Abstract
Flash visual evoked potentials (FVEPs) are often irreproducible during surgery. We assessed the relationship between intraoperative FVEP reproducibility and EEG amplitude. Left then right eyes were stimulated by goggle light emitting diodes, and FVEPs were recorded from Oz–Fz′ (International 10-20 system) in 12 patients. Low cut filters were ≤5 Hz in all patients; two patients also had recordings using 10 and 30 Hz. The reproducibility of FVEP and the amplitude of the concomitant EEG from C4′–Fz were measured. Nine patients had low amplitude EEG (<30 μV); reproducible FVEPs were obtained from all eyes with normal pre-operative vision. The other three patients had high amplitude EEG (>50 μV); FVEPs were absent from three of four eyes with normal pre-operative vision (the other normal eye had a present but irreproducible FVEP). Raising the low cut filter to 10 and 30 Hz (in two patients) progressively reduced EEG and FVEP amplitude, reduced amplifier blocking time and improved FVEP reproducibility. FVEPs were more reproducible in the presence of low amplitude EEG than high amplitude EEG. This is the first report describing the effect of EEG amplitude on FVEP reproducibility during surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The use of intraoperative FVEP monitoring has fallen out of favor due to its propensity for technical failure and lack of correlation with clinical outcome [1, 2]. Inadequate stimulation of the retina (due to frontal scalp reflection) and the effect of anesthesia are considered the main causes of technical failure [3, 4]. Frontal scalp flap reflection often displaces conventional goggle stimulators so that light cannot adequately stimulate the retina, and anesthesia decreases the synaptic efficacy in the brain thereby decreasing FVEP amplitude and reproducibility. Consequently, optic nerve monitoring has been abandoned by most neuromonitoring teams despite a plea for better methodologies [1, 5, 6]. Surprisingly, noise created by high amplitude EEG has not been investigated as a cause for FVEP irreproducibility during surgery.
The American Clinical Neurophysiology Society recommends a recording bandpass of 1–100 Hz for FVEPs in the clinical setting but there are no recommendations for FVEPs during surgery [7, 8]. Consequently, many investigators have used the clinical filter settings for intraoperative FVEP monitoring and found irreproducible FVEPs that did not predict post-operative visual acuity regardless of anesthetic regimen [inhalation anesthesia or total intravenous anesthetic (TIVA)] [1, 2]. Unfortunately, EEG was not recorded in these studies but it is likely their filter settings allowed high amplitude EEG into the recordings of many patients since EEG amplitude, containing a predominant alpha frequency (8–12 Hz), is increased when a patient is under surgical anesthesia [9–11]. This would worsen the FVEP signal to noise ratio because the noise created by EEG may be up to 120 μV while the FVEP amplitude is often less than 5 μV during surgery. Two recent studies showed high FVEP reproducibility when 10 and 20 Hz low cut filters were used, but the affect those filters had on EEG was not mentioned [12, 13].
If FVEP monitoring is to be reproducible, the potentially deleterious effects of EEG should be studied. In this observational study we related EEG amplitude (and other artifacts) to intraoperative FVEP reproducibility for the first time.
2 Materials and methods
2.1 Patient population
Twelve patients between 7 and 73 years of age (mean = 41) were studied. Ten had endonasal surgery for tumour removal near the optic nerve or chiasm, one had craniotomy for resection of an occipital lobe tumour through a brain port and the other had resection of a glial based tumour via a fronto-temporal craniotomy. Pre- and post-operative visual acuity and field deficits were tested by the ophthalmology department. Seven patients had normal pre-operative vision and extra ocular muscle function. Four patients had pre-operative visual deficits related to optic nerve compression and one of them had surgery twice. One had left opthalmoplegia but no visual acuity or field deficits (Table 1). Surgical anesthesia was maintained by TIVA (propofol/remifentanyl infusion) in all patients except two where inhalation agents (desflurane or sevoflurane), remifentanyl and occasional boluses of propofol were used. Changes in anesthetic were timed and recorded in the neuromonitoring log.
2.2 FVEP recording
Left then right eyes were stimulated by commercially available goggle light emitting diode (LED) stimulators (3 LEDs on each side, 640 nm peak wavelength, 10 ms pulse width, 3000mCd of luminous intensity reflected back on an angle to give uniform illumination across the whole lens; Cadwell Instruments, Kennewick, WA, USA) placed over closed eyelids, and recordings were obtained from corkscrew electrodes (Technomed Europe, Maastricht-Airport, Netherlands) placed at Oz–Fz′ (2 cm behind Fz). The stimulus rate was 1.41 Hz. 150 stimulus presentations were included in a single average, but fewer were included if the FVEP was readily reproducible. As this was an observational study, the low cut filter did vary a little from case to case but was always ≤5 Hz (see Table 1). The high cut filter was 100 Hz and the amplifier gain was 20,000 or 50,000. Display gain was adjusted for optimal presentation of waveforms. Total sweep time was 300 or 500 ms. FVEPs were acquired throughout surgery using a Cadwell Elite intraoperative monitoring machine (Cadwell Instruments, Kennewick, WA, USA). Reject settings were adjusted so that artifacts (i.e. electrocautery, movement artifacts) were rejected but all electrophysiological signals were accepted. The FVEP recordings, complete with stimulating/recording parameters and time of acquisition, were automatically stored to disc for later analysis. The FVEP peak-to-peak amplitude was measured from the first negative peak after 60 ms (N1) to the following positive peak (P1) provided there was no EEG amplifier blocking during the acquisition period. Two consecutive FVEPs from the same eye were superimposed to determine waveform reproducibility. The waveform was considered irreproducible when N1–P1 was ill-defined or when its amplitude decreased more than 50 % from baseline for two or more consecutive trials when there was no optic nerve manipulation.
2.3 EEG recording
EEG was continuously recorded from C4′–Fz using the same evoked potential equipment used for the FVEP. The amplifier gain was 20,000 and the recording bandpass was 1.5–100 Hz. Display gain was adjusted for optimal presentation of EEG waveforms. Sweep speed was 200 ms per division. The EEG recordings, complete with recording parameters and time of acquisition, were automatically stored to disc for later analysis. Mean peak-to-peak alpha EEG amplitude was determined for the same period of time the FVEP was acquired provided there was no EEG amplifier blocking. If mean alpha EEG amplitude was less than 30 μV then it was considered “low” amplitude and if it was greater than 50 μV it was considered “high” amplitude. A mean EEG amplitude between 30 and 50 μV was considered “moderate” amplitude.
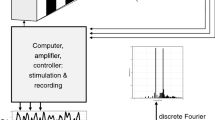
2.4 FVEP recording using multiple channels and multiple low cut filter settings
After observing the relationship between high amplitude alpha EEG and FVEP irreproducibility in one patient, the next two patients had FVEP and EEG simultaneously recorded from Oz–Fz′ and Fz′–Fpz using 3, 10 and 30 Hz low cut filters (six independent recording channels). The 10 and 30 Hz low cut filters were employed to reduce the high amplitude alpha EEG in the FVEP average (our equipment does not have a low cut filter between 10 and 30 Hz). The Fz′–Fpz channel was used to look for Fz′ contribution to the FVEP waveform. The recording equipment and all other recording parameters were the same as those described above in the FVEP and EEG recording sections.
2.5 Signal to noise ratio
For each eye, the signal to noise ratio was calculated from the mean of three consecutive FVEP N1–P1 amplitude measurements (“signal”; measured by author DH) and the mean EEG amplitude (“noise”; measured by author CT) for the same periods of time those FVEPs were acquired, provided there was no change of anesthesia and no amplifier blocking during acquisition time. The person measuring FVEP was blind to the EEG data and vice versa for the person measuring EEG.
The success rate for FVEP monitoring during low amplitude EEG was derived from the number of eyes with normal vision that had reproducible FVEPs throughout surgery (excluding FVEP averages where anesthetic deepened and/or where amplifier blocking occurred) divided by the total number of eyes tested with normal vision. This was compared to the success rate for FVEP monitoring during high amplitude EEG using the same conditions.
3 Results
3.1 Low amplitude EEG and FVEP
Nine patients had low amplitude EEG (less than 30 μV peak-to-peak amplitude) throughout surgery. Reproducible FVEPs were obtained from all eyes with normal pre-operative vision (n = 14). Reproducible FVEPs were also obtained from one of four eyes with pre-operative visual deficits (only finger counting; Table 1, patient 6). The other three eyes had absent FVEPs in 2 (20/200 acuity in one eye; only finger counting, no colour vision and temporal hemianopsia in the other) and a present but irreproducible FVEP in one (20/200 acuity, temporal hemianopsia, impaired colour vision, central scotoma). The mean FVEP signal to noise ratio was 1:4.2 ± 2.7 (range 1:0.7–1:12.5) for all eyes with reproducible FVEPs.
TIVA was used in eight of these patients and inhalation agents in one. The patient with inhalation agents had reproducible FVEPs from both eyes (normal pre-operative vision bilaterally) until there was a change in anesthetic (once after a large bolus of propofol, and again after desflurane was increased from 0.7 to 1.0 MAC combined with a bolus of remifentanyl) (Fig. 1).
Right FVEP (3–100 Hz bandpass filters) in a 70 year old woman undergoing endonasal surgery for removal of a sphenoid sinus tumour during inhalation anesthesia. 30 min of data is shown with the most recent trace displayed at the bottom. She has normal pre-operative vision. EEG is low amplitude or suppressed throughout surgery. FVEP is reproducible throughout surgery except for transient changes associated with boluses of propofol and electrocautery
Electrocautery occasionally caused FVEP amplifier blocking that rendered the sweeps electrically silent but allowed them into the FVEP average thereby diminishing FVEP amplitude (Fig. 1). All patients had transient FVEP amplitude changes that were related to amplifier blocking caused by electrocautery but these FVEP averages were excluded from analysis of success rate.
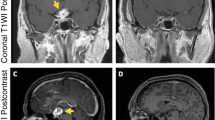
3.1.1 Illustrative case
One patient with TIVA (patient 7, Table) had surgery twice. This patient was included in the low amplitude EEG group. Pre-operatively he had bilateral visual deficits (bitemporal hemianopsia with 20/20 vision in right eye but only finger counting, no colour vision in left eye). His FVEP was reproducible after right eye stimulation and absent after left. The right FVEP signal to noise ratio was 1:0.7. At the end of surgery, as the patient’s anesthetic level lightened, the low amplitude EEG pattern was replaced by higher amplitude alpha dominant EEG pattern that was allowed into the FVEP average making the FVEP less reproducible (Fig. 2). In the second operation (not included in the FVEP success rate analysis so as not to contaminate success rate statistics) the right FVEP and EEG was concomitantly recorded from Oz–Fz′ using 3 different bandpass filters (3–100, 10–100 and 30–100 Hz) during high amplitude EEG (low signal to noise ratio) (Fig. 3). The FVEP P1 was more reproducible when the low cut filter was 10 and 30 Hz compared to that recorded with a 3 Hz low cut filter. This was accompanied by a concomitant progressive decrease in alpha EEG amplitude (~50 % decrease by the 10 Hz low cut filter and ~90 % decrease by the 30 Hz one compared to that recorded using the 3 Hz low cut filter). There was little difference between the amplitude of alpha EEG recorded from C4′–Fz compared to that recorded from Oz–Fz′ (Fig. 3).
Right FVEP (3–100 Hz bandpass filters) in an 18 year old patient undergoing endonasal surgery for removal of a craniopharyngioma during TIVA. 30 min of data is shown with the most recent trace displayed at the bottom. He has bitemporal hemianopsia (20/20 vision in right eye; only finger counting, no colour vision in left eye). P1 is reproducible (circled, top right) when EEG is low amplitude (top left panel), but is irreproducible (circled, bottom right) when EEG amplitude increases (bottom left panel) as depth of anesthesia decreases; EEG enters the FVEP average and contaminates the waveform
Effect of raising the low cut filter on right FVEP reproducibility and high amplitude EEG amplitude during TIVA. 60 min of FVEP data is shown with the most recent trace displayed at the bottom. The FVEP and EEG traces are simultaneously recorded from Oz–Fz′ using 3 independent recording channels (each with different bandpass filters) and 6 different displays (3 for FVEP and 3 for EEG). The FVEP P1 is less reproducible when the low cut filter is at 3 Hz (left panels). The FVEP is progressively more reproducible (peaks more defined but lower amplitude) and the EEG amplitude is progressively decreased when the low cut filter is raised to 10 Hz (middle panels) and 30 Hz (right panels). EEG from C4′–Fz has similar amplitude to that recorded from Oz–Fz′ (bottom two panels on left)
3.1.2 Illustrative case
Another patient with TIVA had the FVEP recorded concomitantly from Oz–Fz′ and Fz′–Fpz using the same bandpass filters (3–100, 10–100 and 30–100 Hz) during low amplitude EEG (high signal to noise ratio) (Fig. 4). The 10 Hz low cut filter had little affect on N1–P1 amplitude or N1 and P1 latency recorded from Oz–Fz′ when compared to that recorded using the 3 Hz filter. The 30 Hz low cut filter greatly reduced N1–P1 amplitude (42 and 37 % for left and right FVEP, respectively) and mildly reduced N1 and P1 latency bilaterally compared to that recorded using the 3 Hz filter. Only the electroretinogram (ERG) was recorded from Fz′–Fpz (not shown). There was no activity resembling FVEP N1–P1 (or its inverse) recorded from Fz′–Fpz.
Effect of different low cut filter settings on FVEP (recorded from Oz–Fz′) during TIVA and low amplitude EEG (very high signal to noise ratio). This 51 year old woman (normal pre-operative vision) has a left craniotomy for removal of a glial based tumour near the tentorium. The 10 Hz low cut filter (middle traces) stabilizes the FVEP but has little affect on the amplitude of the first negative peak–positive trough (P1; P1 may not be the first positive trough but it is what we consistently used to calculate N1–P1 amplitude). The 30 Hz low cut filter (lowest traces) reduces the amplitude of P1 and greatly reduces the amplitude of waveforms after 150 ms
The amount of time the amplifier was blocked after electrocautery was longest for the 3 Hz low cut filter and shortest for the 30 Hz one. The longer the amplifier was blocked (as measured from the EEG channel) the greater the decrease in all peaks of the concomitantly recorded FVEP (Fig. 5). In this case, alpha EEG amplitude from Oz–Fz′ was reduced ~50 % by the 10 Hz low cut filter and ~90 % by the 30 Hz one compared to that recorded using the 3 Hz low cut filter. There was little difference in EEG amplitude recorded from C4′–Fz compared to that recorded from Oz–Fz′.
Effect of electrocautery on amplifier recovery time (top figure; raw EEG) and FVEP (bottom 3 figures) using 3 different low cut filters. The amplifier recovery time is longest when 3–100 Hz bandpass is used. This allows flat traces into the FVEP average thereby reducing the averaged FVEP amplitude and decreasing its reproducibility (bottom left figure). In contrast, the amplifier recovery time is shortest (and FVEP most reproducible) when the 30–100 Hz bandpass is used (bottom right figure) although it decreases FVEP amplitude (note FVEP display gain is 10 μV per division for FVEP at 3–100 and 10–100 Hz compared to 5 μV per division for FVEP at 30–100 Hz). Amplifier blocking occurs more than once during averaging of the decreased FVEP (not shown). EEG is considered “low amplitude” (mean <30 μV)
3.2 High amplitude EEG and FVEP
Three patients had high amplitude alpha EEG (greater than 50 μV peak-to-peak amplitude) throughout surgery (Table 1, patients 10–12). Patient 10 had bilateral pre-operative visual deficits (20/50 in one eye and 20/600 in the other) but the other two had normal pre-operative vision bilaterally. Left/right FVEP reject windows were opened wide for all three patients to allow for FVEP signal averaging. TIVA was used in two patients and 0.5 MAC of desflurane in one. Signal to noise ratio could not be calculated for five eyes as there was no recordable FVEP. Only one eye (normal pre-operative vision) had a FVEP that was present but not reproducible (low signal to noise ratio of 1:33) (Table, patient 12; Fig. 6).
Present but irreproducible FVEP (right panel) during high amplitude EEG (left panel). This 38 year old man with normal pre-operative vision is having endonasal surgery for removal of a pituitary macroadenoma. 120 min of FVEP data is shown with the most recent trace displayed at the bottom. P1 is not reproducible despite 150 stimulus presentations in each FVEP average
3.3 Success rate for FVEP monitoring
The success rate for reproducible FVEP monitoring was 100 % (14/14 eyes) in patients with low amplitude EEG and eyes with normal pre-operative vision. The success rate was 0 % (4/4) in patients with high amplitude EEG and eyes with normal pre-operative vision.
4 Discussion
This is the first report describing the effect of EEG amplitude on FVEP reproducibility during surgery. When high amplitude alpha EEG was present, stimulation of eyes with normal vision failed to evoke reproducible scalp recorded FVEPs. In contrast, when low amplitude alpha EEG was present, stimulation of eyes with normal vision (and one with a visual deficit) evoked reproducible scalp recorded FVEPs. Despite the heterogeneity of our patients (differing pathologies, visual deficits, anesthesia and surgeries) these findings suggest alpha EEG amplitude had the largest impact on FVEP reproducibility. FVEPs were reproducible in patients with low amplitude EEG because the FVEP signal to noise ratio was acceptable (mean 1:4.2). It was impossible to obtain a reproducible FVEP when high amplitude alpha EEG was present. As presumed, the low cut filter had no effect on alpha (8–12 Hz) EEG regardless of whether it was set at 1, 3 or 5 Hz.
The fact that low signal to noise ratio negatively affects evoked potential reproducibility is nothing new or unexpected. Nevertheless, it is surprising that previous studies did not mentioned EEG noise as a cause of FVEP irreproducibility during surgery. This apparent lack of consideration may have been partly due to equipment limitations (i.e. inability to simultaneously perform EEG and FVEP, a limited number of recording channels, no reject windows). They blamed FVEP irreproducibility on the unpredictable nature of the FVEP response itself, anesthesia and specifics of stimulation [14]. Consequently, the technique was abandoned by most neuromonitoring groups and remains so to this day. Unlike previous investigators, we had the advantage of modern equipment that allowed concomitant recording of FVEP and EEG so it was easy to observe the effect of alpha EEG and amplifier blocking on FVEP reproducibility.
Low amplitude EEG appears to be important for stable FVEP recording in the same way reducing electromyographic activity is important for acquiring stable evoked potentials (somatosensory, visual, auditory) in the awake patient. If the anesthetized patient has high amplitude alpha EEG and irreproducible FVEPs then perhaps raising the low cut filter (ideally to 15 Hz) could eliminate the EEG and improve FVEP reproducibility. Unfortunately, many neuromonitoring machines (like ours) do not have 15 or 20 Hz low cut filters but these would be ideal for removing all alpha EEG while at the same time reducing amplifier blocking time.
Amplifier blocking after electrocautery may contribute to FVEP irreproducibility because the resultant flat sweeps are often included in the FVEP average (Figs. 1, 5). Fortunately, we are able to account for amplifier blocking (and fluctuating FVEP amplitude) by observing and later analysing raw EEG concomitantly recorded with FVEP at similar amplifier settings, and then eliminating those averaged FVEPs from analysis. Unfortunately, early investigators likely used equipment incapable of that, so it is possible they were unaware when the amplifier was blocked. Electrocautery detection units (we did not use one in this study) do not shorten amplifier blocking time, but raising the low cut filter to 10 Hz does. For example, we showed that raising the low cut filter from 3 to 10 Hz had almost no effect on N1–P1 amplitude but improved FVEP reproducibility and greatly decreased the amplifier blocking time.
Three decades ago a report was published that recommended raising the low cut filter from 1 to 30 Hz to improve intraoperative somatosensory evoked potential (SSEP) reproducibility [15]. Surprisingly, no reasons were given for why the SSEP reproducibility improved but, from our findings, we suppose it was due to the elimination of alpha EEG and decreased amplifier blocking time. Currently, the 30 Hz low cut filter is the most commonly used low cut filter setting for intraoperative SSEP monitoring [16]. Unfortunately, intraoperative FVEP reproducibility still suffers from low cut filter settings recommended for clinical diagnosis (1 Hz) [17]. Our findings suggest raising the low cut filter to 15 or 20 Hz might eliminate all alpha EEG from the FVEP average, however its effect on FVEP amplitude has not been thoroughly studied (we showed little effect when raising it from 3 to 10 Hz but raising it to 30 Hz decreased N1–P1 amplitude by ~40 % and changed the shape of the waveform; Fig. 4). In any case, FVEP reproducibility is more important than absolute amplitude or latency during surgery so raising the low cut filter to at least 15 Hz may be useful especially when high amplitude EEG and monopolar electrocautery is present. Unfortunately, our evoked potential machine does not have a 15 Hz low cut filter (we have no options between 10 and 30 Hz filter). We are currently comparing FVEP at 3, 10 and 30 low cut filter settings in more patients to determine the trade-off between FVEP amplitude and reproducibility.
Adding more sweeps to the average should also improve FVEP reproducibility but this would increase acquisition time and decrease the ability of the FVEP to quickly detect and prevent optic nerve compromise (we used up to 150 sweeps per average). It is generally accepted that fast detection of neurological compromise is associated with better outcomes due to rapid surgical intervention. In order to keep acquisition time short, the signal to noise ratio must be high so less sweeps are rejected.
One shortfall of this study is that we compared EEG amplitude recorded from one brain region (C4′–Fz) to the FVEP recorded from another (Oz–Fz’). We recorded EEG from C4′–Fpz because it was our usual practice for determining depth of anesthesia during SSEP and motor evoked potential (MEP) monitoring. Once we recognized the negative relationship between high EEG amplitude and FVEP reproducibility, we simultaneously recorded EEG from C4′–Fpz and Oz–Fz′ in two patients and determined both montages recorded similar EEG amplitudes. This was to be expected because both channels had frontal references (propofol and inhalation anesthesia causes an anterior shift of the amplitude dominant alpha EEG) and both had long distances between grid 1 and grid 2 electrodes that would facilitate recording of high amplitude EEG [9, 11]. To determine if activity at Fz′ contributed to (and possibly contaminated) FVEP activity recorded from Oz′–Fz′, we simultaneously recorded from Fpz–Fz′ and Oz–Fz′. There was no activity recorded from Fz′–Fpz that resembled FVEP N1–P1 from Oz–Fz′ (or its inverse). Interestingly, Fpz–Fz′ recorded a robust ERG regardless of side of stimulation. ERG is useful for ensuring adequate retinal stimulation so we use Fz′–Fpz for that purpose.
The contribution of the Fz′ reference to FVEP irreproducibility should be considered. In a previous study, FVEPs recorded from Oz–Fz were compared to those recorded from Oz–earlobe in patients with normal vision and TIVA. Even with the use of an earlobe reference, irreproducible FVEPs occurred in 87 % of patients [2]. Noise is seen in their irreproducible FVEP traces but not reproducible ones, regardless of reference electrode. Accordingly, it is likely that the Fz′ reference site did not unduly contribute to FVEP irreproducibility in our study.
We obtained FVEPs from all patients with normal vision and low amplitude EEG regardless of anesthetic regimen. Nevertheless, recording FVEP during TIVA likely improved the amplitude and reproducibility of the FVEP because, in general, it depresses evoked potential amplitude less than inhalation anesthesia [18]. For example, in a previous study, one patient with normal pre-operative vision had bilaterally irreproducible FVEPs during inhalation anesthesia that became reproducible after switching to TIVA [13]. In another study, FVEPs were obtained from 103 of 104 eyes with TIVA but not in both eyes of one patient with sevoflurane [12]. Both studies had a remarkably high success rate for reproducible FVEPs. Although their success was attributed to improved stimulators with increased luminance [14], they used restrictive low cut filters (either 10 or 20 Hz) that would have decreased the contaminating effect of EEG and amplifier blocking. This may explain why another study that used a 2 Hz low cut filter found TIVA did not improve FVEP reproducibility in 64 eyes with normal vision [2]. In that study, FVEP irreproducibility may have been caused by high amplitude alpha EEG and flat traces (due to amplifier blocking) that were included in the FVEP average.
The pattern of EEG at surgical anesthesia for halogenated agents is different than that for propofol. For propofol, the amplitude and frequency of EEG activity decreases and reaches burst suppression at infusion doses of 150–200 μg/kg/min (bursts consist of slow waves or spindles) [19]. In contrast, halogenated agents at balanced anesthesia doses of 0.7–1 MAC rarely result in a EEG burst suppression pattern; 1.5–2 MAC is necessary for burst suppression in the majority of patients, but this may cause significant hypotension due to vasodilation and myocardial depression [10]. Once EEG burst suppression level is achieved under halogenated agents, bursts have more abrupt, large amplitude waves compared to those produced by propofol anesthesia. Accordingly, propofol is likely better than inhalation anesthesia for reducing alpha EEG amplitude at doses suitable for surgical anesthesia.
Inhalation anesthesia and narcotic induced pupillary constriction have been implicated as being detrimental to FVEP reproducibility [3, 4, 18, 20] but we were able to obtain a reproducible FVEP in a patient with 0.7 mean alveolar concentration (MAC) of desflurane and low amplitude EEG. Nevertheless, after a bolus of propofol was given the EEG became suppressed and the FVEP absent (Fig. 1). After the FVEP amplitude recovered from the bolus of propofol, the desflurane was increased to 1.1 MAC and a bolus of narcotic was given. The FVEP suddenly became low amplitude and irreproducible again (not shown). Accordingly, bolus injections and high MAC of inhalation agents should be avoided.
In rats anesthetized with ketamine, FVEP amplitude increased as EEG power increased [21]. In that study, the mean signal to noise ratio was very high [1:2; mean FVEP amplitude 50 μV, mean raw EEG amplitude 50–100 μV (most power in delta band)] despite the use of a 1 Hz low cut filter. In our study (and theirs) a high signal to noise ratio was necessary for reproducible FVEP recording. Most anesthesiologists are reluctant to use ketamine as the primary anesthetic agent in humans because large doses may increase intracranial pressure, emergence delirium and post-operative hallucinations. However low dose ketamine infusion (4 μg/kg/min) combined with propofol and remifentanil (TIVA technique) has been successfully used for MEP monitoring [22] and, given that it may increase FVEP amplitude, may be useful for FVEP monitoring too.
Our success in obtaining reproducible FVEPs was likely due to operations that did not displace the goggle stimulators (like endonasal surgery) and a cohort of mainly adult patients with few visual deficits. Younger patients generally have high amplitude EEG making FVEP monitoring more difficult. Suppressed EEG has the benefit of ensuring the patient is deeply anesthetized with the trade-off being decreased blood pressure related to the deep anesthesia (in some cases). As stated above, if high amplitude EEG cannot be avoided then perhaps the use of a 15 or 20 Hz low cut filter would be useful. Pattern reversal VEP (PRVEP) N75–P100 amplitude in awake subjects begins to decrease with low cut filtering above 8 Hz and, at 15 Hz, the amplitude is decreased by 46 % [23]. The PRVEP in awake subjects likely has different frequency characteristics than the FVEP in anesthetized patients. Sasaki showed the FVEP was present and reproducible in patients even when a 20 Hz low cut filter was used [13]. We showed, in two patients, that a 30 Hz low cut filter decreased N1–P1 amplitude by about 40 % and changed the shape of the FVEP waveform. In rats, a bandpass of 3.2–320 Hz was optimal for recording the primary cortical FVEP waveform, but the effect of raising the low cut filter on FVEP amplitude was not studied [24].
PRVEPs primarily assess cone function while FVEPs primarily assess rod function and therefore light perception. As a result, it is entirely possible for a patient with normal pre-operative vision to have unchanged FVEPs during surgery yet have a significant visual deficit post-operatively (loss of fine visual acuity mediated by cone vision) [5]. Although there is an imprecise relationship between FVEP and visual function, all eyes with reproducible FVEPs at the end of surgery in our study had no new visual deficits. All eyes with visual deficits (except one) either had absent or irreproducible FVEPs regardless of the amount of EEG. One patient in the “FVEP and low amplitude EEG” group (patient 8, Table) had a reproducible FVEP that deteriorated but recovered during surgery, and that patient woke with no new visual deficits. Other studies, using custom made stimulators and 10 or 20 Hz low cut filters, have shown reproducible scalp recorded FVEPs that accurately predicted post-operative visual function [12, 13]. Monitoring visual pathways posterior to the chiasm is achieved by direct recording from subdural electrodes placed on the visual cortices and a recent report showed FVEP change was related to post-operative visual function [25].
Surgery that involves a frontal scalp flap reflection (not done in this study) causes the stimulating goggles to move and the light axis to deviate. Unfortunately, new stimulators designed to remain stable in those surgeries are not yet commercially available [12, 13]. In the meantime, goggle stimulation can be used for surgery that does not involve frontal scalp flap reflection (like endonasal surgery). Since surgical procedures which result in a change in visual function may be relatively uncommon, a study involving a larger number of patients will be needed to demonstrate a correlation between response changes (if any) and post-operative visual function. Future studies should be performed during those surgeries to determine (a) if raising the low cut filter to 15 Hz improves FVEP reproducibility (b) if intraoperative FVEP change (or no change) can predict post-operative visual function and (c) if intraoperative FVEP monitoring can reduce iatrogenic visual deficits associated with surgery that puts optic pathways (up to and including the optic chiasm) at risk. Raising the low cut filter to a minimum of 10 Hz (15 Hz if available) combined with the use of reject windows and TIVA anesthesia will be important for making those studies possible.
5 Conclusion
Reproducible intraoperative FVEP monitoring has eluded most neuromonitoring teams for decades. We showed that low amplitude EEG greatly contributed to FVEP reproducibility during surgery.
References
Toleikis SC, Toleikis JR. VEP. In: Koht A, Sloan TB, Toleikis JR, editors. Monitoring the nervous system for anesthesiologists and other health care professionals. New York: Springer; 2012. p. 69–93.
Cedzich C, Schramm J. Monitoring of flash visual evoked potentials during neurosurgical operations. Int Anesthesiol Clin. 1990;28(3):165–9.
Wiedemayer H, Fauser B, Armbruster W, Gasser T, Stolke D. Visual evoked potentials for intraoperative monitoring using total intravenous anesthetic. J Neurosurg Anesthesiol. 2003;15:19–24.
Sebel PS, Intram DA, Flynn PJ, Rutherford CF, Rogers H. Evoked potentials during isoflurane anesthesia. Br J Anaesth. 1986;58:580–5.
Cedzich C, Schramm J, Fahlbusch R. Are flash-evoked visual potentials useful for intraoperative monitoring of visual pathway function? Neurosurgery. 1987;21:709–15.
American Electroencephalographic Society guidelines for intraoperative monitoring of sensory evoked potentials. J Clin Neurophysiol. 1987;4(4):397–416.
American Clinical Neurophysiology Society. Guideline 9B. Guidelines on visual evoked potentials. J Clin Neurophysiol. 2006;23(2):138–56.
Odom FV, Bach M, Brigell M, Holder GE, McCulloch DL, Tormene AP, Vaegan. ISCEV standard for clinical visual evoked potentials (2009 update). Doc Ophthalmol. 2010;120:111–9.
Tinker JH, Sharbrough FW, Michenfelder JD. Anterior shift of the dominant EEG rhythm during anesthesia in the java monkey: correlation with anesthetic potency. Anesthesiology. 1977;46:252–9.
Rampil IJ, Lockhart SH, Eger EI II, Yasuda N, Weiskopf RB, Cahalan MK. The electroencephalographic effects of desflurane in humans. Anesthesiology. 1991;74:434–9.
Murphy M, Bruno MA, Riedner BA, et al. Propofol anaesthesia and sleep: a high-density EEG study. Sleep. 2011;34(3):283–91.
Kodama K, Goto T, Sato A, Sakai K, Tanaka Y, Hongo K. Standard and limitation of intraoperative monitoring of the visual evoked potential. Acta Neurochir. 2010;152:643–8.
Sasaki T, Itakura T, Suzuki K, et al. Intraoperative monitoring of visual evoked potential: introduction of a clinically useful method. J Neurosurg. 2010;112:273–84.
Cohen BA, Baldwin ME. Visual-evoked potentials for intraoperative neurophysiology monitoring: another flash in the pan? J Clin Neurophysiol. 2011;28(6):599–601.
Nuwer MR, Dawson EG. Intraoperative evoked potential monitoring of the spinal cord. A restricted filter, scalp method during Harrington instrumentation for scoliosis. Clin Orthop. 1984;183:42–50.
American Clinical Neurophysiology Society. Guideline 11B (2009). Guidelines for intraoperative monitoring of sensory evoked potential. ACNS web site. www.acns.org/pdf/guidelines/Guideline-11B.pdf.
American Clinical Neurophysiology Society. Guideline 9D. Guidelines on short latency somatosensory evoked potentials. J Clin Neurophysiol. 2006;23(2):168–79.
Banoub M, Tetzlaff JE, Schubert A. Pharmacologic and physiologic influences affecting sensory evoked potentials: implications for perioperative monitoring. Anesthesiology. 2003;99(3):716–37.
Huotari AM, Koskinen M, Suominen K, Alahuhta S, Remes R, Hartikainen KM, Jäntti V. Evoked EEG patterns during burst suppression with propofol. Br J Anaesth. 2004;92(1):18–24.
Chi OZ, McCoy CL, Field C. Effects of fentanyl anesthesia on visual evoked potentials in humans. Anesthesiology. 1987;67(5):827–30.
You Y, Thie J, Klistorner A, Gupta VK, Graham SL. Normalization of visual evoked potentials using underlying electroencephalogram levels improves amplitude reproducibility in rats. IOVS. 2012;53(3):1473–8.
Zaarour C, Engelhardt T, Strantzas S, Pehora C, Lewis S, Crawford MW. Effect of low-dose ketamine on voltage requirement for transcranial electrical motor evoked potentials in children. Spine. 2007;32(22):E627–30.
Skuse NF, Burke D. Power spectrum and optimal filtering for visual evoked potentials to pattern reversal. Electroencephalogr Clin Neurophysiol. 1990;77:199–204.
Shaw NA. The effects of low-pass filtering on the flash visual evoked potential of the albino rat. J Neurosci Methods. 1992;44:233–40.
Ota T, Kawai K, Kamada K, Kin T, Saito N. Intraoperative monitoring of cortically recorded visual response for posterior visual pathway. J Neurosurg. 2010;112:285–94.
Conflict of interest
The authors have no conflict of interest and the FVEP studies were performed according to current Canadian laws.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Houlden, D.A., Turgeon, C.A., Polis, T. et al. Intraoperative flash VEPs are reproducible in the presence of low amplitude EEG. J Clin Monit Comput 28, 275–285 (2014). https://doi.org/10.1007/s10877-013-9532-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9532-8