Abstract
Radiography, computed tomography (CT), and magnetic resonance imaging exams of the cervical spine were performed in a 29-year-old man who was ultimately diagnosed with an orthotopic os odontoideum during admission for injuries sustained in a motor vehicle collision. Initial radiography suggested either os odontoideum or an acute fracture of the dens. Further imaging with CT and flexion and extension radiographs confirmed os odontoideum and excluded a dens fracture. Although rare, os odontoideum is an important cervical spine anomaly to consider and to distinguish from an acute fracture of the dens.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Os odontoideum is a cervical spine anomaly of the atlas and axis (C1 and C2) characterized by a round, well-corticated ossicle located superior to and separated from a hypoplastic dens [1, 2]. The etiology of os odontoideum is controversial, as both congenital and acquired etiologies are onsidered. The congenital origin is suggested by twin and familial associations, as well as the higher incidence in patients with Down syndrome, Klippel–Feil syndrome, and multiple epiphyseal dysplasia [3–6]. However, acquired os odontoideum after cervical spine trauma has also been demonstrated [4, 7–9].
Regardless of the etiology, patients with os odontoideum are at greater risk for atlantoaxial instability and resultant spinal cord compression [10]. In the acute setting, proper assessment of post-traumatic cervical spine imaging requires differentiation of os odontoideum from dens fracture. The ossicle in an orthotopic os odontoideum is in anatomic alignment, i.e. located posterior to the anterior arch of C1. A dystopic ossicle is located anywhere else and will generally associate with the foramen magnum; it may also fuse with the basion [11].
Case report
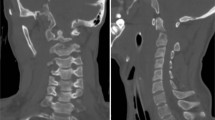
A 29-year-old male with no significant previous medical history was presented to the Emergency Department with posterior midline neck pain following a motor vehicle collision (MVC). The neurological exam was normal. Initial three view cervical spine radiographs (lateral, antero-posterior, and open-mouth dens views) revealed separation of the C2 body from what appeared to be an apical ossicle (Fig. 1a).
Os odontoideum. Lateral radiograph (a) of C1–C2 with collar in place suggests that the apical dens or ossicle (arrow heads) is separated from the body of C2. Sagittally reformatted CT image of the cervical spine at midline (b) reveals a well-corticated ossicle (arrow) separated from C2 by smooth, sclerotic margins of cortex. The anterior arch of C1 is hypertrophied and located just anterior to the ossicle
Although sclerotic margins bordered the cranial end of the C2 body and the presumed ossicle, a cervical spine CT was performed to definitively exclude an acute dens fracture. Sagittally reformatted images confirmed that the margins of both the ossicle and base of the dens were well-corticated and excluded an acute fracture (Fig. 1b).
Flexion and extension radiographs were subsequently performed (Fig. 2) and showed atlantoaxial instability with 13 mm subluxation of C1 on C2. The ossicle remained associated with the anterior arch of C1, maintaining a static relationship with the C1 arch on both the flexion and extension radiographs.
Atlantoaxial instability. Anterior subluxation of 13 mm was present during flexion as measured using the difference in the space (double arrow) between the anterior cortex of the anterior arch of C1 (line) and body of C2 during flexion (a) and extension (b). The os odontoideum remained static in position relative to the hypertrophic anterior arch of C1 during both flexion and extension, thereby precluding a measurement of the anterior atlantodental interval (AADI)
Magnetic resonance imaging of the cervical spine on a 1.5-T scanner using T1-weighted (TR/TE=500/30) and T2-weighted fast spin echo (TR/ETE/ETL=3,000/105/9) was performed [12] to evaluate the spinal canal and its relationship to the cord given the degree of subluxation. No spinal cord compression or canal stenosis was present, and the MRI further confirmed the chronicity of findings as there were no blood products or edema (Fig. 3) as secondary findings of an acute injury.
Discussion
Distinguishing os odontoideum from a dens fracture can be a critical component in the workup of patients in whom acute cervical spine injury is suspected. Although os odontoideum may be well visualized on radiography [2], many features may overlap with a healed dens fracture. The smooth, well-corticated, sclerotic margins and round or oval shape help distinguish os odontoideum from the sharp, non-corticated, and irregular margins of an acute type I/II dens fracture.
Os odontoideum is characterized by a radiolucent band or gap between the C2 body and superior portion of the dens. The ossicle is often located above the superior articular facets of C2 and superior and posterior to the anterior arch of C1. In cases where the radiographic findings are equivocal, cervical spine CT with sagittal and coronal reformatting may better characterize the location and cortical margins.
An understanding of dens development is also important to help distinguish among fracture, developmental variant, and os odontoideum. The dens forms from three ossification centers. Two primary ossification centers coalesce within three months after birth. One secondary ossification center, the ossiculum terminale, develops in the proximal dens epiphysis after eight or ten years and fuses with the rest of the dens between ten and thirteen years [13].
A persistent ossiculum terminale may be seen after adolescence if it fails to fuse with the basal portion of the dens thereby leaving a permanent cartilaginous synchondrosis between the body of C2 and the ossicle [13]. Ossiculum terminale often appears v-shaped and may be distinguished by its more cranial location. The ossicle of persistent ossiculum terminale is smaller than the ossicle of os odontoideum, and is not associated with significant atlantoaxial instability [8].
Patients with os odontoideum may present with chronic or acute manifestations of cervical cord myelopathy [9] resulting from atlantoaxial instability. When evaluating atlantoaxial instability, the anterior atlantodental interval (AADI) is measured as the width of the space between the posterior cortex of the anterior arch of C1 and the anterior cortex of the dens on a lateral flexion radiograph when compared to neutral position [1]. An AADI greater than three millimeters in older children and adults or four millimeters in younger children is considered abnormal [14, 15].
Orthotopic os odontoideum with instability was previously described [4, 16, 17] and the shape of the ossicle was shown to correlate with the degree of myelopathy, greater for patients with a round type than those with cone or blunt-tooth types [16]. Although there are no management standards for treatment of os odontoideum [11], surgical fusion of C1–C2 is generally reserved for active or athletic patients in whom there is a presumed greater risk of sustaining an injury, or for patients with persistent and/or increasing neurological deficits [18, 19].
In conclusion, os odontoideum is an important consideration for patients with imaging abnormalities at C1-C2. When acute cervical spine trauma is imaged, os odontoideum must be distinguished from an acute dens fracture. In cases of cervical cord myelopathy, a multimodality imaging approach that includes CT, MRI, and radiography may be used to identify an os odontoideum and assess the degree of atlantoaxial instability.
References
Harris JH, Mirvis SE (1995) The Radiology of Acute Cervical Spine Trauma. Baltimore. Lippincott, Williams& Wilkins, Baltimore
Granger DK, Rechtine GR (1987) Os odontoideum–a review. Orthop Rev 16:909–916
Sherk HH, Dawoud S (1981) Congenital os odontoideum with Klippel-Feil anomaly and fatal atlanto-axial instability. Report of a case. Spine 6:42–45
Fielding JW, Hensinger RN, Hawkins RJ (1980) Os Odontoideum. J Bone Joint Surg Am 62:376–383
Kirlew KA, Hathout GM, Reiter SD, Gold RH (1993) Os odontoideum in identical twins: perspectives on etiology. Skelet Radiol 22:525–527
Morgan MK, Onofrio BM, Bender CE (1989) Familial os odontoideum. Case report. J Neurosurg 70:636–639
Fielding JW, Griffin PP (1974) Os odontoideum: an acquired lesion. J Bone Joint Surg Am 56:187–190
Hukuda S, Ota H, Okabe N, Tazima K (1980) Traumatic atlantoaxial dislocation causing os odontoideum in infants. Spine 5:207–210
Verska JM, Anderson PA (1997) Os odontoideum. A case report of one identical twin. Spine 22:706–709
Dai L, Yuan W, Ni B, Jia L (2000) Os odontoideum: etiology, diagnosis, and management. Surg Neurol 53:106–108; discussion 108–109
(2002) Os odontoideum. Neurosurgery 50:S148–S155
Rybicki FJ, Ledbetter SM, Mulkern RV (2002) Comparing MRI pulse sequences for a specific clinical task. Emerg Rad 9:178–180
Ogden JA (1984) Radiology of postnatal skeletal development. XII. The second cervical vertebra. Skelet Radiol 12:169–177
Fielding JW, Hawkins RJ, Ratzan SA (1976) Spine fusion for atlanto-axial instability. J Bone Joint Surg Am 58:400–407
Swischuk LE (1999) Normal cervical spine variations mimicking injuries in children. Emerg Rad 1:299–306
Matsui H, Imada K, Tsuji H (1997) Radiographic classification of Os odontoideum and its clinical significance. Spine 22:1706–1709
Schuler TC, Kurz L, Thompson DE, Zemenick G, Hensinger RN, Herkowitz HN (1991) Natural history of os odontoideum. J Pediatr Orthop 11:222–225
Diebener J, Sundaram M (1994) Radiologic case study. Os odontoideum. Orthopedics 17:1083–1085
Spierings EL, Braakman R (1982) The management of os odontoideum. Analysis of 37 cases. J Bone Joint Surg Br 64:422–428
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vargas, T.M., Rybicki, F.J., Ledbetter, S.M. et al. Atlantoaxial instability associated with an orthotopic os odontoideum: a multimodality imaging assessment. Emerg Radiol 11, 223–225 (2005). https://doi.org/10.1007/s10140-005-0406-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-005-0406-3