Abstract
Fungal infections have increased globally due to the increment of the size of population at risk for fungal infection, which is a consequence of the increased use of immunosuppressive drugs and invasive techniques for advanced life support and extended life expectancy among other reasons. Although invasive fungal infections currently are a significant cause of mortality among critically ill patients, development and approval of new systemic antifungal drugs have not occurred at the same rate as the increase in the number of fungal infections. Only one new class of systemic antifungal drugs, Echinocandins, has been included in the antifungal armamentarium in the last 20 years.
The purpose of this chapter is to review the systemic antifungal drugs currently in use, including new insights on pharmacologic and pharmacokinetics properties, clinical indications, adverse events, and resistance mechanisms. Resistance to antifungal drugs is particularly important because it has increased for every drug, including the echinocandins class. New formulations of triazol drugs and combination therapy is also highlighted.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
2.1 Polyenes (Amphotericin B Deoxycholate and Its Lipid-Associated Formulations)
2.1.1 Amphotericin B Deoxicholate
Amphotericin B (Amph B), derives from Streptomyces nodosus, belongs to a group of polyene macrolides characterized by a macrocyclic ring of lactone. Due to its low water solubility, oral bioavailability is low. This drug can be administered intravenous, intrathecal, intraarticular, intravesical, and in surgical sites. This is one of the oldest antifungal drugs but is still used in the fungal therapy because of its broad activity spectrum.
Although amph B is fungicidal in vitro, it may be fungicidal or fungistatic in vivo depending on the concentration of the drug achieved in body fluids and the susceptibility of the fungus [1].
2.1.1.1 Chemical Structure
Amph B is a heptaene macrolide compound comprising of seven conjugated double bonds within the main ring. This drug has an amino sugar called mycosamine, which in the pyranose form is linked to the hydroxyl group at C-19 of the macrolactone ring of amph B through a glycoside side chain, and a free carboxyl group on the macrocycle. Amph B has a molecular formula of C47H73NOI7 and a molecular weight of 924.09 [2, 3] (Fig. 2.1).
Chemical structure of Amphotericin B deoxicholate. Source: Reference [4]
2.1.1.2 Mechanism of Action
Amph B exerts its antifungal action by binding to ergosterol in the fungal cytoplastic membrane resulting in the formation of pores that causes an increase in their permeability with leakage of small molecules from the cytoplasm, leading to fungal death. This drug may have other effects as an oxidative damage to fungal cell or by immunomodulatory properties on the host cells [5,6,7].
2.1.1.3 Pharmacokinetics and Pharmacodynamics
Amph B is not appreciably absorbed when taken orally or subsequent to aerosol administration. Then, the intravenous formulation should be used for fungal systemic diseases. After IV administration, this drug is highly bound (>90%) to plasma proteins mainly to albumin, is weakly dialyzable and it is taken up by reticulo-endothelial organs, especially the liver, spleen and lung [8,9,10].
The activity of amph B depends on its concentration and prolonged post-antifungal effect [11]. Its elimination is biphasic. Initially, it is quickly removed with a half-life of about 24 h, while the second elimination phase has a half-life of up to 15 days [12]. In vitro evaluations have shown evident concentration-dependent killing and maximal antifungal activity at concentrations exceeding the MIC by two- to tenfold [11, 13]. In vivo time-kill studies with amph B against different Candida species have also shown an improved rate and extent of killing with increasing drug concentrations [14, 15].
Additionally, an in vivo study using a rabbit model of invasive pulmonary aspergillosis to evaluate the pharmacokinetics and pharmacodynamics of amph B deoxycholate, amph B lipid complex (ABLC) and liposomal amph B (L-AmB) found that all formulations of amph B induced a dose-dependent reduction in markers of lung injury and circulating fungus-related biomarkers. Dosing of L-AmB of 3 mg/kg/day predicts complete suppression of galactomannan and (1, 3)-d-glucan levels in the majority of patients [16].
The amph B concentration in urine is low, finding only 3% of the dose, and its penetration in cerebrospinal fluid is limited (2–4% of serum concentrations) [17]. Amph B goes through minimally into the vitreous humor and normal amniotic fluid. In the peritoneal fluid, pleura, or joint, fewer than 50% of the serum levels are obtained [18]. Serum level of the drug is not influenced by hepatic or renal function, or by hemodialysis or peritoneal dialysis. Even in anuric and nephrectomized patients, the drug serum levels and its elimination are just the same as in healthy patients. It seems that amph B is eliminated principally by metabolic conversion or by the bile [9, 19]. However, the metabolites are not yet well known.
2.1.1.4 Spectrum of Activities and Resistance
Amph B has activity against a wide range of fungi including most yeasts, and hyaline and dematiaceous molds. Among the yeast, Candida isolates resistant to polyenes are still infrequent. C. lusitaniae and Trichosporum beigelii are two fungi that have intrinsic resistance, and recently some C. krusei and C. glabrata strains with high MICs to amph B has been reported [20,21,22]. In the group of molds, Aspergillus terreus, Scedosporium apiospermum, Scedosporium prolificans, and Fusarium species are usually resistant to amph B [23].
Although breakpoints for polyenes are not available, most microbiologist use a MIC of ≥1 μg/mL to determine if an isolate is not susceptible to amph B. Reduction or absence of ergosterol in the fungal cell membrane has been associated with resistance. These alterations could be due to mutations in genes coding some of the enzymes involved in the synthesis of ergosterol. The mechanisms involved in the resistance of C. albicans isolates to the amph B include a double loss in function of both ERG3 (C-5 sterol desaturase) and ERG11 (lanosterol 14α demethylase) [24, 25]. It has also been identified isolates amph B resistant lacking ERG2, encoding C-8 sterol isomerase, and ERG6, encoding C-24 sterol methyltransferase [26,27,28].
2.1.1.5 Clinical Uses
Despite the emergence of new antifungal drugs in the last decades, amph B deoxycholate or its lipid formulations are still recommended as primary treatment for several severe or refractory fungal infections or as alternative therapy for other forms of these diseases. According to the Infectious Diseases Society of America (IDSA) guidelines for the management of candidiasis [29], amph B deoxycholate is recommended for the treatment of neonates with disseminated candidiasis or candidiasis in central nervous system, for patients with asymptomatic candiduria who undergo urologic procedures, and for symptomatic candida cystitis or symptomatic ascending candida pyelonephritis due to fluconazole-resistant C. glabrata or to C. krusei. This drug is recommended as alternative in the treatment for fluconazole-refractory oropharyngeal/esophageal candidiasis. Amph B deoxycholate or lipid formulations are also indicated for the treatment of cryptococcal meningitis, mucormycosis, moderately severe to severe forms of blastomycosis and histoplasmosis [30,31,32,33].
Aerosolized amph B, in their different formulations, is utilized as prophylaxis (either alone or in combination with systemic antifungals) in patients at highest risk of invasive fungal infections. A recent meta-analysis presented evidence supporting the concept that the prophylactic use of aerosolized amph B effectively reduces the incidence of invasive pulmonary aspergillosis among high-risk patients [34]. The current IDSA guidelines for the diagnosis and management of aspergillosis stated that aerosolized formulations of amph B may be considered for prophylaxis in patients with prolonged neutropenia and in lung transplant recipients (weak strength recommendation; low-quality evidence) [35].
Because of the low intraocular levels attained with systemic administration, intravitreal injection of amph B is useful to reach high confined antifungal activity for the treatment of severe macular involvement and vitritis. The IDSA guidelines suggest treatment with systemic antifungal drug plus local amph B deoxycholate, 5–10 μg/0.1 mL sterile water, for Candida chorioretinitis without vitritis and with macular involvement, and for Candida chorioretinitis with vitritis [29]. In addition, IDSA guidelines recommend intraocular amph B with partial vitrectomy as primary treatment of Aspergillus endophthalmitis and keratitis [34]. There are controversial reports on toxicity of intravitreal injection of amph B deoxycholate in humans, some of them have described low toxicity and others have reported toxic uveitis [36,37,38,39,40,41].
There is not a good evidence to recommend bladder irrigation with amph B deoxycholate for treatment of cystitis but, when this infection is due to fluconazole-resistant species, such as C. glabrata and C. krusei, this method of delivering the antifungal drug directly to the affected site could be used [29, 42].
2.1.1.6 Dosing
Dosing of amph B deoxycholate in adults with normal renal and hepatic function is 0.5–1 mg/kg daily for candidemia, other invasive candidiasis and for endemic dimorphic fungal infections; 1–1.5 mg/kg daily for invasive aspergillosis; 0.3 mg/kg daily for esophageal and oropharyngeal candidiasis; 0.7 mg/kg daily for empiric treatment of febrile neutropenia; and 0.7–1 mg/kg daily (usually with 5-flucytosine) for cryptococcal meningitis in the induction phase of the therapy.
2.1.1.7 Adverse Events and Toxicity
Acute toxicity related to amph B administration is due to stimulation by the antifungal drug of inflammatory cytokine production from innate immune cells via an interaction that requires CD14 and Toll-like receptors [43]. The most frequent acute effects are nausea, vomiting, rigors, fever, hypertension/hypotension, and hypoxia. Other acute adverse events with rare presentation are ventricular arrhythmias, bradycardia, and severe hypertension [44,45,46]. In addition, two cases with fatal leukoencephalopathy associated with the intravenous administration of the amph B has been reported [47].
Chronic toxicity is referred commonly to nephrotoxicity, but there are other events such as hypomagnesemia, hypokalemia, hyperphosphatemia, anemia, and rare cases of hyperbilirubinemia [48,49,50,51]. Reports of anemia of any degree of severity ranges from 33 to 63% in different studies [52,53,54].
The incidence of nephrotoxicity due to amph B is high, ranging from 49 to 65% [55, 56]. This toxicity is result of renal vasoconstriction producing reduction in glomerular filtration rate, and of direct effect on tubular epithelial cell membranes forming pores. The modification in the permeability of the tubular cell membrane will allow the back diffusion of hydrogen ions thereby weakening the acid elimination [57]. There are some factors that influence the nephrotoxicity of amph B such as cumulative dose, average daily dose, abnormal baseline renal function, concomitant nephrotoxic drugs, and patient’s risk category (bone marrow transplant, solid organ transplantation) [58]. Nephrotoxicity is cumulative and dose dependent but it is reversible after amph B treatment is stopped [58, 59]. This toxicity can be decreased by hydration and electrolyte supplementation before amph B infusion [60,61,62,63]. In the case of aerosolized amph B, the most common side effects are cough, bad taste, nausea and vomiting; most of them mild or moderate severity [64,65,66,67].
2.1.1.8 Contraindication
Amph B is contraindicated in those patients who have known hypersensitivity to this antifungal drug, and because the increment risk of nephrotoxicity and hearing impairment, its use is contraindicated with the simultaneous administration of the following drugs: amikacin, cidofovir, cyclosporine, ioversol, neomycin, streptozocin, and tacrolimus. Amph B should be discontinued before iodinated contrast media administration [68].
2.1.1.9 Drug Interactions
Corticosteroids, thiazide, loop diuretics, and neuromuscular blockers increase risk of amph B-induced hypokalaemia. Amph B can also increase the risk of digoxin toxicity [69]. Use of alternative drugs or monitoring of amph B associated adverse events is indicated when some of the above drugs needs to be used. Administration of amph B with most of the antiretrovirals does not cause interactions, but concomitant or sequential use with tenofovir increases the risk of nephrotoxicity [70]. In the same way, concomitant use of zidovudine and amph B results in increased risk of anemia and neutropenia [71].
2.1.1.10 Use in Special Population
Amph B and their lipid formulations do not need dose adjustment for patients with decreased renal function or in patients receiving hemodialysis or continuous renal replacement therapy or for those with moderate or severe hepatic disease.
Children
In pediatric population, pharmacokinetic (PK)/pharmacodynamic (PD) indices of amph B are not validated; therefore, optimal dosing of this drug has not been defined. Amph B pharmacokinetic is very variable in neonates, which may lead to treatment failure or toxicity, and the lack of maturity of the blood-brain barrier in premature infants can be the basis of a better penetration of the antifungal to the CSF [72]. Compared with adults, amph B has a lower volume of distribution and faster clearance in children [72,73,74,75,76]. Even though most of PK studies in children encourage a dosage of 0.5–1 mg/kg/day, a population PK analysis suggested that younger children receiving 1 mg/kg/day might be underexposed, while older children may be overdosed at the same dose [75]. Another study showed that amph B doses of 0.25–1 mg/kg daily to infants causes lower serum concentrations compared with older children and adults [73, 76].
The preferred amph B deoxycholate pediatric dosing is 1–1.5 mg/kg/day. The infusion adverse events and nephrotoxicity due to amph B in children are similar to adults, but fever has been rarely described in infants [77, 78]. Children usually can tolerate higher doses than adults [79].
Pregnancy and Lactation
Amph B is considered as category B (B: animal studies no risk, but human studies not adequate, or animal toxicity but human studies no risk) by the US FDA [80]. ABLC has been evaluated in animals without having found harms to the fetus [81]. Although, there are not well-conducted evaluations of amph B use in pregnancy, its use in pregnant women has been described repeatedly without confirmation of teratogenesis in their neonates [82,83,84,85,86,87,88,89,90,91,92,93,94,95,96].
This is the only systemic antifungal drug that is safe to use during the pregnancy and lactation period, although there are not published data in the last condition. Due to the properties of amph B such as its large molecular size, poor absorption, and high protein binding ability, breast milk amounts are probable insignificant [97]. There is limited information on the use of ABLC and L-AmB in pregnancy [98, 99].
It is known that amph B crosses the placenta and reaches fetal tissues where can persist some weeks after the mother has stopped the drug or given birth. This characteristic possibly would be due to placental deposit or deferred removal by the fetal kidneys [100].
2.1.2 Lipid Formulations of Amphotericin B
Lipid formulations of amph B have higher hydrophobicity, lower nephrotoxicity, and are distributed more efficiently to the sites of fungal infection or inflammation than amph B deoxycholate. The two lipid formulations available in most countries are liposomal amphotericin B (L-AmB) and amphotericin B lipid complex (ABLC), commercially available under the name AmBisome® (Gilead Sciences Inc., Foster City, CA, USA) and Abelcet (Enzon Pharmaceuticals Inc., Bridgewater, NJ, USA; Sigma Tau, Gaithersburg, MD; and Cephalon Limited, Welwin Garden City, UK) respectively. A third lipid formulation, amphotericin B colloidal dispersion (ABCD), is no longer commercially available.
The lipid compositions and particle size are different between the amph B lipid formulations, producing distinct pharmacokinetic parameters and tissue distribution. Then, the lipid formulations of amph B cannot be used interchangeably to treat patients [101,102,103].
ABLC consists of amph B complexed to two phospholipids (l-α-dimyristoylphosphatidylcholine and l-α-dimyristoylphosphatidylglycerol in a 7:3 molar ratio) in a 1:1 drug-to-lipid molar ratio to form a ribbon-like structure with a diameter of 1600–11,000 nm, making it the largest of the lipid formulations [104]. ABLC is taken by macrophages and becomes sequestered in the liver and spleen. It has lower circulating amph B serum concentrations, when it is compared with the amph B deoxycholate, but larger volume of distribution and clearance. Lung concentration of ABLC is higher than the obtained with L-AmB or amph B deoxycholate.
By contrast, molecules of L-AmB are smaller and no captured by the mononuclear phagocyte system. L-AmB consists of amph B integrated into the lipid bilayer of small unilamellar liposomes, which are composed of hydrogenated soy phosphatidylcholine, cholesterol and distearoyl phosphatidylglycerol [105]. After a dose of L-AmB, it reaches a higher peak plasma level (Cmax) than amph B deoxycholate and a larger area under the concentration–time curve. The highest amph B concentrations with the L-AmB administration are found in the liver and in the spleen, followed by kidneys and lungs. Levels in myocardium and brain tissues are low [106].
The ABLC mechanism of action requires that the fungal lipase, a heat labile extracellular product, produces a lipid breakdown within the ribbon-like material with subsequent discharge of amph B into the tissues [107]. The suggested mechanism of action of L-AmB states it binds to the fungal cell wall and disintegrates itself, discharging amph B that binds to ergosterol in the fungal cell membrane [108, 109]. Table 2.1 summarizes the characteristics of the different amphotericin B formulations.
Dissimilar results have been reported in relation to in vitro susceptibility of amph B deoxycholate and lipid formulations. Montagna et al. found great correlation between the in vitro activities of amph B deoxycholate and L-AmB against 604 clinical yeast isolates [125], while Johnson et al. found that MIC 50 and MIC 90 of ABLC were the same to or lower than those of amph B deoxycholate when they were tested against 190 isolates from different fungal species, including Aspergillus fumigatus, Candida spp., and Cryptococcus neoformans [126]. In the later study, the L-AmB was the least active of the different amphotericin B preparations tested, showing 2–4 dilutions higher in their MICs than those of amph B deoxycholate. Carrillo-Muñoz, studying the in-vitro susceptibilities of 120 clinical isolates of yeasts (including different species of Candida, Rhodotorula rubra, Trichosporon spp., Cryptococcus laurentii and C. neoformans), found no statistical significance among MICs of amph B deoxycholate, ABLC, L-AmB and other antifungal drugs when evaluating all strains. However, there were differences in the activity of these drugs for individual species. Amph B deoxycholate and ABLC had high MIC values for an isolate of C. laurentii, while L-AmB, had moderately low MIC for the same isolate. ABLC and L-AmB had higher mean MICs against Trichosporon spp., and L-AmB had high MIC90 values for C. glabrata than amph B deoxycholate [127].
In addition, the manufacturer of AmBisome® (L-AmB) claims that it has in vitro activity equivalent to amph B deoxycholate against the following fungi: Aspergillus species, Candida species, C. neoformans, Fusarium species and Blastomyces dermatitidis [69].
Experimental studies carried out in animals demonstrated that it is necessary higher doses of the two lipid formulations to achieve the same or greater antifungal effect than the obtained by the amph B deoxycholate [123, 128,129,130]. Although it is also true in the clinical setting, the toxicity, mainly nephrotoxicity, is lower when lipid formulations are used [117, 123, 131,132,133,134,135,136,137,138,139]. There is some evidence of greater effectiveness of the lipid formulations of amph B in relation to amph B deoxycholate. When used as induction therapy, L-AmB has demonstrated faster culture conversion in cryptococcal meningitis, and was associated with improved survival and lower toxicity in AIDS patients with moderate to severe disseminated histoplasmosis in comparison to amph B deoxycholate [140, 141]. L-AmB (5 mg/kg/day) also showed superior clinical efficacy to amph B deoxycholate (1 mg/kg/day) in the treatment of neutropenia-associated invasive fungal infections [139].
Any of the lipid formulations of amph B are recommended by the IDSA guidelines for the treatment of non-neutropenic patients with suspected azole- and echinocandin-resistant candidemia, candida suppurative thrombophlebitis, candida endocarditis, and chronic disseminated (hepatosplenic) candidiasis. In addition, they proposed these drugs as an alternative treatment for candidemia in neutropenic and non-neutropenic patients, candida septic arthritis, or osteomyelitis, and as alternative empiric treatment of non-neutropenic patients in the intensive care unit with suspected invasive candidiasis and with intolerance to other antifungal drugs. The same guidelines recommend L-AmB for the initial treatment for central nervous system candidiasis and for candida chorioretinitis without vitritis due to fluconazole/voriconazole-resistant isolates. L-AmB is also suggested as an alternative treatment for central nervous system candidiasis in neonates [29].
For aspergillosis infections, the IDSA guidelines recommend amph B deoxycholate and lipid formulations as alternative treatments for initial or salvage therapy. This document also suggests lipid formulations for refractory and progressive aspergillosis or for empiric and preemptive therapy in allogeneic hematopoietic stem cell transplant recipients and patients treated for acute myelogenous leukemia with prolonged neutropenia who remain persistently febrile despite broad-spectrum antibiotic therapy [35]. The IDSA guidelines also recommend lipid formulations of amph B instead of amph B deoxycholate for patients with cryptococcal meningitis with or predisposed to renal dysfunction and for the treatment of pulmonary, meningitis and disseminated sporotrichosis [30, 142].
2.1.2.1 Dosing
In general, for all fungal infections but CM, the recommended dose of lipid formulations of amphotericin B is 3–5 mg/kg daily for treatment and 1–3 mg/kg daily for prophylaxis. The dose for CM is 3–4 mg/kg per day of L-AmB and 5 mg/kg per day of ABLC, both of them with or without flucytosine, for at least 2 weeks [30, 143]. The pediatric dosing is 5 mg/kg/day of ABLC or L-AmB [144].
2.1.2.2 Adverse Events and Toxicity
In comparison with amph B deoxycholate, rates of infusion related acute reactions are similar with ABLC (60%) but lower with L-AmB (48%) [103, 117]. To reduce infusion-related reactions, it is recommended the use of low-dose hydrocortisone (1 mg/kg), diphenhydramine (25–50 mg), meperidine (0.5 mg/kg), and nonsteroidal anti-inflammatory agents as premedication [118, 135, 145].
Numerous studies have shown that lipid formulations are less nephrotoxic than amph B deoxycholate. The Barrett et al.’s systematic review found that ABLC and L-AmB decreased all-cause risk of mortality and renal toxicity, compared with amph B deoxycholate [146]. Martino’s systematic review also found that ABLC is significantly less nephrotoxic than amph B deoxycholate and can be administered securely to patients with preexisting renal injury [147]. L-AmB used in the treatment of fever in neutropenic patients with cancer showed similar efficacy but significantly less infusion-related reactions and nephrotoxicity than amph B deoxycholate [138]. In comparative trials, adverse events requiring discontinuation of the drug have occurred less frequently when patients received L-AmB (12%), followed by those receiving ABLC (32%) and amph B deoxycholate (44%) [103]. Wade et al. have also reported considerably lower rates of nephrotoxicity, infusion reactions and hypomagnesemia among patients with renal dysfunction and invasive fungal infections receiving L-AmB compared with those receiving ABLC [115].
L-AmB used in 33 consecutive patients at least 65 years old as empirical therapy for the treatment of invasive fungal infections showed equivalent safety and efficacy to those observed in younger patients, but higher incidence of severe hypokalemia when used for extended periods. The incidence of grade III or IV hypokalemia was similar in the older and younger groups [148]. A characteristic triad of acute infusion-related toxicity to L-AmB has been described. The following symptoms alone or in combination of 1 of 3 symptoms can be present: chest pain, dyspnea, and hypoxia; severe abdomen, flank or leg pain; and flushing and urticaria. These reactions occur within the first 5 min of infusion and disappear with administration of diphenhydramine. A multicenter analysis found a mean overall occurrence of 20% (range: 0–100%) of this specific toxicity among 64 centers [149].
2.2 Triazole Antifungal Agents
2.2.1 General Properties
Azoles are a group of antifungals of great importance in the treatment of systemic mycoses that share a common basic chemical structure and mechanism of action, inhibition of membrane sterol synthesis. A major change occurred with the identification of increased antifungal activity of the N substitution in the imidazole ring, which led to the development of current triazoles.
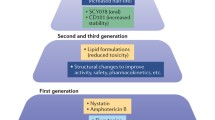
A first generation of triazoles were developed in the eighties and have been in clinical use since then, with limited (itraconazole) or no activity (fluconazole) against filamentous fungi. A second generation of drugs developed in late nineties and more recently is now available (voriconazole, posaconazole, isavuconazole), with improved activity against Aspergillus and other filamentous fungi. Clinical studies have shown their effectiveness in the management of multiple fungal infections.
Triazoles are widely used due to their broad spectrum of antifungal activity, availability of both IV and oral formulations, and safety profile. It is expected that in the future newer agents and more indications will be identified [150, 151].
2.2.1.1 Chemical Structure
The imidazole nucleus is a 5-atom heterocyclic structure with 3 C and 2 N (see Fig. 2.2). This structure is present in nitroimidazoles, utilized in antianaerobic and antiparasitic therapy (metronidazole), and azole antifungals (clotrimazole, miconazole, ketoconazole), currently used for local therapy of superficial infections. The substitution of a C for an N atom originates the term “triazoles” (three N atoms in the ring), and it is associated with significant changes in the antifungal activity and pharmacokinetic properties in relation to older azoles (i.e. ketoconazole). The triazoles have a more specific binding to fungal enzymes than to mammal enzymes for sterol synthesis, more potent antifungal activity, and broader spectrum, less metabolic side effects, and better bioavailability and tissue distribution than older azoles.
2.2.1.2 Mechanism of Action
The structural target for triazoles in the fungal cell is the cellular membrane. Action at this level explains part of older azoles limitations, since their activity would not be completely specific for fungal organisms. Older azoles have also some inhibitory activity on steroid metabolism in mammalian cells; for example, ketoconazole was used in the management of primary Cushing syndrome because of its significant inhibition of corticoid synthesis [157].
Triazoles are inhibitors of the enzyme lanosterol 14-α-demethylase, coded by the gene CYP51A, involved in the synthesis of ergosterol. This enzyme catalyzes the oxidative elimination of 14-methyl group from fungal cell lanosterol (mono-oxigenase P450 activity). Its inhibition causes the accumulation of lanosterol precursors (methyl-esterols) and changes the proper composition of the cell membrane, which produce structural and functional consequences (lanosterol deficiency and decreased membrane fluidity), primarily in cellular reproduction and death. Triazoles block the activity of the enzyme by binding to the active site, and their increased affinity to this site due to the third N atom present in the imidazole ring produces higher antifungal activity [158].
2.2.1.3 Pharmacokinetics
Main pharmacokinetic characteristics of triazoles are displayed in Table 2.2. In summary, these drugs have good oral absorption (with special ingestion requirements for certain formulations of itraconazole and posaconazole), a prolonged half-life (which allows once or twice daily dosing regimens in most cases), good distribution in body tissues with clinical use in different types of invasive disease, and are available in both oral and parenteral formulations [160].
Fluconazole and voriconazole reach higher concentrations in tissues because of their smaller molecular size. Fluconazole shows better concentration in cerebrospinal fluid, and all azoles reach good concentrations in brain tissue. Posaconazole reaches the highest concentration in alveolar cells and voriconazole in bone tissue. Triazoles concentrate similarly well in liver and kidneys [113].
Due to a less predictable absorption, interactions with other drugs, and subject variability of metabolism, therapeutic drug monitoring is recommended to optimize regimens and minimize side effects for itraconazole, voriconazole, and posaconazole [161,162,163]. Trough levels should be tested within 30 min before patient dosing. The recommended target trough plasma levels for triazoles and their recommended day of testing after initiation of therapy are shown in Table 2.3.
2.2.1.4 Spectrum of Activity and Resistance
All members in the class show good activity against most Candida species. Fluconazole is effective against most clinically significant Candida sp. and against Cryptococcus sp., and to a lesser extent against most dimorphic endemic fungi (Histoplasma, Blastomyces, Coccidioides, and Paracoccidioides spp). Itraconazole has a broader spectrum that includes Sporothrix schenckii, Aspergillus spp. and some other filamentous fungi such as dematiaceous fungi and mucorales. Its mold activity is lower than newer triazoles. Voriconazole is active against dose-dependent and fluconazole-resistant Candida species (C. glabrata and C. krusei, respectively). It also shows increased activity against molds, particularly Aspergillus spp., Fusarium spp., S.apiospermium, and dematiaceous fungi. Posaconazole and isavuconazole add to voriconazole spectrum their activity against Mucorales [167, 168].
Resistance to triazoles is well described. Mechanisms of acquisition of resistance include overexpression with increased activity of efflux pumps (ATP binding cassette, ATP and major facilitator superfamily -MFS), and point mutations that cause changes in tridimensional structure or activity of C-14α demethylase [169]. The point mutations cause structural changes in the active site of the demethylase, decreasing the affinity to its ligands. Candida species can be intrinsically resistant as is C. krusei to fluconazole, show dose-dependent susceptibility as C. glabrata versus fluconazole or acquire resistance like C. albicans to azoles, largely by changes in the activity of efflux pumps.
Aspergillus resistance to triazoles with mold activity has also been reported in some places. Specific alterations in coding regions of the enzyme in the CYP51A gene have been associated in some cases with itraconazole and posaconazole resistance and with cross-resistance to all triazoles [170].
Identification of triazole resistance is increasingly available with standardization of methods, identification of clinically relevant breakpoints, and consensus from major international institutions (CLSI, EUCAST) in recent years [171].
2.2.1.5 Clinical Utility
Triazoles have a wide spectrum antifungal activity, which includes both yeast and filamentous fungi. Much more limited in the case of the older generation, but with significant increase of activity in the case of the newer products, such as posaconazole and voriconazole.
Fluconazole continues to be of major importance in the management of different clinical presentations of candidiasis in multiple groups of patients [168], and for consolidation treatment of cryptococcosis. Itraconazole is recommended in the management of dimorphic fungi and to some extent in filamentous organisms.
Voriconazole, posaconazole, and isavuconazole have evolving roles in the management of severe fungal infections by filamentous organisms in the most immunosuppressed individuals. Voriconazole is considered a first choice for invasive aspergillosis in most clinical situations. Posaconazole has been used preferentially in antifungal prophylaxis and Mucor infections, and isavuconazole has shown high efficacy in the treatment of aspergillosis and Mucorales [172].
2.2.1.6 Adverse Events and Drug Interactions
Compared to older azoles (i.e. ketoconazole), currently available drugs show much lesser hormonal inhibition, gastrointestinal side effects, and hepatotoxicity. Triazoles as a group are deemed relatively safe drugs.
Itraconazole most commonly causes nausea (10%) and gastrointestinal symptoms (diarrhea, 8%; vomiting, 6%; abdominal discomfort, 6%). Hyperbilirubinemia and liver enzyme elevation is reported in about 5% [173].
Fluconazole used at doses higher than 400 mg/day can cause headache in 2%, anorexia in 3% of patients and transient ALT elevation in 10% of patients.
Reversible visual disturbances (30%), photosensitivity (20%), hallucinations and confusion (15%) have been described with voriconazole use. Recent reports have associated presentation of skin cancer in immune-suppressed patients with use of voriconazole, which needs further clarification [174, 175].
Side effect profile of posaconazole is very similar to that of fluconazole. Experience with isavuconazole in clinical trials has shown that it is largely well tolerated.
Prolongation of the QTc has been observed with triazoles, including posaconazole [176, 177], and this can cause sudden death. The IKr channel, one of the membrane channels responsible for potassium outflux movement, is inhibited by fluconazole and other triazoles. This inhibition is associated to ventricular repolarization changes that increase vulnerability to cardiac arrhythmias. Patients with other drugs that can cause QTc prolongation, severe bradycardia, hypokalemia, or hypomagnesemia should be cautiously prescribed when used concomitantly with azoles. Contrary to other drugs in the group, isavuconazole has been associated with QTc shortening, of unclear clinical significance.
Triazoles present a significant number of drug interactions [178, 179]. Interactions with immunosuppressants, rifamycins, anticonvulsants, omeprazole, warfarin, statins, and antiretrovirals, amongst others, are particularly important. See Table 2.4 [181].
Interactions of triazole antifungals can be divided into the following categories: modifications of antifungal pharmacokinetics by other drugs, modifications of other drug pharmacokinetics by antifungals, and two-way interactions. The mechanisms involved include azole inhibition of drug metabolizing enzyme cytochrome (CYP) P450 isozymes, such as CYP3A4/5, CYP2C9 and CYP2C19 in varying degrees [182]. Triazoles can also inhibit drug transporter P-glycoprotein (P-gp) within the gastro-intestinal tract and the liver, for which immunosuppressants are substrates.
The degree of these interactions varies greatly, as azole inhibition of relevant enzymes can be dose-dependent and differs in potency and selectivity. Itraconazole and voriconazole are reported to be more potent inhibitors of CYP3A4 than posaconazole and fluconazole. In terms of inhibition of P-gp, itraconazole and posaconazole have the more significant activity [183].
Triazoles are used frequently in transplant patients, either for prevention or treatment of suspected or proven fungal infections, and can interfere with the metabolism and transport of immunosuppressants (i.e. cyclosporine, tacrolimus, sirolimus, and everolimus), which are drugs of narrow therapeutic margin.
Triazoles can increase exposure to immunosuppressant, consequently increasing risk for side effects of these drugs. On the other hand, discontinuation of azoles without dose adjustment of the immunosuppressant drugs may lead to sub-therapeutic immunosuppressant exposure and risk of transplant rejection or graft-versus-host-disease.
As a potent inductor of CYP enzymes, rifampin significantly increases the metabolism of azoles. Concomitant use of rifampin with itraconazole, voriconazole, or isavuconazole should be avoided, and consideration to increasing fluconazole dosing is required if concomitant use is necessary [184].
In the management of HIV-infected patients, fungal infections are frequent and important complications. Efavirenz should not be coadministered with itraconazole or posaconazole. Voriconazole and itraconazole doses >200 mg/day are not advised in patients receiving protease inhibitors. Posaconazole can increase >100% AUC of atazanavir (boosted or unboosted). Fluconazole use does not generally require adjustment of dosing and can be used with most antiretrovirals [181].
2.2.1.7 Dosing and Administration. Use in Special Populations
Dosing criteria for triazoles are already established for general use in adult populations. However, the newer drugs (posaconazole, isavuconazole) still miss clinical pharmacokinetic data for groups of patients such as neonates, younger children, and pregnant women.
Neonates and Children
As more experience is accumulated, use of older triazoles in children is recommended for their routine indications [185, 186]. FDA labeling of voriconazole and posaconazole still restricts their use to older children [187]. In spite of being an older drug, itraconazole has not been developed for pediatric use and does not have formal indications [188]. Recommendations for the use of triazoles in the management of aspergillosis are similar in children and adults, although recognizing that doses of voriconazole are higher in younger children (<12 years) and in younger adolescents with a weight < 40 kg. In these patients, loading dose is 9 mg/kg twice, followed by 4–8 mg/kg (higher dose for invasive molds and more serious infections) [35, 189].
Pregnant Women
According with the FDA classification of drugs and risk category in pregnancy, fluconazole status varies with the dose used. It is considered C when a single 150 mg-dose is indicated, but is D for higher doses. This in based on observation of birth defects in five children exposed in utero to fluconazole, and animal experiments showing teratogenic potential. Fluconazole remains contraindicated in pregnancy with the exception of the lower dose. Itraconazole, isavuconazole and posaconazole are currently classified as category C, while voriconazole is in category D. Current consensus is to restrict use of triazoles in pregnancy, in particular in the first trimester [190].
Renal Failure
Dose adjustment is recommended for fluconazole. Daily dose should be reduced by 50% with a creatinine clearance lower than 50 mL/min. For end-stage renal disease patients (ESRD) on hemodialysis (HD) dose is normal and goes after dialysis. Parenteral voriconazole preparation with cyclodextrin is not recommended in renal failure due to potential accumulation and toxicity of cyclodextrin. Patients who are already on some form of renal replacement therapy do not have any concern as cyclodextrin is efficiently removed by dialysis. Because cyclodextrin contained in Itraconazole oral solution is metabolized by amylase, patients with renal failure can use it without dose adjustment [191].
Liver Failure
Voriconazole has more extensive liver metabolism and in moderate to severe liver failure, its maintenance dose should be reduced to 50% after a regular loading regimen.
Obesity
Fluconazole should be dosed by total body weight to achieve AUC/MIC ratios that have been associated with better outcomes. Posaconazole dose should not be corrected for increased body weight. This has still to be evaluated for the newer formulations (tablet, IV solution). Voriconazole dosing using total body weight can reach supratherapeutic concentrations. Its dose should not be changed for increased body weight or BMI in the case of oral voriconazole. Until further studies are performed, use of either the adjusted body weight or ideal body weight when dosing weight-based IV voriconazole could be justified [192].
2.2.2 Individual Agents
2.2.2.1 Itraconazole
Itraconazole is available as a 100 mg capsule and an oral suspension in cyclodextrin (100 mg/10 mL). Cyclodextrin makes itraconazole soluble and enhances its absorption. Oral absorption of the capsule depends on food intake, although absorption of the solution is best on an empty stomach. Interestingly, coadministration with a cola beverage increases the AUC of the capsule formulation. Absorption of the capsule is decreased with hypochlorhydria, mucositis, and graft-versus-host intestinal changes, conditions that can be present in AIDS patients or bone marrow transplant recipients.
Therapeutic drug monitoring is useful to adjust proper dosing, taking in consideration the method used for adequate interpretation. Tissue, pus and bronchial secretion concentrations of itraconazole are higher than plasma levels. The drug is metabolized in the liver and excreted in feces; prolonging its half-life in cirrhosis. When administered via oral, minimal amount of active itraconazole is eliminated in urine with most of cyclodextrin (>99%) excreted intact in feces.
Itraconazole most frequent side effects are nausea and abdominal discomfort. Frequency of gastrointestinal symptoms is higher with the solution presentation (osmotic effect). Hypokalemia and edema can be seen with higher doses. Itraconazole is contraindicated in pregnancy and in nursing mothers.
Itraconazole is useful in the treatment of dimorphic organisms (Blastomyces spp., Histoplasma sp., Coccidioides spp., Paracoccidioides spp., Sporothrix spp.), especially in less severe forms, less immunocompromised individuals or as consolidation treatment. Because activity against Aspergillus is lower in comparison to newer agents (second generation), indications of itraconazole in aspergillosis are more limited. It is indicated for the management of allergic bronchopulmonary aspergillosis or as an alternative therapy in aspergilloma [35]. Other uses include phaeohyphomycosis, ringworm, onychomycosis, tinea versicolor, and occasionally candidiasis.
Usual daily dose for cutaneous conditions, including sporotrichosis, is 200 mg. An initial loading dose of 200 mg tid for the first 3 days when used in the treatment of deep mycoses is recommended to ensure adequate serum and tissue levels in the short term. Recommended dose for treatment of invasive mycoses, selected forms of aspergillosis or prophylaxis of invasive aspergillosis is 400 mg daily, divided every 12 h.
2.2.2.2 Fluconazole
Fluconazole is an imidazole analogue to ketoconazole with more specific fungal sterol synthesis inhibition and increased antifungal activity. It has good bioavailability (>90%), which is a significant difference with itraconazole, good distribution in fluids and tissues, long serum half-life (approximately 30 h), and relatively low (11–12%) binding to plasma proteins. Its elimination is mostly renal. The molecule has a second triazole ring that decreases lipophilicity and increases unbound drug in blood.
Fluconazole for systemic use is available in capsules, tablet, powder for oral suspension, and injectable form for IV infusion at a concentration of 2 mg/mL. Tolerance to fluconazole is considered good. Liver toxicity is a concern, especially when higher doses are used for treatment of cryptococcosis or disseminated candidiasis.
Fluconazole is active against yeasts and inactive against molds. It can be used to treat mucosal candidiasis (oro-pharyngeal, esophageal, vaginal), disseminated and invasive candidiasis, cryptococcosis, and systemic dimorphic mycoses (histoplasmosis, coccidioidomycosis, paracococcidioidomycosis, and sporotrichosis). Depending on the disease severity, immunologic status or comorbidities of the patient, and available of other antifungals, fluconazole can be an initial treatment, or a consolidation phase treatment in these indications [193].
Fluconazole has had an important role in the management of serious forms of infection by Candida [194], although this role is changing in recent years with newer recommendations favoring use of echinocandins in most seriously ill patients [29, 195, 196]. In the case of invasive candidiasis and candidemia, fluconazole should be considered for patients not critically ill and infected by fluconazole-sensitive organisms, using a loading dose of 800 mg followed by 400 mg daily [29, 195]. In the treatment of mucosal candidiasis, lower doses of fluconazole are appropriate. A single 150 mg is indicated for vulvo-vaginal candidiasis, and daily doses of 100 mg are used for oro-pharyngeal and esophageal candidiasis.
Fluconazole at doses of 800 mg/day combined with amphotericin B is recommended as an alternative regimen for induction treatment in cryptococcal meningitis or disseminated disease in HIV patients when flucytosine is not available. In these patients, doses of 400 or 200 mg daily are used in the consolidation and maintenance phases respectively [30]. Dose of 400 mg daily of fluconazole are recommended as initial antifungal treatment of immunosuppressed and immunocompetent patients with mild-to-moderate pulmonary cryptococcosis [30].
2.2.2.3 Voriconazole
Voriconazole is a second generation triazole that was approved for clinical use in 2002. In voriconazole, the second triazole ring has been replaced with a fluoropyrimidine nucleus, which explains its broader spectrum. The main advantage of Voriconazole over first-generation triazoles is its activity against filamentous fungi, including Aspergillus sp., Fusarium spp., and S. apiospermium [197,198,199]. Despite its broad-spectrum activity against yeast and molds, voriconazole is not active against Mucorales.
Currently, voriconazole is considered the drug of choice for the treatment of invasive aspergillosis [35, 200]. Reported clinical experience shows some promising results with combination of voriconazole and echinocandins as a rescue regimen [201,202,203,204].
Voriconazole is available for oral and parenteral use. It should be taken with empty stomach because food and high content of fat decrease Voriconazole absorption, reducing bioavailability in 20%. Half-life is 6 h, requiring twice daily administration. Parenteral formulation of voriconazole also contains cyclodextrin, which could accumulate in renal failure. Its use in patients with renal impairment should be individualized.
In general, voriconazole is well tolerated. Reversible disturbances in vision (impaired color discrimination, blurring, and photophobia) is reported in about 25–30% of patients and are not seen with other triazoles. Skin rashes, photosensitivity, facial erythema, hallucinations and confusion are other significant side effects. Periostitis has been associated to prolonged use, and serious EKG alterations (torsade de pointes, QTc prolongation) have occurred in patients with predisposing factors to arrhythmia.
For invasive aspergillosis and serious mold infections, a loading dose of 6 mg/kg twice daily is recommended in the first day, followed by 4 mg/kg bid. For the treatment of invasive Candida infections dose should be lower, at 3 mg/kg bid. Oral dosing (tablets) is 400 mg bid the first day and then 200 mg bid for persons of >40 kg. For persons under 40 kg, the recommended dose is 200 mg bid for the first day, followed by 100 mg bid. Intake should be 1 h apart from meals.
2.2.2.4 Posaconazole
This triazole has a broad spectrum of antifungal activity, including Aspergillus and Candida [167]. It can be considered a derivative of itraconazole with structural modifications that enhance its activity and tissue concentration (lipophilic molecule with high concentration in tissues). Oral absorption and bioavailability of posaconazole suspension are difficult to predict, because they are significantly affected by factors like meal ingestion or presence of mucosal lesions in the gastrointestinal tract [205,206,207]. Posaconazole suspension should be taken with high-fat meals to enhance absorption. Although its half-life is long and suggests the possibility of once daily dosing, AUC is higher with bid or tid dosing, which is recommended for the oral suspension.
The newer delayed-release tablet has better absorption, improved bioavailability, and a fourfold increase in maximum concentration, a threefold increase of the area under the curve, and more prolonged presence in plasma. In contrast to the suspension, the effect of food or drugs that may alter gastric acidity is moderate. Additionally, patient intervariability is reduced. All this favorable pharmacokinetic changes allow for once daily dosing [161, 208, 209].
Posaconazole is usually well tolerated. In clinical trials the most common side effects have been gastrointestinal symptoms including nausea and abdominal pain. Initially available only for oral administration, its indications have been mainly referred to prophylaxis of fungal infection in patients at high risk (prolonged neutropenia, acute myeloid leukemia, post-transplant), in particular for filamentous fungal complications [210, 211]. The oral suspension has been evaluated for refractory aspergillosis at a daily dose of 800 mg with a 42% rate of global response [212]. Currently, a formulation for parenteral administration is also available and undergoing phase III clinical trial in the treatment of invasive aspergillosis, with completion estimated for July 2018 [213].
Posaconazole has good activity against Mucor spp. and has a role in the treatment of mucormycosis in combination with surgical procedures, usually after an initial period with amphotericin B [214].
Oral suspension and delayed-release tablet have different dosing regimens. The dose of the suspension is 200 mg tid with food for prophylaxis or 400 mg bid with meals when indicated for treatment [215,216,217], while the 300 mg tablet is administered once a day. Intravenous dosing of 300 mg daily is approved for prophylaxis.
2.2.2.5 Isavuconazole
It is the newest member of the second-generation triazole antifungal approved by the US FDA [159, 168, 180]. It has been approved for the treatment of both invasive aspergillosis and invasive mucormycosis [218]. It is also under investigation for the treatment of candidemia and invasive candidiasis, cryptococcosis, and dimorphic fungi [219].
Isavuconazole is administered as the hydrosoluble prodrug isavuconazonium, which is available in tablets and for parenteral administration. In preclinical and clinical studies, it has shown significant antifungal potency against a broad range of yeasts, dimorphic fungi, and molds. Isavuconazole has a broad spectrum of antifungal activity, similar to amphotericin B.
Clinical experience so far has revealed that isavuconazole may be associated with less toxicity than voriconazole, even when administered without therapeutic drug monitoring. Additionally, the oral formulation is highly bioavailable and the parenteral presentation is b-cyclodextrin–free (due in large part to the presence of aromatic moieties in the molecule). These are interesting properties that will increase interest on isavuconazole as a new addition to the triazole class of antifungals. Isavuconazole dosing is similar when administered either intravenously or orally. In both cases, the loading dose is 200 mg every 8 h for six times, followed by 200 mg daily.
2.2.3 Newer and Investigational Agents: Efinaconazole, Albaconazole, Ravuconazole and Others
A numerous group of newer triazole molecules are currently under different stages of development [220]. Preliminary clinical studies are already available for ravuconazole, albaconazole, and efinaconazole (available as a topical agent).
Ravuconazole is related to fluconazole and voriconazole. It has activity against yeasts (Candida spp. and Cryptococcus spp.), dimorphic fungi and filamentous organisms (dematecious, mucorales). It is not active in vitro against Fusarium spp. Clinical studies for onychomycosis have been reported with a mycological cure rate of 59% and clinical response of 56% [221]. It is still to be determined what potential indications may have and what results are obtained in clinical trials for systemic mycoses.
Albaconazole shows low MICs against Candida spp. and has been clinically studied in the treatment of vulvo-vaginal candidiasis and onychomycosis, and experimentally against S. prolificans. Its long half-life allows for weekly dosing.
Efinaconazole is a potent antifungal drug against T. rubrum, T. mentagrophytes and C. albicans, approved in 2014 for the treatment of onychomycosis. It also has activity against other species of fungus, including some nondermatophytes molds (Acremonium spp., Fusarium spp., Paecilomyces spp., Pseudallescheria spp., Scopulariopsis spp., and Aspergillus spp.), Cryptococcus spp., Trichosporon spp., and other species of Candida different to C. albicans [222].
The list of newer compounds includes RI26638, KP103, T8581, TAK187, FX0685, ZJ522, TAK456, Syn2869, and additional molecular modifications for dioxantriazoles, triazole-quinoxalines, and triazole-benzimidazoles.
The search for newer clinically active compounds might lead to the availability of triazole derivatives with increased antifungal spectrum and effectiveness, as well as better tolerance.
2.3 Echinocandins
Echinocandins are the newest members of the antifungal armamentarium and the first ones targeting the fungal cell wall [223, 224]. Currently, three semi-synthetic echinocandin derivatives have received FDA approval for clinical use: caspofungin (2001), micafungin (2005), and anidulafungin (2006). A fourth compound, the CD101, is under development.
2.3.1 Chemical Structure
Echinocandins are semisynthetic lipopeptides antibiotics, composed of cyclic hexapeptides with modified N-linked acyl lipid side chains [225, 226] (Fig. 2.3).
2.3.2 Mechanism of Action
Echinocandins competitively inhibit the beta-1,3-d-glucan synthesis, a polysaccharide which is an essential component of the fungal cell wall of many fungi. Beta-glucans represent between 30 and 60% of the cell wall mass in yeasts, and its depletion results in fungicidal activity for Candida spp. and fungistatic effect for Aspergillus spp. [230, 231].This mechanism of action is different from the one of other drugs, allowing a potential use of echinocandins in combination therapy [232], and because the target of echinocandins is unique to fungi, then absent in human cell, these drugs cause less toxicity and have fewer drug–drug interactions. In addition, some evidence from in vitro studies and murine models supports an immunomodulatory effect of echinocandins. They can unmask highly antigenic epitopes and amplify the host immune response [233].
2.3.3 Pharmacokinetics and Pharmacodynamics
Although pharmacokinetic and pharmacodynamic characteristics of echinocandins are similar, they differ in dosing, metabolic elimination pathways, and drug interaction profile. Like other large lipopeptide antibiotics, these drugs are poorly absorbed through the gastrointestinal system and must be administered by intravenous infusion. Due to their long half-life (10–26 h), they are dosed once daily, and because echinocandins are highly bound to plasma proteins, administration of a loading dose is recommended for caspofungin and anidulafungin, although it is not yet clear for micafungin. Also, high binding to plasma protein limit distribution of echinocandins to the cerebrospinal fluid and the eye, making them inadequate treatment for infections of these compartments [234,235,236].
Echinocandins are primarily eliminated through nonmicrosomal metabolism nonenzymatic degradation to inactive products, and then their urinary concentration is very low [234, 237]. They are not significantly metabolized by the cytochrome P450 enzymes nor are they substrates or inhibitors of P-glycoprotein pumps. As consequence, they have less drug–drug interactions in comparison with others antifungal drugs. However, caspofungin must be used with caution when severely impaired hepatic function is present.
Caspofungin shows a net terminal half-life of 27–50 h, and degrades spontaneously and is metabolized via hydrolysis and N-acetylation to two inactive metabolites; micafungin has a terminal half-life of approximately 15 h in adults, and is metabolized hepatically by arylsulfatase, catechol O-methyltransferase, and hydroxylation; while anidulafungin shows a terminal half-life of 40–50 h, and is not metabolized but instead eliminated by slow spontaneous degradation. All three echinocandins are nondialyzable, and their breakdown products are excreted predominantly by the fecal route, with only low concentrations of active drugs excreted by urine (less than 2%) [226, 231, 238].
In vitro studies showed that the fungicidal effect of echinocandins against Candida spp. is proportional to the maximum plasma drug concentration, that this effect persist after falling of drug concentration below MICs, and that it seems to correlate with the area under time-concentration curve to MIC ratio [237, 239]. However, similar information related to killing or inhibition of Aspergillus spp. is not completely defined yet [239, 240]. In addition, there are not established strategies to conduct therapeutic drug monitoring for echinocandins [237, 239].
2.3.4 Spectrum of Activity and Resistance
Because echinocandins show a similar spectrum of activity, they could be interchangeable specially when treating candidiasis infections. They have potent activity against many Candida spp. (C. albicans, C. glabrata, C. dubliniensis, C. tropicalis, and C. krusei), and although MICs againts C. parapsilosis and C. guilliermondii are often higher, they are useful drugs against these candida species [241, 242]. The fungicidal activity against Candida spp., including fluconazole-resistant C. glabrata and C. krusei, is the main advantage of echinocandins [226].
Even though echinocandins inhibit growth of Aspergillus species at very low echinocandin levels, their activity against Aspergillus spp. is only fungistatic [223, 243,244,245], this is explained because in Aspergillus species, higher activity of cell wall remodeling and beta-glucan synthase is localized in apical and sub-apical branching points. In guinea pig models, echinocandins seem to potentiate the activity of triazoles against Aspergillus spp. [219, 246].
Although beta-1,3-d-glucan synthase from Cryptococcus spp. is highly inhibit by caspofungin, echinocandins have not activity against C. neoformans and Cryptococcus gattii, neither against Trichosporun spp. [225, 226]. Echinocandins are not effective drugs to treat mycosis produced by endemic dimorphic fungi (Blastomyces dermatitidis, Histoplasma capsulatum, and Coccidioides spp.), due to their modest activity against the mycelial phase of them. In addition, echinocandins have not significant activity against non-Aspergillus molds (Mucorales, Fusarium spp., or Scedosporium spp.) [226, 247,248,249], and only modest in vitro activity, without clinical utility, for some phaeohyphomycetes [250, 251]. Echinocandins are effective agents for prophylaxis of Pneumocystis jirovecci pneumonia although less effective for established pneumonia in experimental models [252, 253].
In contrast with what happens with amphotericin B and triazoles, activity of echinocandins are not affected by presence of biofilm; echinocandins MICs are minimally affected when tested under biofilm conditions. C. albicans inoculum embedded in biofilm is almost completely cleared at the usual echinocandin serum levels [254, 255]. When evaluating activity against C. tropicalis biofilm, micafungin showed high activity while liposomal amphotericin B performed poorly [256]. This unique characteristic of echinocandins makes them particularly useful for the treatment of prosthetic device and catheter-associated infections.
Overall resistance to echinocandins of Candida spp. has been reported in up to 4%, and results from mutations in conserved regions of the gene-encoding glucan synthase (FK1 and FK2) [257, 258], and resistance to echinocandins has been documented for C. albicans, C. glabrata, C. lusitaniae, C. tropicalis, and C. parapsilosis [259, 260]. Previous exposure to an echinocandin had been associated with echinocandin resistance on multivariative analysis [254].
Resistance of C. glabrata is of particular concern, because it is now reported from around the world, at rates between 3 and 15%, and because isolation of strains with resistance to fluconazole and voriconazole and to echinocandins [259, 261,262,263,264]. Among the 162 fluconazole-resistant C. glabrata strains isolated between 2006 and 2010 in the US, resistance to any echinocandin was demonstrated in 18 (11%), while there was no resistance to echinocandins among 110 fluconazole-resistant strains isolated between 2001 and 2004 [262]. All the 18 resistant isolates contained an FKS1 or FKS2 mutation.
Resistance to echinocandins is associated with treatment failure and relapse or recurrence if there was an initial response and with higher rates of mortality at days 14 and 30 [261, 265, 266].
In an organ transplant recipient with persistent candidemia, Imbert and colleagues demonstrated that switching from both azole and echinocandin therapy to liposomal amphotericin B, produced that resistant C. glabrata isolate lost the FKS2 S663P alteration, regaining full susceptibility to echinocandin, while maintaining their pan-azole resistance. Based on this observation, authors suggest that more restricted use and/or a discontinuous administration of echinocandins may limit the spread of clinical resistance to these drugs [267].
2.3.5 Clinical Uses
Echinocandins are extensively used for prevention and empiric treatment of fungal infection, and for treatment of invasive candidiasis, especially in critically ill and neutropenic patients. The three echinocandins have FDA approval for the treatment of esophageal candidiasis and invasive candidiasis in adults. Micafungin has FDA approval to be used as prophylaxis of Candida infections in hematopoietic cell transplanted adults, while caspofungin is approved as empiric treatment for neutropenia febril, and for esophageal candidiasis and invasive candidiasis in children older than 3 months [29, 268, 269]. Echinocandins had demonstrated improved survival when compared to amphotericin B and triazoles in the treatment of candidemia and invasive candidiasis [191, 270, 271] and, similar efficacy to amphotericin B and fluconazole in the treatment of oropharyngeal or esophageal candidiasis. However, they are not frequently used for these latter indications due to their parenteral-only presentation [272,273,274,275,276,277].
Although echinocandins are not the choice to treat aspergillosis, they had shown useful for the treatment of refractory aspergillosis, when used in combination with voriconazol or with amphotericin lipid formulations [278,279,280]. Caspofungin has FDA approval as salvage therapy of invasive aspergillosis, and current IDSA guidelines stated that caspofungin or micafungin can be used to treat aspergillosis in settings in which azole and polyene antifungals are contraindicated [35]. There is also limited evidence supporting the use of echinocandins in combination therapy for the initial treatment of aspergillosis. Association of anidulafungin to voriconazole therapy had shown improved outcome in comparison to monotherapy, although without statistical significance [203, 232, 281].
Because their low urinary excretion rate, echinocandins are not considered for the treatment of UTIs. However, patients with fluconazole-resistant Candida spp. or with hepatic injury and fluconazole-sensitive Candida spp. have been successfully treated with caspofungin [282].
2.3.6 Adverse Events and Toxicity
Due to the target of echinocandins is absent in human cells, these drugs cause less toxicity. Mostly, echinocandins are well tolerated and their adverse events are mild and similar for all the three drugs currently in use. Serious adverse events requiring treatment discontinuation are fewer with these drugs than with other systemic antifungals. Most common adverse events are gastrointestinal symptoms (diarrhea, nausea, vomiting, abdominal pain, abdominal distention, and constipation), laboratorial alterations (increment of aminotransferases and alkaline phosphatase and bilirubin, hypokalemia, among others) and general disorders and administration site conditions (pyrexia, edema peripheral, Infusion-related reaction, pain at the site of infusion). Table 2.5 summarizes the most frequent adverse reactions, with frequency of at least 5% in any of the groups under evaluation, reported in clinical trials testing echinocandins [283,284,285].
Asymptomatic elevation of liver enzymes, 5–13% for aminotransferases and 12% for alkaline phosphatase, is less frequent in patients treated with echinocandins in comparison with azoles and amphotericin B. Because hepatitis, hepatomegaly, hyperbilirubinemia, and hepatic failure have been rarely reported, monitoring of hepatic enzymes is recommended when using echinocandins [226, 283,284,285]. Renal adverse event reported with the use of echinocandins involved mild decrease of serum potassium, reported between 11 and 20% in clinical trials, without significant drug related toxicity observed [226, 283,284,285]. Occurrence of anemia, neutropenia, and thrombocytopenia have been reported between 6 and 15% in clinical trials, but again hematologic toxicity attributed to echinocandins is infrequent [226, 283,284,285].
Infusion of echinocandins produces several histamine-release symptoms, including rash, pruritus, hypotension, bronchospasm, angioedema, and may be some acute cardiovascular events. Their occurrence is associated with the infusion rate and in most patients is enough to slow it to obtain improvement. In the case of anidulafungin, the infusion rate should not exceed 1.1 mg/min [226, 283,284,285]. In addition, rare cases of anaphylaxis, erythema multiforme, Stevens–Johnson syndrome, and skin exfoliation have been associated with the use of echinocandins, although a causal relationship has not been established [283,284,285].
2.3.7 Drug Interactions
Because echinocandins are not significant inhibitors or inducers of the CYP450 enzymatic pathways or p-glycoprotein drug efflux transporters, they have very few drug–drug interactions when compared with other systemic antifungals [226].There are mild interactions of caspofungin with the immunosuppressant tacrolimus and cyclosporine. In the case of tracolimus, standard drug monitoring of tracolimus is recommended. The concomitant use of caspofungin with inducers of hepatic CYP enzymes is expected to reduce the plasma concentration of caspofungin. Then adult patients receiving rifampin, which is a potent inducer of CYP3A4, should receive 70 mg/day and pediatric patients 70 mg/m2/day of caspofungin. The same dosing should be considered when patient receive other inducers such as efavirenz, nevirapine, phenytoin, dexamethasone, or carbamazepine [283].
There is no drug–drug interaction of micafungin with mycophenolate mofetil, cyclosporine, tacrolimus, prednisolone, fluconazole, and voriconazole.
In the case of nifedipine and itraconazole, the concomitant use of micafungin increment their AUC and Cmax, while sirolimus AUC was increased but its Cmax not. It is recommended that patients receiving micafungin with sirolimus, nifedipine or itraconazole should be monitored for these drugs, which dose should be reduced if necessary [284].There is not drug–drug interaction of anidulafungin with cyclosporine, voriconazole, tacrolimus, rifampin, or amphothericin B liposomal [285].
2.3.8 Use in Special Population and Dose Adjustments
Pediatric
Caspofungin and micafungin have FDA approval for use in children. Larger doses based on milligrams per kilogram are prescribed for both children and infants because the increased rate of clearance of these drugs among neonates, infants, and younger children compared with adolescents and adults [226, 286]. Caspofungin is considered safe and effective for pediatric patients older than 3 months, having the same indications as adults, with dosing based on body surface area [283]. Micafungin is approved for pediatric patients older than 4 months and is dosed in mg/kg [284].
Pregnancy and Nursing Mothers
All three echinocandins are class C agents in the pregnancy category. They should be used only if the potential benefit justifies the risk to the fetus. In animal studies, echinocandins caused embryofetal toxicity, including skeletal changes, increment of abortions and visceral abnormalities. Echinocandins could be detected in the plasma of the fetus, indicating they cross the placental barrier in rats. It is unknown if echinocandins are excreted in human breast milk, but they could be detected in the milk of lactating rats. Again, they should be administered to nursing mothers only if the potential benefit justifies the risk [226, 283,284,285].
Dose Adjustments
As described above, a 70 mg/day dose of caspofungin is recommended when adult patients use rifampin concomitantly, while the pediatric dose is 70 mg/m2/day. The same dosing should be considered if there is concomitantly use of other inducer of CYP450, such as carbamazepine, dexamethasone, efavirenz, nevirapine, or phenytoin [283,284,285].There is no need of dose adjustment in presence of renal insufficiency, including patients in hemodialysis or continuous renal replacement therapy [226, 283,284,285]. In the case of adults with mild hepatic insufficiency, maintenance dose of caspofungina is the same. This should be reduced to 35 mg/day in the case of moderate hepatic insufficiency (Child-Pugh score 7 to 9). There is no recommendation available for dosing caspofungin in adults with severe hepatic insufficiency or pediatric patients with any degree of hepatic insufficiency [283]. There is no need of dose adjustment of micafungin or anidulafungin in presence hepatic insufficiency of any degree [284, 285].
Obesity
Because clearance of echinocandins increment with body weight and there is no difference in outcomes of obese and nonobese patients receiving the same dose of caspofungin, it is recommended an increment between 25 and 50% of the daily dose only for patients weighting 75 kg with severe infection [226, 287].
2.3.9 Adult Dosing
The dosing of echinocandins is slightly variable according with the indication. See Table 2.6.
2.3.10 New Echinocandin
Currently, a new echinocandin, named CD101/Bifungina, is under development for topical and weekly IV administration. It exhibits prolonged stability in plasma and aqueous solutions up to 40 °C [288], and has shown in vitro activity against resistant Candida spp. and Aspergillus spp. strains. There are two phase II studies currently enrolling patients.
2.4 Flucytosine
2.4.1 Chemical Structure
Flucytosine (5-fluorocytosine or 5-FC) is a synthetic nucleoside analogs chemically related to anticancer drugs (fluorouracil and floxuridine). Its molecular formula is C4H4FN3O with a MW of 129.1 (Fig. 2.4).
Chemical structure of flucytosine. Source: Reference [289]
2.4.2 Mechanism of Action
Flucytosine is transferred into fungal cells by cytosine permeases, where it is converted into 5-fluorouracil and phosphorylated to 5-fluorodeoxyuridine monophosphate. This compound inhibits thymidylate synthase, a crucial enzyme in the synthesis of 2′-deoxythymidine-5′-monophosphate that is an essential precursor for DNA biosynthesis, therefore disturbing DNA synthesis [290]. In addition, the 5-fluorodeoxyuridine monophosphate can be further phosphorylated and be incorporated to RNA, disrupting protein synthesis [291].
2.4.3 Pharmacokinetics and Pharmacodynamics
A feature of the drug is its almost complete and fast absorption after oral administration, having a bioavailability of 76–89% [292]. The AUC is 62 mg·h/L and the maximal concentration is 80 μg/mL [290]. Flucytosine (5-FC) achieves fungistatic levels quickly and distributes extensively throughout the body fluids, including eyes and the cerebrospinal fluid, where it reaches approximately 75% of serum levels.
The 5-FC half-life in humans with normal kidney function is 3–5 h, but it is considerably delayed to 30–250 h in renal insufficiency [293, 294]. Only 2–4% of 5-FC is protein binding, between 80 and 90% is eliminated unchanged in the urine, and the liver metabolizes only a minimal amount. Flucytosine is removed by hemodialysis in 66–75%, but peritoneal dialysis is not as effective as hemodialysis [292, 295].
2.4.4 Spectrum of Activities and Resistance
Flucytosine is active against C. neoformans and Candida species except C. krusei, but isolates of Aspergillus species are usually nonsusceptible to 5-FC in vitro. Exist synergy with amphotericin B, which modifies the permeability of the fungal cell membrane allowing greater penetration of 5-FC.
Fungi with primary resistance to 5-FC are rare. A mutation in the FCY2 gene, which encodes the cytosine permease, affects the absorption of the drug diminishing accumulation of the drug within the cell [296, 297]. Secondary resistance develops during therapy, especially during monotherapy, and it is based on inactivation of enzymes of the pyrimidine pathway. Mutations in the FCY1 gene that encodes for the cytosine deaminase, or mutation in the FUR1 gene that encodes for the uracil phosphoribosyl transferase induce acquired resistance by interference in the conversion of 5-FC to 5-fluorouracil, or from 5-fluorouracil to 5-fluorouridine monophosphate respectively [296,297,298,299,300].
Other resistance mechanisms have been suggested for C. glabrata. It was found that in the presence of 5-FC the fungal cell wall showed higher resistance to lyticase, suggesting that cell wall alteration occurs in response to 5-FC. Genes CgFPS1 and CgFPS2 of C. glabrata, encoding a plasma membrane aquaglyceroporin, are recognized as factors of 5-FC resistance. Both genes facilitate resistance by declining 5-FC accumulation in C. glabrata cells. Unlike, the deletion of CgFPS2 and particularly of CgFPS1 was found to improve the susceptibility to 5-FC registered for the parental strain [301].
2.4.5 Clinical Uses
Flucytosine should be used in combination therapy, generally with amphotericin B (Amph B), to decrease development of resistance. This combination is recommended as primary therapy for cryptococcal meningitis, severe pulmonary cryptococcosis and cryptococcocemia [30]. Additionally, 5-FC in combination with Amph B is used for patients with refractory Candida infections, such as endocarditis, meningitis, or endophthalmitis and it is also recommended for the treatment of symptomatic ascending Candida pyelonephritis due to fluconazole-resistant C. glabrata [29].
The ESCMID and ECMM guidelines for the management of rare invasive yeast infections recommend amph B alone or in combination with 5-FC for infections due to Geotrichum candidum or Rhodotorula spp. They suggest the combination of amph B and 5-FC for infections due to Saccahromyces cerevisiae, and the combination of triazole plus echinocandin plus 5-FC to treat cerebral abscess due to dematiaceous fungi when surgery is not possible [30, 302].
2.4.6 Adverse Events and Toxicity
The toxicity to 5-FC is dose-dependent. The most frequent adverse events with this drug are bone marrow depression (leukopenia, anemia, and thrombocytopenia) and gastrointestinal disturbances (nausea, vomiting, diarrhea, abdominal pain, anorexia, dry mouth, and duodenal ulcer) [303,304,305,306,307,308]. Although bone narrow toxicity can occur with lower serum concentrations of 5-FC, it is more frequent when the concentration is greater than 100 μg/mL [305, 309]. For this reason, it is necessary to monitor the 5-FC serum concentrations to be sure they range between 25 and 100 μg/mL [310].
Less frequently, toxicity occurs in the central nervous system (headache, drowsiness, confusion, vertigo, and hallucinations) or manifest as liver function test abnormalities (jaundice, bilirubin elevation, increased hepatic enzymes, and acute hepatic injury). Colitis is reported infrequently, with toxicity related to local cytotoxic effect on protein synthesis [311,312,313].
Recently, a study performed in mice suggests that therapy with amph B combined with 5-FC originates a synergistic inflammatory activation in a dose-dependent way in hepatic tissues. Caution when using this antifungal combination is required, particularly for patients with hepatic deficiency [314].
2.4.7 Drug Interactions
Use of clozapine or deferiprone concurrently with 5-FC is not advised. They procainamide. Use of cytosine arabinoside could deactivate the antifungal action of 5-FC by competitive inhibition [290].
It was also noted that drugs which decrease glomerular filtration may extend the half-life of 5-FC [315]. Amph B-associated nephrotoxicity will delay elimination of 5-FC, causing an increase in serum 5-FC concentrations, may increase the risk and severity of bone marrow toxicity. Others agents that can increase the myelotoxic risk and therefore caution should be exercised in their use concomitantly with 5-FC are antineoplastic drugs (cyclophosphamide, doxorubicin, methotrexate, paclitaxel, vinblastine), antiviral agents (gancyclovir, foscarnet), antirretrovirals (zidovudine, lamivudine, didanosine, stavudine), chloramphenicol, dapsone, interferon alfa, linezolid, pentamidine and procainamide.
2.4.8 Use in Special Population
Dose adjustment is necessary in patients with renal dysfunction. In that case, the dose interval has to be extended (see Table 2.7). With a creatinine clearance below 10 mL/min, 5-FC serum levels should be monitored, doing appropriate dose adjustments so not to exceed 80 μg/mL. Because 5-FC is dialyzable, the daily dose must be administered post hemodialysis.
Because of reduced renal function in neonates with a very low birth weight, use of 5-FC in this population should be done with very close monitoring of serum drug levels to avoid large accumulation of 5-FC in plasma [72]. Flucytosine is considered as category C according to the FDA pregnancy category (animal studies show toxicity, human studies inadequate but benefit of use may exceed risk). It is contraindicated during early pregnancy (first trimester) because the drug crosses the human placenta and for its known teratogenic effect in rats and its interference with DNA synthesis in the growing fetus [320, 321]. The delivery of 5-FC in human milk is unknown, and its use during breastfeeding is not recommended. Dosing of 5-FC in obese patients is that for the ideal body weight.
2.5 Terbinafine
Terbinafine is a drug that belongs to the allylamine group, which includes also the topical antimycotic naftifine. Terbinafine is potent inhibitors of ergosterol biosynthesis, available as tablets, spray, cream, and gel formulations.
2.5.1 Chemical Structure
Chemically, terbinafine is (E)-N-(6,6-dimethyl-2-hepten-4-ynyl)-N-methyl-1- naphthalenemethanamine hydrochloride with a MW of 327.90 (Fig. 2.5).
Chemical structure of terbinafine. Source: Reference [322]
2.5.2 Mechanism of Action
Terbinafine acts as antifungal drug by noncompetitive inhibition of squalene epoxidase, an enzyme that converts the squalene into 2,3-oxidosqualene that then form lanosterol, which is a precursor of ergosterol, an essential constituent of fungal membrane. At that point, the intracellular accumulation of squalene, which is toxic to fungal cells, and a deficiency in ergosterol cause a quick cell death [323, 324].
2.5.3 Pharmacokinetics and Pharmacodynamics
Terbinafine is well absorbed from the gastrointestinal tract, with a bioavailability ranging from 70 to 85%, which varies discretely when it is taken with foods no requiring dose modification. It has a low affinity for muscle, spleen, and brain tissues, but it has high affinity for the skin and adipose tissues, which are the largest depot for the antifungal drug [325, 326].
Gastric acidity does not seem to influence the absorption. Terbinafine reaches maximal plasma concentrations approximately 2 h after a single dose, getting high concentrations in the adipose tissue, stratum corneum, dermis, epidermis, sebum, nails, and in the hair follicle [327,328,329]. Penetration of the antifungal drug into the brain ranges between 6 and 43% of the plasma concentration, and is undetectable in CSF [325].
Linear dose-proportional pharmacokinetic has been proven after a range of single doses from 125 to 750 mg of terbinafine [330]. Steady-state plasma levels of terbinafine are attained after 10–14 days of treatment decreasing rapidly after the end of treatment [331, 332]. Plasma half-life ranges from 16 to 26 h after administration of 250 mg of terbinafine in healthy volunteers. A supplementary elimination phase with a half-life of more than 90 h was detected after administration of radiolabelled terbinafine [333,334,335,336].
This antifungal drug is extremely lipophilic, 99% protein bound and it has a good penetration in the keratinized tissue, reaching active concentrations in nail in 1–2 weeks. A characteristic of this drug is to remain in the nail in therapeutic concentrations for a long time after discontinuing the drug. Terbinafine is not detected in sweat [328, 329, 335].
Terbinafine is metabolized by the liver. Several cytochrome isoenzymes are involved in the main pathways of terbinafine metabolism. Some of them are CYP2C9, CYP2C8 and CYP1A2 (N-demethylation), CYP3A4 (deamination), CYP2C9, CYP2C8, CYP2C19, and CYP1A2 (alkyl side chain oxidation) and, CYP2C9 and CYP1A2 (dihydrodiol formation). The multiple cytochrome P-450 s implicated in the metabolism of this drug indicates a reduced potential for drug–drug interactions [337, 338]. Nonetheless, terbinafine may inhibit the metabolism of CYP2D6 substrates. It could be important for the interaction with some drugs that are known substrates of CYP2D6 such as amitriptyline, carvedilol, codeine, haloperidol, metoprolol, paroxetine, risperidone, and tramadol. The coadministration of terbinafine with these drugs with could cause a prolonged increase in their plasma levels [339].
Terbinafine is excreted mainly in the urine (80%) and in small amounts in feces (20%) [335]. In children, a dosage adjustment according to bodyweight is recommended because AUC values are significantly higher than in young adults [340].
2.5.4 Spectrum of Activities and Resistance
Terbinafine has potent antifungal activity against a diversity of dermatophytes isolated from patients worldwide, including Trichophyton tonsurans, Microsporum canis, M. gypseum, T. verrucosum, T. violaceum, M. audouinii, T. rubrum, T. interdigitale, T. mentagrophytes, and Epidermophyton floccosum [341,342,343]. Also, in vitro studies have shown that terbinafine is highly active against Sporothrix brasiliensis, S. schenckii, and S. globosa isolated from clinical samples in Brazil [344, 345], and for a wide variety of agents of chromoblastomycosis [346]. Terbinafine is only moderately active against Madurella mycetomatis isolates [347].
2.5.5 Clinical Uses
Terbinafine is available in different formulations, tablets, and topical preparations such as cream, jelly, spray, and solution. Topical formulations are used to treat superficial fungal infections due to dermatophytes or Candida species.
Terbinafine is the first line treatment for toenail onychomycosis due to dermatophytes [348, 349]. This antifungal drug presents the greatest rate of mycological cure according to results from a systematic review and a network meta-analysis conducted to compare the relative efficacy of treatments for onychomycosis due to dermatophyte [350]. Oral terbinafine has been also proved effective in treating onychomycosis due to Scopulariopsis species [350,351,352].
Terbinafine is also indicated for tinea capitis caused by Trichophyton species in children. A meta-analysis of randomized, controlled trials comparing griseofulvin and terbinafine for the treatment of tinea capitis has shown that terbinafine is superior for tinea capitis caused by Trichophyton spp., whereas griseofulvin is superior when Microsporum spp. is the etiological agent [353, 354]. For other tinea infections (corporis, cruris, or pedis) without response with cream/gel, oral terbinafine may be used.
For cutaneous and lymphocutaneous sporotrichosis, terbinafine administered at a dosage of 500 mg orally twice daily is considered a safe alternative treatment (A-II) to itraconazole [142]. Based in reports showing successful outcome using combination therapy including terbinafine for treating Scedesporium infections, the ESCMID and ECMM joint guidelines proposes the use of caspofungin plus terbinafine as salvage therapy for Scedosporium spp. infections in cystic fibrosis patients with lung transplantation (quality of evidence and strength of recommendation: CIII) and voriconazole plus terbinafine for patients with lung infections, osteomyelitis/septic arthritis and for disseminated infection due to S. prolificans (quality of evidence and strength of recommendation: BIII) [355,356,357,358,359].
ESCMID also recommends use of an azole or terbinafine plus surgery (AIII) for the treatment of eumycetoma or combination therapy with azoles plus terbinafine or flucytosine for refractory eumycetoma cases (B III). High-dose of terbinafine (1000 mg/day) alone for 24–48 weeks had shown to be clinically effective and well tolerated when used to treat patients with eumycetoma, whose only therapeutic option is surgery. Among 23 eumycetoma patients, 16 out of 20 who completed the study showed improvement or cure [360].
Few case reports about successful outcome of the use of terbinafine plus amphotericin B in the treatment of disseminated fusariosis had been published [361, 362].
Terbinafine can be used as alternative to itraconazole (BIII) in the treatment of chromoblastomycosis, and in combination with itraconazole for cases of refractory disease [302]. Terbinafine dosing for the most common indications in adult and pediatric patients are shown in Tables 2.8 and 2.9.
2.5.6 Adverse Events and Toxicity
Terbinafine is an antifungal drug well tolerated even in people over 65 years, many of whom may be taking antihypertensives, antidiabetics, or lipid-lowering agents concomitantly [363]. Adverse reactions related to terbinafine are usually mild in severity. Gastrointestinal complaints are common events [364]. Patients on treatment with this drug may complain of nausea, diarrhea, bloating, dyspepsia, epigastric pain, and other less-frequent gastrointestinal symptoms [365]. More rare effects are skin reactions, cholestatic hepatitis and taste loss [366,367,368,369]. The frequency of taste loss ranges between 0.1 and 1% [369]. Risk factors associated with taste loss due to terbinafine are age (65 years and older, OR: 4.4, 95% CI: 1.4–16.1) and body mass index below 21 kg m2 (OR:4.4, 95% CI: 1.6–14.2). The OR of taste loss in patients 55 years and older with a BMI below 21 kg m2 is 12.8 when comparing with patients below 35 years old (95% CI: 1.9–88.6) [370].
Cutaneous adverse effects of terbinafine have a wide spectrum of presentation and are infrequent, having been reported in less than 2% of the patients. Recently, a case report of terbinafine-induced lichenoid drug eruption in a patient receiving the antifungal drug for 2 weeks was published. Lesions disappeared totally after 8 weeks of drug withdrawal [371]. Other rare cutaneous side effect induced by terbinafine is pityriasis rosea [372]. Also, the induction of subacute cutaneous lupus erythematosus and exacerbation of systemic lupus erythematosus by terbinafine have been reported [373, 374].
The incidence of serious side effect is less than 1%. Cases of Stevens-Johnson syndrome, neutropenia/agranulocytosis, thrombocytopenia, and aplastic anemia have been rarely reported [375,376,377,378,379,380,381,382,383,384]. Hepatotoxicity (including acute hepatitis, cholestasis, acute liver failure and vanishing bile duct syndrome) due to terbinafine has an incidence of 0.5–3/100,000. In most of these events improve after discontinuation of the drug [385,386,387]. A mixed hepatitis-cholestatic liver injury has also been reported [388].
2.5.7 Drug Interactions
Terbinafine does not inhibit or induce CYP 3A4, but it inhibits CYP2D6. Then, interactions with drugs that are metabolized by CYP 2D6 such as tricyclic antidepressants (amitriptyline, amoxapine, clomipramine, doxepin, imipramine, nortriptyline), ß-blockers (atenolol, metoprolol, propranolol, timolol, carvedilol), type B monoamine oxidase inhibitors (rasagiline and selegiline), some antipsychotic (chlorpromazine, haloperidol, risperidone, thioridazine), certain arrhythmics (lidocaine, procainamide), several medications for attention deficit hyperactivity disorder (atomoxetine, methamphetamine, methylphenidate), chloroquine, mirtazapine and dextromethorphan can potentially occur, increasing risk of side effects of these drugs. Concomitant use of tamoxifen with terbinafine should be avoided because it causes a decrease of endoxifen, one of the most important metabolites of tamoxifen, thereby decreasing the effectiveness of tamoxifen [389]. Terbinafine also mildly inhibits the metabolism of cyclosporine with little clinical significance [390].
2.5.8 Use in Special Population
No dosage modification is necessary in elderly patients. Terbinafine is contraindicated for patients with chronic or active hepatic disease [391]. Also, it is not recommended for patients with creatinine clearance lower than 50 mL/min because there are not satisfactory studies to confirm its safety in this population. Terbinafine has not been associated with any teratogenic toxicity in animals. Although it is not known whether terbinafine crosses the human placenta, it is categorized as a Pregnancy Category B drug by the FDA. The product labeling recommends against its use during pregnancy for both, topical and oral formulations. Small amounts of terbinafine are excreted in breast milk contraindicating its use in breastfeeding mothers [392].
References
Takemoto K, Yamamoto Y, Ueda Y (2006) Evaluation of antifungal pharmacodynamic characteristics of AmBisome against Candida albicans. Microbiol Immunol 50:579–586
Donovick R, Gold WH, Pagano JF, Stout HA (1955–1956) Amphotericins A and B, antifungal antibiotics produced by a streptomycete. I. In vitro studies. Antibiot Annu 3:579–586
Mechlinski W, Schaffner CP, Ganis P, Avitabile G (1970) Structure and absolute configuration of the polyene macrolide antibiotic amphotericin B. Tetrahedron Lett 44:3873–3876
National Center for Biotechnology Information. PubChem Compound Database; CID=5280965. https://pubchem.ncbi.nlm.nih.gov/compound/amphotericin%20B. Accessed 29 Jan 2017
Brajtburg J, Powderly WG, Kobayashi GS, Medoff G (1990) Amphotericin B: current understanding of mechanisms of action. Antimicrob Agents Chemother 34:183–188
Nair MP, Schwartz SA (1982) Immunomodulatory effects of amphotericin-B on cellular cytotoxicity of normal human lymphocytes. Cell Immunol 70:287–300
Mesa-Arango AC, Scorzoni L, Zaragoza O (2012) It only takes one to do many jobs: amphotericin B as antifungal and immunomodulatory drug. Front Microbiol 3:286
Christiansen KJ, Bernard EM, Gold JW, Armstrong D (1985) Distribution and activity of amphotericin B in humans. J Infect Dis 152:1037–1043
Collette N, van der Auwera P, Lopez AP, Heymans C, Meunier F (1989) Tissue concentrations and bioactivity of amphotericin B in cancer patients treated with amphotericin B-deoxycholate. Antimicrob Agents Chemother 33:362–368
Bekersky I, Fielding RM, Dressler DE, Lee JW, Buell DN, Walsh TJ (2002) Plasma protein binding of amphotericin B and pharmacokinetics of bound versus unbound amphotericin B after administration of intravenous liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate. Antimicrob Agents Chemother 46:834–840
Ernst EJ, Klepser ME, Pfaller MA (2000) Postantifungal effects of echinocandin, azole, and polyene antifungal agents against Candida albicans and Cryptococcus neoformans. Antimicrob Agents Chemother 44:1108–1111
Atkinson AJ, Bennett JE (1978) Amphotericin B Pharmacokinetics in humans. Antimicrob Agents Chemother 13:271–276
Turnidge JD, Gudmundsson S, Vogelman B, Craig WA (1994) The postantibiotic effect of antifungal agents against common pathogenic yeasts. J Antimicrob Chemother 34:83–92
Andes D, Stamstad T, Conklin R (2001) Pharmacodynamics of amphotericin B in a neutropenic mouse disseminated-candidiasis model. Antimicrob Agents Chemother 45:922–926
Andes D, Safdar N, Marchillo K, Conklin R (2006) Pharmacokinetic-pharmacodynamic comparison of amphotericin B (AMB) and two lipid-associated AMB preparations, liposomal AMB and AMB lipid complex, in murine candidiasis models. Antimicrob Agents Chemother 50:674–684
Al-Nakeeb Z, Petraitis V, Goodwin J, Petraitiene R, Walsh TJ, Hope WW (2015) Pharmacodynamics of amphotericin B deoxycholate, amphotericin B lipid complex, and liposomal amphotericin B against Aspergillus fumigatus. Antimicrob Agents Chemother 59:2735–2745
Luna B, Drew RH, Perfect JR (2000) Agents for treatment of invasive fungal infections. Otolaryngol Clin N Am 33:277–299
Kutty K, Neicheril JC (1987) Treatment of pleural blastomycosis: penetration of amphotericin B into the pleural fluid. J Infect Dis 156:689–690
Craven PC, Ludden TM, Drutz DJ, Rogers W, Haegele KA, Skrdlant HB (1979) Excretion pathways of amphotericin B. J Infect Dis 140:329–341
Tortorano AM, Prigitano A, Biraghi E, Viviani MA (2005) The European Confederation of Medical Mycology (ECMM) survey of candidaemia in Italy: in vitro susceptibility of 375 Candida albicans isolates and biofilm production. J Antimicrob Chemother 56:777–779
Blinkhorm RJ, Adelstein D, Spagnuolo PJ (1989) Emergence of a new opportunistic pathogen, Candida lusitaniae. J Clin Microbiol 27:236–240
Walsh TJ, Melcher GP, Rinaldi MG, Lecciones J, McGough DA, Kelly P, Lee J, Callender D, Rubin M, Pizzo PA (1990) Trichosporon beigelii, an emerging pathogen resistant to amphotericin B. J Clin Microbiol 28:1616–1622
Messer SA, Jones RN, Fritsche TR (2006) International surveillance of Candida spp. and Aspergillus spp.: report from the SENTRY Antimicrobial Surveillance Program (2003). J Clin Microbiol 44:1782–1787
Martel CM, Parker JE, Bader O et al (2010) A clinical isolate of Candida albicans with mutations in ERG11 (encoding sterol 14alphademethylase) and ERG5 (encoding C22 desaturase) is cross-resistant to azoles and amphotericin B. Antimicrob Agents Chemother 54:3578–3583
Sanglard DIscher F, Parkinson T, Falconer D, Bille J (2003) Candida albicans mutations in the ergosterol biosynthetic pathway and resistance to several antifungal agents. Antimicrob Agents Chemother 47:2404–2412
Hull CM, Bader O, Parker JE et al (2012) Two clinical isolates of Candida glabrata exhibiting reduced sensitivity to amphotericin B both harbor mutations in ERG2. Antimicrob Agents Chemother 56:6417–6421
Vandeputte P, Tronchin G, Larcher G et al (2008) A nonsense mutation in the ERG6 gene leads to reduced susceptibility to polyenes in a clinical isolate of Candida glabrata. Antimicrob Agents Chemother 52:3701–3709
Young LY, Hull CM, Heitman J (2003) Disruption of ergosterol biosynthesis confers resistance to amphotericin B in Candida lusitaniae. Antimicrob Agents Chemother 47:2717–2724
Pappas PG, Kauffman CA, Andes DR et al (2016) Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62:e1–50
Perfect JR, Dismukes WE, Dromer F et al (2010) Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 50:291–322
Skiada A, Lanternier F, Groll AH et al (2013) Diagnosis and treatment of mucormycosis in patients with hematological malignancies: guidelines from the 3rd European Conference on Infections in Leukemia (ECIL 3). Haematologica 98(4):492–504
Chapman SW, Dismukes WE, Proia LA et al, Infectious Diseases Society of America (2008) Clinical practice guidelines for the management of blastomycosis: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis 46:1801–1812
Wheat LJ, Freifeld AG, Kleiman MB, et al, Infectious Diseases Society of America (2007) Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 45:807–825
Xia D, Sun WK, Tan MM et al (2015) Aerosolized amphotericin B as prophylaxis for invasive pulmonary aspergillosis: a meta-analysis. Int J Infect Dis 30:78–84
Patterson TF, Thompson GR 3rd, Denning DW et al (2016) Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 63:e1–e60
Naidoff MA, Green WR (1975) Endogenous Aspergillus endophthalmitis occurring after kidney transplant. Am J Ophthalmol 79:502–509
Roney P, Barr CC, Chun CH, Raff MJ (1986) Endogenous Aspergillus endophthalmitis. Rev Infect Dis 8:955–958
Weishaar PD, Flynn HW Jr, Murray TG et al (1998) Endogenous Aspergillus endophthalmitis: clinical features and treatment outcomes. Ophthalmology 105:57–65
Wilmarth SS, May DR, Roth AM, Cole RJ, Nolan S, Goldstein E (1983) Aspergillus endophthalmitis in an intravenous drug user. Ann Ophthalmol 15:470–472
Essman TF, Flynn HW Jr, Smiddy WE et al (1997) Treatment outcomes in a 10-year study of endogenous fungal endophthalmitis. Ophthalmic Surg Lasers 28:185–194
Bae JH, Lee SC (2015) Intravitreal liposomal amphotericin B for treatment of endogenous candida endophthalmitis. Jpn J Ophthalmol 59:346–352
Drew RH, Arthur RR, Perfect JR (2005) Is it time to abandon the use of amphotericin B bladder irrigation? Clin Infect Dis 40:1465–1470
Sau K, Mambula SS, Latz E, Henneke P, Golenbock DT, Levitz SM (2003) The antifungal drug amphotericin B promotes inflammatory cytokine release by a tolllike receptor and CD14-dependent mechanism. J Biol Chem 278:37561–37568
Burke D, Lal R, Finkel KW, Samuels J, Foringer JR (2006) Acute amphotericin B overdose. Ann Pharmacother 40:2254–2259
Wiwanitkit V (2006) Severe hypertension associated with the use of amphotericin B: an appraisal on the reported cases. J Hypertens 24:1445
Rodrigues CA, Yamamoto M, Arantes Ade M, Chauffaille Mde L, Colombo AL, Bordin JO (2006) Amphotericin B-induced severe hypertension in a young patient: case reportand review of the literature. Ren Fail 28:185–187
Walker RW, Rosenblum MK (1992) Amphotericin B associated leukoencephalopathy. Neurology 42:2005–2010
Barton CH, Palh M, Vaziri ND, Cesario T (1984) Renal magnesium wasting associated with amphotericin B therapy. Am J Med 77:471–474
Lucas da Silva PS, Iglesias SB, Waisberg J (2007) Hypokalemic rhabdomyolysis in a child due to amphotericin B therapy. Eur J Pediatr 166:169–171
Sutherland SM, Hong DK, Balagtas J, Gutierrez K, Dvorak CC, Sarwal M (2008) Liposomal amphotericin b associated with severe hyperphosphatemia. Pediatr Infect Dis J 27:77–79
Olin JL, Spooner LM (2006) Amphotericin B-associated hyperbilirubinemia: case report and review of the literature. Pharmacotherapy 26:1011–1017
Bicanic T, Bottomley C, Loyse A et al (2015) Toxicity of Amphotericin B deoxycholate-based induction therapy in patients with HIV-associated cryptococcal meningitis. Antimicrob Agents Chemother 59:7224–7231
Day JN, Chau TT, Wolbers M et al (2013) Combination antifungal therapy for cryptococcal meningitis. N Engl J Med 368:1291–1302
Hamill RJ, Sobel JD, El-Sadr W et al (2010) Comparison of 2 doses of liposomal amphotericin B and conventional amphotericin B deoxycholate for treatment of AIDS associated acute cryptococcal meningitis: a randomized, double-blind clinical trial of efficacy and safety. Clin Infect Dis 51:225–2329
Wingard JR, Kubilis P, Lee L et al (1999) Clinical significance of nephrotoxicity in patients treated with amphotericin B for suspected or proven aspergillosis. Clin Infect Dis 29:1402–1407
White MH, Bowden RA, Sandler ES et al (1998) Randomized, double-blind clinical trial of amphotericin B colloidal dispersion vs. amphotericin B in the empirical treatment of fever and neutropenia. Clin Infect Dis 27:296–302
Lemke A, Kiderlen AF, Kayser O (2005) Amphotericin B. Appl Microbiol Biotechnol 68:151–162
Deray G (2002) Amphotericin B nephrotoxicity. J Antimicrob Chemoth 49(Suppl S1):37–41
Bicanic T, Wood R, Meintjes G et al (2008) High-dose amphotericin B with flucytosine for the treatment of cryptococcal meningitis in HIV-infected patients: a randomized trial. Clin Infect Dis 47:123–130
Llanos A, Cieza J, Bernardo J et al (1991) Effect of salt supplementation on amphotericin B nephrotoxicity. Kidney Int 40:302–308
Stein R, Alexander J (1989) Sodium protects against nephrotoxicity in patients receiving amphotericin B. Am J Med Sci 298:299–304
Girmenia C, Cimino G, Di Cristofano F, Micozzi A, Gentile G, Martino P (2005) Effects of hydration with salt repletion on renal toxicity of conventional amphotericin B empirical therapy: a prospective study in patients with hematological malignancies. Support Care Cancer 13:987–992
Bahr NC, Rolfes MA, Musubire A et al (2014) Standardized electrolyte supplementation and fluid management improves survival during amphotericin therapy for cryptococcal meningitis in resource-limited settings. Open Forum Infect Dis 1(2):ofu070. doi:10.1093/ofid/ofu070
Borro JM, Solé A, de la Torre M et al (2008) Efficiency and safety of inhaled amphotericin B lipid complex (Abelcet) in the prophylaxis of invasive fungal infections following lung transplantation. Transplant Proc 40:3090–3093
Rijnders BJ, Cornelissen JJ, Slobbe L et al (2008) Aerosolized liposomal amphotericin B for the prevention of invasive pulmonary aspergillosis during prolonged neutropenia: a randomized, placebo-controlled trial. Clin Infect Dis 46:1401–1408
Behre GF, Schwartz S, Lenz K et al (1995) Aerosol amphotericin B inhalations for prevention of invasive pulmonary aspergillosis in neutropenic cancer patients. Ann Hematol 71:287–291
Knechtel SA, Klepser ME (2007) Safety of aerosolized amphotericin B. Expert Opin Drug Saf 6:523–532
Andreucci M, Solomon R, Tasanarong A (2014) Side effects of radiographic contrast media: pathogenesis, risk factors, and prevention. Biomed Res Int 2014:741018
AmBisome (amphotericin B) liposome for injection, package insert. Astellas Pharma US, San Dimas, CA. Revised May 2012. https://www.astellas.us/docs/ambisome.pdf. Accessed 28 Oct 2016
Viread (Tenofovir disoproxil fumarate) Package Insert. Gilead Sciences, Inc., Foster City, CA. Revised Feb 2016. http://gilead.com/~/media/files/pdfs/medicines/liver-disease/viread/viread_pi.pdf. Accessed 23 Sept 2016
Retrovir (Zidovudine) Package Insert (2008) Glaxo SmithKline, Research Triangle Park, NC. http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/019910s033lbl.pdf. Accessed 23 Sept 2016
Baley JE, Meyers C, Kliegman RM, Jacobs MR, Blumer JL (1990) Pharmacokinetics, outcome of treatment, and toxic effects of amphotericin B and 5-fluorocytosine in neonates. J Pediatr 116:791–797
Benson JM, Nahata MC (1989) Pharmacokinetics of amphotericin B in children. Antimicrob Agents Chemother 33:1989–1993
Koren G, Lau A, Klein J et al (1988) Pharmacokinetics and adverse effects of amphotericin B in infants and children. J Pediatr 113:559–563
Nath CE, McLachlan AJ, Shaw PJ, Gunning R, Earl JW (2001) Population pharmacokinetics of amphotericin B in children with malignant diseases. Br J Clin Pharmacol 52:671–680
Starke JR, Mason EO Jr, Kramer WG, Kaplan SL (1987) Pharmacokinetics of amphotericin B in infants and children. J Infect Dis 155:766–774
Le J, Adler-Shohet FC, Nguyen C, Lieberman JM (2009) Nephrotoxicity associated with amphotericin B deoxycholate in neonates. Pediatr Infect Dis J 28:1061–1063
Van den Anker JN, van Popele NM, Sauer PJ (1995) Antifungal agents in neonatal systemic candidiasis. Antimicrob Agents Chemother 39:1391–1397
Steinbach WJ (2005) Antifungal agents in children. Pediatr Clin N Am 52:895–915
Federal Register (2008) 73:30832. https://www.gpo.gov/fdsys/pkg/FR-2008-05-29/pdf/E8-11806.pdf. Accessed 20 Sept 2016
Abelcet (amphotericin B lipid complex injection), package insert. Enzon Pharmaceuticals, Inc., Bridgewater, NJ. Revised October 2010. http://dailymed.nlm.nih.gov/dailymed/archives/fdaDrugInfo.cfm?archiveid=41233. Accessed 28 Oct 2016
Ismail MA, Lerner SA (1982) Disseminated blastomycosis in a pregnant woman: review of amphotericin B usage during pregnancy. Am Rev Respir Dis 126:350–353
McCoy MJ, Ellenberg JF, Killam AP (1980) Coccidioidomycosis complicating pregnancy. Am J Obstet Gynecol 137:739–740
Kuo D (1962) A case of torulosis of the central nervous system during pregnancy. Med J Aust 49:558–560
Silberfarb PM, Sarosi GA, Tosh FE (1972) Cryptococcosis and pregnancy. Am J Obstet Gynecol 112:714–720
Curole DN (1981) Cryptococcal meningitis in pregnancy. J Reprod Med 26:317–319
Harris RE (1966) Coccidioidomycosis complicating pregnancy. Report of 3 cases and review of the literature. Obstet Gynecol 28:401–405
Smale LE, Waechter KG (1970) Dissemination of coccidioidomycosis in pregnancy. Am J Obstet Gynecol 107(3):356–361
Hadsall FJ, Acquarelli MJ (1973) Disseminated coccidioidomycosis presenting as facial granulomas in pregnancy: a report of two cases and a review of the literature. Laryngoscope 83:51–58
Hager H, Welt SI, Cardasis JP, Alvarez S (1988) Disseminated blastomycosis in a pregnant woman successfully treated with amphotericin-B. A case report. J Reprod Med 33:485–488
Neiberg AD, Mavromatis F, Dyke J, Fayyad A (1977) Blastomyces dermatitidis treated during pregnancy: report of a case. Am J Obstet Gynecol 128:911–912
Philpot CR, Lo D (1972) Cryptococcal meningitis in pregnancy. Med J Aust 2:1005–1007
Aitken GW, Symonds EM (1962) Cryptococcal meningitis in pregnancy treated with amphotericin B. A case report. J Obstet Gynaecol Br Emp 69:677–679
Youssef D, Raval B, El-Abbassi A, Patel P (2013) Pulmonary blastomycosis during pregnancy: case report and review of the literature. Tenn Med 106:37–39
Nayak SU, Talwani R, Gilliam B, Taylor G, Ghosh M (2011) Cryptococcal meningitis in an HIV-positive pregnant woman. J Int Assoc Physicians AIDS Care (Chic) 10:79–82
Crum NF, Ballon-Landa G (2006) Coccidioidomycosis in pregnancy: case report and review of the literature. Am J Med 119:993.e11–993.e17
Ilett KF, Kristensen JH (2005) Drug use and breastfeeding. Expert Opin Drug Saf 4:745–768
Mueller M, Balasegaram M, Koummuki Y, Ritmeijer K, Santana MR, Davidson R (2006) A comparison of liposomal amphotericin B with sodium stibogluconate for the treatment of visceral leishmaniasis in pregnancy in Sudan. J Antimicrob Chemother 58:811–815
Pipitone MA, Gloster HM (2005) A case of blastomycosis in pregnancy. J Am Acad Dermatol 53:740–741
Dean JL, Wolf JE, Ranzini AC, Laughlin MA (1994) Use of amphotericin B during pregnancy: case report and review. Clin Infect Dis 18:364–368
Adler-Moore JP, Gangneux JP, Pappas PG (2016) Comparison between liposomal formulations of amphotericin B. Med Mycol 54:223–231
Olson JA, Adler-Moore JP, Jensen GM, Schwartz J, Dignani MC, Proffitt RT (2008) Comparison of the physicochemical, antifungal, and toxic properties of two liposomal Amphotericin B Products. Antimicrob Agents Chemother 52:259–268
Wingard JR, White MH, Anaissie E, Raffalli J, Goodman J, Arrieta A, L Amph/ABLC Collaborative Study Group (2000) A randomized, double-blind comparative trial evaluating the safety of liposomal amphotericin B versus amphotericin B lipid complex in the empirical treatment of febrile neutropenia. L Amph/ABLC Collaborative Study Group. Clin Infect Dis 31:1155–1163
Torrado JJ, Espada R, Ballesteros MP, Torrado-Santiago S (2008) Amphotericin B formulations and drug targeting. J Pharm Sci 97:2405–2425
Coukell AJ, Brogden RN (1998) Liposomal amphotericin B: therapeutic use in the management of fungal infections and visceral leishmaniasis. Drugs 55:585–612
Vogelsinger H, Weiler S, Djanani A et al (2006) Amphotericin B tissue distribution in autopsy material after treatment with liposomal amphotericin B and amphotericin B colloidal dispersion. Antimicrob Chemother 57:1153–1160
Perkins WR, Minchey SR, Boni LT et al (1992) Amphotericin B phospholipid interactions responsible for reduced mammalian cell toxicity. Biochim Biophys Acta 1107:271–282
Adler-Moore J (1994) AmBisome targeting to fungal infections. Bone Marrow Transplant 14(Suppl 5):S3–S7
Stone NR, Bicanic T, Salim R, Hope W (2016) Liposomal Amphotericin B (AmBisome(®)): a review of the pharmacokinetics, pharmacodynamics, clinical experience and future directions. Drugs 76:485–500
Latour JF, Fuhrmann C, Lagallarde C, Loreuil F (1996) Amphotericin B intralipid formulation: stability and particle size. J Antimicrob Chemother 37:1165–1169
Mehta J (1997) Do variations in molecular structure affect the clinical efficacy and safety of lipid-based amphotericin B preparations? Leuk Res 21:183–188
Boswell GW, Buell D, Bekersky I (1998) AmBisome (liposomal amphotericin B): a comparative review. J Clin Pharmacol 38:583–592
Bekersky I, Fielding RM, Dressler DE, Lee JW, Buell DN, Walsh TJ (2002) Pharmacokinetics, excretion, and mass balance of liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate in humans. Antimicrob Agents Chemother 46:828–833
Felton T, Troke PF, Hope WW (2014) Tissue penetration of antifungal agents. Clin Microbiol Rev 27:68–88
Wade RL, Chaudhari P, Natoli JL, Taylor RJ, Nathanson BH, Horn DL (2013) Nephrotoxicity and other adverse events among inpatients receiving liposomal amphotericin B or amphotericin B lipid complex. Diagn Microbiol Infect Dis 76:361–367
Ashley ESD, Lewis R, Lewis JS, Martin C, Andes D (2006) Pharmacology of systemic antifungal agents. Clin Infect Dis 43:S28–S39
Wong-Beringer A, Jacobs RA, Guglielmo BJ (1998) Lipid formulations of amphotericin B: clinical efficacy and toxicities. Clin Infect Dis 27:603–618
Groll AH, Piscitelli SC, Walsh TJ (1998) Clinical pharmacology of systemic antifungal agents: a comprehensive review of agents in clinical use, current investigational compounds, and putative targets for antifungal drug development. Adv Pharmacol 44:343–499
Groll AH, Giri N, Petraitis V et al (2000) Comparative efficacy and distribution of lipid formulations of amphotericin B in experimental Candida albicans infection of the central nervous system. J Infect Dis 182:274–282
Dupont B (2002) Overview of the lipid formulations of amphotericin B. J Antimicrob Chemother 49(Suppl 1):31–36
Kethireddy S, Andes D (2007) CNS pharmacokinetics of antifungal agents. Expert Opin Drug Metab Toxicol 3:573–581
Strenger V, Meinitzer A, Donnerer J et al (2014) Amphotericin B transfer to CSF following intravenous administration of liposomal amphotericin B. J Antimicrob Chemother 69:2522–2526
Ostrosky-Zeichner L, Marr KA, Rex JH, Cohen SH (2003) Amphotericin B: time for a new “gold standard”. Clin Infect Dis 37:415–425
Richard JH, Amphotericin B (2013) Formulations: a comparative review of efficacy and toxicity. Drugs 73:919–934
Montagna MT, Lovero G, Coretti C et al (2014) In vitro activities of amphotericin B deoxycholate and liposomal amphotericin B against 604 clinical yeast isolates. J Med Microbiol 63:1638–1643
Johnson EM, Ojwang JO, Szekely A, Wallace TL, Warnock DW (1998) Comparison of in vitro antifungal activities of free and liposome-encapsulated nystatin with those of four amphotericin B formulations. Antimicrob Agents Chemother 42:1412–1416
Carrillo-Muñoz AJ, Quindós G, Tur C et al (1999) In-vitro antifungal activity of liposomal nystatin in comparison with nystatin, amphotericin B cholesteryl sulphate, liposomal amphotericin B, amphotericin B lipid complex, amphotericin B desoxycholate, fluconazole and itraconazole. J Antimicrob Chemother 44:397–401
Clark JM, Whitney RR, Olsen SJ et al (1991) Amphotericin B lipid complex therapy of experimental fungal infections in mice. Antimicrob Agents Chemother 35:615–621
Hostetler JS, Clemons KV, Hanson LH, Stevens DA (1992) Efficacy and safety of amphotericin B colloidal dispersion compared with those of amphotericin B deoxycholate suspension for treatment of disseminated murine cryptococcosis. Antimicrob Agents Chemother 36:2656–2560
Pahls S, Schaffner A (1994) Comparison of the activity of free and liposomal amphotericin B in vitro and in a model of systemic and localized murine candidiasis. J Infect Dis 169:1057–1061
Clark AD, McKendrick S, Tansey PJ, Franklin IM, Chopra R (1998) A comparative analysis of lipid-complexed and liposomal amphotericin B preparations in haematological oncology. Br J Haematol 103:198–204
Enoch DA, Ludlam HA, Brown NM (2006) Invasive fungal infections: a review of epidemiology and management options. J Med Microbiol 55:809–818
Hiemenz JW, Walsh TJ (1996) Lipid formulations of amphotericin B: recent progress and future directions. Clin Infect Dis 22(Suppl 2):S133–S144
Mehta J, Kelsey S, Chu P et al (1997) Amphotericin B lipid complex (ABLC) for the treatment of confirmed or presumed fungal infections in immunocompromised patients with hematologic malignancies. Bone Marrow Transplant 20:39–43
Saliba F, Dupont B (2008) Renal impairment and amphotericin B formulations in patients with invasive fungal infections. Med Mycol 46:97–112
Sharkey PK, Graybill JR, Johnson ES et al (1996) Amphotericin B lipid complex compared with amphotericin B in the treatment of cryptococcal meningitis in patients with AIDS. Clin Infect Dis 22:315–321
Walsh TJ, Hiemenz JW, Seibel NL et al (1998) Amphotericin B lipid complex for invasive fungal infections: analysis of safety and efficacy in 556 cases. Clin Infect Dis 26:1383–1396
Walsh TJ, Finberg RW, Arndt C (1999) at al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med 340:764–771
Leenders AC, Daenen S, Jansen RL et al (1998) Liposomal amphotericin B compared with amphotericin B deoxycholate in the treatment of documented and suspected neutropenia-associated invasive fungal infections. Br J Haematol 103:205–212
Leenders AC, Reiss P, Portegies P et al (1997) Liposomal amphotericin B (AmBisome) compared with amphotericin B both followed by oral fluconazole in the treatment of AIDS-associated cryptococcal meningitis. AIDS 11:1463–1471
Johnson PC, Wheat LJ, Cloud GA, et al, U.S. National Institute of Allergy and Infectious Diseases Mycoses Study Group (2002) Safety and efficacy of liposomal amphotericin B compared with conventional amphotericin B for induction therapy of histoplasmosis in patients with AIDS. Ann Intern Med 137:105–109
Kauffman CA, Bustamante B, Chapman SW, Pappas PG, Infectious Diseases Society of America (2007) Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 45:1255–1265
Bergman SJ, Tyagi I, Ronald K (2010) Antifungal dosing in critically ill patients. Curr Fungal Infect Rep 4:78–86
Würthwein G, Groll AH, Hempel G, Adler-Shohet FC, Lieberman JM, Walsh TJ (2005) Population pharmacokinetics of amphotericin B lipid complex in neonates. Antimicrob Agents Chemother 49:5092–5098
Gallis HA, Drew RH, Pickard WW (1990) Amphotericin B: 30 years of clinical experience. Rev Infect Dis 12:308–329
Barrett JP, Vardulaki KA, Conlon C, et al., Amphotericin B Systematic Review Study Group (2003) A systematic review of the antifungal effectiveness and tolerability of amphotericin B formulations. Clin Ther 25:1295–1320
Martino R (2004) Efficacy, safety and cost-effectiveness of Amphotericin B Lipid Complex (ABLC): a review of the literature. Curr Med Res Opin 20:485–504
Ueda S, Miyamoto S, Kaida K et al (2016) Safety and efficacy of treatment with liposomal amphotericin B in elderly patients at least 65 years old with hematological diseases. J Infect Chemother 22:287–291
Roden MM, Nelson LD, Knudsen TA et al (2003) Triad of acute infusion-related reactions associated with liposomal amphotericin B: analysis of clinical and epidemiological characteristics. Clin Infect Dis 36:1213–1220
Rex JH, Stevens DA (2015) Drugs active against fungi, pneumocystis and microsporidia. In: Mandell, Douglas, Bennett’s principles and practice of infectious diseases, 8th edn. Elsevier Saunders, Philadelphia, PA, pp 485–490
Peyton LR, Gallagher S, Hashemzadeh M (2015) Triazole antifungals: a review. Drugs Today 51:705–718
National Center for Biotechnology Information. PubChem Compound Database; CID:55283. https://pubchem.ncbi.nlm.nih.gov/compound/itraconazole. Accessed 29 Jan 2017
National Center for Biotechnology Information. PubChem Compound Database; CID:3365. https://pubchem.ncbi.nlm.nih.gov/compound/fluconazole. Accessed 29 Jan 2017
National Center for Biotechnology Information. PubChem Compound Database; CID: 468595. https://pubchem.ncbi.nlm.nih.gov/compound/posaconazole. Accessed 29 Jan 2017
National Center for Biotechnology Information. PubChem Compound Database; CID:71616. https://pubchem.ncbi.nlm.nih.gov/compound/voriconazole. Accessed 29 Jan 2017
National Center for Biotechnology Information. PubChem Compound Database; CID: 6918485. https://pubchem.ncbi.nlm.nih.gov/compound/isavuconazole. Accessed 29 Jan 2017
Mast N, Zheng W, Stout CD, Pikuleva IA (2013) Antifungal azoles: structural insights into undesired tight binding to cholesterol-metabolizing CYP46A1. Mol Pharmacol 84:86–94
Shyadehi AZ, Lamb DC, Kelly SL et al (1996) The mechanism of the acyl-carbon bond cleavage reaction catalyzed by recombinant sterol 14 alpha-demethylase of Candida albicans (other names are: lanosterol 14 alpha-demethylase, P-45014DM, and CYP51). J Biol Chem 271:12445–12450
Rybak JM, Marx KR, Nishimoto AT, Rogers PD (2015) Isavuconazole: pharmacology pharmacodynamics, and current clinical experience with a new triazole antifungal agent. Pharmacotherapy 35:1037–1051
Courtney R, Wexler D, Radwanski E, Lim J, Laughlin M (2004) Effect of food on the relative bioavailability of two oral formulations of posaconazole in healthy adults. Br J Clin Pharmacol 57:218–222
Dekkers BG, Bakker M, van der Elst KC et al (2016) Therapeutic drug monitoring of posaconazole: an update. Curr Fungal Infect Rep 10:51–61
Moriyama B, Kadri K, Henning SA, Danner RL, Penzak SR, Walsh TJ (2015) Therapeutic drug monitoring and genotypic screening in the clinical use of voriconazole. Curr Fungal Infect Rep 9:74–87
Pascual A, Calandra T, Bolay S, Buclin T, Blle J, Marchetti O (2008) Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis 46:201–211
Brüggemann RJ, Aarnoutse RE (2015) Fundament and prerequisites for the application of an antifungal TDM service. Curr Fungal Infect Rep 9:122–129
Ashbee HR, Barnes RA, Johnson EM, Richardson MD, Gorton R, Hope WW (2014) Therapeutic drug monitoring (TDM) of antifungal agents: guidelines from the British Society for Medical Mycology. J Antimicrob Chemother 69:1162–1176
Wiederhold NP, Pennick GJ, Dorsey SA et al (2014) A reference laboratory experience of clinically achievable voriconazole, posaconazole, and itraconazole concentrations within the bloodstream and cerebral spinal fluid. Antimicrob Agents Chemother 58:424–431
Nagappan V, Deresinski S (2007) Reviews of anti-infective agents. Posaconazole: a broad-spectrum triazole antifungal agent. Clin Infect Dis 45:1610–1617
Thompson GR 3rd, Rendon A, Dos Santos RR et al (2016) Isavuconazole treatment of cryptococcosis and dimorphic mycoses. Clin Infect Dis 63:356–362
Parker JE, Warrilow AG, Price CL, Mullins JG, Kelly DE, Kelly SL (2014) Resistance to antifungals that target CYP51. J Chem Biol 7:143–161
Cuenca-Estrella M (2014) Antifungal drug resistance mechanisms in pathogenic fungi: from bench to bedside. Clin Microbiol Infect 20(Suppl 6):54–59
Alastruey-Izquierdo A, Melhem MS, Bonfietti LX, Rodriguez-Tudela JL (2015) Susceptibility test for fungi: clinical and laboratorial correlations in medical mycology. Rev Inst Med Trop Sao Paulo 57(Suppl 19):57–64
Wilson DT, Dimondi VP, Johnson SW, Jones TM, Drew RH (2016) Role of isavuconazole in the treatment of invasive fungal infections. Ther Clin Risk Manag 12:1197–1206
Barr VO, Zdyb EG, Postelnick M (2015) The clinical significance of azole antifungals’ effects on the liver and transaminase levels. Curr Fungal Infect Rep 9:190–195
Feist A, Lee R, Osborne S, Lane J, Yung G (2012) Increased incidence of cutaneous squamous cell carcinoma in lung transplant recipients taking long-term voriconazole. J Heart Lung Transplant 31:1177–1181
Zwald FO, Spratt M, Lemos BD et al (2012) Duration of voriconazole exposure: an independent risk factor for skin cancer after lung transplantation. Dermatol Surg 38:1369–1374
Nix DE (2014) Cardiotoxicity induced by antifungal drugs. Curr Fungal Infect Rep 8:129–138
Panos G, Velissaris D, Karamouzos V, Matzaroglou C, Tyllianakis M (2016) Long QT syndrome leading to multiple cardiac arrests after posaconazole administration in an immune-compromised patient with sepsis: an unusual case report. Am J Case Reports 17:295–300
Brüggemann RJM, Alffenaar JC, Blijlevens NMA et al (2009) Clinical relevance of the pharmacokinetic interactions of azole antifungal drugs with other coadministered agents. Clin Infect Dis 48:1441–1458
Gubbins PO, Heldenbrand S (2009) Clinically relevant drug interactions of current antifungal agents. Mycoses 53:95–113
Miceli MH, Kauffman CA (2015) Isavuconazole: a new broad-spectrum triazole antifungal agent. Clin Infect Dis 61:1558–1565
Vadlapatla RK, Patel M, Paturi DK, Pal D, Mitra AK (2014) Clinically relevant drug-drug interactions between antiretrovirals and antifungals. Expert Opin Drug Metab Toxicol 10:561–580
Nivoix Y, Levêque D, Herbrecht R, Koffel JC, Beretz L, Ubeaud-Sequier G (2008) The enzymatic basis of drug-drug interactions with systemic triazole antifungals. Clin Pharmacokinet 47:779–792
Lempers VJC, Martial LC, Schreuder MF et al (2015) Drug-interactions of azole antifungals with selected immunosuppressants in transplant patients: strategies for optimal management in clinical practice. Curr Op Pharmacol 24:38–44
Hohmann C, Kang EM, Jancel T (2010) Rifampin and posaconazole coadministration leads to decreased serum posaconazole concentrations. Clin Infect Dis 50:939–940
Autmizguine J, Guptill JT, Cohen-Wolkowiez M, Benjamin DK Jr, Capparelli EV (2014) Pharmacokinetics and pharmacodynamics of antifungals in children: clinical implications. Drugs 74:891–909
Ramos-Martín V, O'Connor O, Hope W (2015) Clinical pharmacology of antifungal agents in pediatrics: children are not small adults. Curr Opin Pharmacol 24:128–134
Goldman JM, Abdel-Rahman SM (2016) Pharmacokinetic considerations in treating invasive pediatric fungal infections. Exp Op Drug Metabol Toxicol 12:645–655
Drogouti E, Pana ZD, Tragiannidis A, Hempel G, Groll A (2015) Clinical pharmacology of itraconazole in children and adolescents. Curr Fungal Infect Rep 9:65–73
Dokos C, Pieper S, Lehrnbecher T, Groll AH (2012) Pharmacokinetics, safety and efficacy of voriconazole in pediatric patients: an update. Curr Fungal Infect Rep 6:121–126
Pilmis B, Jullien V, Sobel J, Lecuit M, Lortholary O, Charlier C (2015) Antifungal drugs during pregnancy: an updated review. J Antimicrob Chemother 70:14–22
Nair AS (2014) Safety of intravenous voriconazole in renal failure. Med J DY Patil Univ 7:105–107
Payne KD, Hall RG (2016) Dosing of antifungal agents in obese people. Expert Rev Anti-Infect Ther 14:257–267
Kullberg BJ, Arendrup MC (2015) Invasive candidiasis. N Engl J Med 373:1445–1456
Wang JF, Xue Y, Zhu XB, Fan H (2015) Efficacy and safety of echinocandins versus triazoles for the prophylaxis and treatment of fungal infections: a meta-analysis of RCTs. Eur J Clin Microbiol Infect Dis 34:651–659
Pappas PG, Kauffman CA, Andes D, et al, Infectious Diseases Society of America (2009) Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 48:503–535
Andes DR, Safdar N, Baddley JW,et al, Mycoses Study Group (2012) Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clin Infect Dis 54:1110–1122
Denning DW, Ribaud P, Milpied N et al (2002) Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin Infect Dis 34:563–571
Herbrecht R, Denning DW, Patterson TF, et al, Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group (2002) Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 347:408–415
Perfect JR, Marr KA, Walsh TJ et al (2003) Voriconazole treatment for less-common, emerging, or refractory fungal infections. Clin Infect Dis 36:1122–1131
Patterson TF, Boucher HW, Herbrecht R,et al, European Organization for Research and Treatment of Cancer (EORTC) Invasive Fungal Infections Group (IFIG); Pfizer Global Aspergillus Study Group (2005) Strategy of following voriconazole versus amphotericin B therapy with other licensed antifungal therapy for primary treatment of invasive aspergillosis: impact of other therapies on outcome. Clin Infect Dis 41:1448–1452
Singh N, Limaye AP, Forrest G et al (2006) Combination of voriconazole and caspofungin as primary therapy for invasive aspergillosis in solid organ transplant recipients: a prospective, multicenter, observational study. Transplantation 81:320–326
Panackal AA, Parisini E, Proschan M (2014) Salvage combination antifungal therapy for acute invasive aspergillosis may improve outcomes: a systematic review and meta-analysis. Int J Infect Dis 28:80–94
Marr KA, Schlamm HT, Herbrecht R et al (2015) Combination antifungal therapy for invasive aspergillosis: a randomized trial. Ann Intern Med 162:81–89
Panackal AA (2016) Combination antifungal therapy for invasive aspergillosis revisited. Med Mycol Open Access 2(2). pii: 12
Ullmann AJ, Cornely OA, Burchardt A et al (2006) Pharmacokinetics, safety, and efficacy of posaconazole in patients with persistent febrile neutropenia or refractory invasive fungal infection. Antimicrob Agents Chemother 50:658–666
Krishna G, Moton A, Ma L, Medlock MM, McLeod J (2009) Pharmacokinetics and absorption of posaconazole oral suspension under various gastric conditions in healthy volunteers. Antimicrob Agents Chemother 53:958–966
Zoller E, Valente C, Baker K, Klepser ME (2010) Development, clinical utility, and place in therapy of posaconazole for prevention and treatment of invasive fungal infections. Drug Des Devel Ther 4:299–311
Percival KM, Bergman SJ (2014) Update on posaconazole pharmacokinetics: comparison of old and new formulations. Curr Fungal Infect Rep 8:139–145
Wiederhold NP (2015) Pharmacokinetics and safety of posaconazole delayed-release tablets for invasive fungal infections. Clin Pharmacol 8:1–8
Cornely OA, Maertens J, Winston DJ et al (2007) Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med 356:348–359
Bertz H, Drognitz K, Lübbert M (2014) No difference between posaconazole and fluconazole antifungal prophylaxis and mycological diagnostics except costs in patients undergoing AML chemotherapy: a 1-year “real-life” evaluation. Ann Hematol 93:165–167
Walsh TJ, Raad I, Patterson TF et al (2007) Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis 44:2–12
ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT01782131?term=posaconazole+aspergillosis&rank=1. Accessed 17 Nov 2016
Greenberg RN, Mullane K, van Burik JA et al (2006) Posaconazole as salvage therapy for zygomycosis. Antimicrob Agents Chemother 50:126–133
Chitasombat MN, Kontoyiannis DP (2016) Treatment of mucormycosis in transplant patients: role of surgery and of old and new antifungal agents. Curr Opin Infect Dis 29:340–345
Durani U, Tosh PK, Barreto JN, Estes LL, Jannetto PJ, Tande AJ (2015) Retrospective comparison of posaconazole levels in patients taking the delayed-release tablet versus the oral suspension. Antimicrob Agents Chemother 59:4914–4918
Riley TT, Muzny CA, Swiatlo E, Legendre DP (2016) Breaking the mold: a review of mucormycosis and current pharmacological treatment options. Ann Pharmacother 50:747–757
Maertens JA, Raad II, Marr KA et al (2016) Isavuconazole versus voriconazole for primary treatment of invasive mould disease caused by Aspergillus and other filamentous fungi (SECURE): a phase 3, randomised-controlled, non-inferiority trial. Lancet 387:760–769
Falci DR, Pasqualotto AC (2013) Profile of isavuconazole and its potential in the treatment of severe invasive fungal infections. Infect Drug Resist 6:163–174
Carrillo-Muñoz AJ, Giusiano G, Arechavala A et al (2015) Clinical usefulness of triazole derivatives in the management of fungal infections. Rev Esp Quimioter 28:169–182
Gupta AK, Leonardi C, Stolz RR, Pierce PF, Conetta B, Ravuconazole Onychomycosis Group (2005) A phase I/II randomized, double-blind, placebo controlled, dose-ranging study evaluating the efficacy, safety and pharmacokinetics of ravuconazole in the treatment of onychomycosis. J Eur Acad Dermatol Venereal 19:437–443
Jo Siu WJ, Tatsumi Y, Senda H et al (2013) Comparison of in vitro antifungal activities of efinaconazole and currently available antifungal agents against a variety of pathogenic fungi associated with onychomycosis. Antimicrob Agents Chemother 57:1610–1616
Hector RF (1993) Compounds active against cell walls of medically important fungi. Clin Microbiol Rev 6:1
Debono M, Gordee RS (1994) Antibiotics that inhibit fungal cell wall development. Annu Rev Microbiol 48:471
Denning DW (2003) Echinocandin antifungal drugs. Lancet 362:1142
Lewis RE. Pharmacology of echinocandins. Up to date. Literature review current through: May 2016. This topic last updated: Feb 05, 2016
National Center for Biotechnology Information. PubChem Compound Database; CID: 2826718. https://pubchem.ncbi.nlm.nih.gov/compound/caspofungin. Accessed 29 Jan 2017
National Center for Biotechnology Information. PubChem Compound Database; CID: 477468. https://pubchem.ncbi.nlm.nih.gov/compound/micafungin. Accessed 29 Jan 2017
National Center for Biotechnology Information. PubChem Compound Database; CID: 166548. https://pubchem.ncbi.nlm.nih.gov/compound/anidulafungin. Accessed 29 Jan 2017
Fleet GH (1985) Composition and structure of yeast cell walls. Curr Top Med Mycol 1:24
Bowman JC, Hicks PS, Kurtz MB et al (2002) The antifungal echinocandin caspofungin acetate kills growing cells of Aspergillus fumigatus in vitro. Antimicrob Agents Chemother 46(9):3001–3012
Marr KA, Boeckh M, Carter RA et al (2004) Combination antifungal therapy for invasive aspergillosis. Clin Infect Dis 39(6):797–802
Lamaris GA, Lewis RE, Chamilos G et al (2008) Caspofungin-mediated beta-glucan unmasking and enhancement of human polymorphonuclear neutrophil activity against Aspergillus and non-Aspergillus hyphae. J Infect Dis 198:186
Eschenauer G, Depestel DD, Carver PL (2007) Comparison of echinocandin antifungals. Ther Clin Risk Manag 3(1):71–97
Kauffman CA, Carver PL (2008) Update on echinocandin antifungals. Semin Respir Crit Care Med 29(2):211–219
Dodds Ashley ES, Lewis R, Lewis JS, Martin C, Andes D (2006) Pharmacology of systemic antifungal agents. Clin Infect Dis 43(S1):S28–S39
Sucher AJ, Chahine EB, Balcer HE (2009) Echinocandins: the newest class of antifungals. Ann Pharmacother 43:1647–1657
Azanza Perea JR (2016) Echinocandins: applied pharmacology. Rev Iberoam Micol 33(3):140–144
Theuretzbacher U (2004) Pharmacokinetics/pharmacodynamics of echinocandins. Eur J Clin Microbiol Infect Dis 23:805
Cappelletty D, Eiselstein-McKitrick K (2007) The echinocandins. Pharmacotherapy 27:369
Pfaller MA, Boyken L, Hollis RJ et al (2008) In vitro susceptibility of invasive isolates of Candida spp. to anidulafungin, caspofungin, and micafungin: six years of global surveillance. J Clin Microbiol 46:150
Barchiesi F, Spreghini E, Tomassetti S et al (2006) Effects of caspofungin against Candida guilliermondii and Candida parapsilosis. Antimicrob Agents Chemother 50(8):2719–2727
Espinel-Ingroff A (1998) Comparison of in vitro activities of the new triazole Sch56592 and the echinocandins mk-0991 (l-743,872) and ly303366 against opportunistic filamentous and dimorphic fungi and yeasts. J Clin Microbiol 36(10):2950–2956
Nakai T, Uno J, Otomo K et al (2002) In vitro activity of FK463, a novel lipopeptide antifungal agent, against a variety of clinically important molds. Chemotherapy 48(2):78–81
Messer SA, Kirby JT, Sader HS et al (2004) Initial results from a longitudinal international surveillance programme for anidulafungin (2003). J Antimicrob Chemother 54(6):1051–1056
Kirkpatrick WR, Perea S, Coco BJ et al (2002) Efficacy of caspofungin alone and in combination with voriconazole in a guinea pig model of invasive aspergillosis. Antimicrob Agents Chemother 46(8):2564–2568
Diekema DJ, Messer SA, Hollis RJ et al (2003) Activities of caspofungin, itraconazole, posaconazole, ravuconazole, voriconazole, and amphotericin B against 448 recent clinical isolates of filamentous fungi. J Clin Microbiol 41(8):3623–3626
Almyroudis NG, Sutton DA, Fothergill AW et al (2007) In vitro susceptibilities of 217 clinical isolates of zygomycetes to conventional and new antifungal agents. Antimicrob Agents Chemother 51(7):2587–2590
Cuenca-Estrella M, Ruiz-Diez B, Martinez-Suarez JV et al (1999) Comparative in-vitro activity of voriconazole (UK-109,496) and six other antifungal agents against clinical isolates of Scedosporium prolificans and Scedosporium apiospermum. J Antimicrob Chemother 43(1):149–151
Tawara S, Ikeda F, Maki K et al (2000) In vitro activities of a new lipopeptide antifungal agent, FK463, against a variety of clinically important fungi. Antimicrob Agents Chemother 44:57
Kahn JN, Hsu MJ, Racine F et al (2006) Caspofungin susceptibility in Aspergillus and non-Aspergillus molds: inhibition of glucan synthase and reduction of beta-D-1,3 glucan levels in culture. Antimicrob Agents Chemother 50:2214
Ito M, Nozu R, Kuramochi T et al (2000) Prophylactic effect of FK463, a novel antifungal lipopeptide, against Pneumocystis carinii infection in mice. Antimicrob Agents Chemother 44:2259
Schmatz DM, Powles M, McFadden DC et al (1991) Treatment and prevention of Pneumocystis carinii pneumonia and further elucidation of the P. carinii life cycle with 1,3-beta-glucan synthesis inhibitor L-671,329. J Protozool 38:151S
Ramage G, VandeWalle K, Bachmann SP et al (2002) In vitro pharmacodynamic properties of three antifungal agents against preformed Candida albicans biofilms determined by time-kill studies. Antimicrob Agents Chemother 46:3634
Kuhn DM, George T, Chandra J et al (2002) Antifungal susceptibility of Candida biofilms: unique efficacy of amphotericin B lipid formulations and echinocandins. Antimicrob Agents Chemother 46:1773
Marcos-Zambrano LJ, Escribano P, Bouza E, Guinea J (2016) Comparison of the antifungal activity of micafungin and amphotericin B against Candida tropicalis biofilms. J Antimicrob Chemother 71(9):2498–2501
Pham CD, Iqbal N, Bolden CB et al (2014) Role of FKS Mutations in Candida glabrata: MIC values, echinocandin resistance, and multidrug resistance. Antimicrob Agents Chemother 58:4690
Perlin DS, Shor E, Zhao Y (2015) Update on antifungal drug resistance. Curr Clin Microbiol Rep 2(2):84–95
Zimbeck AJ, Iqbal N, Ahlquist AM et al (2010) FKS mutations and elevated echinocandin MIC values among Candida glabrata isolates from U.S. population-based surveillance. Antimicrob Agents Chemother 54:5042
Kofteridis DP, Lewis RE, Kontoyiannis DP (2010) Caspofungin-non-susceptible Candida isolates in cancer patients. J Antimicrob Chemother 65:293
Alexander BD, Johnson MD, Pfeiffer CD et al (2013) Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis 56:1724
Pfaller MA, Castanheira M, Lockhart SR et al (2012) Frequency of decreased susceptibility and resistance to echinocandins among fluconazole-resistant bloodstream isolates of Candida glabrata. J Clin Microbiol 50(4):1199–1203
Naicker SD, Magobo RE, Zulu TG et al (2016) Two echinocandin-resistant Candida glabrata FKS mutants from South Africa. Med Mycol Case Rep 11:24–26
Tan TY, Hsu LY, Alejandria MM et al (2016) Antifungal susceptibility of invasive Candida bloodstream isolates from the Asia-Pacific region. Med Mycol 54(5):471–477
Beyda ND, John J, Kilic A et al (2014) FKS mutant Candida glabrata: risk factors and outcomes in patients with candidemia. Clin Infect Dis 59:819
Wang E, Farmakiotis D, Yang D et al (2015) The ever-evolving landscape of candidaemia in patients with acute leukaemia: non-susceptibility to caspofungin and multidrug resistance are associated with increased mortality. J Antimicrob Chemother 70:2362
Imbert S, Castain L, Pons A et al (2016) Discontinuation of echinocandin and azole treatments led to the disappearance of an FKS alteration but not azole resistance during clonal Candida glabrata persistent candidemia. Clin Microbiol Infect 22(10):891
van Burik JA, Ratanatharathorn V, Stepan DE et al (2004) Micafungin versus fluconazole for prophylaxis against invasive fungal infections during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis 39(10):1407–1416
Walsh TJ, Teppler H, Donowitz GR et al (2004) Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N Engl J Med 351(14):1391–1402
Reboli AC, Rotstein C, Pappas PG et al (2007) Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med 356(24):2472–2482
Mora-Duarte J, Betts R, Rotstein C et al (2002) Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med 347(25):2020–2029
Villanueva A, Gotuzzo E, Arathoon EG et al (2002) A randomized double-blind study of caspofungin versus fluconazole for the treatment of esophageal candidiasis. Am J Med 113(4):294–299
de Wet NT, Bester AJ, Viljoen JJ et al (2005) A randomized, double blind, comparative trial of micafungin (FK463) vs. fluconazole for the treatment of oesophageal candidiasis. Aliment Pharmacol Ther 21(7):899–907
de Wet N, Llanos-Cuentas A, Suleiman J et al (2004) A randomized, double-blind, parallel-group, dose-response study of micafungin compared with fluconazole for the treatment of esophageal candidiasis in HIV-positive patients. Clin Infect Dis 39(6):842–849
Villanueva A, Arathoon EG, Gotuzzo E et al (2001) A randomized double-blind study of caspofungin versus amphotericin for the treatment of Candidal esophagitis. Clin Infect Dis 33(9):1529–1535
Krause DS, Simjee AE, van Rensburg C et al (2004) A randomized, double-blind trial of anidulafungin versus fluconazole for the treatment of esophageal candidiasis. Clin Infect Dis 39(6):770–775
Arathoon EG, Gotuzzo E, Noriega LM et al (2002) Randomized, double-blind, multicenter study of caspofungin versus amphotericin B for treatment of oropharyngeal and esophageal candidiases. Antimicrob Agents Chemother 46(2):451–457
Aliff TB, Maslak PG, Jurcic JG et al (2003) Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer 97(4):1025–1032
Maertens J, Raad I, Petrikkos G et al (2004) Efficacy and safety of caspofungin for treatment of invasive aspergillosis in patients refractory to or intolerant of conventional antifungal therapy. Clin Infect Dis 39(11):1563–1571
Maertens J, Glasmacher A, Herbrecht R et al (2006) Multicenter, noncomparative study of caspofungin in combination with other antifungals as salvage therapy in adults with invasive aspergillosis. Cancer 107(12):2888–2897
Kontoyiannis DP, Hachem R, Lewis RE et al (2003) Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer 98(2):292–299
Grau S, Luque S, Echeverría-Esnal D et al (2016) Urinary micafungin levels are sufficient to treat urinary tract infections caused by Candida spp. Int J Antimicrob Agents 48(2):212–214
Cancidas (caspofungin acetate for injection). Highlights of prescribing information, revised April 2016. www.merck.com/product/usa/pi_circulars/c/cancidas/cancidas_pi.pdf. Accessed 15 Jan 2017
Mycamine (micafungin sodium for injection). Highlights of prescribing information, revised August 2016. www.astellas.us/docs/mycamine.pdf. Accessed 15 Jan 2017
Eraxis (Anidulafungin for injection). Highlights of prescribing information, revised July 2012. www.accessdata.fda.gov/drugsatfda_docs/label/2012/021632s011lbl.pdf. Accessed 15 Jan 2017
Lehrnbecher T, Groll AH (2010) Micafungin: a brief review of pharmacology, safety, and antifungal efficacy in pediatric patients. Pediatr Blood Cancer 55:229
Ryan DM, Lupinacci RJ, Kartsonis NA (2011) Efficacy and safety of caspofungin in obese patients. Med Mycol 49:748
Krishnan BR, James KD, Polowy K et al (2017) CD101, a novel echinocandin with exceptional stability properties and enhanced aqueous solubility. J Antibiot (Tokyo) 70(2):130–135
National Center for Biotechnology Information. PubChem Compound Database; CID: 3366. https://pubchem.ncbi.nlm.nih.gov/compound/flucytosine. Accessed 29 Jan 2017
Vermes A, Guchelaar HJ, Dankert J (2000) Flucytosine: a review of its pharmacology, clinical indications, pharmacokinetics, toxicity and drug interactions. J Antimicrob Chemother 46:171–179
Onishi J, Meinz M, Thompson J et al (2000) Discovery of novel antifungal (1,3)-beta-D-glucan synthase inhibitors. Antimicrob Agents Chemother 44:368–377
Cutler RE, Blair AD, Kelly MR (1978) Flucytosine kinetics in subjects with normal and impaired renal function. Clin Pharmacol Ther 24:333–342
Wade DN, Sudlow G (1972) The kinetics of 5-fluorocytosine elimination in man. Aust NZ J Med 2:153–158
Schönebeck J, Polak A, Fernex M, Scholer HJ (1973) Pharmacokinetic studies on the oral antimycotic agent 5-fluorocytosine in individuals with normal and impaired kidney function. Chemotherapy 18:321–336
Drouhet E, Babinet Chapusot JP, Kleinknecht D (1973) 5-fluorocytosine in the treatment of candidiasis with acute renal insufficiency. Biomedicine 19:408–414
Peman J, Canton E, Espinel-Ingroff A (2009) Antifungal drug resistance mechanisms. Expert Rev Anti-Infect Ther 7:453–460
Espinel-Ingroff A (2008) Mechanisms of resistance to antifungal agents: yeasts and filamentous fungi. Rev Iberoam Micol 25:101–106
Chapeland-Leclerc F, Bouchoux J, Goumar A, Chastin C, Villard J, Noel T (2005) Inactivation of the FCY2 gene encoding purine-cytosine permease promotes cross-resistance to flucytosine and fluconazole in Candida lusitaniae. Antimicrob Agents Chemother 49:3101–3108
Vandeputte P, Pineau L, Larcher G, Noel T, Brèthes D, Chabasse D, Bouchara JP (2011) Molecular mechanisms of resistance to 5-fluorocytosine in laboratory mutants of Candida glabrata. Mycopathologia 171:11–21
Kontoyiannis DP, Lewis RE (2002) Antifungal drug resistance of pathogenic fungi. Lancet 359:1135–1144
Costa C, Ponte A, Pais P et al (2015) New mechanisms of flucytosine resistance in C. glabrata unveiled by a chemogenomics analysis in S. cerevisiae. PLoS One 10:e0135110
Chowdhary A, Meis JF, Guarro J,et al, European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology (2014) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of systemic phaeohyphomycosis: diseases caused by black fungi. Clin Microbiol Infect 20(Suppl 3):47–75
Kauffman CA, Frame PT (1977) Bone marrow toxicity associated with 5-fluorocytosine therapy. Antimicrob Agents Chemother 11:244–247
Wise GJ, Goldberg P, Kozinn PJ, Nawabi IU (1976) Agranulocytosis associated with flucytosine for urinary candidiasis. Urology 8:490–491
Stamm AM, Diasio RB, Dismukes WE et al (1987) Toxicity of amphotericin B plus flucytosine in 194 patients with cryptococcal meningitis. Am J Med 83:236–242
Bennett JE, Dismukes WE, Duma RJ et al (1979) A comparison of amphotericin B alone and combined with flucytosine in the treatment of cryptococcal meningitis. N Engl J Med 301:26–131
White CA, Traube J (1982) Ulcerating enteritis associated with flucytosine therapy. Gastroenterology 83:1127–1129
Harder EJ, Hermans PE (1975) Treatment of fungal infections with flucytosine. Arch Intern Med 135:231–237
Vermes A, van der Sijs IH, Guchelaar HJ (2000) Flucytosine: correlation between toxicity and pharmacokinetic parameters. Chemotherapy 46:86–94
Vermes A, Mathot RAA, van der Sijs IH, Dankert J, Guchelaar HJ (2000) Population pharmacokinetics of flucytosine: comparison and validation of three models using STS, NPEM, and NONMEM. Ther Drug Monit 22:676–687
Fond B, Bentata-Pessayre M, Krivitzky A, Callard P, Dupont B, Delzant G (1983) Iatrogenic colitis during flucytosine treatment for neuromeningeal cryptococcosis. Sem Hop 59:1187
Sohail MA, Ikram U (2014) Flucytosine-induced colitis. BMJ Case Rep. pii: bcr2013203381. doi:10.1136/bcr-2013-203381
Cappell MS (2004) Colonic toxicity of administered drugs and chemicals. Am J Gastroenterol 99:1175–1190
Folk A, Cotoraci C, Balta C et al (2016) Evaluation of hepatotoxicity with treatment doses of flucytosine and amphotericin B for invasive fungal infections. Biomed Res Int 5398730
Holt RJ (1978) Clinical problems with 5-fluorocytosine. Mykosen 21:363–369
Richardson MD, Warnock DW (2003) Fungal infection: diagnosis and management, 3rd edn. Blackwell, Oxford, pp 66–69
Kunka ME, Cady EA, Woo HC, Thompson Bastin ML (2015) Flucytosine pharmacokinetics in a critically ill patient receiving continuous renal replacement therapy. Case Rep Crit Care 2015:927496
Richardson MD, Jones BL (2003) Therapeutic guidelines in systemic fungal infection, 3rd edn. Current Medical Literature, London. Publication link: ca9d0625-7a45-49c0-a3e1-41c6fd17e3c3, pp 53–55
Kuang D, Ronco C (2007) Adjustment of antimicrobial regimen in critically ill patients undergoing continuous renal replacement therapy. In: J-L Vincent (ed) Yearbook of intensive care and emergency medicine, pp 592–606
Stafford CR, Fisher JF, Fadel HE, Espinel-Ingroff AV, Shadomy S, Hamby M (1983) Cryptococcal meningitis in pregnancy. Obstet Gynecol 62:35S–37S
Njoku JC, Gumeel D, Hermsen ED (2010) Antifungal therapy in pregnancy and breastfeeding. Curr Fungal Infect Rep 4:62–69
National Center for Biotechnology Information. PubChem Compound Database; CID: 1549008. https://pubchem.ncbi.nlm.nih.gov/compound/terbinafine. Accessed 29 Jan 2017
Petranyi G, Ryder NS, Stütz A (1984) Allylamine derivatives: new class of synthetic antifungal agents inhibiting fungal squalene epoxidase. Science 224:1239–1419
Ryder NS (1992) Terbinafine: mode of action and properties of the squalene epoxidase inhibition. Br J Dermatol 126(Suppl 39):2–7
Hosseini-Yeganeh M, McLachlan AJ (2001) Tissue distribution of terbinafine in rats. J Pharm Sci 90:1817–1828
Hosseini-Yeganeh M, McLachlan AJ (2002) Physiologically based pharmacokinetic model for terbinafine in rats and humans. Antimicrob Agents Chemother 46:2219–2228
Leyden J (1998) Pharmacokinetics and pharmacology of terbinafine and itraconazole. J Am Acad Dermatol 38:S42–S47
Faergemann J, Zehender H, Jones T, Maibach HI (1990) Terbinafine levels in serum, stratum corneum, dermis epidermis (without stratum corneum), hair, sebum, and sweat. Acta Derm Venereol (Stockh) 71:322–326
Faergemann J, Zehender H, Denouël J, Millerioux L (1993) Levels of terbinafine in plasma, stratum corneum, dermis-epidermis (without stratum corneum), sebum, hair and nails during and after 250 mg terbinafine orally once per day for four weeks. Acta Derm Venereol 73:305–309
Kovarik JM, Kirkesseli S, Humbert H et al (1992) Dose-proportional pharmacokinetics of terbinafine and its A-demethylated metabolite in healthy volunteers. Br J Dermatol 126(Suppl 39):8–13
De Doncker P (1997) Pharmacokinetics of oral antifungal agents. Dermatol Ther 3:46–57
Villars V, Jones TC (1990) Present status of the efficacy and tolerability of terbinafine (Lamisil) used systemically in the treatment of dermatomycoses of skin and nails. J Dermatol Treat 1(Suppl. 2):33–38
Jensen JC (1990) Pharmacokinetics of Lamisil in humans. J Dermatol Treat 1(Suppl 2):15–18
Zehender H, Cabiac MD, Denouei J et al (1994) Elimination kinetics of terbinafine from human plasma and tissues following multiple-dose administration, and comparison with 3 main metabolites. Drug Invest 8:203–210
Debruyne D, Coquerel A (2001) Pharmacokinetics of antifungal agents in onychomycoses. Clin Pharmacokinet 40:441–472
Jensen JC (1989) Clinical pharmacokinetics of terbinafine (Lamisil). Clin Exp Dermatol 14:110–113
Meletiadis J, Chanock S, Walsh TJ (2006) Human pharmacogenomic variations and their implications for antifungal efficacy. Clin Microbiol Rev 19:763–787
Lynch T, Price A (2007) The effect of cytochrome P450 metabolism on drug response, interactions, and adverse effects. Am Fam Physician 76:391–396
Vickers AE, Sinclair JR, Zollinger M et al (1999) Multiple cytochrome P-450s involved in the metabolism of terbinafine suggest a limited potential for drug-drug interactions. Drug Metab Dispos 27:1029–1038
Nejjam F, Zagula M, Cabiac MD et al (1995) Pilot study of terbinafine in children suffering from tinea capitis: evaluation of efficacy, safety and pharmacokinetics. Br J Dermatol 132:98–105
Ghannoum MA, Wraith LA, Cai B, Nyirady J, Isham N (2008) Susceptibility of dermatophyte isolates obtained from a large worldwide terbinafine tinea capitis clinical trial. Br J Dermatol 159:711–713
Fernández-Torres B, Carrillo AJ, Martín E et al (2001) In vitro activities of 10 antifungal drugs against 508 dermatophyte strains. Antimicrob Agents Chemother 45:2524–2528
Carrillo-Muñoz AJ, Giusiano G, Cárdenes D, Fernández-Molina JM, Eraso E, Quindós G, Guardia C, del Valle O, Tur-Tur C, Guarro J (2008) Terbinafine susceptibility patterns for onychomycosis-causative dermatophytes and Scopulariopsis brevicaulis. Int J Antimicrob Agents 31:540–543
Borba-Santos LP, Rodrigues AM, Gagini TB et al (2015) Susceptibility of Sporothrix brasiliensis isolates to amphotericin B, azoles, and terbinafine. Med Mycol 53:178–188
Ottonelli Stopiglia CD, Magagnin CM, Castrillón MR et al (2014) Antifungal susceptibilities and identification of species of the Sporothrix schenckii complex isolated in Brazil. Med Mycol 52:56–64
Daboit TC, Massotti Magagnin C, Heidrich D et al (2014) In vitro susceptibility of chromoblastomycosis agents to five antifungal drugs and to the combination of terbinafine and amphotericin B. Mycoses 57:116–120
van Belkum A, Fahal AH, van de Sande WW (2011) In vitro susceptibility of Madurella mycetomatis to posaconazole and terbinafine. Antimicrob Agents Chemother 55:1771–1773
Ameen M, Lear JT, Madan V, Mohd Mustapa MF, Richardson M (2014) British Association of Dermatologists’ guidelines for the management of onychomycosis 2014. Br J Dermatol 171:937–958
de Sá DC, Lamas AP, Tosti A (2014) Oral therapy for onychomycosis: an evidence-based review. Am J Clin Dermatol 15:17–36
Gupta AK, Daigle D, Foley KA (2015) Network meta-analysis of onychomycosis treatments. Skin Appendage Disord 1:74–81
Gupta AK, Gregurek-Novak T (2001) Efficacy of itraconazole, terbinafine, fluconazole, griseofulvin and ketoconazole in the treatment of Scopulariopsis brevicaulis causing onychomycosis of the toes. Dermatology 202:235–238
Onsberg P (1980) Scopulariopsis brevicaulis in nails. Dermatologica 161:259–264
Chen X, Jiang X, Yang M et al (2016) Systemic antifungal therapy for tinea capitis in children. Cochrane Database Syst Rev 5:CD004685
Gupta AK, Drummond-Main C (2013) Meta-analysis of randomized, controlled trials comparing particular doses of griseofulvin and terbinafine for the treatment of tinea capitis. Pediatr Dermatol 30:1–6
Howden BP, Slavin MA, Schwarer AP, Mijch AM (2003) Successful control of disseminated Scedosporium prolificans infection with a combination of voriconazole and terbinafine. Eur J Clin Microbiol Infect Dis 22:111–113
Bhat SV, Paterson DL, Rinaldi MG, Veldkamp PJ (2007) Scedosporium prolificans brain abscess in a patient with chronic granulomatous disease: successful combination therapy with voriconazole and terbinafine. Scand J Infect Dis 39:87–90
Gosbell IB, Toumasatos V, Yong J, Kuo RS, Ellis DH, Perrie RC (2003) Cure of orthopaedic infection with Scedosporium prolificans, using voriconazole plus terbinafine, without the need for radical surgery. Mycoses 46:233–236
Li JY, Yong TY, Grove DI, Coates PT (2008) Successful control of Scedosporium prolificans septic arthritis and probable osteomyelitis without radical surgery in a long-term renal transplant recipient. Transpl Infect Dis 10:63–65
Tortorano AM, Richardson M, Roilides E, et al, European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group (2014) European ESCMID and ECMM joint guidelines on diagnosis and management of hyalohyphomycosis: Fusarium spp., Scedosporium spp. and others. Clin Microbiol Infect 20(Suppl 3):27–46
N’diaye B, Dieng MT, Perez A, Stockmeyer M, Bakshi R (2006) Clinical efficacy and safety of oral terbinafine in fungal mycetoma. Int J Dermatol 45:154–157
Rothe A, Seibold M, Hoppe T et al (2004) Combination therapy of disseminated Fusarium oxysporum infection with terbinafine and amphotericin B. Ann Hematol 83:394–397
Neuburger S, Massenkeil G, Seibold M et al (2008) Successful salvage treatment of disseminated cutaneous fusariosis with liposomal amphotericin B and terbinafine after allogeneic stem cell transplantation. Transpl Infect Dis 10:290–293
Tavakkol A, Fellman S, Kianifard F (2006) Safety and efficacy of oral terbinafine in the treatment of onychomycosis: analysis of the elderly subgroup in Improving Results in Onychomycosis-Concomitant Lamisil and Debridement (IRON-CLAD), an open-label, randomized trial. Am J Geriatr Pharmacother 4:1–13
Villars VV, Jones TC (1983) Special features of the clinical use of oral terbinafine in the treatment of fungal diseases. Br J Med 308:1275–1279
O’Sullivan DP, Needham CA, Bangs A, Atkin K, Kendall FD (1996) Postmarketing surveillance of oral terbinafine in the UK: report of a large cohort study. Br J Clin Pharmacol 42:559–565
Van’t Wout JW, Herrmann WA, De Vries RA, Stricker BHC (1994) Terbinafine-associated hepatic injury. J Hepatol 21:115–117
Juhlin L (1992) Loss of taste and terbinafine. Lancet 339:1483
Doty RL, Haxel BR (2005) Objective assessment of terbinafine-induced taste loss. Laryngoscope 115:2035–2037
Beutler M, Hartmann K, Kuhn M, Gartmann J (1993) Taste disorders and terbinafine. Br Med J 307:26
Stricker BH, Van Riemsdijk MM, Sturkenboom MC, Ottervanger JP (1996) Taste loss to terbinafine: a case-control study of potential risk factors. Br J Clin Pharmacol 42:313–318
Zheng Y, Zhang J, Chen H, Lai W, Maibach HI (2016) Terbinafine-induced lichenoid drug eruption. Cutan Ocul Toxicol 30:1–3
George A, Bhatia A, Kanish B, Williams A (2015) Terbinafine induced pityriasis rosea-like eruption. Indian J Pharmacol 47:680–681
Bonsmann G, Schiller M, Luger TA, Ständer S (2001) Terbinafine-induced subacute cutaneous lupus erythematosus. J Am Acad Dermatol 44:925–931
Lorentz K, Booken N, Goerdt S, Goebeler M (2008) Subacute cutaneous lupus erythematosus induced by terbinafine: case report and review of literature. J Dtsch Dermatol Ges 6:823–827
Pillans PI, Boyd IW (2007) Toenails and agranulocytosis. Intern Med J 37:572–575
Gupta AK, Soori GS, Del Rosso JQ, Bartos PB, Shear NH (1998) Severe neutropenia associated with oral terbinafine therapy. J Am Acad Dermatol 38:765–767
Ornstein DL, Ely P (1998) Reversible agranulocytosis associated with oral terbinafine for onychomycosis. J Am Acad Dermatol 39:1023–1024
Shapiro M, Li LJ, Miller J (1999) Terbinafine-induced neutropenia. Br J Dermatol 140:1196–1197
Conjeevaram G, Vongthavaravat V, Sumner R, Koff RS (2001) Terbinafine-induced hepatitis and pancytopenia. Dig Dis Sci 46:1714–1716
Aguilar C, Mueller KK (2001) Reversible agranulocytosis associated with oral terbinafine in a pediatric patient. J Am Acad Dermatol 45:632–634
Kovacs MJ, Alshammari S, Guenther L, Bourcier M (1994) Neutropenia and pancytopenia associated with oral terbinafine. J Am Acad Dermatol 31:806
Tsai HH, Lee WR, Hu CH (2002) Isolated thrombocytopenia associated with oral terbinafine. Br J Dermatol 147:627–628
Grunwald MH (1998) Thrombocytopenia associated with oral terbinafine. Int J Dermatol 37:634
Kantarcıoğlu B, Türköz HK, Yılmaz G et al (2014) Aplastic anemia associated with oral terbinafine: a case report and review of the literature. Turk J Haematol 31:411–416
Chitturi S, Farrell GC (2007) Drug-induced liver disease. In: Schiff ER, Sorrell MF, Maddrey WC (eds) Schiff’s diseases of the liver, 10th edn. Lippincott Williams and Wilkins, Philadelphia, pp 924–1005
Gupta AK, del Rosso JQ, Lynde CW, Brown GH, Shear NH (1998) Hepatitis associated with terbinafine therapy: three case reports and a review of the literature. Clin Exp Dermatol 23:64–67
Anania FA, Rabin L (2002) Terbinafine hepatotoxicity resulting in chronic biliary ductopenia and portalfibrosis. Am J Med 112:741–742
Choudhary NS, Kotecha H, Saraf N, Gautam D, Saigal S (2014) Terbinafine induced liver injury: a case report. J Clin Exp Hepatol 4:264–265
Dürrbeck A, Nenoff P (2016) Terbinafine: relevant drug interactions and their management. Hautarzt 67:718–723
Jensen P, Lehne G, Fauchald P, Simonsen S (1996) Effect of oral terbinafine treatment on cyclosporin pharmacokinetics in organ transplant recipients with dermatophyte nail infection. Acta Derm Venereol 76:280–281
WHO Pharmaceuticals. Newsletter 2001, No. 02&03, p 6
(2007) Terbinafine hydrochloride [package insert]. Novartis Pharmaceuticals, East Hanover, NJ
Wagner C, Graninger W, Presterl E, Joukhadar C (2006) The echinocandins: comparison of their pharmacokinetics, pharmacodynamics and clinical applications. Pharmacology 78(4):161–177
Arendrup MC, Boekhout T, Akova M, Meis JF, Cornely OA, Lortholary O, European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology (2014) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of rare invasive yeast infections. Clin Microbiol Infect 20(Suppl 3):76–98
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Bustamante, B., Hidalgo, J.A., Campos, P.E. (2017). Antifungal Drugs. In: Mora-Montes, H., Lopes-Bezerra, L. (eds) Current Progress in Medical Mycology. Springer, Cham. https://doi.org/10.1007/978-3-319-64113-3_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-64113-3_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-64112-6
Online ISBN: 978-3-319-64113-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)