Abstract
Global surgery is increasingly gaining recognition as an important and essential component of the service mix needed to attain Universal Health Coverage. Lack of access to surgical care is not just tragic, it is also too costly for any society, currently and when costs are projected into the future. Research has demonstrated that cost effectiveness of surgical care is comparable to that one of well-known (and well-funded) public health interventions, raising the public pressure for access expansion to affordable surgical care. However, how to finance it remains a significant challenge. The prevailing paradigm that governments could not offer everything to everyone builds its foundation on the wrong mindset; a mindset that invites delaying the expansion of surgical care. It is true that resources can appear finite at a given time, but this equation does not include the potential for innovation, cooperation and decision that can stem from a serious challenge. The world is today, richer, healthier, with greater human capital, and for that, more capable technologically to finally bring surgery to those in need. The response to this call is already coming from multiple corners: groups of likeminded surgeons and health professionals, governments (from high-income countries as well as LMICs), international agencies, philanthropists, corporations and academic centers. Lessons learned from LMICs and from previous experiences in development assistance, realignment of countries priorities and private financial assistance provide tangible examples about how expanding surgical care to many in low resource settings can be done.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Access to surgery
- Development assistance
- Financial sustainability
- Global surgery
- Service delivery
- Universal health coverage
1 Health as a Right and the Movement Towards Universal Health Coverage
Surgery accounts for approximately 30% of the burden of disease; concomitantly, surgical expenses risk pushing approximately 44% of the world’s population into catastrophic expenditures [1]. Healthcare services financing is closely related to the societal agreements reflected in countries laws; these also indicate what societies are willing to pay for and who should be covered. Comprehensive social protection that includes surgical care results more from a rather lengthy social and legal process than from a single act.
The World Health Organization (WHO) defines universal health coverage (UHC) as “access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost” [2]; in other words it is a system that delivers the care people need, when they need it, without falling into financial destitution [3]. UHC has acted as a common term that brings together different concepts, from the Alma-Ata declaration to Health for All. UHC is, according to the 2010 World Health Report, an objective and a strategy to guide health sector reforms for its members [4]. Having this common denominator is important for understanding financing needs, subjects, sources and resources’ channels.
We might believe that acknowledging health as a right, or signing declarations about commitments to universal care, would automatically result in the increase in service delivery output and in the concomitant improvement of the social condition of millions, particularly those who lack services they desperately need. In multiple conversations, participants in one way or another conflate Universal Health Coverage with the right to health. While the relationship between acknowledging health as a right, and creating the legal and regulatory framework that can result in UHC exists; this relationship is by no means linear and causality is in many instances hard to define.
In some instances, the appearance of a proto-UHC concept, like the memorable “Kaiserliche Botschaft”, or the 1881 Imperial Message from Whilehm I, which marked the origin of the modern welfare stateFootnote 1—and the “Bismarck Model”-, offered very basic coverage to a small portion of the population. It took Germany 105 years to offer truly “Universal” healthcare [5]. It is important to note that a specific right to health is not in the German Federal Constitution (although it is enshrined in the constitutions of several BundesländerFootnote 2 [6]). In contrast, Chile the first country to acknowledge health as a right in its constitution in 1925 [7], presents a different—almost opposite- case; as the first institutions devised to provide care in the Latin-American country were established in the 1940’s, reaching universal coverage in the late 80’s after multiple reforms [8]. In fact, less than 40% of national constitutions addressed health rights before 1970; the world would have to wait for almost 30 years until the vast majority (over 90%) of the countries legally acknowledged—from partially to comprehensive- health as a right [9]. Even when countries did not consider health as right, public institutions offered healthcare services; an example is Colombia, a country that had social contracts and institutions that offered a broad array of healthcare services to selected populations (i.e. public sector workers) decades before health became a right in the constitutional reform of 1991 [10]. In this country the heated discussion about the reach and scope of the new law, in terms of coverage and access, ended up with a form of social agreement summarized in the slogan TOTOYA (Todo, para todos, ya! Or Everything, for everyone, now!) [11]. This acknowledgement empowered Colombians to sue the Government when it did not meet their economic or civil rights. A report by the Human Rights Ombudsman’s Office, estimated that 674,612 legal actions of this kind took place between 1999 and 2008 [12]. Litigations in this country includes demands for a wide array of procedures that go from drug therapies to surgeries, creating an important pressure on the public finances.
Important as it is to establish the necessary legal substrata for adequate healthcare financing; examples show that, historically, countries that have attained universal health coverage seem to follow a pattern in which they initially have pervasive internal pressures for the universal provision of care; then, society demands deep involvement from the government, although roles vary from country to country. Finally, the road to UHC is never straight, shaped by multiple negotiations instead of design, and achieving universal coverage takes time.Footnote 3 Understanding this, the 58th World Health Assembly (WHA) in 2005 called to its members to plan for the transition to UHC, including financing and social health insurance plans, aiming to attain universal coverage. Ten years later, the 68th WHA set 2030 as a concrete deadline for its members to achieve UHC, stressing on different elements such as financial protection, access to affordable quality services and medicines for all. In summary, UHC now embodies the right to health and offers a roadmap for universal healthcare that, in theory, includes surgical care in the template;Footnote 4 but more work must be done to ensure affordable surgery and anesthesia are considered as they are: Essential for quality and equitable care.
2 Scarce Resources, Delivery Failure and the Global Cost of Lack of Access to Surgery
Over the last 50 years, important progress has been made in advancing surgical care globally. Development cooperation programs have helped expand access to surgery in low resource settings, contributing to the social and economic progress of entire regions. In spite of the progress made, important challenges remain. The Lancet Commission on Global Surgery estimates that, just because of OR existing infrastructure, more than 2 billion people do not receive surgical care [13], and approximately 5 billion people lack access to timely safe and affordable surgery [14]. Large demand of services for a scanty supply is a compounding negative factor that makes surgery in poor areas, prohibitively expensive, inviting heavy—but not always effective- regulation or simply inaction from an overwhelmed society.
The cost of not having surgery: Societal and opportunity costs and losses. The need is particularly acute in the poorest regions. More than nine persons out of ten in Sub-Saharan Africa do not have access to timely and affordable surgical services when needed. The immense cost inadequate surgical care places on, particularly, poor societies is twofold: moral and economic. The moral cost of early, avoidable death or decreased quality of life is unfathomable; the economic cost of productivity loss due to early death and disability can be calculated, but still does not capture other opportunity costs such as increased investment due to aggregated income. Even more, this approach does not address the fact that poor surgical infrastructure and lack of access to surgical care, also pushes those with means to seek for expensive care abroad [15]—which amounted to more than $ 3 billion in revenues for US hospitals in 2013 [16], further contributing with a vicious circle of lack of investment and poverty.
Seeing surgical care (and healthcare in general) just as a cost, creates a singularity that diminishes its true economic contribution. On one side, it is an economic activity that generates revenues, salaries, investments in infrastructure and technology, all of which have a compounding factor in the rest of the economy (the entertainment industry offers a contrasting vision: we do not consider it as a societal cost). On the other side, it helps individuals to continue with—and prolong- their own contributions to the economy through labor and knowledge. In essence, access to surgical care is essential for poor regions of the world to improve their human capital, and to help to their economic development and poverty reduction.
As an example, in 2015, WHO estimated that in SSA, 47% of all productivity losses, approximately $1.4 trillion, were due to Non-Communicable Diseases (NCDs) and injuries, which in many instances are treated with surgery [17]. Contrast this figure with the $3,178 trillion spent in healthcare in the US in that year [18], or to the $1.7 trillion of the global cost of healthcare in 1990 [19]. It means that productivity losses in the African continent were equivalent to 44% of all healthcare expenditures in the US—arguably the “most expensive healthcare system”- and equivalent to almost 8% of the total American economic output of that year.
Lack of action in developing strong surgical infrastructure (human and material), has a compounded cost effect. According to the Lancet Commission on Global Surgery, by 2030 the potential loss related to lack of surgery in LMIC’s could ascend to $12.3 trillion or a full 2% of GDP growth.Footnote 5 The World Bank estimated the total size of the Chinese economy output in 2019 at $ 14.34 trillion [20].
Another perspective that also provides a sense of economic magnitude of the problem is the future cost of not providing surgery when needed. In 2010, road-traffic injuries generated 75·5 million disability adjusted life-years (DALYs), approximately 20 million DALYs more than 1990. Investment in surgical care and infrastructure has probably been negatively impacted by the perception of surgery as an expensive intervention. In fact, surgery compares favorably with well-known public health interventions in terms of cost-effectiveness. For instance, male circumcision in Africa at $ 13.78 per DALY is lower than antiretroviral treatment with a range from $453.74 to 648.20 per DALY. Other examples are in the table below [21].
Procedure | Cost per Daly Adverted |
|---|---|
Circumcision | $13.87 |
HIV ART | $453.74–$648.20 |
Cataract repair (Nepal) | $7.29 |
Inguinal hernia repair (Ghana) | $12.88 |
Expanded Program on Immunization | $12.96–$25.93 |
General surgery | $82.32 |
Ophthalmic surgery | $136 |
BCG Vaccine | $51.86–220.39 |
It could be argued that, amongst its many contributions to the discussion around access to affordable surgical care globally, the work that the Lancet Commission has done to increase awareness of the cost effectiveness of surgery, and placing it in the realm of desirable public health intervention, is simply remarkable.
Market failure in surgical services provision, the role of the government and the need for innovative financing. Competitive free markets are considered an efficient vehicle to make demand meet supply at an optimal price point. However, markets might fail when there is no balance between what suppliers might offer and what informed consumers would demand. As health services demand is mostly constructed around needs, poverty is a factor that makes difficult for that theoretical equilibrium to happen.Footnote 6 Market failures can be addressed through judicious and discipline government interventions, and the specter of individuals’ catastrophic expenditures associated to health services delivery, particularly surgical care, makes the possibility and clamor for such an intervention increasingly possible.
Around the world close to 33 million cases of catastrophic surgical expenditures take place every year, and approximately 3.8 million persons are continuously in risk, should they need sudden surgical care. They are close to 22% of all individuals (approximately 150 million) who face catastrophic expenditures every year. Catastrophic expenses affect particularly the poor of the world. While this is true in all levels of economic development, it is more evident in SSA, South and South East Asia. It is important to note that almost all catastrophic health care expenses in the upper and high middle-income countries fall on the poor [22]. Findings show that individuals in lower-middle income countries tend to face more catastrophic expenditures than those in low-income countries as surgery, because as a function of income, costs are up to 15% higher in the former than the later. In the economic transition from low to lower-middle income, surgery costs can grow faster than household incomes, and for that reason, policy makers in countries making this positive economic transition, must anticipate this situation.
When considering third party financing for surgery, it is important to note that in addition to surgical direct costs, non-medical costs such as lodging, food and transportation, contribute substantially to catastrophic expenditures. When these are taken into consideration, models predict that an additional 48.5 million cases of catastrophic expenditures occur, resulting in roughly 81 million annual cases globally [23].
Scarcity in Human Resources for Health and infrastructure results in care rationing. For the last twenty years, world health leaders have paid special attention to the pressing issue of human resources in health. In 2006, it was evident that in spite of the initial attention to the subject, worrying trends about health professional workers density just continued. At that time, reports showed that 57 countries had less than 2.3 workers per 1,000 population, out of which 36 were in SSA, 6 in South East Asia and 5 in the Americas; not a single country from Europe fell under this critical threshold. In 2013, the situation has not improved much; following the same classification, 31 out of 54 countries were in Africa, and 7 in South East Asia. The health workers shortage in 2006 was estimated at 4.3 million; by 2013, the gap had grown to 7.2 million. If this trend continuous, by 2035 we will need 12.9 million health workers more. The shortage, if conditions do not change, will likely be more acute in Africa [24].
This structural shortage is explained by the lack of formal training, particularly in Sub-Saharan Africa. In the region there are 11 countries with no medical school and 24 with just one. The continent graduates roughly 10,000 doctors a year, joining a pool of 145,000; similar in size to that one of UK; which has a population that is just a fraction-equivalent to less than 7%.Footnote 7 A compounding factor is the shortage of HRH in high-income countries—particularly nurses and physicians-, where a mix of misallocation or resources [25], changes in labor laws for trainees and stagnant number of training centers [26] have stimulated the importation of foreign providers, mainly from Africa and South East Asia. For East Africa to reach the same providers density as Canada, would have to train 42,000 more doctors.Footnote 8 Also, almost totally absent is the training of healthcare administrators and hospital managers, who can contribute to the overall systemic improvement [27].
Service delivery infrastructure poses an additional challenge. Extremely low density of bedsFootnote 9; need for reliable access to energy, water, and to an adequate supply of oxygen, make providing care difficult. For that reason, 24-hour provision of services is limited to less than 50% of the operational structure in some SSA countries and basic infrastructure is lacking [28].
Elements described make for a perfect storm in healthcare supply, particularly surgery as, different from primary care, requires a dedicated infrastructure and a team of professionals and managers that are not always available. In classic economy, demand for scarce goods results in higher prices and in a supply at a much lower level than society would be willing to get. While prices of surgical services in low resource settings might be lower than those in high-income regions, the truth is that, even at that low level, most people cannot afford them or simply there is not enough for everybody. Clearly, thinking creatively is of the essence to solve this tragic conundrum.
3 How Is Health and Surgical Care Paid?
Sources of healthcare payment can be divided into private and public; and into individual, pooling or government transfers. Government transfers are usually resources financed through taxation and other government revenues (i.e. mining rights and royalties, public enterprises, etc.). Pooling happens through social or voluntary health insurance. Private insurance plays an important role in high-income countries to fund services, including surgeries, not covered by public plans or other private insurance. These plans can be primary, which are the main source of insurance in the US and Chile (and roughly 10% of the German population), supplementary (85% of the Dutch population) and complementary (95% of the French population) [29].
Individual direct payments to the care provider are referred as out-of-pocket payments. They can cover the price of services and products received, or they can be part of the insurance (pooling) arrangement. If the later, they can be co-payment, or the amount paid for every service received (a fix amount or a proportion of the service cost); and/or a deductible, which is usually an amount the insurance holder must pay (in one or multiple services) before reaching a certain threshold, in which the insurance starts providing coverage.
A different, but important form of global health financing is Development Cooperation (also known as Official Development Assistance or ODA), that involves foreign governments (through multilateral or bilateral programs) and private foundations. While not focused in surgery, they have played an important role in advancing the global fight against infectious diseases.
In general when looking at a low-income country national health accounts, it is quite difficult to establish with clarity the cost of specific interventions, like surgery. In many instances, these are aggregated to track a disease, like TB, or a program, like maternal health (which also includes surgery) [30]. This makes difficult to understand contribution, impact and service delivery capacity, and ultimately, how resources are allocated. However, general trends in payment or service delivery can offer an idea about how surgery is probably paid for in different settings.
In low-income countries, funding pools (government allocations and public and private insurance) finance only 38% of healthcare; a stark contrast with 60% in middle-income countries and 80% in high-income countries. It is also a core belief that the poorest of the poor need total subsidization and that low-income groups need, at least, some levels of subvention [31]. As pooling is an important source for surgical care (because of risk and cost), governments can either encourage citizens to enroll in national health insurance schemes, pay for services through direct budgetary allocations or through private contributions to regulated private insurance schemes. These solutions might work relatively well in middle- and higher middle-income countries, but due to a small taxation base it is difficult to do it in low- and lower-income countries. However, there is a fundamental problem with the contributive base of low-income countries: governments do not have a wide taxation base as vast proportions of the population are poor, and many who work, do it in the informal sector, which does not pay taxesFootnote 10.
Private sector is a major provider of all types of healthcare services in low- and middle-income countries. In Africa, the private sector (from traditional practitioners/healers, to private clinics, to mission hospitals) roughly provides 50% of health services. Healthcare expenditures follow a similar proportion; 50% go to private providers and 50% to the public sector. Surprisingly, this proportion is very similar for all economic quintiles [32]. These providers benefit (at least until 2019) from generalized economic growth, and from the perceived or real failures of the public sector to meet needs and expectations. In many instances, prices paid for surgical care in public facilities (that add costs by managing long waiting lists) are not substantially different from those offered by private institutions, in some instances located in the same area.Footnote 11
Research shows that globally, medicines and clinical services are responsible for the majority of healthcare expenditures. Inpatient care (which includes hospitalization, medicines and medical diagnostic services) is a proxy for surgery aggregate costs. It presents significant variations from country to country and between income groups inside a country; inpatient cost share ranges from 15% in low-income countries to 33% in upper middle-income countries. Outpatient care presents a stark contrast; it goes from 27% and 24% share in low-income and upper-middle income countries respectively; which means that while outpatient and inpatient care has a similar economic weight in upper-middle income countries, in low-income countries, the larger share of outpatient services could indicate a significant unmet need of surgical care. It does not come as a surprise that comparing the same groups of countries, low-income countries spend 13% in non-communicable diseases, while middle-income countries spend 29%, a proportion that mirrors the outpatient and inpatient “divide”. It seems that allocation of resources reflect more systemic response capacities than response to health needs of the population.
Sources of payment also differ significantly between country groups. Low-income countries use 22% of domestic public sources to finance healthcare needs, while middle-income countries domestic public sources funded 44% of their healthcare expenditures. More significantly, in low-income countries external aid contributes to 30% to the total health expenditures, while this contribution drops to 11% in middle-income countries. It is important to note that two thirds of foreign aid goes to infectious diseases (with HIV taking the lion share) in both country groups, underscoring the interest of the donor community in this needed, albeit particular area of intervention. Out-of-pocket in low and lower middle-income countries cover 41% of total healthcare expenditures. In fact, in low-income countries, private sources explain up to 57% of injuries costs, another proxy for surgical costs.
In the 2005–2018 period, foreign aid more than doubled. However, as external aid increased, health priorities in domestic budgets declined. In low-income countries, government budgetary allocation to health has decreased from 7% in 2000 to 5.5% in 2018; in this group, military expenditures are still larger than health expenditures. Had domestic expenditures at least remained at similar levels, governments would have been presented an opportunity to expand social protection in their respective countries, with increased chances to expand access to surgical care as well.
Private health insurance (PHI) seems inadequate for low-income countries; if disposable income is low, opportunities for investing in risk mitigation seem equally low. That said, PHI is an alternative way to finance healthcare that has been used in a variety of settings, from most OECD countries todayFootnote 12 to lower-middle income countries with large aggregate economies. In 1980, PHI companies started providing coverage services in a country like Colombia, which at that time had a GDP per capita of $1,240 ($4,150 in 2019 dollars), preceding by almost a decade when the national health reform introduced the concept of regulated competition. Healthcare financing—and by extension surgical financing- seems a fertile battleground for ideological warfare. It is clearly a complex problem. It requires a multidimensional approach that goes beyond the capacity of a single sector to respond to changing needs. The public-private divide seems nonsensical, at least from this perspective; it almost seems a lost opportunity for harnessing societal resources to create long lasting value.
4 The Spark: How Surgical Programs Can Advance in Low Resource Settings
To bring surgery to the regions and places in the world where is not accessible or not affordable, is inherently difficult. Experience shows that putting will, minds and financial resources together, has consistently helped us to surmount problems that seemed intractable. The 20th century and the beginning of the 21st brought new challenges, opportunities and innovative responses to social problems that we can use as tracers for interventions aiming to scale up access to surgical care worldwide. In the past few decades corporate social responsibility (CSR), philanthropy and development cooperation have emerged as important vehicles and contributors to advance complex programs and shape the global health agenda. Advancing global surgery is a long-term endeavor requiring the joint effort of host governments, international agencies, philanthropists, and civil society, not only as a way to procure necessary funds, but also knowledge and a structure that defines rules of engagement and identifies areas of responsibility.
CSR interventions. Corporate social responsibility (CSR) refers to activities, programs and strategies that businesses and corporations advance in areas of social interest like human rights, social welfare and environmental protection to name a few, intended to project a positive image for the institution, brands or products that the enterprise commercializes. Interventions might have different communication objectives, ranging from managing adverse public relations caused by an accident or quality process oversight, to strengthening the corporate image when entering discussions with regulatory authorities. As a result, target audiences can vary significantly, from authorities, to existing and potential investors, to the general public.
Because of the prominence of some cases, and because it is becoming a more ubiquitous communication tool, CSR has increasingly attracted the attention of development agencies and international organizations when seeking for potential partners to advance development agenda elements that require additional funding, and see positively the participation of civil society (commercial) actors. CSR has also attracted the attention of some governments; for instance, the Indian Government has required all for-profit companies contribute 2% of their profits to charitable causes as a form of compulsory CSR [33]. While this particular order distorts the intention of CSR as a corporate PR tool associated to the company’s profit generation objectives, also indicates that third parties see the potential in involving corporations in social causes different from its commercial intent.
Companies like medical equipment, devices and supply manufacturers, and pharmaceutical companies are in business that have a direct effect on human health. Many of these companies are highly visible, which can be an asset, but also a potential source of reputational risk if things do not go well, even when making corporate decisions such as setting prices, discontinuing a product line or delaying entering a market without strong purchasing power. For these companies, CSR has become increasingly important; as such, there are important programs—such as differential pricing- for pharmaceutical products sold at significantly discounted prices in low and middle-income countries, where the need because of disease burden and economic disparities is greater.
CSR is a tool that not only helps to repair battered reputations, but also can help develop stronger bonds with employees and stakeholders and improve relationships with host governments. Establishing public and private partnerships will become a central part of business strategy that uses CSR tools to benefit the organization’s image, achieve social impact through philanthropic means and turn them into sources of competitive advantage in new markets that while not economically developed today, have a positive economic and social outlook.Footnote 13
Global surgery stakeholders and advocates must change the traditional perspective of corporations as external partners that provide funding and expertise to support the health development agenda in LMICs, giving room for establishing more productive and sustainable, mutually beneficial engagements. Global surgery stakeholders can help public health authorities and planners in developing agencies and host governments work closely with corporations interested not just in procuring funding for specific programs, but also engaging them in the broader and longer-term objective of developing sustainable markets [34].
Working in global surgery can help corporations in the domestic environment to improve its relationship with their stakeholders by providing a highly visible intervention, aligned with the global health development agenda, while simultaneously serving to advance foreign markets understanding, and creating conditions for long-term development and returns. This could also open the doors to financing mechanisms with social purpose, giving these interventions a new meaning, potentially improving overall standing and value of the corporation [35].
The role of philanthropy. At the beginning of the 20th century, philanthropists like John D. Rockefeller and Andrew Carnegie contributed with their immense fortunes to advance the fight against disease. Institutionalization of their support has made their impact as long lasting as sustainable. While at that time, their interventions filled a void of what today many could consider as a government function, by mid-century, the cost of care and the increasing role of governments in healthcare services delivery and research, made wane the initial importance of private donors as charitable endeavors supporting global health [36]. However, the incursion in the global health scene of modern philanthropists has significantly changed programs policy design and implementation. In the US, there are more than 100,000 private foundations with approximately $ 569 billion in assetsFootnote 14, contributing to global health activities. The Bill & Melinda Gates Foundation is the largest with financing greater than the entire WHO budget [37].
Private donors attract less scrutiny than CSR programs, in spite that both, private foundations and corporations largely funded efforts to achieve the Millennium Development Goals.Footnote 15 For instance, an important entity such as the Global Fund receive substantial funding from private foundations for its operations. Different from corporations that are subject to consumers boycott, or government officials scrutiny, private foundations have a greater independence in their charitable efforts. While some may criticize this lack of oversight, this concern might actually reflect an important strength of private donors: they are not subject to the political vagaries, therefore can remain steady in pursuing long-term global health objectives. That persistence has paid off in policy areas, like helping to bring greater transparency in the selection process of WHO’s Director General, or in the protracted research effort for a vaccine against HIV.Footnote 16
Global surgery stakeholders can harness the long-term endurance capacity that private foundations can provide precisely because of its particular independence. Defining what is important in global health is a dialectic process that requires looking at a myriad of possibilities, almost all of them promising greater human wellbeing. Working jointly with ascending or established relevant foundations, can help to develop the steady course needed to succeed in interventions in which persevering is essential. Global surgery offers that kind of field.
As an example, a team supported by the Swanson Foundation introduced laparoscopic surgery in Mongolia as part of a program to improve surgical care in that country. This was not the original intent, but is what resulted after discussions between the team and local practitioners. After 20 years of sustained support, this service is now offered in all Regional Diagnostic Treatment Referral Centers in that country, as an example of what can be achieved with targeted philanthropic support [38]. It is important to note that private companies CSR programs from Storz, Cardinal Health, Johnson and Johnson, and several others, have also provided resources for this program.Footnote 17
Development cooperation assistance. Since the institutionalization of development cooperation after the success of the Marshal Plan, with the creation of USAID, high-income countries have developed increasingly sophisticated vehicles to support health programs in low and middle-income countries, initially as an instrument of the nation’s public diplomacy. Per-capita international aid of health programs more than doubled between 2000 and 2018 in real terms. International aid represented 25% of low-income countries health expenditures, in 2000 the official development assistance (ODA) accounted for 16% of the low-income country expenditures. Trends show in 2010, 13% of ODA to low-income countries went from 13% in 2010 to 20% in 2018. Development cooperation programs increased its focus in low-income countries and in health.Footnote 18 Africa receives 54% of aid resources for health [39]. ODA adheres to the five principles of the Paris Declaration; harmonization and alignment being the most important for this analysis. It means that donor countries coordinate between them, as much as they can, the allocation of resources to health programs in a host country and, at the same time, align that investment with the country’s health plan. It has resulted in more than 50% of aid resources going to fight infectious diseases.Footnote 19 In the case of the US, only $ 100 million, out of almost $ 9 billion, went to “non-traditional disease” which includes surgical diseases. Some other programs have a minor surgery component (circumcision for HIV prevention, and obstetric and iatrogenic fistula, as well as cesarean section for maternal health programs). While ODA resources are vast, allocations to surgery are not significant and they focus in a narrow subset of surgical services.
In spite of their focus, some programs have contributed to advance surgery in LMICs. In 1973, Profamilia Colombia introduced laparoscopy for tubal ligation with USAID technical and financial support. The country’s GDP was then $ 435 (Approx. $ 2,570 today). As the organization increased its outcome, it also improved its experience, so much so that by 1995 the organization provided close to 70 thousand surgeries. The organization estimated that in 2010, the direct cost of a laparoscopy was $ 60 per surgery, half the cost of the traditional laparotomy [40]. It is important to note that, before the Colombian health reform, Profamilia offered its surgical services at a very low nominal fee to the poorest of the poor, and charged patients based on their ability to pay. After the reform took place, the government contracted out with organizations like Profamilia to offer healthcare services to the general population.
To make surgery an ODA priority, global surgery advocates can work jointly with bilateral organizations, looking for opportunities to submit joint proposals with host governments in low-income countries interested in improving its surgical access and quality. This might offer the opportunity to influence other governments as well and nudge donors to support these programs in full alignment with the host nation’s health priorities.
5 The Long Run: How to Sustain Efforts in Surgical Services Delivery
Complex problems rarely have a single solution. Usually different elements (knowledge, resources, etc.) have to be brought together to effectively address and solve it. Expanding access to quality surgery in low resource settings is a complex problem that requires multiple approaches. In this section we will see different approaches and how they can jointly work to provide effective and sustainable financing.
The role of government. Governments have a fundamental role as funders or direct providers of surgical care [41]. A distinct feature is that governments in high-income countries pay for a larger proportion of healthcare services, than governments in low- and lower-income countries.Footnote 20 We have seen that health financing is challenging for low-income country governments and might need significant adjustment to their national budgets to increase funding for health. Additionally, a narrow taxation base, makes funding difficult. As a result, it is essential to develop vehicles that can help governments to take advantage of initial support provided through development cooperation or through CSR and philanthropic efforts.
Governments give incentives to providers to ensure output and quality to improve access to health care services, including surgery. They also provide subsidies to the demand to incentivize the use of certain type of healthcare services, to reduce its financial burden.
Governments have several mechanisms for channeling financial incentives to both sides of the economic equation; for providers: pay for performance, prepayment, schemes and contracting; for service users: conditional cash transfers, vouchers and community loan funds (to pay for transportation or lodging) amongst others [42].
Demand side financing and incentives to providers are usually implemented together (an example is the Nepal Aama program—see box below [43]) where cash payments to women, incentives to providers and free delivery care are all offered [44]. As incentives and subsidies (also known as resource allocation and purchasing arrangements, or RAPs) seek to modify the perception of price for the consumer, while stimulating quantity of services offered, the supply and demand curves will meet at a different point (less services at higher prices) than they would meet without the intervention [45]. This approach brings he advantages of fee for service for providers, while empowering consumers to look for better quality care.
-
The Aama Surakshya Programme is a Maternity Incentive Scheme (MIS) implemented by the Government of Nepal, with support from the UK’s Department for International Development in 2009 and it is still in operation. It aims to provide free delivery care to all women at the point of use by reducing financial barriers to women seeking institutional care. It has the following elements:
-
Incentives to women: Transport incentives offered to all women delivering in an institution, including additional cash payment on completing Four Antenatal Care Visits (4ANC).
-
Unit cost to health facilities: Institutions receive a reimbursement per delivery provided.
-
Incentives to health worker: Providers receive a stipend per delivery (includes home deliveries as well) paid with the reimbursement to health facilities.
Public-Private Partnerships/blended financing. Blended financing is a term that refers to bringing together resources from philanthropists, governments and international institutions to strategically fund development programs. It helps attract investors to countries that struggle to find them, particularly in social sectors. In 2015, this mechanism helped raise $27 billion of private capital [46]. In 2018, The World Bank’s IDA issued $1.5 billion bonds that generated an ordering demand for $ 4.6 billion [47]. These instruments can help attract philanthropists, medical devices manufacturers, social insurers and many other private actors, to fund targeted health areas. Health has attracted close to 30% of the capital mobilized [46].
There are different funding mechanisms to place resources mobilized, ensuring that financial allocation is related to program performance. Some of these results driven funding mechanisms include: Debt buy-downs, development impact bonds, impact investment funds and loan guarantees amongst others [48].
The role of NGOs. For decades, governments and development cooperation agencies have worked with NGOS to advance national social agendas. The role of NGOs as institutions that can effectively meet needs of underserved groups is well known. USAID has worked with NGOS all over the world to provide reproductive and maternal health services, helping these organizations to improve their technical and managerial capacity, preparing them to function after donor support ends. In countries like Bangladesh, NGOs provide approximately 10% of primary care services to the poor (including tubal ligation, circumcision, cesarean section and fistula surgery services).Footnote 21 These organizations are not just extensions of the public sector, but also an important source of innovation. Institutions like the Edna Adan Hospital in Somaliland helped to train nurses to manage obstetric fistula; or Profamilia in Colombia, trained nurses in IUD insertion, formerly consider a medical intervention in that country. These examples serve to visualize how innovation might just happen when resources (human, financial or physical) are rearranged to perform a function. In both cases, the solution addressed an issue of scarcity (not enough trained personnel) to provide quality care and at a much lower cost, which helped to expand access.
Private sector involvement. Private sector providers, funders and suppliers are central to achieve the objective of expanding access and improving quality surgical care in low-resource settings. In SSA 50% of healthcare services are provided by private providers, so most likely any solution must consider this formidable force.
Governments in Africa can work with development cooperation agencies to establish impact investment funds that provide financing to private providers interested in developing surgical facilities. Governments could also work simultaneously with local banks to create loan guarantees with multilateral agencies financing. These activities could even help to develop new financing mechanisms.
Private investors can join forces to set up transnational insurance schemes in sub regions in Africa (like in the East African Community) to take advantage of the larger aggregate demand to establish financially viable, cost-effective insurance schemes. Using instruments like impact bonds, local entrepreneurs can collaborate with PHIs companies in high-income countries to develop the technical capacity to provide innovative insurance products that can complement those of local governments.
More importantly, direct contributions to surgical service delivery have appeared in private institutions (for profit and non-profit alike) in low middle-income countries in different moments and in different surgical specialties. Profamilia in Colombia created a singular surgical ecosystem that helped scale up a surgical procedure that, because of high volumes achieved, resulted in better quality and lower costs. Aravind Eye Care in India scaled up eye surgeries, improved surgical procedures, reaching the poor in a low-middle income country. They developed a business model that invites emulation.
While obstacles are real, multiple individuals have shown that what we deem impossible is possible. The world has never been richer and interconnected than today. Putting together a clear vision. Leadership and decision, we can take advantage of current technological and financial innovations to pursue the objective to provide quality surgery to all, everywhere, and when needed.
6 The Ecosystem
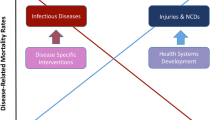
The global surgery financial ecosystem Fig. 4.1 involves an array of players with coinciding and diverging interests, which have a common gravitating point around the patients they exist to serve (even if it is a fraction of the organization like ODA agencies and governments). The value exchange takes its real dimension when institutions involved deliver health, and in this particular case, health through surgery.
The graph below Fig. 4.1 depicts the transactional elements described in the previous sections, giving a sense of the systemic complexity, not just because of the variety of actors involved, but also because of the foundational elements that make service delivery an action that fulfills a right, or complies with the law of the land, while aiming to develop wellbeing and wealth. Solid arrows represent the flow of financial resources and their direction; dotted lines refer to the flow of surgical services and supplies. It also provide a sense of the role organizations play or can play in sharing resources and sparking economic exchanges that can result in viable, sustainable systems.
7 Conclusion
Expanding access to affordable, quality surgical care, to reach all in need is a complex, extremely difficult enterprise; but is not impossible. Perhaps for the first time in history, humanity has the knowledge, technical means, organizational and legal structures and financial resources that turn this idea into an attainable objective. Is not just the progress reflected in wealth in high-income countries that provides the example that it is possible? It is the multiple experiences of a myriad of interventions in low and middle-income countries that signal that it can be done, and should be done.
The increasingly pervasive inclusion of surgery in the country’s definition of Universal Health Coverage packages is also a testament that the idea of globalized, universal access to surgery has left the expert’s realm and is becoming a general public concern.
The debate if the surgery should be expanded through public or private means offers a false dichotomy, as societies are constructed through a myriad of pacts and societal contracts that responds to immediate and distant realities, to concrete axiologies and different belief structures. Low-income countries must harness resources (knowledge, capital, labor, etc.) from different sectors to be able to respond to the call and challenge of offering surgical care to all; it is also their responsibility. Governments, enterprises, foundations and individual philanthropists from high- and high-middle income countries can share their respective resources—including experience- with institutions in low-income countries, helping them find adequate responses to their challenges and obstacles in meeting people’s surgical needs.
Stakeholders thrusting the idea of global surgery attainability are encouraged to find responses from the multiple lessons learned and the new ideas they can extract from combining experiences and having conversations that help create not one, but multiple pertinent paradigms. We must understand that solutions are general in concept but specific in context; we must be ready to get thousands of responses, all relevant in addressing the universal challenge we face.
Notes
- 1.
Konrad Obermann, Peter Müller, Hans-Heiko Müller, Burkhard Schmidt, Bernd Glazinski; Understanding the German Health Care System; Mannheim Institute of Public Health.
- 2.
Germany is a federal republic consisting of sixteen states, commonly known as bundesland (plural Bundesländer).
- 3.
William D Savedoff; op. cit.
- 4.
Lawrence O Gostin; op. cit.
- 5.
Desmond T. Jumbam, op. cit.
- 6.
Musgrove, op. cit.
- 7.
Ibid.
- 8.
Ibid.
- 9.
CIA Factbook, Jan 2014.
- 10.
According to WHO’s Global spending on health 2020, in 2018 tax revenues in low-income countries represented less than 13% of GDP.
- 11.
Ibid.
- 12.
Sato; op. cit.
- 13.
Ibid.
- 14.
These accumulated holdings are larger than the 2019 economic output of countries like Sweden, Argentina or Austria (“GDP (current US$)”. World Development Indicators. World Bank. Accessed on 2/18/21).
- 15.
Ibid.
- 16.
Koop; op. cit.
- 17.
Conversation with Dr. Ray Price (2-26-21).
- 18.
Global spending on health 2020; op. cit.
- 19.
Global spending on health 2020; op. cit.
- 20.
Global spending on health 2020; op. cit.
- 21.
Between 2008 and 2011, the author served as the Chief of Party of Smiling Sun in Bangladesh. This network of NGOs provided services to close to 15 million Bangladeshis.
References
Shrime MG, Dare A, Alkire BC, Meara JG. A global country-level comparison of the financial burden of surgery. BJS. 2016;103:1453–1461.
Mckee M et al. Universal health coverage: a quest for all countries but under threat in some. Value Health. 2013;16.1:539–45.
Savedoff WD, de Ferranti D, Smith AL. Victoria Fan; Political and economic aspects of the transition to universal health coverage Lancet. 2012;380:924–32.
Greer SL, Méndez CA. MPH, universal health coverage: a political struggle and governance challenge. Am J Public Health. 2015;105:S637–S639. https://doi.org/10.2105/AJPH.2015.302733.
Bump JB (2010) The long road to universal health coverage. A century of lessons for development strategy (PDF). Seattle: PATH. Retrieved February 18, 2021.
Pestalozza C. Das Recht auf Gesundheit. Verfassungsrechtliche Dimensionen [The right to health. Constitutional dimensions]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 200750(9):1113–8. German. https://doi.org/10.1007/s00103-007-0310-y. PMID: 17828472.
Nishtar S, Choked Pipes, Reforming Pakistan’s mixed health system. Oxford University Press 2010.
Titelman D. Reformas al sistema de salud en Chile: Desafíos pendientes, Unidad de Financiamiento para el desarrollo División de Comercio Internacional y Financiamiento para el Desarrollo, Santiago de Chile, septiembre de 2000.
Heymann J et al. Constitutional rights to health, public health and medical care. The status of health protections in 191 countries. Global Public Health 8.6 (2013): 651.
Flood C, Gross A (eds) The right to health at the public/private divide, a global comparative study. Cambridge University Press, 2014.
Lineamientos generales para la implementación de la Política Pública Nacional de Discapacidad e Inclusión Social en entidades territoriales 2013–2022 https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/PS/politica-publica-discapacidad.pdf . Retrieved February 19, 2021.
Gostin LO, Monahan JT, Kaldor J, DeBartolo M, Friedman EA, Gottschalk K, Kim SC, Alwan A, Binagwaho A, Burci GL, Cabal L, DeLand K, Evans TG, Goosby E, Hossain S, Koh H, Ooms G, Periago MR, Uprimny R, Yamin AE. The legal determinants of health: harnessing the power of law for global health and sustainable development. Lancet 2019;393: 1857–910.
Alkire BC, Raykar NP, Shrime MG, Weiser TG, Bickler SW, Rose JA, Nutt CT, Greenberg SLM, Kotagal M, Riesel JN, Esquivel M, Uribe-Leitz T, Molina G, Roy N, Meara JG, Farmer PE. Global access to surgical care: a modelling study. Lancet Glob Health. 2015;3:e316–23.
Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J, Mérisier ED, El-Halabi S, Farmer PE, Gawande A, Gillies R, Greenberg SLM, Grimes CE, Gruen RL, Ismail EA, Kamara TB, Lavy C, Lundeg G, Mkandawire NC, Raykar NP, Riesel JN, Rodas‡ E, Rose J, Roy N, Shrime MG, Sullivan R, Verguet S, Watters D, Weiser TG, Wilson IH, Yamey G, Yip W. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–62.
Negrette JC. Presentation to HBI, London April 5, 2017.
Chambers A. Trends in US Health Travel Services Trade; USITC Executive Briefing on Trade, 2015.
Jumbam DT, Reddy CL, Makasa E, Boatin AA, Rogo K, Chu KM, Nangombe BT, Oladapo OT, Meara JG, Maswime S, MBCh, FCOG(SA), PhD. Investing in surgery: a value proposition for African leaders; White paper, Target journal: The Lancet.
Kamal R, McDermott D, Ramirez G, Cox C. How has U.S. spending on healthcare changed over time?; Health System Tracker Peterson-KFF website. https://www.healthsystemtracker.org/chart-collection/u-s-spending-healthcare-changed-time/#item-start. Accessed on 2/17/21.
Musgrove P. Health Economics in Development; 2004 The International Bank for Reconstruction and Development/The World Bank.
“GDP (current US$)”. World Development Indicators. World Bank. Retrieved 2/15/21.
Chao TE, Sharma K, Mandigo M, Hagander L, Resch SC, Weiser TG, Meara JG. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. Lancet Glob Health. 2014;2:e334–45.
Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3 (S2):S38–44.
Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3 (S2):S38–44.
Dalton SC. The current crisis in human resources for health in Africa: the time to adjust our focus is now. Trans R Soc Trop Med Hyg. 2014;108:526–527.
Kerns C, Willis D. The Problem with U.S. Health Care Isn’t a shortage of doctors. HBR. 2020.
deVries C; Price R. global surgery and public health: a new paradigm. Jones & Bartlett Learning, 2012.
The importance of human resources management in healthcare: a global context; Kabene SM, Orchard C; Howard JM, Soriano MA. Raymond Leduc. Human Resources for Health. 2006, 4:20.
Hsia RY, Mbembati NA, Macfarlane S, Kruk ME. Access to emergency and surgical care in sub-Saharan Africa: the infrastructure gap. Health Policy Plann. 2012;27:234–244.
Azusa Sato; Presentation at Prince Mahidol Conference, Bangkok; London School of Economics/Asian Development Bank, 01/26/16.
Global spending on health 2020: weathering the storm. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Mills A. Health care systems in low- and middle income countries. N Engl J Med. 2014;370:552–7.
Healthy Partnerships How Governments Can Engage the Private Sector to Improve Health in Africa; The International Bank for Reconstruction and Development/The World Bank; 2011.
Hayley Droppert and Sara Bennett; Corporate social responsibility in global health: an exploratory study of multinational pharmaceutical firms; Globalization and Health (2015) 11:15.
Wofford D, MacDonald S, Rodehau C. Acall to action on women’s health: putting corporate CSR standards for workplace health on the global health agenda. Global Health. 2016;12:68.
Du S, Bhattacharya CB, Sen S. Maximizing business returns to corporate social responsibility (CSR): the role of CSR communication. Int J Manag Rev (2010).
Everett Koop C, Pearson CE, Roy Schwartz M [eds] Critical issues in global health; koop foundation, In., and the National Center for Health Education. Published by Jossey-Bass, 2002.
Stuckler D, Basu S, McKee M. Global Health Philanthropy and Institutional relationships: how should conflicts of interest be addressed?. PLoS Med. 2011;8(4).
Price R et al. World journal of surgery, improving surgical care in mongolia: a model for sustainable development, 2012.
Aid spent on health: ODA data on donors, sectors, recipients; Development Initiatives. https://devinit.org/resources/aid-spent-health-oda-data-donors-sectors-recipients/#note-KjHccT2KO. Retrieved 2/22/21.
Gerencia Salud Sexual y Reproductiva, PROFAMILIA; Juan Carlos Negrette, Improving Access to Quality Health Services Through “High-Tech” Interventions in LMICs; Presentation at Prince Mahidol Award Conference, Bangkok, Thailand, 1/26/16.
Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg. 2008;32:533–536.
Bowser D, Gupta J, Nandakumar A. The effect of demand- and supply-side health financing on infant, child, and maternal mortality in low- and middle-income countries. Health Syst Reform. 2016;2(2):147–159.
Review of the Maternity Incentive and Free Delivery Care Program (the Aama Surkshya Programme) in Nepal, January 2020, http://www.nhssp.org.np/Resources/PPFM/Review%20of%20Aama%20Surakshya%20Programme%20in%20Nepal%20-%20January%202020.pdf. Accessed 2–28-2021.
Witter S, Somanathan A. Demand-side financing for sexual and reproductive health services in low and middle-income countries: a review of the evidence; The World Bank, East Asia and the Pacific Region, Human Development Department; Policy Research Working Paper 6213,0 October 2012.
Preker A et al. Public ends, private means: strategic purchasing of health services; the international Bank for Reconstruction and Development/The World Bank, 2007.
Greater than the Sum of its Parts: Blended Finance Roadmap for Global Health; Center for Innovation and Impact (CII), US Agency for International Development, USAID; Accessed 2/21/21.
Peters AW, Pyda J, Menon G, Suzuki E, Meara JG. The world bank group: innovative financing for health and opportunities for global surgery. Surgery. 2019;165(2):263–272.
Greater than the Sum of its Parts: Blended Finance Roadmap for Global Health; Center for Innovation and Impact (CII), US Agency for International Development, USAID. Accessed 2/21/21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Negrette, J.C. (2022). Global Surgery Financing, Challenges and Possibilities. In: Kpodonu, J. (eds) Global Cardiac Surgery Capacity Development in Low and Middle Income Countries. Sustainable Development Goals Series. Springer, Cham. https://doi.org/10.1007/978-3-030-83864-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-83864-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-83863-8
Online ISBN: 978-3-030-83864-5
eBook Packages: MedicineMedicine (R0)