Abstract
In the vast majority of fragility fractures of the pelvis, fractures of the posterior and anterior pelvic ring occur combined. Fractures of the pubic rami above and below the obturator foramen are much more frequent than fractures of the pubic bone and fractures at the anterior lip of the acetabulum. Retrograde transpubic screw fixation is a minimally invasive technique for stabilization of pubic rami fractures. The anterior column corridor is a straight corridor between the anterior cortex of the superior pubic ramus near to the pubic tubercle and the external cortex of the ilium above the acetabulum. The minimal canal diameter, measured in 160 Japanese, was on average 13.5 mm for men and 10.7 mm for women. The mean length of the corridor was 124.6 mm in men and 123.8 mm in women. The spatial orientation of the cylinder, measured on 82 Chinese, was 39.7°, 20.8° and 42.7° to the transverse, coronal and sagittal planes, respectively. In Europeans, the average length of the corridor was 127.2 mm, the narrowest diameter 14.6 mm. Consequentially, the insertion of a 7.3 mm screw should be possible in all patients. Biomechanical studies are controversial. One study demonstrated that fixation of the anterior pelvic ring with a retrograde transpubic 4.5 mm screw obtains the same stability as with conventional 3.5 mm plating. Another study found a lower stability for retrograde screw fixation than for plate fixation of pubic ramus fractures. Preoperative planning, intraoperative imaging and the different steps of the procedure are explained in detail. There are only a few literature data on complications and outcome. In a retrospective study on 68 retrograde transpubic screw fixations; there were no neurologic, vascular or urologic complications. There were 16% fixation failures, related to lateral compression type injuries and higher patient age. To prevent implant loosening, we recommend using the maximum length of the anterior column corridor with the tip of the screw perforating the lateral cortex of the ilium above the acetabulum.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Pubic ramus fracture
- Minimally-invasive fixation
- Anterior column corridor
- Retrograde transpubic screw
- Operation technique
1 Introduction
The main goals in treating fragility fractures of the pelvis (FFP) are reduction of pain and restoration of stability of the pelvic ring, allowing early mobilization to prevent immobilization-associated complications. The pelvic ring is a circular structure; fractures of the anterior pelvic ring are very often combined with fractures of the posterior pelvis. Scheyerer et al. conducted a retrospective study to evaluate the posterior pelvic ring in patients with pubic ramus fractures [1]. One hundred and seventy-seven patients with complete diagnostics, including a CT scan, were reviewed. In patients with no obvious other injury than the pubic ramus fractures in the a.p. radiograph, an injury of the posterior pelvic ring was found in 96.8% in CT. The study included high-energy as well as low-energy pelvic ring injuries [1]. Alnaib et al. conducted a prospective study on 67 patients with fragility fractures of the pelvis [2]. Fifty-four female and thirteen male patients with an average age of 87.5 years were included. Isolated sacral fractures were only present in 9%. Fifty-four percent of the patients with a single pubic ramus fracture had an associated sacral fracture. Sixty-one percent of the patients with two pubic ramus fractures had an associated sacral fracture [2]. In the study of Lau et al. including 37 patients above 65 years of age with a pubic ramus fracture, a posterior pelvic ring lesion was detected in 59% [3]. In our retrospective study of 245 patients above the age of 65 with FFP, only 44 patients (18%) had an isolated anterior pelvic ring fracture and 3 (1.2%) an isolated posterior pelvic ring fracture. The remaining 198 patients (80.8%) had a combination of anterior and posterior pelvic ring fractures [4]. We conclude that posterior and anterior pelvic ring injuries are combined in the vast majority of patients.
Anterior pelvic ring fractures or disruptions are located at the pubic symphysis , in the pubic bone near to the symphysis, at the superior and inferior pubic ramus involving the obturator foramen; and at the anterior lip of the acetabulum. In our retrospective study, we observed that most of the anterior pelvic ring fractures in elderly are pubic ramus fractures. Less frequent are pubic bone and anterior lip fractures. Instabilities of the pubic symphysis are the least frequent [4]. In a retrospective study of Starr et al. on 145 anterior pelvic ring fractures operatively treated with percutaneous screw fixation, 22 were located medial to the obturator foramen, 100 above and 23 lateral to the obturator foramen [5]. The low number of symphyseal disruptions in the elderly may be due to the fragile cortical and trabecular bone [6], while ligaments become stiffer [7], but there are no biomechanical studies, which confirm this hypothesis. Fractures and dislocations are situated at areas of highest strain and lowest stiffness, i.e. in the sacral ala, the sciatic notch with the adjacent ilium, the supra-acetabular region, the quadrilateral surface, and the pubic rami [8]. This leads to consistent fracture patterns in the posterior pelvic ring [9, 10]. Similarly, the anterior pelvic ring breaks at its weakest point, which is the pubic ramus. Sometimes, instabilities of the pubic symphysis and bone defects near to it have been observed in chronic FFP (Fig. 19.1). In these cases, we suppose that the primary instability was located in the pubic bone. Subsequently and due to continuous and repetitive movements, bone resorption occurs and finally involves the nearby joint [11].
Seventy-four-year-old female with long history of rheumatoid arthritis. The patient already had bilateral total hip replacements. She has a limited walking distance due to chronic pain in the lower lumbar spine and at the pubic symphysis . A.p. pelvic overview reveals a bone defect of the left pubic bone with widening of the pubic symphysis and cortical reaction. Irregularities of the bone structure can also be seen at the right sacral ala
Different fixation techniques have been developed for stabilization of the anterior pelvic ring in high-energy pelvic disruptions. External fixation and open reduction and plate fixation (ORIF) are the most frequently used. These techniques are also valid for fixation of anterior pelvic ring fractures in FFP. More recently, the anterior subcutaneous pelvic internal fixator has been introduced as a less-invasive technique [12]. Retrograde medullary superior pubic ramus screw fixation is another minimal invasive technique. The technique has been described several decades ago but never gained wide acceptance [13, 14]. The popularity of retrograde screw insertion is increasing now due to the increasing number of FFP, the minimal invasiveness of the procedure and the high stability of the fixation [15].
2 Rationale
Fractures of the anterior or posterior pelvic ring involve an interruption of the ring structure with loss of pelvic stability. Biomechanical studies by Tile et al. showed that stability of a cadaveric pelvic ring is diminished by 30% when the anterior pelvis is ruptured [16]. Nevertheless, when only the anterior pelvic ring is broken and diastasis between the fracture fragments not large, non-operative treatment will be the first choice. This choice of treatment is valid for fractures in adults and in elderly with FFP Type I. Analgesic therapy, bed rest and careful mobilization will lead to fracture healing and good functional recovery in the great majority of patients [17, 18].
In FFP, isolated anterior pelvic fractures account for merely 18%. More than 80% of patients with FFP have a combination of anterior with posterior pelvic ring instability. These are FFP Type II (except of FFP Type IIa), FFP Type III and FFP Type IV in the classification of Rommens and Hofmann [4]. In these fracture types, loss of stability is much higher than 30%, when compared with the intact pelvis. Consequently, non-operative therapy is challenging in some patients with FFP Type II and in most patients with FFP Type III and IV. Cumbersome management due to longer periods of immobilization and severe pain leads to prolonged recovery time and higher complication rates. Operative therapy is, therefore, recommended in all FFP Type III and FFP Type IV. When conservative treatment is not successful after 1 week, operative therapy is also recommended in FFP Type II [19].
The surgical intervention should be as minimal invasive as possible. Prolonged surgeries may provoke additional pain, increased blood loss, higher risk of infection and endanger the limited physiological reserves of the patient. Minimally invasive fixation of pubic rami fractures is feasible with a retrograde transpubic screw through the “anterior column corridor”. It can be done through an incision of a few centimeters near to the pubic symphysis. While splinting the fracture of the superior pubic ramus, the stability of the anterior pelvic ring is restored. This reduces pain immediately. However, retrograde transpubic screw fixation must be regarded as additional fixation to posterior pelvic ring fixation. If done as only procedure in patients with combined anterior and posterior fractures of the pelvic ring, there will be a higher risk of screw loosening, delayed union and nonunion of the pubic ramus fractures due to remaining posterior pelvic instability [5].
3 The Anterior Column Corridor
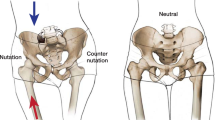
The superior pubic ramus is part of the anterior column of the acetabulum. Judet et al. described the innominate bone as an inversed Y structure, with the acetabular cavity hanged up between and being part of the two columns [20]. They distinguished the ilio-pubic as the anterior and the ilio-ischial as the posterior column. The anterior column comprises the iliac wing, anterior part of the ilium body, the anterior lip of the acetabulum, the superior pubic ramus and the pubic bone. In all patients, there exists a straight corridor between the anterior cortex of the superior pubic ramus near to the pubic tubercle and the external cortex of the ilium above the acetabulum [21]. The “anterior column corridor” lies inside the superior pubic ramus and passes medially and cranially of the acetabular cavity without penetrating it (Fig. 19.2). Its anterior and posterior entry portal, its anatomical landmarks, its dimension and orientation has recently been the subject of several anatomical and radiological studies.
Different 3D–projections of an intact pelvic ring. A retrograde transpubic screw is inserted through the left anterior column corridor. (a) a.p. pelvic view. (b) pelvic inlet view. (c) pelvic outlet view. (d) obturator-outlet view (e) iliac inlet view (f) axial projection of the anterior column corridor
Routt et al. 1995 published the technique and first results of retrograde transpubic screw placement in 24 patients. They identified an ideal starting point just inferior to the pubic tubercle and lateral to the pubic symphysis [13]. Suzuki et al. studied the anatomy of the pubic ramus and adjacent soft tissue structures in 160 Japanese (80 men and 80 women) using 3D reconstructions of pelvic CT scans. The minimal canal diameter (=maximum diameter of any implant) was on average 13.5 mm for men and 10.7 mm for women. The authors found a positive correlation between the canal diameters at the base of the corridor (para-symphyseal region) to body weight in both men and women. In women, the canal diameters at the base were also correlated to height. The canal diameters at the acetabulum were not correlated to height or weight. The mean length of the corridor was 124.6 mm in men and 123.8 mm in women. The minimum distances from the pubis to the bladder/ iliac artery/iliac vein were 0 and 0 mm/4.9 and 4.6 mm/ 0.8 and 0.2 mm in men and women, respectively. The central axis of the anterior column corridor in supine position runs at a mean of 66° and 67° cephalad and 54.1° and 55.9° laterally for men and women, respectively [21]. Chen et al. created virtual cylindrical tubes, which were placed within 164 anterior column corridors obtained from CT data of 82 Chinese adults without pelvic bone pathology [22]. The mean maximum diameter of the cylindrical implant was 8.16 mm with a length of 109.4 mm. The spatial orientation of the cylinder was 39.7°, 20.8° and 42.7° to the transverse, coronal and sagittal planes, respectively. The anterior insertion point was localized in average 18.4 mm laterally to the pubic symphysis and 17.8 mm caudally to the rim of the superior pubic ramus. The length and diameter was larger in males, with the distance to the symphysis being shorter [22]. Puchwein et al. obtained 3D reconstructions of pelvic CT data of 50 polytraumatized patients (35 males and 15 females with a mean age of 41.3 years) without pelvic injury. Virtual bolts were placed in the anterior column without perforating any cortical layer or penetrating the hip joint. The length between the entry point and exit point was measured; and the areas with the smallest cortex-bolt distance were identified. The shortest distance between the bolt and the hip joint was also measured. The average length of the bolt was 127.2 mm, the narrowest diameter 14.6 mm. Consequentially, the insertion of a 7.3 mm screw should be possible in all patients. The average distance between the bolt and the hip was 3.9 mm. The bolt was oriented with an average of 39° in the sagittal plane and 15° in the coronal plane (Fig. 19.3) [23].
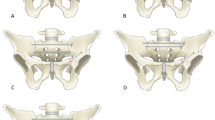
Postoperative transverse CT cuts through the pelvis of the 82-year old female depicted in Figs. 11.9, 11.12 and 11.13. (a) CT-cut through the pubic symphysis (b) CT-cut through the pubic rami. (c) CT-cut through the roof of the acetabulum. (d) CT-cut though the ilium superior to the acetabulum. The screws run completely within the bony corridor and reach the lateral cortex of the ilium above the acetabulum
Dienstknecht et al. measured the distance from the entry point at the anterior cortex of the superior pubic ramus to different landmarks, which easily can be recognized intra-operatively in anteroposterior and oblique fluoroscopic pelvic views [24]. The following landmarks were identified within a 2.5 cm range in all specimens: pubic tubercle, iliopectineal eminence, the superior rim of the superior pubic ramus, and the anterior inferior iliac spine. The authors found that there was little gender difference, except a smaller distance to the cranial rim of the superior pubic ramus in females. They stressed the significance of anatomical landmarks in percutaneous fixation of anterior pelvic ring fractures. When relying on these landmarks, screw placement can be performed safely [24].
We learn from these studies that the anterior column corridor exists in all adult humans. The length of the corridor differs between Asians and Europeans. Chinese adults have the shortest corridor (±110 mm) whereas corridors of Japanese and Europeans have similar lengths (±130 mm). The maximal diameter of a virtual cylinder filling-up the anterior column corridor was smaller in Chinese than in Japanese or Europeans. Consequently, the screw diameter should be adapted individually. Women will need smaller diameter screws than men. It therefore is recommended to analyze the CT data in different reconstructions before surgery. Data on the spatial orientation of the corridor can hardly be compared. Striking is that the angle to the sagittal plane (direction towards lateral) was comparable in the studies of Suzuki [21] (±55°), Chen [22] (±43°) and Puchwein [23] (±39.0°) and did not differ between men and women. The values of the angle to the coronal plane (direction towards cranial) were more differing. This value certainly is depending on the inclination of the pelvic ring of the supine patient. We therefore recommend holding the drill bit in a 45°-45° position to the transverse and sagittal planes with the tip of the drill at the ideal entry portal before starting the drilling procedure (see Sect. 19.5).
4 Biomechanical Studies
Simonian et al. demonstrated that fixation of the anterior pelvic ring with a retrograde transpubic 4.5 mm screw obtains the same stability as with conventional 3.5 mm plating [25]. An anteroposterior compression type II (APC-II) unstable pelvic ring injury was created in cadavers. Under physiological loading, the stability of the construct with a contoured ten-hole 3.5 mm reconstruction plate fixed with four resp. six cortical screws or with a retrograde screw with a length of 80 mm resp. 130 mm was not significantly different. These techniques were tested on the same cadaveric pelvis in a random sequence. Solid large fragment 4.5 mm stainless steel screws were used for retrograde transpubic screw insertion. The authors concluded that retrograde screw fixation is a valid alternative to plate fixation of pubic ramus fractures [25].
Gras et al. compared different screw types with standard plate fixation of anterior column fractures [26]. They tested anterior column plate fixation versus infra- and supraacetabular titanium, stainless steel, or biodegradable Poly-L-Lactid screws. The fixation strength of plate osteosynthesis and titanium screws was similar; strength of stainless steel and Poly-L-Lactid screws was inferior to the abovementioned [26].
In a more recent study, Acklin et al. found a lower stability for retrograde screw fixation than for plate fixation of pubic ramus fractures [27]. A ten-hole plate with six cortical screws was tested against an 80 mm long 7.3 mm partially threated cannulated screw. Displacement and gap angle were significantly higher for the retrograde screw during cyclic loading. The screw osteosynthesis failed due to screw cutting through the cancellous bone. The plate construct failed under higher loads due to bending [27].
From a biomechanical point of view, retrograde medullary superior pubic ramus fixation can be regarded as a valid alternative to plate fixation. To avoid cutting through the cancellous bone, as described by Acklin et al. [27], we recommend using long screws, which perforate the lateral cortex of the ilium above the acetabulum. Thanks to the firm attachment of the screw tip in cortical bone, the screw is anchored in the cortical bone, despite its cancellous profile. In contrast to what the results of the biomechanical study of Simonian et al. suggest [25], we recommend the use of large diameter screws (e.g. 7.3 mm) (Fig. 19.4).
Seventy-four-year-old female with spontaneous pain in the right groin. Initially, no specific therapy was given. Admission 3 months later due to continuous and immobilizing pain. (a) A.p. pelvic overview reveals a right-sided pubic ramus fracture. (b) Pelvic inlet view shows a non-displaced left-sided pubic ramus fracture. (c) Pelvic outlet view excludes any vertical displacement. The bone structure of the left and right sacral ala is irregular. (d) Transverse CT-cut through the posterior pelvis shows bilateral sacral ala fractures with slight widening of the fracture gap, which is typical for chronic instability. (e) Sagittal CT-reconstruction through the midline of the sacrum shows a slightly displaced horizontal fracture between S1 and S2. (f) Oblique CT-reconstruction through the small pelvis. The bilateral sacral ala fracture and the right-sided pubic ramus fracture are seen. The patient has a FFP Type IVb lesion. (g) Pelvic a.p. overview 5 months after surgery. Minimal-invasive surgical stabilization was done. The posterior instabilities have been treated with a transsacral bar, the anterior instabilities with two retrograde transpubic screws. (h) Pelvic inlet view. (i) Pelvic outlet view. The patient is free of complaints and independent for activities of daily life
5 Surgical Technique
The patient is placed supine and eccentrically on a radiolucent operation table, with his/her feet at the end of the radiolucent carbon table. This enables free movement of the C-arm for intra-operative pelvic inlet and outlet views. The lumbosacral spine is supported with a blanket, giving more stability to the pelvic ring during drilling [13]. Before draping, the area of interest is analyzed in different fluoroscopic views and the ideal inclination of the C-arm for the iliac-inlet (I-I) and obturator-outlet (O-O) oblique projections registered and marked on the machine. Due to anatomical variations and different pelvic incidences, these values may vary from patient to patient [28]. The skin area around the pubic symphysis must be free; draping is done appropriately to enable free access to the ideal entry point of the screw through the skin. It is also recommended leaving the umbilicus free for better orientation of the midline longitudinal axis of the patient’s body. Anatomical landmarks are palpated and marked on the skin. The surgeon stands opposite to the side of the pubic ramus fracture. The C-arm is placed at the side of the injury, the monitor besides the C-arm more cranial to it. The screen should be located in the working field of the surgeon. To facilitate orientation, the image seen on the screen is orientated identically to the surgeon’s view of the operative site. Horizontal on the table must be horizontal on the screen, anterior on the table in the upper part of the screen, posterior in the lower part of the screen. On the broken side, the whole anterior pelvic ring should be visible in a.-p. and oblique views to facilitate localization of the entry portal, and adequate orientation of the drill before and during the drilling procedure [14].
Before skin incision, a long drill bit is placed on the skin of the lower abdomen and adjusted along the anterior column corridor using the a.p. view (Fig. 19.5a–e). This pathway is marked on the skin. A small skin incision is made in line with the corridor. The incision is situated in the midline just below the pubic symphysis or slightly lateral, on the opposite side of the fracture. A trajectory to the anterior pubic bone is prepared using blunt scissors. A 2.8 mm drill bit, protected by a sleeve or drill guide, is placed above the entry point of the bone. As shown in several studies, the entry point is situated approximately 20 mm lateral to the pubic symphysis and approximately 20 mm below the superior rim of the superior pubic ramus [22, 24]. At first, the drill bit is hold in 45°-45° inclinations to the frontal and sagittal planes. Under image intensifier control, the location of the drill tip is adjusted until it lies precisely in line with the optimal trajectory of the screw. For this, the image intensifier is inclined into I-I and O-O positions, consecutively. While the drill bit enters the canal, it moves cranially and laterally through the superior pubic ramus. A.p., I-I and O-O views are repeated during the drilling procedure to secure correct position of the drill bit. Special attention is paid to avoid penetration into the hip joint. The drilling procedure is continued until the tip of the drill bit reaches and perforates the lateral cortex of the ilium above the acetabulum (Fig. 19.5f–i) [29]. Especially in osteoporotic bone, repetitive careful hammer blows can be used to push the drill forward into the anterior column corridor. As shown by several authors, the length of the trajectory in the bone may reach 130 mm [18, 21, 23]. The most medial-anterior part of the trajectory is over-dilled with a drill bit of 4.5 mm. A 7.3 mm cannulated screw of appropriate length is inserted over the 2.8 mm drill bit. The use of a washer is not necessary. The screw head lies in the thick tendinous attachment of the adductor muscles at the pubic bone (Fig. 19.5j–o). The screw primarily splints the superior pubic ramus fracture; it does not realize strong compression. When the drill bit cannot pass the acetabulum without perforating the joint, a shorter screw must be chosen.
Technique of retrograde medullary superior pubic ramus screw fixation. Sixty-five year old male with left-sided sacral ala fracture and bilateral pubic ramus fractures after a fall with his bicycle. (a) A.p. pelvic overview. (b) Coronal CT-cut through the anterior pelvic ring shows complete fracture of the left superior pubic ramus and incomplete fracture of the right superior pubic ramus. (c) A.p. fluoroscopic view of the left anterior pelvic ring and hip joint. (d) The drill bit is placed over the abdomen so that it superimposes the anterior column corridor. (e) A.p. fluoroscopic view with the drill bit on the abdomen. (f) Pelvic outlet view after insertion of the drill bit through the entry portal lateral to the pubic symphysis and below the superior ridge of the pubic ramus. (g) Iliac-inlet view of the left anterior pelvic ring with the tip of the drill bit inside the superior pubic ramus reaching the fracture. (h) Obturator-outlet view with the drill bit passing the roof of the left acetabulum. (i) iliac-inlet view with the drill bit inside the anterior column corridor and its tip perforating the lateral cortex of the ilium above the acetabulum. The white arrows show the inner cortex of the superior pubic ramus. (j and k) Obturator-outlet view of the left anterior pelvic ring after insertion of the screw. Position of the fluoroscope (view from the foot end of the patient) (j) and fluoroscopic view (k). (l and m) Iliac-inlet view of the left anterior pelvic ring after insertion of the screw. Position of the fluoroscope (view from the foot end of the patient) (l) and fluoroscopic view (m). (n) Postoperative pelvic inlet view. (o) Postoperative pelvic outlet view
Fracture reduction must be obtained before or during the drilling procedure. When both fracture fragments are displaced, but still in line with the anterior column corridor, reduction can easily be obtained with closed manipulation: careful pulling (external rotation) or pushing (internal rotation) on the ipsilateral iliac wing will close the fracture gap. If closed manipulation does not reduce the fracture adequately, minimally invasive techniques may be used. A small-size periosteal elevator or a bone hook is placed directly on the medial fracture fragment. Therefore, a small incision is made through the rectus abdominis muscle just above the fracture gap, alternatively through the linea alba. With the instrument in place and under image intensifier control, the medial fragment is brought in line with the lateral. When this maneuver also fails, the incision through the linea alba is enlarged and direct manipulation with the surgeon’s fingers is carried out [5]. As an alternative, the drill bit and cannulated screw are inserted in the medial-anterior fragment first and this fragment aligned to the proximal through direct manipulation with the screw. Once aligned, the drill bit is forwarded and the screw inserted in the proximal fragment [29].
6 Results
There is only little evidence available for intra-operative complications and outcomes of retrograde superior pubic ramus fixation in pelvic ring fractures. Winkelhagen et al. used retrograde superior pubic ramus screw fixation in isolated pubic ramus fractures in six elderly patients without posterior pelvic ring pathology in conventional radiographs [30]. The mean age of the six female patients was 81 years. The surgery was performed because of severe and immobilizing pain despite pain therapy. There were no intraoperative complications. There was no screw breakage or loosening. After 1 year, four patients had returned to their preoperative functional status, one patient died and one patient suffered from ipsilateral arthritis of the hip, which prevented evaluation of outcome of pubic ramus screw fixation [30].
Starr et al. published a unique and large series of retrograde transpubic screw fixations in anterior pelvic ring instabilities [5]. Eighty-two patients, who underwent 108 screw fixation procedures, were followed until fracture healing, which averaged 9 months (range 2–52 months). The average age of the patients was 35 years (range 14–85 years). This patient population was not comparable with those having a fragility fracture of the pelvis. Only nine patients (11%) suffered a fall, the other patients were victims of traffic accidents. There were 68 retrograde and 40 antegrade screw fixations. There were no intra-operative neurologic, vascular or urologic complications. There was an average blood loss of 34 cc and fluoroscopy time of 7 min. There were 16% failures of fixation (11/68). The average age of the patients with failure of fixation was 55 years. Patients aged ≥60 years failed significantly more often. Ten of the eleven patients were female, six were older than 60 years. In all but one patient, there was an internal rotation deformity (lateral compression injury) with a partial recurrence of the internal rotation deformity after failure. There was a higher rate of failure in the patients with a short medial-anterior fragment, when the fracture was localized near to the pubic symphysis . Only two patients underwent revision surgery [5].
The study by Starr et al., although retrospective, suggests that age and gender are risk factors for failure of fixation. Failure ratio might be higher in FFP than in the abovementioned series. A possible reason is the lower holding power of the retrograde screw in the osteoporotic bone, especially when the screw tip ends in the cancellous bone of the ilium. We, therefore, recommend using the maximum length of the anterior column corridor. When the screw tip perforates the outer cortex of the ilium, it has a stronger hold in the cortical bone and there is a lower risk of loosening (Fig. 19.6). Fractures near to the pubic symphysis with a short medial-anterior fracture fragment are less appropriate for retrograde screw fixation. There is low stability because the screw does not find good anchorage in the short medial-anterior fragment. For these types of fractures, we recommend a plate osteosynthesis.
A 73-year-old female with history of chronic pain after a fall. There has been a pain therapy with mobilization. (a) Pelvic a.p. overview 6 months after the fall reveals bilateral anterior pubic rami fractures with callus formation but without healing. (b) Pelvic inlet view. (c) Pelvic outlet view. (d) Axial CT-cut through the posterior pelvis reveals a left-sided ilium fracture with bridging callus, and bilateral sacral ala instabilities. (e) Multiplanar reconstruction of the pelvic ring showing anterior and posterior instabilities. The sacral corridor is too small for a safe transsacral bar placement. (f) Coronal CT-cut shows bilateral anterior instabilities. (g) Postoperative pelvic a.p. overview. The anterior instabilities were transfixed with two retrograde transpubic screws. The tip of both screws perforates the lateral cortex of the ilium, realizing the highest possible stability. The posterior instabilities were fixed with a transiliac internal fixator and two iliosacral screws. (h) Postoperative pelvic inlet view. (i) Postoperative pelvic outlet view (courtesy from Rommens et al. [31])
Conclusion
The large majority of fragility fractures of the pelvis is characterized by a combination of a fracture of the anterior and the posterior pelvic ring. When treating the posterior pelvic ring operatively, surgical fixation of the anterior pelvic ring should also be considered. Minimally-invasive approaches have the advantage of being less aggressive with short operation time, minimal soft tissue damage and minimal blood loss [31]. Retrograde transpubic screw fixation is a valid alternative to other fixation techniques. When performed carefully under intra-operative image intensification monitoring, the procedure is safe. Stability is comparable to plate osteosynthesis. There is a higher risk of loosening or implant failure when the whole length of the anterior column corridor is not used and the screw tip ends in cancellous bone. Failure of fixation has been reported to be around 15% in a large series of pelvic ring fractures. Bone healing is the rule, although it may take a long period of time.
References
Scheyerer MJ, Osterhoff G, Wehrle S, Wanner GA, Simmen HP, Werner CM. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury. 2012;43(8):1326–9.
Alnaib M, Waters S, Shanshal Y, Caplan N, Jones S, St Clair Gibson A, Kader D. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthop Traumatol. 2012;13(2):97–103. doi:10.1007/s10195-012-0182-2.
Lau TW, Leung F. Occult posterior pelvic ring fractures in elderly patients with osteoporotic pubic rami fractures. J Orthop Surg (Hong Kong). 2010;18(2):153–7.
Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44(12):1733–44.
Starr AJ, Nakatani T, Reinert CM, Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: what predicts fixation failure? J Orthop Trauma. 2008;22:81–7.
Osterhoff G, Morgan EF, Shefelbine SJ, Karim L, McNamara LM, Augat P. Bone mechanical properties and changes with osteoporosis. Injury. 2016;47(Suppl 2):S11–20.
Hammer N, Lingslebe U, Aust G, Milani TL, Hädrich C, Steinke H. Ultimate stress and age-dependent deformation characteristics of the iliotibial tract. J Mech Behav Biomed Mater. 2012;16:81–6.
Leung AS, Gordon LM, Skrinskas T, Szwedowski T, Whyne CM. Effects of bone density alterations on strain patterns in the pelvis: application of a finite element model. Proc Inst Mech Eng H. 2009;223(8):965–79.
Linstrom NJ, Heiserman JE, Kortman KE, Crawford NR, Baek S, Anderson RL, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976). 2009;34(4):309–15.
Wagner D, Kamer L, Sawaguchi T, Richards GR, Noser H, Rommens PM. Bone mass distribution of the sacrum assessed by 3D CT statistical models – implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg. 2016;98(7):584–90.
Hall FM, Goldberg RP, Kasdon EJ, Glick H. Post-traumatic osteolysis of the pubic bone simulating a malignant lesion. J Bone Joint Surg Am. 1984;66(1):121–6.
Hiesterman TG, Hill BW, Cole PA. Surgical technique: a percutaneous method of subcutaneous fixation for the anterior pelvic ring: the pelvic bridge. Clin Orthop Relat Res. 2012;470(8):2116–23.
Routt M, Simonian P, Grujic L. The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: a new technique. J Orthop Trauma. 1995;9:35–40.
Gänsslen A, Krettek C. Retrograde transpubic screw fixation of transpubic instabilities. Oper Orthop Traumatol. 2006;18:330–40.
Rommens PM. Is there a role for percutaneous pelvic and acetabular reconstruction? Injury. 2007;38(4):463–77.
Tile M, Hearn T, Vrahas M. In: Tile M, Helfet D, Kellam J, editors. Biomechanics of the Pelvic Ring. Chapter 4 in: Fractures of the Pelvis and Acetabulum. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2003. p. 32–45.
Finiels H, Finiels PJ, Jacquot JM, Strubel D. Fractures of the sacrum caused by bone insufficiency. Meta-analysis of 508 cases. Presse Med. 1997;26:1568–73.
Krappinger D, Kammerlander C, Hak DJ, Blauth M. Low-energy osteoporotic pelvic fractures. Arch Orthop Trauma Surg. 2010;130(9):1167–75.
Rommens PM, Ossendorf C, Pairon P, Dietz S-O, Wagner D, Hofmann A. Clinical pathways for fragility fractures of the pelvic ring: personal experience and review of the literature. J Orthop Sci. 2015;20(1):1–11. Review
Judet R, Judet J, Letournel E. Fractures of the acetabulum. Classification and surgical approaches for open reduction. J Bone Joint Surg. 1964;46A:1615–46.
Suzuki T, Soma K, Shindo M, Minehara H, Itoman M. Anatomic study for pubic medullary screw insertion. J Orthop Surg. 2008;16(3):321–5.
Chen KN, Wang G, Cao LG, Zhang MC. Differences of percutaneous retrograde screw fixation of anterior column acetabular fractures between male and female: a study of 164 virtual three-dimensional models. Injury. 2009;40:1067–72.
Puchwein P, Enninghorst N, Sisak K, Ortner T, Schildhauer TA, Balogh ZJ, Pichler W. Percutaneous fixation of acetabular fractures: computer-assisted determination of safe zones, angles and lengths for screw insertion. Arch Orthop Trauma Surg. 2012;132(6):805–11.
Dienstknecht T, Müller M, Sellei R, Nerlich M, Müller FJ, Fuechtmeier B, Berne A. Screw placement in percutaneous acetabular surgery: gender differences of anatomical landmarks in a cadaveric study. Int Orthop. 2013;37:673–9.
Simonian PT, Routt ML Jr, Harrington RM, Tencer AF. Internal fixation of the unstable anterior pelvic ring: a biomechanical comparison of standard plating techniques and the retrograde medullary superior pubic ramus screw. J Orthop Trauma. 1994;8(6):476–82.
Gras F, Marintschev I, Schwarz CE, Hofmann GO, Pohlemann T, Culemann U. Screw- versus plate-fixation strength of anterior column fractures: a biomechanical study. J Trauma Acute Care Surg. 2012;72(6):1664–70.
Acklin YP, Zderic I, Buschbaum J, Varga P, Inzana JA, Grechenig S, Richards RG, Gueorguiev B, Schmitz P. Biomechanical comparison of plate and screw fixation in anterior pelvic ring fractures with low bone mineral density. Injury. 2016;47(7):1456–60.
Eastman JG, Routt ML Jr. Correlating preoperative imaging with intraoperative fluoroscopy in iliosacral screw placement. J Orthop Traumatol. 2015;16(4):309–16.
Mosheiff R, Liebergall M. Technical tricks. Maneuvering the retrograde medullary screw in pubic ramus fractures. J Orthop Trauma. 2002;16(8):594–6.
Winkelhagen J, van den Bekerom MPJ, Bolhuis HW, Hogervorst M. Preliminary results of cannulated screw fixation for isolated pubic ramus fractures. Strat Traum Limb Recon. 2012;7:87–91.
Rommens PM, Wagner D, Hofmann A. Fragility fractures of the pelvis. JBJS Rev. 2017;5(3). pii: 01874474-201703000-00004) doi:10.2106/JBJS.RVW.16.00057.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Rommens, P.M., Wagner, D., Hofmann, A. (2017). Retrograde Transpubic Screw Fixation. In: Rommens, P., Hofmann, A. (eds) Fragility Fractures of the Pelvis. Springer, Cham. https://doi.org/10.1007/978-3-319-66572-6_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-66572-6_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-66570-2
Online ISBN: 978-3-319-66572-6
eBook Packages: MedicineMedicine (R0)