Abstract
Research over the past 15 years has dramatically changed how surgical care is viewed within global health. Once thought as too expensive and inappropriate for settings of limited resources, surgical care is now recognized as an essential component of strong health systems and capable of treating a wide spectrum of important clinical problems in a highly cost-effective manner. More so, the economic losses from untreated surgical conditions far exceed any expenditure that would be required to scale-up surgical care—making surgical care an attractive investment for promoting economic growth in low- and middle-income countries (LMICs). In this chapter, we trace the remarkable transformation in thinking that has occurred around the economic issues of surgical care in settings of limited resources. To do so, we provide a brief overview of global economic development and its relationship to health, review the economic case for surgical care in LMICs, and conclude with a discussion of financing of surgical care in the era of new Sustainable Development Goals. With efforts already underway to scale-up surgical care in some countries, the economics of surgical care will continue to be one of the most important topics in global surgery.
“Instead of development assistance for health, funding surgery is health assistance for development.”
Ramiro Guerrero
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Economic development
- Global surgery
- Global health history
- Surgical scale-up
- Cost-effectiveness
- Developmental assistance for health
- Millennium development goals
- Sustainable development goals
- Disease control priorities
- Lancet commission on global surgery
- Lancet commission on investing in health
Introduction
Surgical care in LMICs, a therapeutic necessity for the treatment of almost a third of the burden of human diseases, has long been hindered by the misconception that it is too expensive for settings of limited resources, or that it has limited public health value [1]. The consequences of this neglect have made a bad situation worse. Currently, almost 70% of the world’s population lacks access to safe, affordable, and timely surgical and anesthesia care, including over 90% of those living in the world’s poorest regions [2]. Fortunately, research over the past 15 years is changing how surgical care is viewed within global health. A more contemporary view of emergency and essential surgical care is that it is a cross-cutting intervention with a role in a wide spectrum of clinical problems; capable of addressing a large burden of disease while strengthening health systems, and cost-effective as many other widely accepted public health interventions.
In this chapter, we trace the remarkable transition in thinking that has occurred around the economics of surgical care in LMICs. First, we provide a brief overview of global economic development and its relationship to health. We then review research demonstrating the economic importance of surgical care. The chapter concludes with a section on the financing of surgical care in the era of the new Sustainable Development Goals (SDGs).
Brief Overview of Global Economic Development and Its Relationship to Health
The Essentials
-
A new focus on global economic development originated post-World War II
-
Global economic growth has been substantial but uneven
-
A healthy population is critical for economic growth, and vice versa
-
The World Bank and other institutions view improved health as a vehicle for growth
The concept that global economic development is important originated in the reconstruction period following World War II [3]. The rationale for this new found enthusiasm for global economic development is perhaps best illustrated by some of the comments made by President Harry Truman in his 1949 inaugural speech [4]:
More than half the people of the world are living in conditions approaching misery. Their food is inadequate; they are victims of disease. Their economic life is primitive and stagnant. Their poverty is a handicap and a threat both to them and to more prosperous areas. For the first time in history humanity possesses the knowledge and the skill to relieve the suffering of these people … I believe that we should make available to peace-loving peoples the benefits of our store of technical knowledge in order to help them realize their aspirations for a better life… Greater production is the key to prosperity and peace. And the key to greater production is a wider and more vigorous application of modem scientific and technical knowledge.
By the time Harry Truman was elected president, international efforts were already underway to improve social and economic development in some of the least developed areas of the world. The World Bank was created in 1944 with the stated goal of eradicating global poverty, attempting to do this by providing loans to developing countries for capital programs [5]. In 1948, the World Health Organization (WHO) was organized with the mandate to attain the highest possible level of health for all people through coordination of international public health efforts [6].
Since then, the world has made significant gains in reducing the number of those most impoverished. According to the World Bank’s most recent estimates, the percent of the world’s population living at or below $1.90 per day has declined from 44% in 1981 to 12.7% in 2012 [7]. These numbers translate into almost a billion people living at or below the $1.90 per day in 2012. If the slightly higher income cutoff of $3.10 per day is used, this exceeds two billion people. Moreover, reductions in poverty have not been uniform across the world. As an example, more than two-fifths of individuals in Sub-Saharan Africa still live in poverty.
It has long been recognized that economic development and health are inextricably linked [8]. In general, economic growth results in higher private incomes that allow for greater investments in social services such as healthcare, safe drinking water, and public education. The converse is also true: healthier populations achieve greater economic growth. The reason for the latter is that improved health and adequate nutrition lead to increased productivity; decreased disability and illness reduce production losses by creating a more robust labor pool; and healthy children are better prepared for learning, education, and economic advancement [9]. In fact, an increase in life expectancy of a population from 50 to 70 years is estimated to raise the rate of GDP growth by 1.4% per year, while undernutrition is known to reduce global economic output anywhere from 0.23% to 4.7% [10, 11]. Improvements in social services (such as access to healthcare) also address income inequality, as the impact of social services is usually distributed evenly across the community, benefiting everyone.
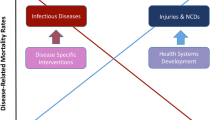
In the late 1980s, the World Bank began to focus more closely on health care in LMICs. As part of this effort, they reviewed their disease control priorities and began using cost-effective analysis to inform decision making on how to distribute the limited resources available for health care in LMICs. This process resulted in the 1993 publication of the first edition of Disease Control Priorities in Developing Countries (DCP1) [12]. In the same year, the World Bank examined the case for investing in health in their 16th Annual World Development Report (WDR) [13]. WDRs are the World Bank’s chief mechanism for evaluating the evidence on a specific topic and for developing and sharing its policy messages with countries, development agencies, and the academic community; and are one of the world’s most widely distributed economic publications. The WDR 1993: Investing in Health [13] showed finance ministers that well-chosen health expenditures were not an economic drain but an investment in economic prosperity and individual wellbeing. It argued that allocation of resources toward cost-effective interventions for high-burden diseases offered a rapid and inexpensive pathway to improvements. The WDR 1993 used the findings of DCP1 and was based on the first global and regional estimates of numbers of deaths by age, sex, and cause and of the burden (including the disability burden) from more than 100 specific diseases and conditions.
On the 20th anniversary of the WDR1993, a Lancet Commission revisited the case for investment in health and proposed a new investment strategy to achieve dramatic health gains by 2035 [14]. The key findings of the Commission report, as stated in executive summary, are shown in Panel 3.1.
Panel 3.1 The Key Findings of the Lancet Commission on Investing in Health [14]
-
There is an enormous payoff from investing in health. The returns on investing in health are impressive. Reductions in mortality account for about 11% of recent economic growth in low- and middle-income countries (LMICs), as measured in their national income accounts. However, although these accounts capture the benefits that result from improved economic productivity, they fail to capture the value of better health in and of itself. Between 2000 and 2011, about 24% of the growth in full income in LMICs resulted from the value of additional life-years (VLYs) gained. This more comprehensive understanding of the economic value of health improvements provides a strong rationale for improved resource allocation across sectors.
-
A “grand convergence” in health is achievable within our lifetimes. A unique characteristic of our generation is that collectively we have the financial and the ever-improving technical capacity to reduce infectious, child, and maternal mortality rates to low levels universally by 2035, to achieve a “grand convergence” in health. With enhanced investments to scale up health technologies and systems, these rates in most LMICs would fall to those presently seen in the best-performing middle-income countries. Achievement of convergence would prevent about ten million deaths in 2035 across LMICs relative to a scenario of stagnant investments and no improvements in technology. With use of VLYs to estimate the economic benefits, over the period 2015–2035 these benefits would exceed costs by a factor of about 9–20, making the investment highly attractive.
-
Fiscal policies are a powerful and underused lever for curbing of noncommunicable diseases and injuries. The burden of deaths from noncommunicable diseases (NCDs) and injuries in low- and middle-income countries can be reduced by 2035 through inexpensive population-based and clinical interventions. Fiscal policies are an especially promising lever for reducing this burden (see last section of the chapter for further details).
-
Progressive universalism, a pathway to universal health coverage (UHC), is an efficient way to achieve health and financial protection. The Commission endorsed two pro-poor pathways to achieving UHC within a generation. In the first, publicly financed insurance would cover essential health-care interventions to achieve convergence and tackle noncommunicable diseases and injuries. This pathway would directly benefit the poor because they are disproportionately affected by these problems. The second pathway provides a larger benefits package, funded through a range of financing mechanisms, with poor people exempted from payments.
The significance of the Lancet Commission on Investing in Health is that it represents a culmination of economic thinking on global health development over the past 30 years. Moreover, it delineates a pathway through which dramatic health gains can be achieved by 2035.
The Economic Case for Surgical Care in LMICs
The Essentials
-
Surgical conditions comprise a large proportion of the global burden of disease
-
The Disease Control Priorities (DCP)-2 and DCP-3 unequivocally demonstrate the cost-effectiveness of surgical care at the first-level hospital
-
The Lancet Commission on Global Surgery showed significant economic losses due to the burden of surgical conditions
Although surgery is only briefly mentioned in DCP1 and WDR 1993, both are incredibly important from a surgical perspective, as nearly every important economic theme in global surgery (e.g., cost-effective analysis) evolved from these works. Why surgical care was not better represented in this initial work is an important question, but probably best explained by the minimal data demonstrating surgical conditions as an important public health problem at the time. Further, it was not until almost a decade later that the comparative cost-effective analysis methods were applied to surgical care. In a seminal study from Bangladesh in 2003, McCord and Chowdhury reported that the cost of emergency obstetric care at a rural hospital in Bangladesh was US $11 per disability adjusted life-year (DALY) averted [15]. This finding surprised many in the public health field at the time, as these costs compared favorably with many other primary health care interventions, such as vitamin A distribution (US $9 per DALY averted), acute lower respiratory infection detection and home treatment (US $20 per DALY averted), or measles immunization (US $30 per DALY averted) [16, 17]. The concept of the DALY is shown in Fig. 3.1, with important economic principles in global surgery described in Panel 3.2. The cost of selected surgical interventions and how they compare to other global health preventions and treatment are shown in Fig. 3.2.
Panel 3.2 Important Concepts in the Economics of Surgical Care in LMICs [29–31]
How Is Cost-Effectiveness Calculated?
Several metrics can be used to measure cost-effectiveness of surgical interventions. Three of the most popular are:
-
Cost per DALY averted (DALY = YLL + YLD)
-
Cost per life year saved (LYS)
-
Cost per quality associated life year (QALY)* gained
*The QALY is a measure of the quality and quantity of a life lived. In some ways, it is simply the inverse measure of the DALY, but there are many important nuances [29].
What Is Considered “Cost-Effective”?
It depends on the country from whose perspective cost-effectiveness is calculated. According to the World Health Organization’s Commission on Macroeconomics and Health [9], an intervention that costs less than triple a country’s per capita GDP, it is considered “cost effective,” whereas if it costs less than the country’s per capita GDP, it is considered “very cost effective.” Unfortunately, cost effectiveness data is still scarce in most of the low-resource world.
What Is Benefit Cost Analysis (BCA)?
BCA attempts to estimate the net economic benefit of an intervention in monetary terms. It thereby allows researchers to investigate the potential economic return on an investment. It allows governments to compare investments in health as opposed to other sectors (transportation, education, etc.).
How Does BCA’s Estimate of Economic Benefit Extend Beyond GDP and DALYs?
The BCA approach assumes that GDP per capita does not fully capture a country’s economic welfare, and hence develops a methodology to value additional life years in economic terms [30]. It employs the value of statistical life (VSL) concept (e.g. if an individual would be willing to pay US$7 to decrease the risk of mortality by one in one million, then this individual’s VSL would be US$7,000,000) [31]. The economic benefit, then, is calculated as the DALYs averted * value of statistical life-year (VSLY).
Fortunately, the lack of attention to surgical conditions in DCP1 would begin to be remedied in the Disease Control Priorities, Second edition (DCP2) with a chapter focusing on surgical care [18]. The DCP2 chapter, perhaps best known for its estimate that 11% of the global burden of disease was treatable by surgical care, demonstrated that surgical treatment provided in low-tech community hospitals is cost-effective. DCP2 was also a step forward in several other respects. While DCP1 focused on clusters of the diseases, DCP2 drew together implementation responses to groups of conditions—for example, schools, health systems, and integrated management of childhood diseases. DCP2 also included discussions on research priorities and product development opportunities.
The marked success of the surgical chapter in DCP2 led to an entire volume being devoted to surgical care in the third edition of the Disease Control Priorities (DCP3). The DCP3 project, which is ongoing, involves the World Bank, the World Health Organization (WHO), the Gates Foundation, and several other notable groups. Released in February 2015, the Essential Surgical volume of DCP3 is the most comprehensive effort to date to evaluate the cost-effectiveness and population-wide effect of surgical care [19]. The important findings of the Essential Surgical volume of DCP3 are shown in Panel 3.3.
Panel 3.3 Important Findings of the Essential Surgical Volume of DCP3 [19]
-
Provision of essential surgical procedures would avert about 1.5 million deaths a year, or 6–7% of all avertable deaths in low-income and middle-income countries.
-
The avertable burden from scaling up basic surgical care at first-level hospitals and advanced care in specialized clinics in LMICs (116.1 million DALYs per year) exceeds the unaddressed global burdens of HIV/AIDS (81.6 million DALYs), tuberculosis (49.4 million DALYs), or malaria (82.7 million DALYs).
-
Essential surgical procedures rank among the most cost-effective of all health interventions. These procedures are all very cost-effective, with most costing $10–$100 per disability-adjusted life year (DALY) averted. This puts cost-effectiveness of surgical care in the same range as accepted and extremely cost-effective public-health interventions such as immunizations and bed nets for prevention of malaria.
-
Measures to expand access to surgery, such as task sharing, have been shown to be safe and effective while countries make long-term investments in building surgical and anesthesia workforces.
-
Substantial disparities remain in the safety of surgical care, driven by high perioperative mortality rates including anesthesia-related deaths in LMICs.
-
The large burden of surgical disorders, cost-effectiveness of essential surgery, and strong public demand for surgical services suggest that universal coverage of essential surgery should be financed early on the path to universal health coverage.
Several months after the release of the Essential Surgical Volume of DCP3 the Lancet Commission on Global Surgery published their findings [20]. Close collaboration between the two groups ensured that research efforts would not be duplicated. The Lancet Commission on Global Surgery brought together an international, multidisciplinary team of 25 commissioners, supported by more than 500 advisors, collaborators, and contributors from 110 countries and 6 continents. The Commission focused on solutions within domains of health-care delivery and management; workforce, training, and education; economics and finance; and information management. The Commission had five key messages, a set of indicators and recommendations to improve access to safe, affordable surgical and anesthesia care in LMICs, and a template for a national surgical plan. The key messages from the Commission report are shown in Panel 3.4. Considered together, the Essential Surgery volume of DCP3 and Lancet Commission on Global Surgery provide a strong economic argument for including emergency and essential surgical care as part of health care systems in LMICs.
Panel 3.4 Key Messages from The Lancet Commission on Global Surgery [20]
-
Five billion people do not have access to safe, affordable surgical, and anesthesia care when needed. Access is worst in low-income and lower-middle income countries, where nine of ten people cannot access basic surgical care.
-
One-hundred forty-three million additional surgical procedures are needed in LMICs each year to save lives and prevent disability. Of the 313 million procedures undertaken worldwide each year, only 6% occur in the poorest countries, where over a third of the world’s population lives. Low operative volumes are associated with high case-fatality rates from common, treatable surgical conditions. Unmet need is greatest in eastern, western, and central sub-Saharan Africa, and South Asia.
-
Thirty-three million individuals have catastrophic health expenditure due to payment for surgery and anesthesia care each year. An additional 48 million cases of catastrophic expenditure are attributable to the nonmedical costs of accessing surgical care. A quarter of people who have a surgical procedure will have financial catastrophe as a result of seeking care. The burden of catastrophic expenditure for surgery is highest in low-income and lower-middle-income countries and, within any country, lands most heavily on poor people.
-
Investing in surgical services in LMICs is affordable, saves lives, and promotes economic growth. To meet present and projected population demands, urgent investment in human and physical resources for surgical and anesthesia care is needed. If LMICs were to scale-up surgical services at rates achieved by the present best-performing LMICs, two-thirds of countries would be able to reach a minimum operative volume of 5,000 surgical procedures per 100,000 population by 2030. Without urgent and accelerated investment in surgical scale-up, LMICs will continue to have losses in economic productivity, estimated cumulatively at US $12.3 trillion (2010 US$, purchasing power parity) between 2015 and 2030. Globally, this will amount to $21 trillion in losses of economic productivity, and up to 2% of GDP in some of the world’s poorest economies (Fig. 3.3).
-
Surgery is an “indivisible, indispensable part of health care”. Surgical and anesthesia care should be an integral component of a national health system in countries at all levels of development. Surgical services are a prerequisite for the full attainment of local and global health goals in areas as diverse as cancer, injury, cardiovascular disease, infection, and reproductive, maternal, neonatal, and child health. Universal health coverage and the health aspirations set out in the post-2015 Sustainable Development Goals will be impossible to achieve without ensuring that surgical and anesthesia care is available, accessible, safe, timely, and affordable.
Financing Surgical Care in the Era of the Sustainable Development Goals (SDG)
The Essentials
-
Achieving the SDGs will require universal access to surgical and anesthesia care
-
Economic losses in LMICs from burden of surgical conditions will amount to $12.3 trillion through 2030
-
The estimated cost of scaling up surgical care in LMICs is between $300 and 500 billion
-
A combination of international and national-level funding sources will be required to finance the surgical scale-up
The SDGs, which have an end target date of 2030, have the potential to further catalyze the progress that has been made in global health. In contrast to the Millennium Development Goals (MDGs) which had eight specific targets to address extreme poverty—with several relating directly to health, the new agenda has one overarching health goal—SDG3 ensure healthy lives and promote wellbeing for all at all ages. As noted by Abdullah and Henry [21], surgery best fits under target 3.8: achieve universal health coverage, including financial risk protection, access to quality essential health care services and access to safe, effective, quality, and affordable essential medicines and vaccines for all. Surgical care also has a role in ending poverty (SDG 1) and achieving gender equality through access to essential reproductive health services (SDG 5). The consideration here is that surgical care, especially its role in strengthening health systems aligns well with the SDGs. Further, synergism exists between the SDGs and World Health Assembly Amendment 68.15 “Strengthening emergency and essential surgical care and anesthesia as a component of Universal Health Coverage” [22].
The most important question facing global surgery is how to finance the surgical scale in LMICs that is so badly needed. Keeping in mind that little effort has been made to develop surgical care in LMICs, and this neglect has resulted in massive deficits in workforce and infrastructure, the amount of money to bring surgical care up to even minimal levels will be massive. One of the many important contributions of The Lancet Commission on Global Surgery was their estimate on the projected cost to reach minimal surgical standards by 2030. These estimate range from $300 to $550 billion through 2030 or $16 to $31 billion annually [23]. A middle-of-the-road approach, using rates of scale-up seen during Mongolia’s recent health system expansion (increase in surgical volume by 8.9% per year), would cost $420 billion through 2030, or $23 billion per year. The variability in the estimates comes from different choices for the unit cost of surgical procedures, infrastructure construction costs, and the proposed rate of scale-up of surgical services. An important caveat to the Lancet Commission estimate is that it does not include training costs for the global surgical workforce.
In addition to scale-up costs, affordability of surgical care must be considered as a part of its financing. The reason for this is that scaling up of surgical access without concurrent increases in financial risk protection could cause inadvertent harm. Currently, out-of-pocket user-fees constitute the bulk of financing mechanism for surgical care in much of the low-resource world. Again, of the relative few who are able to access surgery, over 81 million people experience financial catastrophe after payment for surgical care [24]. If the world had complete access to surgical care, an estimated 3.9 billion—over half of the global population—would be at risk for catastrophic expenditure. Financing of surgical care must be done in concurrence with global goals toward universal health coverage. As noted earlier in the chapter, while the cost of scaling up surgical care at first glance may seem prohibitive, the cost of inaction is even higher—an estimated $21 trillion in losses of economic productivity by 2030, representing 2% of GCP in some of world’s poorest economies (Fig. 3.3).
Short of developing a global surgery fund to address the cost of the surgical scale-up—which seems unlikely given the current global economy—the Lancet Commission on Investing in Health, the Lancet Commission on Global Surgery, and the Disease Control Priorities outline several options:
-
Obtain funding through existing development assistance for health (DAH) programs . DAH has been defined as “financial and in-kind contributions made by channels of development assistance—that is, by institutions whose primary purpose is providing development assistance to improve health in developing countries” [25]. In 2013, donors disbursed a total of $31.3 billion to improve health in LMICs, more than five times the amount that was disbursed in 1990 [26]. Much of this was distributed amongst select, specific health goals—with the majority going to infectious diseases and the remainder to maternal and child health. To our knowledge, DAH has thus far not been applied directly to surgery. Regardless, given that the cost of surgical scale-up alone would be $23 billion/year and that total DAH funding currently totals $31.3 billion for all health causes combined, it would be insufficient for long-term scale-up of surgical care.
-
Increase governmental spending on surgical care. Typically, governments spend 20 times more of their own resources on health than they receive in assistance. This is extremely important as the distribution of the majority of health-care dollars within a country is set by local priorities. In many ways, this is good news, as economies across the world are growing and such growth translates into a potential for greater tax-revenue and increased availability of resources for government spending on health. Projecting mid-range economic growth of about 4% per year, LIC economies will approach $1 trillion and lower middle income economies will approach $8.7 trillion by 2035 [26]. As such, annual costs of scale-up would represent less than 10% of new economic growth amongst the world’s low- and lower-middle-income economies in 2035. Nevertheless, many of the poorest countries simply do not have enough resources for meaningful investment in surgical care.
-
Develop new revenue streams for funding surgical care. One of the key reasons the MDGs were so successful was that it created new financing mechanisms such as the Global Fund to Fight AIDS, Tuberculosis and Malaria and Gavi, the Vaccine Alliance, allowing remarkable progress on critical health challenges [8]. Similarly, new financing strategies will be necessary for surgery. One such strategy is to broaden the tax base with health-promoting taxation, such as a tax on tobacco and alcohol consumption [14, 27]. In addition to compelling evidence that taxes on these industries can change usage behavior and shift the burden of noncommunicable diseases over the coming decades, taxation of these industries could be a significant source of revenue. A tobacco tax in India alone could generate as much as $2 billion annually [28]. Improved intersector allocation of domestic resources can be another source of funds for scale-up of health systems. Global energy subsidies, for example, amount to over $2 trillion annually on a post-tax basis. In sub-Saharan Africa, energy subsidies amount to over 3.5% of GDP—well exceeding the proportion allocated to entire health budget in many countries in Africa and beyond [14].
Aligning surgical care with the larger global health agenda, especially as it relates to health system strengthening, will be an important strategy for the scale up of surgical care in LMICs. Given the amount of resources required, and the economic state of some of the poorest countries, a broad-based approach combining domestic government financing with external DAH support will be necessary, at least in the early stages.
Finally, a great deal of effort has been directed toward making a moral case for improving surgical care in LMICs. This argument, based on health equity and social justice principles, is straightforward, obvious, and compelling. For those still unconvinced, there is now strong economic argument for improving surgical care in settings of limited resources. Emergency and essential surgical is highly cost-effective and can yield a high return on investment. Perhaps, most important is that inadequate surgical care can exact a devastating toll on economic growth of LMICs. Policymakers worldwide should take notice.
References
Shrime MG, Bickler SW, Alkire BC, Mock C. Global burden of surgical disease: an estimation from the provider perspective. Lancet Glob Health. 2015;3:S8.
Alkire BC, Raykar NP, Shrime MG, Weiser TG, Bickler SW, Rose JA, et al. Global access to surgical care: a modelling study. Lancet Glob Health. 2015;3:e316–23.
Contreras R. Competing theories of economic development. Transl Law Contemp Probl. 1999;9:93–108.
Truman Inaugural Address, January 20, 1949. https://www.trumanlibrary.org/whistlestop/50yr_archive/inagural20jan1949.htm.
Kapur D, Lewis J, Webb R. The world bank: its first half century. Washington, DC: Brookings Institution Press; 1997.
History of WHO (n.d.). http://www.who.int/about/history/en/.
Global Monitoring Report 2015/2016: development goals in an era of demographic change: global monitoring report. http://www.worldbank.org/en/publication/global-monitoring-report.
The Millennium Development Goals Report. 2015. http://www.undp.org/content/dam/undp/library/MDG/english/UNDP_MDG_Report_2015.pdf.
Macroeconomics and health: investing in health for economic development: report of the Commission on Macroeconomics and Health (n.d.). http://www1.worldbank.org/publicsector/pe/PEAMMarch2005/CMHReport.pdf.
Barro RJ. Determinants of economic growth: a cross-country empirical study. National Bureau of Economic Research; 1996. http://unpan1.un.org/intradoc/groups/public/documents/apcity/unpan027110.pdf.
Arcand J-L. Undernourishment and economic growth: the efficiency cost of hunger. Food & Agriculture Org; 2001. http://www.fao.org/docrep/003/x9280e/x9280e00.htm.
Disease Control Priorities in Developing Countries. New York: Oxford University Press; 1993. http://www.who.int/surgery/challenges/disease-control-priorities.pdf.
World Development Report. 1993. https://openknowledge.worldbank.org/handle/10986/5976.
Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, et al. Global health 2035: a world converging within a generation. Lancet. 2013;382:1898–955.
McCord C, Chowdhury Q. A cost effective small hospital in Bangladesh: what it can mean for emergency obstetric care. Int J Gynecol Obstet. 2003;81:83–92.
Ozgediz D, Riviello R. The “other” neglected diseases in global public health: surgical conditions in sub-Saharan Africa. PLoS Med. 2008;5(6):e21.
Grimes CE, Henry JA, Maraka J, Mkandawire NC, Cotton M. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014;38:252–63.
Debas HT, McCord C, Thind A, Gosselin R. Surgery. In: DT J, editor. Dis. control priorities dev. ctries. 2nd ed. New York: The World Bank and Oxford University Press; 2006.
Mock CN, Donkor P, Gawande A, Jamison DT, Kruk ME, Debas HT. Essential surgery: key messages from disease control priorities, 3rd ed. Lancet. 2015;385:2209–19.
Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624.
Henry JA, Abdullah F. Global Surgical care in the UN post-2015 sustainable development agenda. World J Surg 2015. doi:10.1007/s00268-015-3249-4.
World Health Assembly 68.15. Strengthening emergency and essential surgical services as a component of universal health coverage. Geneva: WHO; 2015. http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_31-en.pdf.
Verguet S, Alkire BC, Bickler SW, Lauer JA, Uribe-Leitz T, Molina G, et al. Timing and cost of scaling up surgical services in low-income and middle-income countries from 2012 to 2030: a modelling study. Lancet Glob Health 2015;3:S28–37.
Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modeling study. Lancet Glob Health.2015;3(S2):S38–44.
Schieber GJ, Gottret P, Fleisher LK, Leive AA. Financing global health: mission unaccomplished. Health Aff. 2007;26:921–34.
IHME. Financing global health 2013: transition in age of Austerity. Seattle: 2014. http://www.healthdata.org/policy-report/financing-global-health-2013-transition-age-austerity.
Verguet S, Gauvreau CL, Mishra S, MacLennan M, Murphy SM, Brouwer ED, et al. The consequences of tobacco tax on household health and finances in rich and poor smokers in China: an extended cost-effectiveness analysis. Lancet Glob Health 2015;3:e206–16.
Jha P, Joseph R, Li D, et al. Tobacco taxes: a win-win measure for fiscal space and health. Mandaluyong City: Asian Development Bank; 2012.
Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Health. 2009;12:S5–9.
Alkire B, Vincent J, Meara J. Benefit-cost analysis for selected surgical interventions in low- and middle-income countries. In: Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN, editors. Essential surgery: disease control priorities, vol 1, 3rd ed. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2015. Chapter 21.
Andersson H, Treich, N. Chapter 17: The value of statistical life. In: Lindsey, R, Quinet, E, Vickerman, R, editors. A Handb Transp Econ. Edward Elgar Publishing Limited. Cheltenham, UK; 2011; p. 396–424.
Disability-adjusted life year (n.d.). Wikipedia. https://en.wikipedia.org/wiki/Disability-adjusted_life_year#/media/File:DALY_disability_affected_life_year_infographic.svg. Creative commons license: CC BY-SA 3.0.
Chao TE, Sharma K, Mandigo M, Hagander L, Resch SC, Weiser TG, et al. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health. 2014;2:e334–45.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Raykar, N.P. et al. (2017). The Economic Case for Surgical Care in Low-Resource Settings. In: Park, A., Price, R. (eds) Global Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-49482-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-49482-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-49480-7
Online ISBN: 978-3-319-49482-1
eBook Packages: MedicineMedicine (R0)