Abstract
As described throughout this book, most strokes occur secondary to the interaction of multiple genes in combination with both lifestyle and environmental factors, thereby making stroke a prototypical complex disease. While this may be true for most forms of ischemic and hemorrhagic stroke, there are several established monogenetic disorders (i.e., transmitted via Mendelian inheritance) that may present with stroke. In some situations, stroke can be the predominant clinical feature, while in others, stroke can occur infrequently. In this chapter, we will describe such disorders focusing on clinical manifestations (Table 10.1) and then present details regarding the established genetic and diagnostic testing (Table 10.2) that are available. Given the disparate relationships between these disorders and stroke, the disorders have been classified in Tables 10.1 and 10.2 based upon their predominant etiologic mechanisms, including large arterial diseases, small vessel diseases, hematological diseases, mitochondrial diseases, and connective tissue disorders. The disorders are presented in the same order in both tables. For completeness and ease of reference, we have also included several monogenetic disorders in our tables that have dedicated chapters elsewhere in this book, including MELAS syndrome (see Chap. 8), CADASIL syndrome (see Chap. 6), and sickle cell disease (see Chap. 9).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
As described throughout this book, most strokes occur secondary to the interaction of multiple genes in combination with both lifestyle and environmental factors, thereby making stroke a prototypical complex disease. While this may be true for most forms of ischemic and hemorrhagic stroke, there are several established monogenetic disorders (i.e., transmitted via Mendelian inheritance) that may present with stroke. In some situations, stroke can be the predominant clinical feature, while in others, stroke can occur infrequently. In this chapter, we will describe such disorders focusing on clinical manifestations (Table 10.1) and then present details regarding the established genetic and diagnostic testing (Table 10.2) that are available. Given the disparate relationships between these disorders and stroke, the disorders have been classified in Tables 10.1 and 10.2 based upon their predominant etiologic mechanisms, including large arterial diseases, small vessel diseases, hematological diseases, mitochondrial diseases, and connective tissue disorders. The disorders are presented in the same order in Tables 10.1 and 10.2. For completeness and ease of reference, we have also included several monogenetic disorders in our tables that have dedicated chapters elsewhere in this book, including MELAS syndrome (see Chap. 8), CADASIL syndrome (see Chap. 6), and sickle cell disease (see Chap. 9).
We also emphasize that an outstanding reference for such disorders is Online Mendelian Inheritance in Man (OMIM).Footnote 1 This database catalogues all known diseases with a genetic component and—when possible—links them to the relevant genes in the human genome and provides references for further research and tools for genomic analysis of a catalogued gene. OMIM is one of the databases housed in the US National Center for Biotechnology Information (NCBI) and is included in its search menus.Footnote 2 Another federally funded online database, Gene Test-Gene Clinics, provides an international directory of genetic testing laboratories and genetics clinics. We encourage readers to utilize these websites and our listed references to attain additional information if a monogenetic form of stroke is suspected.
In summary, this chapter has been designed as a concise initial reference for readers regarding important monogenetic stroke disorders. This chapter emphasizes established clinically relevant information, as well as introducing several concepts important for interpreting the continually evolving literature on stroke genetics. Lastly, we close with a brief summary of responsible genetic testing.
Definition of Terms
Several terms used throughout this chapter require definition:
Allele—Alternative forms of a gene or marker locus due to changes at the level of DNA.
Autosomal dominant—A disease inheritance pattern that requires only one mutated copy of the gene in a single autosomal chromosome (1–22). Only one copy is necessary for a person to be affected.
Autosomal recessive—A disease inheritance pattern that requires two mutated copy of the gene in a single autosomal chromosome (1–22). Two copies are necessary for a person to be affected.
Complex trait—A trait with a genetic component that is not strictly Mendelian (dominant, recessive, sex-linked). Complex traits may involve the interaction of two or more genes to produce a phenotype or may involve gene-environment interactions.
Genotype—The observed alleles at a genetic locus for an individual. For an autosomal locus, a genotype is composed of two alleles, one transmitted maternally and the other transmitted paternally.
Mendelian trait—A trait that is controlled by a single locus and shows a simple Mendelian inheritance pattern. Such disorders are inherited according to Mendel’s laws.
Phenotype—The observed manifestations of a genotype. The phenotype may be an observed trait, a particular type of clinical event, or may be expressed physiologically.
Polymorphism—Genetic loci at which there are two or more alleles that are each present at a frequency of at least 1% in the population.
X-linked dominant—A disease inheritance pattern that requires only one mutated copy of a gene on the X chromosome; only one copy is necessary for a person to be affected. Males and females are both affected in these disorders, with males typically being more severely affected than females. The sons of a man with an X-linked dominant disorder will all be unaffected (since they receive their father’s Y chromosome), and his daughters will all inherit the condition. A woman with an X-linked dominant disorder has a 50% chance of having an affected fetus with each pregnancy.
X-linked recessive—A disease inheritance pattern in which a mutation in a gene on the X chromosome causes the phenotype to be expressed (1) in males (who are necessarily hemizygous for the gene mutation because they have only one X chromosome) and (2) in females who are homozygous for the gene mutation (i.e., they have a copy of the gene mutation on each of their two X chromosomes). The chance of passing on the disorder differs between men and women; the sons of a man with an X-linked recessive disorder will not be affected, and his daughters will carry one copy of the mutated gene. A woman who is a carrier of an X-linked recessive disorder (XRXr) has a 50% chance of having sons who are affected and a 50% chance of having daughters who carry one copy of the mutated gene and are therefore carriers.
Monogenetic or Mendelian Disorders
Rare Mendelian disorders arising from single-gene defects have been described in which stroke is a prominent presenting feature. It should be emphasized that these are not “stroke genes” but rather mutations that may have stroke as an accompanying manifestation. There are several reasons to recognize monogenetic conditions associated with stroke. First, there may be specific treatments that can alter the course of the disease (e.g., transfusion therapy and sickle cell disease); such treatments are often more effective if the disease is identified early. Second, natural history or prognostic information may be available, including the possibility of anticipating problems in other organ systems (e.g., Fabry disease and renal failure). Finally, diagnosis and counseling may be of benefit to family members of the affected case, potentially leading to earlier diagnosis and amelioration of the disease.
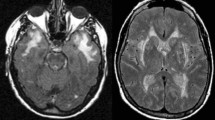
The search for monogenetic stroke etiologies begins with the history and physical examination. As mentioned, we have chosen to illustrate the established monogenetic disorders associated with stroke as categorized by the most common mechanism and etiological causes (i.e., large arterial diseases, small vessel diseases, hematological diseases, mitochondrial diseases, and connective tissue disorders). Table 10.1 [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114] highlights clues to these disorders from the history and examination. Table 10.2 [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114] describes other features of these disorders including associated laboratory findings, inheritance patterns, the resulting pathophysiologic defect, and the availability of diagnostic testing. We suggest that readers concerned for a monogenetically suspected case of stroke read through the tables to evaluate for similarities with their case. Utilizing the patient’s history and exam findings, note other organ system abnormalities such as the eyes (e.g., COL4A1, TREX, MELAS), the kidneys (e.g., Fabry disease), and the heart (e.g., familial hypercholesterolemia, connective tissue disorders). Further, the appearance of the stroke(s) on imaging can also be used to further isolate the diagnosis. For example, looking for patterns of strictly small infarcts with white matter changes involving the bilateral extreme capsules and anterior temporal poles might imply CADASIL. As another example, strokes that appear to fluctuate with time and/or do not conform to vascular territories might imply MELAS. Additionally, vessel imaging including magnetic resonance angiography (MRA) or computed tomography angiography (CTA) can also assist with diagnosis; for example, evidence of the pathognomonic “string of beads” sign in the internal carotid artery as seen with fibromuscular dysplasia and vertebrobasilar dolicoectasia as often seen in Marfan syndrome. Magnetic resonance venography (MRV) demonstrating cerebral venous thrombosis may imply a hypercoagulable state such as a factor V Leiden mutation. While we have attempted to make our tables as comprehensive as possible, we also suggest reviewing our references for each condition, and we recommend these other excellent review articles [115,116,117,118,119,120,121,122], as well as the OMIM reference for the specific disease.
Lastly, a genetic cause should be considered in any young stroke patient who lacks established vascular risk factors or whose initial workup is negative for an etiologic cause. Clinicians should always ask about a familial history of stroke (see Chap. 10). A family history of stroke, particularly at an early age, is probably the strongest indicator of a potential underlying genetic etiology. As such, to maximize the likelihood of detecting a familial condition, a structured approach to the family history is needed. This should include recording the family pedigree in detail, including, at a minimum, all first-degree relatives (i.e., parents, siblings, and children). The major medical conditions of all family members should be recorded as well as age at onset for relevant medical conditions and age at death. Depending on the context, this information from the pedigree should be included for second- and third-degree relatives. A pedigree diagram helps highlight patterns of transmission (e.g., an autosomal dominant pattern versus a maternal transmission pattern as seen in mitochondrial disorders).
Responsible Genetic Testing
Here, we address the questions of when genetic testing is indicated and what is the appropriate context for genetic testing. Genetic tests include analyses not only of DNA or RNA for the purpose of detecting a genetic condition but also analyses of proteins and certain metabolites for the same purpose. Unlike other types of laboratory tests, genetic tests provide information not only about the tested person but also about his or her relatives or descendants. The most appropriate criteria to be used to evaluate the risks and benefits of genetic tests and how these criteria should apply to different categories of genetic tests have been the subject of much societal scrutiny and, in the United States, the focus of several relatively recently instituted federal policies. It has been proposed that the decision to use a particular genetic test in a particular individual should include consideration of analytical validity, clinical validity, and clinical utility, including social consequences.
Analytical validity refers to whether the test is reliable and valid in measuring what it purports to measure. Clinical validity refers to the accuracy of the test in diagnosing or predicting risk of disease and is measured by sensitivity and specificity, which are test characteristics, and predictive value, which is also a function of the prevalence of the disease in the population. Clinical utility refers to outcomes associated with a positive or negative test result.
Here, we also emphasize that genetic testing may have unintended social consequences affecting both the patient and their family through what is termed as genetic discrimination. Genetic discrimination occurs when people are treated differently by their employer or insurance company because they have a gene mutation that causes or increases the risk of an inherited disorder. Several countries have laws that help protect people against genetic discrimination; however, genetic testing remains a fast-moving field, and these laws do not necessarily cover every situation. In the United States, it was widely recognized that there was a need for federal legislation to limit risks pertaining to discrimination in employment or health insurance on the basis of genetic information. As such, in 2008, the Genetic Information Nondiscrimination Act (GINA) was signed into law [123, 124]. GINA protects individuals from the misuse of genetic information in health insurance and employment and was created to remove barriers to the appropriate use of genetic services by the public.
Under GINA, group and individual health insurers cannot:
Use a person’s genetic information to set eligibility requirements or establish premium or contribution amounts
Request or require that a person undergo a genetic test
Under GINA, employers cannot:
Use a person’s genetic information in decisions about hiring, firing, job assignments, or promotions
Request, require, or purchase genetic information about an employee or family member
Types of Genetic Information Protected by GINA:
Family medical history
Carrier testing; i.e., sickle cell anemia and other conditions
Prenatal genetic testing; i.e., amniocentesis, chorionic villus sampling, and other techniques
Susceptibility and predictive testing; e.g., BRCA testing for risk of breast or ovarian cancer, testing for Huntington disease, or hereditary nonpolyposis colorectal cancer (HNPCC) testing for risk of colon cancer
Analysis of tumors or other assessments of genes, mutations, or chromosomal changes
It is important to note that GINA regulates health insurers and employers, not health-care professionals. The law does not require that health-care professionals counsel patients about GINA. Doing so, however, might help your patients feel more comfortable about providing family history information, taking a genetic test, or participating in genetic research. The law should not keep practitioners from taking a comprehensive family history; rather it protects patients from having that information misused. More recently the Equal Employment Opportunity Commission (EEOC) amended various GINA regulations providing further clarification on acceptable workplace wellness programs with these new guidelines going into effect in July 2016. The new amendments require that (1) employee wellness programs are voluntary; (2) employers cannot deny health care coverage for non-participation, or (3) take adverse employment actions against or coerce employees who do not participate in wellness programs. Additionally, the new GINA regulations cover spousal participation in wellness programs and employers may not ask employees or covered dependents to agree to permit the sale of their genetic information in exchange for participation in wellness plans. [125]
Consideration of the aforementioned factors implies the need to individualize the decision for genetic testing. It should be apparent that the clinical validity, clinical utility, and social consequences of a test could vary greatly depending on whether it is performed for diagnostic or prognostic purposes, individual testing, or population screening; whether a treatment is available for the condition; and whether the genotype has a high or low probability of being associated with the disease phenotype. While there is currently no formal mandate, there is a consensus [126] that genetic education and counseling, as well as written informed consent, should accompany certain types of “high-scrutiny” genetic testing. “High-scrutiny” tests include those that have a relatively low clinical validity and utility but pose a high risk of adverse social consequence. For example, a test whose purpose is predictive, which detects a variant with a low probability of being associated with disease, and for which there is no proven intervention, would fall into this category. It follows from this line of reasoning that the obligation to ensure that the patient is well informed and participates in the decision to proceed with genetic testing depends on where the test falls on the spectrum from low to high scrutiny. An online and freely available e-learning course by the Centers for Disease Control and Prevention reviews the application of the Clinical Laboratory Improvement Amendments (CLIA) requirements to molecular genetic testing and quality assurance measures for molecular genetic testing as consistent with good laboratory practices [127].
Several examples are now mentioned illustrating these considerations with respect to genetic screening for stroke prevention. One obvious example is the value of screening young African-American stroke patients for sickle cell disease, this is widely accepted because this information directly influences treatment of the initial stroke and strategies for preventing recurrent stroke [53,54,55,56,57,58,59,60]. In contrast, the issues relating to factor V Leiden mutation testing are more complex. A consensus statement by the American College of Medical Genetics recommends that factor V Leiden mutation testing be performed in any person with venous thrombosis in an unusual site, including cerebral vein thrombosis [75]. Although the finding of heterozygosity for this mutation (lifetime risk of venous thrombosis is approximately 10%) does not currently change management or prophylaxis for most patients, the finding of homozygosity (lifetime risk of venous thrombosis >80%) would dictate consideration of lifelong antithrombotic prophylaxis. While more controversial [75], another benefit of testing for factor V Leiden mutation in cerebral venous thrombosis is that relatives of those possessing one or more of the mutant alleles could choose to be screened. Knowledge of factor V Leiden status in asymptomatic relatives could influence a woman’s decision to use oral contraceptive or could lead to antithrombotic prophylaxis during periods of increased risk, such as the postpartum period. Routine testing is not currently recommended for young patients with arterial stroke, even those with a family history [75], although testing could play a role in the evaluation of persons with suspected paradoxical embolism. In contrast to stroke attributable to a Mendelian trait, most candidate genes for stroke have a low probability of being associated with disease and do not have proven interventions. For these reasons, testing for such candidate stroke genes would fall into the category of high-scrutiny genetic tests at this time.
One final consideration that warrants emphasis is that the costs of genetic testing are not always covered by insurance, and that these costs are often quite high. As such, we suggest practitioners discuss this issue with the patient and their family ‘pre-test’, such that there is time to attain insurance authorization for the test. Most insurance companies have prespecified testing policies that typically emphasize that genetic testing be medically necessary to establish a molecular diagnosis of an inheritable disease, emphasizing that the patient is:
Displaying clinical features, or is at direct risk of inheriting the mutation in question (presymptomatic).
That the result of the test will directly impact the treatment being delivered.
After history, physical examination, pedigree analysis, genetic counseling, and completion of conventional diagnostic studies, a definitive diagnosis remains uncertain, and a specific diagnosis is suspected.
Conclusion
While technological and research advances are accelerating our ability to understand the interplay between genetics and the environment in the pathogenesis of stroke, there are several established monogenetic disorders that cause stroke. Such disorders should be considered in any young patient whose initial workup for stroke is negative. Monogenetic disorders should also be considered in situations in which multiple family members are affected, notably this can be across several disparate organ systems. Through the use of a detailed medical and family history and physical exam, practitioners can determine if an established monogenetic disease seems likely and then weigh the options regarding genetic testing. If a monogenetic form of stroke is suspected, referring a patient for genetic counseling should be considered. As with any stroke, the ultimate goals of these efforts are disease prevention and treatment optimization.
Acknowledgement and Disclaimer
Dr. Cole’s effort on this project was supported by the American Heart Association CVGPS Pathway Grant (Award #: 15GPSPG23770000, the Department of Veterans Administration (VA), Department of Neurology and Medical Research Service, and the National Institutes of Health/National Institute of Neurological Disorders and Stroke (Grant U01-NS069208–01); its contents are the responsibility of the authors and do not necessarily reflect the official views of the AHA, the VA or the NIH.
References
Homocystinuria (OMIM: 236200). http://www.omim.org/. Accessed 1 June 2016.
U.S. National Center for Biotechnology Information (NCBI). http://www.ncbi.nlm.nih.gov/omim. Accessed 1 June 2016.
Gene test—gene clinics. https://www.genetests.org/disorders/. Accessed 1 June 2016.
Lentz SR. Mechanisms of homocysteine-induced atherothrombosis. J Thromb Haemost. 2005;3:1646–54.
Abahji TN, Nill L, Ide N, et al. Acute hyperhomocysteinemia induces microvascular and macrovascular endothelial dysfunction. Arch Med Res. 2007;38:411–6.
Upchurch Jr GR, Welch GN, Fabian AJ, et al. Homocyst(e)ine decreases bioavailable nitric oxide by a mechanism involving glutathione peroxidase. J Biol Chem. 1997;272:17012–7.
Dayal S, Wilson KM, Leo L, et al. Enhanced susceptibility to arterial thrombosis in a murine model of hyperhomocysteinemia. Blood. 2006;108:2237–43.
Kelly PJ, Furie KL, Kistler JP, et al. Stroke in young patients with hyperhomocysteinemia due to cystathionine β-synthase deficiency. Neurology. 2003;60:275–9.
Chauveheid MP, Lidove O, Papo T, Laissy JP. Adult-onset homocystinuria arteriopathy mimics fibromuscular dysplasia. Am J Med. 2008;121:e5–6. Accessed 1 June 2016
Familial hyper-cholesterolemia—type II-a (OMIM: 143890). http://www.omim.org/. Accessed 1 June 2016.
Familial HDL deficiency—type I (OMIM: 205400). http://www.omim.org/. Accessed 1 June 2016.
Goldstein JL, Brown MS. The LDL receptor locus and the genetics of familial hypercholesterolemia. Annu Rev Genet. 1979;13:259–89.
Hobbs HH, Brown MS, Goldstein JL. Molecular genetics of the LDL receptor gene in familial hypercholesterolemia. Hum Mutat. 1992;1:445–66.
Garg A, Simha V. Update on dyslipidemia. J Clin Endocrinol Metab. 2007;92:1581–9.
Yamauchi T, Tada M, Houkin K, Tanaka T, Nakamura Y, Kuroda S, Abe H, Inoue T, Ikezaki K, Matsushima T, Fukui M. Linkage of familial moyamoya disease (spontaneous occlusion of the circle of Willis) to chromosome 17q25. Stroke. 2000;31:930–5.
Kamada F, Aoki Y, Narisawa A, Abe Y, Komatsuzaki S, Kikuchi A, Kanno J, Niihori T, Ono M, Ishii N, Owada Y, Fujimura M, Mashimo Y, Suzuki Y, Hata A, Tsuchiya S, Tominaga T, Matsubara Y, Kure S. A genome-wide association study identifies RNF213 as the first Moyamoya disease gene. J Hum Genet. 2011;56:34–40.
Mineharu Y, Liu W, Inoue K, Matsuura N, Inoue S, Takenaka K, Ikeda H, Houkin K, Takagi Y, Kikuta K, Nozaki K, Hashimoto N, Koizumi A. Autosomal dominant moyamoya disease maps to chromosome 17q25.3. Neurology. 2008;70:2357–63.
Sakurai K, Horiuchi Y, Ikeda H, Ikezaki K, Yoshimoto T, Fukui M, Arinami T. A novel susceptibility locus for moyamoya disease on chromosome 8q23. J Hum Genet. 2004;49:278–81.
Herve D, Touraine P, Verloes A, Miskinyte S, Krivosic V, Logeart D, Alili N, Laredo JD, Gaudric A, Houdart E, Metzger JP, Tournier-Lasserve E, Woimant F. A hereditary moyamoya syndrome with multisystemic manifestations. Neurology. 2010;75:259–64.
Roder C, Peters V, Kasuya H, Nishizawa T, Wakita S, Berg D, Schulte C, Khan N, Tatagiba M, Krischek B. Analysis of ACTA2 in European moyamoya disease patients. Eur J Paediatr Neurol. 2011;15:117–22.
Herve D, Philippi A, Belbouab R, Zerah M, Chabrier S, Collardeau-Frachon S, Bergametti F, Essongue A, Berrou E, Krivosic V, Sainte-Rose C, Houdart E, et al. Loss of alpha-1-beta-1 soluble guanylate cyclase, the major nitric oxide receptor, leads to moyamoya and achalasia. Am J Hum Genet. 2014;94:385–94. Note: Erratum—Am J Hum Genet 2014;94: 642
CADASIL—cerebral autosomol dominant subcortical infarcts and leukoencephaly (OMIM: 125310). http://www.omim.org/. Accessed 1 June 2016.
Reyes S, Viswanathan A, Godin O, Dufouil C, Benisty S, Hernandez K, et al. Apathy: a major symptom in CADASIL. Neurology. 2009;72:905–10.
Monet-Leprêtre M, Bardot B, Lemaire B, Domenga V, Godin O, Dichgans M, et al. Distinct phenotypic and functional features of CADASIL mutations in the Notch3 ligand binding domain. Brain. 2009;132:1601–12.
Tikka S, Mykkänen K, Ruchoux MM, Bergholm R, Junna M, Pöyhönen M, et al. Congruence between NOTCH3 mutations and GOM in 131 CADASIL patients. Brain. 2009;132:933–9.
Joutel A, Favrole P, Labauge P, Chabriat H, Lescoat C, Andreux F, et al. Skin biopsy immunostaining with a Notch3 monoclonal antibody for CADASIL diagnosis. Lancet. 2001;358:2049–51.
Singhal S, Rich P, Markus HS. The spatial distribution of MR imaging abnormalities in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy and their relationship to age and clinical features. AJNR Am J Neuroradiol. 2005;26:2481–7.
Liem MK, Lesnik Oberstein SA, Haan J, van der Neut IL, Ferrari MD, van Buchem MA, et al. MRI correlates of cognitive decline in CADASIL: a 7-year follow-up study. Neurology. 2009;72:143–8.
CARASIL (OMIM: 600142). http://www.omim.org/. Accessed 1 June 2016.
Arima K, Yanagawa S, Ito N, Ikesa S. Cerebral arterial pathology of CADASIL and CARASIL (Maeda syndrome). Neuropathology. 2003;23:327–34.
Yanagawa S, Ito N, Aruna K, Ikeda S. Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy. Neurology. 2002;58:817–20.
Razvi SSM, Bone I. Single gene disorders causing ischaemic stroke. J Neurol. 2006;253:685–700.
Lanfranconi S, Markus H. COL4A1 mutations as a monogenetic cause of cerebral small vessel disease: a systematic review. Stroke. 2010;41:e513–8.
Alamowitch S, Plaisier E, Favrole P, Prost C, Chen Z, Van Agtmael T, Marro B, Ronco P. Cerebrovascular disease related to COL4A1 mutations in HANAC syndrome. Neurology. 2009;73:1873–82.
Plaisier E, Alamowitch S, Gribouval O, Mougenot B, Gaudric A, Antignac C, Roullet E, Ronco P. Autosomal-dominant familial hematuria with retinal arteriolar tortuosity and contractures: a novel syndrome. Kidney Int. 2005;67:2354–60.
Plaisier E, Gribouval O, Alamowitch S, Mougenot B, Prost C, Verpont MC, Marro B, Desmettre T, Cohen SY, Roullet E, Dracon M, Fardeau M, Van Agtmael T, Kerjaschki D, Antignac C, Ronco P. COL4A1 mutations and hereditary angiopathy, nephropathy, aneurysms, and muscle cramps. N Engl J Med. 2007;357:2687–95.
Hara K, Shiga A, Fukutake T, Nozaki H, Miyashita A, Yokoseki A, et al. Association of HTRA1 mutations and familial ischemic cerebral small-vessel disease. N Engl J Med. 2009;360:1729–39.
Mendioroz M, Fernández-Cadenas I, Del Río-Espinola A, Rovira A, Solé E, Fernández-Figueras MT, et al. A missense HTRA1 mutation expands CARASIL syndrome to the Caucasian population. Neurology. 2010;75:2033–5.
Fabry disease (OMIM 301500). http://www.omim.org/. Accessed 1 June 2016.
Fellgiebel A, Müller MJ, Ginsberg L. CNS manifestations of Fabry’s disease. Lancet Neurol. 2006;5:791–5.
Sims K, Politei J, Banikazemi M, Lee P. Stroke in Fabry disease frequently occurs before diagnosis and in the absence of other clinical events: natural history data from the Fabry Registry. Stroke. 2009;40:788–94.
Mehta A, Beck M, Elliott P, Giugliani R, Linhart A, Sunder-Plassmann G, et al. Enzyme replacement therapy with agalsidase alfa in patients with Fabry’s disease: an analysis of registry data. Lancet. 2009;374:1986–96.
Rolfs A, Böttcher T, Zschiesche M, Morris P, Winchester B, Bauer P, et al. Prevalence of Fabry disease in patients with cryptogenic stroke: a prospective study. Lancet. 2005;366:1794–6.
Wozniak MA, Kittner SJ, Tuhrim S, Cole JW, Stern B, Dobbins M, et al. Frequency of unrecognized Fabry disease among young European-American and African-American men with first ischemic stroke. Stroke. 2010;41:78–81.
Baptista MV, Ferreira S, Pinho-E-Melo T, Carvalho M, Cruz VT, Carmona C, et al. Mutations of the GLA gene in young patients with stroke: the PORTYSTROKE study—screening genetic conditions in Portuguese young stroke patients. Stroke. 2010;41:431–6.
Brouns R, Thijs V, Eyskens F, Van den Broeck M, Belachew S, Van Broeckhoven C, et al. Belgian Fabry study: prevalence of Fabry disease in a cohort of 1,000 young patients with cerebrovascular disease. Stroke. 2010;41:863–8.
Brain small vessel disease with hemorrhage—COL4A1 (OMIM 607595). http://www.omim.org/. Accessed 1 June 2016.
Yamamoto Y, Craggs L, Baumann M, Kalimo H, Kalaria RN. Review: molecular genetics and pathology of hereditary small vessel diseases of the brain. Neuropathol Appl Neurobiol. 2001;37:94–113.
TREX spectrum disorders (OMIM: 192315). http://www.omim.org/. Accessed 1 June 2016.
Kavanaugh D, Spitzer D, Kothari P, et al. New roles for the major human 3′–5′ exonuclease TREX1 in human disease. Cell Cycle. 2008;7:1718–25.
Jen J, Cohen AH, Yue Q, et al. Hereditary endotheliopathy with retinopathy, nephropathy, and stroke (HERNS). Neurology. 1997;49:1322–30.
Richards A, van den Maagdenberg AM, Jen JC, et al. C-terminal truncations in human 3′–5′ DNA exonuclease TREX1 cause autosomal dominant retinal vasculopathy with cerebral leukodystrophy. Nat Genet. 2007;39:1068–70.
Sickle cell disease (OMIM: 603903). http://www.omim.org/. Accessed 1 June 2016.
Adams RJ, McKie VC, Hsu L, et al. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. N Engl J Med. 1998;339:5–11.
Ohene-Frempong K, Weiner SJ, Sleeper LA, et al. Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood. 1998;91:288–94.
Nichols FT, Jones AM, Adams RJ. Stroke prevention in sickle cell disease (STOP) study guidelines for transcranial Doppler testing. J Neuroimaging. 2001;11:354–62.
Adams RJ. Lessons from the stroke prevention trial in sickle cell anemia (STOP) study. J Child Neurol. 2000;15:344–9.
Pegelow CH, Wang W, Granger S, et al. Silent infarcts in children with sickle cell anemia and abnormal cerebral artery velocity. Arch Neurol. 2001;58:2017–21.
Prengler M, Pavlakis SG, Prohovnik I, Adams RJ. Sickle cell disease: the neurological complications. Ann Neurol. 2002;51:543–52.
Steinberg MH, Barton F, Castro O, et al. Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: risks and benefits up to 9 years of treatment. JAMA. 2003;289:1645–51.
Protein C deficiency (OMIM: 176860). http://www.omim.org/. Accessed 1 June 2016.
Griffin JH, Evatt B, Zimmerman TS, et al. Deficiency of protein C in congenital thrombotic disease. J Clin Invest. 1981;68:1370–3.
Bertina RM, Broekmans AW, Krommenhoek-van Es C, van Wijngaarden A. The use of a functional and immunologic assay for plasma protein C in the study of the heterogeneity of congenital protein C deficiency. Thromb Haemost. 1984;51:1–5.
Bertina RM, Broekmans AW, van der Linden IK, Mertens K. Protein C deficiency in a Dutch family with thrombotic disease. Thromb Haemost. 1982;48:1–5.
Berdeaux DH, Abshire TC, Marlar RA. Dysfunctional protein C deficiency (type II): a report of 11 cases in 3 American families and review of the literature. Am J Clin Pathol. 1993;99:677–86.
Protein S deficiency (OMIM: 176880, 612336). http://www.omim.org/. Accessed 1 June 2016.
Comp PC, Nixon RR, Cooper MR, Esmon CT. Familial protein S deficiency is associated with recurrent thrombosis. J Clin Invest. 1984;74:2082–8.
Engesser L, Broekmans AW, Briet E, et al. Hereditary protein S deficiency: clinical manifestations. Ann Intern Med. 1987;106:677–82.
Factor V Leiden mutation (OMIM: 227400). http://www.omim.org/. Accessed 1 June 2016.
de Paula SA, Ribeiro DD, Carvalho MG, et al. Factor V Leiden and increased risk for arterial thrombotic disease in young Brazilian patients. Blood Coagul Fibrinolysis. 2006;17:271–5.
Margaglione M, D’Andrea G, Giuliani N, et al. Inherited prothrombotic conditions and premature ischemic stroke: sex difference in the association with factor V Leiden. Arterioscler Thromb Vasc Biol. 1999;19:1751–6.
Hamedani AG, Cole JW, Mitchell BD, Kittner SJ. Meta-analysis of factor V Leiden and ischemic stroke in young adults: the importance of case ascertainment. Stroke. 2010;41:1599–603.
Longstreth Jr WT, Rosendaal FR, Siscovick DS, et al. Risk of stroke in young women and two prothrombotic mutations: factor V Leiden and prothrombin gene variant (G20210A). Stroke. 1998;29:577–80.
Nabavi DG, Junker R, Wolff E, et al. Prevalence of factor V Leiden mutation in young adults with cerebral ischaemia: a case-control study on 225 patients. J Neurol. 1998;245:653–8.
Grody WW, Griffin JH, Taylor AK, et al. American College of Medical Genetics consensus statement on factor V Leiden mutation testing. Genet Med. 2001;3:139–48.
MELAS—Mitochondrial encephalopathy lactic acidosis and stroke (OMIM:540000). http://www.omim.org/. Accessed 1 June 2016.
Pavlakis SG, Phillips PC, DiMauro S, De Vivo DC, Rowland LP. Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes: a distinctive clinical syndrome. Ann Neurol. 1984;16:481–8.
Hirano M, Pavlakis SG. Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS): current concepts. J Child Neurol. 1994;9:4–13.
Ko CH, Lam CW, Tse PW, Kong CK, Chan AK, Wong LJ. De novo mutation in the mitochondrial tRNALeu(UUR) gene (A3243G) with rapid segregation resulting in MELAS in the offspring. J Paediatr Child Health. 2001;37:87–90.
Pang CY, Huang CC, Yen MY, et al. Molecular epidemiologic study of mitochondrial DNA mutations in patients with mitochondrial diseases in Taiwan. J Formos Med Assoc. 1999;98:326–34.
Nishino I, Komatsu M, Kodama S, Horai S, Nonaka I, Goto Y. The 3260 mutation in mitochondrial DNA can cause mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS). Muscle Nerve. 1996;19:1603–4.
Sato W, Hayasaka K, Shoji Y, et al. A mitochondrial tRNA(Leu)(UUR) mutation at 3,256 associated with mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes (MELAS). Biochem Mol Biol Int. 1994;33:1055–61.
Peterson PL. The treatment of mitochondrial myopathies and encephalomyopathies. Biochim Biophys Acta. 1995;1271:275–80.
Lam CW, Lau CH, Williams JC, Chan YW, Wong LJ. Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS) triggered by valproate therapy. Eur J Pediatr. 1997;156:562–4.
DiMauro S, Schon EA. Mitochondrial respiratory-chain diseases. N Engl J Med. 2003;348:2656–68.
Ehlers-Danlos syndrome—type IV (OMIM: 130050). http://www.omim.org/. Accessed 1 June 2016.
Superti-Furga A, Gugler E, Gitzelmann R, Steinmann B. Ehlers-Danlos syndrome type IV: a multi-exon deletion in one of the two COL3A1 alleles affecting structure, stability, and processing of type III procollagen. J Biol Chem. 1988;263:6226–32.
Germain DP, Herrera-Guzman Y. Vascular Ehlers-Danlos syndrome. Ann Genet. 2004;47:1–9.
Marfan syndrome (OMIM: 154700). http://www.omim.org/. Accessed 1 June 2016.
Sponseller PD, Hobbs W, Riley LH, Pyeritz RE. The thoracolumbar spine in Marfan syndrome. J Bone Joint Surg Am. 1995;77:867–76.
Chan YC, Ting CW, Ho P, Poon JT, Cheung GC, Cheng SW. Ten-year epidemiological review of in-hospital patients with Marfan syndrome. Ann Vasc Surg. 2008;22:608–12.
Ballabio E, Bersano A, Bresolin N, Candelise L. Monogenic vessel diseases related to ischemic stroke: a clinical approach. J Cereb Blood Flow Metab. 2007;27:1649–62.
Pyeritz RE. The Marfan syndrome. Annu Rev Med. 2000;51:481–510.
Schievink WI, Michels VV, Piepgras DG. Neurovascular manifestations of heritable connective tissue disorders. Stroke. 1994;25:889–903.
Wityk R, Zanferrari C, Oppenheimer S. Neurovascular complications of Marfan syndrome: a retrospective, hospital-based study. Stroke. 2002;33:680–4.
Silverman IE, Berman DM, Dike GL, et al. Vertebrobasilar dolichoectasia associated with Marfan syndrome. J Stroke Cerebrovasc Dis. 2000;9:196–8.
Fibromuscular dysplasia (OMIM: 135580). http://www.omim.org/. Accessed 1 June 2016.
Mettinger KL, Ericson K. Fibromuscular dysplasia and the brain. I. Observations on angiographic, clinical and genetic characteristics. Stroke. 1982;13:46–52.
Plouin PF, Perdu J, LaBatide-Alanore A, et al. Fibromuscular dysplasia. Orphanet J Rare Dis. 2007;2:28.
Meyers DS, Grim CE, Keitzer WF. Fibromuscular dysplasia of the renal artery with medial dissection. A case simulating polyarteritis nodosa. Am J Med. 1974;56:412–6.
Janzen J, Vuong PN, Rothenberger-Janzen K. Takayasu’s arteritis and fibromuscular dysplasia as causes of acquired atypical coarctation of the aorta: retrospective analysis of seven cases. Heart Vessels. 1999;14:277–82.
Siegert CE, Macfarlane JD, Hollander AM, van Kemenade F. Systemic fibromuscular dysplasia masquerading as polyarteritis nodosa. Nephrol Dial Transplant. 1996;11:1356–8.
Sperati CJ, Aggarwal N, Arepally A, Atta MG. Fibromuscular dysplasia. Kidney Int. 2009;75:333–6.
Niizuma S, Nakahama H, Inenaga T, et al. Asymptomatic renal infarction, due to fibromuscular dysplasia in a young woman with 11 years of follow-up. Clin Exp Nephrol. 2005;9:170–3.
Connor A, Mathieson P. A string of beads. Am J Med. 2008;121:580–2.
Olin JW. Recognizing and managing fibromuscular dysplasia. Cleve Clin J Med. 2007;74:273–82.
Begelman SM, Olin JW. Fibromuscular dysplasia. Curr Opin Rheumatol. 2000;12:41–7.
Pseudoxanthoma elasticum—AD form (OMIM: 177850), AR form (OMIM: 264800). http://www.omim.org/. Accessed 1 June 2016.
Struk B, Neldner KH, Rao VS, St Jean P, Lindpaintner K. Mapping of both autosomal recessive and dominant variants of pseudoxanthoma elasticum to chromosome 16p13.1. Hum Mol Genet. 1997;6:1823–8.
Gheduzzi D, Guidetti R, Anzivino C, et al. ABCC6 mutations in Italian families affected by pseudoxanthoma elasticum (PXE). Hum Mutat. 2004;24:438–9.
Sherer DW, Bercovitch L, Lebwohl M. Pseudoxanthoma elasticum: significance of limited phenotypic expression in parents of affected offspring. J Am Acad Dermatol. 2001;44:534–7.
Chassaing N, Martin L, Calvas P, et al. Pseudoxanthoma elasticum: a clinical, pathophysiological and genetic update including 11 novel ABCC6 mutations. J Med Genet. 2005;42:881–92.
Hu X, Plomp AS, van Soest S, et al. Pseudoxanthoma elasticum: a clinical, histopathological, and molecular update. Surv Ophthalmol. 2003;48:424–38.
Laube S, Moss C. Pseudoxanthoma elasticum. Arch Dis Child. 2005;90:754–6.
Recommended Review Articles
Ballabio E, Bersano A, Bresolin N, Candelise L. Monogenic vessel diseases related to ischemic stroke: a clinical approach. J Cereb Blood Flow Metab. 2007;27:1649–62.
Yananoto Y, Craggs L, Baumann M, Kalimo H, Kalaria R. Review: molecular genetics and pathology of hereditary small vessel diseases of the brain. Neuropathol Appl Neurobiol. 2011;37:94–113.
Razvi SS, Bone I. Single gene disorders causing ischaemic stroke. J Neurol. 2006;253:685–700.
Meschia J, Worrall B, Rich S. Genetic susceptibility to ischemic stroke. Nat Rev Neurol. 2011;317:369–78.
Testai FD, Gorelick PB. Inherited metabolic disorders and stroke part 1: Fabry disease and mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes. Arch Neurol. 2010;67:19–24.
Testai FD, Gorelick PB. Inherited metabolic disorders and stroke part 2: homocystinuria, organic acidurias, and urea cycle disorders. Arch Neurol. 2010;67:148–53.
Tan RY, Markus HS. Monogenic causes of stroke: now and the future. J Neurol. 2015;262(12):2601–16.
Bersano A, Markus HS, Quaglini S, Arbustini E, Lanfranconi S, et al. Clinical pregenetic screening for stroke monogenic diseases: results from Lombardia GENS Registry. Stroke. 2016. pii: STROKEAHA.115.012281. [Epub ahead of print]
The genetic information nondiscrimination act (GINA). http://www.nchpeg.org/index.php?option=com_content&view=article&id=97&Itemid=120. Accessed 1 June 2016
Genetic information nondiscrimination Act of 2008. http://ginahelp.org/. Accessed 1 June 2016.
Pak Y. Gregerson JP. EEOC issues new guidance on employee wellness programs. The National Law Review (2016). ISSN 2161-3362. http://www.natlawreview.com/article/eeoc-issues-new-guidance-employee-wellness-programs. Accessed 1 June 2016.
Chen B, Gagnon M, Shahangian S, et al. Good laboratory practices for molecular genetic testing for heritable diseases and conditions. CDC MMWR. 2009;58:1–29. http://www.cdc.gov/mmwr/pdf/rr/rr5806.pdf/. Accessed 1 June 2016
Good laboratory practices for molecular genetics testing. http://www.cdc.gov/labtraining/cdc-lab-training-courses/good_lab_practices_molecular_genetics_testing.html Accessed 1 June 2016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Cole, J.W., Stack, C.A. (2017). Other Monogenetic Stroke Disorders. In: Sharma, P., Meschia, J. (eds) Stroke Genetics. Springer, Cham. https://doi.org/10.1007/978-3-319-56210-0_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-56210-0_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56208-7
Online ISBN: 978-3-319-56210-0
eBook Packages: MedicineMedicine (R0)