Abstract
Introduction and hypothesis
To improve our understanding of the differences in commonly used synthetic prolapse meshes, we compared four newer generation meshes to Gynecare PS™ using a tensile testing protocol. We hypothesize that the newer meshes have inferior biomechanical properties.
Methods
Meshes were loaded to failure (n = 5 per group) generating load–elongation curves from which the stiffness, the load at failure, and the relative elongation were determined. Additional mesh samples (n = 3) underwent a cyclic loading protocol to measure permanent elongation in response to subfailure loading.
Results
With the exception of Popmesh, which displayed uniform stiffness, other meshes were characterized by a bilinear behavior. Newer meshes were 70–90% less stiff than Gynecare™ (p < 0.05) and more readily deformed in response to uniaxial and cyclical loading (p < 0.001).
Conclusion
Relative to Gynecare™, the newer generation of prolapse meshes were significantly less stiff, with irreversible deformation at significantly lower loads.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Synthetic meshes are commonly used in most urogynecologic procedures including sacrocolpopexy, sub-urethral slings, colposuspension, and anterior and posterior repairs. A recent web-based survey of American Urogynecological Society surgeons revealed that 93% of respondents use some form of synthetic mesh when performing a sacrocolpopexy and 58% when performing vaginal reconstructive surgery [1]. There is consistent and robust evidence supporting the use of synthetic mesh in an abdominal approach with sacrocolpopexy [2]; however, data supporting the use of synthetic material in vaginal reconstructive surgery is limited to case series and observational studies [3, 4]. Biochemical data and clinical experience suggest that the endogenous tissues of women with prolapse are weaker [5, 6] and, therefore, prone to failure. Thus, clinicians who advocate the use of mesh aim to improve the permanency and success of reconstructive procedures that currently have a failure rate in excess of 30% [7].
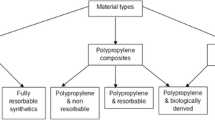
A wide range of biomaterials are available to clinicians for incontinence and prolapse procedures with little quantitative data on which to base the selection of a particular material. Although limited data suggests that, in terms of anatomical [8] and biomechanical [9] outcomes, synthetic polypropylene meshes are superior to biologic meshes, there is significant evidence that the complications associated with synthetic meshes can cause significant morbidity including infection, erosion, exposure, and pain [8, 10]. In addition, the vaginal tissue to be augmented is often structurally compromised, atrophic, and devascularized. Such poor tissue quality increases the risk of poor tissue incorporation into the mesh potentially resulting in suboptimal healing and mesh exposure or erosion into an adjacent viscous. Moreover, there is evidence that meshes shrink in vivo leading to increased stiffness, pain, and poor restoration of the normal properties of the vagina [9]. In this way, the choice of the appropriate mesh for surgical augmentation is extremely important. To date, graft materials are largely based on those successfully used for abdominal hernia repairs. Thus, there is not enough experimental or clinical data to determine how they will perform for prolapse repairs.
Synthetic graft materials differ by composition (monofilament vs multifilament), flexibility [7], pore size, surface properties (coated vs non-coated), and architecture (knit vs woven). Type I, large-pore monofilament is the preferable synthetic material [8, 10–14]. The goal of a synthetic mesh is to improve the durability of a prolapse repair by increasing tissue strength with the least amount of burden on the host tissue. That is, in addition to restoring anatomy, the mesh must not interfere with vaginal properties such as distensibility and flexibility. However, the specific characteristics of a mesh that are necessary to achieve these goals are not known. In general, it is thought that knitted monofilament, lighter weight, larger pore size, increased porosity, and decreased density are associated with improved host tolerability and, consequently, lower rates of exposure, erosion, and infection. The initial mesh designed specifically for prolapse repairs is Gynecare PS™ (Ethicon, Sommersville, NJ, USA), a lighter weight (44 g/m2) version of a heavier polypropylene mesh by the same manufacturer used in abdominal wall hernia repairs. More recently, additional meshes have appeared on the market with modifications that purportedly decrease mesh burden and improve host tolerability. For example, Popmesh™ (Caldera, Agoura Hills, CA, USA) is manufactured as an ultra-light-weight (19 g/m2) polypropylene material with increased flexibility for increased patient comfort following tissue incorporation. Timesh™ (PFM, Oceanside, CA, USA) is composed of titanized polypropylene to reduce mesh exposure associated with foreign body reaction, decrease mesh shrinkage, and increase biocompatibility. It is available in various densities including a light (35 g/m2) and an extra-light (16 g/m2) mesh. Pelvitex™ (C.R. Bard, Covington, GA, USA) is marketed with a hydrophilic porcine collagen I coat for enhanced healing, increased strength, and durability. The collagen allegedly acts as a barrier between the vagina and the mesh to reduce the risk of mesh erosion. Polyform™ (Boston Scientific, Natick, MA, USA) is an uncoated polypropylene mesh that is marketed as a softer, thinner mesh and is said to be lighter (40 g/m2) and less stiff than other commonly used prolapse meshes. A lower stiffness potentially makes the mesh less intrusive and more compatible with the properties of the vagina following tissue incorporation. In this way, a less stiff mesh is less likely to erode into an adjacent organ (e.g., bladder or rectum) or result in a mesh exposure.
In this study, we contend that prior to determining the behavior of a mesh in vivo, one must have a comprehensive understanding of its mechanical behavior ex vivo. By improving our understanding of the differences between meshes prior to host incorporation, we will have a more durable foundation upon which to base differences in the behavior of meshes that may occur in vivo. Thus, we aimed to quantify and define differences in commonly used prolapse meshes relative to Gynecare PS™ utilizing a tensile testing protocol. We chose Gynecare PS™ as the “gold standard” based solely on the fact that it was the original prolapse mesh to appear on the market and it is considered the “gold standard” upon which other meshes are based. Uniaxial tensile testing was performed to simulate in vivo loading conditions after an abdominal sacrocolpopexy. Similarly, cyclical testing was performed to mimic small increasing in intrabdominal pressure in the early postoperative period.
Materials and methods
Sterile samples of five full-length meshes [Gynecare PS™ (Ethicon, Sommersville, NJ, USA), Pelvitex™ (C.R. Bard), Popmesh™ (Caldera), Timesh™ (PFM), and Polyform™ (Boston Scientific)] were obtained. Table 1 delineates the material, structure, thickness, weight, and novel features of the meshes provided by the manufacturer. Samples were removed from the sterile packing and divided into 15 × 5 cm sections for tensile tests. These dimensions were chosen to simulate the size of mesh implanted surgically in an abdominal prolapse repair. In addition, a small 1.0-cm2 section was removed from the end of each mesh for imaging by light microscopy. A total of five samples of each mesh were obtained and tested separately (n = 5) using a uniaxial load to failure protocol. An additional three meshes from each groups were subject to a uniaxial cyclical loading protocol.
Imaging
Following imaging by standard light microscopy, micrographs were examined, and pore sizes were estimated by a blinded technician. To do this, all pores within a sample were traced, and then the average size was quantified using Metamorph version 7.5™ (Molecular Devices, Sunnyvale, CA, USA).
Tensile testing protocol
The methods for tensile testing have been described previously [14]. Briefly, mesh samples were attached to a custom set of clamps to form a clamp–mesh–clamp construct. Clamp to clamp distances were measured. To ensure that samples were tested consistently, an aspect ratio (length to width ratio) of three was maintained for all samples.
Once the meshes were properly affixed in the clamps, each sample was placed in a 37°C saline bath with one clamp rigidly affixed to the base of the Instron ™ 4502 (Instron, Norwood, MA, USA) screw driven testing apparatus and the other fixed to a load cell that was attached to the crosshead of the testing apparatus. After allowing 10 min to equilibrate, a preload of 0.1 N was applied using an elongation rate of 10 mm/min. This removes all slack within the sample allowing for measurements of the clamp to clamp distance. After this procedure, the samples were loaded to failure along the longitudinal axis at a rate of 50 mm/min. The load at failure in newtons and the elongation in millimeters were obtained. The relative elongation of the samples was calculated by dividing the elongation by the initial clamp to clamp distance.
Load vs relative elongation curves were plotted and analyzed. Most curves were bilinear, with two distinct regions that we chose to define separately because of their disparate mechanical behavior. Initial deformation of the meshes was characterized by a distinct region of low stiffness that transitioned into a second region characterized by high stiffness. We defined the point between the low and high stiffness regions as the point of inflection (Fig. 2). The low stiffness region (N/mm) was quantitatively defined as the minimum slope over the first 15% interval of relative elongation. The high stiffness region (N/mm) was defined as the maximum slope over the second 30% interval of relative elongation. The inflection point was defined as the intercept of the two tangent lines fit in these two regions. The load (N) and relative elongation (%) at failure were also recorded.
An additional three samples per mesh type (n = 3) were cyclically tested (C1–C3) in order to further assess the permanent elongation of the mesh described previously [13]. This test is designed to assess how the meshes will respond to repetitive loading, i.e.,under the assumption that the prolapse meshes will sustain repetitive subfailure loads in vivo as a result of activities that increase intra-abdominal pressure during the early postoperative period. Briefly, samples were preloaded to 0.1 N at a rate of 10 mm/min, and the cross-head position was set to zero. The clamp-to-clamp distance was measured; meshes were then cycled from 0.5 to 5 N (C1), 0.5–15 N (C2), and finally 0.5–5 N (C3), each for ten cycles. The relative elongation after each portion of the cyclical loading protocol (C1–C3) was again measured by applying a 0.1-N preload and measuring the difference between the current crosshead position and its initial position. This represented the permanent deformation of the mesh in response to cyclical loading.
Statistical analysis
Sample size calculations were based on initial data from a previous study [13] that tested Gynecare TVT™ slings. Five samples per group were needed to detect a minimum of 100% difference in low stiffness, 15% difference in the inflection point, and 75% difference in permanent elongation between Gynecare and other brands with 80% power. A one-way analysis of variance was used to assess differences between groups. A post hoc comparison was performed using Dunnett’s multiple comparison procedure.
Results
Analysis by light microscopy revealed that in spite of being manufactured from a common material (polypropylene), the knit patterns for all the meshes were distinct (Fig. 1). Pore diameters were as follows: Pelvitex, 1.36 mm; Popmesh, 2.37 mm; Gynecare, 2.44 mm; Polyform, 1.73 mm; and Timesh, 1.71 mm. In terms of area, Gynecare PS had the largest pore size at 5.82 mm2 (2.44 mm diameter) and Timesh had the smallest at 1.16 mm2 (1.71 mm diameter). The results of the mechanical testing protocol revealed that the general shape of most of the load–relative elongation curves for each mesh type were bilinear (Fig. 2). In other words, there were two distinct regions of stiffness (slope) within the curves. Initially, these curves displayed a region of low stiffness (lower slope value or flatter curve) at which time the meshes easily deformed under the application of even a small load (e.g., 2 lbs). This was followed by a transition into a region of high stiffness (high slope value and steep curve) indicating that the mesh had become more resistant to deformation. We use the term “inflection point” to quantitate the point of transition between the low- and high-stiffness regions. The inflection point observed in biomechanical testing corresponds to the point where the mesh transitioned from low (easily pulled apart) to high stiffness (resistant to deformation). This is clinically important because it corresponds to the forces at which mesh behaves more stiff, as mesh stiffness has been one of the parameters that have been hypothesized to contribute to exposures or erosions. This parameter is reported for all meshes, with the exception of Popmesh, which displayed a distinct uniform linear behavior (i.e., a single stiffness value throughout the test, see Fig. 3). As a result, for Popmesh, only one stiffness value is reported, and there was by definition no inflection point.
Comparisons between groups revealed that the low stiffness region was significantly higher for Gynecare (0.27 ± 0.09 N/mm) when compared to Pelvitex, Polyform, and Timesh at 0.07 ± 0.03, 0.05 ± 0.01, and 0.02 ± 0.01 N/mm, respectively. The corresponding stiffness of Popmesh in this region of the load–relative elongation curve was similar to Gynecare measuring 0.36 ± 0.09 N/mm. On average, the inflection point corresponded to approximately 10 N of applied load or roughly 2.2 lbs. At the inflection point, Gynecare, Polyform, Pelvitex, and Timesh elongated an average of 20% of their initial length, with relative elongation values of 33.33 ± 9.62%, 25.44 ± 7.09%, 41.28 ± 19.23%, and 18.03 ± 9.10% (p = .043), respectively. Thus, at loads less than 3 lbs, these meshes permanently deformed to exceed their initial length by roughly 3 cm. As stated previously, no value could be reported for Popmesh. In the high-stiffness region, the loads applied to the mesh likely exceed that which is expected under normal physiologic conditions. Nevertheless, Gynecare was the stiffest mesh in this region of the load–relative elongation curve with a slope of 1.25 ± 0.21 N/mm, p < 0.05, while the newer meshes were significantly less stiff, 0.36 ± 0.09, 0.69 ± 0.13, 0.87 ± 0.07, and 0.17 ± 0.013 N/mm (Popmesh, Polyform, Pelvitex, and Timesh respectively).
There was a strong positive correlation between mesh weight and load at failure (r = 0.938, p < 0.001). Mesh weight inversely correlated with load at failure with the lighter meshes failing at the lowest loads. There was a positive correlation with pore size and load at failure (r = 0.44, P = 0.023). Timesh and Popmesh failed at 9.62 ± 1.21 and 21.40 ± 6.13 N, corresponding to 61.66 ± 4.52% and 60.95 ± 9.96% relative elongation, respectively. For the remaining meshes, the failure behaviors were similar. Gynecare, Polyform, and Popmesh failed at 68.34 ± 12.45, 51.67 ± 8.53, and 55.35 ± 6.99 N, respectively, having reached 71.50 ± 2.97, 60.95 ± 9.96, 92.25 ± 16.70, and 100.65 ± 8.62% of their initial length. As previously observed, all meshes tended to fail near the clamp [13]. As a result, these data are likely underestimating the true failure values.
The cyclical loading protocol was developed to simulate repetitive loading that may occur in vivo in response to repetitive intermittent increases in intra-abdominal pressure (e.g., coughing, sneezing, and getting up from a chair). Typical curves for cyclical loading of Gynecare PS are shown in Fig. 4 and results are provided in Table 2. The permanent elongation after C1 (cycling between 0.5 and 5 N, 0.1–1.0 lbs, for 10 cycles) for the Gynecare mesh was different from all other samples tested. Gynecare samples elongated to 3.0% of its initial length, which was significantly lower than all other meshes, Popmesh elongated 9.2% ± 0.7 (p = .002), Polyform 11.3% ± 2.6 (p < 0.001), Pelvitex 19.9% ± 1.4 (p < 0.001), and Timesh 23.6% ± 1.0 (p < 0.001) after C1.
The permanent elongation after C2 (cycling between 0.5 and 15 N, 0.1–3 lbs, for 10 cycles) of the Gynecare mesh was also distinct from all other samples. After C2, Gynecare samples elongated to 20% of its initial length, which was significantly lower than all other meshes, Popmesh (31.6% ± 4.3, p = 0.003), Polyform (28.7% ± 2.4, p = 0.013), and Pelvitex (37.5 ± 2.8, p < 0.001).With the same loading protocol, Timesh failed as predicted from the load to failure data, as its average failure load (9.62 N) exceeded in C2. Permanent elongation remained significant after C3; this cycle repeated the loading conditions of C1. Gynecare samples remained elongated to 20% of the initial length, which was significantly lower than all other meshes, Popmesh (32.1% ± 4.0, p < 0.001), Polyform (29.6% ± 1.7, p = 0.002), and Pelvitex (39.5% ± 1.2, p < 0.001).
Discussion
We performed ex vivo uniaxial tensile testing of synthetic prolapse meshes to distinguish newer mesh tensile behavior relative to the original prolapse mesh Gynecare PS™. In order to simulate loading conditions to those after abdominal sacrocolpopexy, we utilized a uniaxial loading test. Our goal was to improve our understanding of how these modifications may impact in vivo behavior prior to launching in vivo studies. As the first mesh designed specifically for prolapse repairs and the most widely used synthetic mesh, Gynecare mesh was considered the “gold standard” in this study. The most important findings of the study were that relative to Gynemesh PS ™, the newer prolapse meshes have distinct tensile behaviors but are all generally less stiff (i.e., deform more easily under a given load). Indeed, at loads less than 3 lbs, these meshes irreversibly deformed by 3–20%.
All meshes (with the exception of Popmesh) displayed bilinear behavior demonstrating that they initially deform easily in response to a low load, but their stiffness increases by orders of magnitude as the load applied increases. Gynecare mesh was the stiffest mesh in the low-stiffness region and was roughly 2–10% stiffer than the newer prolapse meshes despite its larger pore size. Mesh erosion and exposure have previously been correlated to the stiffness of the mesh [15]. Erosions (or exposure) occur in up to 12.0% of patients when meshes are placed abdominally [16]. Increased mesh stiffness may translate into increased risk for exposure or erosion in the presence of excessive load bearing (e.g., heavy postoperative lifting or chronic coughing). Future studies in which host tolerability of a low- and high-stiffness mesh are compared in vivo will definitively determine the impact of decreased mesh stiffness on its biological behavior in vivo.
In the low-stiffness region, which corresponds to more physiologic loads experienced by the mesh in vivo, meshes deformed an average of 30% of their initial length. At failure, meshes were roughly 80% longer (10 cm) than their initial length. While the loads seen in the high-stiffness region (40 N or 10 lbs) and at failure (70 N or 15 lbs) can likely be considered supraphysiologic, the easy irreversible deformability at such low loads is surprising. Nevertheless, it appears that the decreasing mesh stiffness creates a tradeoff between improved host tolerability and increased susceptibility to permanent elongation and, hence, anatomical failure.
It does not appear that coating the meshes with synthetic or biological materials significantly impacts mechanical properties. The objective of these coatings is to provide a relative inert barrier between the host tissues and the graft so as to decrease the risk of mesh erosion and exposure. The titanium-coated Timesh™ failed easily at the lowest loads. Most likely, this is simply due to the lighter weight of the mesh rather than an effect of the titanium. Pevitex™, coated with a porcine derived collagen, elongated to more than 100% of its initial length before failure at 55 N. It is possible that in vivo, the activated collagen would allow this mesh to withstand greater loads prior to failure. However, it is unlikely that failure loads are clinically relevant and not likely to be attained in vivo.
With cyclical loading, we also observed that there is a significant amount of mesh deformation that is irreversible. This finding might be of considerable importance in the early postoperative period prior to tissue ingrowth when the mesh may possibly move more freely between host tissues. With continued consecutive increases in intra-abdominal pressure, meshes may undergo significant permanent alteration in length that could translate into early postoperative failures.
It is generally thought that increased pore size and overall porosity of a mesh improves host tolerability by reducing the mesh burden, thereby producing a less pronounced foreign body reaction. Surprisingly, the pore size of each of these newer meshes was smaller than that of Gynecare. Thus, although these meshes had smaller pore sizes and decreased porosity, they were less stiff. Future studies will be needed to determine whether the overall stiffness or porosity of a material has a greater impact on host tolerability. Clearly, all of these parameters will have to be investigated further in future in vivo studies to understand their relative impact on outcomes.
Currently, the emphasis in clinical outcomes following a mesh procedure has been the restoration of anatomy. Most studies are limited by a small sample size; a lack of a consensus on what defines an anatomic cure, and a failure to consistently report adverse outcomes. Procedures incorporating synthetic mesh continue to be plagued by high erosions rates, dyspareunia, de novo urgency, stress incontinence, and urinary retention [17]. Clinically and particularly problematic is the fact that on exam following surgery, synthetic meshes significantly change the texture of the vaginal wall and can be palpated as a stiff material below the surface of the vaginal epithelium. Moreover, the sites of graft placement have poor distensibility and flexibility indicating properties that are not compatible with those of the non-grafted vagina. It is unclear which characteristics of synthetic mesh contribute most significantly to postoperative morbidity. It is important however to establish a basis for which clinicians can recognize structural differences in the synthetic meshes available for prolapse repair.
The major weakness of this paper was the use of ex vivo tensile testing; therefore, the biological response to these meshes, their mechanical properties, pore size, and coating could not be determined. It is clear that such testing must be completed after the graft has been well incorporated into the host tissue, as there will be considerable load sharing between the mesh and the newly incorporated host tissue.
An editorial written by Isom-Batz and Zimmern stated that “as a group we must demand higher standards…many new products are used currently despite limited scrutiny regarding their safety and long term efficacy” [18]. By characterizing each of these meshes’ structural properties and design differences, we hope to provide a basis to help clinicians gain insight into the outcomes following mesh repair, which is a fundamental first step in allowing clinicians to reach a more educated decision for patient graft choice. Future studies will involve the use of an animal model to explore mesh behavior after periods of healing and host incorporation, enabling us to define parameters most relevant to clinicians in the selection of prolapse meshes.
References
Pulliam SJ, Ferzandi TR, Hota LS, Elkadry EA et al (2007) Use of synthetic Mesh in pelvic reconstructive surgery: a survey of attitudes and practice pattern of urogynecologists. Int Urogynecol J 11:1–9
Nygaard IE, McCreery R, Brubaker L, Connolly A Cundiff G, Weber AM, Zyczynski H, Pelvic Floor Disorders Network (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104:805–823
Nicita G (1998) A new operation for genitourinary prolapse. J Urol 160:741–745
Floof CG, Drutz HP, Waja L (1998) Anterior colporrhaphy reinforced with Marlex. Mesh for treatment of cystocele. Int Urogynecol J Pelvic Floor Dysfunct 9:200–2004
Jameson JS, Chia YW, Kamm MA et al (1994) Effects of age, sex, and parity on anorectal function. Br J Surg 81:1689–1692
Jones NHJ, Healy JC, King LJ (2003) Pelvic Connective Tissue resilience decreases with vaginal delivery, menopause and uterine prolapse. Br J Surg 90:466–472
Olsen AL, Smith VJ, Bergstom JO et al (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Chen CG, Ridgeway B, Paraiso MF (2007) Biologic grafts and Synthetic meshes in pelvic reconstructive Surgery. Clin Obstet and Gynecol 50(2):383–411
Dora C, Dimarco D, Zobitz M, Elliot D (2004) Time dependent variations in biomechanical properties of cadaveric fascia, porcine dermis, porcine small intestine submucosa, polypropylene mesh and autologous fascia in the rabbit model: implication for sling surgery. J Urol 171:1970–1973
Fenner DE (2000) New surgical mesh. Clin Obstet Gynecol 43:647–652
Amrute K, Badlani G (2006) Female incontinence: a review of biomaterials and minimally invasive techniques. Current Opinion Urol 16:54–59
Cosson M, Debodinance P, Boukerrou M, Chauvet MP, Lobry P, Crepin G, Ego A (2003) Mechanical properties of synthetic implants used in repair of prolapse and urinary incontinence in women: which is the ideal material. Int Urogynecol J 14:169–178
Amid PK (1997) Classification of biomaterials and their related complications in abdominal wall surgery. Hernia 1:15–21
Moalli PM, Papas N, Menefee S Abramowitch S (2008) Tensile properties of six commonly used mid-urethral slings. Int Urogynecol J 19:655–663
Kohli N, Walsh PM, Roat TW, Karram MM (1998) Mesh erosion after abdominal sacrocolpopexy. Obstet Gynecol 92:999–1004
Mistrangelo E, Mancuso S, Nadalini C, Lijoi D, Costantini L (2007) Rising use of synthetic mesh in transvaginal pelvic reconstructive surgery: A review of risk of vaginal erosion. J Minim Invasive Gynecol 14:564–569
Huebner M, Fenner DE (2006) The use of graft material in vaginal pelvic floor surgery. Int J Obstet Gynecol 92:279–288
Isom-Batz G, Zimmern PE (2007) Vaginal mesh for incontinence and/or prolapse: caution required!. Expert Rev Med Devices 4:675–679
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, K.A., Feola, A., Meyn, L. et al. Tensile properties of commonly used prolapse meshes. Int Urogynecol J 20, 847–853 (2009). https://doi.org/10.1007/s00192-008-0781-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-008-0781-x