Abstract
This paper has been edited for clarity, correctness and consistency with our house style. Please check it carefully to make sure the intended meaning has been preserved. If the intended meaning has been inadvertently altered by the editing changes, please make any corrections needed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
An anterior approach to the craniovertebral junction (CVJ) and, particularly, to the odontoid process of the second cervical vertebra has classically been performed, in neurosurgical settings, via a transoral route. Such a technique is still considered the gold-standard treatment for odontoid process diseases.
However, the advent of endoscopy in neurosurgery and the development and refinement of endonasal approaches to the entire midline skull base [1,2,3,4,5] have meant that this field, once dominated by microsurgery, has become a territory of exploration for neurosurgeons, who have dedicated clinical and scientific efforts in this direction. In fact, the endoscopic endonasal approach to the craniocervical junction, and to the odontoid process, is among the areas of most interest for which endoscopic techniques have been developed.
Several anatomical and/or clinical studies have been reported, showing the interest of approaching the craniocervical junction (CCJ) through the nasal corridor [6, 7]. The availability of new technologies—such as endoscopes, high-definition endoscopic cameras, navigation systems, ultrasound micro-Doppler, dedicated endonasal instruments and bipolar forceps—has opened new horizons for management of pathologies involving this complex region, using the natural nasal corridors; this way/approach has demonstrated remarkable improvements in the quality of disease resection and in functional outcomes with lower morbidity.
The endonasal route provides direct access to the surgical field, minimizing the mucosal and neurovascular manipulation: it follows a natural path that goes from the nostrils to the mucosa covering the rhinopharynx, the rhinopharyngeal muscles, the anterior arch of C1 and, finally, the odontoid process. As a consequence, the endoscopic endonasal approach is less invasive and does not require additional surgical manoeuvres such as (1) mouth retraction; (2) tongue compression or even splitting; (3) possible injury to the teeth; (4) injury to the uvula and/or the soft palate and velum pendulum; or (5) neurovascular manipulation through the oropharynx. Theoretically, such facts imply a lower rate of postoperative complications related to invasiveness, with lower rates of postoperative dysphagia and respiratory complications, possibly due to the fact that with the endoscopic approach, extubation coincides with the end of the procedure. This allows more rapid mobilization and a reduction in the recovery time for natural feeding, which is then reflected, of course, in the hospitalization time. Seen in this light, the endoscopic endonasal approach offers a viable alternative to the more established transoral approach, especially for the clear advantages that the endoscopic technique offers in cases where there is a full indication to execute it. On the other hand, in cases of dural opening the endonasal approach is associated with difficulty of dural closure, with associated higher risks of postoperative cerebrospinal fluid (CSF) leakage and meningitis. Given the intrinsic features of the endoscope, the endonasal route provides a wider, panoramic and multiangled view of the region and also allows close-up views of the relevant anatomical structures on the surgical field.
Anterior Versus Posterior Approach
The decision making between an anterior or a posterior approach depends on different particular aspects: (1) the direction of the compression; and (2) the surgeon’s confidence and experience with the approaches, and thus the possibility to perform reduction of the compression with an anterior, posterior or combined approach. In general, irreducible anterior subluxation associated with spinal cord compression requires an anterior approach, whereas reducible posterior compression requires a posterior surgical route. However, different complex diseases, acquired or congenital, can cause an alteration of atlantoaxial relationships and anterior cervicomedullary junction compression. In these cases, fixation or posterior stabilization may be not sufficient to resolve the ventral compression. In fact, in recent years, the option of a combined anterior and posterior approach has become the best choice according to many authors.
Transoral Approach and Transnasal Approach
Several surgical routes have been described for the craniovertebral junction (CVJ) region because of its complex anatomy and vital surrounding structures. During recent decades, the transoral approach with microscopic assistance has been proposed as the standard procedure for performing anterior odontoidectomy, considering the aetiology of the disease, the mechanism of compression and, finally, its reducibility [8,9,10,11]. The transoral approach has been considered the gold-standard approach for the surgical treatment of pathologies of the anterior CVJ. Specifically, in the absence of spinal cord contusion or progressive myelopathy, posterior decompression and fusion are sufficient to achieve an acceptable outcome. Odontoidectomy is necessary when there is irreducible bony compression of the spinal cord or soft tissue pannus causing severe ventral compression and resulting in progressive myelopathy.
The risk of bacterial contamination, need for prolonged postoperative intubation and nasogastric tube feeding, tongue swelling and nasopharyngeal incompetence after transoral surgery have led authors to identify alternative routes to approach this region.
The anterior aspect of the craniocervical region can be exposed also via a transnasal approach, although some anatomical limitations exist. In the transnasal route, exposure of the C2 body below the odontoid process is limited by the posterior part of the hard palate; however, angled endoscopes, drills and dedicated instruments provide access downward to the lower edge of the C2 body [12,13,14,15]. On the other hand, the transoral approach is limited by the degree of mouth opening, the size of the patient’s tongue, and the position of the uvula and the soft palate. The inferior limit of the access, usually the C3 vertebra, is determined by the degree of mouth opening, the size of the patient’s oral cavity and the prominence of the incisors. However, also for the transoral approach, the use of angled endoscopes and instruments directs the approach superiorly, increasing the rostral access above the anterior arch of the atlas to the lower clivus and C2 [16, 17]. One of the main anatomical landmarks to consider, especially in the transoral route, is the course of the vertebral artery (VA). After ascending through the transverse foramen of the axis and atlas, approximately 15 mm from the midline, the VA courses medially along the upper surface of the posterior arch of the atlas to reach its dural entrance. It is mandatory to preserve the segment of the VA ascending between the C1 and C2 transverse processes.
Once the anterior arch of C1 is exposed, it must be drilled to expose the odontoid process of C2. Another difference between the transoral and transnasal approaches is the visualization of the ligamentous complex. For instance, the apical ligament is easily visualized directly ahead of the endoscope in the transnasal route, but in the transoral approach it is not seen until later, after removal of the odontoid process. The main step in anterior odontoidectomy is represented by the drilling of the dens. In the transnasal approach, the dens is seen directly ahead. The anterior cortical surface and core of the dens are drilled, and the cortical shell is removed. On the other hand, the base of the dens is more easily accessed for drilling by the transoral route. In addition, a different view is offered by these two approaches regarding the exposure of the upper, middle or lower clivus. The standard endoscopic transnasal transsphenoidal approach allows one to reach the upper clivus, which corresponds to the posterior wall of the sphenoid sinus. Thus, the middle and lower clivus are viewed directly ahead in the transnasal approach. The access to the middle and lower clivus generally does not require opening of the sphenoid sinus. On the other hand, in the transoral approach the middle and upper clivus are not usually accessible because this would require soft and hard palate opening, with splitting of the tongue or mandible, to gain upward angulation. However, manoeuvres such as using an angled endoscope, retracting the uvula sufficiently and opening the mouth widely provide safe access to the lower clivus.
Indications
Odontoidectomy is a procedure that is necessary in all cases in which there is impairment of the nervous structures of the craniocervical junction due to an irreducible alteration of the relations that the odontoid process conducts with neighbouring neurovascular structures.
Various pathologies may cause atlantoaxial misalignment and bulbomedullary junction compression; among them are congenital malformations such as Arnold–Chiari malformation type II, genetic degenerative transformation such as in Down’s syndrome, chronic inflammation related to rheumatoid arthritis and/or metabolic disorders, and, finally, posttraumatic alterations (Fig. 1).
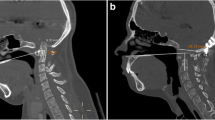
Preoperative neuroimaging studies. T2-weighted (a) sagittal and (b) axial magnetic resonance imaging (MRI) of the craniovertebral junction, showing bulbomedullary compression by an extradural mass lesion of the odontoid process (rheumatoid pannus). (c, d) Three-dimensional reconstruction of computed tomography angiography (CTA) of the same patient
The irreducibility is a crucial concept on the path that leads to the indication for surgery. In fact, several studies have confirmed that, when feasible, reduction of the compression by putting the craniocervical junction in traction and subsequent fixation—and in cases of compression due to rheumatoid pannus, posterior stabilization of the craniocervical junction—lead in some instances to improvement or even resolution of the ventral compression.
Therefore, the indications for odontoidectomy arise in all cases in which there is irreducible atlantoaxial subluxation associated with severe brainstem and/or spinal cord compression causing progressive neurological dysfunction. In most cases, the pathological process may be due to (1) irreducible basilar impression [18,19,20,21,22,23]; (2) ventral compression, as in cases of rheumatoid pannus that is not resolved after posterior stabilization [24,25,26]; (3) significant retroflexion of the odontoid process or basilar invagination associated with Chiari malformation [27]; (4) the presence of os odontoideum [28,29,30]; or (5) posttraumatic pseudoarthrosis or misalignment. Several recent experiences have enlarged the indications for endoscopic endonasal odontoidectomy to treat intradural lesions [3, 5, 31,32,33].
Feasibility of the Endoscopic Endonasal Odontoidectomy
The goal of the surgical operation is to completely remove the odontoid process of C2 and achieve sufficient decompression of the ventral brainstem and CVJ. In the debate between microsurgery and the endoscopic technique, it has been remarked that in the endonasal approach, there can be difficulty in reaching the lower portion of the craniocervical junction and, namely, the base of the dens. To understanding this aspect, numerous studies have been performed on cadavers and on radiological images, with the purpose of delineating the limits and then the indications for the endoscopic approach to odontoid process pathology. Leading authors have widely reported the feasibility of the endoscopic endonasal approach (EEA) to the CVJ [3, 6].
In cases of a low junction, located far below the level of the hard palate, it could be quite difficult, if not impossible, to reach the anterior arch of C1 and the base of the odontoid process. Such cases can represent an indication for the transoral approach. On the other hand, in cases of a higher junction, the dens is more easily reachable and removable by the nasal route.
To preoperatively assess the feasibility of odontoidectomy via an endoscopic endonasal route, on a midline sagittal computed tomography (CT) slice with a bone window it is possible to draw four lines representing possible paths from the piriform aperture of the nasal bones, which target the odontoid process and allow assessment of the inferior limit for surgical exposure. Predicting the inferior limit of the CVJ is crucial to choose the appropriate approach in an area that is considered a transitional area between the endonasal and transoral routes.
Nasopalatine Line
One of the criticisms of the EEA to the upper cervical spine is the limited exposure inferiorly. Endonasal dissection of the upper cervical spine is limited superiorly by the nasal bones and the soft tissues of the nose, and inferiorly by the hard palate and soft palate [34, 35]. The line created by connecting the most inferior point of the nasal bone to the posterior edge of the hard palate in the midsagittal plane is defined as the nasopalatine line (NPL) and is considered a limitation of caudal dissection with straight endoscopic instruments. The angle created by this line and the plane of the hard palate—the nasopalatine angle (NPA)—provides the window of exposure to the skull base and upper cervical spine. The mean nasopalatine angle is 27.1 ± 0.7°. The mean point of intersection between the NPL and the vertebral column is reported to be 8.9 ± 1.8 mm above the base of the C2 vertebral body. The NPL is considered by several authors to be a controversial predictor of the maximal extent of inferior dissection in endoscopic endonasal resection of the odontoid process [34], considering that the inferior limit predicted by the NPL was found to have a mean value of 12.7 mm, below the real inferior extent of surgical dissection. Various pathological factors (basilar invagination) and physiological factors (head positioning) affect the point of intersection of the NPL with the cervical spine. To improve caudal exposure, the use of angled instruments or drills may be of value. Additionally, retraction of the soft palate and drilling of the posterior edge of the hard palate may improve the exposure but may increase the risks of palatal dehiscence and velopharyngeal insufficiency.
Nasoaxial Line
The nasoaxial line (NAxL) is defined as a line constructed on the midsagittal plane using a starting point that corresponds to the midpoint of the distance from the rhinion to the anterior nasal spine of the maxillary bone and a second point at the tip of the posterior nasal spine of the palatine bone. It extends posteriorly and inferiorly to the cervical spine. To predict (more accurately than using NPL) the lower limit of the EEA to reach the CVJ through the correspondence between CT measurements and the real surgical limit, a cadaver study was performed to evaluate the predictive value of the NAxL. The findings supported the close correspondence between the NAxL, drawn on preoperative CT images, and the anatomical surgical extent [36].
Hard Palate Line
The hard palate line (HPL) is defined as a line that passes through the anterior and posterior edges of the hard palate (the anterior nasal spine of the maxillary bone and the posterior nasal spine of the palatine bone, respectively) and intersects with the craniovertebral junction posteriorly. This line represents the long axis of the hard palate [37]. It is considered a reliable marker of the inferior extension of the CVJ especially in congenital abnormalities, such as platybasia with associated basilar invagination, where the tip of the odontoid process is often above the plane of the hard palate [38].
Rhinopalatine Line
The rhinopalatine line is defined as a line constructed on the midsagittal plane, using a starting point that corresponds to the two-thirds point of the distance from the rhinion to the anterior nasal spine of the maxillary bone and a second point at the posterior nasal spine of the palatine bone. The line is extended posteriorly and inferiorly, ending at the cervical spine. There have been great efforts made by different groups to study the inferior limit of the EEA. De Almeida et al. [34] described the nasopalatine (NPL) as a good and accurate predictor of the inferior limit of the EEA, but in their study, the NPL always gave a result below the inferior extent of surgical dissection with a mean value of 12.7 mm. Consequently, the nasoaxial line was reported to predict, more accurately and reliably, the inferior caudal exposure with the EEA. Similarly, it was found that the NAxL also overpredicted the lower limits of the approach [37]. The rhinopalatine line (RPL) seemed to be the most accurate predictor in several studies.
This predictor accounts also for patient anatomical variability, such as the presence of nasal and palatal osseous and soft structures, together with the hard palate’s direction and length, which represent the most significant factors that limit the inferior extension of the EEA. The RPL cannot be used to predict the lateral limits of the EEA in CVJ surgery.
Operative Technique
Depending on individual patients’ pathologies, we perform endoscopic endonasal odontoidectomy followed by posterior decompression and fusion in a single-stage surgery.
To accurately choose the correct approach, we consider, on a sagittal CT scan, the relationship between the nasopalatine and rhinopalatine lines and the upper cervical spine.
We routinely use a neuronavigation system (StealthStation S7®; Medtronic, Minneapolis, MN, USA) based on contrast-enhanced magnetic resonance imaging (MRI) with angiographic time-of-flight (TOF) sequences merged with a 1-mm layer CT scan of the brain and cervical spine in a single volume. Generally, we use the optical tracking of the StealthStation S7® merged with the angiographic TOF sequences to provide feasible preoperative images regarding the relationship between the CVJ bony and vascular structures such as the vertebral and carotid arteries. Somatosensory evoked potential neuromonitoring is used routinely.
Patient Positioning and Preparation
Following general anaesthesia and orotracheal intubation, the patient is placed in a supine position with the trunk elevated by about 20°. The head is slightly turned to the right (maximum 10°), not flexed, and fixed in a radiolucent Mayfield-Kees three-pin headclamp. The head is kept parallel to the floor and maintained without flexion or extension during the posterior fusion, when the patient is turned from the supine position to the prone position. In all cases we use the O-arm® system (Medtronic) in the phase of posterior fusion. On this, the optical reference of the neuronavigator is mounted, in case the optical system is used. The magnetic reference is positioned on the patient’s head, in case the electromagnetic system is used. We administer antibiotic prophylaxis with cefazolin 2 g 1 h before the procedure.
Nasal Phase
The nose is prepped with cottonoids soaked with diluted iodopovidone 5% solution inside the two nostrils. A 0° angled lens and an 18 cm endoscope associated with a high-definition (HD) camera (Karl Storz, Tuttlingen, Germany) is introduced into the right nostril. Identification of the usual anatomical nasal landmarks is performed (the inferior turbinate laterally and the nasal septum medially). As a standard endoscopic endonasal procedure, above the inferior turbinate, the middle turbinate is identified and luxated laterally, with cottonoids soaked with diluted adrenaline (epinephrine) placed between the middle turbinate and the nasal septum to prevent bleeding of the nasal mucosa. The same manoeuvres are carried out in the left nostril. The endoscope advances parallel to the floor of the nasal cavity until the choana is reached. With the aid of the neuronavigation system, the anatomical landmarks are verified. The mucosa over the posterior and inferior aspect of the nasal septum is cauterized with monopolar coagulation or, better still, with bipolar forceps. We do not routinely perform removal of the anterior wall of the sphenoid sinus since a transsphenoidal corridor is rarely needed unless higher exposure is required in cases where the tip of the dens goes quite high or where more space is required for the surgical manoeuvres because of the patient’s individual anatomy. Afterward, an inferior septectomy is performed with sufficient removal of the vomer bone and extending inferiorly down to the hard palate. The most superior limit reached is the clivus–nasal septum junction. At this stage a few important anatomical landmarks should be identified, which guide the surgeon to stay oriented: (1) the clivus–septum junction superiorly; (2) the Eustachian tubes laterally; and (3) the nasal floor/soft palate inferiorly as marked by the hard and soft palate. The neuronavigation will confirm the position of such surgical landmarks and give the correct direction for the subsequent surgical steps.
Nasopharynx Phase
The key points of the nasal phase allow the widest exposure of the rhinopharynx and avoidance of any conflict between instruments during the next surgical steps. The nasopharynx mucosa is incised on the midline (Fig. 2a), and the muscles are dissected bilaterally to expose the anterior arch of C1 (Fig. 2b). Several authors have described a reverse U-shaped nasopharyngeal flap prepared with monopolar electrocautery, elevated and reflected caudally to the level of the soft palate to improve the surgical field. The craniocaudal extension of the flap involves the inferior third of the clivus superiorly and the C2 vertebral body inferiorly; the lateral margins of the operative exposure includes the lateral masses of the C1 vertebra. The U-shaped nasopharynx flap extends the surgical corridor laterally, but on the other hand it increases the risk of injury to the parapharyngeal carotids, which are located laterally to the superior pharyngeal constrictor muscle. We prefer doing a straight midline opening of the nasopharynx because it guarantees sufficient exposure and a lower risk of vascular damage. Then, we proceed with skeletonizing of the anterior arch of C1 and of the odontoid process in a subperiosteal fashion.
C1 Anterior Arch Preservation in Selected Cases
Recently, several authors have reported their experience in the matter of endoscopic endonasal odontoidectomy, focusing on the preservation of the C1 anterior arch during the craniovertebral junction phase, avoiding posterior fixation [32, 39]. Particularly in cases of rheumatoid arthritis or other inflammatory diseases, the anterior arch of the atlas is preserved by drilling the odontoid base, weakening its apex and leading to pulling downward of the dens in the working area. Subsequent removal of the axis with other remaining compressive inflammatory lesions is performed using a combination of a high-speed drill, ultrasonic bone curette and standard Kerrison rongeurs [32, 39]. According to such authors, working above and below the C1 anterior arch and its preservation not only represent an element of stability but also provide an important opportunity for reconstruction and to reinforce the closure. Additionally, the same groups, in cases of inveterate Anderson–D’Alonzo type II fractures or the combination of an odontoid fracture with a fracture of the anterior arch of C1, have proposed a technique of anterior fixation and anterior C1 arch reconstruction [40].
Craniovertebral Junction Phase and Closure
In our technique, the anterior arch of the atlas is exposed and removed using the high-speed drill with diamond burrs and Kerrison rongeurs. Posteriorly, the odontoid process of C2 is exposed (Fig. 2c), separated from the alar and apical ligaments, dissected from the transverse ligament, thinned using the microdrill and finally removed (Fig. 2d). At this point, a wide surgical corridor is created. The odontoidectomy is performed carefully by using the high-speed drill, Kerrison rongeurs and, in cases of lesions with a soft consistency, curettes and pouches or ultrasound aspiration. When the removal is complete, the dural plane appears to pulsate and indicates optimal decompression of the brainstem (Fig. 3a, b).
After satisfactory haemostasis is achieved, the closure is guaranteed with a layer of fibrin glue only in the absence of possible dural tearing (Fig. 3c). In the case of CSF leakage, packing with Gelfoam/Surgicel and fibrin glue is used to reinforce the closure. In these cases we consider the possibility of positioning an extended lumbar drain (ELD) at the end of the operation. We close the nasopharynx mucosa with a single stich because the median opening allows faster closure of the muscles at the end of the endoscopy time. Generally, we position a nasogastric tube under endoscopic control (Fig. 3d).
Posterior Fusion
The second step of the operation is characterized by the posterior occipitocervical fusion. The patient, already fixed to the Mayfield-Kees three-pin carbon fibre radiolucent headholder, is turned from the supine position to the prone position with the head parallel to the floor and with a slight degree of extension. This position considers the C0–C2 angle, which is formed by the posterior extension of the hard palate and the vertical line passing through the dens, and avoids breathing impairment related to the flexion. A midline incision is performed, starting from the inion, to the spinous process of C6. The fascia is exposed and incised on the midline with monopolar cautery. The muscle dissection is performed along the raphe in a subperiosteal fashion from the basiocciput to the posterior complex of C5. The bone landmarks are clearly visible: (1) the occipital bone; (2) the posterior arch and lateral masses of C1; and (3) the posterior complex from C1 to C5.
Generally, we remove the posterior arch of C1 because in most of our cases it is contributing to the bulbopontine compression. The lateral masses of C3 and C4 are identified and verified through the O-arm® system. The fixation system we use in all cases is the Vertex titanium system (Medtronic). The high-speed drill is used to prepare the position of the screws within the lateral masses of C3 and C4. The polyaxial screws are inserted according to the Magerl technique [41] to avoid vascular injuries. In the basiocciput the monoaxial screws are positioned 2 cm from the inion on both sides and 1 cm above the sinuses. The length of the screws we use is 8 mm. After the screws are positioned, the two rods are pulled to obtain the correct alignment of the cervical spine and finally fixed through the wrench of the wing nuts. The bone fusion is improved with the addition of bone substitutes. The last verification with the O-arm® system is done at the end of the procedure. At discharge we recommend use of a cervical collar for 2 months.
Series Presentation
In the Neurosurgical Clinic at the University of Messina, a series of four endonasal endoscopic odontoidectomies were performed. Demographic, clinical and management details are summarized in Tables 1 and 2.
All four patients were female, ranging between 62 and 82 years of age (mean age 67.75 years). Three patients were admitted with a neurological onset characterized by tetraparesis; in one patient, motor deficits were prevalent in the right arm. Urinary incontinence was present in two patients. One patient presented with severe dysphagia with both solids and liquids. In two patients, the symptoms were related to the presence of a rheumatoid synovial pannus, while the other two cases showed signs and symptoms due to a complex malformation of the craniocervical junction and to misalignment of the odontoid process following a previous non-fused Anderson–D’Alonzo type II fracture, respectively. Interestingly, the patient affected by the complex CCJ malformation had previously undergone occipitocervical stabilization at another institution. She then underwent an attempted transoral odontoidectomy, which failed because of the higher position of the dens. She was subsequently referred to our clinic for anterior decompression performed through an endoscopic endonasal odontoidectomy. In the remaining three patients, anterior decompression and posterior stabilization were performed during the same operation.
The mean length of stay was 14.5 days (range 9–19 days). In all patients there was improvement of the neurological conditions in comparison with the preoperative status. In one patient the swallowing dysfunction resolved, allowing early oral feeding. In two cases, implementation of parenteral nutrition was necessary for a few days. In one case the nasogastric tube was left in place to facilitate enteral feeding.
Postoperative Management
In our practice, according to the general clinical condition of the patient and the length of sedation, we prefer to keep the patient in our intensive care unit for 24 h. This occurred in two of the four cases we treated. In our department, the primary aim is early mobilization of the patient to lower the risks associated with extended bed rest. In addition, use of a nasogastric tube guarantees sufficient caloric intake, with the addition of parenteral nutrition, when required. We perform at least two endoscopic postoperative controls: one in the first 24 h and one before discharge. During such checks we verify the closure of the surgical wound and the possible presence of CSF leakage, and then we remove the nasogastric tube under endoscopic control. This manoeuvre can be performed only after testing of the function of the lower cranial nerves by an otolaryngologist. In our series, removal of the nasogastric tube occurred in three patients: on the eighth postoperative day in two patients, and on the seventh postoperative day in the other one. In our series, before discharge, a CT scan of the head and cervical spine was performed to assess the degree of the odontoidectomy and the correct positioning of the screws and rods of the posterior fusion, and MRI was performed to evaluate the decompression of the neurovascular structures. A further control was performed after 3 months. All patients started a physical rehabilitation programme, which was also continued after discharge (Fig. 4).
Intraoperative pictures of the endoscopic endonasal approach. (a) Incision into the rhinopharynx (rPh). (b) Drilling of the anterior arch of C1. (c) Drilling of the odontoid process (OP) of C2. (d) Freeing of the remaining part of the dens from the ligaments. C 1 tub anterior tubercle of C1, ET Eustachian tubes, lig ligaments
Intraoperative pictures of the endoscopic endonasal approach. (a) Removal of pannus (p) causing compression. (b) Dura mater (DM) of the craniovertebral junction. (c) Closure of the muscle and mucosal incision with the aid of fibrin glue (fg). (d) Endoscopic control of the surgical field 3 days later, showing optimal closure of the incision. The asterisk denotes the nasogastric tube. C 2 base of the dens (body of C2), ET Eustachian tube, rPh rhinopharynx, SP soft palate
Postoperative neuroimaging studies of the same patient shown in Fig. 1. (a) T2-weighted sagittal magnetic resonance imaging (MRI) of the craniovertebral junction (CVJ) showing optimal decompression of the bulbomedullary junction. (b, c) Intraoperative O-arm® images showing removal of the odontoid process. (d–f) Three-dimensional reconstruction of the postoperative computed tomography (CT) scan of the CVJ
References
Cappabianca P, Cavallo LM, Esposito F, de Divitiis O, Messina A, de Divitiis E. Extended endoscopic endonasal approach to the midline skull base: the evolving role of transsphenoidal surgery. In: Pickard JD, Akalan N, Di Rocco C, Dolenc VV, Lobo Antunes J, Mooij JJA, Schramm J, Sindou M, editors. Advances and technical standards in neurosurgery. Vienna: Springer; 2008. p. 152–99.
Cavallo LM, De Divitiis O, Aydin S, Messina A, Esposito F, Iaconetta G, Talat K, Cappabianca P, Tschabitscher M. Extended endoscopic endonasal transsphenoidal approach to the suprasellar area: anatomic considerations—part 1. Neurosurgery. 2008;61(3 Suppl):24–33.
Cavallo LM, Messina A, Cappabianca P, Esposito F, de Divitiis E, Gardner P, Tschabitscher M. Endoscopic endonasal surgery of the midline skull base: anatomical study and clinical considerations. Neurosurg Focus. 2005;19(1):E2.
Esposito F, Becker DP, Villablanca JP, Kelly DF. Endonasal transsphenoidal transclival removal of prepontine epidermoid tumors: technical note. Neurosurgery. 2005;56(2 Suppl):E443.
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus. 2005;19(1):E4.
Cavallo LM, Cappabianca P, Messina A, Esposito F, Stella L, de Divitiis E, Tschabitscher M. The extended endoscopic endonasal approach to the clivus and cranio-vertebral junction: anatomical study. Childs Nerv Syst. 2007;23(6):665–71.
Messina A, Bruno MC, Decq P, Coste A, Cavallo LM, de Divittis E, Cappabianca P, Tschabitscher M. Pure endoscopic endonasal odontoidectomy: anatomical study. Neurosurg Rev. 2007;30(3):189–94.
Crockard HA. The transoral approach to the base of the brain and upper cervical cord. Ann R Coll Surg Engl. 1985;67(5):321–5.
Crockard HA, Pozo JL, Ransford AO, Stevens JM, Kendall BE, Essigman WK. Transoral decompression and posterior fusion for rheumatoid atlanto-axial subluxation. J Bone Jt Surg Br. 1986;68(3):350–6.
Perrini P, Benedetto N, Guidi E, Di Lorenzo N. Transoral approach and its superior extensions to the craniovertebral junction malformations: surgical strategies and results. Neurosurgery. 2009;64(5 Suppl 2):331–42. https://doi.org/10.1227/01.NEU.0000334430.25626.DC.
Perrini P, Benedetto N, Di Lorenzo N. Transoral approach to extradural non-neoplastic lesions of the craniovertebral junction. Acta Neurochir. 2014;156(6):1231–6.
Cappabianca P, Cavallo LM, Esposito F, de Divitiis E. Endoscopic endonasal transsphenoidal surgery: procedure, endoscopic equipment and instrumentation. Childs Nerv Syst. 2004;20(11–12):796–801.
Cappabianca P, de Divitiis O, Esposito F, Cavallo LM, de Divitiis E. Endoscopic skull base instrumentation. In: Anand VK, Schwartz TH, editors. Practical endoscopic skull base surgery. San Diego: Plural Publishing; 2007. p. 45–56.
Cappabianca P, Esposito F, Cavallo LM, Corriero OV. Instruments. Cranial, Craniofacial Skull Base Surg. 2010;2010:7–15.
Esposito F, Di Rocco F, Zada G, Cinalli G, Schroeder HWS, Mallucci C, Cavallo LM, Decq P, Chiaramonte C, Cappabianca P. Intraventricular and skull base neuroendoscopy in 2012: a global survey of usage patterns and the role of intraoperative neuronavigation. World Neurosurg. 2013;80(6):709–16.
de Divitiis O, Conti A, Angileri FF, Cardali S, La Torre D, Tschabitscher M. Endoscopic transoral–transclival approach to the brainstem and surrounding cisternal space: anatomic study. Neurosurgery. 2004;54(1):125–30.
Visocchi M, Doglietto F, Della Pepa GM, Esposito G, La Rocca G, Di Rocco C, Maira G, Fernandez E. Endoscope-assisted microsurgical transoral approach to the anterior craniovertebral junction compressive pathologies. Eur Spine J. 2011;20(9):1518–25.
Goel A, Bhatjiwale M, Desai K. Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg. 1998;88(6):962–8.
Karam YR, Menezes AH, Traynelis VC. Posterolateral approaches to the craniovertebral junction. Neurosurgery. 2010;66(3 Suppl):135–40. https://doi.org/10.1227/01.NEU.0000365828.03949.D0.
Menezes AH. Craniocervical developmental anatomy and its implications. Childs Nerv Syst. 2008;24(10):1109–22.
Menezes AH, VanGilder JC. Transoral–transpharyngeal approach to the anterior craniocervical junction. Ten-year experience with 72 patients. J Neurosurg. 1988;69(6):895–903.
Smoker WR. Craniovertebral junction: normal anatomy, craniometry, and congenital anomalies. Radiographics. 1994;14(2):255–77.
Smoker WRK, Khanna G. Imaging the craniocervical junction. Childs Nerv Syst. 2008;24(10):1123–45.
Joaquim AF, Appenzeller S. Cervical spine involvement in rheumatoid arthritis—a systematic review. Autoimmun Rev. 2014;13(12):1195–202.
Pare MC, Currier BL, Ebersold MJ. Resolution of traumatic hypertrophic periodontoid cicatrix after posterior cervical fusion: case report. Neurosurgery. 1995;37(3):531–4.
Sandhu FA, Pait TG, Benzel E, Henderson FC. Occipitocervical fusion for rheumatoid arthritis using the inside–outside stabilization technique. Spine. 2003;28(4):414–9.
Klekamp J. Chiari I malformation with and without basilar invagination: a comparative study. Neurosurg Focus. 2015;38(4):E12.
Arvin B, Fournier-Gosselin MP, Fehlings MG. Os odontoideum: etiology and surgical management. Neurosurgery. 2010;66(3 Suppl):22–31. https://doi.org/10.1227/01.NEU.0000366113.15248.07.
Matsui H, Imada K, Tsuji H. Radiographic classification of os odontoideum and its clinical significance. Spine. 1997;22(15):1706–9.
Vargas TM, Rybicki FJ, Ledbetter SM, MacKenzie JD. Atlantoaxial instability associated with an orthotopic os odontoideum: a multimodality imaging assessment. Emerg Radiol. 2005;11(4):223–5.
Cappabianca P, Cavallo LM, Esposito F, de Divitiis O, Messina A, de Divitiis E. Extended endoscopic endonasal approach to the midline skull base: the evolving role of transsphenoidal surgery. In: Pickard JD, editor. Advances and technical standards in neurosurgery. Vienna: Springer; 2007. p. 1–48.
Iacoangeli M, Gladi M, Alvaro L, Di Rienzo A, Specchia N, Scerrati M. Endoscopic endonasal odontoidectomy with anterior C1 arch preservation in elderly patients affected by rheumatoid arthritis. Spine J. 2013;13(5):542–8.
Kassam AB, Gardner PA, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM. Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg. 2008;108(4):715–28.
De Almeida JR, Zanation AM, Snyderman CH, Carrau RL, Prevedello DM, Gardner PA, Kassam AB. Defining the nasopalatine line: the limit for endonasal surgery of the spine. Laryngoscope. 2009;119(2):239–44.
Kassam AB, Snyderman C, Gardner P, Carrau R, Spiro R. The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report. Neurosurgery. 2005;57(1 Suppl):E213.
Aldana PR, Naseri I, La Corte E. The naso-axial line: a new method of accurately predicting the inferior limit of the endoscopic endonasal approach to the craniovertebral junction. Neurosurgery. 2012;71:ons308–14. https://doi.org/10.1227/NEU.0b013e318266e488.
La Corte E, Aldana PR, Ferroli P, Greenfield JP, Hartl R, Anand VK, Schwartz TH. The rhinopalatine line as a reliable predictor of the inferior extent of endonasal odontoidectomies. Neurosurg Focus. 2015;38(4):E16.
El-Sayed IH, J-C W, Ames CP, Balamurali G, Mummaneni PV. Combined transnasal and transoral endoscopic approaches to the craniovertebral junction. J Craniovertebr Junction Spine. 2010;1(1):44–8.
Gladi M, Iacoangeli M, Specchia N, Re M, Dobran M, Alvaro L, Moriconi E, Scerrati M. Endoscopic transnasal odontoid resection to decompress the bulbo-medullary junction: a reliable anterior minimally invasive technique without posterior fusion. Eur Spine J. 2012;21(Suppl 1):55–60. https://doi.org/10.1007/s00586-012-2220-4.
Re M, Iacoangeli M, Di Somma L, Alvaro L, Nasi D, Magliulo G, Gioacchini FM, Fradeani D, Scerrati M. Endoscopic endonasal approach to the craniocervical junction: the importance of anterior C1 arch preservation or its reconstruction. Acta Otorhinolaryngol Ital. 2016;36(2):107–18.
Suchomel P, Stulik J, Klezl Z, Chrobok J, Lukas R, Krbec M, Magerl F. Transarticular fixation of C1–C2: a multicenter retrospective study. Acta Chir Orthop Traumatol Cechoslov. 2004;71(1):6–12.
Competing Interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
No financial support was received for this work.
Rights and permissions
Copyright information
© 2019 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Abbritti, R.V. et al. (2019). Endoscopic Endonasal Odontoidectomy and Posterior Fusion in a Single-Stage Surgery: Description of Surgical Technique and Outcome. In: Visocchi, M. (eds) New Trends in Craniovertebral Junction Surgery. Acta Neurochirurgica Supplement, vol 125. Springer, Cham. https://doi.org/10.1007/978-3-319-62515-7_29
Download citation
DOI: https://doi.org/10.1007/978-3-319-62515-7_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-62514-0
Online ISBN: 978-3-319-62515-7
eBook Packages: MedicineMedicine (R0)