Abstract
Objective
To comprehensively summarize the associations between retinol, vitamins A, C, and E and breast cancer, and quantitatively estimate their dose–response relationships.
Methods
We searched PubMed, Embase, and Cochrane databases (from January 1982 to 15 March 2011) and the references of the relevant articles in English with sufficient information to estimate relative risk or odds ratio and the 95% confidence intervals, and comparable categories of vitamins. Two reviewers independently extracted data using a standardized form, with any discrepancy adjudicated by the third reviewer.
Results
Overall, 51 studies met the inclusion criteria. Comparing the highest with the lowest intake, total vitamin A intake reduced the breast cancer risk by 17% (pooled OR = 0.83, 95% CI: 0.78–0.88). Further subgroup analysis based on study design did not change the significant reduction. Although the dietary vitamin A, dietary vitamin E, and total vitamin E intake all reduced breast cancer risk significantly when data from all studies were pooled, the results became nonsignificant when data from cohort studies were pooled. The significant association between total retinol intake and breast cancer in all studies became nonsignificant in case–control studies but remain significant in cohort studies. No significant dose–response relationship was observed in the higher intake of these vitamins with reduced breast cancer risk.
Conclusions
Our results indicate that both the total intake of vitamin A and retinol could reduce breast cancer risk. However, associations between other vitamins and breast cancer seem to be limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is by far the most frequent cancer among women with an estimated 1384,000 new cases and 458,000 deaths worldly in 2008 (GLOBOCAN 2008). Since the changes in the incidence of breast cancer among migrant populations were reported [1, 2], environmental factors, particularly dietary factors, have been postulated to play important roles in the etiology of breast cancer [2–4]. Retinol and vitamins A, C, and E are hypothesized to reduce the risk of breast cancer due to their roles in the regulation of cell differentiation and apoptosis (retinol, vitamin A) [5], anti-inflammation and antioxidant activities (vitamin E) [6], and prooxidant breakage of cellular oxidative DNA (vitamin C) [7]. A number of case–control and prospective cohort studies have investigated the relationships between these vitamins and breast cancer [8–32]. However, the results remain inconsistent. Three meta-analyses have been reported: the first on the association between dietary vitamin C and breast cancer in 1990 [33], pooling the results of 12 case–control studies; the second on the association between dietary vitamin C and breast cancer in 2000 [34], pooling the results of 4 case–control studies and 5 cohort studies; and the third on the association between vitamin E supplements and breast cancer in 2007 [35], pooling the results of 3 RCTs. No meta-analysis about the associations between retinol, vitamin A, and dietary vitamin E and breast cancer has been reported. Since the first three meta-analyses were published, 25 inconsistent observational studies with large sample have been published [8–32]. Meanwhile, among these vitamins, which one plays a greater role in breast cancer risk remains unclear. Therefore, we performed a meta-analysis and meta-regression to comprehensively and comparatively assess the associations between retinol, vitamins A, C, and E and breast cancer.
Materials and methods
Primary search strategy
We conducted a literature search using PubMed, Embase, and the Cochrane library from January 1982 to 15 March 2011 with the following keywords: “retinol,” “vitamin A,” “vitamin C,” “vitamin E,” “ascorbic acid,” “tocopherol,” and “breast, mammary cancer, and/or carcinoma and/or neoplasm.” Papers were restricted to human studies published in English. Additional articles were obtained from the reference lists of the selected articles, reviews, and from the PubMed option “Related articles.”
Criteria for inclusion and exclusion
Studies about the association between these vitamins and breast cancer, regardless of sample size, were only included if they met the following criteria: (1) Sufficient information was provided to estimate the relative risk (RR) or odds ratio (OR) and 95% confidence intervals. (2) The reported categories for consumption of these vitamins had to be comparable. (3) The studies were unrelated. (4) For articles with same population resources or overlapping datasets, the largest or most recent one was included.
Data extraction
Two reviewers (F.L. and C.X.) independently extracted data using a standardized data extraction form. Any discrepancy was discussed and adjudicated by a third reviewer (B.N.) until a consensus was achieved. Information extracted from each article included the following: first author, year of publication, country of origin (continent), type of study design, number of cases and controls, odds ratio (OR) or relative risk (RR), and corresponding 95% confidence intervals for “non-reference v.s. reference” intake including “the highest v.s. the lowest intake” and adjustment variables. The lowest intake level was defined as “reference intake,” and other intake levels were defined as “non-reference intake.” For subjects in different continents, data were extracted separately and categorized as Asia, Europe, and America. The studies were subgrouped into RCT, cohort, and case–control, which were further subgrouped into hospital-based and population-based case–control studies.
We considered these vitamins intake (retinol, vitamins A, C, and E) as combined intake if the authors only presented intake level but did not provide information about whether it was dietary intake or if the author stated that it was from supplements and dietary sources together. Otherwise, the dietary vitamin intake and dietary supplements were extracted separately.
The distributions of intake levels of these vitamins were partitioned into 2–5 categories in the articles reviewed. All the categories with different units (e.g., μg/day, mg/day, IU/day, and g/day) were converted into mg/day for retinol, vitamins C and E, and IU/day for vitamin A. The midpoint of every category was used as the intake level; for the highest category, the intake level was defined as it is 1.2 times [36].
For retinol, the highest intake level was approximately “6000 mg/day,” and the lowest intake level was about “1000 mg/day;” for vitamin A, they were about “10000 IU/day” and “3000 IU/day,” respectively; for vitamin C, they were about “300 mg/day” and “50 mg/day,” respectively; and for vitamin E, they were about “20 mg/day” and “4 mg/day,” respectively.
Most of the estimated associations between these vitamins and breast cancer were adjusted for some confounders or their combinations. If both the crude OR/RR and multivariate-adjusted OR/RR were provided, the one reflecting the greatest adjustment was extracted, as suggested by Chene et al. [37]. If only crude OR/RR or number of cases and controls was provided, the crude OR/RR or number of cases and controls was extracted to pool the risk estimates. For studies that displayed both crude OR/RR (95% CI) and multivariate-adjusted OR/RR (95% CI), the data were extracted separately and compared, as suggested by Trock et al. [38]. The ratio of the pooled odds ratios of adjusted ORs to crude ORs was considered as a confounding odds ratio (ORc). If ORc > 1, it indicated that ORs adjusted for confounding factors exhibited larger odds ratios than those not adjusted. Conversely, if ORc < 1, it indicated that ORs adjusted for confounding factors exhibited smaller odds ratios than those not adjusted [38].
Quality Score Assessment
The two reviewers (F.L. and C.X.) independently assessed the quality of the studies reviewed using the quality score assessment (Supplemental Table 2), which is based on both traditional epidemiological considerations and dietary issues. Total scores ranged from 0 (worst) to 22 (best) (Supplemental Table 3). Any differences were adjudicated by a third reviewer (B. N.).
Statistical analysis
We pooled study-specific ORs or RRs and 95% CI for both “individual non-reference v.s. reference intake” and “the highest intake v.s. the lowest intake” to evaluate the associations between these vitamins and breast cancer. I 2 was adopted to assess heterogeneity among studies [39]. When heterogeneity was not an issue (I 2 < 50%), fixed effect model with Mantel–Haenszel method was used to calculate the pooled OR. Otherwise, a random effect model with inverse variance method was used. Sensitivity analyses were carried out to evaluate whether the removal of one study at a time would influence the results and whether the category levels would influence the results. The significant α level of 0.05 was used.
For the dose–response analysis, the individual LnOR/RRs in a single study related to an exposure was modeled in the following way [36]:
x j , j = 1 …, j − 1 was the value of exposure in the jth non-reference exposure category, and bwas estimated by the inverse variance–weighted least squares as follows [36].
where w j = v−1, y j = lnRRj, and x was the value of exposure. When the j − 1 values of y j was independent, the standard error of b was:
The variance of the LnRR was calculated by the following way.
Based on b and the standard error of b in a single study, we calculated the OR and 95% CI corresponding to different exposure levels (3 exposure levels were used in our study) in every study and pooled the ORs and 95% CI corresponding to the 3 exposure levels of all these studies, respectively. At last, we conducted a trend test for the pooled ORs corresponding to the 3 exposure levels of these vitamins using Spearman’s correlation.
Publication bias was investigated with funnel plots. Furthermore, linear regression approach [40] and rank correlation method [41] were adopted. Meta-analysis was conducted with Comprehensive Meta-analysis (Version 2 Biostat, Inc., USA). Meta-regression was performed by SAS 9.1 (SAS Institute, Cary, NC, USA).
Results
Characteristics of included studies
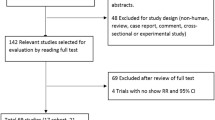
Figure 1 summarizes the process of identifying eligible articles. After screening, 51 studies entered the meta-analysis. As shown in Supplemental Table 1, there were 36 case–control studies, including 23 hospital-based case–control studies [10–12, 14, 16, 24, 26, 28, 29, 31, 42–54] and 13 population-based case–control studies [17–20, 22, 23, 25, 30, 32, 55–58], 2 nested case–control studies [13, 59], 1 case–cohort study [60], 9 cohort studies [8, 9, 15, 21, 27, 61–64], and 3 RCTs [65–67].
Results of meta-analysis for the associations between retinol, vitamins A, C, and E and breast cancer risk
Retinol
There were 23 studies on the relationship between total retinol and breast cancer. In one study, the ORs were analyzed in pre-and postmenopausal women, respectively [8], so we considered them to be 2 independent comparisons. As shown in Table 1, 24 comparisons entered the meta-analysis. Comparing “the highest” with “the lowest” intake, the total intake of retinol significantly reduced the breast cancer risk by 6% (pooled OR = 0.94, 95% CI: 0.89–0.99; p = 0.01; I 2 = 11.84%) (Table 1). Analysis based on study design found that the significant association remained only in the cohort studies (pooled OR = 0.91, 95% CI: 0.84–0.98; with I 2 = 27.34%) (Table 4).
The pooled ORs remained significant in premenopausal women when stratified by menopause status (Table 2) and in studies with quality score ≥ 16 stratified by quality score. A more significant association was observed in American studies (pooled OR = 0.88, 95% CI: 0.82–0.94; p < 0.01; I 2 = 0.00%) than in Asian and European studies (p = 0.02) (Table 3).
No significant association was observed both between the dietary intake and the combined intake of retinol and breast cancer risk.
Vitamin A
There were 22 studies on the relationship between vitamin A and breast cancer. In one study, the ORs were analyzed in pre- and postmenopausal women, respectively [29]. In another study [59], the ORs for total vitamin A and vitamin A supplements were analyzed separately, so we considered them to be 4 independent comparisons. As shown in Table 1, 24 comparisons entered the meta-analysis. Comparing “the highest” with “the lowest” intake, the total intake of vitamin A significantly reduced the breast cancer risk by 17% (pooled OR = 0.83, 95% CI: 0.78–0.88; p < 0.01; I 2 = 49.46%). Further subgroup analysis based on study design and continents of studies did not change the significant reduction, but the pooled ORs became nonsignificant in postmenopausal women (marginally significant in premenopausal women (p = 0.05)) when stratified by menopause status (Tables 1, 2, 3, 4; Fig. 2) and in studies with quality score < 16 stratified by quality score. A moderate significant association was observed in studies published before 2000 (p = 0.00) compared with studies published after 2000 (p = 0.11) (data not shown).
Since high heterogeneity existed in the case–control studies (I 2 = 56.12%), further subgroup analysis based on the types of control was performed, and the heterogeneity decreased in both subgroups. The pooled OR in the hospital-based case–control studies was 0.69 (95% CI: 0.61–0.78, with I 2 = 41.97%), significantly lower than that of population-based controls (pooled OR = 0.97, 95% CI: 0.77–1.22, with I 2 = 50.59%) (p = 0.01).
The dietary intake of vitamin A significantly reduced the breast cancer risk by 18% (OR = 0.82, 95% CI: 0.72–0.93; p < 0.01; I 2 = 59.71%). Analysis based on study design found that the significant association only remained in the case–control studies. The heterogeneity decreased in both subgroups of controls; the pooled OR in the hospital-based case–control studies was 0.69 (I 2 = 51.95%, 95% CI: 0.55–0.88), not significantly lower than that of population-based controls (pooled OR = 0.86, 95% CI: 0.76–0.96; I 2 = 44.42%) (p = 0.20).
The combined intake of vitamin A also reduced the breast cancer risk significantly, but we did not conduct subgroup analysis because of few studies. Only marginal significance was observed between vitamin A supplements and the breast cancer risk.
Vitamin C
There were 37 studies on the relationship between vitamin C and breast cancer. In 3 studies, the ORs were analyzed in pre-and postmenopausal women, respectively [8, 23, 27]. In 3 other studies [55, 59, 64], the ORs for dietary vitamin C (or total vitamin C) and vitamin C supplements were analyzed separately, so we considered them to be 12 independent comparisons. As shown in Table 1, 43 comparisons entered the meta-analysis. Comparing “the highest” with “the lowest” intake, the total intake of vitamin C significantly reduced the breast cancer risk by 15% (OR = 0.85, 95% CI: 0.77–0.93; p < 0.01, I 2 = 76.78%); the dietary intake of vitamin C significantly reduced the risk by 23% (OR = 0.77, 95% CI: 0.68–0.87; p < 0.01, I 2 = 80.48%). In further subgroup analysis based on study design, both the significant associations remained only in the case–control studies.
The heterogeneity for the association between total vitamin C and breast cancer decreased in the population-based case–control studies, but it was slightly increased in the hospital-based case–control studies. The pooled OR in the hospital-based case–control studies was 0.52 (95% CI: 0.39–0.71, with I 2 = 85.00%), significantly lower than that of population-based controls (pooled OR = 0.94, 95% CI: 0.86–1.03, with I 2 = 38.23%) (p < 0.01). The heterogeneity for the association between dietary vitamin C and breast cancer also decreased in the population-based case–control studies (I 2 = 30.89%), but it was slightly increased in the hospital-based case–control studies (I 2 = 85.88%). The pooled ORs were significantly lower in the hospital-based case–control studies than those of population-based case–control studies (p < 0.01).
Because of high heterogeneity (I 2 = 85.00%) and relatively lower pooled OR for the association between total vitamin C and breast cancer in the hospital-based case–control studies, we further conducted subgroup analysis based on continent and year of publication. The heterogeneity decreased in the 4 Asian studies, but it was slightly increased in the 2 American studies and the 8 European studies. The heterogeneity also decreased to some extent both in the studies published before and after 2000; the pooled OR in the studies published before 2000 was 0.65 (95% CI: 0.48–0.87; with I 2 = 76.03%), significantly different from that of studies published after 2000 (OR = 0.38, 95% CI: 0.25–0.58; with I 2 = 72.96%).
Adverse association between vitamin C supplements and breast cancer was observed; however, the pooled OR became nonsignificant (pooled OR = 1.04, 95% CI: 0.94–1.15) excluding the study by Cui et al. [21], which accounted for 45.14% weights of the meta-analysis. No significant association was observed in the combined intake of vitamin C and breast cancer with pooled OR of 0.99 (95% CI: 0.88–1.10; I 2 = 59.39%).
Vitamin E
There were 38 studies on the relationship between vitamin E and breast cancer. In 3 studies, the pooled ORs were analyzed in pre- and postmenopausal women, respectively [23, 27, 29]. Two other studies [55, 59] analyzed dietary vitamin E (or total vitamin E) and vitamin E supplements separately, so we considered them to be 10 independent comparisons. As shown in Table 1, 43 comparisons entered the meta-analysis. Comparing “the highest” with “the lowest” intake, total intake of vitamin E significantly reduced the breast cancer risk by 11% (OR = 0.89, 95% CI: 0.81–0.97; p = 0.01, I 2 = 68.27%); dietary intake of vitamin E significantly reduced the risk by 18% (OR = 0.82, 95% CI: 0.73–0.91; p < 0.01, I 2 = 72.06%). In further subgroup analysis based on study design, both the significant association between total and dietary vitamin E and breast cancer became nonsignificant in cohort studies.
The heterogeneity for the association between total vitamin E and breast cancer decreased in the population-based case–control studies, but it was slightly increased in the hospital-based case–control studies. The pooled OR in the hospital-based case–control studies was 0.72 (95% CI: 0.56–0.93, with I 2 = 76.90%), not significantly different from that of population-based controls (pooled OR = 0.89, 95% CI: 0.75–1.05, with I 2 = 55.85%) (p = 0.17). The heterogeneity for the association between dietary vitamin E and breast cancer was reduced in both subgroups of controls. No significant difference was observed between the pooled ORs in the 14 hospital-based case–control studies (pooled OR = 0.65, 95% CI: 0.51–0.83, with I 2 = 68.96%) and those of 6 population-based case–control studies (pooled OR = 0.87, 95% CI: 0.77–0.98, with I 2 = 45.22%) (p = 0.07).
No significant associations were observed in the associations between vitamin E supplements and combined intake of vitamin E and breast cancer.
We also conducted the pooled OR comparing every non-reference category with the lowest category. Because of the smaller increment of the intake levels of these vitamins, significance was only observed in some of the individual estimates between these vitamins and breast cancer (Supplemental Table 4).
Results of sensitivity analysis
The removal of one study had no significant influence on the pooled ORs of the associations between retinol, vitamins A, C, and E and breast cancer, respectively.
Five of the 18 studies on the association between dietary vitamin A and breast cancer provided far lower category of intake levels [22, 25, 26, 31, 42], and the pooled OR of the 5 studies was similar (pooled OR = 0.83, 95% CI: 0.76–0.92) to the pooled OR based on the 18 studies (pooled OR = 0.82, 95% CI: 0.72–0.93); another study by Zhang [28] did not provide the category of intake levels. Omitting one of the 6 studies had no influence on the pooled ORs, and when all the 6 studies were omitted, the pooled ORs for the association between dietary vitamin A and breast cancer became nonsignificant (pooled OR = 0.92, 95% CI: 0.84–1.01).
Dose–response relationship
We identified a significant dose–response relationship in higher intake of total retinol and reduced breast cancer risk (p = 0.04), which was influenced by one study [54]. Excluding the study made the significant dose–response relationship become marginally significant (p = 0.06). No significant dose–response relationship was observed in increasing intake of vitamins A, C, and E and risk reduction of breast cancer (Table 5).
Confounding OR
All the ORcs were lower than 1 without statistical significance except the ORc of the association between dietary vitamin A intake and breast cancer risk (ORc = 1.08) (data not shown).
Publication bias
Publication bias was observed in the associations between dietary vitamin C, total vitamin C, and vitamin E supplements and breast cancer using Begger’s regression and Egger’s regression approach. After adjustment with Trim and fill method, both the significant associations between dietary and total vitamin C and breast cancer became nonsignificant, and the association between vitamin E supplements and breast cancer was still nonsignificant. Details are summarized in Table 6. The funnel plots for associations between total retinol, total vitamins A, C, and E and breast cancer are shown in Fig. 3.
In subgroup analyses stratifying by study design, publication bias for the associations between dietary and total vitamin C and breast cancer was only observed in the case–control studies. The adjustment by Trim and fill method made the associations between dietary and total vitamin C and breast cancer in the case–control studies both become nonsignificant.
Discussion
Our meta-analysis suggested that the total vitamin A intake significantly reduced breast cancer risk; further subgroup analysis based on study design did not change the significant reduction. Both combined intake of vitamin A and vitamin A supplements reduced breast cancer risk significantly. The associations between total retinol, dietary and total vitamin E, dietary vitamin A and breast cancer were limited by study design.
Considered the intake levels of these vitamins, the intake levels of retinol and vitamin A varied largely across studies reviewed. For total retinol and total vitamin A, removal of the studies that provided far lower category levels had no influence on the pooled ORs. For dietary vitamin A, 5 of the 18 studies provided far lower category levels [22, 25, 26, 31, 42], and omitting all the 5 studies made the pooled ORs become nonsignificant. The intake levels of vitamins C and E were relatively comparable; the category of intake levels had little influence on the pooled ORs. In order to eliminate the variance of category levels, we conducted meta-regression. No significant dose–response relationship was observed in increasing intake of these vitamins and risk reduction of breast cancer.
In our meta-analysis, total and dietary vitamin C intake could not significantly reduce the risk of breast cancer, which was different from the significant result of the meta-analysis by Gandini et al. [34] (OR = 0.80, 95% CI: 0.68–0.95, pooling the results of 5 cohort and 4 case–control studies) and another meta-analysis by Howe et al. [33] (OR = 0.69, p < 0.001, pooling the results of 12 case–control studies). Since subgroup analysis showed that dietary vitamin C intake significantly reduced breast cancer risk only in case–control studies but not in cohort studies, more cohort studies were included in our meta-analysis than those in the meta-analysis by Gandini et al. [34]. The nonsignificant association may be limited by the cohort studies without significance. Adverse association between vitamin C supplements and breast cancer was observed in our meta-analysis. After excluding the study by Cui et al. [21], which accounted for 45.14% weights of the meta-analysis, the pooled RR became nonsignificant (pooled RR = 1.04, 95% CI: 0.94–1.15), similar to the single RCT [67]. The benefit effect of vitamin C supplements in the primary prevention of breast cancer seems to be limited.
The result of this meta-analysis on the association between dietary vitamin E and breast cancer was similar to that on the association between vitamin E supplements and breast cancer [35], on pooling the results of 3 RCTs with a null result. Maybe vitamin E has an effect only in combination with other dietary components, such as polyunsaturated fatty acids [68], or that a vitamin E supplement may confer protection against breast cancer among women with insufficient dietary intake of vitamin E [18].
In subgroup analyses, all the associations between dietary vitamins A, C, and E and breast cancer were significant in the case–control studies, but not in the cohort studies, with exception of the significant association between total vitamin A and breast cancer both in the case–control and cohort studies and the significant association between total retinol and breast cancer in the cohort studies but nonsignificant in the case–control studies. This may be caused by larger recall bias in the case–control studies for vitamins A, C, and E.
The heterogeneity persisted in case–control studies, but the cohort studies had little heterogeneity with exception of cohort studies on association between total vitamin C and breast cancer. The high heterogeneity in this meta-analysis may be due to the following reasons: (1) various ages of the study population; (2) the different stages of breast cancer patients, 5 case–control studies only involving invasive breast cancer patients [16, 17, 25, 29, 32]; (3) the bias from the collection of dietary information, the definition of food groups, and the diverse time periods before interview across studies especially in the case–control studies.
The pooled ORs generated on the 51 studies can significantly increase the statistical power. However, like all meta-analyses, limitations should be considered in this meta-analysis. Firstly, the interactions among these vitamins may reinforce the associations with breast cancer. Lack of the original data of the studies reviewed limited our further evaluation of potential interactions. Secondly, studies focused on the associations between these vitamins and breast cancer were relatively less in Asia. Finally, not all studies on these vitamins were used to calculate meta-regression because of non-comparable reference category, especially with respect to dose levels.
Conclusions
Our results indicate that higher total vitamin A and retinol intake could significantly reduce breast cancer risk. Association between other vitamins and breast cancer seems to be limited by study design. Given these limitations and the results of this meta-analysis, it is premature to recommend higher dietary vitamin A, any kinds of vitamin C intake and vitamin E intake for the primary prevention of breast cancer.
References
Buell P (1973) Changing incidence of breast cancer in Japanese-American women. J Natl Cancer Inst 51(5):1479–1483
Thomas DB, Karagas MR (1987) Cancer in first and second generation Americans. Cancer Res 47(21):5771–5776
Armstrong B, Doll R (1975) Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer 15(4):617–631
Kelsey JL, Horn-Ross PL (1993) Breast cancer: magnitude of the problem and descriptive epidemiology. Epidemiol Rev 15(1):7–16
Altucci L, Gronemeyer H (2001) The promise of retinoids to fight against cancer. Nat Rev Cancer 1(3):181–193
Aggarwal BB, Sundaram C, Prasad S, Kannappan R (2010) Tocotrienols, the vitamin E of the 21st century: its potential against cancer and other chronic diseases. Biochem Pharmacol 80(11):1613–1631
Ullah MF, Khan HY, Zubair H, Shamim U, Hadi SM (2011) The antioxidant ascorbic acid mobilizes nuclear copper leading to a prooxidant breakage of cellular DNA: implications for chemotherapeutic action against cancer. Cancer Chemother Pharmacol 67(1):103–110
Zhang S, Hunter DJ, Forman MR, Rosner BA, Speizer FE, Colditz GA, Manson JE, Hankinson SE, Willett WC (1999) Dietary carotenoids and vitamins A, C, and E and risk of breast cancer. J Natl Cancer Inst 91(6):547–556
Cho E, Spiegelman D, Hunter DJ, Chen WY, Zhang SM, Colditz GA, Willett WC (2003) Premenopausal intakes of vitamins A, C, and E, folate, and carotenoids, and risk of breast cancer. Cancer Epidemiol Biomarkers Prev 12(8):713–720
Bohlke K, Spiegelman D, Trichopoulou A, Katsouyanni K, Trichopoulos D (1999) Vitamins A, C and E and the risk of breast cancer: results from a case-control study in Greece. Br J Cancer 79(1):23–29
Ronco A, De Stefani E, Boffetta P, Deneo-Pellegrini H, Mendilaharsu M, Leborgne F (1999) Vegetables, fruits, and related nutrients and risk of breast cancer: a case-control study in Uruguay. Nutr Cancer 35(2):111–119
Adzersen KH, Jess P, Freivogel KW, Gerhard I, Bastert G (2003) Raw and cooked vegetables, fruits, selected micronutrients, and breast cancer risk: a case-control study in Germany. Nutr Cancer 46(2):131–137
Nissen SB, Tjonneland A, Stripp C, Olsen A, Christensen J, Overvad K, Dragsted LO, Thomsen B (2003) Intake of vitamins A, C, and E from diet and supplements and breast cancer in postmenopausal women. Cancer Causes Control 14(8):695–704
Levi F, Pasche C, Lucchini F, La Vecchia C (2001) Dietary intake of selected micronutrients and breast-cancer risk. Int J Cancer 91(2):260–263
Michels KB, Holmberg L, Bergkvist L, Ljung H, Bruce A, Wolk A (2001) Dietary antioxidant vitamins, retinol, and breast cancer incidence in a cohort of Swedish women. Int J Cancer 91(4):563–567
Do MH, Lee SS, Jung PJ, Lee MH (2003) Intake of dietary fat and vitamin in relation to breast cancer risk in Korean women: a case-control study. J Korean Med Sci 18(4):534–540
Moorman PG, Ricciuti MF, Millikan RC, Newman B (2001) Vitamin supplement use and breast cancer in a North Carolina population. Public Health Nutr 4(3):821–827
Dorjgochoo T, Shrubsole MJ, Shu XO, Lu W, Ruan Z, Zheng Y, Cai H, Dai Q, Gu K, Gao YT et al (2008) Vitamin supplement use and risk for breast cancer: the Shanghai Breast Cancer Study. Breast Cancer Res Treat 111(2):269–278
Wang C, Baumgartner RN, Yang D, Slattery ML, Murtaugh MA, Byers T, Hines LM, Giuliano AR, Baumgartner KB (2009) No evidence of association between breast cancer risk and dietary carotenoids, retinols, vitamin C and tocopherols in Southwestern Hispanic and non-Hispanic White women. Breast Cancer Res Treat 114(1):137–145
Challier B, Perarnau JM, Viel JF (1998) Garlic, onion and cereal fibre as protective factors for breast cancer: a French case-control study. Eur J Epidemiol 14(8):737–747
Cui Y, Shikany JM, Liu S, Shagufta Y, Rohan TE (2008) Selected antioxidants and risk of hormone receptor-defined invasive breast cancers among postmenopausal women in the Women’s Health Initiative Observational Study. Am J Clin Nutr 87(4):1009–1018
Malin AS, Qi D, Shu XO, Gao YT, Friedmann JM, Jin F, Zheng W (2003) Intake of fruits, vegetables and selected micronutrients in relation to the risk of breast cancer. Int J Cancer 105(3):413–418
Gaudet MM, Britton JA, Kabat GC, Steck-Scott S, Eng SM, Teitelbaum SL, Terry MB, Neugut AI, Gammon MD (2004) Fruits, vegetables, and micronutrients in relation to breast cancer modified by menopause and hormone receptor status. Cancer Epidemiol Biomarkers Prev 13(9):1485–1494
Mannisto S, Pietinen P, Virtanen M, Kataja V, Uusitupa M (1999) Diet and the risk of breast cancer in a case-control study: does the threat of disease have an influence on recall bias? J Clin Epidemiol 52(5):429–439
Mignone LI, Giovannucci E, Newcomb PA, Titus-Ernstoff L, Trentham-Dietz A, Hampton JM, Willett WC, Egan KM (2009) Dietary carotenoids and the risk of invasive breast cancer. Int J Cancer 124(12):2929–2937
Sharhar S, Normah H, Fatimah A, Fadilah RN, Rohi GA, Amin I, Cham BG, Rizal RM, Fairulnizal MN (2008) Antioxidant intake and status, and oxidative stress in relation to breast cancer risk: a case-control study. Asian Pac J Cancer Prev 9(2):343–349
Nagel G, Linseisen J, van Gils CH, Peeters PH, Boutron-Ruault MC, Clavel-Chapelon F, Romieu I, Tjonneland A, Olsen A, Roswall N et al (2010) Dietary beta-carotene, vitamin C and E intake and breast cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Breast Cancer Res Treat 119(3):753–765
Zhang CX, Ho SC, Chen YM, Fu JH, Cheng SZ, Lin FY (2009) Greater vegetable and fruit intake is associated with a lower risk of breast cancer among Chinese women. Int J Cancer 125(1):181–188
Bonilla-Fernandez P, Lopez-Cervantes M, Torres-Sanchez LE, Tortolero-Luna G, Lopez-Carrillo L (2003) Nutritional factors and breast cancer in Mexico. Nutr Cancer 45(2):148–155
Potischman N, Swanson CA, Coates RJ, Gammon MD, Brogan DR, Curtin J, Brinton LA (1999) Intake of food groups and associated micronutrients in relation to risk of early-stage breast cancer. Int J Cancer 82(3):315–321
Lee MM, Chang IY, Horng CF, Chang JS, Cheng SH, Huang A (2005) Breast cancer and dietary factors in Taiwanese women. Cancer Causes Control 16(8):929–937
Longnecker MP, Newcomb PA, Mittendorf R, Greenberg ER, Willett WC (1997) Intake of carrots, spinach, and supplements containing vitamin A in relation to risk of breast cancer. Cancer Epidemiol Biomarkers Prev 6(11):887–892
Howe GR, Hirohata T, Hislop TG, Iscovich JM, Yuan JM, Katsouyanni K, Lubin F, Marubini E, Modan B, Rohan T et al (1990) Dietary factors and risk of breast cancer: combined analysis of 12 case-control studies. J Natl Cancer Inst 82(7):561–569
Gandini S, Merzenich H, Robertson C, Boyle P (2000) Meta-analysis of studies on breast cancer risk and diet: the role of fruit and vegetable consumption and the intake of associated micronutrients. Eur J Cancer 36(5):636–646
Alkhenizan A, Hafez K (2007) The role of vitamin E in the prevention of cancer: a meta-analysis of randomized controlled trials. Ann Saudi Med 27(6):409–414
Berlin JA, Longnecker MP, Greenland S (1993) Meta-analysis of epidemiologic dose-response data. Epidemiology 4(3):218–228
Chene G, Thompson SG (1996) Methods for summarizing the risk associations of quantitative variables in epidemiologic studies in a consistent form. Am J Epidemiol 144(6):610–621
Trock BJ, Hilakivi-Clarke L, Clarke R (2006) Meta-analysis of soy intake and breast cancer risk. J Natl Cancer Inst 98(7):459–471
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Negri E, La Vecchia C, Franceschi S, D’Avanzo B, Talamini R, Parpinel M, Ferraroni M, Filiberti R, Montella M, Falcini F et al (1996) Intake of selected micronutrients and the risk of breast cancer. Int J Cancer 65(2):140–144
Graham S, Marshall J, Mettlin C, Rzepka T, Nemoto T, Byers T (1982) Diet in the epidemiology of breast cancer. Am J Epidemiol 116(1):68–75
Zaridze D, Lifanova Y, Maximovitch D, Day NE, Duffy SW (1991) Diet, alcohol consumption and reproductive factors in a case-control study of breast cancer in Moscow. Int J Cancer 48(4):493–501
Katsouyanni K, Willett W, Trichopoulos D, Boyle P, Trichopoulou A, Vasilaros S, Papadiamantis J, MacMahon B (1988) Risk of breast cancer among Greek women in relation to nutrient intake. Cancer 61(1):181–185
Lee HP, Gourley L, Duffy SW, Esteve J, Lee J, Day NE (1991) Dietary effects on breast-cancer risk in Singapore. Lancet 337(8751):1197–1200
London SJ, Stein EA, Henderson IC, Stampfer MJ, Wood WC, Remine S, Dmochowski JR, Robert NJ, Willett WC (1992) Carotenoids, retinol, and vitamin E and risk of proliferative benign breast disease and breast cancer. Cancer Causes Control 3(6):503–512
Qi XY, Zhang AY, Wu GL, Pang WZ (1994) The association between breast cancer and diet and other factors. Asia Pac J Public Health 7(2):98–104
Levi F, La Vecchia C, Gulie C, Negri E (1993) Dietary factors and breast cancer risk in Vaud, Switzerland. Nutr Cancer 19(3):327–335
Potischman N, McCulloch CE, Byers T, Nemoto T, Stubbe N, Milch R, Parker R, Rasmussen KM, Root M, Graham S (1990) Breast cancer and dietary and plasma concentrations of carotenoids and vitamin A. Am J Clin Nutr 52(5):909–915
Landa MC, Frago N, Tres A (1994) Diet and the risk of breast cancer in Spain. Eur J Cancer Prev 3(4):313–320
Richardson S, Gerber M, Cenee S (1991) The role of fat, animal protein and some vitamin consumption in breast cancer: a case control study in southern France. Int J Cancer 48(1):1–9
Marubini E, Decarli A, Costa A, Mazzoleni C, Andreoli C, Barbieri A, Capitelli E, Carlucci M, Cavallo F, Monferroni N et al (1988) The relationship of dietary intake and serum levels of retinol and beta-carotene with breast cancer. Results of a case-control study. Cancer 61(1):173–180
La Vecchia C, Decarli A, Franceschi S, Gentile A, Negri E, Parazzini F (1987) Dietary factors and the risk of breast cancer. Nutr Cancer 10(4):205–214
Freudenheim JL, Marshall JR, Vena JE, Laughlin R, Brasure JR, Swanson MK, Nemoto T, Graham S (1996) Premenopausal breast cancer risk and intake of vegetables, fruits, and related nutrients. J Natl Cancer Inst 88(6):340–348
Graham S, Hellmann R, Marshall J, Freudenheim J, Vena J, Swanson M, Zielezny M, Nemoto T, Stubbe N, Raimondo T (1991) Nutritional epidemiology of postmenopausal breast cancer in western New York. Am J Epidemiol 134(6):552–566
Iscovich JM, Iscovich RB, Howe G, Shiboski S, Kaldor JM (1989) A case-control study of diet and breast cancer in Argentina. Int J Cancer 44(5):770–776
Rohan TE, McMichael AJ, Baghurst PA (1988) A population-based case-control study of diet and breast cancer in Australia. Am J Epidemiol 128(3):478–489
Rohan TE, Howe GR, Friedenreich CM, Jain M, Miller AB (1993) Dietary fiber, vitamins A, C, and E, and risk of breast cancer: a cohort study. Cancer Causes Control 4(1):29–37
Verhoeven DT, Assen N, Goldbohm RA, Dorant E, van’t Veer P, Sturmans F, Hermus RJ, van den Brandt PA (1997) Vitamins C and E, retinol, beta-carotene and dietary fibre in relation to breast cancer risk: a prospective cohort study. Br J Cancer 75(1):149–155
Kushi LH, Fee RM, Sellers TA, Zheng W, Folsom AR (1996) Intake of vitamins A, C, and E and postmenopausal breast cancer. The Iowa Women’s Health Study. Am J Epidemiol 144(2):165–174
Hunter DJ, Manson JE, Colditz GA, Stampfer MJ, Rosner B, Hennekens CH, Speizer FE, Willett WC (1993) A prospective study of the intake of vitamins C, E, and A and the risk of breast cancer. N Engl J Med 329(4):234–240
Graham S, Zielezny M, Marshall J, Priore R, Freudenheim J, Brasure J, Haughey B, Nasca P, Zdeb M (1992) Diet in the epidemiology of postmenopausal breast cancer in the New York State Cohort. Am J Epidemiol 136(11):1327–1337
Shibata A, Paganini-Hill A, Ross RK, Henderson BE (1992) Intake of vegetables, fruits, beta-carotene, vitamin C and vitamin supplements and cancer incidence among the elderly: a prospective study. Br J Cancer 66(4):673–679
Lee IM, Cook NR, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE (2005) Vitamin E in the primary prevention of cardiovascular disease and cancer: the Women’s Health Study: a randomized controlled trial. Jama 294(1):56–65
Lonn E, Bosch J, Yusuf S, Sheridan P, Pogue J, Arnold JM, Ross C, Arnold A, Sleight P, Probstfield J et al (2005) Effects of long-term vitamin E supplementation on cardiovascular events and cancer: a randomized controlled trial. JAMA 293(11):1338–1347
Lin J, Cook NR, Albert C, Zaharris E, Gaziano JM, Van Denburgh M, Buring JE, Manson JE (2009) Vitamins C and E and beta carotene supplementation and cancer risk: a randomized controlled trial. J Natl Cancer Inst 101(1):14–23
Gower JD (1988) A role for dietary lipids and antioxidants in the activation of carcinogens. Free Radic Biol Med 5(2):95–111
Acknowledgments
Thanks J. Love for reviewing the paper.
Conflict of interest
All authors read and approved the final manuscript. None of the authors had any conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fulan, H., Changxing, J., Baina, W.Y. et al. Retinol, vitamins A, C, and E and breast cancer risk: a meta-analysis and meta-regression. Cancer Causes Control 22, 1383–1396 (2011). https://doi.org/10.1007/s10552-011-9811-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-011-9811-y