicine (R0)