Abstract
Sexual dysfunction is present in almost one third of women with pelvic organ prolapse (POP), causing loss of self-confidence, difficulties in relating to the other sex and abandonment of sexual intercourse.
Only in recent years, the problem of sexuality after POP surgery has been emphasised, and specific questionnaires are available. Among them, the Female Sexual Function Index (FSFI) is a generic questionnaire that has been used in many studies to assess sexual function in women with POP before and after surgery. The ability of a new questionnaire, PISQ-IR, to document condition-specific impact and measure symptoms, including urinary and anal incontinence and POP, suggests this robust tool may be most useful for characterising symptoms in women with POP than generic sexual questionnaires. In addition, the items of the questionnaire were designed to evaluate both sexually active and sexually inactive women and were written to be independent of sexual orientation.
What happens after POP surgery?
Sexual function is significantly improved after vaginal POP surgery. However when a colpoperineorrhaphy is associated with an anterior repair, no improvement in sexual function and higher rates of dyspareunia are reported.
POP surgery with mesh may cause the new onset or worsening of dyspareunia. Instead, sexual activity, desire, arousal, orgasm and satisfaction remain unchanged.
The abdominal sacrocolpopexy, performed via laparotomic, laparoscopic or robotic approaches, gives positive results on sexuality, mainly in desire, arousal and orgasm.
Regarding the uterus-sparing surgery, sacrospinous hysteropexy, the most studied vaginal technique, gives favourable results on sexuality, although the majority of these studies are flawed by selection and information bias, short follow-up or lack of adequate control groups.
Abdominal and laparoscopic hysterosacropexy has the main advantage of ensuring a normal vaginal axis and a good vaginal length, which is mandatory for sexual activity. The main disadvantage is the continuous surveillance required for cervical and uterine malignancies.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Pelvic Organ Prolapse (POP)
- Female Sexual Function Index (FSFI)
- Uterus-sparing Surgery
- Sacrospinous Hysteropexy (SSH)
- Normal Vaginal Axis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
7.1 Introduction
Sexual dysfunction is present in almost one third of women with pelvic organ prolapse (POP), as epidemiological studies have shown [1–3]. POP can cause loss of self-confidence, difficulties in relating to the other sex and even abandonment of sexual intercourse [4]. Women with POP are less satisfied with their sexual activity compared to women without: they show a lower degree of emotional closeness to their partner and say that they feel desire and pleasure less frequently. Also, they are more likely to feel pain during intercourse [5]. Anatomically, this could be due to mechanical obstruction or laxity of the vaginal wall or both. In addition, when POP and urinary incontinence are associated, sexual activity worsened because of coital incontinence that can be present concomitantly.
It has been shown that women seeking treatment for advanced prolapse have lower quality of life scores [6, 7], and their body image is decreased. The value of body image in female sexual function is an aspect that has been investigated only recently. It often leads to feelings of shame, embarrassment and the impression of being less sexually attractive, all of which reduce quality of life (QoL). It also has a negative impact on sexual function, particularly on desire and sexual satisfaction [8].
Women not frequently discuss the impact of POP on sexual function with their doctors. Improvement in sexual life is a commonly reported treatment goal for them since they expect that the surgery will allow them to recover the ability to be intimate without feeling embarrassed [9].
Sexual function may improve with anatomical correction of POP. The gains from the correction of POP must be weighed against the effects of surgery in the vaginal area. Since the vagina is a sexual organ and its adequate functioning is dependent on normal anatomical and neurovascular factors, we can expect that any POP surgery will affect sexual function [10, 11].
So far, the data on the impact of POP surgery on sexual life are inconclusive. The discrepancy in these results may be due to both cultural and methodological factors. First, expectations from sexual relationships and woman’s comfort in expressing her sexual problems vary with their country of origin and cultural background. Secondly, methodological differences make difficult to compare varying outcomes from different studies and to interpret differences in how those outcomes are measured, e.g. how to quantify sexual responses.
The questionnaires are the best instruments to measure sexual function. Among them, the Female Sexual Function Index (FSFI) is a generic questionnaire that has been used in many studies to assess sexual function in women with POP before and after surgery [12]. The Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ), together with its short form (PISQ-12), is another validated specific sexual function questionnaire that was designed to assess changes in sexual health. It was and still is the first specific questionnaire for the evaluation of sexual function in heterosexual women with pelvic floor disorders who are sexually active [13, 14]. A recently reviewed version of PISQ, the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire IUGA-Revised (PISQ-IR), has been validated. This was designed as a condition-specific measure of sexual function in women with pelvic floor dysfunction, including urinary and anal incontinence and POP. In addition, the items of the questionnaire were designed to evaluate both sexually active and sexually inactive women and were written to be independent of sexual orientation [15].
Several techniques – including vaginal, open abdominal and laparoscopic approaches – have been proposed to correct POP, with varying success rates. It is also now accepted that different techniques in POP surgery have very different impacts on sexual function. Considering that surgical dissection may result in tissue damage, devascularisation and denervation, which may lead to a drop in vaginal blood flow and more fibrosis, what happens in female sexuality after POP repair with each type of surgery?
7.2 Vaginal POP Surgery Using Native Tissue
For native tissue repair, a recent systematic review has been published [16]. This review only included studies that reported on sexual function of sexually active women with symptomatic prolapse who underwent vaginal surgery with native tissues and in which women acted as their own controls. Papers including patients who had concomitant incontinence surgery or vaginal mesh procedures were excluded from this review. The study concluded that sexual function is significantly improved after surgery. Dyspareunia was significantly reduced following native tissue POP surgery, and postoperative chances of improvement or no change in dyspareunia was 4.8 times greater than the risk of deterioration. However, when a colpoperineorrhaphy was performed in combination with an anterior repair, no improvement in sexual function and higher rates of dyspareunia rates were reported [17–19].
The use of levator plication sutures to repair the posterior compartment and enterocele is considered the main reason causing dyspareunia: if performed, levator plication needs careful assessment of vaginal width to ensure that vaginal capacity is not compromised by overtight sutures [20]. Dyspareunia can also be caused by excessive scarring with consequent lack of elasticity of the vagina.
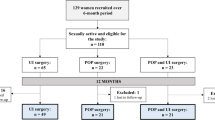
7.3 Vaginal POP Surgery with Mesh
Vaginal surgery with synthetic mesh or graft materials was proposed to reinforce the pubocervical and rectovaginal fascia in order to provide support to the pelvic floor. Implantation of synthetic mesh might damage vaginal innervation and vascularisation, which could cause sexual dysfunction and in some cases may cause the new onset or worsening of dyspareunia. This may be due to a decrease in stress shielding of the underlying vaginal wall after implantation of mesh, which in turn may result in an atrophic stiff vagina and less lubrication [21]. In addition, considering that the most common complications of POP surgery with mesh are mesh exposure (Fig. 7.1) and shrinkage, we can assume that the first complication could explain, at least partly, the increased dyspareunia reported by some patients, while the presence of shrinkage may result in a less pliable vagina and consequent pain during intercourse, worsening significantly sexual function [22].
Other aspects of sexual function remain unchanged. No significant difference is reported in degree of sexual activity, sexual desire, sexual arousal, orgasm and satisfaction. There is no correlation between these results and anatomical correction [23, 24] or position of the mesh: there are no beneficial or detrimental effects in sexual function after either anterior only or anterior and posterior mesh positioning.
In the last Cochrane systematic review on the surgical management of POP, Maher et al. analysed sexual function and dyspareunia in women undergoing mesh surgery in the anterior, posterior and apical compartments [25]. After anterior polypropylene mesh repair, no differences in sexual function or de novo dyspareunia were identified when compared with anterior colporrhaphy (Table 7.1).
Finally insufficient informations are available to provide evidence-based recommendations on sexual function after vaginal mesh repair in the posterior compartment. However, after the 2011 FDA advertisement, confirmed in 2014, the use of mesh for posterior compartment is not recommended.
7.4 Abdominal and Laparoscopic Surgery
The most studied procedure for correction of advanced POP is colposacropexy (CSP). Since its introduction by Lane in 1962 [34], CPS has proven to be an effective and durable technique for correcting apical prolapse, giving significant improvements in prolapse symptoms, urinary function and QoL.
Traditionally, CSP has been performed via a laparotomy (abdominal sacral colpopexy); however the use of laparoscopic and robotic approaches is increasing. To date, only few studies have focused on the relationship between CSP and sexuality, but the results so far are positive. Using a validated questionnaire, Costantini et al. showed that patients had significant post-op improvements in their total FSFI scores and in the domains of desire, arousal and orgasm [35]. Thibault et al. demonstrated that this improvement occurs in the first 3 months after surgery [36].
7.5 The Role of Hysterectomy
Over the past few decades, the psychological and emotional value of reproductive organs has changed profoundly. Uterus-sparing surgery is becoming more popular worldwide, and consensus is growing that the uterus can be preserved at the time of pelvic reconstructive surgery in appropriately selected women who desire it.
In fact, anatomical modifications induced by hysterectomy can damage sexuality through lack of uterine contractions and altered perception of orgasm. Moreover hysterectomy can cause vaginal shortening and damage to nerve endings and may also have psychological effects with loss of self-esteem [37]. Damage to the innervation of the uterine cervix and the upper vagina following hysterectomy could affect lubrication and orgasm. The internal orgasm occurs essentially in the cervix and is provoked by stimulation of the fibre endings of the uterovaginal plexus that surround the cervix and the upper vagina. Therefore, the loss of most of the uterovaginal plexus is likely to have adverse effects on sexuality [38]. On the other hand, uterus-sparing surgery raises concerns about the most suitable approach (vaginal, abdominal, laparoscopic), the risks of partial POP resolution, mesh-associated complications, new onset of urinary incontinence, increased recurrence rate with some approaches, failure to improve urinary function, failure to improve bowel and sexual symptoms, longevity of outcome and lifetime risk of cancer [39].
Sacrospinous hysteropexy (SSH) is one of the most studied vaginal techniques for uterus preservation and consists in the unilateral attachment of the posterior uterine cervix or the uterosacral ligaments to the right sacrospinous ligament, about 2 cm medial from the ischial spine, using a combination of permanent and delayed absorbable sutures. Favourable results have been demonstrated on sexuality, although the majority of these studies are flawed by selection and information bias, short follow-up or lack of adequate control groups (Table 7.2).
Abdominal and laparoscopic hysterosacropexy has the main advantage of ensuring a secure proximal and distal vaginal anchorage without tension with a normal vaginal axis and a good vaginal length, which is mandatory for sexual activity. Comparing patients who underwent hysterosacropexy (HSP) and hysterectomy with CSP, Costantini et al. demonstrated that there were no differences in outcomes, in terms of subjective, objective and patient’s satisfaction [44]. The advantages of HSP include maintaining pelvic anatomy integrity, which is crucial in prolapse resolution, and significantly reducing blood loss, operating times and hospital stays, while the main disadvantage is the continuous surveillance required for cervical and uterine cancer. A further study of the same group demonstrated no substantial differences regarding sexual activity in patients in which the uterus has been spared (HPS group) as opposed to those in whom it has been removed (CSP group): data obtained from FSFI questionnaire demonstrated that there were no significant differences between the two groups in terms of total score and also comparing the examined individual domains – desire, arousal, lubrication, orgasm, satisfaction and pain [45]. The main reason for these results is that, as the uterus preservation is a woman’s choice, the two groups represent different kinds of women, i.e. the women who decided to remove the uterus are women in which it doesn’t represent as sexual organ. On the contrary the women who prefer uterus-sparing surgery are women in which the uterus plays a role in their femininity and obviously in their sexual life.
Conclusion
Our knowledge on female sexual function is still in its initial stages. In the past, little or no consideration has been given to the problem of sexuality among patients who underwent pelvic surgery for urogenital prolapse, and only in recent years, this aspect has been emphasised.
Much deeper investigations are needed to clarify the effect on sexuality of variables such as educational level, profession and cultural differences, which are not directly related to POP status but could represent major biases. The evaluation of sexual function through specific questionnaires makes easier to identify the sexual dysfunctions associated with the pelvic floor disorders.
Moreover, data on sexual outcome should be included in preoperative counselling and in outcome evaluation after POP surgery. The inclusion of a new condition-specific questionnaire as an outcome measure allows an analysis of the impact of POP treatments on women’s sexual function. The ability of the PISQ-IR to document condition-specific impact and to measure symptoms suggests this robust tool may be more useful than generic sexual questionnaires for characterising symptoms in women with POP.
Abbreviations
- CSP:
-
Colposacropexy
- FSFI:
-
Female Sexual Function Index
- HSP:
-
Hysterosacropexy
- PISQ:
-
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire
- PISQ-12:
-
Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire-short form
- PISQ-IR:
-
Pelvic Organ Prolapse/Incontinence Sexual Questionnaire IUGA-Revised
- POP:
-
Pelvic organ prolapse
- QOL:
-
Quality of life
- SSH:
-
Sacrospinous hysteropexy
References
Handa VL, Cundiff G, Chang HH, Helzlsouer KJ. Female sexual dysfunction and pelvic floor disorders. Obstet Gynecol. 2008;111:1045–52.
Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC, Continence Program for Women Research Group. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2002;99(2):281–9.
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–7; discussion 1337–8.
Filocamo MT, Serati M, Frumenzio E, Li Marzi V, Cattoni E, Champagne A, Salvatore S, Nicita G, Costantini E. The impact of mid-urethral slings for the treatment of urodynamic stress incontinence on female sexual function: a multicenter prospective study. J Sex Med. 2011;8(7):2002–8.
Athanasiou S, Grigoriadis T, Chalabalaki A, Proptopapas A, Antsaklis A. Pelvic organ prolapse contributes to sexual dysfunction: a cross-sectional study. Acta Obstet Gynecol Scand. 2012;91(6):704–9.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194:1455–61.
Lowenstein L, Gamble T, Deniseiko Sanses TV, et al. Sexual function is related to body image perception in women with pelvic organ prolapse. J Sex Med. 2009;6:2286–91.
Zielinski R, Miller J, Low LK, Sampselle C, DeLancey JO. The relationship between pelvic organ prolapse, genital body image, and sexual health. Neurourol Urodyn. 2012;31:1145–8.
Sung VW, Rogers RG, Barber MD, Clark MA. Conceptual framework for patient-important treatment outcomes for pelvic organ prolapse. Neurourol Urodyn. 2014;33(4):414–9.
Lakeman MM, Laan E, Roovers JP. The effects of prolapse surgery on vaginal wall sensibility, vaginal vasocongestion, and sexual function: a prospective single centre study. Neurourol Urodyn. 2014;33:1217–24.
Weber MA, Lakeman MM, Laan E, Roovers JP. The effects of vaginal prolapse surgery using synthetic mesh on vaginal wall sensibility, vaginal vasocongestion, and sexual function: a prospective single-center study. J Sex Med. 2014;11:1848–55.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino Jr R. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208.
Rogers RG, Kammerer-Doak D, Villarreal A, Coates K, Qualls C. A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol. 2001;184:552–8.
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C. A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:164–8.
Rogers RG, Rockwood TH, Constantine ML, Thakar R, Kammerer-Doak DN, Pauls RN, Parekh M, Ridgeway B, Jha S, Pitkin J, Reid F, Sutherland SE, Lukacz ES, Domoney C, Sand P, Davila GW, Espuna Pons ME. A new measure of sexual function in women with Pelvic Floor Disorders (PFD): the Pelvic Organ Prolapse/Incontinence Sexual Questionnaire, IUGA-Revised (PISQ-IR). Int Urogynecol J. 2013;24:1091–103.
Jha S, Gray T. A systematic review and meta-analysis of the impact of native tissue repair for pelvic organ prolapse on sexual function. Int Urogynecol J. 2015;26:321–7.
Colombo M, Vitobello D, Proietti F, Milani R. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. BJOG. 2000;107(4):544–51.
Haase P, Skibsted L. Influence of operations for stress incontinence and/or genital descensus on sexual life. Acta Obstet Gynecol Scand. 1988;67(7):659–61.
Dua A, Jha S, Farkas A, Radley S. The effect of prolapse repair on sexual function in women. J Sex Med. 2012;9(5):1459–65.
Ulrich D, Dwyer P, Rosamilia A, Lim Y, Lee J. The effect of vaginal pelvic organ prolapse surgery on sexual function. Neurourol Urodyn. 2015;34(4):316–21.
Jones KA, Feola A, Meyn L, Abramowitch SD, Moalli PA. Tensile properties of commonly used prolapse meshes. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(7):847–53. doi:10.1007/s00192-008-0781-x. Epub 2009 Mar 28.
Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Effects of vaginal prolapse surgery on sexuality in women and men; results from a RCT on repair with and without mesh. J Sex Med. 2012;9(4):1200–11.
Long CY, Juan YS, Wu MP, Liu CM, Chiang PH, Tsai EM. Changes in female sexual function following anterior with and without posterior vaginal mesh surgery for the treatment of pelvic organ prolapse. J Sex Med. 2012;9(8):2167–74.
Altman D, Elmér C, Kiilholma P, Kinne I, Tegerstedt G, Falconer C, Nordic Transvaginal Mesh Group. Sexual dysfunction after trocar-guided transvaginal mesh repair of pelvic organ prolapse. Obstet Gynecol. 2009;113(1):127–33.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;4:CD004014.
Sivaslioglu AA, Unlubilgin E, Dolen I. A randomized comparison of polypropylene mesh surgery with site-specific surgery in the treatment of cystocoele. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(4):467–71.
Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008;111(4):891–8.
Allahdin S, Glazener C, Bain C. A randomised controlled trial evaluating the use of polyglactin mesh, polydioxanone and polyglactin sutures for pelvic organ prolapse surgery. J Obstet Gynaecol. 2008;28(4):427–31.
Carey M, Higgs P, Goh J, Lim J, Leong A, Krause H, Cornish A. Vaginal repair with mesh versus colporrhaphy for prolapse: a randomised controlled trial. BJOG. 2009;116(10):1380–6.
Iglesia CB, Sokol AI, Sokol ER, Kudish BI, Gutman RE, Peterson JL, Shott S. Vaginal mesh for prolapse: a randomized controlled trial. Obstet Gynecol. 2010;116(2 Pt 1):293–303.
Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C, Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011;364(19):1826–36.
Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG. 2011;118(12):1518–27.
Withagen MI, Vierhout ME, Hendriks JC, Kluivers KB, Milani AL. Risk factors for exposure, pain, and dyspareunia after tension-free vaginal mesh procedure. Obstet Gynecol. 2011;118(3):629–36.
Lane FE. Repair of posthysterectomy vaginal-vault prolapse. Obstet Gynecol. 1962;20:72–7.
Costantini E, Porena M, Lazzeri M, Mearini L, Bini V, Zucchi A. Changes in female sexual function after pelvic organ prolapse repair: role of hysterectomy. Int Urogynecol J. 2013;24(9):1481–7.
Thibault F, Costa P, Thanigasalam R, Seni G, Brouzyine M, Cayzergues L, De Tayrac R, Droupy S, Wagner L. Impact of laparoscopic sacrocolpopexy on symptoms, health-related quality of life and sexuality: a medium-term analysis. BJU Int. 2013;112(8):1143–9.
Achtari C, Dwyer PL. Sexual function and pelvic floor disorders. Best Pract Res Clin Obstet Gynaecol. 2005;19(6):993–1008.
Hasson HM. Cervical removal at hysterectomy for benign disease. Risks and benefits. J Reprod Med. 1993;38(10):781–90.
Costantini E, Lazzeri M, Zucchi A, Bini V, Mearini L, Porena M. Five-year outcome of uterus sparing surgery for pelvic organ prolapse repair: a single-center experience. Int Urogynecol J. 2011;22(3):287–92.
Maher CF, Cary MP, Slack MC, Murray CJ, Milligan M, Schluter P. Uterine preservation or hysterectomy at sacrospinous colpopexy for uterovaginal prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(6):381–4.
Hefni M, El-Toukhy T, Bhaumik J, Katsimanis E. Sacrospinous cervicocolpopexy with uterine conservation for uterovaginal prolapse in elderly women: an evolving concept. Am J Obstet Gynecol. 2003;188(3):645–50.
van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350–5; discussion 355.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16.
Costantini E, Mearini L, Bini V, Zucchi A, Mearini E, Porena M. Uterus preservation in surgical correction of urogenital prolapse. Eur Urol. 2005;48:642–9.
Zucchi A, Costantini E, Mearini L, Fioretti F, Bini V, Porena M. Female sexual dysfunction in urogenital prolapse surgery: colposacropexy vs hysterocolposacropexy. J Sex Med. 2008;5:139–45.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Pons, M.E., Natale, F., Costantini, E. (2017). POP and Impact of Surgery on Female Sexual Life. In: Costantini, E., Villari, D., Filocamo, M. (eds) Female Sexual Function and Dysfunction. Springer, Cham. https://doi.org/10.1007/978-3-319-41716-5_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-41716-5_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41714-1
Online ISBN: 978-3-319-41716-5
eBook Packages: MedicineMedicine (R0)