Abstract
Intense research efforts have been devoted to the exploration of breast cancer risk factors aiming at subsequent use in the development of prevention strategies. Age at menarche/menopause and childbearing patterns are proxies of exposure to endogenous oestrogens; circulating hormone levels, depending also on the use of exogenous oestrogens, are involved in the causation of the disease due to proliferative effects on breast epithelial tissue. Several modifiable lifestyle-related risk factors have been identified including obesity, alcohol consumption and physical inactivity, which increase breast cancer risk, especially in postmenopausal women, by up to 40%. Findings regarding the effect of diet remain inconclusive, apart from the established linear association of alcohol consumption with breast cancer risk. Exploration of specific components and the impact of these factors on disease outcome remains also to be established.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Oestrogens, the primary female sex hormones, are mainly involved in the formation of female sex organs and secondary sex characteristics, including breast development, control of the menstrual cycle and reproduction. Concerning their effect on breast tissue, oestrogens are directly responsible for inducing the ductal component of breast development, as well as for fat deposition and connective tissue growth. Therefore, they are highly linked to female breast growth during puberty and breast maturation during pregnancy which lead to lactation and breast-feeding. Over and beyond their physiological central role in breast epithelial tissue growth, however, oestrogens are also involved in breast carcinogenesis through a proliferative impact on breast tissue.
Breast cancer, the most common type of cancer among women both in the developed and the developing world, is on the increase. Genetic risk factors account for a steadily increasing proportion of disease causation as scientists develop a better understanding of the numerous potent, moderate and minor impact genes and polymorphisms on risk (see ► Chap. 5). Interestingly, lifestyle factors, including physical activity, weight and diet, seem to contribute most to the observed increase in the frequency of female breast cancer. Hence, identification of factors implicated in oestrogen-induced carcinogenicity and recommendations on modifiable behaviours are elements of paramount importance for cancer prevention programmes. This chapter aims to summarize current evidence on the impact of exposure to oestrogens, use of exogenous pharmaceutical agents related to female hormones, obesity, exercise and diet on breast cancer risk and outcome; to present potential gains in breast cancer prevention where behaviour modification is to be achieved at population level; and to introduce domains for further research.
1.1 Endogenous Oestrogens and Proxy Measurements of Oestrogen Exposure
1.1.1 Endogenous Oestrogens
Among oestrogens, oestradiol, the most biologically active oestrogen during reproductive years, and oestrone, the major circulating oestrogen after menopause, comprise the most well-studied female hormones. Oestradiol may be found in the circulation either bound to sex hormone-binding globulin and albumin or in an unbound form; free and albumin-bound oestradiol is thought to be highly active and readily available to breast tissue. On the other hand, oestrone can be directly converted to oestradiol either in the peripheral adipose tissue or by sulphatase and 17-beta-dehydrogenase intracellularly in breast cells [1].
Early evidence regarding the association between circulating oestrogen levels and breast cancer risk was derived from case-control studies despite their inherent limitations on account of oestrogen levels after diagnosis and via heterogeneous assessment methodologies (direct measurement, extraction or mass spectroscopy). Subsequently, these results were confirmed in large prospective studies, and an association between high circulating oestrogen levels and risk of breast cancer in postmenopausal women was established. A recent meta-analysis of these studies, encompassing 4302 breast cancer cases, showed that in postmenopausal women incremental quantiles of oestradiol levels (E2) increased breast cancer risk by a factor of two (OR for highest vs. lowest quantile = 2.15) [2]; a similar effect was also reported for oestrone (E1; OR = 1.81). Indeed, this study confirmed findings from an older pooled analysis [3], which had shown an increase in risk of postmenopausal breast cancer by increasing quantile of free oestradiol, bioavailable oestradiol, total oestradiol, oestrone and oestrone sulphate. Interestingly, more recently diverse effects by levels of hormone receptor expression of the tumour were shown, particularly the elevated risk of postmenopausal breast cancer by increasing circulating oestrogen levels pertained only to the hormone receptor-positive tumours [4], providing evidence for a biologically plausible explanation on the action of oestrogens via these receptors. The data for premenopausal women are limited due to cyclical variations in hormone levels during reproductive years making these studies challenging. Despite this a recent pooled analysis of seven prospective studies showed an increased risk of premenopausal breast cancer when concentrations of total oestradiol (OR = 1.19), free oestradiol (OR = 1.17) and oestrone (OR = 1.27) were doubled [5].
1.1.2 Proxies of Endogenous Oestrogen Exposure: Early Age at Menarche and Late Age at Menopause
Menarche signals the onset of exposure to ovarian hormone cycling, whereas menopause signals its cessation and the transition to a hypo-oestrogenemic environment. Evidence suggesting that earlier menarche and later menopause increase the breast cancer risk is consistent and quantified to a 5% increase in the risk with a 1-year decrease of age at menarche according to the largest to-date study of 120,000 breast cancer cases [6]. Adolescents with an earlier menarche have been shown to have increased urinary oestrogens around puberty, indicating increased exposure to ovarian hormones at a time of high breast tissue responsiveness [7]. There is also evidence that earlier menarche may determine circulating oestrogen levels even later in women’s life, at the menopausal transition [8].
Conversely, breast cancer risk in postmenopausal women decreases by 2.9% by 1-year increment of age at menopause [6]. Possible reasons for the protective effect of earlier menopause seem to be the abrupt decrease of circulating sex hormone levels during menopause [9] and the shorter overall period of exposure to cycling endogenous hormones. The evidence for a decreased breast cancer risk conferred in case of surgical menopause via bilateral oophorectomy is compelling [10]. In particular, a 50% lower risk was observed among women with oophorectomy before the age of 45 years [11], whereas the risk did not seem to decrease among women after hysterectomy with preservation of the ovaries [12].
1.1.3 Proxies of Endogenous Oestrogen Exposure: Childbearing
Nulliparous women are known to be at increased breast cancer risk compared to parous women [13], but this effect is more complex than initially thought. In particular, prospective studies have found that there is a transient increased risk after delivery among parous compared to same-age nulliparous women for a short-term period calculated up to 15 years [14]. Eventually, however, this effect reverses with a long-lasting protection of parous women for the rest of their lives and a further modestly decreased level of risk for every subsequent pregnancy. Thus, the cumulative breast cancer risk is overall decreasing with parity, given that breast cancer is more common among older women, and the increased risk following a pregnancy is extended to a period until the 40th to 50th year of age when baseline breast cancer rates are generally lower [15].
A younger age at first pregnancy is associated with decreased breast cancer risk [13, 16]. Although varying by study, each additional year of age at first childbearing leads to an increased premenopausal and postmenopausal breast cancer risk of 5% and 3%, respectively [16]. Additionally, women bearing their first child after 35 years compared to those with a first full-time pregnancy before 20 years, show an increased breast cancer risk of 30% [13].
The mechanisms underlying the parity-breast cancer associations relate to lifetime and parity-induced changes in the breast tissue. Before childbearing, the breast tissue of a woman of reproductive age contains a large number of undifferentiated glandular epithelial cells, characterized by higher proliferation and division rates and a stronger malignant potential, whose differentiation is gradually evolving. Parity promotes the differentiation of these cells making them more resistant to carcinogenic stimuli, thus decreasing the risk of breast cancer [17]. An earlier pregnancy indicates an earlier differentiation of glandular epithelial cells and thus a shortened period of exposure of undifferentiated cells to potential carcinogenic factors.
1.2 Exogenous Hormone Administration
Given the proliferative effects of oestrogens on breast tissue, the widespread use of exogenous hormones has rationally drawn research attention. Hormone regimens are mainly administered either as oral contraceptives (OC) during reproductive years, as part of infertility treatment, or as menopausal hormone replacement therapy (HRT). Another interesting new and unexplored research field is the effect for breast cancer risk of hormone medications for feminization in transgender individuals.
1.2.1 Oral Contraceptives
Oral contraceptives (OCs), introduced in the 1960s, represent the most common form of hormonal contraception reaching an 82% ever use among US women [18]. The majority of OCs contain both an oestrogen and a synthetic progestin. OC synthesis over time has undergone a major change in the dose of oestrogen, from higher than 100 μg to a considerably decreased 20–30 μg of ethinyloestradiol in the currently most frequently used OC.
The findings regarding a potential association with breast cancer risk remain rather inconsistent, despite the vast number of publications. Overall, a moderately higher breast cancer risk among OC users is found restricted to premenopausal breast cancer and recent use. In a recent meta-analysis of 44 case-control and cohort studies, the overall risk of breast cancer among OC users was 1.08 (95% CI, 1.003–1.165); the high heterogeneity between studies, though, raised concerns regarding the robustness of the findings [19]. The results supported a stronger association with recent OC use (<5 years, OR = 1.21) gradually attenuating with longer period since last use (5–10 years, OR = 1.17; 10–20 years, OR = 1.13; >20 years, OR = 1.02). The findings, showing increased risk in premenopausal and generally younger women [20, 21], but not in postmenopausal women [22], shown in previous studies, were also confirmed in the meta-analysis. Furthermore, OC have been associated with a comparably increased risk of premenopausal breast cancer in both parous (OR = 1.24) and nulliparous women (OR = 1.29); among parous women, however, the association is stronger in those who started OC use before their first full-term pregnancy [20]. A large pooled analysis [22], entailing worldwide available data up to 1996 on the association of breast cancer with OC use, showed an approximate 20% increased risk only among women under 45 years who were recent OC users. The risk was independent of the duration of use, but disappeared 10 years after OC quitting. No dose-response pattern in terms of duration of OC use seemed to apply [19], and no interaction with other breast cancer risk factors, such as BMI or family history, was evident [22].
The effect of OC on breast cancer risk seems to be mediated by either ethinyloestradiol or synthetic progestin derivatives of 19-nortestosterone that possess estrogenic activity [23]. Only a few studies have, however, examined the effect by oestradiol dose or progestin compound. A case-control study of younger women (20–44 years old) with breast cancer (1640 cases, 1492 controls) showed that those who used OC with ethinyloestradiol doses >35 μg were at higher risk compared to users of OC with lower doses, an effect more profound among women <35 years. The risk did not differ by recent progestin compounds, whereas pills with high progestin and oestrogen potency significantly increased the risk [21]. In conclusion, the reduction of oestradiol dose may have led to a decrease in the risk of breast cancer associated with OC use; more studies are needed, however, on the type of OC used and tentative associations with breast cancer subtypes.
1.2.2 Ovarian-Stimulating Agents
The emergence of infertility as a public health issue during the last decades and the use of ovarian-stimulating agents for its treatment rationally raised concerns regarding the tentative negative long-term effects of these agents. Ovarian-stimulating agents encompass oestrogen receptor modulators, like clomiphene citrate and tamoxifen, FSH, hCG, human menopausal gonadotrophin and GnRH analogues, and are typically administered during the follicular phase of the menstrual cycle aiming to stimulate ovulation. More frequently, ovarian-stimulating agents are used in complex protocols in the context of the controlled ovarian hyperstimulation phase of assisted reproductive technologies. Despite their definite effect on modifying circulating oestrogen and progesterone levels, however, current evidence, as synopsized by two recent meta-analyses, does not support any effect of ovarian-stimulating agents on the risk of subsequent breast cancer [24, 25]. The lack of association seemed to be robust independently of the drug used or the cycles of administration, whereas when used in the context of in vitro fertilization, no effect was evident when comparisons pertained to either women of the general population or women with history of infertility.
1.2.3 Hormone Replacement Therapy
HRT use was initiated in the 1960s, became popular in the developed world and reached its peak in the late 1990s. Oestrogen/progestogen combination is the most common form of HRT used for women with a natural menopausal transition, as opposed to oestrogen-only therapies used for hysterectomized women [26]; progestogens were used to protect the endometrium against the proliferative effects of unopposed oestrogens [27]. Most early scientific reports from observational studies showed beneficial effects of HRT on women’s health [28]. The initial promising findings were thereafter reversed in the Women’s Health Initiative (WHI) randomized controlled trial, published in 2002 [29]. The trial was terminated early due to increasing rates of adverse health outcomes among postmenopausal women using oestrogen plus progestogen therapy [29,30,31]. Questions were raised about the safety of HRT given that trial findings for increasing risk of cardiovascular disease, breast cancer and dementia outweighed the reported beneficial action against fractures and colon cancer [29,30,31].
Summarizing the results of epidemiologic studies on HRT effects is challenging, given the wide variation in doses, patterns of use and the varying combinations of different oestrogen and progestogen compounds over time. A meta-analysis, pooling results from 51 observational studies, showed a higher breast cancer risk among women using HRT, increasing with longer duration of use (RR = 1.35 among HRT users of >5 years) [32]; the summary findings were later confirmed in the large Nurses’ Health Study [33], the Million Women Study [34] and the WHI trial [30]. Previous studies had shown an increased risk primarily for in situ and not invasive cancer [35, 36] supporting a hypothesis that the higher breast cancer risk among HRT users was due to the most intense surveillance for breast cancer. Recent studies, however, confirmed a significant increase also for invasive breast cancer [32, 35, 36]. The effect is stronger for women of lower weight and BMI [32], possibly on account of lower baseline oestrogen levels among lean women and the abrupt increase following HRT administration. Additionally, Asian and women with high breast density seem to be more susceptible to the tumorigenic effects of HRT [37].
Concerns about the diverse effects of different types of HRT on breast cancer risk were initially raised after publication of the differential Women’s Health Initiative oestrogen-only and combined oestrogen-progesterone trials among 10,739 hysterectomized women [38] and 16,608 naturally menopausal women, respectively. Indeed, combined therapy with oestrogen and progestogen exerts a more pronounced breast cancer risk compared to «monotherapy» with oestrogen [29]. Despite the evidence for a causative association in the combined therapy arm, the oestrogen-only arm also showed a sizeable, though marginally significant, inverse association with breast cancer risk (RR = 0.77, 95% CI: 0.59–1.01). The WHI study, however, enrolled women many years after menopause (mean age 64 years) with a relatively high proportion of overweight women (BMI ≥ 30 kg/m2 in 45% of study subjects) [38] and a short follow-up (7.1 years), as the study was terminated due to the increased risk of adverse effects.
In terms of type of oestrogen or type of progestogen used, data were mainly contributed by European studies, with a higher variability in the formulas used. The Million Women Study showed no difference between conjugated oestrogen and ethinyloestradiol [34], whereas the French E3N study showed that the increased risk of breast cancer among combined HRT users is restricted to those receiving synthetic progestins and not progesterone or dydrogesterone [39], possibly on account of their increased androgenic action [40]. Despite the rationale that the route of oestrogen administration could change their effect due to differences in their metabolism, contemporary studies do not support differential effects of oral, transdermal or implanted oestrogens [34, 39].
The association of HRT with the risk of breast cancer-specific histology is an emerging research field within pathology. Generally, the findings are consistent towards an association of combined oestrogen-progesterone therapy with the risk of oestrogen and progesterone receptor-positive breast cancer but not with receptor-negative tumours [41,42,43,44]. Regarding particular histology, the WHI did not show any specific association of combined HRT with ductal or lobular carcinomas, even though the study was relatively underpowered [30]. Other studies show, however, a trend for stronger associations with lobular carcinomas, compared to ductal tumours [45, 46].
Conclusively, after myths on the overall protective effects of HRT have been debunked and replaced with well-established findings on a relationship between breast cancer risk and use of combined oestrogen-progesterone HRT, its use dropped dramatically; current guidelines recommend HRT only for relief of severe menopausal symptoms and deceleration of bone mass loss in the lowest possible dose and for the shortest possible time period [26, 47, 48].
1.2.4 Feminizing Therapy in Transgender Individu als
Since the beginning of the 1900s, societal awareness (and more recently acceptance) of transgender individuals considering themselves «trapped in their own body» has developed. Cross-sex hormonal treatment is now recommended as an important component of the endocrine regimen in transsexual people [49]. In male-to-female individuals, the treatment comprises combined administration of anti-androgens or GnRH analogues to block the activity of androgens or suppress the gonadotrophin axis on androgen production, respectively. In addition oestrogens are administered to promote the development of female characteristics. The negative findings of the oestrogen-only therapies on breast cancer risk in hysterectomized women in the WHI trial [38], along with the lack of evidence on increased risk of breast cancer among women with Turner’s syndrome receiving HRT for long periods [50], provided indirect evidence that cross-sex therapies for male-to-female individuals may not lead to an increased breast cancer risk among transsexuals. To date, up to 30 years of follow-up studies on transgender individuals seem to confirm initial findings, showing no evidence for increased risk of breast cancer among either male-to-female or female-to-male individuals [51,52,53]. Follow-up and further research is warranted to allow exploration of specific epidemiological parameters.
2 Effect of Obesity and Exercise
Overweight and obesity are expanding on a worldwide basis, reaching levels of 60–70% of the adult population in developed countries; alarmingly increasing are also the rates in developing countries. In the USA, the impact of overweight and obesity has been estimated to account for 20% of cancer deaths in women, a trend that has been implied as a cause of the concurrent overall breast cancer incidence increase [54]. The association between obesity and breast cancer risk varies by menopausal status. The findings regarding weight change throughout a woman’s lifetime, implicating also the beneficial role of physical activity, are also interesting. The common proposed mechanism for both of these associations pertains to oestrogenic activity, whereas other factors may prove to be equally or more important, particularly in respect to the more aggressive tumour immunophenotypes. Among them, insulin, insulin-like growth factor-I (IGF-I) and leptin, as well as angiogenic and a range of other transcription factors, have been implicated in the obesity-breast cancer association [55].
2.1 Obesity
2.1.1 The Bimodal Role of Adiposity Among Premenopausal and Postmenopausal Women
A vast number of studies have explored the association between BMI and breast cancer risk showing a differential pattern depending on menopausal status. Specifically, adiposity has been associated with a decreased risk in premenopausal but increased risk in postmenopausal women [56]. A 15% decrease per 5 kg/m2 increase in BMI has been recorded for premenopausal cancer; according to the Nurses’ Health Study, the effect of BMI on premenopausal breast cancer risk could be explained by the BMI at the age of 18 years [57]. It has also been suggested that this effect in premenopausal women could be mediated by obesity-related amenorrhea and subsequent lower exposure to endogenous oestrogen levels in these women [58].
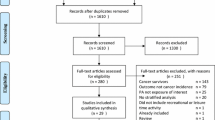
On the other hand, a strong increase of around 12% per 5 kg/m2 BMI increment in breast cancer risk has been reported in obese postmenopausal women [59]. In a meta-analysis, the authors found that obesity contributed to increased breast cancer risk in a nonlinear dose-response manner in postmenopausal women, and it is important to realize that body weight control may be a crucial process to reduce breast cancer susceptibility (◘ Fig. 4.1) [60]. Interestingly, the higher risk may primarily apply for oestrogen and progesterone receptor-positive tumours [61]. Family history of breast cancer and HRT seem to modify this association; particularly, having a relative with breast cancer strengthened the effect of a high BMI [62], whereas among HRT users this effect was moderate [63].
Dose-response meta-analysis for the association between BMI and risk of breast cancer in postmenopausal women (From Xia et al. [60]
2.1.2 Weight Change
A number of studies have assessed the effect of weight change during lifetime on breast cancer risk. The majority of studies pertain to postmenopausal breast cancer and show an increased risk with weight gain after 18 years of age; the effect over adulthood is estimated at 5% per 5 kg of weight gain [56, 64]. Furthermore, weight gain after menopause has been also found to independently increase breast cancer risk (OR: 1.18 for weight gain of at least 10 kg compared to women with no weight change) [64]. It is worth noting, however, that periods of potential weight loss have not been taken into account. The published data for premenopausal breast cancer are limited. In one report no effect was found [65], whereas another study showed a marginally significant decrease in breast cancer risk among women reporting weight loss since the age of 18 years [66].
2.1.3 Central Adiposity
Of interest is also the association of breast cancer with fat distribution, besides overall adiposity. Central adiposity is linked to metabolic-hormonal changes leading to insulin resistance, as well as hyperandrogenemia and excess conversion of peripheral androgens to oestrogens. Waist-to-hip ratio is considered a reliable measure of central adiposity and has been consistently associated with postmenopausal breast cancer [56, 67]. Again findings for premenopausal breast cancer remain inconsistent and inconclusive; as contrasted to BMI, however, two meta-analyses have shown an increased risk of premenopausal cancer in women with central adiposity [67, 68]. The results were heterogeneous, though, whereas the effect seemed to be stronger among women of Asian origin.
2.2 Exercise
Physical activity is considered an established primary breast cancer prevention strategy for both premenopausal and postmenopausal women [69]; indeed, sustained regular activity throughout life seems to provide the highest benefit [70]. Noticeably, it has been estimated that elimination of physical inactivity would result in a decrease of breast cancer incidence by 10% [71]. The first study aiming to assess this association, using a detailed lifetime physical activity assessment, showed a 58% decreased risk of breast cancer among premenopausal women with an average of 3.8 h of exercise per week, compared to those who reported no exercise [72]. Similarly, a decreased risk by 45% for breast cancer in postmenopausal women in the highest physical activity category was found [73]. A large recent meta-analysis summarizing evidence from 31 cohort studies confirmed the results and showed an overall 13% decrease in risk among women reporting the highest versus the lowest level of physical exercise. A dose-response pattern was recorded, and the overall estimate was stronger for premenopausal women and women with normal BMI values, compared to overweight, and confined to oestrogen/progesterone receptor-negative tumours [74]. Interestingly, in a systematic review of the literature, occupation-related, household, recreational and walking-associated physical activity all seemed to independently decrease the risk for breast cancer [75].
2.3 Underlying Mechanisms for Obesity and Exercise
The adverse effects of obesity and the beneficial actions of physical activity are generally considered to be exerted via common mechanisms. The proposed actions could be generally synopsized as (a) exposure to oestrogens, (b) changes in insulin-related factors and adipokines and (c) anti- or pro-inflammatory actions and other protective mechanisms. These are described below.
2.3.1 Exposure to Oestrogens
Body fat in postmenopausal women is a main source of oestrogen secretion via aromatization of androgens [76]. Therefore, the higher oestrogen levels in obese postmenopausal women seem to be responsible for the increased risk of breast cancer after menopause; similarly, the observed protective effects of physical activity seem to be mainly mediated by the subsequent body fat loss associated with regular exercise in this age group.
Physical activity, in premenopausal women, where the association between adiposity and breast cancer risk is reversed, seems to act via independent mechanisms. Specifically, high levels of physical exercise in reproductive years are associated with reduced levels of circulating oestradiol and progesterone, possibly because of irregular or anovulatory menstrual cycles or a shortened luteal phase. Lastly, in puberty, vigorous activity could delay the onset of menarche, which has been associated with a decreased risk of breast cancer.
2.3.2 Downregulation of Insulin-Related Factors
Physical activity may prevent breast tumour development by lowering levels of the hormones insulin and insulin-like growth factor-I (IGF-I) [77]. Decreased insulin upregulates sex hormone-binding globulin (SHBG), leading to lower levels of bioavailable oestradiol [78]; it also seems to decrease the bioavailability of IGF-I [79]. IGF-I acts as a mitogen in breast epithelial cells, promoting transformation and suppressing apoptosis [80]; consequently, lower circulating levels of IGF-I are associated with a decreased breast cancer risk [81].
2.3.3 Benefits on Obesity-Related Adipokine Levels
Adipose tissue is considered an endocrine organ which produces and secretes adipokines, involved in the mediation of inflammatory diseases and obesity. In a recent study, adiponectin, leptin, visfatin and resistin were all found to be risk factors for breast cancer in postmenopausal females. In particular, leptin, resistin and visfatin levels were positively correlated with TNM staging, tumour size, lymph node metastasis and histological grading in postmenopausal subgroups [82]. As a result, physical exercise and its inhibitory effect upon adipose tissue provide downregulatory signals for decreased adiponectin secretion.
2.3.4 Anti-inflammatory and Other Protective Mechanisms
Chronic inflammation is now considered a key process in carcinogenesis, and physical activity has been known to suppress increased levels of inflammation, whereas obesity is now recognized as a chronic inflammatory disorder [83, 84]. Other proposed protective mechanisms of exercise against breast cancer risk include an exercise-induced decrease in breast density, reduction in oxidative stress, enhancement of immune function, promotion of tumour suppressor genes and intracellular anticarcinogenic pathways [85].
3 Effects of Diet
Diet has been associated with the development or progression of major human cancers, including breast, prostate and colorectal tumours. It is a modifiable factor, which has been the subject of intensive research interest as it provides a window for preventive intervention strategies, due also to the immense interest of lay people in associating their dietary habits with cancer risk and breast cancer risk, in particular.
3.1 Macronutrients and Food Items
Among macronutrients and food items, dietary fibre has been proposed to reduce breast cancer risk via decreasing reabsorption of oestrogens in the gastrointestinal system [86], yet evidence remains inconclusive [87, 88]. Regarding fat intake, there are experimental studies suggesting that an increased fat intake could induce mammary gland tumours in rodents [89]. On a molecular level, fatty acids could influence the carcinogenic process through mechanisms related to modifications of cell membrane structure, metabolic effects and impact on translational signals and gene expression [87]; findings from humans, however, do not seem to strongly support this hypothesis [87, 88, 90]. Regarding other food groups, high dietary intake of carbohydrates has been suggested to increase breast cancer via induced hyperinsulinemia.
Many studies on the association of specific dietary factors with breast cancer have been published showing conflicting results, notably inverse, positive or null associations [91]. Briefly, consumption of fruit, vegetables and fish, as well as soy-based food and isoflavone intake, seems to be associated with decreased breast cancer risk, possibly on account of their antioxidant effects and the decrease in oestrogen levels related to soy-based food. Meat intake, apart from being associated with colorectal cancer, has been also found in some studies to increase breast cancer risk, but the evidence is limited [87, 88].
3.2 Dietary Patterns
A lower breast cancer incidence has been encountered by women who live in Mediterranean countries compared to those in Northern European countries, such as the UK or the USA; in this context, the Mediterranean pattern of diet has been considered as a tentative contributing factor. In the small MeDiet study, study subjects were randomized into a dietary intervention group (n = 58) following a traditional, controlled Mediterranean diet for 6 months and a control (n = 57) group, which continued to follow their regular diet. At baseline, no significant difference was observed in urinary levels of individual oestrogens comparing intervention and control women. After 6 months, however, whereas no major change was noted in the control group, as expected, women in the intervention group showed a significant reduction (over 40%, p < 0.02) of total oestrogen levels [92]. These findings need to be further confirmed in the hope that this strategy may be part of breast cancer prevention strategies. A number of studies have also explored whether the so-called Western diet, traditionally including high red and processed meats, refined grains, potatoes and starches, snacks, sweets, fried foods and soft drinks, impacts on breast cancer risk; the majority, however, have not found statistically significant associations [87].
3.3 Micronutrients
Evidence regarding the association of micronutrients with breast cancer risk in both premenopausal and postmenopausal women is not consistent. Despite the reported antioxidant effects of vitamin C, vitamin E and selenium, most cohort studies do not confirm these results. By contrast, the protective effect of vitamin A and retinol intake seems to merit further research [93] taking into account variations in absorption, metabolism and excretion of carotenoids between individuals [94].
Regarding other micronutrients, higher dietary folate intake has been associated with decreased breast cancer risk, especially among women reporting higher alcohol consumption indicating an interactive effect [95]. Similarly, a higher dietary intake of methionine, but not vitamin B6 and B12, has been proposed to have an inverse association, especially for postmenopausal women [96]. These molecules are considered essential for DNA synthesis, repair and methylation, and their deficiency could lead to DNA instability and proneness to carcinogenic mutations [97]. Lastly, there are some suggestions of an inverse association between vitamin D, as well as calcium intake and breast cancer risk [98, 99], which were not confirmed, however, in the results of a randomized trial assessing the link between use of combined calcium and vitamin D supplementation with breast cancer risk [100].
3.4 Alcohol Consumption
Alcohol consumption is considered to be causally related to breast cancer risk, with a 7–10% increase in risk for each 10 g (~1 drink) of alcohol daily consumption by premenopausal or postmenopausal women [101]. A dose-response pattern is noted with heavy drinking increasing the risk by approximately 60% and enhanced associations for hormone receptor-positive tumours [102]. Proposed mechanisms include the effect of alcohol on circulating oestrogen levels and the carcinogenic role of ethanol metabolites or the effect of alcohol on epithelial-mesenchymal transition, epithelium-stroma interaction and epigenetic regulation of gene expression in the breast [101]. Alcohol consumption may cause a rise in oestrogen levels by promoting aromatase activity that converts androgens to oestrogens, inhibiting oestrogen degradation, decreasing melatonin secretion that inhibits oestrogen production and increasing hepatic redox state that results in a decrease in steroid metabolism. Additionally, acetaldehyde and free radicals, alcohol metabolites, may cause DNA damage promoting carcinogenesis. Lastly, the decrease in folate levels due to antagonism by alcohol may contribute to breast cancer development [101].
3.5 Non-alcoholic Beverages
Caffeine was implicated in breast tumorigenesis, on account of an observation that coffee consumption reduction was associated with regression of fibrocystic breast disease [103]. The results of subsequent large cohort studies are synopsized in a recent meta-analysis [104] showing no association. Of note, however, are suggestions for a small inverse association specific for green tea consumption and its association with breast cancer incidence and recurrence, possibly on account of its antioxidant actions [105], which does not apply for black tea consumption [106].
4 Conclusions
Breast cancer remains the leading type of malignancy in women worldwide with a profoundly higher incidence in the developed compared to developing countries. Increasing trends have been evident in Western communities for several decades. Lifestyle changes leading to obesity and physical inactivity, higher alcohol consumption and variable use of exogenous oestrogens are believed to have contributed to the observed increase of the disease. Higher oestrogen exposure, indicated by proxies, such as earlier age at menarche, later menopause and adverse childbearing patterns, has been witnessed in parallel [107]. There is no strong evidence that other macro- or micronutrients are clearly included in the aetiology of the disease.
Intense research over the last few decades has broadened our understanding of the aetiology of the disease and revealed modifiable factors offering applicable preventive targets (◘ Fig. 4.2). According to the World Cancer Research Fund, 40% of postmenopausal breast cancers would have been prevented, where it is possible to reduce alcohol consumption, physical inactivity and obesity [41]. In order to formulate public health recommendations and tangible prevention guidelines, future research should focus on specific components of modifiable risk factors, such as type and timing of physical activity, and their geographical, ethnical and cultural customization. Indispensable is further exploration of the model of oestrogen- or other hormone-induced carcinogenesis, the findings of which should be clinically integrated into breast cancer prevention and control programmes.
Key Points
-
Oestrogens are involved in breast carcinogenesis by exerting proliferative effects on breast epithelial tissue.
-
High levels of serum oestrogens have been linked with increased risk of breast cancer, especially among postmenopausal women.
-
Proxies of high lifetime exposure to endogenous oestrogens, like early menarche and late menopause, are associated with increased risk of breast cancer, whereas premenopausal oophorectomy seems to decrease the subsequent risk. Childbearing and young age at first pregnancy decrease the lifetime risk for breast cancer.
-
Well-documented findings support the finding that the use of combined oestrogen-progesterone hormone replacement therapy (HRT) increases the risk for breast cancer in postmenopausal women.
-
Oral contraceptives, ovarian stimulation for infertility treatment and hormone therapy for transgender individuals do not seem to increase breast cancer risk.
-
A bimodal pattern has been observed regarding the association of obesity with breast cancer, with an increased risk for postmenopausal and a decreased risk for premenopausal women.
-
Physical exercise decreases the risk of breast cancer in a dose-response pattern, thus comprising a target for preventive strategies.
-
Body fat comprises the main source of oestrogens in postmenopausal women via aromatization of androgens, and this is thought to be the main mechanism underlying the aggravating effect of obesity, as well as the protective action of exercise. Other mechanisms include the IGF-I system, adipokines and inflammation.
-
Alcohol consumption is a well-established risk factor for breast cancer.
-
There is no consistent evidence regarding association with other dietary patterns.
References
Feigelson HS, Henderson BE. Estrogens and breast cancer. Carcinogenesis. 1996;17(11):2279–84.
Key TJ, Appleby PN, Reeves GK, Travis RC, Brinton LA, Helzlsouer KJ, et al. Steroid hormone measurements from different types of assays in relation to body mass index and breast cancer risk in postmenopausal women: reanalysis of eighteen prospective studies. Steroids. 2015;99(Pt A):49–55.
Key T, Appleby P, Barnes I, Reeves G, Endogenous H. Breast cancer collaborative G. Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst. 2002;94(8):606–16.
Sieri S, Krogh V, Bolelli G, Abagnato CA, Grioni S, Pala V, et al. Sex hormone levels, breast cancer risk, and cancer receptor status in postmenopausal women: the ORDET cohort. Cancer Epidemiol Biomark Prev. 2009;18(1):169–76.
Endogenous H, Breast Cancer Collaborative G, Key TJ, Appleby PN, Reeves GK, Travis RC, et al. Sex hormones and risk of breast cancer in premenopausal women: a collaborative reanalysis of individual participant data from seven prospective studies. Lancet Oncol. 2013;14(10):1009–19.
Collaborative Group on Hormonal Factors in Breast C. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13(11):1141–51.
Haslam SZ. The ontogeny of mouse mammary gland responsiveness to ovarian steroid hormones. Endocrinology. 1989;125(5):2766–72.
Madigan MP, Troisi R, Potischman N, Dorgan JF, Brinton LA, Hoover RN. Serum hormone levels in relation to reproductive and lifestyle factors in postmenopausal women (United States). Cancer Causes Control. 1998;9(2):199–207.
Rannevik G, Jeppsson S, Johnell O, Bjerre B, Laurell-Borulf Y, Svanberg L. A longitudinal study of the perimenopausal transition: altered profiles of steroid and pituitary hormones, SHBG and bone mineral density. Maturitas. 1995;21(2):103–13.
Irwin KL, Lee NC, Peterson HB, Rubin GL, Wingo PA, Mandel MG. Hysterectomy, tubal sterilization, and the risk of breast cancer. Am J Epidemiol. 1988;127(6):1192–201.
Trichopoulos D, MacMahon B, Cole P. Menopause and breast cancer risk. J Natl Cancer Inst. 1972;48(3):605–13.
Kelsey JL, Gammon MD, John EM. Reproductive factors and breast cancer. Epidemiol Rev. 1993;15(1):36–47.
Lambe M, Hsieh CC, Chan HW, Ekbom A, Trichopoulos D, Adami HO. Parity, age at first and last birth, and risk of breast cancer: a population-based study in Sweden. Breast Cancer Res Treat. 1996;38(3):305–11.
Lambe M, Hsieh C, Trichopoulos D, Ekbom A, Pavia M, Adami HO. Transient increase in the risk of breast cancer after giving birth. N Engl J Med. 1994;331(1):5–9.
Bernstein L, Ross RK. Endogenous hormones and breast cancer risk. Epidemiol Rev. 1993;15(1):48–65.
Ewertz M, Duffy SW, Adami HO, Kvale G, Lund E, Meirik O, et al. Age at first birth, parity and risk of breast cancer: a meta-analysis of 8 studies from the Nordic countries. Int J Cancer. 1990;46(4):597–603.
Russo J, Tay LK, Russo IH. Differentiation of the mammary gland and susceptibility to carcinogenesis. Breast Cancer Res Treat. 1982;2(1):5–73.
Mosher WD, Martinez GM, Chandra A, Abma JC, Willson SJ. Use of contraception and use of family planning services in the United States: 1982-2002. Adv Data. 2004;10(350):1–36.
Gierisch JM, Coeytaux RR, Urrutia RP, Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review. Cancer Epidemiol Biomark Prev. 2013;22(11):1931–43.
Kahlenborn C, Modugno F, Potter DM, Severs WB. Oral contraceptive use as a risk factor for premenopausal breast cancer: a meta-analysis. Mayo Clin Proc. 2006;81(10):1290–302.
Althuis MD, Brogan DR, Coates RJ, Daling JR, Gammon MD, Malone KE, et al. Hormonal content and potency of oral contraceptives and breast cancer risk among young women. Br J Cancer. 2003;88(1):50–7.
Collaborative Group on Hormonal Factors in Breast C. Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53 297 women with breast cancer and 100 239 women without breast cancer from 54 epidemiological studies. Lancet. 1996;347(9017):1713–27.
Isaksson E, von Schoultz E, Odlind V, Soderqvist G, Csemiczky G, Carlstrom K, et al. Effects of oral contraceptives on breast epithelial proliferation. Breast Cancer Res Treat. 2001;65(2):163–9.
Sergentanis TN, Diamantaras AA, Perlepe C, Kanavidis P, Skalkidou A, Petridou ET. IVF and breast cancer: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(1):106–23.
Zreik TG, Mazloom A, Chen Y, Vannucci M, Pinnix CC, Fulton S, et al. Fertility drugs and the risk of breast cancer: a meta-analysis and review. Breast Cancer Res Treat. 2010;124(1):13–26.
North American Menopause S. The 2012 hormone therapy position statement of: the North American Menopause Society. Menopause. 2012;19(3):257–71.
Furness S, Roberts H, Marjoribanks J, Lethaby A, Hickey M, Farquhar C. Hormone therapy in postmenopausal women and risk of endometrial hyperplasia. Cochrane Database Syst Rev. 2009;2:CD000402.
LeBlanc ES, Janowsky J, Chan BK, Nelson HD. Hormone replacement therapy and cognition: systematic review and meta-analysis. JAMA. 2001;285(11):1489–99.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the women’s health initiative randomized controlled trial. JAMA. 2002;288(3):321–33.
Chlebowski RT, Hendrix SL, Langer RD, Stefanick ML, Gass M, Lane D, et al. Influence of estrogen plus progestin on breast cancer and mammography in healthy postmenopausal women: the women’s health initiative randomized trial. JAMA. 2003;289(24):3243–53.
Shumaker SA, Legault C, Rapp SR, Thal L, Wallace RB, Ockene JK, et al. Estrogen plus progestin and the incidence of dementia and mild cognitive impairment in postmenopausal women: the women’s health initiative memory study: a randomized controlled trial. JAMA. 2003;289(20):2651–62.
Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Collaborative Group on Hormonal Factors in Breast Cancer. Lancet. 1997;350(9084):1047–59.
Chen WY, Manson JE, Hankinson SE, Rosner B, Holmes MD, Willett WC, et al. Unopposed estrogen therapy and the risk of invasive breast cancer. Arch Intern Med. 2006;166(9):1027–32.
Beral V, Million Women Study C. Breast cancer and hormone-replacement therapy in the Million women study. Lancet. 2003;362(9382):419–27.
Colditz GA, Hankinson SE, Hunter DJ, Willett WC, Manson JE, Stampfer MJ, et al. The use of estrogens and progestins and the risk of breast cancer in postmenopausal women. N Engl J Med. 1995;332(24):1589–93.
Schairer C, Byrne C, Keyl PM, Brinton LA, Sturgeon SR, Hoover RN. Menopausal estrogen and estrogen-progestin replacement therapy and risk of breast cancer (United States). Cancer Causes Control. 1994;5(6):491–500.
Hou N, Hong S, Wang W, Olopade OI, Dignam JJ, Huo D. Hormone replacement therapy and breast cancer: heterogeneous risks by race, weight, and breast density. J Natl Cancer Inst. 2013;105(18):1365–72.
Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–12.
Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study. Breast Cancer Res Treat. 2008;107(1):103–11.
Campagnoli C, Abba C, Ambroggio S, Peris C. Pregnancy, progesterone and progestins in relation to breast cancer risk. J Steroid Biochem Mol Biol. 2005;97(5):441–50.
Rosenberg LU, Magnusson C, Lindstrom E, Wedren S, Hall P, Dickman PW. Menopausal hormone therapy and other breast cancer risk factors in relation to the risk of different histological subtypes of breast cancer: a case-control study. Breast Cancer Res. 2006;8(1):R11.
Ursin G, Tseng CC, Paganini-Hill A, Enger S, Wan PC, Formenti S, et al. Does menopausal hormone replacement therapy interact with known factors to increase risk of breast cancer? J Clin Oncol. 2002;20(3):699–706.
Chen WY, Hankinson SE, Schnitt SJ, Rosner BA, Holmes MD, Colditz GA. Association of hormone replacement therapy to estrogen and progesterone receptor status in invasive breast carcinoma. Cancer. 2004;101(7):1490–500.
Li CI, Malone KE, Porter PL, Weiss NS, Tang MT, Cushing-Haugen KL, et al. Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA. 2003;289(24):3254–63.
Biglia N, Mariani L, Sgro L, Mininanni P, Moggio G, Sismondi P. Increased incidence of lobular breast cancer in women treated with hormone replacement therapy: implications for diagnosis, surgical and medical treatment. Endocr Relat Cancer. 2007;14(3):549–67.
Reeves GK, Beral V, Green J, Gathani T, Bull D, Million Women Study C. Hormonal therapy for menopause and breast-cancer risk by histological type: a cohort study and meta-analysis. Lancet Oncol. 2006;7(11):910–8.
Baber RJ, Panay N, Fenton ATIWG. 2016 IMS recommendations on women’s midlife health and menopause hormone therapy. Climacteric. 2016;19(2):109–50.
Panay N, Hamoda H, Arya R, Savvas M, British Menopause S, Women’s Health C. The 2013 British Menopause Society & Women’s health concern recommendations on hormone replacement therapy. Menopause Int. 2013;19(2):59–68.
Meriggiola MC, Jannini EA, Lenzi A, Maggi M, Manieri C. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline: commentary from a European perspective. Eur J Endocrinol. 2010;162(5):831–3.
Bosze P, Toth A, Torok M. Hormone replacement and the risk of breast cancer in Turner’s syndrome. N Engl J Med. 2006;355(24):2599–600.
Gooren LJ, van Trotsenburg MA, Giltay EJ, van Diest PJ. Breast cancer development in transsexual subjects receiving cross-sex hormone treatment. J Sex Med. 2013;10(12):3129–34.
Brown GR, Jones KT. Incidence of breast cancer in a cohort of 5,135 transgender veterans. Breast Cancer Res Treat. 2015;149(1):191–8.
Mueller A, Gooren L. Hormone-related tumors in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol. 2008;159(3):197–202.
Berger NA. Obesity and cancer pathogenesis. Ann N Y Acad Sci. 2014;1311:57–76.
Stephenson GD, Rose DP. Breast cancer and obesity: an update. Nutr Cancer. 2003;45(1):1–16.
Wiseman M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc. 2008;67(3):253–6.
Michels KB, Terry KL, Willett WC. Longitudinal study on the role of body size in premenopausal breast cancer. Arch Intern Med. 2006;166(21):2395–402.
Key TJ, Pike MC. The role of oestrogens and progestagens in the epidemiology and prevention of breast cancer. Eur J Cancer Clin Oncol. 1988;24(1):29–43.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371(9612):569–78.
Xia X, Chen W, Li J, Chen X, Rui R, Liu C, et al. Body mass index and risk of breast cancer: a nonlinear dose-response meta-analysis of prospective studies. Sci Rep. 2014;4:7480.
Ahn J, Schatzkin A, Lacey JV Jr, Albanes D, Ballard-Barbash R, Adams KF, et al. Adiposity, adult weight change, and postmenopausal breast cancer risk. Arch Intern Med. 2007;167(19):2091–102.
Carpenter CL, Ross RK, Paganini-Hill A, Bernstein L. Effect of family history, obesity and exercise on breast cancer risk among postmenopausal women. Int J Cancer. 2003;106(1):96–102.
Lahmann PH, Hoffmann K, Allen N, van Gils CH, Khaw KT, Tehard B, et al. Body size and breast cancer risk: findings from the European prospective investigation into cancer and nutrition (EPIC). Int J Cancer. 2004;111(5):762–71.
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE. Adult weight change and risk of postmenopausal breast cancer. JAMA. 2006;296(2):193–201.
Lahmann PH, Schulz M, Hoffmann K, Boeing H, Tjonneland A, Olsen A, et al. Long-term weight change and breast cancer risk: the European prospective investigation into cancer and nutrition (EPIC). Br J Cancer. 2005;93(5):582–9.
Michels KB, Terry KL, Eliassen AH, Hankinson SE, Willett WC. Adult weight change and incidence of premenopausal breast cancer. Int J Cancer. 2012;130(4):902–9.
Connolly BS, Barnett C, Vogt KN, Li T, Stone J, Boyd NF. A meta-analysis of published literature on waist-to-hip ratio and risk of breast cancer. Nutr Cancer. 2002;44(2):127–38.
Harvie M, Hooper L, Howell AH. Central obesity and breast cancer risk: a systematic review. Obes Rev. 2003;4(3):157–73.
Colditz GA, Bohlke K. Priorities for the primary prevention of breast cancer. CA Cancer J Clin. 2014;64(3):186–94.
Lynch BM, Neilson HK, Friedenreich CM. Physical activity and breast cancer prevention. Recent Results Cancer Res. 2011;186:13–42.
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–29.
Bernstein L, Henderson BE, Hanisch R, Sullivan-Halley J, Ross RK. Physical exercise and reduced risk of breast cancer in young women. J Natl Cancer Inst. 1994;86(18):1403–8.
Carpenter CL, Ross RK, Paganini-Hill A, Bernstein L. Lifetime exercise activity and breast cancer risk among post-menopausal women. Br J Cancer. 1999;80(11):1852–8.
Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. 2013;137(3):869–82.
Friedenreich CM, Cust AE. Physical activity and breast cancer risk: impact of timing, type and dose of activity and population subgroup effects. Br J Sports Med. 2008;42(8):636–47.
Grodin JM, Siiteri PK, MacDonald PC. Source of estrogen production in postmenopausal women. J Clin Endocrinol Metab. 1973;36(2):207–14.
Rao G. Insulin resistance syndrome. Am Fam Physician. 2001;63(6):1159–63. 65-6
Nestler JE, Powers LP, Matt DW, Steingold KA, Plymate SR, Rittmaster RS, et al. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991;72(1):83–9.
Conover CA, Lee PD, Kanaley JA, Clarkson JT, Jensen MD. Insulin regulation of insulin-like growth factor binding protein-1 in obese and nonobese humans. J Clin Endocrinol Metab. 1992;74(6):1355–60.
Sachdev D, Yee D. The IGF system and breast cancer. Endocr Relat Cancer. 2001;8(3):197–209.
Rinaldi S, Peeters PH, Berrino F, Dossus L, Biessy C, Olsen A, et al. IGF-I, IGFBP-3 and breast cancer risk in women: the European prospective investigation into cancer and nutrition (EPIC). Endocr Relat Cancer. 2006;13(2):593–605.
Assiri AM, Kamel HF, Hassanien MF. Resistin, visfatin, adiponectin, and leptin: risk of breast cancer in pre- and postmenopausal saudi females and their possible diagnostic and predictive implications as novel biomarkers. Dis Markers. 2015;2015:253519.
Moldoveanu AI, Shephard RJ, Shek PN. The cytokine response to physical activity and training. Sports Med. 2001;31(2):115–44.
Rundle A. Molecular epidemiology of physical activity and cancer. Cancer Epidemiol Biomark Prev. 2005;14(1):227–36.
Friedenreich CM. Physical activity and breast cancer: review of the epidemiologic evidence and biologic mechanisms. Recent Results Cancer Res. 2011;188:125–39.
Cohen LA. Dietary fiber and breast cancer. Anticancer Res. 1999;19(5A):3685–8.
Albuquerque RC, Baltar VT, Marchioni DM. Breast cancer and dietary patterns: a systematic review. Nutr Rev. 2014;72(1):1–17.
Vera-Ramirez L, Ramirez-Tortosa MC, Sanchez-Rovira P, Ramirez-Tortosa CL, Granados-Principal S, Lorente JA, et al. Impact of diet on breast cancer risk: a review of experimental and observational studies. Crit Rev Food Sci Nutr. 2013;53(1):49–75.
Fay MP, Freedman LS. Meta-analyses of dietary fats and mammary neoplasms in rodent experiments. Breast Cancer Res Treat. 1997;46(2–3):215–23.
Holmes MD, Liu S, Hankinson SE, Colditz GA, Hunter DJ, Willett WC. Dietary carbohydrates, fiber, and breast cancer risk. Am J Epidemiol. 2004;159(8):732–9.
Ferrini K, Ghelfi F, Mannucci R, Titta L. Lifestyle, nutrition and breast cancer: facts and presumptions for consideration. Ecancermedicalscience. 2015;9:557.
Carruba G, Cocciadiferro L, Di Cristina A, Granata OM, Dolcemascolo C, Campisi I, et al. Nutrition, aging and cancer: lessons from dietary intervention studies. Immun Ageing. 2016;13:13.
Fulan H, Changxing J, Baina WY, Wencui Z, Chunqing L, Fan W, et al. Retinol, vitamins a, C, and E and breast cancer risk: a meta-analysis and meta-regression. Cancer Causes Control. 2011;22(10):1383–96.
Stahl W, Sies H. Uptake of lycopene and its geometrical isomers is greater from heat-processed than from unprocessed tomato juice in humans. J Nutr. 1992;122(11):2161–6.
Chen P, Li C, Li X, Li J, Chu R, Wang H. Higher dietary folate intake reduces the breast cancer risk: a systematic review and meta-analysis. Br J Cancer. 2014;110(9):2327–38.
Wu W, Kang S, Zhang D. Association of vitamin B6, vitamin B12 and methionine with risk of breast cancer: a dose-response meta-analysis. Br J Cancer. 2013;109(7):1926–44.
Davis CD, Uthus EO. DNA methylation, cancer susceptibility, and nutrient interactions. Exp Biol Med (Maywood). 2004;229(10):988–95.
Hong Z, Tian C, Zhang X. Dietary calcium intake, vitamin D levels, and breast cancer risk: a dose-response analysis of observational studies. Breast Cancer Res Treat. 2012;136(1):309–12.
Chen P, Hu P, Xie D, Qin Y, Wang F, Wang H. Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res Treat. 2010;121(2):469–77.
Chlebowski RT, Johnson KC, Kooperberg C, Pettinger M, Wactawski-Wende J, Rohan T, et al. Calcium plus vitamin D supplementation and the risk of breast cancer. J Natl Cancer Inst. 2008;100(22):1581–91.
Liu Y, Nguyen N, Colditz GA. Links between alcohol consumption and breast cancer: a look at the evidence. Womens Health. 2015;11(1):65–77.
Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer. 2015;112(3):580–93.
Marshall LM, Hunter DJ, Connolly JL, Schnitt SJ, Byrne C, London SJ, et al. Risk of breast cancer associated with atypical hyperplasia of lobular and ductal types. Cancer Epidemiol Biomark Prev. 1997;6(5):297–301.
Li XJ, Ren ZJ, Qin JW, Zhao JH, Tang JH, Ji MH, et al. Coffee consumption and risk of breast cancer: an up-to-date meta-analysis. PLoS One. 2013;8(1):e52681.
Ogunleye AA, Xue F, Michels KB. Green tea consumption and breast cancer risk or recurrence: a meta-analysis. Breast Cancer Res Treat. 2010;119(2):477–84.
Nie XC, Dong DS, Bai Y, Xia P. Meta-analysis of black tea consumption and breast cancer risk: update 2013. Nutr Cancer. 2014;66(6):1009–14.
Britt K. Menarche, menopause, and breast cancer risk. Lancet Oncol. 2012;13(11):1071–2.
Munsell MF, Sprague BL, Berry DA, Chisholm G, Trentham-Dietz A. Body mass index and breast cancer risk according to postmenopausal estrogen progestin use and hormone receptor status. Epidemiol Rev. 2014;36(1):114–36.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Petridou, E.T., Georgakis, M.K., Antonopoulos, C.N. (2018). Effect of Oestrogen Exposure, Obesity, Exercise and Diet on Breast Cancer Risk. In: Wyld, L., Markopoulos, C., Leidenius, M., Senkus-Konefka, E. (eds) Breast Cancer Management for Surgeons. Springer, Cham. https://doi.org/10.1007/978-3-319-56673-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-56673-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56671-9
Online ISBN: 978-3-319-56673-3
eBook Packages: MedicineMedicine (R0)