Abstract
One of the important goals of surgical procedures involving the visual pathways (retina, optic nerve (ON), optic chiasm, optic tracts, lateral geniculate nucleus in the thalamus, optic radiation, and occipital visual cortex) is the preservation of visual function and in cases of visual impairment, where possible, its improvement (Banoub et al., Anesthesiology 99:716, 2003; Luo et al., PLoS One 10:e0120525, 2015; Houlden et al., J Clin Monit Comput 28:275–285, 2014; Duffau, Acta Neurochir 153:1929–1930, 2011). With these goals in mind, efforts to evaluate and enhance the usefulness of intraoperative monitoring (IOM) of the visual pathways that began in the early 1970s have continued. Since Wright et al. (Trans Ophthalmol Soc U K 93:311–314, 1973) published their report of continuous intraoperative monitoring of visual pathways, utilizing brief flashes of strobe light to evoke electroretinographic (F-ERGs) and visual-evoked potentials (F-VEPs), during orbital surgery, a number of other researchers have strived to evaluate ways in which to monitor the visual pathways in intraoperative settings (Handel, Ann Plast Surg 2:257–258, 1979; Allen et al., Clin Neurosurg 28:457–481, 1981; Grundy, Anesthesiology 58:72–87, 1983; Albright and Sclabassi, J Neurosurg 63:138–140, 1985; Costa e Silva et al., Neurol Res 7:11–16, 1985; Burrows et al., Anesthesiology 73:632–636, 1990; Sloan, Int Anesthesiol Clin 34:109–136,1996; Duffau et al., Acta Neurochir (Wien) 146:265–269, 2004; Benedičič and Bošnjak, Doc Ophthalmol Adv Ophthalmol 122:115–125, 2011;Benedičič and Bošnjak, Acta Neurochir (Wien) 153:1919–1927, 2011; Landi et al., Clin Neurol Neurosurg 113:119–122; 2011; San-Juan et al., Clin Neurol Neurosurg 113:680–682, 2011; Chung et al., Acta Neurochir (Wien) 154:1505–1510, 2012; Ogawa et al., Acta Neurochir (Wien) 155:1879–1886, 2013; Kamio et al., Neurol Med Chir (Tokyo) 54:606–611, 2014; Padalino et al., Surg Neurol Int 4:40, 2013).
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Intraoperative monitoring
- Visual pathways
- Visual-evoked potentials
- Visual pathway stimulation
- Flash electrographic response
- Flash VEP response
- Monocular stimulation
- Binocular stimulation
- Light stimulation
- Flash stimulation
- Retinal stimulation
Introduction
One of the important goals of surgical procedures involving the visual pathways (retina, optic nerve (ON), optic chiasm, optic tracts, lateral geniculate nucleus in the thalamus, optic radiation, and occipital visual cortex) is the preservation of visual function and in cases of visual impairment, where possible, its improvement [1–4]. With these goals in mind, efforts to evaluate and enhance the usefulness of intraoperative monitoring (IOM) of the visual pathways that began in the early 1970s have continued. Wright et al. [5] are generally credited with the first report of a method for continuous monitoring of the visual pathways in 1973; utilizing brief flashes of light to evoke electroretinographic (F-ERGs) and visual-evoked potentials (F-VEPs) during orbital surgery. This triggered a number of other researchers to test their usefulness [2, 3, 6–21]. While some have reported favorable results and outcomes [5, 22–31], others have dismissed their use, citing technical difficulties associated with the delivery of visual delivery in an operating room (OR) setting, large inter- and intra-individual variability, instability and unreliability of the visual responses [32–36], their susceptibility to anesthetics, particularly inhalational agents [32–37], and lastly and most damning, the poor correlation of IOM results to postoperative functional outcomes. All of these findings have led to a general disenchantment with their intraoperative use [7, 12, 18, 32–35, 37–45].
Still, on a case-by-case basis, monitoring of visual-evoked potentials (F-VEPs) has helped guide surgeries of the orbit [46–48], and anterior visual pathways during tumor or lesion removal where its use has helped identify encroachment of tumors on the optic chiasm, and has aided in the differentiation of normal ON tissue from tumor tissue; especially when the tumor encompasses the ON [2, 12–15, 19, 20]. Direct ON stimulation has helped navigate during surgical removal of tumors involving the anterior visual pathway and skull base tumors [13–15, 49, 50] with good outcomes. Though improved microsurgical techniques during procedures involving the sellar and parasellar regions [19] have significantly reduced the incidence of visual complications related to ON or chiasmal manipulation and/or devascularization, the potential remains for real-time, inadvertent, and potentially harmful maneuvers that may cause prolonged or intense indirect traction or compression of the ON to go unnoticed. Concern for preventing devastating outcomes to the visual pathway has encouraged a small but dedicated group of researchers to pursue refinement of the techniques for IOM of the visual pathways [2, 3, 13, 15, 19–25].
Other reports of beneficial use of IOM visual pathway monitoring have been contained in the literature. F-ERGs [51, 52] and F-VEPs [36, 37, 53, 54] have been reported to be helpful in assessing the depth of anesthesia. F-ERGs have been utilized in monitoring retinal function during eye surgery [46, 47, 54–56] and endovascular procedures involving orbital or periorbital vascular lesions [21] with good outcomes. They also have been used to monitor retinal perfusion during procedures employing extracorporeal circulation and hypothermic circulatory arrest [11, 57]. F-VEPs have reportedly been helpful for anatomic navigation of the optic radiations during surgical treatment of an occipital arteriovenous malformation [17], and by use of diffusion tensor imaging-based tractography for functional monitoring of the visual pathway [58]. Finally, visual-evoked responses obtained from direct stimulation of the optic tract have been used as a method for globus pallidus internus (GPi) targeting during pallidotomy [59, 60] and deep brain stimulation (DBS) interventions for treatment of Parkinson’s disease where such procedures are performed under general anesthesia or for patients who otherwise are unable to cooperate during the procedure [16]. Although many of the above reports involved case report(s) or series, their findings suggest that further examinations of these monitoring methodologies and applications are needed. A better understanding of visual stimuli, the portions of the visual pathways that are stimulated, the methods for recording neurophysiologic responses, the effects of surgical manipulation, anesthetic management, and other perioperative factors on responses, will hopefully lead to improved IOM results. This in turn may spark renewed interest in research to further enhance techniques and outcomes for IOM of the visual pathways.
Anatomy and Physiology of the Visual System
The optic structures of the eye project images onto the light-sensitive receptors of the retina, where a surprisingly high degree of neural processing is accomplished through the retina’s complex pattern of interconnections between excitatory and inhibitory neurons . Some nerve fibers have small excitatory fields surrounded by inhibitory areas, and others have inhibitory center areas surrounded by excitatory ones. As a result, a good stimulus for exciting the visual pathway would be one that undergoes changes in contrast gradients (i.e., pattern-reversal). Because, in general, patient cooperation is not possible for the majority of surgical procedures, it is not feasible to utilize stimulation using high-contrast pattern reversing checkerboard stimuli that are used in diagnostic testing. Hence, the frequently employed stimulus for eliciting VEP responses for monitoring purposes has been flash stimuli [24, 61–63]. While the spatial distribution of the light over the visual field of each eye is transmitted to the brain through the optic nerves, very little information regarding the temporal variations in illumination is conveyed. Therefore it is key to note that when flash stimuli are employed for IOM monitoring purposes, what is actually being monitored is the visual pathways for light perception and not for visual acuity [64].
The neural information of flash stimuli travels from the optic chiasm onward, via the optic tracts to the lateral geniculate body in the thalamus, which then projects via connections to the visual cortex (Fig. 4.1) [64]. Though coding of the visual system has been intensively studied yielding a wealth of information about the retina’s complex neural network responses [65], information about the gross response from the ON and lateral geniculate body to flash stimuli remains relatively sparse, and in general, early cortical activation following flash visual stimulation is not well understood in humans [65]. It is important to note that the optic pathways cross at the chiasm such that monocular or binocular flash stimuli used in monitoring will produce bilateral pathway activation behind the chiasm unless a means of hemifield visual stimulation can be utilized (as can be done in awake subjects).
Schematic drawing of the visual pathway. OC optic chiasm, SC superior colliculus, LV lateral ventricle (from Moller et al. [64]; with permission)
Eliciting and Recording Flash Visual-Evoked Potentials
Depending on the portion(s) of the visual pathways at risk during surgical procedures, a number of strategies for stimulation of those pathways have been explored.
Flash Electrographic Response
Responses generated by stimulation of the retina (F-ERG) have played a fundamental role in the diagnostic evaluation of retinal health [66]. For IOM purposes, they have been primarily used to ensure retinal and visual pathway stimulation . They also have been used to monitor surgeries of the orbit and as a measure of anesthetic depth [46, 47, 51, 52]. The main components of the F-ERG are a negative-going a-wave with latencies occurring between 24.2 ± 1.1 and 27.2 ± 3.7 ms and a positive-going b-wave with latencies of 45.0 ± 1.5–55.1 ± 7.4 ms. The a-wave, in response to a bright flash, largely reflects photoreceptor function but there may be a contribution from postreceptoral structures [67]. The b-wave, which is of higher amplitude than the a-wave in normal subjects, reflects postphototransduction activity. The origin of the ERGs’ a- and b-waves is reportedly a combination of activities that include photoreceptor potentials, potassium-mediated current flow, and DC potentials within Müller cells [67]. The F-ERG to a flash stimulus is a mass response; thus F-ERG responses can appear normal when dysfunction is confined to small retinal areas (e.g., macular dysfunction). It has been reported that despite the macula’s high photoreceptor density, an eye with purely macular disease has a normal bright single flash ERG response [67]. Typical ERG-VEP responses to flash stimuli delivered by light-emitting diode (LED) goggles are included in Fig. 4.2.
An example of intraoperative flash electroretinograms (F-ERGs) recorded from surface electrodes placed in the orbital notches bilaterally and referenced 3 cm laterally and flash visual-evoked responses (F-VEPs) recorded from electrodes placed at left occipital (O1), mid-occipital (Oz), and right occipital (O2) scalp locations is shown. The responses were obtained at baseline for a patient undergoing endovascular cerebral angiography with stenting and coiling for treatment of a right ophthalmic artery aneurysm. The rate of flash stimulation was 1.1/s. An average of 100 responses was obtained. Anesthetic management included induction with thiopental, sufentanil and dexmedetomidine (1 μg/kg), and maintenance with sufentanil infusion, 0.5 MAC of isoflurane and continuous infusion of dexmedetomidine (0.7 μg/kg/h)
Flash VEP Response
The F-VEP is generated by postretinal areas of the central nervous system in response to visual light stimulation and is a reflection of activity in segments of the primary visual pathway that project through the lateral geniculate body to the cortical visual fields. The response is composed of a triphasic waveform with an initial small positive deflection (40–50 ms), followed by a second negative deflection at 70–89 ms (often referred to as N70 or N1), followed by a positive wave at about 100 ms (P100 or P1) [68]. Though not unequivocally documented, the generator sites for the three waves of the F-VEP to LED stimulation are believed to originate from the lateral geniculate, striatum, and areas 17, 18, and 19 of the visual cortex [27, 68, 69].
Techniques for Eliciting F-ERG and F-VEP
The lack of suitable equipment for visual stimulation has been a severe handicap to the use of ERG-VEP for IOM. Pattern-reversal stimuli or multifocal electroretinographic stimuli (which are routinely utilized in diagnostic settings to evaluate retinal function related to acuity) cannot be utilized on unconscious patients in the OR setting given the requirement for their cooperation and visual fixation on the stimuli. Moreover, the shift in dark vs. light pattern/contrast of these stimuli, which is key to stimulating the retinal structures related to visual acuity, would certainly be diminished if not lost if one were to try to deliver these stimuli through closed eyelids. Because flash stimuli do not require patient fixation and cooperation and can be delivered through closed eyelids, they have been the most frequently used stimulus in the OR setting. Unfortunately, early research demonstrated that even when flash stimuli were employed for clinical diagnostic use (e.g., for assessment of ON pathology in multiple sclerosis patients), VEP responses to bright flashes were found to be normal while their responses to pattern-reversal stimulation were abnormal [68]. Moreover, the amplitude and latency of VEPs elicited by the above flash stimulation methods unfortunately demonstrate considerable patient inter- and intra-variability of amplitude both in diagnostic and intraoperative settings [70]; especially in neonates, where maturation of the cerebral cortex appears to play a factor [71]. So although flash stimulation has largely been the stimulus of choice for IOM, it is not the best stimulus for assessing the preservation of fine visual acuity and function. Rather it has been used to assess in a rudimentary fashion whether response to stimulation can be conveyed along various points of the visual pathways [71]. Even so, it is important to note that when there is preexisting visual dysfunction that may disrupt the ability to convey such stimulation, recording responses may be compromised, although that has not been entirely confirmed. Multiple studies [2, 3, 20, 23–25] reported that preexisting severe visual dysfunction (even for patients with preexisting visual acuities of <0.4 (20/50)) negatively impacted their ability to record F-VEPs while others indicate that F-VEPs for IOM can be obtained successfully from some patients with severe visual deficits [3, 19], when onset of the dysfunction was acute.
Devices for Flash Stimulation
Researchers have worked to develop improvements in devices for the delivery of flash stimuli for IOM use, since the problems of delivering stimuli may be key to developing more effective activation of the pathways that correlate with functional vision. Initially a traditional strobe light was used to elicit responses but was found to be cumbersome in the OR and delivery of the flash could be ineffective since it might be partially obscured by the scalp flap and drapes if a bicoronal scalp incision is used, thus requiring a modification of the surgical approach.
Fiberoptic haptic lens [72] and scleral contact lens [26] connected to photostimulators were developed to provide flash stimuli in the 1970 and 1980s. Although some claim the resulting responses were more robust than those later obtained with LED stimulation (especially through dilated eyes) [72], use of contact lens for IOM has lost favor due to the invasive nature of the technique (e.g., lid sutures to keep the corneal lens recording/stimulating device in place) and the potential risk of corneal abrasions and ulcerations with their use. The American Electroencephalographic Society (AEEGS) Guidelines for IOM recommend that such hard lens stimulators be kept on the eyes for a maximum of 45 min (limiting their practical use for a majority of surgical procedures) and that users need to carefully examine the safety data from the stimulator’s developer before employing such lenses in the OR [73].
Because most shy away from the use of contact lens stimulators, LEDs mounted in eye patches [23–25] or goggles [9, 27] have been used, but the latter are bulky, require a headband, and can interfere with surgery. Their use also carries some risks . Care needs to be taken to ensure that the goggles are well-supported by the bony ridge of the patient’s orbit and that they remain in place during the surgery. Should they inadvertently slip down and put direct pressure on the globe of the eye, they can cause central retinal artery thrombosis [9].
Type of Light Stimulation
The AEEGS issued a recommendation that flash VEPs induced by white stroboscopic light (F-VEPs) be differentiated from those induced by red LEDs (LED-VEPs) [73] by utilizing the appropriate abbreviations. However, in general, in the IOM literature, the terms F-ERG and F-VEPs have been used to represent both. However, abbreviations aside, the two methods of stimulation may actually activate different retinal and cortical pathways [12]. Newer LED stimulating goggles and patches provide significantly increased luminosity [23–25]. Although safety data regarding their use is scant, authors reporting on their IOM use have not reported any postoperative sequelae, including cases involving lengthy neurosurgical procedures [2, 3, 20, 23–25].
Monocular vs. Binocular Stimulation
Although binocular stimulation has been used for some studies, when the goal is to evaluate individual retinal and anterior pathways, the visual stimulus should be delivered and recorded monocularly with responses from the contralateral eye, if clinically unaffected, used as a control [73].
Pupillary Size and Retinal Luminance
When employing flash stimuli to elicit F-ERGs and F-VEPs, efforts to maintain pupil size and retinal luminance throughout the surgical procedure are important because these parameters affect the response latency and amplitude. Kriss et al. [74] showed that F-VEP latency through closed eyes is increased when compared to those recorded through open eyes. Intraoperative use of narcotics often results in miotic pupils that reduce retinal luminance, and staged dosing of narcotics during the surgical procedure may induce changes in latency and amplitude that may be misinterpreted as a surgically related event. It has been recommended that maximal dilation of the pupils be done through use of conjunctival instillation of mydriatics at the start of the case [73], but that may be contraindicated when perioperative assessment of pupillary response is required or preferred. Of note, recent and notably successful reports of intraoperative recordings of F-ERG and F-VEPs did not employ pupil dilation as part of their total intravenous anesthetic and monitoring management: propofol [2], administration of opioids [23–25], or remifentanil [2]. It is important to note that those with successful IOM recordings of F-VEPs employed newer and brighter 16 LED arrays embedded in soft round silicone disks [2, 20, 23–25] or in goggles [3, 18] with luminosity adjustable from 500 to 20,000 Lumens (Lx), which helped to ensure retinal illumination and stimulation.
Recording F-ERGs and F-VEPs
The recommended standards for IOM of VEPs were issued in 1987 by the American EEG Society [73]. To obtain consistent results, the guidelines advised that the following parameters be documented and remain constant throughout the IOM period. Though no such standards for IOM recording of ERG have been published, the following would likely apply to them as well. Given the expected high degree of F-VEP response variability even in awake subjects [73], each patient with a reproducible response should serve as his or her own control in the IOM setting. A simultaneous recording of F-ERG responses is useful for confirmation of retina stimulation.
Before the surgeon approaches the optic pathways, the monitoring team should have identified reproducible waves to be used as benchmarks for meaningful assessment during subsequent monitoring during critical stages of the surgery. Stacked plots of sequentially recorded averages are indispensable for assessing changes during surgery. Interpretation of intraoperative VEPs should be done in relation to pharmacologic, physiologic, and surgical factors. Change in response trends should be reported as soon as identified, and immediate steps should be taken to prevent the risk of lasting damage and to optimize normal function [73].
Stimulus Color
The color of the flash or LED (white vs. red) should be indicated on the record and kept constant throughout the case.
Stimulus Rate
For transient F-ERGs and F-VEPS , a stimulus rate of 1–2.5 Hz is suggested and for steady-state responses a rate of 8–30 Hz may be used. Steady-state stimulation has not gained wide use for monitoring purposes. In a study published in 2004, their use during surgery for monitoring purposes did not facilitate improved or more stable F-VEP recordings [42].
Recording Electrodes and Their Placement
Corneal or scleral lenses for IOM recording of ERG responses were supplanted in the 1980s with less invasive devices and methods. Corneal recording devices using a Burian Allen electrode and other devices placed on or near the cornea yielded larger, robust responses but are rarely used due to the risks of corneal abrasion and ulceration with IOM use. F-ERGS can be recorded from skin with subcutaneous needles or skin disc electrodes placed at the center of the right lower lid proximal to the lid margin (infraorbital notch), and referenced to an electrode 2 cm lateral to the lateral canthus where the largest amplitudes of ERG responses from skin can be obtained [75, 76]. Esakowitz et al. [77] compared the relative amplitudes of F-ERG b-wave responses when recording with corneal versus other electrode types placed on the skin. The largest response amplitudes were obtained with the Burian Allen electrode (125 uV, 100 %), with other corneal electrodes yielding responses of less amplitude in proportion to those made with the Burien Allen electrode: JET (93 %), C-glide (78 %), gold foil (60 %), and DTL (60 %). Recordings from skin electrodes yielded the smallest response amplitudes (14 %). Obviously, one has to weigh the risks and benefits of the use of these devices for recording F-ERGs [77]. F-ERGs recorded with noncorneal versus corneal electrodes, except for amplitude differences, are nearly identical in both time (a- and b-wave latencies) and frequency domains (dominant power spectrum peaks), meaning noncorneal F-ERGs do not differ significantly from corneal ERGs aside from amplitude [78].
One intriguing way to record F-ERGs was recently reported by Houlden et al. [3]. In their small sample of study patients (N = 12), they were able to reliably record F-ERGs from EEG electrodes placed at Fz′ (2 cm behind Fz) and referenced to FPz (10–20 International EEG placement) to confirm retinal stimulation in the patients (N = 12) evaluated in their study. Though a novel and appealing recording methodology for F-ERGs, further studies are needed in larger patient populations to confirm its feasibility and utility for IOM.
For F-VEPs, standard subdural needle or surface EEG electrodes may be used to record scalp responses [73]. Ota et al. [29] reported that F-VEPs acquired with subdural electrodes better reflect cortical activity since they have considerably greater spatial resolution and amplitude when compared to responses acquired from surface EEG electrodes placed on the scalp. Single-channel response recordings are acquired using the 10–20 International nomenclature for the placement of EEG electrodes with electrodes typically placed at the midline occipital (5 cm above inion) to midline frontal (MQ-MF or Oz-Fz) positions. The AEEGS guidelines [73] recommend a second channel be recorded for signal confirmation (however, few studies employ them). When used, the secondary set of electrodes would be placed at midline occipital and referenced to linked earlobes (MQ-Ipsilateral Earlobe (AI)/Contralateral Earlobe (A2) or Oz-AI/A2) locations. Typically the ground electrode is placed at CZ. Additional channels may be used to study the scalp distribution of VEPs [73].
Analysis Periods for F-ERGs and F-VEPs
The AEEGS guidelines recommend the use of analysis periods of 100–200 ms for F-ERG [79] and 250–500 ms for F-VEP [73]. A total of 50–200 responses are commonly recorded per average [73], with the caveat that the number per average should remain constant throughout the monitoring period. At least two consecutive ERG and VEP averages should be acquired to confirm the reproducibility of the ERG and VEP waveforms after setup and prior to surgical incision to establish a baseline (control) recording [23, 73].
Amplifier Settings for Recording F-ERG and F-VEP
For years the standard “clinical diagnostic settings” for system bandpass settings for F-VEPs have also been employed for IOM purposes, which are 1 to 200–300 Hz (−3 dB) with filter roll-off slopes not exceeding 12 dB/octave for low frequencies and 24 dB/octave for high frequencies. If irreducible artifacts occurred, filter settings could be adjusted to 5–100 Hz. Digital smoothing and filtering could also be employed to reduce artifact, and filter settings should remain constant throughout the monitoring session [73].
Houlden et al. [3] recently suggested that the difficulties in recording F-VEPs in IOM settings may be due to the high mean alpha EEG amplitudes (>50 μV) in patients, contributing “noise” that impedes recording the F-VEP “signal.” For 9 of 12 patients with low mean alpha EEG amplitudes (<30 μV), IOM F-VEPs were reproducible, including one whose vision was limited to finger counting. To improve the recording of responses in three patients with high mean alpha amplitudes (>50 μV), Houlden et al. [3] elected to see if raising the low pass settings had any effect. In these patients, they simultaneously recorded EEG from Oz–Fz and Fz–Fpz′ using 3-, 10-, and 30-Hz low cut filters (six independent recording channels) and two channels of F-VEP using low cut filters settings of 10 and 30 Hz. They found that F-VEP amplitude reductions were minimal for low pass filter settings of 3–10 Hz but at 30 Hz, the F-VEP’s N1–P1 amplitude decreased by about 40 % and its morphology was significantly altered. They also found that as the low pass filter setting increased, the “noise” contribution to the averaged F-VEP associated with electrocautery blocking time was also reduced. Based on those findings, Houlden et al. recommended using 15–20 Hz as a low pass filter setting for F-VEP responses. Houlden et al. points out that over 30 years ago, Nuwer and Dawson [80] recommended increasing the low cut filter settings from 1 to 30 Hz to improve intraoperative somatosensory-evoked potential (SSEP) reproducibility, but at the time, did not offer any reasons why the change improved the SSEP response. Houlden et al. [3] suggested that the improvement was due to reduction from the averaged response of the patient’s alpha EEG and artifact due to electrocautery amplifier blocking . Though it seems a simple enough change to implement, only one recent study, by Kamio et al. [20], has employed a higher low bandpass setting (20 Hz) during recordings of F-VEP. Hopefully others will take the opportunity to test Houlden et al.’s hypotheses and determine whether indeed raising the low pass filter setting improves the reproducibility of F-VEP responses in IOM settings.
Monitoring Criteria
Given the documented variability of flash VEPs, responses recorded from patients in operative settings cannot be universally characterized [73]. That and perhaps the technical difficulties associated with obtaining reproducible F-VEPs in operative settings have contributed a lack of clear guidelines for warning criteria to be used during surgery to preserve the visual pathway. For recent neurosurgical procedures involving removal of intraorbital, parasellar, and cortical lesions, Kodama et al. [23] and Sasaki et al. [24, 25] have used a warning criterion whereby a F-VEP amplitude decrease >50 % from baseline control levels prompted cessation of the surgical procedure until recovery of the F-VEP occurred and provided that other factors (e.g., anesthesia, use of bipolar cautery) could not be used to explain the amplitude changes. Martinez Piñeiro et al. [81] reported on monitoring patients undergoing endovascular treatment of their occipital arteriovenous malformations (AVM) with F-VEPs. He reported successful intraoperative recordings and postoperative outcomes employing the same stimulation methods and parameters that Kodama et al. [23] and Sasaki et al. [24, 25] used as well as their warning criteria. On the other hand, Kamio et al. [20], who examined the use of F-VEPs for patients undergoing transphenoidal surgery for tumor removal, employed a warning criterion of either an increased or decreased amplitude of greater than 50 % compared to control levels. In a study utilizing a similar study population, Chacko et al. [40] used a complete loss of visual responses as the warning criteria to halt surgery until responses returned to baseline. Hussain et al. [44], reporting on the use of monitoring F-VEPs from five patients undergoing functional endoscopic sinus surgery, was the only study involving the anterior visual pathway to employ an increase in F-VEP P100 latency as an indicator of optic nerve compression. They noted that for this criterion to be useful for IOM, the patient’s intraoperative diastolic blood pressure had to remain higher than 50 mmHg, oxygen saturations 98 % or higher, and bleeding to be minimized. Given the notable disparity of F-VEP IOM warning criteria in the previously discussed studies, it is clear that more research is needed to better define IOM F-VEP warning criteria that better correlate with patient outcomes.
Regarding warning criteria for studies utilizing F-ERGs for monitoring, Padalino et al. [21] used them to monitor retinal perfusion during a single case involving endovascular treatment of a dural AVM supplied by the bilateral superficial temporal, ophthalmic, and the right middle meningeal arteries. The intraoperative monitoring warning criteria that they employed was a 10-ms increase in the F-ERG latency and a 30 % decrease in its amplitude compared with baseline and control responses from the other eye. As with the warning criteria for F-VEPs during IOM, further study is needed to define and confirm warning criteria for use of F-ERGs for IOM.
Other IOM Applications with F-ERG and F-VEP
Keenan et al., Burrows et al., and Reilly et al. [11, 82, 83] have explored the F-VEP as an objective measure of the short-term effects of various cardiopulmonary procedures on neurophysiological function given the cortex’s sensitivity to small changes in cerebral perfusion due to its proximity to the watershed area of the posterior and middle cerebral arteries. Reilly et al. [83] showed that F-VEPs are a more sensitive indicator of central nervous system (CNS) stress provoked by combined hypothermia and hypoxia than EEG. Burrows et al. [11] found F-VEPs to be an objective measure of neurophysiologic function in the visual pathway during profound hypothermic circulatory arrest (PHCA) in neonates and infants undergoing surgical correction of congenital heart defects . Although their findings seemed promising as an IOM tool for such cases, Markand et al. [84] found VEPs to be too inconsistent during the surgical course of hypothermia and recovery; and that their disappearance at temperatures below 25 °C made them less than ideal for monitoring brain function during hypothermia. Even Burrows and Bissonnette [85] appear to have abandoned the use of F-VEPs for this application, opting instead to use other measures of cerebral blood flow (transcranial Doppler sonography) for monitoring perfusion during CPB surgery in their subsequent study.
However, the use of F-ERGs to monitor cardiac surgery and extracorpeal circulation may serve as a new area to consider for IOM purposes. Indeed, monitoring the retina as an extension of the brain for such cases has been encouraged by Nenekidis et al. [86]. They believed that better quantification of the hemodynamic state of retina–optic nerve head (ONH) during on-pump CPB, is needed, stating that, “The retina provides a ‘window’ for the study of cerebral microcirculation; it lies in the territory of the internal carotid artery and has a blood barrier analogous to the blood–brain barrier. It would seem reasonable to assume that the changes observed in the retinal microcirculation also occur in brain. The central nervous system can suffer from the same pathophysiological entities that affect the retina and the ONH during hypothermic CPB procedures.” During CPB procedures , retinal ischemia and infarction due to emboli, anterior ischemic optic neuropathy (AION) , posterior ischemic optic neuropathy (PION) , damage of nerve fibers, chorioretinal hypoperfusion and hypoxia secondary to hemodynamic and hematologic changes have resulted in profound visual deficits and other neuro-ophthalmological complications [86]. Because F-ERG responses are sensitive to (1) alteration of blood flow as a consequence of the reduction of perfusion pressure and (2) to body hypothermia, associated with hemodilution, which helps to depress neural function and neural tissue oxygen requirements, but may also bring on tissue hypoxia, it stands to reason that focus be given to the use of F-ERGs as a tool to monitor patients undergoing cardiosurgical procedures with CPB. A recent, intriguing recent paper by Brandli and Stone [87], while not directly related to intraoperative monitoring and performed in rats, suggests that F-ERGs are indeed sensitive to ischemia, even when the induced ischemia is remote to the retina. A pilot study done by Nebbioso et al. [57] examined the use of F-ERGs for monitoring patients during extracorporeal circulation (ECC) , both hypothermic and normothermic with some promising results. Under hypothermic ECC, they reported that the amplitude of the F-ERG response decreased by 50 % while those under normothermic ECC only decreased 10 %. Recovery of response amplitudes to baseline levels occurred upon the end of ECC and with the rewarming of the patient, with the exception of one individual whose F-ERG response recovery was very prolonged. That patient required postoperative ventilatory support and a long stay in the intensive care unit [57]. Time and further studies will tell whether use of F-ERGs will become a useful tool for monitoring and maintaining adequate retinal as well as cerebral microcirculation and perfusion during surgical procedures.
Retinal Stimulation and Intracranial Recording of Responses
Recording directly from cortical structures for lesions of the visual pathways, though feasible (albeit in studies with relatively small sample sizes), has limited utility but has yielded responses with greater amplitudes and better signal-to-noise ratio [45]. Møller et al. [88] recorded compound action potentials directly from optic nerve (ONEP) elicited by short light flashes via LEDs during tumor resection in two patients and was able to record responses that had an initial small positive deflection, with a latency of about 45 ms, followed by a negative wave with a latency of 60–70 ms, although considerable individual variation in the shape and size of those responses was observed [88].
In another application of this type of recording, Curatolo et al. [89] found that monitoring the responses recorded from the visual cortex during photic stimulation proved to be a reliable technique for preserving central vision during occipital lobe surgery [89]. Ota et al. also evaluated the usefulness of cortically recorded VEPs as an IOM tool of the posterior visual pathway in 17 patients who underwent posterior craniotomy for lesions or epileptic foci in the parietal, posterior temporal, and/or occipital lobes; reporting detection of VEPs in over 90 % of cases with preserved vision that was independent of the type of anesthesia employed for those procedures [29].
In still another application of this type of recording, photic stimulation while recording averaged visual responses in the optic tract during pallidotomy and deep brain stereotaxic surgery has been reported to be useful in guiding those surgeries [16, 59]. Such recordings have also been useful in determining the generators for scalp-derived VEP responses. Tobimatsu et al. [90] was able to record VEPs using pattern-reversal stimuli in eight awake patients with Parkinson’s disease undergoing stereotactic pallidotomy using a depth recording electrode located at or below the stereotactic target in the ventral part of the GPi and dorsal to the optic tract. They simultaneously recorded VEPs from the scalp to provide information for differentiation of the generators of the scalp VEP components. In such cases where little or no anesthesia is used during surgery, the option to use pattern reversal and other visual stimuli that provide more information in visual pathway function (e.g., visual acuity), may open up a new era for using VEPs for monitoring purposes. Indeed, their use during other “awake” procedures (e.g., endovascular stenting and coiling procedures) when visual function is at risk, has yet to be fully explored.
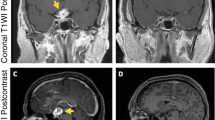
Direct Electrical Stimulation of Optic Nerve
Bošnjak and Benedičič [14, 15, 50] evaluated the feasibility and utility of recording scalp VEP responses to direct electrical stimulation (eVEP) of the ON during tumor removal surgery involving the anterior visual optic pathways [14], skull base [15], and during orbital enucleation due to malignant melanoma of the choroid or the ciliary body [91]. To acquire cortical potentials elicited by electrical epidural stimulation of the optic nerve (ON), insulated platinum needle-stimulating electrodes with a noninsulated ball tip were attached epidurally to both sides of the ON. Bošnjak et al. [50] used the following procedure for placement of these electrodes, noting that “When the exit of the optic nerve (ON) from the periorbit is fully visualized through a small fenestration of the orbital apex, needle electrodes are placed in contact on each side of the ON into the cleft between the nerve itself and the basal remnants of the lateral walls of the optic canal. The needles are manipulated during positioning with bipolar forceps through grip connectors. After placing the epidural stimulating electrodes , their position is secured with wet cotton patties laid over the orbital apex and leads.” Monopolar optic nerve potentials after retinal flash or electrical epidural stimulation of the ON were then recorded with insulated platinum ball-tipped wire electrodes placed on the surface of the ON using an extracephalic reference electrode. The distance between the stimulating and recording electrodes was approximately 25 mm. The same recording electrodes were used for monopolar recordings from structures outside of the visual pathway to collect control data. The electrical stimulus consisted of a rectangular current pulse of varying intensity (0.2–5.0 mA) and duration (0.1–0.3 ms) using a stimulation rate of 2 Hz [14, 15]. The bandpass filter settings utilized in previous studies were 1–1000 Hz when recording these cortical potentials after electrical epidural stimulation of the ON. The analysis time used was between 10 and 300 ms. Each trace was generated from the average of 100 responses. Of note, considerable stimulus-related artifact from direct ON stimulation does present a technical hurdle to recording these potentials [14, 15]. Using this stimulation and recording technique, Benedičič and Bošnjak [14, 15] concluded that it was beneficial in preventing ON damage and improving outcomes. They did not report any warning criteria used in the studies and their sample sizes were small [4]. The typical eVEP they recorded consisted of N20 and N40 waves (Fig. 4.3) [50]. Considerable variability in the amplitude of the responses was observed (e.g., N40 wave amplitudes prior to tumor removal varied as much as 25 %). Not surprisingly, artifact was observed with use of bipolar coagulation, ultrasonic aspirator, laser, and craniotome-hampered IOM [15]. In one patient with an ON sheath meningioma and vision limited to light sensation, only the N20 wave was observed (see Fig. 4.3) [50]. In their subsequent report of IOM monitoring for a very small sample (N = 3) of patients undergoing orbital enucleation due to malignant melanoma of the choroid or the ciliary body, both F-VEPS and cortical potentials from direct stimulation of the optic nerve were inconsistent or absent in patients with a history (>3 months) of severe visual deterioration, but obtainable from a single patient with a short history of mild visual impairment [91]. Clearly, more studies are needed to confirm the utility of direct electrical stimulation of the optic nerve for visual pathway IOM use and for the development of effective preoperative criteria for patients in whom these techniques may be useful, as well as warning criteria that correlates with and improves patient outcomes.
(a) An example of a typical electrically elicited visual-evoked potential (eVEP) response is depicted. The response consists of a larger N20 wave and a smaller N40 wave. The stimulus duration was 0.5 ms, and its frequency 2 Hz. An average of 100 responses was obtained. (b) The eVEP responses recorded from a patient with an optic nerve sheath meningioma and visual perception of light only is shown for which a decreased N20 wave and absent N40 wave are observed (from Bošnjak and Benedičič [50]; with permission)
Duffau et al. [13] described the use of intraoperative electrical stimulations (IES) during surgery to help identify and preserve afferent visual fibers during removal of a low-grade glioma invading the whole temporal lobe and temporo-occipital junction. They used a 5-mm spaced bipolar electrode to deliver biphasic current stimuli (pulse frequency of 60 Hz, single-pulse duration of 1 ms, and amplitude of 5 mA) to cortex involving the optic tracts, in a nonsedated patient, to guide tumor removal. By mapping the optic radiations using this electrical stimulation and obtaining the patient’s report of visual effects related to that stimulation, they were able to detect the posterior and deep functional boundary of the tumor resection, and to avoid production of a postoperative symptomatic homonymous hemianopsia. Given the incidence of visual field defects following surgeries involving the posterior temporal lobe and temporo-parieto-occipital junction (TPOJ) with considerable risk for the occurrence of permanent homonymous hemianopsia, it may be of great interest for surgeons and IOM practitioners to consider conducting further research in the application of this direct electrical stimulation technique to help preserve visual function and improve patient outcomes for those undergoing such procedures [13].
Effects of Temperature
In conscious humans, F-VEP latency is 10–20 % longer at 33 °C than at 37 °C. With increasing hypothermia, progressive increases in F-VEP latency and decreases in F-VEP amplitude occur with complete loss of the components of the responses at 25–27 °C. When cooling occurred more swiftly, F-VEP responses disappeared at higher temperatures than when a slower cooling process was utilized [92].
Effects of Anesthesia on F-ERGs
Although for IOM purposes, F-ERG responses are most frequently being employed for confirmation of stimulation of the retina, gaining an understanding of the reported effects of anesthetic and sedative agents on retinal responses, and conducting additional studies to further elucidate the effects of these agents on retina physiology, is of interest.
Wongpichedchai et al. [93] evaluated the effects of halothane in a pediatric population, on dark-adapted (scotopic) and light-adapted (photopic) F-ERGs and found it had little effect on the a-wave and b-wave latency and amplitude of the scotopic F-ERG and amplitudes and latencies of the F-ERG photopic responses to red flashes and 30 Hz flickering white light. In another study, Tremblay et al. [66] retrospectively compared the effects of sedatives and inhalational agents on scotopic and photopic F-ERGs in a small sample of pediatric patients diagnosed free of retinal disease. In that study, F-ERGs were recorded in subjects who either were (1) conscious (no anesthetic or sedative medications) [n = 9]; (2) under sedation (chloral hydrate [75–125 mg/kg] and pentobarbital sodium sedation [5–6 mg/kg]) (n = 9); or (3) under general anesthesia (intravenous injection of propofol [2 mg/kg] with or without fentanyl 4 μg/kg, and maintained with isoflurane 2–3 % or halothane 1–2.4 % with 50 % O2 and 50 % N2O [n = 9]). They found that sedation appeared to decrease a- and b-wave amplitudes of the scotopic bright-flash F-ERG responses, without affecting the responses’ latencies. Though Tremblay et al. [66] reported that F-ERG responses recorded under photopic conditions showed minimal changes in latencies and amplitudes, if one examines the table provided in the paper [66] (Table 4.1), it appears that while the amplitude of the responses are not affected, the latencies of the photopic responses recorded under anesthesia versus consciousness are significantly and statistically increased and that the same holds true for F-ERG responses recorded under sedation versus under anesthesia [66].
Early studies by Raitta et al. [94] evaluated F-ERG responses recorded in ten adults before and 15–20 min after induction of anesthesia with a combination of thiopentone sodium, halothane, and nitrous oxide (N2O) and found that the amplitudes of F-ERG a- and b-waves were significantly decreased when compared with preoperative levels, but that latencies were unchanged. The findings of a study by Yagi et al. [52] evaluated the effects of enflurane on F-ERG in a small sample of patients undergoing surgical procedures and found that use of enflurane significantly increased latencies of F-ERG a-waves and b-waves and decreased their amplitudes but did not have any significant effects on F-ERG b-wave responses, with increasing concentrations of enflurane (0, 0.8, and 1.7 %) [52]. Interestingly, a study conducted by Ioholm et al. [95] in adult populations examined photopic F-ERGs before and after surgery under general anesthesia induced with sevoflurane (8 %) in 100 % oxygen (O2) and maintained with sevoflurane (range, 0.05–0.31 %, mean 0.22 ± 0.07 %) and nitrous oxide (mixture of 33 % O2 and 66 % N2O). The F-ERG responses were recorded preoperatively from unpremedicated American Society of Anesthesiologist (ASA) classification I and II patients, and again immediately following discharge from the recovery room, and 24 h following sevoflurane/N2O anesthesia. Ioholm et al. [95] found that the F-ERG b-wave latency in these subjects was increased at both postoperative time points compared with preoperative responses and that b-wave amplitudes were also decreased postoperatively compared with their preoperative levels. Similar findings were obtained in a subsequent study conducted by Ioholm [96]. Of interest, Sasaki et al. [24] reported that “after induction of inhalation anesthesia with sevoflurane, ERG data were not reproducible” [24]. An example of the comparison of the F-ERG responses obtained by Sasaki et al. [24] with anesthesia employing sevoflurane versus total intravenous infusion of propofol with fentanyl is shown in Fig. 4.4. Given the variance in the reports regarding the effects on F-ERG responses to different combinations of sedative and halogenated agents, one would have to agree with Tremblay’s conclusion that normal retinal physiology is affected by sedation and anesthesia through different mechanisms that remain to be fully elucidated by future research [66].
Illustrates the reproducibility of ERG and VEP following induction of inhalation and venous anesthesia in the same patient, same eye (without visual dysfunction). F-ERG and VEPs were obtained twice to confirm the reproducibility of the data in the absence of surgical procedures. Following induction with inhalation anesthesia (left), F-ERG responses were not reproducible and the VEP amplitude was also affected. Conversely, following induction of propofol-based infusion anesthesia, reproducibility of ERG and VEPs were both good (from Sasaki et al. [24] with spelling modifications: revised “Seboflurene” to “Sevoflurane”; with permission)
Total intravenous anesthesia (TIVA) utilizing propofol and opioid medication is touted as F-ERG friendly. Indeed F-ERGs obtained from 20 normal children undergoing evaluations of their visual function under anesthesia with propofol and fentanyl versus topical anesthesia showed that F-ERG b-wave response latencies were only slightly increased and b-wave amplitudes decreased when propofol and fentanyl versus topical anesthesia were employed and were not statistically different [97]. This finding was further supported by an animal study conducted in pigs [98]. Although no specific reports have been published on the effects of bolus administrations of fentanyl or other opioids on F-ERGs in humans during surgery, bolus administrations (additional injections of fentanyl every 60 min) were used in Sasaki’s et al. study [24], with what can presumed to be little detriment to their use of F-ERG responses (chiefly to ensure retinal stimulation) for IOM purposes.
Effects of Anesthesia on VEPs
A summary of the effects of anesthesia on F-VEPS prepared by Banoub et al. is shown in Table 4.2 [1]. F-VEPs are very sensitive to the effects of anesthetics and physiologic factors because they represent polysynaptic cortical activity. Because flash stimulation activates both temporal and nasal parts of the retina and the nasal fibers cross to the contralateral side at the level of the optic chiasma, retrochiasmatic lesions cannot be monitored [33]. In addition, VEPs are highly dependent on appropriate stimulation of the retina and may be unduly affected by narcotic-induced pupillary constriction [99].
The findings included in Table 4.1 suggest volatile anesthetics prolong VEP latency and decrease F-VEP amplitudes in a dose-dependent fashion. Nakagawa et al. [37] found that even at a 1 % (0.5 minimum alveolar concentration [MAC] ) concentration of sevoflurane, responses were significantly decreased. At 1.5 MAC, responses could not be interpreted [37]. However, as mentioned previously, conflicting information about the effect of low-dose sevoflurane on F-VEP responses have been reported, with one researcher finding amplitude decreases with its use [37] while another did not find any such decrease [29], although the latter recorded responses directly from cortex and those responses are reportedly not as susceptible to the effects of inhalational agents as those recorded from scalp [45, 88]. Nitrous oxide (N2O) alone considerably reduces VEP amplitude. Its use in addition to volatile anesthetics can make VEP responses unrecordable. Increased concentrations of nitrous oxide significantly increase VEP latencies.
In general, it appears that opioid and ketamine or propofol-based anesthetic techniques (TIVA), along with those employing low-dose volatile anesthetics without nitrous oxide, seem to facilitate intraoperative recording of VEPs but do not ensure it. In some cases, the use of these anesthetic protocols may involve a high incidence of false-positive and false-negative results [33].
Opioids (e.g., fentanyl, alfentanil, sufentanil, and remifentanil) reportedly have a very mild effect on other evoked responses [100], which presumably extend to VEP responses. However, it is important to keep in mind that bolus administration of opioids has been reported to significantly reduce the amplitude of scalp-recorded responses [101]. Chi et al. [99] studied the effects of incremental doses of fentanyl (10 μg/kg) given every 10 min for a total dose of 60–90 μg/kg for patients undergoing coronary artery bypass graft procedures and observed that while fentanyl administration did not affect latency, amplitude was decreased. They posited that those decreases may be due to changes to retinal luminance related to pupillary-induced constriction associated with fentanyl bolus administration [99]. Accordingly, bolus administraton of fentanyl, while not precluded during such surgeries, may indirectly affect F-VEP responses induced by retinal flash stimulation, and therefore should be taken into account if responses change post-administration. Loughnan et al. [100] showed that neither fentanyl, 200 μg, nor diazepam, 20 mg administered intravenously, significantly changed F-VEP latency or amplitude, suggesting that an anesthetic technique based on these two drugs might be suitable when intraoperative evoked potential monitoring is required to assess ischemia and preservation of visual-evoked responses [100].
With respect to anesthetic techniques that employ infusion of propofol , although most of the new studies for visual pathway IOM espouse the use of propofol, Neuloh [45] points out that TIVA alone cannot ensure success, as one recent study found that “a satisfactory rate of successful VEPs could not be achieved despite use of TIVA for anesthetic management” [41]. Moreover, a couple of studies have found that the amplitude of VEP is strongly affected by the concentration of propofol and that caution and perhaps further studies are needed in evaluating VEP in patients undergoing propofol anesthesia. Nakagawa et al. [37] found that at a propofol concentration of 3.0 μg/mL (80–100 μg/kg/min), VEP amplitudes were decreased significantly compared with the amplitude at 1.5 μg/mL concentration (40–50 μg/kg/min). It led him to conclude that a propofol-based TIVA technique appears to induce less change in evoked potentials, including VEP, than halogenated agents [37]. Hamaguchi et al. [36] further investigated the influence of propofol concentration on F-VEP components in three patients with cranial aneurysm and four with brain tumor. Anesthesia was maintained with intravenous propofol using target controlled infusion. Changes in F-VEP amplitude and latency were measured during three propofol concentrations (effect site concentrations of 1.5, 2.0, and 3.0 μg × mL−1, and correlated with bispectral index (BIS) readings at each concentration. At 3.0 μg × mL−1 propofol concentration, F-VEP amplitude was decreased significantly compared with the amplitude at 1.5 μg × mL−1 concentration. No significant change was observed with the latency of F-VEP. The value of BIS at 3.0 μg × mL−1 propofol concentration also decreased significantly compared with 2.0 μg × mL−1 concentration.
Thankfully, neuromuscular blocking drugs do not directly influence F-VEP responses. In fact, their use may contribute to an improved signal-to-noise ratio by eliminating electromyographic artifact [12].
Conclusion
A number of researchers [2, 3, 13–15, 19–21, 23, 25, 78, 79] have continued their efforts to overcome the poor reputation that IOM of the visual pathways has had for several decades. By employing new and brighter stimuli, direct cortical stimulation methods, and monitoring new types of cases, these researchers hope to spawn revitalization of research that will help evaluate, establish, and improve the usefulness of visual pathway intraoperative monitoring. Certainly, the success of Sasaki et al. [24, 25] (93.5 %), Kodama et al. [23] (97 %), and subsequent research [19, 20] for acquisition of stable scalp F-VEPs recordings during surgeries involving the anterior pathways, with good correlation of monitoring results and visual outcomes, have been encouraging. Their ability to achieve those goals has largely been attributed to the combined use of (1) a brighter reusable (sterilizable); (2) flexible LED stimulating devices that guarantee supramaximal retinal stimulation, even when VEPs cannot be recorded; and (3) use of TIVA with propofol to minimize the effects of anesthetics on the responses. However, monitoring of patients with preoperative visual deficits remains controversial. Indeed, Kodama et al. limited their monitoring to patients with preoperative acuities of less than 0.4 (20/50) [23]. Because impaired preoperative vision is a major predictor of postoperative deterioration [45], eliminating such patients from monitoring limits the broad usefulness of VEPs for IOM of these surgical procedures. Regarding enhancements in anesthetic management, it is still not clear that the use of TIVA with propofol ensures F-VEP recording in all patients [41]. Still, there clearly is a need for continuous monitoring during cases involving the visual pathways, and indeed studies indicating that they were able to detect ischemic response changes in the F-VEP that would have been missed by imaging data [58] make a compelling argument to encourage those who would continue efforts to optimize the methodologies for use of VEPs for IOM purposes. Certainly, replication of their protocols and confirmation of their results will help solidify their methods. Only time will tell if others take up that cause [5, 45]. The development of visual stimulation methodologies that can better assess visual acuity during surgical procedures, coupled with improved anesthetic management techniques may serve to revitalize the efforts to confirm the usefulness of IOM of the visual pathways: a plea that was issued years ago and still remains true [73].
References
Banoub M, Tetzlaff JE, Schubert A. Pharmacologic and physiologic influences affecting sensory evoked potentials: implications for perioperative monitoring. Anesthesiology. 2003;99:716.
Luo Y, Regli L, Bozinov O, Sarnthein J. Clinical utility and limitations of intraoperative monitoring of visual evoked potentials. PLoS One. 2015;10(3):e0120525.
Houlden DA, Turgeon CA, Polis T, Sinclair J, Coupland S, Bourque P, et al. Intraoperative flash VEPs are reproducible in the presence of low amplitude EEG. J Clin Monit Comput. 2014;28:275–85.
Duffau H. Intraoperative monitoring of visual function. Acta Neurochir (Wien). 2011;153:1929–30.
Wright JE, Arden G, Jones BR. Continuous monitoring of the visually evoked response during intra-orbital surgery. Trans Ophthalmol Soc U K. 1973;93:311–4.
Handel N, Law J, Hoehn R, Kirsch W. Monitoring visual evoked response during craniofacial surgery. Ann Plast Surg. 1979;2:257–8.
Allen A, Starr A, Nudleman K. Assessment of sensory function in the operating room utilizing cerebral evoked potentials: a study of fifty-six surgically anesthetized patients. Clin Neurosurg. 1981;28:457–81.
Grundy BL. Intraoperative monitoring of sensory-evoked potentials. Anesthesiology. 1983;58:72–87.
Albright AL, Sclabassi RJ. Cavitron ultrasonic surgical aspirator and visual evoked potential monitoring for chiasmal gliomas in children. Report of two cases. J Neurosurg. 1985;63:138–40.
Costa e Silva I, Wang AD, Symon L. The application of flash visual evoked potentials during operations on the anterior visual pathways. Neurol Res. 1985;7:11–6.
Burrows FA, Hillier SC, McLeod ME, Iron KS, Taylor MJ. Anterior fontanel pressure and visual evoked potentials in neonates and infants undergoing profound hypothermic circulatory arrest. Anesthesiology. 1990;73:632–6.
Sloan TB. Evoked potential monitoring. Int Anesthesiol Clin. 1996;34:109–36.
Duffau H, Velut S, Mitchell M-C, Gatignol P, Capelle L. Intra-operative mapping of the subcortical visual pathways using direct electrical stimulations. Acta Neurochir (Wien). 2004;146:265–9. discussion 269–70.
Benedičič M, Bošnjak R. Optic nerve potentials and cortical potentials after stimulation of the anterior visual pathway during neurosurgery. Doc Ophthalmol Adv Ophthalmol. 2011;122:115–25.
Benedičič M, Bošnjak R. Intraoperative monitoring of the visual function using cortical potentials after electrical epidural stimulation of the optic nerve. Acta Neurochir (Wien). 2011;153:1919–27.
Landi A, Pirillo D, Cilia R, Antonini A, Sganzerla EP. Cortical visual evoked potentials recorded after optic tract near field stimulation during GPi-DBS in non-cooperative patients. Clin Neurol Neurosurg. 2011;113:119–22.
San-Juan D, de Dios Del Castillo CJ, Villegas TG, Elizondo DL, Torrontegui JAF, Anschel DJ. Visual intraoperative monitoring of occipital arteriovenous malformation surgery. Clin Neurol Neurosurg. 2011;113:680–2.
Chung SB, Park CW, Seo DW, Kong DS, Park SK. Intraoperative visual evoked potential has no association with postoperative visual outcomes in transsphenoidal surgery. Acta Neurochir (Wien). 2012;154:1505–10.
Ogawa Y, Nakagawa A, Washio T, Arafune T, Tominaga T. Tissue dissection before direct manipulation to the pathology with pulsed laser-induced liquid jet system in skull base surgery: preservation of fine vessels and maintained optic nerve function. Acta Neurochir (Wien). 2013;155:1879–86.
Kamio Y, Sakai N, Sameshima T, Takahashi G, Koizumi S, Sugiyama K, et al. Usefulness of intraoperative monitoring of visual evoked potentials in transsphenoidal surgery. Neurol Med Chir (Tokyo). 2014;54:606–11.
Padalino DJ, Melnyk V, Allott G, Deshaies EM. Electroretinography during embolization of an ophthalmic arteriovenous fistula. Surg Neurol Int. 2013;4:40.
Goto T, Tanaka Y, Kodama K, Kusano Y, Sakai K, Hongo K. Loss of visual evoked potential following temporary occlusion of the superior hypophyseal artery during aneurysm clip placement surgery. J Neurosurg Pediatr. 2007;107:865–7.
Kodama K, Goto T, Sato A, Sakai K, Tanaka Y, Hongo K. Standard and limitation of intraoperative monitoring of the visual evoked potential. Acta Neurochir (Wien). 2010;152:643–8.
Sasaki T, Itakura T, Suzuki K, Kasuya H, Munakata R, Muramatsu H, et al. Intraoperative monitoring of visual evoked potential: introduction of a clinically useful method. J Neurosurg. 2010;112:273–84.
Sasaki T, Ichikawa T, Sakuma J, Suzuki K, Matsumoto M, Itakura T, et al. Intraoperative monitoring of visual evoked potentials [in Japanese]. Masui. 2006;55:302–13.
Feinsod M, Selhorst JB, Hoyt WF, Wilson CB. Monitoring optic nerve function during craniotomy. J Neurosurg. 1976;44:29–31.
Herzon GD, Zealear DL. Intraoperative monitoring of the visual evoked potential during endoscopic sinus surgery. Otolaryngol Head Neck Surg. 1994;111:575–9.
Zaaroor M, Pratt H, Feinsod M, Schacham SE. Real-time monitoring of visual evoked potentials. Isr J Med Sci. 1993;29:17–22.
Ota T, Kawai K, Kamada K, Kin T, Saito N. Intraoperative monitoring of cortically recorded visual response for posterior visual pathway. J Neurosurg. 2010;112:285–94.
Wilson WB, Kirsch WM, Neville H, Stears J, Feinsod M, Lehman RA. Monitoring of visual function during parasellar surgery. Surg Neurol. 1976;5:323–9.
Koshino K, Kuroda R, Mogami H, Takimoto H. Flashing diode evoked responses for detecting optic nerve function during surgery. Med J Osaka Univ. 1978;29(1–2):39–47.
Cedzich C, Schramm J, Fahlbusch R. Are flash-evoked visual potentials useful for intraoperative monitoring of visual pathway function? Neurosurgery. 1987;21:709.
Raudzens PA. Intraoperative monitoring of evoked potentials. Ann N Y Acad Sci. 1982;388:308–26.
Cedzich C, Schramm J, Mengedoht CF, Fahlbusch R. Factors that limit the use of flash visual evoked potentials for surgical monitoring. Electroencephalogr Clin Neurophysiol. 1988;71:142–5.
Cedzich C, Schramm J. Monitoring of flash visual evoked potentials during neurosurgical operations. Int Anesthesiol Clin. 1990;28:165–9.
Hamaguchi K, Nakagawa I, Hidaka S, Uesugi F, Kubo T, Kato T. Effect of propofol on visual evoked potentials during neurosurgery. Masui. 2005;54:998–1002.
Nakagawa I, Hidaka S, Okada H, Kubo T, Okamura K, Kato T. Effects of sevoflurane and propofol on evoked potentials during neurosurgical anesthesia. Masui. 2006;55:692–8.
Nau HE, Hess W, Pohlen G, Marggraf G, Rimpel J. Evoked potentials in intracranial operations: current status and our experiences [in German]. Anaesthesist. 1987;36:116–25.
Lorenz M, Renella RR. Intraoperative monitoring: visual evoked potentials in surgery of the sellar region [in German]. Zentralbl Neurochir. 1989;50:12–5.
Chacko AG, Babu KS, Chandy MJ. Value of visual evoked potential monitoring during trans-sphenoidal pituitary surgery. Br J Neurosurg. 1996;10:275–8.
Wiedemayer H, Fauser B, Armbruster W, Gasser T, Stolke D. Visual evoked potentials for intraoperative neurophysiologic monitoring using total intravenous anesthesia. J Neurosurg Anesthesiol. 2003;15:19–24.
Wiedemayer H, Fauser B, Sandalcioglu IE, Armbruster W, Stolke D. Observations on intraoperative monitoring of visual pathways using steady-state visual evoked potentials. Eur J Anaesthesiol. 2004;21:429–33.
Bergholz R, Lehmann TN, Fritz G, Rüther K. Fourier transformed steady-state flash evoked potentials for continuous monitoring of visual pathway function. Doc Ophthalmol. 2007;116:217–29.
Hussain SS, Laljee HC, Horrocks JM, Tec H, Grace AR. Monitoring of intra-operative visual evoked potentials during functional endoscopic sinus surgery (FESS) under general anaesthesia. J Laryngol Otol. 1996;110:31–6.
Neuloh G. Time to revisit VEP monitoring? Acta Neurochir (Wien). 2010;152:649–50.
Miyake Y, Horiguchi M. Electroretinographic alterations during vitrectomy in human eyes. Graefes Arch Clin Exp Ophthalmol. 1998;236:13–7.
Miyake Y, Yagasaki K, Horiguchi M. Electroretinographic monitoring of retinal function during eye surgery. Arch Ophthalmol. 1991;109:1123–6.
Montezuma SR, Rizzo JF, Ziv OR. Combined vitrectomy lens and contact electrode for erg recording during surgery. Retina. 2002;22:828–9.
Kikuchi Y, Sasaki T, Matsumoto M, Oikawa T, Itakura T, Kodama N. Optic nerve evoked potentials elicited by electrical stimulation. Neurol Med Chir (Tokyo). 2005;45:349–55. discussion 354–5.
Bošnjak R, Benedičič M. Direct epidural electrical stimulation of the optic nerve: a new method for intraoperative assessment of function. J Neurosurg Pediatr. 2008;109:647–53.
Tashiro C, Muranishi R, Gomyo I, Mashimo T, Tomi K, Yoshiya I. Electroretinogram as a possible monitor of anesthetic depth. Graefes Arch Clin Exp Ophthalmol. 1986;224:473–6.
Yagi M, Tashiro C, Yoshiya I. Changes in the electroretinogram during enflurane anesthesia [in Japanese]. Masui. 1989;38:1438–43.
Nogawa T, Katayama K, Okuda H, Uchida M. Changes in the latency of the maximum positive peak of visual evoked potential during anesthesia. Nihon Geka Hokan. 1991;60:143–53.
Zimmerer R, Rana M, Schumann P, Gellrich N-C. Diagnosis and treatment of optic nerve trauma. Facial Plast Surg. 2014;30:518–27.
Zimmerer R, Schattmann K, Essig H, Jehn P, Metzger M, Kokemüller H, et al. Efficacy of transcutaneous transseptal orbital decompression in treating acute retrobulbar hemorrhage and a literature review. Craniomaxillofac Trauma Reconstr. 2014;7:17–26.
Zhu Y, Song G, Tang D, Zhai X, Tian W. Monitor visual function with flash visual evoked potential during orbital surgery [in Chinese]. Zhonghua Yan Ke Za Zhi. 2000;36:445–8.
Nebbioso M, Lenarduzzi F, Pucci B, Plateroti AM, Rispoli E. Surgical management by means of electroretinographic examination during extracorporeal circulation. Ann Ital Chir. 2012;83:523–8.
Kamada K, Todo T, Morita A, Masutani Y, Aoki S, Ino K, et al. Functional monitoring for visual pathway using real-time visual evoked potentials and optic-radiation tractography. Neurosurgery. 2005;57(1 Suppl):121–7.
Lozano A, Hutchison W, Kiss Z, Tasker R, Davis K, Dostrovsky J. Methods for microelectrode-guided posteroventral pallidotomy. J Neurosurg. 1996;84:194–202.
Yokoyama T, Sugiyama K, Nishizawa S, Yokota N, Ohta S, Uemura K. Visual evoked potentials during posteroventral pallidotomy for Parkinson’s disease. Neurosurgery. 1999;44:815–22. discussion 822–4.
Cohen BA, Baldwin ME. Visual-evoked potentials for intraoperative neurophysiology monitoring: another flash in the pan? J Clin Neurophysiol. 2011;28:599–601.
Thirumala PD, Habeych ME, Crammond DJ, Balzer JR. Neurophysiologic intraoperative monitoring of olfactory and optic nerves. J Clin Neurophysiol. 2011;28:538–42.
Schumann P, Kokemüller H, Tavassol F, Lindhorst D, Lemound J, Essig H, et al. Optic nerve monitoring. Craniomaxillofac Trauma Reconstr. 2013;6:75–86.
Moller A. Evoked potentials in intraoperative monitoring. New York: Williams & Wilkins; 1988.
Inui K, Sannan H, Miki K, Kaneoke Y, Kakigi R. Timing of early activity in the visual cortex as revealed by simultaneous MEG and ERG recordings. Neuroimage. 2006;30:239–44.
Tremblay F, Parkinson JE. Alteration of electroretinographic recordings when performed under sedation or halogenate anesthesia in a pediatric population. Doc Ophthalmol. 2003;107:271–9.
Holder GE. Electrophysiological assessment of optic nerve disease. Eye (Lond). 2004;18:1133–43.
Chiappa K. Evoked potential in clinical medicine. New York: Raven; 1983.
Towle VL, Cakmur R, Cao Y, Brigell M, Parmeggiani L. Locating VEP equivalent dipoles in magnetic resonance images. Int J Neurosci. 1995;80(1–4):105–16.
Nehamkin S, Windom M, Syed TU. Visual evoked potentials. Am J Electroneurodiagnostic Technol. 2008;48:233–48.
Walsh P, Kane N, Butler S. The clinical role of evoked potentials. J Neurol Neurosurg Psychiatry. 2005;76 Suppl 2:ii16–22.
Harding GF, Smith VH, Yorke HC. A contact lens photostimulator for surgical monitoring. Electroencephalogr Clin Neurophysiol. 1987;66(3):322–6.
American Electroencephalographic Society. Guidelines for intraoperative monitoring of sensory evoked potentials. J Clin Neurophysiol. 1987;4:397–416.
Kriss A, Halliday AM, Halliday E, Pratt RT. Evoked potentials following unilateral ECT. II. The flash evoked potential. Electroencephalogr Clin Neurophysiol. 1980;48:490–501.
Noonan BD, Wilkus RJ, Chatrian GE, Lettich E. The influence of direction of gaze on the human electroretinogram recorded from periorbital electrodes: a study utilizing a summating technique. Electroencephalogr Clin Neurophysiol. 1973;35:495–502.
Rubinstein MP, Harding GF. The visually evoked subcortical potential: is related to the electroretinogram? Invest Ophthalmol Vis Sci. 1981;21:335–44.
Esakowitz L, Kriss A, Shawkat F. A comparison of flash electroretinograms recorded from Burian Allen, JET, C-glide, gold foil, DTL and skin electrodes. Eye (Lond). 1993;7(Pt 1):169–71.
Gur M, Gath I. Time and frequency analysis of simultaneously recorded corneal and non-corneal electroretinogram. J Biomed Eng. 1979;1:172–4.
Hood DC, Bach M, Brigell M, Keating D, Kondo M, Lyons JS, et al. ISCEV guidelines for clinical multifocal electroretinography (2007 edition). Doc Ophthalmol. 2008;116:1–11.
Nuwer MR, Dawson EC. Intraoperative evoked potential monitoring of the spinal cord. A restricted filter, scalp method during Harrington instrumentation for scoliosis. Clin Orthop. 1984;183:42–50.
Martinez Piñeiro A, Cubells C, Garcia P, Castaño C, Dávalos A, Coll-Canti J. Implementation of intraoperative neurophysiological monitoring during endovascular procedures in the central nervous system. Interv Neurol. 2015;3:85–100.
Keenan NK, Taylor MJ, Coles JG, Prieur BJ, Burrows FA. The use of VEPs for CNS monitoring during continuous cardiopulmonary bypass and circulatory arrest. Electroencephalogr Clin Neurophysiol. 1987;68:241–6.
Reilly EL, Kondo C, Brunberg JA, Doty DB. Visual evoked potentials during hypothermia and prolonged circulatory arrest. Electroencephalogr Clin Neurophysiol. 1978;45:100–6.
Markand ON, Warren CH, Moorthy SS, Stoelting RK, King RD. Monitoring of multimodality evoked potentials during open heart surgery under hypothermia. Electroencephalogr Clin Neurophysiol. 1984;59:432–40.
Burrows FA, Bissonnette B. Cerebral blood flow velocity patterns during cardiac surgery utilizing profound hypothermia with low-flow cardiopulmonary bypass or circulatory arrest in neonates and infants. Can J Anaesth. 1993;40:298–307.
Nenekidis I, Pournaras CJ, Tsironi E, Tsilimingas N. Vision impairment during cardiac surgery and extracorporeal circulation: current understanding and the need for further investigation. Acta Ophthalmol. 2012;90:e168–72.
Brandli A, Stone J. Remote ischemia influences the responsiveness of the retina: observations in the rat. Invest Ophthalmol Vis Sci. 2014;55:2088–96.
Møller AR, Burgess JE, Sekhar LN. Recording compound action potentials from the optic nerve in man and monkeys. Electroencephalogr Clin Neurophysiol. 1987;67:549–55.
Curatolo JM, Macdonell RA, Berkovic SF, Fabinyi GC. Intraoperative monitoring to preserve central visual fields during occipital corticectomy for epilepsy. J Clin Neurosci. 2000;7:234–7.
Tobimatsu S, Shima F, Ishido K, Kato M. Visual evoked potentials in the vicinity of the optic tract during stereotactic pallidotomy. Electroencephalogr Clin Neurophysiol. 1997;104:274–9.
Benedičič M, Beltram M, Olup BD, Bošnjak R. Cortical potentials after electrical intraneural stimulation of the optic nerve during orbital enucleation. Doc Ophthalmol Adv Ophthalmol. 2012;125:195–202.
Russ W, Kling D, Loesevitz A, Hempelmann G. Effect of hypothermia on visual evoked potentials (VEP) in humans. Anesthesiology. 1984;61:207–10.
Wongpichedchai S, Hansen RM, Koka B, Gudas VM, Fulton AB. Effects of halothane on children’s electroretinograms. Ophthalmology. 1992;99:1309–12.
Raitta C, Karhunen U, Seppäläinen AM. Changes in the electroretinogram and visual evoked potentials during general anaesthesia using enflurane. Graefes Arch Clin Exp Ophthalmol. 1982;218:294–6.
Iohom G, Collins I, Murphy D, Awad I, O’Connor G, McCarthy N, et al. Postoperative changes in visual evoked potentials and cognitive function tests following sevoflurane anaesthesia. Br J Anaesth. 2001;87:855–9.
Iohom G, Whyte A, Flynn T, O’Connor G, Shorten G. Postoperative changes in the full-field electroretinogram following sevoflurane anaesthesia. Eur J Anaesthesiol. 2004;21:272–8.
Andréasson S, Tornqvist K, Ehinger B. Full-field electroretinograms during general anesthesia in normal children compared to examination with topical anesthesia. Acta Ophthalmol. 1993;71:491–5.
Tanskanen P, Kylmä T, Kommonen B, Karhunen U. Propofol influences the electroretinogram to a lesser degree than thiopentone. Acta Anaesthesiol Scand. 1996;40:480–5.
Chi OZ, McCoy CL, Field C. Effects of fentanyl anesthesia on visual evoked potentials in humans. Anesthesiology. 1987;67:827–30.
Loughnan BL, Sebel PS, Thomas D, Rutherfoord CF, Rogers H. Evoked potentials following diazepam or fentanyl. Anaesthesia. 1987;42:195–8.
Sloan T. Anesthesia and intraoperative neurophysiological monitoring in children. Childs Nerv Syst. 2009;26:227–35.
Uhl RR, Squires KC, Bruce DL, Starr A. Effect of halothane anesthesia on the human cortical visual evoked response. Anesthesiology. 1980;53:273–6.
Chi OZ, Field C. Effects of isoflurane on visual evoked potentials in humans. Anesthesiology. 1986;65:328–30.
Kameyama Y. Effect of isoflurane and sevoflurane on evoked potentials and EEG. Jpn J Anesth. 1994;43:657–64.
Sebel PS, Flynn PJ, Ingram DA. Effect of nitrous oxide on visual, auditory and somatosensory evoked potentials. Br J Anaesth. 1984;56:1403–7.
Yamashiro H. Differentiation of brain stem anesthesia from high spinal anesthesia using auditory brain stem response. Masui. 1990;39:1704–7.
Fenwick PBC, Stone SA, Bushman J, Enderby D. Changes in the pattern reversal visual evoked potential as a function of inspired nitrous oxide concentration. Electroencephalogr Clin Neurophysiol. 1984;57:178–83.
Hou WY, Lee WY, Lin SM, Liu CC, Susceto L, Sun WZ, Lin SY. The effects of ketamine, propofol and nitrous oxide on visual evoked potentials during fentanyl anesthesia. Ma Zui Xue Za Zhi. 1993;31:97–102.
Chi OZ, Ryterband S, Field C. Visual evoked potentials during thiopentone-fentanyl-nitrous oxide anaesthesia in humans. Can J Anaesth. 1989;36:637–40.
Russ W, Luben V, Hempelmann G. Der EinfluB der Neuroleptanalgesie auf das visuelle evozierte Potential (VEP) des Menschen. Anaesthesist. 1982;31:575–8.
Makela K, Harkainen K, Rorarius M, Jantti V. Suppression of F-VEP during isoflurane-induced EEG suppression. Electroencephalogr Clin Neurophysiol. 1996;100:269–72.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Toleikis, S.C., Toleikis, J.R. (2017). Visual-Evoked Potentials. In: Koht, A., Sloan, T., Toleikis, J. (eds) Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals. Springer, Cham. https://doi.org/10.1007/978-3-319-46542-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-46542-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-46540-1
Online ISBN: 978-3-319-46542-5
eBook Packages: MedicineMedicine (R0)