Abstract
The metabolism of bone cells is strongly regulated by estrogens and, therefore, the risk for osteoporosis is favoured by menopause. Fragility fractures define the outcome to be prevented in osteoporosis. Because age adds to menopause as a risk factor, and menopause occurs at a relatively young age, preventive measures are desirable during the early post-menopausal period. Physical activity, balanced nutrition and restraint of toxics, smoking and alcohol excess, should be universally encouraged. Attention to osteoporosis risk factors should be a part of every basic clinical assessment of menopausal women. The identification of strong risk factors, like the presence of previous fragility fracture, fracture identification in first-degree relatives, or age older than 65 years, imposes additional evaluation, including bone densitometry. When pharmacological treatment is needed, the array of anti-resorptives includes selective estrogen receptor modulators (SERMs), bisphosphonates and denosumab. SERMs add reduction of risk for breast cancer (raloxifene and may be bazedoxifene) and a protection against vertebral fractures. The reduction of risk for hip fracture requires bisophosphonates or denosumab.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Osteoporosis and Women
Osteoporosis is a disease in which reduced bone mass and microarchitectural deterioration of bone tissue increase the risk for fragility fracture. Osteoporosis integrates one of the non-communicable diseases (NCD) with a higher impact in ageing population. Based on the densitometric reference established by the technical report of the World Health Organisation (WHO) in 1994 [1], osteoporosis emerged as a disease affecting 75 million people in Europe, North America and Japan. That prevalence was found by using bone mineral density (BMD) as diagnostic criterion, which in women establishes osteoporosis when reaching 2.5 standard deviations or more below the average value for young healthy population [2].
The more recent evidence that BMD is a strong, but insufficient, parameter to assess the risk for fragility fracture in many subjects has uncovered the role of clinical factors, like age or others, which have also emerged as strong risk factors (Fig. 8.1). Moreover, the availability of osteoporotic fracture data from cohorts at different geographical settings has made possible the integration of clinical parameters into the prediction of risk for fracture. New tools have been designed in which both clinical and densitometric factors are integrated and provide an absolute risk for fracture. It has been again the WHO that has issued the Fracture Risk Assessment Tool (FRAX) [3]. FRAX provides a 10-year absolute individual risk for fragility fracture and is sensitive to the varying conditions of different populations in the world.
Age is a strong risk factor for fragility fracture. The figure shows the 10-year hip fracture probability in a Swedish population according to age and bone mineral density (BMD) at the hip, which is presented as T-score. It is obvious that the lower the bone density (lower T value) the higher the risk for hip fracture. However, for a given T value, and particularly in ranges below −1 (osteopenia), age imposes dramatic differences in risk. With permission of Springer Verlag from Kanis et al. Osteoporos Int. 2001;12:989–95. Permission obtained through Copyright Clearance Center, Inc
Therefore, the emphasis is now fracture, instead of BMD, a most-needed approach to better identify those individuals that will suffer from the more than 8.9 million fractures occurring annually worldwide. Indeed, the lifetime risk for osteoporotic fracture, which moves between 30 and 40% in developed countries, approaches that for coronary heart disease. Complications of osteoporotic fractures include both increased morbidity and mortality, which translate into 2.8 million disability-adjusted life years (DALYs) annually. These figures are above those accounted by hypertension and rheumatoid arthritis [4].
One strong risk factor for osteoporosis is gender. Women have an increased vulnerability, since one in three women over age 50 will suffer from an osteoporotic facture vs. one in five men [5]. A more fragile habitus, with thinner bone constitution, is a variable influencing the higher risk of women. Another important variable is menopause, one unique endocrinological phenomenon of women. Albright already observed the impact of the abrupt fall in ovarian hormonal production on the risk for fragility fractures in women with surgical menopause [6]. The arrival of reliable densitometers confirmed that the fall in the circulating level of oestrogens at menopause was associated with an accelerated loss of bone density.
2 The Biological Basis
2.1 Structure of Bone
Bone is the system that maintains the body in an erect position. Against its static aspect, bone is a live tissue subjected to continuous change. The composition of bone includes cells and inert material. Three main cellular types, osteoblasts, osteoclasts and osteocytes, distribute according to a framework provided by mineral, a calcium salt called hydroxyapatite, and a net of intertwined collagen fibres.
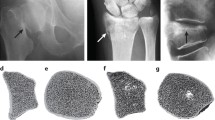
Two different forms of structures may be found in bone. Trabecular bone is a sponge-like design that fills up the vertebral bodies, where a network of trabecular plates determines a porous texture occupied by bone marrow. The transmission of tension through the trabeculae facilitates the flexibility required for energy absorption while maintaining a quite light fabric. Cortical bone, instead, is the basic component of long bones. Layers of bone are tightly overlapped to produce a thick structure most optimised to support loading. Cortical bone results from massive overlapping of osteons, structures composed of concentric layers of compact bone (lamellae) that surround a central canal (Haversian canal). The composition of lamellae is that of compact bone, i.e. the net of collagen fibres immersed into the hydroxyapatite mineral matrix.
2.2 Bone Cells
Osteoclasts, osteoblasts and osteocytes habit, and exert regulatory functions, in this apparently inhospitable environment. Both osteoclasts and osteoblasts are cells deriving from progenitors at the bone marrow, which occupies spaces close to the surface of mineralised bone. Their role is crucial for the renovation of bone while maintaining an adequate bone mass. The key system is the bone multicellular unit (BMU), in which osteoclasts and osteoblasts renovate bone at any location in the skeleton.
Bone resorption is the role of osteoclasts, which in this way eliminate areas that are damaged due to repeated loading. The formed cavities are then occupied by osteoblasts, which deposit osteoid, the proteinaceous matrix that will be slowly mineralised to produce new bone. One key duty of the BMU is the complete restitution of the digested bone, so that the balance is neutral and no loss of bone mass occurs.
Osteocytes derive from osteoblasts buried within the mineralised bone that they have contributed to create. Osteocytes occupy a network of hollow spaces (lacuna), which are communicated by a network of canaliculi through which cytoplasmic processes interconnect other osteocytes to form a full network. There is not a complete idea of the functional role of osteocytes, although there is growing consensus in that they constitute a finely tuned sensor system detecting the bone areas in which, because of material fatigue, damage or other reasons, remodelling is desirable. In this sense, osteocytes may be considered as the guardians of bone quality [7]. Recent studies have shown that this function seems mediated, at least in part, by the contribution of osteocytes to the pool of one cytokine, the receptor activator of NFkB ligand (RANKL) [8, 9], which is crucial in the differentiation of osteoclasts from progenitor cells [10]. The differentiation of osteoclasts is coupled, as previously mentioned, to that of osteoblasts, which refill the resorbed cavity and keep unaltered the structure of the bone. A scheme of the bone cells is presented in Fig. 8.2.
The illustration shows a scheme of the basic multicellular unit (BMU), where the three main cellular types, osteoclasts, osteoblasts and osteocytes, are presented. The canopy of the bone-lining cells and one associated marrow capillary are also included in the figure. The network of the osteocyte canaliculi is well connected with every agent of interest, thus providing a stable structure for intercellular communication between the different cellular types in the BMU. With permission of Elsevier from Khosla S et al. Trends Endocrinol Metab. 2012;23:576–81. Permission conveyed through Copyright Clearance Center, Inc
2.3 Oestrogen Regulation
The initial observation by Albright that the loss of oestrogens in women increased the risk for osteoporotic fracture could only be adequately clarified in later years. Oestrogen receptors were initially described at the level of mRNA expression in cell cultures, experimental animals and human tissues [11,12,13]. Subsequent studies corroborated the presence of both alpha- and beta-ER in human cartilage and bone, this time at the level of protein [14, 15]. Both ER subtypes were detected in histological sections of the growth plate and in mineralised bone, and also in the three basic cellular types, osteoblasts, osteoclasts and osteocytes, although with different distribution patterns.
Parallel clinical observation confirmed that oestrogens behave as major regulators of bone metabolism not only in women, but also in men [16, 17]. Moreover, pioneer data from Lindsay et al. confirmed that treatment with oestrogens prevented the bone loss in ovariectomised women [18]. More refined work in the latter years has confirmed details supporting the role of oestrogens at different steps of bone metabolism (reviewed in [19]).
One first effect of oestrogens concerns the limitation of bone remodelling. Additionally, oestrogens have been demonstrated to limit bone resorption. This is consistent with the observation of net bone loss with oestrogen decline, which is already detected at early stages of perimenopause [20] and is maintained until late in the postmenopausal years [21]. The impact of oestrogen decrease is confirmed by the clear increment of biochemical markers of bone resorption, at rates of 79–97% [21], in both blood and urine in postmenopausal women. The increase in resorption markers is accompanied by the concomitant increase in markers of bone formation, but in a lower magnitude. The biological basis of this observation is the acceleration in the activation of BMUs, in which the differentiation of both osteoclasts and osteoblasts from progenitor cells is increased, but with a deviation in favour of bone resorption in all cases. A net loss of bone, consequently, results.
One first effect of oestrogens concerns the reduction of bone remodelling through direct action on osteocytes, the main regulatory cells. Studies in humans have shown that increased osteocyte apoptosis, as demonstrated in bone biopsies, associates with depletion of oestrogens by GnRH analogues administered to premenopausal women [22], and that this effect is followed by the activation of BMUs.
Further experimental work has confirmed that there is a direct effect of oestrogens on osteoclasts too. For example, the selective deletion of ERα in mice is followed by loss of bone mass and the extension of the lifespan of osteoclasts in trabecular bone [23]. Vice versa, oestrogens have been demonstrated to suppress the differentiation of osteoclasts by several mechanisms, including the interference with RANKL [24], the overexpression of osteoprotegerin, the decoy receptor of RANKL or the own reduction in the production of RANKL and other pro-resorption cytokines by different cell types (for a review see [19]).
Together with the activation of bone resorption, the deficiency in oestrogens also determines defects in bone formation through a direct action on osteoblasts. Contrary to osteoclasts, oestrogens reduce apoptosis and increase lifespan of osteoblasts. The details of the mechanisms involved in this action of oestrogens are being investigated, although experiences in different models suggest that oestrogens might interfere with oxidative stress and reduce NF-κB, the latter being involved in impairing bone formation subsequent to bone resorption in BMUs [19].
As other NCDs, osteoporosis has a long subclinical period that is susceptible to risk reduction strategies. Menopause defines a period of particular interest because of two main reasons, the increased deterioration of bone mass that initiates at this period and the wide receptivity of women to health promotion during this phase of their lives. It is therefore important to design a most appropriate strategy, which should include both diagnosis and management.
3 Diagnosis
There are not specificities that make different diagnostic strategies for osteoporosis in the particular case of the menopausal woman. The basic principle that the main purpose of the action against the disease should be the reduction of the fragility fracture remains as a mainstay in the management plan.
3.1 Clinical Assessment
Also as for other stages in life, a detailed clinical anamnesis will provide whether there are clinical risk factors. They should be preferably integrated in the context of any of the available tools for calculating absolute facture risk. The FRAX risk calculator, which provides absolute risk at 10 years, is supported by the WHO and by other scientific societies, like the National Osteoporosis Foundation (NOF) [25], International Osteoporosis Foundation [26], or others (Fig. 8.3). More risk calculators have been proposed, like the Q-fracture [27] or others, but they have not demonstrated clear advantages. The existence of a prior fragility fracture or parental history of hip fracture, for example, continues to be a strong risk factor, which should receive particular attention, as described in most guidelines [28].
The screen page of the FRAX tool German model (https://www.shef.ac.uk/FRAX), with permission of the World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield Medical School, UK
3.2 Imaging
Additional diagnostic tools include imaging techniques, where bone densitometry is the main pillar. The status of bone tissue, not only its density, may be measured by several techniques, like quantitative computed tomography and quantitative ultrasound. Densitometry based on X-ray is, nonetheless, the universal priority and, therefore, we will focus on that technique. The basis of its utility resides in that the absorption of X-ray is very sensitive to the calcium content of the tissue. Dual-energy X-ray absorptiometry (DXA) is the most widely used technique, which is taken as a reference for the diagnosis of osteoporosis according to the WHO criteria (see above). Both areal and volumetric density may be measured, but areal BMD is commonly used because it accounts for approximately two-thirds of bone strength and, consequently, is considered a strong risk factor for fracture. An additional advantage of DXA resides in its capacity to visualise deformities of the vertebral bodies, thus avoiding the additional use of conventional X-ray assessment.
In addition to its value to ascertain the risk for future fracture, the information obtained from DXA may also be used as a referent baseline to monitor the evolution of a particular patient. This is of interest in the case of postmenopausal women, because the rate of bone loss has an individual profile, and some women, those defined as “fast losers” in some studies, show a specific sensitivity to oestrogen drop. Also, observational studies have confirmed that the change rate of BMD in a treated patient is useful to determine the evolution of the future fracture risk [29]. The slow response of BMD to treatment is, however, a difficulty for taking advantage of this option of DXA. Moreover, the absence of BMD increase does not necessarily imply the absence of therapeutic response.
Trabecular bone score (TBS) is a novel method that, based upon the spine imaging provided by some specific densitometers, may give information that relates with bone texture and microarchitecture. A series of recent studies have suggested that TBS may improve fracture risk prediction over that provided by conventional DXA, particularly in some specific cases, like diabetes [30]. The potential of TBS, nonetheless, still needs investigation.
3.3 Biochemical Markers
Bone biochemical markers are analytes that result from the metabolic events in bone. Some of them are produced as a consequence of resorption by osteoclasts while others are released as a result of the osteoblastic activity. Since both cell types are coupled in the remodelling process because of the activation of the BMUs, both types of markers increase during raised resorption.
The great potential advantage of bone markers is that, if they are specific enough and the analytical method is sufficiently precise, a real-time report of the status of bone metabolism may be obtained. The magnitude of the treatment response, for example, might be assessed without waiting for the densitometric response.
Furthermore, their baseline value may be taken as an indicator of the magnitude of the resorptive process and, should this behave as a stable phenomenon, a certain prognosis of the fracture risk might be seized [31]. This is a very important feature to better detect the most abundant profile of fractured subjects, who have normal or only slightly decreased BMD for their age [32].
The choice of bone markers keeps increasing in parallel with the better knowledge of bone metabolism [33]. Resorption markers include collagen degradation proteins, noncollagenous proteins, osteoclastic enzymes and, more recently, osteocyte activity markers. Degradation products of type 1 collagen are produced by the activity of cathepsin K, an osteoclastic enzyme. Both the carboxy (CTX-1) and the amino-terminals (NTX-1) may be measured and are the most consolidated options. Indeed, CTX1 in serum has been recommended as reference bone resorption marker by IOF.
Formation markers have had less use. The list includes procollagen type I propeptides, osteocalcin and alkaline phosphatase. The procollagen type I propeptides are originating mainly from activated osteoblasts and result from the posttranslational cleavage of type I procollagen molecules by proteases. Both the N- and the C-terminal, PINP or PICP, are produced, but the most reliable and preferred is PINP, which is the reference formation marker in most studies. The practical value of PINP has increased considerably in the latter years.
In practice, the main limitation of bone markers is their variability, mainly due to the circadian and seasonal variation of bone metabolism. Even so, they may be taken as an adjunct to DXA for aspects like identification of fast losers in postmenopause, the above-mentioned prediction of fracture risk, and for monitoring the effect of anti-resorptive therapy. This latter advantage is of value only when using anti-resorptives capable of achieving a substantial reduction in bone turnover, like bisphosphonates or denosumab.
4 Management
The acceleration of bone resorption initiates prior to menopause [20], and the phenomenon keeps for many years, probably up to the end of life [34]. This means that, considering the global life expectancy, this state will last for 30 or more years. Moreover, it is known that most fragility fractures, including hip and vertebral, attain a significant incidence at relatively advanced age, not earlier than 70 years. Also important, most anti-resorptives have shown efficacy in clinical trials in which the median age of the participating women was advanced, far from the immediate postmenopausal period, and their prolonged use is not free of disadvantages [35]. Putting all these arguments together, it seems that most of the women that enter menopause should attend the reduction of osteoporosis risk with an armamentarium in which potent anti-resorptives are not a first option. Then, the identification of the optimal way to manage this long period of women’s life raises several questions.
4.1 Assessment of Osteoporosis Risk
Osteoporosis should be an issue in the routine management of menopausal women. The purpose should be the identification and evaluation of high-risk individuals. A detailed clinical history is mandatory to disclose whether there are specific clinical risk factors, particularly the strong ones, a history of previous fragility fracture and parental history of hip fracture. The review of the list of clinical risk factors included in FRAX may help because it is quick and at the same time may be useful to position the woman in relation to her future (10 years) risk for fracture.
The option of a systematic DXA assessment is a matter of some debate. The majority of guidelines do not recommend its practice until the age of 65 years unless there are one of the strong risk factors mentioned above [36]. This is so because, even accepting that the proportion of women with osteoporosis at 50 years that will suffer from a fracture in the next 10 years is approximately 45%, a 96% of the fractures will occur in women without osteoporosis [28]. One Australian study has added low body mass index as an independent risk factor, although the study referred to densitometric osteoporosis and not to fragility fracture [37]. There is no established recommendation on the use of biochemical markers.
4.2 Lifestyle as a Risk Reduction Strategy
Menopause is an excellent opportunity to implement healthy lifestyle in women who do not meet the criteria for DXA scanning. As mentioned above, they will be majority. This includes avoidance of toxics, mainly alcohol abuse and tobacco, good nutrition and regular practice of exercise. Regular physical activity may reduce the progression of ageing-associated sarcopenia, slow or even equilibrate the loss of bone mass and improve neuromotor coordination to decrease the risk of falls. Additionally, there is an impact on mood and wellness, which may translate into improvement of the quality of life, and on other organs and systems. So, it is a most appropriate option, which should be strongly recommended, to manage this period in the life of women [38].
Nutrition has received attention, particularly in what refers to the adequate intake of protein, calcium and vitamin D. The literature on the effect of calcium and vitamin D on the reduction of fracture is mixed, specifically in what refers to pharmacologic calcium. No discernible effect of calcium on hip fracture was detected in a meta-analysis pooling data from seven prospective cohort studies including 170,991 women. Moreover, data from Swedish women attending the mammography national programme and followed for 19 years showed that women with higher calcium intakes, well above the 1 g/day, had an increased risk for hip fracture [39] (Fig. 8.4). Moreover, some studies have shown that high dosages of pharmacologic calcium may be harmful in that there is an increase in kidney stones [40] and even myocardial infarction (24% increased risk in a meta-analysis pooling randomised studies) [41].
Average intake of dietary calcium and time to first hip fracture as calculated by Swedish investigators working with the data from the Swedish Mammography Cohort. This database includes 61,433 women born between 1914 and 1948 and followed for 19 years. Models were adjusted for a series of confounding variables. Increases in calcium ingestion above 1000–1200 mg/day were associated with increased risk. Hazard ratio is indicated by the solid line and 95% confidence intervals by dashed lines. With permission of the bmjGroup from Warensjö E et al. BMJ. 2011;342:d1473
The possibility that high intakes of calcium, with or without vitamin D, may be harmful has moved scientific societies to strengthen a clear message. The recommended nutrient intake (RNI) of calcium is 1000 mg/day, which should slightly increase to 1200 mg/day in populations at higher risk, as postmenopausal women [42]. Dietary sources of calcium are the preferred option. The corresponding dose of vitamin D should be 800 UI/day, which may be acquired from diet and from fortified dairy products. Fortified yoghurts, for example, contain 200 UI vitamin D.
Some debate has also arisen about the potential of vitamin D to reduce the risk for falls. No definitive conclusion has been reached, particularly because some data have been published arguing that high dosages of vitamin D may even increase the risk for falls.
4.3 Hormone Therapy
The whole cascade of symptoms, quality-of-life deterioration and health threats presenting in women’s lives at menopause is precipitated and caused by the drastic decline in hormone output, and more specifically, the fall of oestrogens. Consequently, it may be conceived that the reposition of the hormone should reinstate several, if not all, of the lost benefits.
In the case of osteoporosis, the pathophysiological features described above are clearly linked with oestrogen loss. Accordingly, oestrogen replacement should act to reverse every observed action, something consistently reproduced at each step. So, experimental data confirm that oestrogens impair osteoclast differentiation, and maintain osteocyte survival and osteoblast function [19].
At the clinical level, data obtained years ago with the most primitive densitometers clearly confirmed that oestrogens could prevent menopause-associated loss of bone mineral content, as described at the metacarpus in a landmark study by Lindsay et al. [18]. More than 20 years later, the same group performed a dose-dependent study showing that even low dosages of oestrogens were able to maintain, and even to slightly increase, BMD at the spine [43]. Similar results have been observed with low-dose transdermal oestradiol [44], and have been widely reproduced. The consistence of the findings confirms that the protective effect on the bone may be attained with dosages below those required for symptom control.
Hormones do not seem to have a significant residual effect after treatment withdrawal, with most of the BMD gain being lost in 1–2 years [45]. Interestingly, comparison with other anti-resorptives in osteoporosis prevention (BMD effect) in menopausal women has shown non-inferiority of hormones, with advantages at some specific territories like the forearm [46].
More ambitious studies have taken the reduction of fracture as an endpoint. The clearest evidence was provided by the Women’s Health Initiative (WHI) study, which clearly showed an increase in BMD and a reduction in fracture at the spine, the hip and the forearm, although only the hip effect was significant after adjustment for multiple comparisons [47]. Importantly, this effect was found in a population of healthy women.
The detrimental effects on other systems obscured the good performance of oestrogens on the bone in the WHI study. The rise in the diagnoses of breast cancer and the vascular effects, including increases in coronary heart disease, stroke and deep venous thrombosis, were the basis for recommendations of scientific societies and government institutions against the use of oestrogens to prevent chronic disease. This also applied to osteoporosis. Despite being the actor pathophysiologically entitled to restore the trigger mechanisms, and their excellent performance at both experimental and clinical level, the use of oestrogens to prevent or treat osteoporosis is discouraged, or taken as a last option, by most guidelines from scientific societies and governmental bodies.
4.4 Pharmacological Compounds
4.4.1 Selective Oestrogen Receptor Modulators (SERMs)
Advances in pharmacological chemistry together with the better knowledge of ER biochemistry have generated a number of synthetic compounds that have a molecular conformation distinct to oestrogens but share their potential to interact with the ER. The structural differences with oestrogens determine that their agonist/antagonist equilibrium changes as a result of the three-dimensional molecular configuration or the target tissue [48]. SERMs are grouped into families according to the root biochemical structure, and several of them have been approved for use with humans [49].
The most attractive property of SERMs is that molecules may be shaped to maintain the advantages of oestrogens, for example in osteoporosis, while getting rid of the disadvantages. This search of the perfect SERM keeps being a constant in the latter years.
Two compounds, raloxifene and bazedoxifene, have been approved for treating osteoporosis in several countries. Both raloxifene and bazedoxifene have demonstrated increases in BMD and effective reduction of vertebral, but not hip fractures [50, 51]. There was a protective effect against nonvertebral fractures in corresponding post hoc analyses [51, 52]. The size of the impact on the bone seems slightly lower than that achieved by oestrogens. Interestingly, raloxifene has demonstrated reduction in the risk for breast cancer [53], although as for oestrogens, an increase in deep vein thrombosis was apparent in the pivotal studies [50, 51]. Health economy analyses have shown acceptable cost/effectiveness of SERMs [54, 55].
Bazedoxifene has demonstrated a more antagonistic effect than raloxifene in endometrium, and this interesting property has been taken as the basis for development of new formulations in which bazedoxifene is mixed with oestrogens to counterbalance the oncogenic potential of oestrogens on the endometrium or the breast.
4.4.2 Other Anti-resorptives
The armamentarium of drugs with proved effectiveness against osteoporosis keeps increasing at good pace. The bone-forming agents emerge among the most recent novelties [56, 57], but the interest in the field of postmenopausal osteoporosis continues being focused in anti-resorptives. This is so because menopause favours bone loss since the fall of oestrogens increases bone resorption. Bisphosphonates and denosumab are two well-consolidated options that have proved effectiveness as anti-resorptives.
4.4.2.1 Bisphosphonates
These molecules are incorporated into the mineralised bone because of their affinity for calcium. Bisphosphonates are toxic for osteoclasts, so that they condition cellular demise when ingested in the course of the osteoclast-dependent resorptive action. In such a simple way, bisphosphonates drastically reduce bone turnover. Several compounds have been marketed and are now very good cost-effective options [58]. Alendronate, risedronate, clodronate, zoledronate and ibandronate have been those with higher popularity. They may be administered by oral and intravenous route. Oral bisphosphonates may be used in weekly and monthly doses with similar impact on BMD and bone markers as that of the daily administration. Randomised controlled trials including high-risk women have shown that oral bisphosphonates reduce vertebral fractures by approximately 40–50% and hip fracture by 51% (alendronate) [59], and by 30% (risedronate) [60] in some specific populations.
The highly effective reduction of bone turnover has become a difficulty in the long-term use of bisphosphonates. The lack of a minimal activity of the BMUs has favoured two rare but serious adverse events, osteonecrosis, particularly at the jaw [61], and atypical femoral fractures [62]. This has popularised the new strategy of drug holiday [63], which aims at intercalating periods without treatment in the course of long-term use of bisphosphonates.
4.4.2.2 Denosumab
The first biological treatment in osteoporosis is represented by denosumab, a human (IgG2) antibody that binds to RANKL, thus drastically reducing the differentiation of osteoclasts. The dose of 60 mg administered in the form of subcutaneous injection every 6 months achieved a reduction of vertebral fractures by 68% and hip fractures by 40% as compared with placebo [64].
Because denosumab is a powerful anti-resorptive, and similar to bisphosphonates, the antibody has been associated with increased risk for osteonecrosis of the jaw and atypical femoral fractures [65].
Conclusion
Osteoporosis is a disease with a strong gender profile. Menopause adds risk and therefore is a period of particular attention. Moreover, the age at menopause is still early enough to implement lifestyle measures that will provide benefit not only for bone but also for other systems, like the vasculature, the muscle, the central nervous system or others.
Fractures are rare at the age of menopause unless women suffer from additional risk factors. This is why the health exams at this period of the women’s life should include a review of the risk factors for osteoporosis. Most women will be free of them and, consequently, should be advised healthy lifestyle only. This will include the avoidance of toxics, tobacco or excessive consumption of alcohol, a balanced diet in which the recommended amount of calcium (1200 mg/day) plus vitamin D (800 UI) is achieved, and regular physical activity. These measures will improve general health and quality of life and, again, should be the only recommendation to the widest majority of women.
Women with risk factors are fortunately very few, and should be studied adequately. This adds a bone densitometry and, if risk is sufficiently high, the use of anti-resorptive drugs. The selection of the drug should account that women living the early phases of menopause, usually aged less than 60 years, have a long life expectancy in front. Since one strong risk factor of osteoporosis is age, the indication for treatment will keep being stronger as years pass. This is why SERMs add two advantages, the reduction of the risk of breast cancer (raloxifene) and a smooth reduction of bone turnover, which discards the risks of jaw osteonecrosis or atypical femoral fracture. Also, SERMs reduce the risk of vertebral fractures, which rank prior to hip fracture in the chronologic sequence of osteoporotic fractures. After a certain number of years, SERMs may be changed for bisphosphonates [66]. This sequence, however, results from clinical judgement and has not been substantiated by any study. Therefore, initiation with bisphosphonates, for example, may be a good option as well. Denosumab, instead, should be left for women with higher risk of fracture [64, 65], which means women of more advance age, or with high risk for hip fracture.
References
http://apps.who.int/iris/bitstream/10665/39142/1/WHO_TRS_843_eng.pdf. Accessed 27 Dec 2016.
Kanis JA, Melton LJ III, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res. 1994;9:1137–41.
https://www.shef.ac.uk/FRAX/tool.jsp?lang=en. Accessed 27 Dec 2016.
http://www.who.int/chp/topics/Osteoporosis.pdf. Accessed 27 Dec 2016.
Kanis JA, Johnell O, Oden A, Sembo I, Redlund-Johnell I, Dawson A, et al. Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int. 2000;11:669–74.
Reifenstein EC Jr, Albright F. The metabolic effects of steroid hormones in osteoporosis. J Clin Invest. 1947;26:24–56.
Atkins GJ, Findlay DM. Osteocyte regulation of bone mineral: a little give and take. Osteoporos Int. 2012;23:2067–79.
Xiong J, Onal M, Jilka RL, Weinstein RS, Manolagas SC, O'Brien CA. Matrix-embedded cells control osteoclast formation. Nat Med. 2011;17:1235–41.
Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med. 2011;17:1231–4.
Riggs BL. The mechanisms of estrogen regulation of bone resorption. J Clin Invest. 2000;106:1203–4.
Braidman IP, Davenport LK, Carter DH, Selby PL, Mawer EB, Freemont AJ. Preliminary in situ identification of estrogen target cells in bone. J Bone Miner Res. 1995;10:74–80.
Arts J, Kuiper GGJM, Janssen JMMF, Gustafsson J-A, Lowik CWGM, Pols HAP, et al. Differential expression of estrogen receptors and during differentiation of human osteoblast SV-HFO cells. Endocrinology. 1997;138:5067–70.
Vidal O, Kindblom L-G, Ohlsson C. Expression and localization of estrogen receptor in murine and human bone. J Bone Miner Res. 1999;14:923–6.
Bord S, Horner A, Beavan S, Compston J. Estrogen receptors alpha and beta are differentially expressed in developing human bone. J Clin Endocrinol Metab. 2001;86:2309–14.
Nilsson O, Chrysis D, Pajulo O, Boman A, Holst M, Rubinstein J, et al. Localization of estrogen receptors-alpha and -beta and androgen receptor in the human growth plate at different pubertal stages. J Endocrinol. 2003;177:319–26.
Bilezikian JP, Morishima A, Bell J, Grumbach MM. Increased bone mass as a result of estrogen therapy in a man with aromatase deficiency. N Engl J Med. 1998;339:599–603.
Falahati-Nini A, Riggs BL, Atkinson EJ, O’Fallon WM, Eastell R, Khosla S. Relative contributions of testosterone and estrogen in regulating bone resorption and formation in normal elderly men. J Clin Invest. 2000;106:1553–60.
Lindsay R, Hart DM, Aitken JM, MacDonald EB, Anderson JB, Clarke AC. Long-term prevention of postmenopausal osteoporosis by oestrogen. Evidence for an increased bone mass after delayed onset of oestrogen treatment. Lancet. 1976;1:1038–41.
Khosla S, Oursler MJ, Monroe DG. Estrogen and the skeleton. Trends Endocrinol Metab. 2012;23:576–81.
Sowers MR, Finkelstein JS, Ettinger B, Bondarenko I, Neer RM, Cauley JA, et al. Study of Women’s Health Across the Nation. The association of endogenous hormone concentrations and bone mineral density measures in pre- and perimenopausal women of four ethnic groups: SWAN. Osteoporos Int. 2003;14:44–52.
Garnero P, Sornay-Rendu E, Chapuy MC, Delmas PD. Increased bone turnover in late postmenopausal women is a major determinant of osteoporosis. J Bone Miner Res. 1996;11:337–49.
Tomkinson A, Reeve J, Shaw RW, Noble BS. The death of osteocytes via apoptosis accompanies estrogen withdrawal in human bone. J Clin Endocrinol Metab. 1997;82:3128–35.
Martin-Millan M, Almeida M, Ambrogini E, Han L, Zhao H, Weinstein RS, et al. The estrogen receptor-alpha in 45 osteoclasts mediates the protective effects of estrogens on cancellous but not cortical bone. Mol Endocrinol. 2010;24:323–34.
Srivastava S, Toraldo G, Weitzmann MN, Cenci S, Ross FP, Pacifici R. Estrogen decreases osteoclast formation by down-regulating receptor activator of NF-kappa B ligand (RANKL)-induced JNK activation. J Biol Chem. 2001;276:8836–40.
https://www.nof.org. Accessed 27 Dec 2016.
https://www.iofbonehealth.org. Accessed 27 Dec 2016.
Hippisley-Cox J, Coupland C. Derivation and validation of updated QFracture algorithm to predict risk of osteoporotic fracture in primary care in the United Kingdom: prospective open cohort study. BMJ. 2012;344:e3427.
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24:23–57.
Leslie WD, Majumdar SR, Morin SN, Lix LM. Change in bone mineral density is an indicator of treatment-related antifracture effect in routine clinical practice: a registry-based cohort study. Ann Intern Med. 2016;165:465–72.
Silva BC, Leslie WD. Trabecular bone score: a new DXA-derived measurement for fracture risk assessment. Endocrinol Metab Clin N Am. 2017;46:153–80.
Garnero P, Sornay-Rendu E, Claustrat B, Delmas PD. Biochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: the OFELY study. J Bone Miner Res. 2000;15:1526–36.
Siris ES, Miller PD, Barrett-Connor E, Faulkner KG, Wehren LE, Abbott TA, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001;286:2815–22.
Shetty S, Kapoor N, Bondu JD, Thomas N, Paul TV. Bone turnover markers: emerging tool in the management of osteoporosis. Indian J Endocrinol Metab. 2016;20:846–52.
Zebaze RM, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M, Price RI, et al. Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet. 2010;375:1729–36.
Black DM, Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2016;374:254–62.
Papaioannou A, Morin S, Cheung AM, Atkinson S, Brown JP, Feldman S, et al. 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ. 2010;182:1864–73.
Davis SR, Tan A, Bell RJ. Targeted assessment of fracture risk in women at midlife. Osteoporos Int. 2015;26:1705–12.
Stojanovska L, Apostolopoulos V, Polman R, Borkoles E. To exercise, or, not to exercise, during menopause and beyond. Maturitas. 2014;77:318–23.
Warensjö E, Byberg L, Melhus H, Gedeborg R, Mallmin H, Wolk A, et al. Dietary calcium intake and risk of fracture and osteoporosis: prospective longitudinal cohort study. BMJ. 2011;342:d1473.
Wallace RB, Wactawski-Wende J, O’Sullivan MJ, Larson JC, Cochrane B, Gass M, et al. Urinary tract stone occurrence in the Women’s Health Initiative (WHI) randomized clinical trial of calcium and vitamin D supplements. Am J Clin Nutr. 2011;94:270–7.
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040.
https://www.nationalacademies.org/hmd/. Accessed 14 Aug 2016.
Lindsay R, Gallagher JC, Kleerekoper M, Pickar JH. Effect of lower doses of conjugated equine estrogens with and without medroxyprogesterone acetate on bone in early postmenopausal women. JAMA. 2002;287:2668–76.
García-Pérez MA, Moreno-Mercer J, Tarín JJ, Cano A. Similar efficacy of low and standard doses of transdermal estradiol in controlling bone turnover in postmenopausal women. Gynecol Endocrinol. 2006;22:179–84.
Gallagher JC, Rapuri PB, Haynatzki G, Detter JR. Effect of discontinuation of estrogen, calcitriol, and the combination of both on bone density and bone markers. J Clin Endocrinol Metab. 2002;87:4914–23.
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C, Osteoporosis Methodology Group and The Osteoporosis Research Advisory Group. Meta-analyses of therapies for postmenopausal osteoporosis. IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev. 2002;23:570–8.
Cauley JA, Robbins J, Chen Z, Cummings SR, Jackson RD, LaCroix AZ, et al. Effects of estrogen plus progestin on risk of fracture and bone mineral density: the Women’s Health Initiative randomized trial. JAMA. 2003;290:1729–38.
Cano A, Hermenegildo C. Modulation of the oestrogen receptor: a process with distinct susceptible steps. Hum Reprod Update. 2000;6:207–11.
Riggs BL, Hartmann LC. Selective estrogen-receptor modulators—mechanisms of action and application to clinical practice. N Engl J Med. 2003;348:618–29.
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–45.
Silverman SL, Christiansen C, Genant HK, Vukicevic S, Zanchetta JR, de Villiers TJ, et al. Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo-, and active-controlled clinical trial. J Bone Miner Res. 2008;23:1923–34.
Delmas PD, Genant HK, Crans GG, Stock JL, Wong M, Siris E, et al. Severity of prevalent vertebral fractures and the risk of subsequent vertebral and nonvertebral fractures: results from the MORE trial. Bone. 2003;33:522–32.
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295:2727–41.
Borgström F, Ström O, Kleman M, McCloskey E, Johansson H, Odén A, et al. Cost-effectiveness of bazedoxifene incorporating the FRAX® algorithm in a European perspective. Osteoporos Int. 2011;22:955–65.
Kim K, Svedbom A, Luo X, Sutradhar S, Kanis JA. Comparative cost-effectiveness of bazedoxifene and raloxifene in the treatment of postmenopausal osteoporosis in Europe, using the FRAX algorithm. Osteoporos Int. 2014;25:325–37.
Ruiz C, Abril N, Tarín JJ, García-Pérez MA, Cano A. The new frontier of bone formation: a breakthrough in postmenopausal osteoporosis? Climacteric. 2009;12:286–300.
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375:1532–43.
Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, Neer RM, et al. Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab. 2012;97:2272–82.
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet. 1996;348:1535–41.
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med. 2001;344:333–40.
Khan A, Morrison A, Cheung A, Hashem W, Compston J. Osteonecrosis of the jaw (ONJ): diagnosis and management in 2015. Osteoporos Int. 2016;27:853–9.
Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29:1–23.
Silverman SL, Adachi JD, Dennison E, International Osteoporosis Foundation Epidemiology/Quality of Life Working Group. Bisphosphonate drug holidays: we reap what we sow. Osteoporos Int. 2016;27:849–52.
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–65.
Cano A, Silvan JM, Estévez A, Baró F, Villero J, Quereda F, et al. Spanish Menopause Society position statement: use of denosumab in postmenopausal women. Maturitas. 2014;79:117–21.
Cano A, Mendoza N, Sánchez-Borrego R, Osteoporosis Guideline Writing Group from the Spanish Menopause Society. Sequential use of antiresorptives in younger women. Osteoporos Int. 2014;25:1191–2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Cano, A., García-Pérez, M.Á. (2017). Postmenopausal Osteoporosis. In: Cano, A. (eds) Menopause. Springer, Cham. https://doi.org/10.1007/978-3-319-59318-0_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-59318-0_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59317-3
Online ISBN: 978-3-319-59318-0
eBook Packages: MedicineMedicine (R0)