Abstract
Swallowing is a complex physiological event consisting of simultaneous and sequential coordinated contractions of the muscles of the orofacial, pharyngeal, laryngeal, and esophageal region. The videofluoroscopic swallowing study (VFSS) is a dynamic X-ray examination of the upper digestive tract considered the gold standard not only to assess swallowing function and disorders but also for planning the rehabilitation therapy and type of nutrition and for the results of the therapy evaluation. Dysphagia is a common clinical problem whose prevalence is increasing with the aging population in the whole world. Aspiration is the most severe form of swallowing disorders and is a common but underrecognized clinicopathologic entity; it may be clinically silent and have varied radiographic manifestations. The spectrum of aspiration-induced lung disease (AILD) imaging patterns must be known by both the radiologist and the clinician and managed in a multidisciplinary team. In dysphagic patient noninvasive ventilation (NIV) may have a beneficial impact on swallowing by making some strategies to ensure a good synchronization between ventilation and swallowing.
In this chapter, we will review the different types of aspiration lung diseases, focusing on their imaging features and differential diagnosis (DD).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Key Facts
-
Dysphagia and aspiration syndromes are strongly related.
-
Dysphagia and aspiration may be silent.
-
VFSS provides a comprehensive evaluation of the oral, palatal, pharyngeal, and pharyngoesophageal segments of deglutition.
Swallowing is an array of synergistic interdependent movements, initiated by a complex set of sensory inputs that generate pressures and forces for propelling ingested materials through the upper aerodigestive tract and simultaneously protect the upper airway [1].
Respiration and swallowing utilize a common passageway, and the two activities must be coordinated so that mutual compromise does not occur. A high degree of coordination between respiration and swallowing is required to maintain adequate ventilation without causing pulmonary aspiration [2]. In an advanced stage of neuromuscular disorders or multisystem diseases with respiratory muscle dysfunction, swallowing disorders due to deficiency of upper airway muscles are frequently observed and can lead to aspiration and malnutrition. Furthermore, dysphagia is an increasing problem with age (presbyphagia) and one of the most critical problems in patients with long-term, progressive congenital or acquired diseases (Table 1) [3].
Dysphagia and aspiration syndromes are strongly related, may be overt or silent, and lead to severe consequences, such as malnutrition, dehydration, pneumonia, or airway obstruction. Aspiration is defined as “the inhalation of oropharyngeal or gastric contents into the laryngeal or lower respiratory tract” [4]. A prompt assessment of the swallowing function is crucial to organize proper interventions and prevent complications in dysphagic patients. Dysphagic patients are 3 times, and those with confirmed aspiration 11 times, more likely to develop aspiration pneumonia [4]. Macroaspiration can cause a wide spectrum of airways/lung diseases with various clinical presentations and can be overt or silent, and its content can be variable (e.g., oropharyngeal or gastric).
Dysphagia is of great interest to radiologists because the dynamic radiological examination of swallowing, the videofluoroscopic swallowing study (VFSS), is considered the gold standard not only for a diagnostic purpose (helps to identify the causes of aspiration, often treatable) but also for planning the rehabilitation therapy and type of nutrition, and for the results of the therapy evaluation [5,6,7].
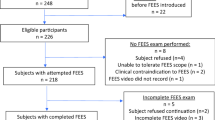
Since 1988 the fiber-optic endoscopic evaluation of swallowing (FEES) has appeared alongside VFSS and has become increasingly employed [8]. Due to availability, expertise needed, patient compliance, and the evolution of the swallowing disorder, sometimes rapidly progressive, an instrumental examination should be performed on every patient with suspected dysphagia. A better understanding of the swallowing problems associated with these disorders may help in guiding treatment, choosing technical aids, modifying the consistency of foods, swallowing rehabilitation, and nutritional support by the nonoral route.
Anatomic/Physiological Background and VFSS Technique
Eating, swallowing, and breathing are tightly functionally coordinated systems. Swallowing is a complex physiologic act consisting of simultaneous and sequential contractions of orofacial, pharyngeal, laryngeal, and esophageal muscles to propel ingested materials through the upper aerodigestive tract with simultaneous protection of the airways. It involves approximately 50 paired muscles and virtually all levels of the central nervous system (cerebral cortex, brain stem swallowing center, motoneurons, and sensory receptors in the oropharynx, larynx, and esophagus by cranial nerves V, VII, IX, X, XII).
Schematically, in normal swallowing, it is possible to distinguish (Fig. 1) the following:
-
An oral preparatory phase: the bolus is manipulated by lingual motion, mixed with saliva, and masticated, sized, shaped, and if necessary, also tasted or savored. All the actions of this phase are conscious and voluntary, the swallow reflex is absent, and the airway remains open for the usual purpose of respiration.
-
An oral propulsive phase: the tongue starts to squeeze the bolus between the soft palate and itself. A groove or channel becomes evident in the tongue, and its pressure conveys the food bolus posteriorly into the back of the mouth. As the bolus passes the posterior faucial pillars, the involuntary swallow reflex occurs [9].
-
A pharyngeal phase: five main physiologic events can be distinguished:
-
Nasopharyngeal seal
-
Elevation and anterior displacement of the larynx and hyoid bone
-
Laryngeal closure
-
Bolus compression and propulsion
-
Cricopharyngeal opening
-
-
An esophageal phase: a normal primary peristalsis as an aboral contraction wave that progressively obliterates the esophageal lumen is appreciable.
Pathophysiological Mechanisms of Dysphagia
Symptoms of dysphagia have been reported in about 60% of institutionalized elderly people [10]. The altered swallowing mechanism of elderly people is in part related to sarcopenia, the age-related loss of skeletal muscle mass, and can lead to diminishing lingual pressure, with consequent disorders in pharyngeal swallowing or to reduced pharyngeal constrictor muscle contractility with delay in pharyngeal transit.
Other two main pathophysiological mechanisms operate in these patients:
-
1.
The triggering of the swallowing reflex for the voluntarily initiated swallows is delayed, disordered, and eventually absent.
-
2.
The cricopharyngeal sphincter muscle of the pharyngoesophageal segment became hyper-reflexic and hypertonic.
Delayed bolus transit, palatal weakness predisposing to nasal regurgitation, decreased laryngeal elevation, and bolus residue after swallowing are other mechanisms that determine swallow impairment and aspiration. The weakness and the impaired coordination of facial, oral, and pharyngeal muscles compromise all the phases of swallowing [11]. As a result, the laryngeal protective system and the bolus transport system of deglutition lost their coordination during voluntarily initiated oropharyngeal swallowing.
Pathological VFSS Findings
Lateral (LL) and Anteroposterior (AP) Direct Neck Radiograph
Ideally all patients should be examined in both lateral and frontal (AP) positions. In the real life, the examination starts and ends only in latero-lateral (LL) projection with the bedside or wheelchair patient and should always begin with the assessment without contrast medium.
Laryngeal thyroid, cricoid, and most of the arytenoid are hyaline cartilages that undergo enchondral ossification over aging both in males and in females and may cause VFSS misdiagnosis.
VFSS on LL Projection
Latero-lateral projection best allows documentation of the contrast medium passage in the laryngeal vestibule (penetration) and/or in the trachea (aspiration). Small and then gradually increasing amounts of contrast medium of different texture are administered. This allows the radiologist to identify the food textures responsible for aspiration [12]. In more severe deficits, the contrast agent (barium, gastrografin) can be administered through a syringe connected to a tube placed in the oral cavity.
Aspiration-Induced Lung Disease (AILD)
Key Facts
-
Aspiration into the airways and lung can cause a wide spectrum of pulmonary diseases with various clinical presentations.
-
Aspiration-induced lung diseases are often underdiagnosed in the clinical setting.
-
Noninvasive ventilation may have a beneficial impact on these inhalational injuries.
Aspiration represents a broad spectrum of diseases, with patterns of tracheobronchial tree and lung injury that overlap, both pathologically and radiographically, finally leading to respiratory distress [13,14,15,16].
These patterns are determined by the aspirated content and volume, the chronicity, as well as host defenses (Table 2). Microaspiration, or silent aspiration, is commonly suspected in patients with refractory respiratory symptoms, including unexplained chronic cough, asthma, chronic obstructive pulmonary disease, bronchiolitis, bronchiectasis, and idiopathic pulmonary fibrosis. In very ill patients, inability to ventilate (diaphragm weakness and chest wall stifness) and decreased airflow velocity usually restrict secretion clearance, and decrease coughing limits airway clearance. On the past few years, the importance of cough augmentation and airway clearance has been increasingly recognized. Diagnostically, it may be helpful to distinguish respiratory disorders directly caused by macroaspiration, such as diffuse aspiration bronchiolitis (DAB), aspiration-related organizing pneumonia (OP), acute respiratory distress syndrome (ARDS), and exogenous lipoid pneumonia, from respiratory conditions in which microaspiration is more likely to play an indirect aggravating role, such as in chronic cough, asthma, chronic obstructive pulmonary disease (COPD), cystic fibrosis (CF), non-CF bronchiectasis, and idiopathic pulmonary fibrosis (IPF). Evaluation for aspiration-induced lung diseases (AILDs) usually entails visualization of the airways with laryngoscopy or bronchoscopy and pulmonary function testing. AILDs, such as aspiration pneumonitis, aspiration pneumonia, and exogenous lipoid pneumonia, are generally diagnosed by clinical and radiologic findings.
Aspiration Pneumonia (with or Without Abscess Formation)
Because of its low pH, gastric contents are sterile under normal conditions. Thus, aspiration is required but not sufficient for the formation of aspiration pneumonia that refers to an infectious process secondary to aspiration of colonized oropharyngeal secretions [17, 18]. It usually results in localized segmental or lobar airspace consolidations in dependent portions of lung, with or without an associated parapneumonic effusion. In supine patients, the material is most commonly aspirated into the right middle lobe, into the posterior segments of the upper lobes, or into the superior and posterior basal segments of the lower lobes. This primarily happens because of the larger caliber and more vertical course of the right main bronchus compared with the left [13, 19]. These secretions or food debris-filled airways cause airspace opacities that can become more confluent and appear as consolidation, with patent airways within these regions appearing as air bronchograms (Fig. 2).
Dysphagia after stroke and aspiration pneumonia. (a) Acute right MCA territory infarct in a 63-year-old man. (b) After 8 months at emergency department, a bedside CXR shows a lower right lobe consolidation in this patient with recurrent fever, chills, and productive cough. HRCT chest axial image (c) confirms lower right lobe consolidation. (d) VFSS shows posterior oral leakage, vallecular and sinus residue, and tracheal aspiration. Dysphagia affects more than 50% of stroke survivors. Fortunately, only 15–20% of these patients remain dysphagic after 6 months
Heterogeneous opacities on CXR and thin-slice CT usually represent small areas of atelectasis caused by distal airway obstruction by aspirated material [20]. Aspirated material can also be seen filling the airways, which is an important clue to the diagnosis. In normal individuals resolution is commonly observed within 24–48 h as mucociliary action and coughing clear the airways, and persistent opacities for more than 4–5 days suggest superimposed infection. In addition, depending on the bacterial contents of the aspirate, abscess formation, cavitation, or empyema may result. The differential diagnosis (DD) includes other causes of segmental or lobar consolidation, such as community-acquired pneumonia, pulmonary contusion or hemorrhage, or pulmonary infarct [20].
Aspiration Pneumonitis and Mendelson Syndrome
Aspiration pneumonitis is caused by the acute inhalation of a large volume of acidic gastric contents, resulting in chemical lung injury. A cascade of inflammatory response follows this initial injury and includes recruitment of inflammatory cells and release of various inflammatory mediators. This disorder is known as Mendelson syndrome when the acute aspiration is massive and when aspirated contents have a pH of <2.5 [21]. First described in association with obstetric anesthesia, it is now known to occur in patients with markedly decreased levels of consciousness from multiple causes (drug overdose, following head trauma, seizures). Recurrent small-volume aspirations of refluxed gastric contents during sleep appear to result in chronic and less severe forms of lung injury, such as diffuse aspiration bronchiolitis or chronic exogenous lipoid pneumonia (when oil-based substances [e.g., mineral oil laxative] are aspirated). On imaging, the severity of the resulting lung injury depends on the pH and volume of the aspirate, including airway thickening with ground-glass opacities and nodules in a centrilobular and peribronchovascular distribution. Because of dispersion of the aspirate by coughing, the distribution can be diffuse, bilateral, and symmetric. The DD of diffuse aspiration pneumonitis includes aspiration pneumonia, community-acquired pneumonia, cardiogenic or noncardiogenic pulmonary edema, pulmonary hemorrhage, and acute hypersensitivity pneumonitis [14].
Bronchiectasis
Bronchiectasis, defined by irreversibly widened bronchi due to damage to the bronchial walls, usually arises from some combination of bronchial obstruction and infection [22]. Bronchiectasis is a well-known sequela of chronic pulmonary aspiration that can result in significant respiratory morbidity and death (Fig. 3) [23].
Zenker diverticulum. (a, b) VFSS examination in a 68-year-old man with dysphagia, cough, and halitosis. AP and LL views show a large Zenker diverticulum, extending inferiorly and compressing the cervical esophagus. (c, d) HRCT chest axial images show multiple bilateral centrilobular nodules and cylindrical bronchiectasis in the lower lobes. Uncoordinated swallowing, impaired relaxation, and spasm of the cricopharyngeus muscle leads to an increase in pressure within the distal pharynx, so that its wall herniates through the point of least resistance
Diffuse Aspiration Bronchiolitis (DAB)
Bronchiolitis refers to a broad spectrum of disorders characterized by inflammation and fibrosis of the bronchioles (internal diameter of ≤2 mm). DAB describes the resultant inflammation of bronchioles secondary to aspiration. There is a high association of DAB with oropharyngeal dysphagia, bedridden status, dementia, and neurological disorders. Its onset is often insidious, making it difficult to establish a direct association with food intake. On imaging, DAB resembles diffuse panbronchiolitis, typically manifesting as unilateral or bilateral centrilobular nodules, tree-in-bud nodularity, bronchial wall thickening, and poorly marginated acinar areas of increased attenuation (Fig. 4) [24]. Mosaic attenuation or segmental and subsegmental air trapping can be seen in expiratory imaging. In contrast to asthma, imaging findings are often concentrated in the lower lobes or dependent aspects of the lungs. Associated imaging findings include an esophageal mass, hiatal hernia, or air-fluid level in the esophagus. DD for this pattern is broad and includes other causes of small airway disease, such as infectious bronchiolitis, diffuse panbronchiolitis, cystic fibrosis, allergic bronchopulmonary aspergillosis, and collagen vascular disorders [25].
Hiatal hernia, GERD, and diffuse aspiration bronchiolitis (DAB) in a 58-year-old woman with fever. HRCT chest axial images (a, b) and coronal reconstruction (c) show a large hiatal hernia in (b) and diffuse lobular bronchioles dilatation filled by mucus and pus (tree-in-bud pattern). This pattern is a known manifestation of various entities as aspiration of infected oral secretions or other irritant material into small airways. (d) VFSS lateral view shows associated tracheal aspiration
Tracheobronchial Foreign Body
Big-sized foreign body aspiration may result in obstruction of the central airway and sudden death from asphyxiation. In a small-sized inhaled and retained foreign body, most patients present with a nonresolving cough, sometimes associated with exertional dyspnea, chest pain, or hemoptysis. Imaging findings can include postobstructive atelectasis or rarely hyperinflation, air trapping, recurrent pneumonia, bronchial wall thickening, and bronchiectasis; complications are distal abscess formation and parenchymal necrosis. Chest CT scanning often provides additional diagnostic information including demonstration of an intrabronchial mass, which may be mistaken for an endobronchial malignancy [26]. Expiratory images may show air trapping in the affected segment (or lobe). When bronchial obstruction is chronic, consolidative opacities from postobstructive pneumonia may be demonstrated along with bronchiectasis. On high-resolution computed tomography (HRCT) of the chest, lentil aspiration pneumonia manifests as centrilobular nodules, some with a tree-in-bud configuration [27]. Pill aspiration represents a unique type of foreign body aspiration because some pills such as potassium and iron preparations may dissolve in the airways, causing intense bronchial inflammation and stenosis [28]. DD for this pattern is similar to that described for aspiration bronchiolitis. An additional concern in adults is that aspiration of undigested food can have similar imaging characteristics to an endobronchial neoplasm and can be associated with lymphadenopathy and lobar collapse when chronic.
Near Drowning
In near drowning, defined as severe asphyxia caused by submersion in water but not resulting in death, chemical and organic contaminants in the aspirated water are thought to cause adult respiratory distress syndrome. Radiographic findings are often presented as scattered ground-glass opacities that progress to patchy airspace consolidation over the next several days. Mild cases may present as perihilar ground-glass opacity, progressing to coalescent opacities in severe cases. Ground-glass opacities and consolidation likely represent pulmonary edema and adult respiratory distress syndrome, largely secondary to fluid entering the alveoli from the blood or disruption of the surfactant production.
Chronic Exogenous Lipoid Pneumonia
The aspiration of oily material, whether mineral, vegetable, or animal, commonly mineral oil, leads to exogenous lipoid pneumonia. The severity of the reaction depends largely on the amount of free fatty acid in the aspirate. The lung parenchyma in these cases may show fibrosis, as well as a histiocytic reaction involving the accumulation of lipid-laden macrophages. Radiographically, the distribution is predominantly basilar and paramediastinal. Early in the disease course, centrilobular or panlobular ground-glass opacities are identified, which progress to volume loss and interlobular septal thickening. When present, airspace consolidation or mass-like opacities with attenuation values of ≤10HU are diagnostic of this condition and can be seen in either the acute or chronic setting. Ground-glass opacities associated with interlobular septal thickening in a “crazy paving” pattern have also been described [13]. The DD of focal consolidation or mass-like opacity can include carcinoma and acute bacterial pneumonia or OP. The differential for a “crazy paving” pattern is broad and includes alveolar proteinosis, pneumocystis pneumonia, and diffuse alveolar damage or hemorrhage.
Chronic Interstitial Lung Disease (Chronic-ILD) and Organizing Pneumonia
Chronic aspiration may be asymptomatic or present nonspecifically with symptoms such as chronic cough or dyspnea. Gastroesophageal reflux disease (GERD) with repeated reflux of gastric contents into the superior esophagus and pharynx also likely contributes to chronic microaspiration.
Secondary aspiration organizing pneumonia (OP) pattern is often basilar predominant and peripheral or bronchovascular in distribution. A suggestive imaging finding of OP is the reverse halo sign, also called the atoll sign or fairy ring sign. Another pattern that may be related to chronic aspiration is a usual interstitial pneumonia (UIP) pattern of pulmonary fibrosis [29].
Implications for Noninvasive Ventilation (NIV) Approach
Breathing-swallowing coordination is one of the most important airway defense mechanisms. Swallowing normally occurs during expiration, and the subsequent respiration reinitiates with expiration; this expiration-swallow-expiration (E-SW-E) pattern at mid-to-low lung volumes poses significant physiologic advantages for hyolaryngeal anterior-superior movement, airway closure, and pharyngoesophageal segment opening, preventing the pharyngeal contents from invading the lower airway. Expiration-followed swallow is a mechanism helpful in clearing the pharyngeal recesses of foreign residues before subsequent inspiration and may prevent low-grade recurrent aspiration. Moreover, when swallowing interrupts in the expiratory phase of the respiratory cycle, the elastic recoil of the lungs and the chest wall can generate a subglottic positive pressure which is considered as a key component of swallowing efficiency [30]. Patients with respiratory insufficiency due to either chronic obstructive pulmonary disease (COPD) or neuromuscular diseases (NMD) equally swallow during the expiratory and inspiratory phases of respiration. The use of a patient-controlled NIV during swallowing significantly improved breathing-swallowing coordination in ventilated dysphagic patients with severe respiratory failure by increasing the pattern of expiration-followed swallowing and reducing dyspnea and aspiration.
Breathing-swallowing discoordination more frequently occurs in dysphagic patients [2]. Respiration after swallowing is more frequently resumed with inspiration in patients with COPD than in healthy subjects, which may predispose patients to aspiration-related exacerbation [31]. In noninvasive ventilation continuous positive airway pressure (CPAP) decreases the swallowing-inspiration frequency and alleviates the risk of aspiration in patients with COPD [32, 33]. NIV use significantly improved swallowing fragmentation (defined as the number of respiratory interruptions of the swallowing of a single bolus) and breathing-swallowing synchronization with a significant increase of swallows followed by an expiration [34]. The use of patient-controlled NIV improves swallowing parameters in patients with severe neuromuscular respiratory failure requiring daytime NIV, without impairing swallowing comfort [34].
Multidisciplinary Team
Dysphagia affects most patients with NMD, and each patient with dysphagia is different owing to the underlying neurological impairment. Aspiration can cause a wide spectrum of pulmonary diseases (AILD), is often silent/occult and undetected clinically, and has the potential for dire consequences. Etiologic diagnosis is possible by VFSS and by knowledge of the chest imaging patterns, and the radiologist plays an important role in suggesting the diagnosis when proved by VFSS. A multidisciplinary management is needed, including neurologist, respiratory physician, intensivist, ENT specialist, nutritionist, speech pathologist, and last but not least radiologist.
References
Martin-Harris B. Clinical implications of respiratory–swallowing interactions. Curr Opin Otolaryngol Head Neck Surg. 2008;16(3):194–9. https://doi.org/10.1097/MOO.0b013e3282febd4b.
Yagi N, Oku Y, Nagami S, Yamagata Y, Kayashita J, Ishikawa A, Domen K, Takahashi R. Inappropriate timing of swallow in the respiratory cycle causes breathing-swallowing discoordination. Front Physiol. 2017;8:676. https://doi.org/10.3389/fphys.2017.00676.
Carucci LR, Turner MA. Dysphagia revisited: common and unusual causes. Radiographics. 2015;35(1):105–22. https://doi.org/10.1148/rg.351130150.
Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–71. https://doi.org/10.1056/NEJM200103013440908.
Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler A, Scharitzer M, Oschatz E. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol. 2002;178:393–8. https://doi.org/10.2214/ajr.178.2.1780393.
Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing–Normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691–707. https://doi.org/10.1016/j.pmr.2008.06.001.
Jaffer NM, Ng E, Au FW, Steele CM. Fluoroscopic evaluation of oropharyngeal dysphagia: anatomic, technical, and common etiologic factors. AJR Am J Roentgenol. 2015;204:49–58. https://doi.org/10.2214/AJR.13.12374.
Bastian RW. The videoendoscopic swallowing study: an alternative and partner to the videofluoroscopic swallowing study. Dysphagia. 1993;8:359–67. https://doi.org/10.1007/BF01321780.
Page EB (2006) Understanding the modified barium swallow study. Radiographic imaging CEU Source, LLC. http://www.radiographicceu.com/article23.html.
Siebens H, Trupe E, Siebens A, Cook F, Anshen S, Hanauer R, et al. Correlates and consequences of eating dependency in institutionalized elderly. Am J Geriatr Soc. 1986;1986(34):192–8. https://doi.org/10.1111/j.1532-5415.1986.tb04202.x.
Fattori B, Grosso M, Bongioanni P, Nacci A, Cristofani R, AlSharif A, Licitra R, Matteucci F, Rossi B, Rubello D, Ursino F, Mariani G. Assessment of swallowing by oropharyngoesophageal scintigraphy in patients with amyotrophic lateral sclerosis. Dysphagia. 2006;21:280–6. https://doi.org/10.1007/s00455-006-9052-5.
Armán JA, Lorente-Ramos RM, García PG, Lorduy TC. Videofluoroscopic evaluation of Normal and impaired oropharyngeal swallowing. Radiographics. 2019;39(1):78–9. https://doi.org/10.1148/rg.2019180070.
Marom EM, McAdams HP, Erasmus JJ, Goodman PC. The many faces of pulmonary aspiration. Am J Roentgenol. 1999;172:121–8. https://doi.org/10.2214/ajr.172.1.9888751.
Prather AD, Smith TR, Poletto DM, Tavora F, Chung JH, Nallamshetty L, Hazelton TR, Rojas CA. Aspiration-related lung diseases. J Thorac Imaging. 2014;29:304–9. https://doi.org/10.1097/RTI.0000000000000092.
Hu X, Lee JS, Pianosi PT, Ryu JH. Aspiration-related pulmonary syndromes. Chest. 2015;147:815–23. https://doi.org/10.1378/chest.14-1049.
Scheeren B, Marchiori E, Pereira J, Meirelles G, Alves G, Hochhegger B. Pulmonary computed tomography findings in patients with chronic aspiration detected by videofluoroscopic swallowing study. Br J Radiol. 2016;89:20160004. https://doi.org/10.1259/bjr.20160004.
The Japanese Respiratory Society. Aspiration pneumonia. Respirology. 2004;9:S35–7. https://doi.org/10.1111/j.1440-1843.2003.00548.x.
Shigemitsu H, Afshar K. Aspiration pneumonias: under-diagnosed and under-treated. Curr Opin Pulm Med. 2007;13:192–8. https://doi.org/10.1097/MCP.0b013e3280f629f0.
Franquet T, Gimenez A, Roson N, Torrubia S, Sabaté JM, Pérez C. Aspiration diseases: findings, pitfalls, and differential diagnosis. Radiographics. 2000;20:673–85. https://doi.org/10.1148/radiographics.20.3.g00ma01673.
Komiya K, Ishii H, Umeki K, Kawamura T, Okada F, Okabe E, Murakami J, Kato Y, Matsumoto B, Teramoto S, Johkoh T, Kadota J. Computed tomography findings of aspiration pneumonia in 53 patients. Geriatr Gerontol Int. 2013;13:580–5. https://doi.org/10.1111/j.1447-0594.2012.00940.x.
Landay MJ. Aspiration of gastric contents. AJR Am J Roentgenol. 1999;173:244. https://doi.org/10.2214/ajr.173.1.10397143.
Trinick RE, Bunni L, Thorburn K, Hackett AP, Dalzell M, McNamara PS. An observational study examining the relationship between respiratory symptoms, airway inflammation and bacteriology in children with severe neurodisability. PLoS One. 2015;10(4):e0124627. https://doi.org/10.1371/journal.pone.0124627.
Lee AS, Ryu JH. Aspiration pneumonia and related syndromes. Mayo Clin Proc. 2018;93:752–62. https://doi.org/10.1016/j.mayocp.2018.03.011.
Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G. Tree-in-bud pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2005;25:789–801. https://doi.org/10.1148/rg.253045115.
Pipavath SJ, Lynch DA, Cool C, et-al. Radiologic and pathologic features of bronchiolitis. AJR Am J Roentgenol. 2005;185(2):354–63. https://doi.org/10.2214/ajr.185.2.01850354.
Kim M, Lee KY, Lee KW, Bae KT. MDCT evaluation of foreign bodies and liquid aspiration pneumonia in adults. AJR Am J Roentgenol. 2008;190(4):907–15. https://doi.org/10.2214/AJR.07.2766.
Marom EM, McAdams HP, Sporn TA, Goodman PC. Lentil aspiration pneumonia: radiographic and CT findings. J Comput Assist Tomogr. 1998;22:598–600. https://doi.org/10.1097/00004728-199807000-00016.
Mehta AC, Khemasuwan D. A foreign body of a different kind: pill aspiration. Ann Thorac Med. 2014;9:1–2. https://doi.org/10.4103/1817-1737.124404.
Cardasis JJ, MacMahon H, Husain AN. The spectrum of lung disease due to chronic occult aspiration. Ann Am Thorac Soc. 2014;11:865–73. https://doi.org/10.1513/AnnalsATS.201310-360OC.
Gross RD, Carrau RL, Slivka WA, Gisser RG, Smith LJ, Zajac DJ, et al. Direct measurement of subglottic air pressure while swallowing. Dysphagia. 2006;116:753–61. https://doi.org/10.1007/s00455-011-9389-2.
Gross RD, Atwood CW Jr, Ross SB, Olszewski JW, Eichhorn KA. The coordination of breathing and swallowing in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179(7):559–65. https://doi.org/10.1164/rccm.200807-1139OC.
Yoshimatsu Y, Tobino K, Nagami S, Yagi N, Oku Y. Breathing-swallowing discoordination and inefficiency of an airway protective mechanism puts patients at risk of COPD exacerbation. Int J Chron Obstruct Pulmon Dis. 2020;15:1689–96. https://doi.org/10.2147/COPD.S257622.
Hori R, Ishida R, Isaka M, Nakamura T, Oku Y. Effects of noninvasive ventilation on the coordination between breathing and swallowing in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2019;14:1485–94. https://doi.org/10.2147/COPD.S205543.
Garguilo M, Lejaille M, Vaugier I, Orlikowski D, Terzi N, Lofaso F, Prigent H. Noninvasive mechanical ventilation improves breathing-swallowing interaction of ventilator dependent neuromuscular patients: a prospective crossover study. PLoS One. 2016;11(3):e0148673. https://doi.org/10.1371/journal.pone.0148673.
Acknowledgments
I want to express my sincere gratitude to the medical radiology technician (TSRM) Dr. Giovanni Colombo for helping to obtain radiological images.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Valente, T. (2023). Videofluoroscopy and Swallowing Evaluation and Pattern of Inhalation Injury. Implications for Noninvasive Ventilatory Approach. In: Esquinas, A.M., De Vito, A., Barbetakis, N. (eds) Upper Airway Disorders and Noninvasive Mechanical Ventilation. Springer, Cham. https://doi.org/10.1007/978-3-031-32487-1_26
Download citation
DOI: https://doi.org/10.1007/978-3-031-32487-1_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-32486-4
Online ISBN: 978-3-031-32487-1
eBook Packages: MedicineMedicine (R0)