Abstract
Swallowing is an organized bodily function that occurs in four phases and involves the fine coordination of 30 different pairs of nerves and muscles. Problems arise when there are structural and/or functional defects in this highly coordinated process. “Aspiration” refers to an inadvertent inhalation of oropharyngeal secretions/gastric contents below the level of the true vocal cords into the respiratory tract.
Almost half of healthy adults aspirate routinely during the night; however, several structural and functional abnormalities in the aerodigestive tract predispose certain populations to a higher risk. The elderly are especially vulnerable. Age-related structural abnormalities (such as cervical osteophytes, Zenker’s diverticulum, esophageal strictures) can interfere with normal swallowing and lead to aspiration. Furthermore, nursing home residents harbor potentially dangerous pathogens due to poor oral hygiene—that if aspirated can lead to pneumonia. Other high-risk groups include those with bowel dysmotility (bowel obstruction, scleroderma, etc.) or altered consciousness (seizure disorder, alcohol use, or other drug abuse). Aggressive use of acid-suppressive medications (PPIs, H2 receptor blockers) also increases risk for aspiration pneumonia, both in the community and in critically ill mechanically ventilated.
About 5–15% of all community-acquired pneumonia is secondary to aspiration and aspiration pneumonia carries a higher 30-day mortality when compared to other community-acquired pneumonias. A diagnosis requires a high index of suspicion and can be challenging. Diagnostic testing includes a bedside evaluation of swallowing, use of a modified barium swallow study, video fluoroscopic swallow study, or a flexible endoscopic evaluation of swallowing (FEES).
Aspiration can cause a wide variety of clinical syndromes including chemical pneumonitis, aspiration pneumonia, and adult respiratory distress syndrome (ARDS). It is important to differentiate aspiration pneumonitis from pneumonia—as the latter involves pathogenic bacteria and entails antimicrobial treatment. Unchecked aspiration often leads to chronic lung damage (diffuse aspiration bronchiolitis, refractory asthma, bronchiectasis, lipoid pneumonias, and even idiopathic pulmonary fibrosis).
All aspiration does not necessitate antimicrobial therapy and it is important to identify risk factors that predispose patients to a higher bacterial burden in the event of an aspiration (i.e., chronic alcoholism, bowel dysmotility, stroke). These patients are likely to benefit from timely initiation of empiric antimicrobial therapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Patient Question: What Controls Normal Swallowing and What Is “Aspiration”?
Answer to patient : Swallowing is a highly organized bodily function. A healthy adult can swallow up to 2000 times a day. Each act of swallowing involves the fine coordination of 30 separate pairs of nerves and muscles and is under both our voluntary (conscious) and involuntary control (controlled by central nervous system without our awareness). There are four separate stages of swallowing. The first stage allows the sensation of “taste” and involves the breakdown of food into smaller, more digestible, particles with the help of teeth (mechanical grinding) and enzymes that are released from salivary glands in the mouth (chemical digestion). These smaller digested food particles form a “food bolus” that is propelled by a forceful motion of the tongue to the back of the mouth (oropharynx). Up until this point swallowing is under conscious control. Further stages of swallowing are controlled by the central nervous system and are not under voluntary (conscious) control. The next, and most complex stage, involves movement of the epiglottis and voice box (larynx) into a position that prevents the food bolus from entering the lungs and is conducted with a coordination of muscles such that the “windpipe” is temporarily sealed off—preventing entry into the lungs. Once past this stage, food enters the esophagus and progresses to be digested further. As is clear, a miscoordination in any of these steps can lead to ineffective swallowing and “aspiration.”
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Normal healthy adults swallow ~30 times per hour while awake [1] and each act of swallowing lasts approximately 10+ seconds. Swallowing occurs in four phases and requires the fine coordination of more than 30 pairs of nerves and muscles [2, 3].
An initial “ oral phase ” is under voluntary control and is divided into the “preparatory ” and “propulsive ” stages. The preparatory stage accumulates the food within a closed chamber (oral cavity bound by lips anteriorly, hard palate superiorly, and pharyngeal wall posteriorly) to form a bolus. With the help of dentition and enzyme-rich saliva, food is broken down to smaller particles. It is during this phase that chemoreceptors, located on the tongue and the palate, detect taste and other aesthetics of food—leading to pleasure (or displeasure). During the “propulsive” phase the palate moves upwards to seal off the nasopharynx (preventing nasal regurgitation) and the tongue moves downwards, hence establishing a wide continuum between the oral and pharyngeal cavities. Then, with a forceful piston-like motion of the tongue, the food bolus is propelled into the oropharynx [2].
The “ pharyngeal phase ” is a reflexive (neural-mediated) and most complex stage of swallowing. With the nasopharynx sealed off, contraction of the superior constrictor muscles propagates the bolus downwards towards the upper esophageal sphincter (UES). The suprahyoid muscles pull the hyoid bone (and the larynx) up and outwards and the epiglottis rapidly flips downwards whereby allowing a temporary closure of the laryngeal vestibule for approximately 0.6–0.7 s during deglutition [2]. The cricopharyngeus muscle (makes up the UES) relaxes allowing the bolus to the next “ esophageal phase .” Esophageal peristalsis then moves the bolus downwards towards the lower esophageal sphincter (LES) which relaxes to allow food into the stomach.
Figure 17.1 depicts the four phases of swallowing.
Swallowing is finely coordinated with respiration in order to prevent aspiration, and swallowing is dominant over respiration in health. Physical closure of the laryngeal vestibule, as described above, and a temporary neural-mediated suppression of respiration (for about 0.5–1.5 s) [4] allow this to take place in a safe manner [4, 5] in healthy adults. Problems arise when there are structural and/or functional defects in this highly coordinated act.
“ Aspiration ” refers to the inadvertent inhalation of oropharyngeal secretions or gastric contents below the level of the true vocal cords and into the lower respiratory tract [6, 7]. Penetration is the term used to describe entry of food material into the larynx but above the vocal cords [7]. Aspiration is also distinct from regurgitation which implies a “reflux” of gastric contents into the esophagus and oropharynx without contamination of the lower respiratory tract.
Patient Question: What Are the Risk Factors That Predispose to Aspiration?
Answer to patient : Almost half of healthy adults routinely aspirate small volumes of oral or stomach contents (see questions 4 and 5 below) during sleep. Several important conditions and risk factors predispose patients to aspiration. Patients at risk can be divided into the young adult population versus a more elderly and dependent population.
Firstly, young adults with chronic conditions such as a seizure disorder, or those with gut motility (bowel movement) problems such as scleroderma (a condition that causes slow bowel movement), chronic constipation (such as cystic fibrosis patients), those with feeding tubes or others with drug or alcohol use and overdose problems, are more likely to aspirate.
It is perhaps easier to think of elderly patients in terms of those residing in the community versus those residing in nursing homes. In general increasing age is an independent risk factor for aspiration. With age, the body becomes frail, loses coordination, and may develop weaknesses such as outpouchings in the upper digestive tract that can “hide” or sequester food and later cause regurgitation (vomiting) of food leading to aspiration. Older patients also have a higher risk for having acid reflux disease (heartburn) that is associated with an increased risk for aspiration.
In particular, nursing home residents have poorer oral hygiene and have several potentially dangerous bacteria in their mouth that when aspirated lead to pneumonia. They are also more likely to suffer from disorders such as stroke, Parkinson’s disease, and dementia (memory loss)—all of which lead to their inability to safely carry out the act of swallowing.
Another important group of patients at risk for aspiration pneumonia are patients on long-term acid-suppressive medications (such as omeprazole, zantac). These medications work to suppress the acidic contents of the stomach in an attempt to prevent injury when acidic stomach contents reflux—however they also allow harmful bacteria to flourish within the stomach environment. Without stomach acid, these bacteria are more readily able to cause pneumonia after aspiration takes place.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Some degree of aspiration is inevitable—and even “normal.” As described in detail later in this chapter, almost half of healthy normal adults aspirate routinely during the night. However, several structural and functional abnormalities in the aerodigestive tract place certain populations at a higher risk for aspiration.
Amongst these, the elderly are an especially high-risk group. They may be further subdivided into those living independently in the community, and those who are institutionalized.
For elderly patients living in the community, a risk for aspiration may stem partly from the physical age-related changes that take place in the human body. Structural abnormalities such as cervical osteophytes (bony outgrowths of the vertebra indenting the oropharyngeal tract) [8], Zenker’s diverticula (pharyngeal outpouching representing weakened muscular spots) [9], and esophageal strictures and webs [10] can lead to misdirection of the food bolus and hence aspiration. Gastroesophageal reflux disease (GERD) is also more common in the elderly and increasing age correlates with the severity of GERD and its complications (erosive esophagitis, Barrett’s esophagus) [6, 11].
To demonstrate this increased risk, Kikuchi et al. studied 14 otherwise healthy elderly patients (averaging 77 years) hospitalized with community-acquired pneumonia and compared their aspiration events with age-matched controls without pneumonia. They concluded that elderly patients hospitalized with community-acquired pneumonia were seven times more likely to have aspirated than their age-matched controls (71 vs. 10%) [12]. Other studies too have correlated increasing age (independent of neurological disease) with a higher incidence of impaired oropharyngeal deglutition [13]. Based on these observations, one may argue that age (and associated physiological changes in the body) alone is a risk for aspiration [14].
Institutionalized elderly patients are a different story. They are reported to suffer from poor oral hygiene and care [15, 16] and harbor serious pathogens (Enterobacteriaceae, Pseudomonas aeruginosa, and Staphylococcus aureus) in their oral cavity [6]. In a study on the dental health of patients living in 55 residential homes in the United Kingdom, large numbers of patients were found to have an increased incidence of oral ulcers, glossitis, and coronal and root caries [16]. Consequently, improving oral care is shown to reduce the incidence of pneumonia by almost one and a half times in such groups [17].
The institutionalized elderly are also more likely to suffer from neurological complaints or use of medications that impair swallowing. An interesting study of 1946 patients found that 10% of patients with community-acquired pneumonia and 30% of patients with continuing-care facility (CCF)-associated pneumonia were due to aspiration [18]. Amongst the CCF-pneumonia group, as many as 72.4% of patients had dysphagia secondary to a neurological disease (i.e., stroke, dementia, multiple sclerosis, mental retardation, brain tumors, movement, Parkinson’s disease, and Alzheimer’s disease) that posed a risk for their aspiration. In addition many of the CCF patients were taking centrally acting medications that could cause sedating or xerogenic (drying) effects reducing salivary flow [18]. Depending on the methods used, up to 78% of patients who have had a stroke exhibit dysphagia and may aspirate at least in the acute phase after a CVA [19].
For adults with community-acquired pneumonia it appears that factors that lead to an altered or a decreased level of consciousness (i.e., alcohol use, 12.9%; drug overdose, 21.3%; or hepatic encephalopathy 7.7%) are the main risk factors leading to aspiration [18, 20].
Other risk factors in the community affecting all ages include the aggressive use of acid-suppressive medications (such as proton pump inhibitors (PPIs) and H2 receptor blockers). Approximately 40–70% of medical inpatients receive acid-suppressive medications and as many as 50% are new prescriptions. PPIs are linked with an almost 1.5–1.89 times higher risk for community-acquired pneumonia [21, 22]. In a large hospital-based epidemiological cohort, use of PPIs was associated with 30% increased odds of hospital-acquired pneumonia (HAP) in non-ventilated patients and this risk was highest within the first few days to a week of PPI use [23]. Acid suppression allows survival of bacterial pathogens (that would normally be killed in acidic contents). Reflux and further aspiration events allow these pathogenic bacteria to find their way into the lungs and cause infection.
This risk from acid suppression has also been demonstrated in critically ill, mechanically ventilated patients. In a randomized controlled trial, patients were assigned to use of sucralfate, antacid, or H2 receptor blocker use. The group with sucralfate use was demonstrated to have significantly lower rates of gastric colonization and late-onset pneumonia (4 days later) when compared to the antacid and H2 blocker groups [24]. These data support the hypothesis that suppression of gastric pH leads to higher rates of gastric bacterial colonization and higher rates of hospital-acquired pneumonia [25] and current guidelines recommend against use of stress ulcer prophylaxis in patients without a clear indication for their use [26].
Patient Question: How Common Are Aspiration and Aspiration Pneumonia?
Answer to patient : As described earlier, small-volume aspiration takes place routinely in almost half of healthy normal adults. About 15% of patients in the community setting develop pneumonia as a result of aspiration and aspiration pneumonia is associated with worse survival than other community-acquired pneumonias .
Larger volume aspiration pneumonia is also the second most common reason for nursing home patients to require admission to a hospital and is the leading cause of death in this group of patients. Aspiration complicates 1 of every 3000 cases of general anesthesia and continues to be not only a significant financial burden on health care costs but also associated with high rates of death.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Aspiration is very common and can occur in both health and disease. The incidence depends on the methods used to detect aspiration, with some sensitive techniques detecting clinically insignificant “microaspirations ” while others (e.g., swallow studies) identifying larger boluses of material passing the vocal cords (see question 4 for details). Huxley et al. studied aspiration in 20 normal and 10 patients with depressed consciousness by injecting indium131 chloride (radioactive tracer) via a catheter directed into their nasopharynx. Radioactive tracer uptake was seen on post-sleep lung scans (as evidence of nocturnal aspiration) in 45% (9 out of 20) of healthy subjects and 7 out of 10 (70%) patients with depressed consciousness during sleep [20].
In a similar experiment, Gleeson et al. also studied aspiration events in ten healthy adults using radioactive tracer uptake in lungs and sleep patterns using sleep polysomnography over two separate nights [27]. Radioactive tracer solution was instilled in the nasopharynx of all subjects during nocturnal sleep. Although no particular sleep behavior (time spent in bed, sleep efficiency, supine sleep time, etc.) was associated with a higher risk, it was demonstrated that 5 of 10 (50%) healthy subjects silently aspirate on at least one of every two nights while asleep.
However, as described earlier, certain populations are much more likely to aspirate and suffer from clinical consequences of this aspiration.
Epidemiological studies indicate that approximately 5–15% of all community-acquired pneumonia is secondary to aspiration [6]. Aspiration pneumonia has a significantly higher 30-day mortality (21%) when compared to community-acquired pneumonia and patients are more likely to be admitted to the intensive care unit (ICU) and require mechanical ventilation [28].
Aspiration pneumonia has been reported to be the second most frequent principal diagnosis amongst Medicare patients [29]. Amongst nursing home residents aspiration pneumonia is the second most common infection (21%) after urinary tract infections, has an annual incidence of new cases between 18 and 48%, and has a higher mortality rate than that of any other nosocomial infection [30].
Aspiration is also well recognized as a complication of general anesthesia occurring in 1 of every 2000–3000 cases in adults [31]. Anesthetic agents can suppress airway protective reflexes and predispose patients to aspiration. Aspiration pneumonia accounts for as many as 10–30% of all deaths associated with anesthesia [6, 32].
It comes as no surprise that “aspiration pneumonia” is considered by some to be an epidemic. Admission rates and health care costs for patients with the diagnosis have risen rapidly. Aspiration pneumonia is associated with longer hospital stays (mean increase of 9 days), increased total hospital charges (mean increase of $22,000), higher ICU admission rates (odds ratio 4.0), and a higher in-hospital mortality (OR; 7.6) [30, 33].
Patient Question: What Are the Symptoms of Aspiration and How Is It Diagnosed?
Answer to patient : Some aspiration has no signs or symptoms, and thus is called “silent.” When present, symptoms of aspiration can range from subtle, unexplained coughing that persists over several weeks to wheezing similar to that seen in asthma. Choking may be obvious when a patient eating suddenly develops breathing difficulty and distress for no other clear reason. Aspiration may occur in small amounts ( microaspiration ) and go unwitnessed or be obvious when a patient actively vomits and inhales contents into his/her lungs ( macroaspiration ).
Bedside swallow evaluations can be performed by trained speech specialists, nurses, and physicians. Concerning signs include drowsy mental state or a cough brought on with swallowing. While very helpful in directing therapy when positive, bedside measures can be falsely reassuring when negative and should be followed with more advanced testing when suspicion for aspiration is high. Advanced tests can be conducted in the presence of a speech therapist and a radiologist and involve recording a video while observing a patient swallow. Direct observation of swallowing allows a much closer look at the problem and can also help with real-time feeding with different consistencies and food types to observe which foods and which swallowing techniques make swallowing safest for the patient.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Aspiration may be asymptomatic (silent or unwitnessed) or symptomatic (micro- or macroaspiration). Microaspiration refers to aspiration of small amounts of gastric contents or oropharyngeal secretions (usually <1 mL). Macroaspiration , on the other hand, refers to the visible aspiration of large amounts of bowel or gastric contents [7]. Signs of acute aspiration include sudden choking, shortness of breath, or chest pain while eating. Most adults, however, are likely to have subtle symptoms—such as a chronic unexplained cough or wheezing.
A diagnosis of aspiration pneumonia requires a high index of suspicion and can be challenging.
Historically bedside evaluation of swallowing has evolved from the care of patients suffering from stroke and resultant dysphagia [19].
A direct observation of swallowing; special attention to certain indicators of altered swallowing such as decreased consciousness, dysarthria, coughing, or choking while eating; and presence of a weak and delayed cough in response to aspiration can alert the physician to a potential problem. However, bedside evaluations are insensitive [6, 34]. In a study by Smithard et al., bedside clinical assessment had a sensitivity of only 47–70% (depending on who performed the assessment) and missed approximately 30–53% aspirators [34]. Such patients are likely to silently aspirate (without any overt signs of distress) and evaluation of ineffective swallowing for these patients must be combined with objective instrumental tests.
A modified barium swallow study (MBSS) or video fluoroscopic swallow (VFS) is a noninvasive test that reviews the oral, pharyngeal, and cervical esophageal stages of swallowing while the patient is upright and swallowing varying consistencies of barium-coated or water-soluble contrast mediums. This test is performed by speech therapists in conjunction with radiologists who acquire a video of swallowing to help elucidate a physiological reason for dysfunctional swallowing. This test has been traditionally considered a gold standard for diagnosing dysphagia .
A barium swallow is conducted by the radiologist while the patient is upright or, less commonly, supine. The esophageal phase of swallowing is observed for any structural or motility etiologies as a causation of aspiration.
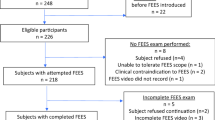
FEES (or flexible endoscopic evaluation of swallowing ) was first described in 1988 by Langmore et al. [35]. This modality can be performed by a trained speech therapist and involves viewing the oropharyngeal and laryngeal phases of swallowing via a nasally inserted laryngoscope. A FEES has several parts to it. First a preliminary assessment of anatomy is conducted and the movement of structures inside the mouth in response to secretions, etc. is observed. The second part includes observing the patient to swallow meals of varying consistencies and bolus sizes of liquids and solids. This allows the examiner to try several different combinations of consistencies and volumes and different strategies to determine which is handled best by an individual patient. Laryngeal penetration (appearance of contrast in the laryngeal vestibule) and aspiration (food below the vocal cords) can be identified using this technique. The esophageal phase cannot be assessed using this technique. This test is portable and can easily be conducted in the patient’s home environment with family/caregiver participation [14].
Lastly, esophagogastroduodenoscopy (EGD) is an invasive test that can be performed by a gastroenterologist and can help identify mucosal and other structural abnormalities along the esophageal tract.
Studies evaluating the consistency of results using FEES versus video fluoroscopy (VFS/modified barium swallow (MBSS) suggest a great degree of agreement between the two tests. A study on 21 patients by Langmore et al. [36] evaluating four features (aspiration, penetration, spillage, and residue) concluded that FEES agreed with the results of video fluoroscopy in 90% of cases (sensitivity 0.88, specificity 0.5, positive predictive value 0.69, negative predictive value 0.63). In general both tests complement one another and are considered “therapeutic” in that they allow a greater patient feedback during the test and real-time modification of behavioral strategy and bolus type—in order to achieve the most effective, safest swallowing. FEES may be considered superior for patients with severe dysphagia who have not had any oral intake for several weeks [14].
Patient Question: What Can Happen to Me as a Result of Aspiration?
Answer to patient : Harmful effects of aspiration depend on the amount and nature of the materials aspirated. Aspiration of acidic liquid stomach contents can lead to an inflammation of the smaller airways that presents with wheezing and shortness of breath—very similar to the tell-tale signs of asthma.
Aspiration of solid contents such as solid foreign objects can lead to a blockage of one of the main or central airways leading to asphyxiation or choking. Aspiration of a foreign object is considered a medical emergency as it can lead to death. It requires urgent steps to remove the aspirated materials. Recently aspirated iron tablets or potassium pills have become a focus of attention as these are particularly corrosive (causing chemical burn) and can seriously damage the lining of the airways. If a foreign object is not promptly removed, it can lead to long-term problems of causing stenosis (narrowing) of the bronchial tubes as well as formation of fistulae (abnormal connection between the lungs and other organs) that are extremely difficult to repair and treat.
As explained later in this chapter, the majority of patients who aspirate have no signs or symptoms or develop pneumonia. Some patients have repeated aspiration, and large amounts of bacteria in their oral cavity. Patients whose immune systems are otherwise depressed are more likely to develop pneumonia after aspiration.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Aspiration can result in several different clinical syndromes—and pH and volume of aspirated contents are critical determinants of the degree of lung injury [6, 37]. Both micro- and macroaspiration can result in immediate and long-term injury to the lungs.
Some acute consequences of aspiration include aspiration pneumonitis, aspiration pneumonia, and asphyxiation (or choking).
Aspiration or chemical pneumonitis (also known as Mendelson’s syndrome ) was described in 1946 while observing obstetric patients undergoing general anesthesia. Patients suffered from an acute asthma-like reaction likely from aspiration of liquid contents. By instilling 0.1 N hydrochloric acid into rabbit lungs, Mendelson elicited a pattern of lung injury similar to that seen in humans and highlighted the importance of acidic gastric contents in causing acute lung injury or pneumonitis [38]. Since then several experiments have shown that neutralizing acidic contents of aspirate can mitigate the extent of lung injury [6]. Most authors agree that a volume of more than 20–25 mL and a pH less than 2.5 are critical to causing chemical pneumonitis in adults [6, 37,38,39]. Studies in rats have demonstrated this to be a biphasic process. There is an initial phase of intense direct chemical burn from acidic contents causing increased capillary permeability and leakage—followed by a quiescent period over the next 2–3 h. At 4 to 6 h an aggressive neutrophilic response peaks and the release of inflammatory mediators leads to lung injury much like the adult respiratory distress syndrome (ARDS) [37].
It is important to differentiate aspiration pneumonitis from pneumonia—as the latter involves pathogenic bacteria development of a distinct radiographic infiltrate in a patient at risk for aspiration and entails antimicrobial therapy.
Table 17.1 depicts differentiating points between aspiration pneumonia and pneumonitis .
In general a bacterial infection is not thought to play a primary role early in the process of aspiration as acidic contents suppress gastric flora. During silent aspiration adults aspirate volumes in the range of 0.01–0.2 mL [27] and although this may introduce bacteria in sufficient amounts (104–105 organisms per milliliter) [27, 40] host defenses are usually able to combat disease. Bacterial infection (aspiration pneumonia) develops in situations where host defenses are compromised (impaired glottis closure, cough reflex, acid suppression with medications, impaired ciliary clearance, depressed humoral or cell-mediated immunity) or when a bacterial inoculum is large and deleterious enough to overwhelm defenses [6].
Aspiration of solid components (foreign-body aspiration or FBA) is more common in children and adults with advanced age. In 2014, approximately 4864 people died from choking in the United States and 2751 of them were over the age of 75 [41]. Acute aspiration of a large FB into a central airway can result in asphyxiation and even death—and requires immediate intervention to relieve obstruction. Depending on the size, type, and location of aspirated contents patients can develop serious long-term consequences such as recurrent post-obstructive pneumonias, hemoptysis, and bronchial stenosis from chronic obstruction. Pills (iron and potassium chloride tablets in particular) are being increasingly recognized for causing extensive chemical burn and inflammation in the bronchial epithelium [42, 43].
Patient Question: What Are the Long-Term Consequences of Aspiration?
Answer to patient : Unfortunately, aspiration can harm us in both the short and the long term. The chronic, repetitive damage from inhalation of acidic stomach contents and bacteria can lead to chronic lung conditions such as bronchiectasis. Bronchiectasis refers to an abnormal enlargement (dilation) of the smaller airways that leads to a difficulty in clearing mucus and secretions. This in turn can become a nidus for infections.
Patients with untreated or inadequately treated aspiration pneumonia can develop a lung abscess , a known complication of aspiration. Signs and symptoms of a lung abscess can include unexplained fevers, foul-smelling breath, chest pain, etc.
Importantly, aspiration is being linked to the development of lung fibrosis (also known as idiopathic pulmonary fibrosis or IPF ) and it is possible that early control and treatment of aspiration can lead to an improved survival in this formidable disease.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Aspiration can be injurious in both the short and the long term. While acute effects of macroaspiration are usually self-evident and can be addressed promptly (i.e., choking or acute bronchopneumonia)—the effects of chronic microaspiration may be more occult and a diagnosis may be missed until late into disease progression.
Microaspiration is a repetitive and insidious insult that is shown to cause lung damage in the form of diffuse aspiration bronchiolitis [44], bronchiolitis obliterans in lung transplant recipients [45, 46], refractory asthma [47], bronchiectasis [46, 48], lipoid pneumonia [49], and idiopathic pulmonary fibrosis [50]. Some of these chronic effects are reviewed below.
Exogenous lipoid pneumonia can develop from the inhalation of animal or vegetable oils—such as mineral oil (laxatives), petroleum-based lubricants, and decongestants (Vaseline (Unilever), Vicks VapoRub, or lip gloss). Clinical presentation may include a dry cough, dyspnea, fever, or unexplained weight loss and radiographic findings range from subtle ground-glass opacities to dense consolidation and a “crazy-paving” pattern. A CT evidence of fat attenuation (−30 HU (Hounsfield units)) within areas of consolidation is considered to be pathognomonic for this process [49]. Patients may have undergone several rounds of antibiotics without improvement for a non-resolving pneumonia before an accurate diagnosis is made. Therefore a high clinical suspicion, familiarity with clinical situations that predispose patients (i.e., patients with chronic constipation likely to be using mineral oils), and an awareness of key radiographic findings are critical to making an accurate and timely diagnosis. Long-standing inflammation can lead to secondary fibrosis and result in end-stage lung disease, even cor pulmonale.
In a study on 25 patients, Cardasis et al. [46] reviewed histological specimens from patients with chronic occult aspiration and demonstrated that recurrent bronchiolitis (multi-lobar, centrilobular nodules and tree-in-bud appearance), persistent patchy pneumonias with fat attenuation (lipoid), and bronchiolar thickening were some of the most common changes seen with aspiration. Severe and chronic cases developed frank bronchiectasis and fibrosis, and on histology, poorly formed granulomas, exogenous lipoid pneumonia, and foreign body-type multinucleated giant cells with or without foreign material were seen. The authors highlighted that lower lobe distribution alone should not be relied upon to “rule in” a diagnosis of aspiration as almost 73% of patients in this study had upper lobe involvement. They also emphasized that occult aspiration should not only be considered in the differential of chronic fibrotic interstitial pneumonitis (i.e., idiopathic pulmonary fibrosis (IPF), nonspecific interstitial pneumonitis (NSIP), hypersensitivity pneumonitis (HP)) but also especially in the case of an undifferentiated ILD with histological evidence of poorly formed granulomas.
Importantly, there is considerable ongoing debate surrounding the association of microaspiration and idiopathic pulmonary fibrosis (IPF). Although there is no direct evidence that microaspiration causes IPF , studies have identified an association between risk factors for aspiration, such as GERD, and advanced lung disease.
It has been shown that GERD is associated with aspiration [51], chronic cough [52], and aspiration-related lung injury [6, 53, 54]. Newer studies also reveal a high prevalence of GERD (almost 67–88%) amongst patients with IPF [53, 55, 56]. If left untreated, GERD can lead to allograft rejection and bronchiolitis obliterans syndromes amongst lung transplant recipients [45, 57]—all of which are considered unfortunate rate-limiting steps in the survival of lung transplant recipients. It is hence not surprising that aggressive treatment of reflux alone is shown to achieve clinical stability in the form of reduced oxygen dependence [58], reduced rate of lung function decline [56], and improved survival [59] amongst IPF and lung transplant populations.
Despite these advances—there are many unanswered questions regarding the role of aspiration and lung fibrosis. Does microaspiration cause IPF or does IPF cause microaspiration? Does microaspiration lead to acute exacerbations of IPF ? Studies on surrogate markers for aspiration such as reflux disease help to extrapolate that chronic microaspiration is perhaps one of the many pathogenic mechanisms for the development and progression of IPF . It is clear, however, that much work still remains to be done.
Patient Question: Do I Need Antibiotics for Aspiration?
Answer to patient : It is important to recognize that not all aspiration events require antimicrobial therapy. In fact, an overuse of antibiotics over the last era has led to significant problems of drug-resistant infections and other antibiotic -associated side effects. Hence both physicians and patients need to be very careful when prescribing or taking antibiotics.
Many initial aspiration events are simply an inhalation of gastric acid and a “chemical burn” of the lung tissue. This can lead to a range of responses spanning the spectrum from a complete lack of symptoms (asymptomatic) to an intense inflammatory reaction that leads to fever, cough, low oxygen measurements, and distress. Most patients recover from this initial episode with the help of oxygen and supportive care. However a smaller group of patients do not improve immediately and may require artificial respirators (mechanical ventilators) to support their breathing until their lung injury resolves. With time and supportive measures most patients completely recover from this injury.
Physicians are trained to recognize which patients are at a higher risk for a bacterial infection after an aspiration event. For example, residents of nursing homes (who may be unable to perform their own oral cares) or elderly patients who suffer from a stroke or younger adults with a history of seizures or alcohol/drug use are also more likely to have harmful bacteria in their mouth that can soil their lungs during an aspiration. It is these patients who should be identified as they may benefit from a timely use of antibiotics in the event of an aspiration.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
All aspiration does not necessitate antimicrobial therapy , and as elaborated earlier, a bacterial infection is usually not considered a primary event early in the course of an aspiration.
It is simpler perhaps to think of aspiration as potentially leading to one of the three injurious and separate clinical syndromes [60]:
-
Chemical pneumonitis (chemical “burn” or injury)
-
Primary bacterial pneumonia
-
Secondary bacterial pneumonia
Chemical injury can cause no symptoms or precipitate a dramatic clinical deterioration with the onset of fevers, cough, severe hypoxemia, and new radiographic infiltrates (upper or lower lobes depending on the position during which aspiration takes place) [6, 32]. However a large majority of patients (~ 60%) undergo complete resolution of hypoxemia and radiographic infiltrates within 2–4 days of the initial insult [60, 61]. These patients demonstrate an inflammatory reaction to a pure chemical injury [6, 62] and good supportive care (airway clearance therapy, supplemental oxygen, and positive pressure (if needed)) is usually sufficient to resolve their lung injury.
Not everyone is as fortunate. Up to 12% of patients are reported to die shortly after an acute aspiration event [61] and about 15–30% of patients develop an acute respiratory distress syndrome (ARDS) within the first 24–36 h from chemical injury alone [6, 54, 60]. These patients frequently have larger numbers of comorbid conditions and develop a very sudden and severe inflammatory reaction that causes pulmonary capillary leakage, development of proteinaceous edema, and severe hypoxemia necessitating mechanical ventilation (see Table 17.1). In clinical practice these patients benefit from empiric broad-spectrum antimicrobials up front—as intense chemical injury disrupts the integrity of the pulmonary capillary membranes, weakening host defenses and increasing the risk of nosocomial pneumonia [63].
A smaller subset of patients (~25%) undergo clinical worsening a few days after an initial improvement from chemical pneumonitis [60, 61]. These patients have developed a secondary bacterial pneumonia that is associated with a much higher mortality (~60%) [60, 61]. Prompt antimicrobial therapy is necessary and empiric agents should target the organisms that are likely to be acquired in the specific clinical setting. For example patients who suffer from an aspiration event within the health care setting (hospital, nursing homes, dialysis centers, etc.) are more likely to acquire resistant organisms like methicillin-resistant Staphylococcus aureus (MRSA) or resistant gram-negative rods such as Pseudomonas aeruginosa than patients who aspirate in the community setting [60].
A small proportion of patients develop a true bacterial pneumonia as a primary event during aspiration ( primary bacterial pneumonia ). To illustrate this, a study by Mier et al. revealed that only 19 out of 52 patients with aspiration pneumonia have bacterial pathogens in substantial counts (>1000 colony-forming units (CFUs/mL)) on respiratory sampling [64]. These patients inhale a bacterial burden sufficient enough to launch disease. In general primary aspiration pneumonia has all the features of any other bacterial pneumonia (fevers, cough, and foul-smelling sputum) but may be more indolent in onset than chemical pneumonitis .
Chemical pneumonitis can be difficult to differentiate from a primary bacterial pneumonia. The decision to initiate antimicrobials early in the course can be guided by knowledge of the actual aspiration event (i.e., a clearly witnessed macroaspiration or a questionable microaspiration) as well as awareness of the high-risk conditions that predispose patients to a large bacterial burden. For example patients suffering from seizure disorders, stroke, chronic alcoholism, esophageal dysmotility, severe constipation, or bowel obstruction [6, 65]; those using tube feedings/gastrostomy tubes [66], histamine H2 antagonists, or proton pump inhibitors; or elderly and nursing home patients who suffer from poor dentition and oral health—all are predisposed to a higher bacterial burden and appear to benefit from early empirical antibiotics after aspiration.
In general, the IDSA guidelines recommend the use of β-lactam/β-lactamase inhibitor combination or clindamycin as first-line agents for aspiration pneumonia (insert IDSA). There are no definite recommendations but in general a 7–10-day course can be employed for uncomplicated pneumonias.
The idea that all aspiration pneumonias involve anaerobic pathogens has been challenged and largely discounted. Data from the 1970s (when transtracheal aspirates were used for respiratory sampling) suggested that anaerobes played a central role in aspiration pneumonia [67]. Moreover, the risks of such “blind” antibiotic therapy have come to light [68] and have prompted a more judicious use of these agents. The medical community now agrees that most cases of aspiration pneumonia do not involve anaerobic pathogens and studies demonstrate good recovery without use of specific anti-anaerobe treatment [67, 69].
Several reviews have looked at risks in specialized populations for specific pathogens. For example elderly patients, in particular nursing home residents (receiving poor oral care) may be colonized with pathogens such as Enterobacteriaceae, Pseudomonas aeruginosa, and Staphylococcus aureus [6]. A study by El Solh et al. demonstrated a preponderance of gram-negative enteric bacilli as the predominant pathogen amongst nursing home patients who aspirated [69]. This study also concluded that, although the risk for anaerobic pathogens is probably overestimated, a poorer functional status correlates with a higher risk for anaerobic pathogens.
Hence according to the IDSA guidelines anaerobic coverage is only clearly indicated in patients with a classic pulmonary aspiration syndrome such as after a seizure event or stroke and alcohol or drug overdose, or in patients with aspiration with known gastroesophageal dysmotility syndromes or gingival disease (such as the elderly from nursing homes) [70]. In addition anaerobic coverage should be considered in patients with an indolent course, complicated pneumonias, putrid discharge, or necrotizing pneumonias or lung abscess formation [65].
Another important consideration includes aspiration events taking place in the hospital setting. The bacteriology of hospital-acquired pneumonia includes gram-negative flora (47%), Staphylococcus aureus (31%), and anaerobic bacteria (35%) [65]. Hence these aspiration events should include antimicrobials targeted against resistant gram negatives as well as an anti-staphylococcal agent [60].
When using anaerobic coverage, several studies have highlighted clindamycin as a superior agent, especially when a lung abscess is suspected [71]. Other agents such as metronidazole have anaerobic coverage but do not penetrate lung tissue as well and should be used in conjunction with a β-lactam/β-lactamase inhibitor.
Figure 17.2 presents an overview of empiric antimicrobial coverage in aspiration pneumonia .
Patient Question: What Can Be Done to Prevent Aspiration Pneumonia?
Answer to patient : Several steps can be taken to prevent aspiration in vulnerable patients. A bedside swallow evaluation can be performed by your health nurse or a physician. Advanced techniques (such as video fluoroscopy or FEES) can also help guide an assessment of this risk. Patients can be taught to use a “chin-tuck” or “head-tilt” approach or have thin liquids in a honey or nectar-thickened consistency to reduce aspiration. In addition, family and health care workers can be trained to identify those at a higher risk of aspiration such as patients with stroke, Parkinson’s disease, bowel movement disorders, or seizure disorders or the elderly who are unable to function on their own.
In some cases patients with advanced dementia (memory loss) and difficulty with swallowing ( dysphagia ) may benefit from the placement of a feeding tube (PEG; percutaneous endoscopic gastrostomy tube). PEG tubes help with a better, more consistent delivery of medications in these patients; however it is important to note that they do not reduce the risk of aspiration. Despite all attempts to minimize risks in this patient population, aspiration is frequently the immediate cause of death.
Patients who are on artificial respirators (mechanical ventilators) may have a higher rate of gastric acid reflux and this may increase their risk for aspiration. Several studies have now shown some things that can be implemented to reduce this risk. For instance, frequent oral cares provided by bedside nurses using antiseptics such as chlorhexidine or a ‘head-of-bed’ elevation while on a respirator can reduce the risk for developing pneumonia while on a respirator.
(1–2-min evidence-based reading for clinician): Epidemiology, genetics and pathophysiology, diagnostic test results, treatment options, etc.
Patients with dysphagia , stroke, abnormalities of the aerodigestive tract, etc. are at a much higher risk for aspiration. Once identified to be at a higher risk, several dietary and behavioral measures can be instituted to reduce the risk for aspiration [14]. Methods such as instituting a honey-thickened or nectar consistency of thin liquids have been shown to reduce the risk of aspiration amongst patients with dementia and Parkinson’s disease [72]. Other modifications such as keeping the chin tucked or reducing bite size may be helpful [6, 14].
Patients who continue to aspirate despite these measures may be candidates for placement of a feeding tube. It is important to note that although percutaneous gastrostomy (percutaneous endoscopic gastrostomy or PEG tube) placement is more effective in delivering oral medications and achieving prescribed nutrition in patients with dysphagia —several studies have now established that they do not reduce the risk or incidence of aspiration pneumonia in comparison with nasogastric or post-pyloric tubes [6, 73]. In fact treatment of chronic aspiration in patients particularly with altered mental status outside the acute care setting is difficult. A consequence of aspiration is the most common immediate cause of death in this patient population [74].
Patients who are mechanically ventilated and on enteral nutrition (with nasogastric tubes) are also at a higher risk for aspiration. These patients are consistently demonstrated to have a high incidence of GERD [6, 75] that promotes pneumonia by retrograde oropharyngeal colonization and aspiration into the lower airways. In addition, the presence of a NG tube impairs closure of the lower esophageal sphincter and further increases this risk. A randomized clinical trial on 86 intubated patients on enteral nutrition was interrupted early when it was clear that a semi-recumbent positioning, in comparison with supine positioning, substantially reduced the risk of a nosocomial aspiration pneumonia/ventilator-associated pneumonia (VAP) (3 of 39 [8%] vs. 16 of 47 [34%]; 95% CI for difference 10.0–42.0, p = 0.003) [76]. Hence head-of-bed elevation is a standard and relative inexpensive practice to reduce the risk of aspiration-related nosocomial pneumonias in mechanically ventilated patients.
Other factors such as suctioning of subglottic drainage and use of silver-coated endotracheal tubes have not been shown to be associated with a mortality benefit. Measurement of gastric volume does not correlate with aspiration risk and is associated with poorer caloric feeding due to frequent interruptions and is not routinely recommended [77]. Another trial looked at the role of instituting VAP bundle using five interventions: semi-recumbent position, stress ulcer prophylaxis, deep-vein thrombosis prophylaxis, adjustment of sedation so that the patient can follow command, and daily assessment for extubation—and demonstrated a substantial (71%) reduction in VAP rates amongst mechanically ventilated patients [78].
The risk of aspiration may be highest peri-extubation due to the lingering effects of sedative agents, laryngeal muscle edema, or injury and it is recommended that enteral nutrition be held at least 6 h after extubation in case of need for re-intubation and that diet be slowly progressed starting with pureed soft foods [6].
References
Crary MA, Carnaby GD, Sia I, Khanna A, Waters MF. Spontaneous swallowing frequency has potential to identify dysphagia in acute stroke. Stroke. 2013;44(12):3452–7.
Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154(5):953–63.
Jones B. Normal and abnormal swallowing: imaging in diagnosis and therapy. 2nd ed. New York: Springer; 2003. xviii, 287p
Nishino T, Hiraga K. Coordination of swallowing and respiration in unconscious subjects. J Appl Physiol (1985). 1991;70(3):988–93.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19(4):691–707. vii
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344(9):665–71.
Zaloga GP. Aspiration-related illnesses: definitions and diagnosis. JPEN J Parenter Enteral Nutr. 2002;26(6 Suppl):S2–7; discussion S-8.
Di Vito J. Cervical osteophytic dysphagia: single and combined mechanisms. Dysphagia. 1998;13(1):58–61.
Ferreira LE, Simmons DT, Baron TH. Zenker's diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus. 2008;21(1):1–8.
Ferguson DD. Evaluation and management of benign esophageal strictures. Dis Esophagus. 2005;18(6):359–64.
Soumekh A, Schnoll-Sussman FH, Katz PO. Reflux and acid peptic diseases in the elderly. Clin Geriatr Med. 2014;30(1):29–41.
Kikuchi R, Watabe N, Konno T, Mishina N, Sekizawa K, Sasaki H. High incidence of silent aspiration in elderly patients with community-acquired pneumonia. Am J Respir Crit Care Med. 1994;150(1):251–3.
Tracy JF, Logemann JA, Kahrilas PJ, Jacob P, Kobara M, Krugler C. Preliminary observations on the effects of age on oropharyngeal deglutition. Dysphagia. 1989;4(2):90–4.
Wirth R, Dziewas R, Beck AM, Clavé P, Hamdy S, Heppner HJ, et al. Oropharyngeal dysphagia in older persons - from pathophysiology to adequate intervention: a review and summary of an international expert meeting. Clin Interv Aging. 2016;11:189–208.
Castronuovo E, Capon A, Di Lallo D. Oral health of elderly occupants in residential homes. Ann Ig. 2007;19(5):463–72.
Simons D, Kidd EA, Beighton D. Oral health of elderly occupants in residential homes. Lancet. 1999;353(9166):1761.
Yoneyama T, Yoshida M, Matsui T, Sasaki H. Oral care and pneumonia. Oral Care Working Group. Lancet. 1999;354(9177):515.
Reza Shariatzadeh M, Huang JQ, Marrie TJ. Differences in the features of aspiration pneumonia according to site of acquisition: community or continuing care facility. J Am Geriatr Soc. 2006;54(2):296–302.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36(12):2756–63.
Huxley EJ, Viroslav J, Gray WR, Pierce AK. Pharyngeal aspiration in normal adults and patients with depressed consciousness. Am J Med. 1978;64(4):564–8.
Laheij RJ, Sturkenboom MC, Hassing RJ, Dieleman J, Stricker BH, Jansen JB. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA. 2004;292(16):1955–60.
Lambert AA, Lam JO, Paik JJ, Ugarte-Gil C, Drummond MB, Crowell TA. Risk of community-acquired pneumonia with outpatient proton-pump inhibitor therapy: a systematic review and meta-analysis. PLoS One. 2015;10(6):e0128004.
Herzig SJ, Howell MD, Ngo LH, Marcantonio ER. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA. 2009;301(20):2120–8.
Prod'hom G, Leuenberger P, Koerfer J, Blum A, Chiolero R, Schaller MD, et al. Nosocomial pneumonia in mechanically ventilated patients receiving antacid, ranitidine, or sucralfate as prophylaxis for stress ulcer. A randomized controlled trial. Ann Intern Med. 1994;120(8):653–62.
Eom CS, Jeon CY, Lim JW, Cho EG, Park SM, Lee KS. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011;183(3):310–9.
Spirt MJ, Stanley S. Update on stress ulcer prophylaxis in critically ill patients. Crit Care Nurse. 2006;26(1):18–20. 2-8; quiz 9
Gleeson K, Eggli DF, Maxwell SL. Quantitative aspiration during sleep in normal subjects. Chest. 1997;111(5):1266–72.
Lanspa MJ, Jones BE, Brown SM, Dean NC. Mortality, morbidity, and disease severity of patients with aspiration pneumonia. J Hosp Med. 2013;8(2):83–90.
Baine WB, Yu W, Summe JP. Epidemiologic trends in the hospitalization of elderly Medicare patients for pneumonia, 1991–1998. Am J Public Health. 2001;91(7):1121–3.
Langmore SE, Skarupski KA, Park PS, Fries BE. Predictors of aspiration pneumonia in nursing home residents. Dysphagia. 2002;17(4):298–307.
Janda M, Scheeren TW, Nöldge-Schomburg GF. Management of pulmonary aspiration. Best Pract Res Clin Anaesthesiol. 2006;20(3):409–27.
Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993;78(1):56–62.
Kozlow JH, Berenholtz SM, Garrett E, Dorman T, Pronovost PJ. Epidemiology and impact of aspiration pneumonia in patients undergoing surgery in Maryland, 1999–2000. Crit Care Med. 2003;31(7):1930–7.
Smithard DG, O'Neill PA, Park C, England R, Renwick DS, Wyatt R, et al. Can bedside assessment reliably exclude aspiration following acute stroke? Age Ageing. 1998;27(2):99–106.
Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988;2(4):216–9.
Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991;100(8):678–81.
Kennedy TP, Johnson KJ, Kunkel RG, Ward PA, Knight PR, Finch JS. Acute acid aspiration lung injury in the rat: biphasic pathogenesis. Anesth Analg. 1989;69(1):87–92.
Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anesthesia. Am J Obstet Gynecol. 1946;52:191–205.
Teabeaut JR. Aspiration of gastric contents; an experimental study. Am J Pathol. 1952;28(1):51–67.
Onofrio JM, Toews GB, Lipscomb MF, Pierce AK. Granulocyte-alveolar-macrophage interaction in the pulmonary clearance of Staphylococcus aureus. Am Rev Respir Dis. 1983;127(3):335–41.
National. Choking Prevention and Rescue Tips 2016. http://www.nsc.org/learn/safety-knowledge/Pages/safety-at-home-choking.aspx.
Kim ST, Kaisar OM, Clarke BE, Vandenburg RA, Allen DH, Bell SC, et al. ‘Iron lung’: distinctive bronchoscopic features of acute iron tablet aspiration. Respirology. 2003;8(4):541–3.
Mehta AC, Khemasuwan D. A foreign body of a different kind: pill aspiration. Ann Thorac Med. 2014;9(1):1–2.
Matsuse T, Oka T, Kida K, Fukuchi Y. Importance of diffuse aspiration bronchiolitis caused by chronic occult aspiration in the elderly. Chest. 1996;110(5):1289–93.
D'Ovidio F, Mura M, Tsang M, Waddell TK, Hutcheon MA, Singer LG, et al. Bile acid aspiration and the development of bronchiolitis obliterans after lung transplantation. J Thorac Cardiovasc Surg. 2005;129(5):1144–52.
Cardasis JJ, MacMahon H, Husain AN. The spectrum of lung disease due to chronic occult aspiration. Ann Am Thorac Soc. 2014;11(6):865–73.
Sontag SJ, Schnell TG, Miller TQ, Khandelwal S, O'Connell S, Chejfec G, et al. Prevalence of oesophagitis in asthmatics. Gut. 1992;33(7):872–6.
McShane PJ, Naureckas ET, Tino G, Strek ME. Non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2013;188(6):647–56.
Betancourt SL, Martinez-Jimenez S, Rossi SE, Truong MT, Carrillo J, Erasmus JJ. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. AJR Am J Roentgenol. 2010;194(1):103–9.
Lee JS, Collard HR, Raghu G, Sweet MP, Hays SR, Campos GM, et al. Does chronic microaspiration cause idiopathic pulmonary fibrosis? Am J Med. 2010;123(4):304–11.
Ravelli AM, Panarotto MB, Verdoni L, Consolati V, Bolognini S. Pulmonary aspiration shown by scintigraphy in gastroesophageal reflux-related respiratory disease. Chest. 2006;130(5):1520–6.
Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):80S–94S.
Sweet MP, Patti MG, Hoopes C, Hays SR, Golden JA. Gastro-oesophageal reflux and aspiration in patients with advanced lung disease. Thorax. 2009;64(2):167–73.
Raghavendran K, Nemzek J, Napolitano LM, Knight PR. Aspiration-induced lung injury. Crit Care Med. 2011;39(4):818–26.
Tobin RW, Pope CE, Pellegrini CA, Emond MJ, Sillery J, Raghu G. Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998;158(6):1804–8.
Raghu G, Freudenberger TD, Yang S, Curtis JR, Spada C, Hayes J, et al. High prevalence of abnormal acid gastro-oesophageal reflux in idiopathic pulmonary fibrosis. Eur Respir J. 2006;27(1):136–42.
Belperio JA, Weigt SS, Fishbein MC, Lynch JP. Chronic lung allograft rejection: mechanisms and therapy. Proc Am Thorac Soc. 2009;6(1):108–21.
Linden PA, Gilbert RJ, Yeap BY, Boyle K, Deykin A, Jaklitsch MT, et al. Laparoscopic fundoplication in patients with end-stage lung disease awaiting transplantation. J Thorac Cardiovasc Surg. 2006;131(2):438–46.
Lee JS, Ryu JH, Elicker BM, Lydell CP, Jones KD, Wolters PJ, et al. Gastroesophageal reflux therapy is associated with longer survival in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;184(12):1390–4.
Daoud E, Guzman J. Q: are antibiotics indicated for the treatment of aspiration pneumonia? Cleve Clin J Med. 2010;77(9):573–6.
Bynum LJ, Pierce AK. Pulmonary aspiration of gastric contents. Am Rev Respir Dis. 1976;114(6):1129–36.
Folkesson HG, Matthay MA, Hébert CA, Broaddus VC. Acid aspiration-induced lung injury in rabbits is mediated by interleukin-8-dependent mechanisms. J Clin Invest. 1995;96(1):107–16.
Delclaux C, Roupie E, Blot F, Brochard L, Lemaire F, Brun-Buisson C. Lower respiratory tract colonization and infection during severe acute respiratory distress syndrome: incidence and diagnosis. Am J Respir Crit Care Med. 1997;156(4 Pt 1):1092–8.
Mier L, Dreyfuss D, Darchy B, Lanore JJ, Djedaïni K, Weber P, et al. Is penicillin G an adequate initial treatment for aspiration pneumonia? A prospective evaluation using a protected specimen brush and quantitative cultures. Intensive Care Med. 1993;19(5):279–84.
Bartlett JG, O'Keefe P, Tally FP, Louie TJ, Gorbach SL. Bacteriology of hospital-acquired pneumonia. Arch Intern Med. 1986;146(5):868–71.
Gomes GF, Pisani JC, Macedo ED, Campos AC. The nasogastric feeding tube as a risk factor for aspiration and aspiration pneumonia. Curr Opin Clin Nutr Metab Care. 2003;6(3):327–33.
Bartlett JG. How important are anaerobic bacteria in aspiration pneumonia: when should they be treated and what is optimal therapy. Infect Dis Clin N Am. 2013;27(1):149–55.
Donskey CJ, Chowdhry TK, Hecker MT, Hoyen CK, Hanrahan JA, Hujer AM, et al. Effect of antibiotic therapy on the density of vancomycin-resistant enterococci in the stool of colonized patients. N Engl J Med. 2000;343(26):1925–32.
El-Solh AA, Pietrantoni C, Bhat A, Aquilina AT, Okada M, Grover V, et al. Microbiology of severe aspiration pneumonia in institutionalized elderly. Am J Respir Crit Care Med. 2003;167(12):1650–4.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–72.
Perlino CA. Metronidazole vs clindamycin treatment of anerobic pulmonary infection. Failure of metronidazole therapy. Arch Intern Med. 1981;141(11):1424–7.
Logemann JA, Gensler G, Robbins J, Lindblad AS, Brandt D, Hind JA, et al. A randomized study of three interventions for aspiration of thin liquids in patients with dementia or Parkinson’s disease. J Speech Lang Hear Res. 2008;51(1):173–83.
Strong RM, Condon SC, Solinger MR, Namihas BN, Ito-Wong LA, Leuty JE. Equal aspiration rates from postpylorus and intragastric-placed small-bore nasoenteric feeding tubes: a randomized, prospective study. JPEN J Parenter Enteral Nutr. 1992;16(1):59–63.
Brunnström HR, Englund EM. Cause of death in patients with dementia disorders. Eur J Neurol. 2009;16(4):488–92.
Orozco-Levi M, Torres A, Ferrer M, Piera C, el-Ebiary M, de la Bellacasa JP, et al. Semirecumbent position protects from pulmonary aspiration but not completely from gastroesophageal reflux in mechanically ventilated patients. Am J Respir Crit Care Med. 1995;152(4 Pt 1):1387–90.
Drakulovic MB, Torres A, Bauer TT, Nicolas JM, Nogué S, Ferrer M. Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trial. Lancet. 1999;354(9193):1851–8.
Reignier J, Mercier E, Le Gouge A, Boulain T, Desachy A, Bellec F, et al. Effect of not monitoring residual gastric volume on risk of ventilator-associated pneumonia in adults receiving mechanical ventilation and early enteral feeding: a randomized controlled trial. JAMA. 2013;309(3):249–56.
Berenholtz SM, Pham JC, Thompson DA, Needham DM, Lubomski LH, Hyzy RC, et al. Collaborative cohort study of an intervention to reduce ventilator-associated pneumonia in the intensive care unit. Infect Control Hosp Epidemiol. 2011;32(4):305–14.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Aqeel, M., Jacobs, E.R. (2018). Aspiration Pneumonia/Bronchitis. In: Bardan, E., Shaker, R. (eds) Gastrointestinal Motility Disorders . Springer, Cham. https://doi.org/10.1007/978-3-319-59352-4_17
Download citation
DOI: https://doi.org/10.1007/978-3-319-59352-4_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59350-0
Online ISBN: 978-3-319-59352-4
eBook Packages: MedicineMedicine (R0)