Abstract
Most restorative dental materials are inert and biocompatible and are used in the restoration and reconstruction of teeth. Among them, glass-ceramics (GCs) are of great importance because they are easy to process and have outstanding esthetics, translucency, low thermal conductivity, high strength, chemical durability, biocompatibility, wear resistance, and hardness similar to that of natural teeth. However, research and development are still underway to further improve their mechanical properties and esthetics to enable them to compete with their current contenders (e.g., zirconia and hybrids) for posterior restorations. Throughout this chapter, we summarize the processing, properties, and applications of restorative dental glass-ceramics. Current commercial dental glass-ceramics are explained, and also selected papers that address promising types of dental glass-ceramics are reviewed. Finally, we include trends on relevant open issues and research possibilities.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
The dental materials market is composed of several segments, including implants, cores, restorative materials, impression materials, dental cements, and bonding agents [1]. Most restorative dental materials are inert and biocompatible and are used in the restoration and reconstruction of teeth [1]. Among these materials, restorative dental glass-ceramics are of great importance because they are easy to process via advanced technology like CAD/CAM and have outstanding esthetics, translucency, low thermal conductivity, high strength, chemical durability, biocompatibility, wear resistance, and hardness similar to that of natural teeth [2–14].
Glass-ceramics were discovered by D. R. Stookey at Corning Glass Works, USA, in 1953. They are polycrystalline materials produced by controlled heat treatment of certain glasses that contain one or more crystal phases embedded in a residual glass matrix [14]. The distinct chemical/physical properties of these phases and glass matrix have led to various unusual combinations of properties and applications in the domestic, space, defense, health, electronics, architecture, chemical, energy, and waste management fields . For instance, restorative dental glass-ceramics can mimic the tooth properties and are used as inlays, onlays, full crowns, partial crowns, bridges, and veneers [14]. Figure 9.1 shows a selection of these applications.
Examples of restorative dental glass-ceramics: (a) three-unit bridge, (b) crown, (c) onlay, (d) veneer [14]
The basic stages of the synthesis of glass-ceramics, which involve melting, forming, and controlled heat treatment, are explained in many textbooks and review papers [11–14]. These stages for a controlled double-stage heat treatment are illustrated schematically in Fig. 9.2.
In general, dental technicians prepare dental glass-ceramics using the following four popular methods [13, 14]: lost-wax casting, heat-pressing, CAD/CAM (computer-aided design and computer-aided manufacturing), and pressureless sintering.
In lost-wax casting , a model of the restoration which is prepared by a dentist is shaped on the cast using a particular type of wax. The model is invested in special refractory materials. During firing stage, wax burnout takes place at 900 °C, and the ceramic mold is partially sintered. The material for fabrication of a glass-ceramic is supplied as a glassy ingot, which is located in a furnace specially designed for casting. The glass ingot becomes liquid during heating, and following a short time hold at 1300–1500 °C, the melt is forced into a mold by centrifugal force. The glass casting is retrieved, excess glass is polished off, and after the final controlled heat treatment and coloring processes, the glass-ceramic restoration is ready for clinical use [13, 14]. In the heat-pressing method, the dental technician uses as-prepared glass-ceramic ingot to produce the final restoration. First, a mold is produced via the previously described lost-wax procedure. The mold and glass-ceramic ingot are placed in a furnace specially designed for this processing method. Once the glass-ceramic ingot has become a very viscous liquid of approximately 1011 Pa.s, it is forced by an Al2O3 plunger (via application of a relatively low force of 200–300 N) into the hollow portion of the mold at approximately 1000–1200 °C. After the cylinder has adequately cooled, the investment material is removed from the glass-ceramic restoration by blasting it with silica sand, aluminum oxide, glass beads, or silicon carbide grit [13, 14]. In the third method, machinable restorative glass-ceramics are fabricated using a CAD/CAM system. Typically, CAD/CAM dental restorations are machined from solid blocks of partially crystallized glass-ceramics (containing a machinable crystal phase) that are subjected to further heat treatment to fully develop the glass-ceramic and achieve adequate properties and color that closely match the basic shade of the restored tooth [13, 14]. In the fourth method, known as pressureless sintering, a thin layer of glass-ceramic is veneered over restorative materials such as zirconia, metals, or glass-ceramics. Veneering is performed to adjust the final shade of the restoration. In general, a slurry containing glass-ceramic fine powders plus coloring agents is brushed over the surface. The artifact is held in a furnace at an appropriate temperature for the required time to sinter and crystallize the glass-ceramic and fuse it to the restoration [13, 14].
Glass-ceramics always contain a residual glassy phase and one or more embedded crystal phases. The crystal content varies between 0.5% and 99.5% but most frequently lies between 30% and 70%, and the remaining content is the residual glass phase. The types of crystals, crystal volume fraction, distribution in the matrix, and physicochemical properties of both the crystals and the residual glass control the properties of glass-ceramics (including dental GCs), such as translucency, strength, fracture toughness, machinability, and chemical durability [13, 14]. These properties should meet the minimum requirements of the ISO 6872 standards [15]. Therefore, a dental glass-ceramic must have notably good chemical, mechanical, and optical properties comparable to those of natural teeth [15]. For example, the chemical durability must be higher than that of natural teeth. The mechanical properties of dental glass-ceramics such as fracture strength (σ), fracture toughness (KIC), and wear resistance are highly important for avoiding material damage and breakage. In terms of optical properties , these materials must exhibit translucency, color, opalescence, and fluorescence similar to those of natural teeth [15].
An analysis of glass-ceramic research and commercialization suggests that glass-ceramics for biomedical applications are of great importance [3]. For example, our comprehensive review on the history and trends of commercial bioactive and inert glass-ceramics revealed that persistent competition exists among dozens of companies and academia to develop new bioactive dental glass-ceramics (BDGCs) or restorative dental glass-ceramics (RDGCs) [13]. Therefore, throughout this chapter, we summarize the properties and applications of commercial restorative dental glass-ceramic in Sect. 2. Recent researches and survival rates of commercial dental glass-ceramics are also reviewed. In this context, in Sect. 3, we report on selected valuable papers that have addressed promising types of dental glass-ceramics. Finally, we include future trends, open issues, and guidance from a materials engineering perspective in Sect. 4.
9.2 Commercial Dental Glass-Ceramics
Various types of restorative dental glass-ceramics have already reached the market. These materials and their typical characteristics are listed in Table 9.1. Additionally, the main mechanical properties, commercial names, and recommended applications for these materials are summarized in Table 9.2. More details on these products have been reported in our recent review paper [13] and Höland and Beall’s book [14].
Hereafter, we review current status and recent developments regarding to the commercial restorative dental glass-ceramics (Tables 9.1 and 9.2).
9.2.1 Mica-Based Glass-Ceramics
Mica-based glass-ceramics such as Dicor® are old materials which are still used by dentists and technicians who know and trust them. However, a high risk of fracture is observed, and a relatively low mechanical strength and difficult processing conditions are the main drawbacks of mica-based glass-ceramics, which restrict their application and popularity [13, 14]. Therefore, numerous attempts in the 1990s and early 2000s were made to overcome the weakness of this material. Prof. Denry’s group at Ohio State University pioneered modifications of the composition of Dicor® and improved its properties. The Denry group replaced potassium with lithium and developed tainiolite, a lithium-containing tetrasilicic fluormica (KLiMg2Si4O10F2) with improved thermal and mechanical properties [16]. By changing the glass composition, a new glass-ceramic was developed based on the crystallization of mica (KNaMg2Si4O10F2) and K-fluorrichterite (KNaCaMg5Si8O22F2) crystals, which were tougher (Sect. 9.3.1) [17–19]. Uno et al. [20] and Qin et al. [21] substituted K+ or Na+ with Ba2+ or Ca2+ as the interlayer ions of mica crystals, which resulted in the formation of high-strength mica glass-ceramics [20, 21]. Oriented mica glass-ceramics fabricated by hot-pressing or extrusion processes had higher strength and toughness than the conventional castable mica glass-ceramics that contained randomly oriented mica crystals with a house-of-cards structure [22–26]. In addition, these materials could be reinforced with ZrO2 crystallized from the bulk glass [27–31]. It has been reported that a calcium mica-based nanocomposite containing nano-size (20–50 nm) tetragonal-ZrO2 particles exhibits notably a high flexural strength (500 MPa) and fracture toughness (3.2 MPa.m½) [27]. The excellent mechanical performance is related to crack deflection by mica plates and ZrO2 particles [27]. According to Serbena et al. [32], the main toughening mechanisms in glass-ceramics (without the chance of phase transformation toughening) are caused by crack bowing and trapping (for low crystallized volume fractions), as well as by the greater elastic modulus and fracture toughness of the crystal precipitates. All of these modifications improved the properties of mica-based glass-ceramics, but they still could not compete with alternative materials such as lithium disilicate GC to survive in this competitive market.
9.2.2 Leucite-Based Glass-Ceramics
Leucite glass-ceramics are used as veneers, inlays, onlays, and anterior and posterior crowns, but their strength is insufficient for fixed posterior bridges. For bridges, this type of GC is veneered onto a flexible, tough metallic framework [14]. However, the risk of the glass-ceramic pulling away from the metal surface still exists. Therefore, sintering should be carefully performed within a temperature range of 550–900 °C, and shrinkage must be controlled to prevent tearing [33, 34]. Michel et al. [35] attempted to minimize this risk by developing nano-coatings on leucite-fluorapatite glass-ceramic particles prior to sintering. The coating influences the rheology of the slurry and the properties of the veneer. The following two substances were chosen for the coatings: (a) a combination of inorganic chemicals (ZnCl2, AlCl3, or BCl3) and polyethylene glycol (PEG) and (b) an exclusive polymer. Both groups of materials positively improved the sintering properties of the glass-ceramics and suppressed extensive tearing [35]. A nano-sized leucite glass-ceramic was further developed by Theocharopoulos et al. [36], who sintered nano-sized commercial glass particles (Ceramco® and IPS Empress®) prepared by high-energy milling to trigger surface crystallization of leucite crystals at the nanoscale. As a result, these new glass-ceramics showed an increased leucite crystal number at the nanoscale (median crystal sizes of ~0.05 μm2). These new glass-ceramics had a higher mean bending strength than the competing commercial materials. The mean bending strengths were, e.g., 255 ± 35 MPa for the nano-leucite glass-ceramic, 76 ± 7 MPa for Ceramco® (restorative porcelain), and 166 ± 31 MPa for IPS Empress® (Leucite GC) [36]. More recently, Aurélio et al. [37] observed an increased bending strength and decreased surface roughness for a leucite-based glass-ceramic sintered at a higher sintering temperature after machining. The crystalline structure was not modified. However, increased sintering time and firing below Tg significantly reduced the fracture strength [37]. Leucite-based glass-ceramics are also well suited for the CAD/CAM process developed by Ivoclar Vivadent AG. This glass-ceramic consists of a total of four to eight main and intermediate layers [38].
In 2000–2011, novel low-wear/high-strength leucite-based glass-ceramics were developed at Queen Mary University by Dr. Cattell’s team to prevent fracture and wear of dental ceramic restorations. Dr. Cattell began his research to overcome problems related to the brittle fracture of porcelain restorations and their poor survival rates and intended to develop leucite-based glass-ceramics by heat extrusion. This novel method led to a homogenous distribution of fine crystals and increased reliability (Weibull modulus, m = 9.4, and σ = 159 MPa) compared with commercial materials (m = 6.1 and σ = 120 MPa, Empress®) [39]. Additionally, controlling the leucite crystal size to 0.15 ± 0.09 μm2 was the key to enhancing the properties of Dr. Cattell’s glass-ceramic [40, 41]. The Cattell team also focused on the fundamental aspects of nucleation and crystal growth of leucite glass-ceramics and powder processing to control surface crystallization and produce first fine and later nanoscale leucite glass-ceramics [42]. These studies were critical to reduce the size of the leucite crystals and had enormous benefits in terms of reduced enamel wear, improved esthetics, and increased strength. Leucite glass-ceramics were subsequently produced with significantly higher flexural strength (σ > 250 MPa), reliability (m = 12), and lower enamel wear [43, 44]. This material could be processed using heat extrusion, CAD-CAM, and 3D printing and was later commercialized by Den-Mat Holdings as an esthetic restorative material with the name of Lumineers® (Table 9.2).
9.2.3 Lithium Disilicate Glass-Ceramics
Lithium disilicate (LS2) glass-ceramics are the third generation of dental glass-ceramic, which were introduced for single- and multiple-unit frameworks. These materials are available as a heat-pressable ingot and a partially crystallized machinable block and are successfully used to produce a crown or bridge framework with mechanical properties that were almost three times higher than those of the leucite-based glass-ceramic. Currently, lithium disilicate glass-ceramic is the most popular restorative glass-ceramic in the field of dental materials, and numerous researches are underway to further improve their properties [13, 14]. Chung et al. [45] have reported that repeated heat-pressing can produce a statistically significant increase in the flexural strength of lithium disilicate glass-ceramic (IPS Empress® II). An interesting study by Lien et al. [46] revealed that intermediate heat treatments in temperature ranges below 590 °C, between 590 and 780 °C, and above 780 °C can influence the final microstructure and properties of the lithium disilicate glass-ceramic (IPS e.max® CAD). The finely knitted mesh of Li2O-SiO2 predominated below 590 °C; spherical-like phases of Li2O-SiO2, Li2O-2SiO2, and Li3PO4 emerged between 590 and 780 °C; and irregularly oblate crystals of Li2O-2SiO2 arose above 780 °C. At each of those three evolutionary stages, the glass-ceramic formed through controlled crystallization often yielded a microstructure that possessed interesting and sometimes peculiar combinations of properties. Additionally, the growth of Li2O-2SiO2 crystals within the IPS e.max® CAD blocks was independent of the overall heating time but dependent on a minimum temperature threshold (780 °C). Groups of samples heated above the minimum temperature threshold (780 °C) up to 840 °C exhibited enhanced flexural strength, fracture toughness, and elastic modulus compared with those of groups that were intentionally not heated above 780 °C [46].
Recent research by Al Mansour et al. [47] showed that spark plasma sintering (SPS) can be used to refine the microstructure of lithium disilicate glass-ceramics (IPS e.max® CAD). Densification by SPS results in textured and fine nanocrystalline microstructures. This group believes that SPS generated glass-ceramic might have unique properties and could be useful in the production of CAD/CAM materials for dentistry [47].
Although P2O5 and ZnO initiate microphase separation, which induces the crystallization pathways and kinetics, it appears that ZrO2 has a more beneficial effect on the crystallization and strengthening of lithium disilicate glass-ceramics [48, 49]. New commercial lithium disilicate glass-ceramics for CAD/CAM are advertised as tougher and more reliable due to the presence of at least 10 wt% ZrO2 dissolved in the residual glass. These glass-ceramics (Table 9.2) are Celtra Duo® (Dentsply), IPS e.max CAD® (Ivoclar), and Suprinity® (Vita). Zirconia influences the crystallization by hampering crystal growth. With increasing ZrO2 content, the crystals become smaller. By increasing the crystallization temperature, the crystal growth decreases, as expected. The translucency of the glass-ceramic can be adjusted by adding ZrO2. A highly translucent glass-ceramic with a contrast ratio of ~0.4 and high three-point bending strength (700–800 MPa) was developed [48].
The current dental glass-ceramics still show a lower load-bearing capacity than polycrystalline ceramics (e.g., Al2O3 and ZrO2); therefore long-span restorative and high-stress areas (e.g., three-unit bridges, implant abutments, etc.) are restricted to ZrO2, Al2O3, or metals. A brand new strategy for strengthening these materials was pursued by Belli et al. [50] to form reinforcing sites by microstructural design of LS2 GC. Such approach demonstrated a potential for application with lithium disilicate (LS2) glass-ceramics, which contain needlelike Li2Si2O5 crystals that deflect propagating cracks. By a special process of heat-pressing of the glass melt through specifically oriented injection channels, crystals were aligned in patterns that led to high mechanical anisotropy (Fig. 9.3) [50]. A strong anisotropic fracture behavior was obtained with the LS2 glass-ceramic through local crystal alignment, leading to fracture energies higher than for the isotropic 3Y-TZP ceramic (Fig. 9.4) [50].
Cross section of a LS2 dental bridge showing the crystal alignment pattern. Different crystal orientations can be distinguished on the gold-sputtered cross section from the different “shadows” on the surface. An S-shaped bundle of parallel crystals formed orthogonal to the long axis of the bridge to the left of the distal connector, right at the midspan. Around it, in the area defined by the dotted lines, crystals follow a distinct orientation due to the convex geometry of the artificial tooth pontic. Mixed orientation patterns formed above the distal connector, leading to negative crack deflection angles and wavy fracture surfaces [50]
Plots of the fracture energy G versus the phase angle ψ. In (a) G was normalized by the mode-I fracture toughness G IC to illustrate the increase or decrease in energy to fracture. In (b) the total energy consumed in the fracture was plotted and showed that for notches submitted to higher phase angles, the energy to fracture of the LS2 glass-ceramic became comparable and even surpassed that of the 3Y-TZP ceramic [50]
9.2.4 Apatite-Based Glass-Ceramics
To further improve the translucency and shade match and to adjust the wear behavior to that of the natural tooth, lithium disilicate, leucite glass-ceramics, and sintered ZrO2 are veneered with an appropriate apatite-containing glass-ceramic using a pressureless sintering process. These glass-ceramics are offered in powdered form for the slurry layering technique and is available in all classical tooth shades [13, 14]. The properties, applications, and typical compositions of these glass-ceramics are summarized in Tables 9.1 and 9.2. Through the development of apatite-based glass-ceramics, researchers reached a stage at which it became possible to produce restorations that contain building blocks in the form of needlelike apatite, similar to those of natural teeth. The needlelike apatite crystals positively influence the esthetic properties and various mechanical parameters of the material. The base glass also contains fluorine, which induces the formation of fluorapatite (Ca5(PO4)3F) and enhances the chemical properties of the material (Table 9.1). Therefore, this glass-ceramic is available (Table 9.2) as a sintered glass-ceramic to replace dentin, reproduce the incisal area, and create specific optical effects (e.g., opalescence over a metallic substrate) [13, 14].
9.2.5 Lithium Zirconium Silicate Glass-Ceramic
After the development of the ZrO2 root canal post and implant abutment, a restorative material was required that can be placed on ZrO2. To fulfill this need, a lithium zirconium silicate glass-ceramic was developed by Schweiger et al. [51] to adjust the coefficient of linear thermal expansion to that of ZrO2 and achieve a certain degree of opacity. This glass-ceramic is layered on the ZrO2 post via heat-pressing and is available in the market (Table 9.2). The improved mechanical properties of the glass-ceramic containing 20 wt% ZrO2 make this material appropriate for use in the posterior region because the esthetics and the opacity of the glass-ceramic play a less important role in this region of the mouth. Finally, the coefficients of linear thermal expansion for glass-ceramics are somewhat lower than that of the ZrO2 post. As a result of this adjustment, a crack-free bond between the glass-ceramic and the ZrO2 abutment is achieved [14, 51].
9.2.6 Survival Rates of Dental Glass-Ceramics
A recent comprehensive review and meta-analysis revealed that survival rates for ceramic inlays, onlays, and overlays including glass-ceramics were between 92% and 95% at 5 years (n = 5811 restorations) and were 91% at 10 years (n = 2154 restorations). Failures were related to fractures/chipping (4%), followed by endodontic complications (3%), secondary caries (1%), debonding (1%), and severe marginal staining (0%). Odds ratios (95% confidence intervals) were 0.19 (0.04–0.96) and 0.54 (0.17–1.69) for pulp vitality and type of tooth involved (premolars vs. molars), respectively. Ceramic inlays, onlays, and overlays showed high survival rates at 5 years and 10 years, and fractures were the most frequent cause of failure [52]. Furthermore, Fradeani et al. [53] reported on the survival rate of leucite glass-ceramic crowns. Crowns were studied over periods ranging from 4 to 11 years. The probability of survival of 125 crowns was 95.2% at 11 years (98.9% in the anterior segment and 84.4% in the posterior segment). Only six crowns had to be replaced. Most of the 119 successful crowns were rated as excellent. According to Kaplan-Meier method, the cumulative survival rate of lithium disilicate crowns is 94.8% after 9 years [54], but only 71.4% of three-unit bridges survive after 10 years [55]. Therefore, crowns made of a lithium disilicate framework can be safely used in the anterior and posterior regions [54], but bridges present a higher risk of fracture than metal-porcelain prostheses or other more recently developed ceramic materials, such as zirconia and alumina [55, 56]. Among the machinable dental glass-ceramics, LS2 has shown significant superior clinical survival rates. This has been shown from a recent database retrospective cohort study performed by Belli et al. [57]. They connected clinical reality and structural investigations on reasons to fracture. They investigated the clinical lifetime of nearly 35,000 all-ceramic restorations placed over 3.5 years (Fig. 9.5), from which 491 fractures were reported. The study also pointed to a trend of clinicians replacing the use of leucite-based glass-ceramics toward the LS2 glass-ceramics for inlays, onlays, crowns, and ZrO2-supported bridges. They concluded that LS2 glass-ceramics increasingly gain acceptability and use within clinical indications [57].
Kaplan-Meier survival curves comparing the restoration type for the same restorative system. IPS e.max CAD and IPS Empress CAD are lithium disilicate and leucite-based glass-ceramics, respectively [57]
9.3 Miscellaneous Dental Glass-Ceramics
As described previously, dental glass-ceramics are attractive materials for dental restoration. However, compared with those of metals and ceramics, the low mechanical strength and fracture toughness of these materials restrict their application for long-term high load-bearing posterior restorations. Therefore, continuous attempts have been made to develop new glass-ceramics with improved mechanical properties and good clinical performance. Some of these glass-ceramics are fluorrichterite, fluorcanasite, diopside, and apatite-mullite glass-ceramics.
9.3.1 Fluorrichterite Glass-Ceramics
The main characteristics of fluorrichterite glass-ceramics are their high fracture toughness (KIC > 3 MPa.m½), optical translucency, and high resistance to thermal shock [14]. High-performance laboratory tableware and domestic kitchenware are manufactured from these glass-ceramics [14]. In 1999, Denry and Holloway [17] began to develop fluorrichterite glass-ceramic for use in dentistry and first investigated the role of MgO content in a glass composition of 67.5SiO2–2Al2O3–12MgO–9CaF2–4Na2O–3.5K2O–1Li2O–1BaO (wt%). The hypothesis was that increasing the amount of magnesium might promote the crystallization of double-chain silicate (amphibole) crystals. The high fracture toughness of amphibole-based glass-ceramics is due to the random orientation of the interlocked crystals, which gives rise to crack deflection [14]. Denry and Holloway also found that in a glass containing 18 wt% MgO, both mica and fluorrichterite are crystallized. In this material, the microstructure consists of interlocked acicular crystals of fluorrichterite (5–10 μm) and mica, and this structure promoted crack deflection and arrest [17]. Furthermore, this same research group increased the sodium amounts in a base glass composition of 57.7SiO2–23.9MgO–6CaF2–0Na2O–8.5K2O–3Li2O–1BaO (wt%). Increasing sodium content led to a decrease in all transformation temperatures, including the onset of melting. A decrease in the viscosity of the glass-ceramics was observed for the glass-ceramic composed of fluorrichterite and mica and was retained after heat treatment at 1000 °C for 4 h [18]. The glass-ceramic containing 1.9 wt% sodium had the highest mean fracture toughness of 2.26 ± 0.15 MPa.m½, which was not significantly different from that of the control material (OPC®, Pentron) [19]. The microstructure of this glass-ceramic exhibited prismatic fluorrichterite and interlocked sheetlike mica crystals, which deflect propagating cracks. Crystallization of fluorrichterite might account for the significant increase in fracture toughness compared with that of mica-based glass-ceramics (as an example) [19]. In Fig. 9.6, crack deflection is observed at each interaction between the crack front and the fluorrichterite crystals [19].
Scanning electron micrographs of Vickers indentation-induced cracks in the fluorrichterite glass-ceramic containing (a) 1.9 wt% sodium and (b) the glass-ceramic containing 3.8 wt% sodium [19]
The effect of crystallization heat treatment on the microstructure and biaxial strength of fluorrichterite glass-ceramics was also reported by the same authors [58], who observed twofold variation in the biaxial flexural strength of fluorrichterite glass-ceramics depending on the temperature and duration of the crystallization heat treatment. This result was believed to be due to the formation of a low-expansion surface layer composed of roedderite (K2Mg5Si12O30). The expansion mismatch promoted the development of surface compressive stresses and efficiently increased the flexural strength of the glass-ceramic. Higher heat treatment temperatures or longer durations likely led to an increase in thickness of this layer, thereby reducing the intensity of the surface compressive stresses and causing a decrease in strength. In addition, these conditions caused a coarsening of the microstructure that could also weaken the glass-ceramic by reducing the number of possible crack-crystal interactions [58]. The significance and long-term goal of Denry and Holloway’s work was to develop a dental glass-ceramic processed at low temperature, e.g., with heat-pressing, that retained the fluorrichterite microstructure and excellent mechanical properties. Later on, other scientists also attempted to crystallize different chain silicate minerals, such as diopside or wollastonite, in the vicinity of mica crystals to benefit from their toughening ability [59–61]. Almuhamadi et al. [62] and Sinthuprasirt et al. [63] also prepared diopside and leucite-diopside glass-ceramics, respectively, to produce novel strong and thermally compatible veneers for zirconia restoration to overcome chipping and failure issues. The improvements were significant, but it appears that these materials have not yet been considered for clinical applications.
9.3.2 Fluorcanasite Glass-Ceramics
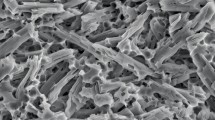
Fluorcanasite (Ca5Na4K2Si12O30F4) is another double-chain silicate mineral which its crystallization in glasses with an acicular interlocked microstructure (Fig. 9.7) gives rise to strength and fracture toughness of the resulting glass-ceramics [14].
SEM micrograph of a fracture surface of the canasite glass-ceramic (×2500 magnification) [64]
A number of initial studies were performed by Anusavice’s and Noort’s team at Florida and Sheffield Universities, respectively, to evaluate potential application of fluorcanasite glass-ceramics in restorative dentistry. In the period 1997–2003, van Noort et al. [65] demonstrated that fluorcanasite glass-ceramics derived from the base glass composition of 60SiO2–10Na2O–5K2O–15CaO–10CaF2 (wt%) show promising properties and can be fabricated using conventional routes [64–66]. At the same time, Anusavice and Zhang [67] reported that the chemical durability of fluorcanasite glass-ceramics is not adequate for dental applications and they were not able to improve either chemical durability or mechanical strength via the addition of Al2O3 up to 15 wt%. It was observed that increased Al2O3 content significantly affected the crystal size, crystal shape, aspect ratio, and crystal aggregation characteristics of the fluorcanasite glass-ceramics [67, 68]. In an attempt to control the solubility of this glass-ceramic, systematic additions of SiO2 and AlPO4 were tested by Bubb et al. [69]. The solubility was reduced from 2359 to 624 μg/cm2 (according to ISO 6872). An initial increase was observed in biaxial flexural strength, i.e., 123–222 MPa with small additions, but larger additions reduced the strength to 147 MPa. These findings were attributed to an increased volume fraction of residual glassy matrix [69]. Stockes et al. [70] attempted to further reduce the chemical solubility of these glass-ceramics by investigating the mixed alkali effect due to variation in the K and Na contents. They found that by changing the alkali ratio of the base glass composition (the above composition) from K/(K+Na) = 0.33 to 0.47, it was possible to significantly reduce the chemical solubility of the glass-ceramic. This glass-ceramic exhibited a minimum chemical solubility of 650 μg/cm2 at a composition of K/Na = 7/8. This solubility is acceptable for dental core ceramics, which should have a solubility of less than 2000 μg/cm2, but it is not suitable for direct contact with the mouth environment, which requires a solubility of less than 100 μg/cm2 [15, 70]. Finally, Pollington and van Noort [71] managed to adjust the chemical solubility and mechanical properties of the glass-ceramic with ZrO2 addition, and their optimum composition approximately contained 61SiO2–6Na2O–8K2O–11CaO–12CaF2–2ZrO2 (wt%). The appropriate melting schedule for this composition was found to be 1 h of holding and stirring at 1350 °C. The heat treatment schedule of 2 h nucleation and 2 h crystallization produced the greatest amount of the fluorcanasite phase. The glass-ceramic had an acceptable chemical solubility (722 ± 177 μg/cm2) and high biaxial flexural strength (250 ± 26 MPa), fracture toughness (4.2 ± 0.3 MPa.m½), and hardness (5.2 ± 0.2 GPa) and had the potential for use as a core material for veneered resin-bonded ceramic restorations. Furthermore, this fluorcanasite glass-ceramic was found to be machinable using standard CAD/CAM technology and demonstrated a high degree of translucency [71]. It has also been proved that this glass-ceramic forms a sufficient and durable bond when bonded with a composite resin, without the need for acid etching with HF solution [72]. More recently, Eilaghi et al. [73] have shown that fluorcanasite glass-ceramic can be pressureless sintered at 1000 °C to an appropriate relative density of 91.3 ± 0.1% and desirable mechanical properties (σ = 137 ± 7 MPa and KIC = 2.6 ± 0.1 MPa.m½) [73].
9.3.3 Apatite-Mullite Glass-Ceramics
In the mid-1990s, Hill et al. [74] introduced apatite-mullite glass-ceramics as potential dental or bioactive glass-ceramics. The optimum glass composition was 33.33SiO2–11.11P2O5–22.22Al2O3–22.22CaO–11.11CaF2 in mol%. This glass-ceramic, which was heat treated at approximately 900 °C, consisted of elongated fluorapatite (Ca10(PO4)6F2) and mullite (3Al2O3.2SiO2) crystals. Crystallization occurred by an internal nucleation mechanism that involved prior amorphous phase separation. A fracture toughness value greater than 3 MPa.m½ was reported [74, 75]. Later, Gorman and Hill [76, 77] attempted to develop a dental restoration material using a similar glass-ceramic via the heat-pressing technique by reducing the Al2O3 content and envisioning that this reduction could adjust the viscosity for heat-pressing [76, 77]. The conclusion of these researchers was that glasses with various Al2O3 contents are easily formed and crystallized to fluorapatite. Mullite and anorthite were formed as a second crystal phase. However, crystallization during heat-pressing resulted in a loss of control of the process but was not considered detrimental if the future growth of these crystals could be controlled [76]. A fracture toughness of 2.7 ± 0.4 MPa.m½ was reported for the glass-ceramic containing 32.6SiO2–10.9P2O5–20.3Al2O3–32.6CaO–3.6CaF2 (mol%) that was heat treated for 8 h at 1150 °C. The highest flexural strength of 194 ± 75 MPa was obtained by heat-pressing the same glass for 1 h at 1150 °C. Increasing the holding time increased the crystal size and the extent of microcracking in this glass-ceramic, thus lowering the flexural strength. Microcracks appeared to increase the fracture toughness of the glass-ceramics, probably by a crack termination mechanism [77]. However, the relatively high solubility of apatite-mullite glass-ceramics was always the main issue [78]. Consequently, Fathi et al. [79] evaluated the effect of varying the CaF2 content on the chemical solubility. They increased the CaF2 in the initial glass from 4 to 20 mol%. All compositions easily formed glasses and, upon heat treatment, crystallized to form apatite and apatite-mullite. Increasing the CaF2 content led to an increase in bending strength but also increased the solubility. The chemical solubility (150–380 μg/cm2) was still higher than that of the control glass-ceramic (IPS Empress® II, 78 μg/cm2) but was acceptable for a dental core ceramic [79, 80]. A maximum bending strength of 157 ± 15 MPa was reported for a sample containing 20 mol% CaF2 [80]. These same researchers also added TiO2 and ZrO2 to control the mechanical properties and solubility [81, 82], and their studies demonstrated that up to 1 mol% of ZrO2 and TiO2 were effective for controlling the solubility and mechanical properties of these apatite-mullite glass-ceramics [81]. The lowest chemical solubility and highest bending strength were 204 ± 29 μg/cm2 and 174 ± 38 MPa, respectively [81]. However, increasing the TiO2 concentration to greater than 2.5 wt% led to a significant increase in solubility and reduced bending strength [82]. Mollazadeh et al. [83] showed that 3 wt% TiO2 and BaO addition increased the bending strength and fracture toughness of apatite-mullite glass-ceramics. However, 3 wt% ZrO2 and an extra amount of SiO2 had no significant effect [83]. The mechanical properties of the resulting glass-ceramics after temperature changes (5–60 °C) in aqueous media remained nearly unchanged for the samples containing TiO2 and ZrO2, whereas a high reduction was observed with the addition of BaO and extra amounts of SiO2. Furthermore, after immersion in hot water, the concentration of Ca2+ and F− ions released from samples with BaO or with excess amounts of SiO2 was higher than those of TiO2- and ZrO2-containing glass-ceramics [84]. It is apparent that these apatite-mullite glass-ceramics are promising restorative materials, but their high chemical solubility still restricts their application for use in the mouth environment . Therefore, these materials must be first considered for core buildup.
9.4 Conclusions and Trends
Restorative dental materials are moving from metal alloy-containing to all-ceramic restorations, and this chapter demonstrates that glass-ceramics work well as all-ceramic restorations. The following ten topics warrant further research [13]:
-
1.
Research and development are underway to further improve the fracture toughness and esthetics of dental glass-ceramics to enable them to compete with their current contenders (e.g., zirconia and hybrids) for posterior restorations. We agree with Höland et al. [85] that comprehensive knowledge of toughening mechanisms is a necessary step to open new directions for development of tough glass-ceramics. Therefore, future research activities should be focused on gaining a better understanding of the mechanisms of toughening, such as transformation toughening, bridging, microcracking, and pulling out, that can be stimulated by controlled crystallization of different crystals with a variety of morphologies and microstructures. Additionally, various coloring agents and pigments should be deeply and thoroughly tested to adjust the shades and esthetics of glass-ceramics. On the other hand, the morphology of crystals from the nano- to microscale, which can be controlled by precise adjustment of the chemical composition and crystallization process, might strongly influence their optical properties, but the published information on these topics is scarce.
-
2.
New methods (e.g., meta-analyses) can be used to expand the range of glass-ceramic composition. For instance, it was recently demonstrated that new nano-glass-ceramics with a notably high ZrO2 content can be synthesized using sol-gel methods [86, 87]. The technology required to achieve this goal could rely on chemistry-based and applied nanotechnology.
-
3.
New or improved sintering/crystallization processes, such as microwave heating [88], laser crystallization [89, 90], spark plasma sintering [47, 91], biomimetic assemblage of crystals [92], textured crystallization, and electron beam crystallization, should be further developed.
-
4.
Chemical strengthening of RDGCs by ion exchange, as tested by Kawai et al. [93] and Fischer et al. [94–96], is a promising route and should be further pursued.
-
5.
Glass-ionomer composites are widely used in restorative dentistry. We believe that glass-ceramic powders, including bioactive formulations, can also be used as inorganic fillers in these composite restoratives. In at least two research studies, Liu et al. [97] and Mollazadeh et al. [98] used porous mica-fluorapatite and fluorapatite-mullite glass-ceramic fillers to reinforce dental resin-based composites.
-
6.
New coating technologies and the properties of coatings on dental implants should be improved. For example, degradation over time, which leads to detachment of coating, is a noticeable drawback.
-
7.
The development of restorative glass-ceramics or composites which in contact with bone and surrounding tissues show a cement-like behavior and facilitate biological surface responses for marginal attachment is another challenging field of research.
-
8.
Glass-ceramic matrix composites have been rarely investigated for restorative dentistry and demand additional attention.
-
9.
Dental tissue engineering for construction of tooth organs is a brand new and highly interesting direction. A clear and distinct shift is occurring in regenerative medicine from use of synthetic materials or tissue grafts to a more explicit approach that applies scaffolds for hosting cells and/or biological molecules to create functional replacement tissues in diseased or damaged dental sites.
-
10.
Finally, (expensive, time-consuming) clinical tests should be encouraged to evaluate dental glass-ceramics in real application cases.
All of these ideas and several others not reported in this work can only be achieved by increasing interactions among materials engineers and scientists, chemists, dentists, and biologists.
References
Sakaguchi RL, Powers JM. Craig’s restorative dental materials. 13th ed. Netherland: Elsevier; 2011.
Zanotto ED. A bright future for glass-ceramics. Am Ceram Soc Bull. 2010;89(8):19–27.
Montazerian M, Singh SP, Zanotto ED. An analysis of glass-ceramic research and commercialization. Am Ceram Soc Bull. 2015;94(4):30–5.
Höland W. Biocompatible and bioactive glass-ceramics – state of the art and new directions. J Non-Cryst Solids. 1997;219:192–7.
Höland W, Rheinberger V, Apel E, van’t Hoen C, Höland M, Dommann A, Obrecht M, Mauth C, Graf-Hausner U. Clinical applications of glass-ceramics in dentistry. J Mater Sci Mater Med. 2006;17(11):1037–42.
Höland W, Rheinberger V. Dental glass-ceramics. In: Kokubo T, editor. Bioceramics and their clinical applications. Cambridge: Woodhead Publishing Limited; 2008. p. 548–68.
Höland W, Rheinberger V. Bioengineering of glass-ceramics and ceramics for dental restoration. In: Garcia A, Durand C, editors. Bioengineering: principles, methodologies and applications. Hauppauge: Nova Science Publishers; 2010. p. 169–78.
Pollington S. Novel glass-ceramics for dental restorations. J Contemp Dent Pract. 2011;12(1):60–7.
Johnson A, Sinthuprasirt P, Fathi H, Pollington S. Current glass-ceramic systems used in dentistry. In: Nandyala SH, Santos JD, editors. Current trends on glass and ceramic materials. Sharjah: Bentham Science Publishers Ltd.; 2013. p. 49–72.
Saint-Jean SJ. Dental glasses and glass-ceramics. In: Shen JZ, editor. Advanced ceramics for dentistry. Netherland: Elsevier; 2014. p. 255–77.
Montazerian M, Zanotto ED. History and trends of bioactive glass-ceramics. J Biomed Mater Res A. 2016;104(5):1231–49.
Montazerian M, Zanotto ED. Bioactive glass-ceramics: processing, properties and applications. In: Boccaccini AR, Brauer DS, Hupa L, editors. Bioactive glasses: fundamentals, technology and applications. London: Royal Society of Chemistry; 2016. p. 27–33.
Montazerian M, Zanotto ED. Bioactive and inert dental glass-ceramics. J Biomed Mater Res A. n.d. doi: 10.1002/jbm.a.35923, 2017;105(2):619–39.
Höland W, Beall G. Glass-ceramic technology. 2nd ed. Westerville: The American Ceramic Society & Wiley; 2012.
ISO 6872. Dentistry – ceramic materials. 2015.
Denry IL, Lejus AM, Théry J, Masse M. Preparation and characterization of a new lithium-containing glass-ceramic. Mater Res Bull. 1999;34(10–11):1615–27.
Denry IL, Holloway JA. Effect of magnesium content on the microstructure and crystalline phases of fluoramphibole glass-ceramics. J Biomed Mater Res. 2000;53(4):289–96.
Denry IL, Holloway JA. Effect of sodium content on the crystallization behavior of fluoramphibole glass-ceramics. J Biomed Mater Res. 2002;63(1):48–52.
Denry IL, Holloway AJ. Elastic constants, Vickers hardness, and fracture toughness of fluorrichterite-based glass-ceramics. Dent Mater. 2004;20(3):213–9.
Uno T, Kasuga T, Nakajima K. High-strength mica-containing glass-ceramics. J Am Ceram Soc. 1991;74(12):3139–41.
Qin F, Zheng S, Luo Z, Li Y, Guo L, Zhao Y, Fu Q. Evaluation of machinability and flexural strength of a novel dental machinable glass-ceramic. J Dent. 2009;37(10):776–80.
Cheng K, Wan J, Liang K. Hot-pressed mica glass-ceramics with high strength and toughness. J Am Ceram Soc. 1999;82(6):1633–4.
Cheng K, Wan J, Liang K. Enhanced mechanical properties of orientated mica glass-ceramics. Mater Lett. 1999;39(6):350–3.
Habelitz S, Carl G, Rüssel C. Processing, microstructure and mechanical properties of extruded mica glass-ceramics. Mater Sci Eng A. 2001;307(1–2):1–14.
Denry IL, Baranta G, Holloway JA, Gupta PK. Effect of processing variables on texture development in a mica-based glass-ceramic. J Biomed Mater Res B. 2003;64(2):70–7.
Denry IL, Holloway JA. Effect of heat pressing on the mechanical properties of a mica-based glass-ceramic. J Biomed Mater Res B. 2004;70(1):37–42.
Uno T, Kasuga T, Nakayama S, Ikushima AJ. Microstructure of mica-based nanocomposite glass-ceramics. J Am Ceram Soc. 1993;76(2):539–41.
Bürke H, Durschang B, Meinhardt J, Müller G. Nucleation and crystal growth kinetics in ZrO2-strengthened mica-glass-ceramics for dental application. Glass Sci Technol Glastechnische Ber. 2000;73(1):270–7.
Li H, You D, Zhou C, Ran J. Study on machinable glass-ceramic containing fluorophlogopite for dental CAD/CAM system. J Mater Sci Mater Med. 2006;17(11):1133–7.
Montazerian M, Alizadeh P, Eftekhari Yekta B. Pressureless sintering and mechanical properties of mica glass-ceramic/Y-PSZ composite. J Eur Ceram Soc. 2008;28(14):2687–92.
Montazerian M, Alizadeh P, Eftekhari Yekta B. Processing and properties of a mica-apatite glass-ceramic reinforced with Y-PSZ particles. J Eur Ceram Soc. 2008;28(14):2693–9.
Serbena FC, Mathias I, Foerster CE, Zanotto ED. Crystallization toughening of a model glass-ceramic. Acta Mater. 2015;86:216–28.
Höland W, Rheinberger V, Wegner S, Frank M. Needle-like apatite-leucite glass-ceramic as a base material for the veneering of metal restorations in dentistry. J Mater Sci Mater Med. 2000;11(1):11–7.
Szabó I, Nagy B, Völksch G, Höland W. Structure, chemical durability and microhardness of glass-ceramics containing apatite and leucite crystals. J Non-Cryst Solids. 2000;272(2–3):191–9.
Michel K, Pantano CG, Ritzberger C, Rheinberger V, Höland W. Coatings on glass-ceramic granules for dental restorative biomaterials. Int J Appl Glas Sci. 2011;2(1):30–8.
Theocharopoulos A, Chen X, Wilson RM, Hill RG, Cattell MJ. Crystallization of high-strength nano-scale leucite glass-ceramics. Dent Mater. 2013;29(11):1149–57.
Aurélio IL, Fraga S, Dorneles LS, Bottino MA, May LG. Extended glaze firing improves flexural strength of a glass ceramic. Dent Mater. 2015;31(12):e316–24.
Ritzberger C, Apel E, Höland W, Peschke A, Rheinberger VM. Properties and clinical application of three types of dental glass-ceramics and ceramics for CAD-CAM technologies. Dent Mater. 2010;3(6):3700–13.
Cattell MJ, Chadwick TC, Knowles JC, Clarke RL, Lynch E. Flexural strength optimization of a leucite reinforced glass ceramic. Dent Mater. 2001;17(1):21–33.
Cattell MJ, Chadwick TC, Knowles JC, Clarke RL, Samarawickrama DYD. The nucleation and crystallization of fine grained leucite glass-ceramics for dental applications. Dent Mater. 2006;22(10):925–33.
Cattell MJ, Chadwick TC, Knowles JC, Clarke RL. Development and testing of glaze materials for application to the fit surface of dental ceramic restorations. Dent Mater. 2009;25(4):431–41.
Chen XI, Chadwick TC, Wilson RM, Hill R, Cattell MJ. Crystallization of high strength-fine-sized leucite glass-ceramics. J Dent Res. 2010;89:1510–6.
Chen XI, Chadwick TC, Wilson RM, Hill R, Cattell MJ. Crystallization and flexural strength optimization of fine-grained leucite glass-ceramics for dentistry. Dent Mater. 2011;27(11):1153–61.
Theocharopoulos A, Chen X, Hill R, Cattell MJ. Reduced wear of enamel with novel fine and nano-scale leucite glass-ceramics. J Dent. 2013;41(6):561–8.
Chung K-H, Liao J-H, Duh J-G, Chan DC-N. The effects of repeated heat-pressing on properties of pressable glass-ceramic. J Oral Rehabil. 2009;36(2):132–41.
Lien W, Roberts HW, Platt JA, Vandewalle KS, Hill TJ, Chu TG. Microstructural evolution and physical behavior of a lithium disilicate glass-ceramic. Dent Mater. 2015;31(8):928–40.
Al Mansour F, Karpukhina N, Grasso S, Wilson RM, Reece MJ, Cattell MJ. The effect of spark plasma sintering on lithium disilicate glass-ceramics. Dent Mater. 2015;31(10):e226–35.
Apel E, van’t Hoen C, Rheinberger V, Höland W. Influence of ZrO2 on the crystallization and properties of lithium disilicate glass-ceramics derived from a multi-component system. J Eur Ceram Soc. 2007;27(2–3):1571–7.
Khalkhali Z, Eftekhari Yekta B, Marghussian VK. Mechanical and chemical properties of Zr and P-doped lithium disilicate glass ceramics in dental restorations. Int J Appl Ceram Technol. 2012;9(3):497–506.
Belli R, Wendler M, Zorzin JI, da Silva LH, Petschelt A, Lohbauer U. Fracture toughness mode mixity at the connectors of monolithic 3Y-TZP and LS2 dental bridge constructs. J Eur Ceram Soc. 2015;35(13):3701–371.
Schweiger M, Frank M, Clausbruch CV, Höland W, Rheinberger V. Microstructure and properties of a composite system for dental applications composed of glass-ceramics in the SiO2–Li2O–ZrO2–P2O5 system and ZrO2-ceramic (TZP). J Mater Sci. 1999;34(18):4563–72.
Morimoto S, Rebello de Sampaio FBW, Braga MM, Sesma N, Özcan M. Survival rate of resin and ceramic inlays, onlays, and overlays: a systematic review and meta-analysis. J Dent Res. 2016;95(5):985–94.
Fradeani M, Redemagni M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: a retrospective study. Quintessence Int. 2002;33(7):503–10.
Gehrt M, Wolfart S, Rafai N, Reich S, Edelhoff D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig. 2013;17(1):275–84.
Solá-Ruiz MF, Lagos-Flores E, Román-Rodriguez JL, Highsmith JR, Fons-Font A, Granell-Ruiz M. Survival rates of a lithium disilicate-based core ceramic for three-unit esthetic fixed partial dentures: a 10-year prospective study. Int J Prosthodont. 2013;26(2):175–80.
Makarouna M, Ullmann K, Lazarek K, Boening KW. Six-year clinical performance of lithium disilicate fixed partial dentures. Int J Prosthodont. 2011;24(3):204–6.
Belli R, Petschelt A, Hofner B, Hajtó J, Scherrer SS, Lohbauer U. Fracture rates and lifetime estimation of CAD/CAM all-ceramic restorations. J Dent Res. 2016;95(1):67–73.
Denry IL, Holloway JA. Effect of crystallization heat treatment on the microstructure and biaxial strength of fluorrichterite glass-ceramics. J Biomed Mater Res B Appl Biomater. 2007;80(2):454–9.
Tulyaganov DU, Agathopoulos S, Fernandes HR, Ventura JM, Ferreira JMF. Preparation and crystallization of glasses in the system tetrasilicic mica-fluorapatite-diopside. J Eur Ceram Soc. 2004;24(13):3521–8.
Alizadeh P, Eftekhari Yekta B, Javadi T. Sintering behavior and mechanical properties of the mica-diopside machinable glass-ceramics. J Eur Ceram Soc. 2008;28(8):1569–73.
Faeghi-Nia A, Marghussian VK, Taheri-Nassaj E, Pascual MJ, Durán A. Pressureless sintering of apatite/wollastonite-phlogopite glass-ceramics. J Am Ceram Soc. 2009;92(7):1514–8.
Almuhamadi J, Karpukhina N, Cattell M. Diopside glass-ceramics for dental and biomedical applications. Adv Sci Technol. 2014;96:15–20.
Sinthuprasirt P, van Noort R, Moorehead R, Pollington S. Evaluation of a novel multiple phase veneering ceramic. Dent Mater. 2015;31(4):443–52.
Johnson A, Shareef MY, van Noort R, Walsh JM. Effect of furnace type and ceramming heat treatment conditions on the biaxial flexural strength of a canasite glass-ceramic. Dent Mater. 2000;16(4):280–4.
van Noort R, Shareef MY, Johnson A, James PF. Properties of a canasite-based castable glass-ceramic. J Dent Res. 1997;76(21):61–61.
Johnson A, Van Noort R, Hatton PV, Walsh JM. The effect of investment material and ceramming regime on the surface roughness of two castable glass-ceramic material. Dent Mater. 2003;19(3):218–25.
Anusavice KJ, Zhang N-Z. Chemical durability of dicor and fluorocanasite-based glass-ceramics. J Dent Res. 1998;77(7):1553–9.
Zhang N-Z, Anusavice KJ. Effect of alumina on the strength, fracture toughness, and crystal structure of fluorcanasite glass-ceramics. J Am Ceram Soc. 1999;82(9):2509–13.
Bubb NL, Wood DJ, Streit P. Reduction of the solubility of fluorcanasite based glass ceramics by additions of SiO2 and AlPO4. Glass Technol. 2004;45(2):91–3.
Stokes CW, Van Noort R, Hand R. Investigation of the chemical solubility of mixed-alkali fluorcanasite forming glasses. J Non-Cryst Solids. 2006;352(2):142–9.
Pollington S, van Noort R. Manufacture, characterisation and properties of novel fluorcanasite glass-ceramics. J Dent. 2012;40(11):1006–17.
Pollingtona S, Fabianelli A, van Noort R. Microtensile bond strength of a resin cement to a novel fluorcanasite following different surface treatments. Dent Mater. 2010;26(9):864–72.
Eilaghi M, Montazerian M, Eftekhari Yekta B. Effect of partial substitution of K2O for Na2O on sintering, crystallization and mechanical properties of SiO2−CaO−K2O−Na2O−CaF2 glass-ceramics. Trans Indian Ceram Soc. 2016;75(1):1–6.
Hill RG, Wood DJ. Apatite-mullite glass ceramics. J Mater Sci Mater Med. 1995;6(6):311–8.
Clifford A, Hill RG. Apatite-mullite glass-ceramics. J Non-Cryst Solids. 1996;196:346–52.
Gorman CM, Hill RG. Heat-pressed ionomer glass-ceramics part I: an investigation of flow and microstructure. Dent Mater. 2003;19(4):320–6.
Gorman CM, Hill RG. Heat-pressed ionomer glass-ceramics. Part II. Mechanical property evaluation. Dent Mater. 2004;20(3):252–61.
Hill RG. Bioactive glass-ceramics. In: Ducheyne P, editor. Comprehensive biomaterials, Volume 1: metallic, ceramic and polymeric biomaterials; 2011. p. 181–6.
Fathi H, Johnson A, van Noort R, Ward JM, Brook IM. The effect of calcium fluoride (CaF2) on the chemical solubility of an apatite-mullite glass-ceramic material. Dent Mater. 2005;21(6):551–6.
Fathi H, Johnson A, van Noort R, Ward JM. The influence of calcium fluoride (CaF2) on biaxial flexural strength of apatite-mullite glass-ceramic materials. Dent Mater. 2005;21(9):846–51.
Fathi HM, Miller C, Stokes C, Johnson A. The effect of ZrO2 and TiO2 on solubility and strength of apatite-mullite glass-ceramics for dental applications. J Mater Sci Mater Med. 2014;25(3):583–94.
Fathi HM, Johnson A. The effect of TiO2 concentration on properties of apatite-mullite glass-ceramics for dental use. Dent Mater. 2016;32(2):311–22.
Mollazadeh S, Eftekhari Yekta B, Javadpour J, Yusefi A, Jafarzadeh TS. The role of TiO2, ZrO2, BaO and SiO2 on the mechanical properties and crystallization behavior of fluorapatite-mullite glass-ceramics. J Non-Cryst Solids. 2013;361(1):70–7.
Mollazadeh S, Ajalli S, Kashi TSJ, Eftekhari Yekta B, Javadpour J, Jafari S, Youssefi A, Fazel A. The effect of aqueous media on the mechanical properties of fluorapatite-mullite glass-ceramics. Dent Mater. 2015;31(11):1370–6.
Höland W, Rheinberger V, Apel E, Ritzberger C, Rothbrust F, Kappert H, Krumeich F, Nesper R. Future perspectives of biomaterials for dental restoration. J Eur Ceram Soc. 2009;29(7):1291–7.
Persson C, Unosson E, Ajaxon I, Engstrand J, Engqvist H, Xia W. Nano grain sized zirconia-silica glass ceramics for dental applications. J Eur Ceram Soc. 2012;32(16):4105–10.
Montazerian M, Schneider JF, Eftekhari Yekta B, Marghussian VK, Rodrigues AM, Zanotto ED. Sol-gel synthesis, structure, sintering and properties of bioactive and inert nano apatite-zirconia glass-ceramics. Ceram Int. 2015;41(9):11024–45.
Mahmoud M, Folz D, Suchicital C, Clark D, Fathi Z. Variable frequency microwave (VFM) processing: a new tool to crystallize lithium disilicate glass. Ceram Eng Sci Proc. 2006;27(6):143–53.
Liu J, Zhang B, Yan C, Shi Y. The effect of processing parameters on characteristics of selective laser sintering dental glass-ceramic powder. Rapid Prototyp J. 2010;16(2):138–45.
Cam P, Neuenschwander B, Schwaller P, Köhli B, Lüscher B, Senn F, Kounga A, Appert C. A novel laser-based method for controlled crystallization in dental prosthesis materials, progress in biomedical optics and imaging – proceedings of SPIE 9306. 2015. Article number 930607.
Fu L, Wu C, Grandfield K, Unosson E, Chang J, Engqvist H, Xia W. Transparent single crystalline ZrO2-SiO2 glass nanoceramic sintered by SPS. J Eur Ceram Soc. 2016;36(14):3487–94.
Fu Q, Beall G, Smith C. Nature-inspired design of strong, tough glass-ceramics, MRS Bulletin, accepted. 2017.
Kawai K, Inoue M, Tsuchitani Y. Effect of ion-exchange treatment on mechanical properties of new dental ceramics. Am J Dent. 2003;16(5):347–50.
Fischer H, Marx R. Suppression of subcritical crack growth in a leucite-reinforced dental glass by ion exchange. J Biomed Mater Res A. 2003;66(4):885–9.
Fischer H, Brehme M, Telle R, Marx R. Effect of ion exchange of glazed dental glass ceramics on strength parameters. J Biomed Mater Res A. 2005;72(2):175–9.
Fischer H, De Souza RA, Wätjen AM, Richter S, Edelhoff D, Mayer J, Martin M, Telle R. Chemical strengthening of a dental lithium disilicate glass-ceramic material. J Biomed Mater Res Part A. 2008;87(3):582–7.
Liu Y, Tan Y, Lei T, Xiang Q, Han Y, Huang B. Effect of porous glass–ceramic fillers on mechanical properties of light-cured dental resin composites. Dent Mater. 2009;25(6):709–15.
Mollazadeh S, Javadpour J, Eftekhari Yekta B, Jafarzadeh TS, Youssefi A. Synthesis and characterisation of dental composite materials reinforced with fluoroapatite-mullite glass-ceramic particles. Adv Appl Ceram. 2013;112(5):294–300.
Acknowledgments
The authors are grateful to the São Paulo Research Foundation (FAPESP, # 2013/07793-6) for financial support of this work and for the postdoctoral fellowship granted to Maziar Montazerian (# 2015/13314-9).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Montazerian, M., Zanotto, E.D. (2017). Restorative Dental Glass-Ceramics: Current Status and Trends. In: Kaur, G. (eds) Clinical Applications of Biomaterials. Springer, Cham. https://doi.org/10.1007/978-3-319-56059-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-56059-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-56058-8
Online ISBN: 978-3-319-56059-5
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)