Abstract
Berberine is a quaternary ammonium salt from the protoberberine group of isoquinoline alkaloids. It is found in such plants as Berberis [e.g. Berberis aquifolium (Oregon grape), Berberis vulgaris (barberry), Berberis aristata (tree turmeric)], Hydrastis canadensis (goldenseal), Xanthorhiza simplicissima (yellowroot), Phellodendron amurense [2] (Amur corktree), Coptis chinensis (Chinese goldthread), Tinospora cordifolia, Argemone mexicana (prickly poppy) and Eschscholzia californica (Californian poppy). In vitro it exerts significant anti-inflammatory and antioxidant activities. In animal models berberine has neuroprotective and cardiovascular protective effects. In humans, its lipid-lowering and insulin-resistance improving actions have clearly been demonstrated in numerous randomized clinical trials. Moreover, preliminary clinical evidence suggest the ability of berberine to reduce endothelial inflammation improving vascular health, even in patients already affected by cardiovascular diseases. Altogether the available evidences suggest a possible application of berberine use in the management of chronic cardiometabolic disorders.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
Cardiovascular diseases are yet the most common causes of death and one of the first causes of disability in industrialized countries and despite the efforts towards primary prevention of cardiovascular disease, many patients still remain at risk [1]. Lifestyle interventions such as diet and/or physical activity are the most cost-effective approach in delaying or preventing the onset of cardiovascular disease [2]. Moreover, people without a history of cardiovascular disease who lack common risk factors have a significantly greater risk of cardiovascular and all-cause mortality if they do not adhere to a healthy lifestyle [3]. However, lifestyle programs are often difficult to follow for long periods and some risk parameters, such as cholesterolemia, are relatively resistant to changes in dietary habits and physical activity [4]. On the other hand, a relatively large number of dietary supplements and nutraceuticals have been studied for their supposed or demonstrated ability to reduce cholesterolemia in humans [5]. The third National Cholesterol Educational Program suggested to integrate dietary supplements such as soluble fibres, omega-3 polyunsaturated fatty acids (PUFA), plant sterols and soy protein in the diet in order to achieve an optimal LDL-cholesterolemia [6]. These suggestions have been supported also by the recent new European guidelines of the management of dyslipidemias [7] that also cite some other nutraceuticals as potentially useful lipid-lowering substances. Since cardiovascular disease prevention needs a life course approach, both the tolerability and safety of dietary supplements/nutraceuticals used to control plasma cholesterol levels has to be adequately defined as well as the risk/benefit ratio of their assumption. A relatively large number of recent reviews already described the mechanism of action and the efficacy of the different nutraceuticals and botanicals with lipid-lowering effects [8–10]. In particular, Berberine (BBR) exhibits many different biological activities; among them, the best characterized are antioxidant, anti-inflammatory, cholesterol-lowering and anti-hyperglycemic effects.
2.1.1 Physico-Chemical and Pharmacological Properties of Berberine
Berberine is a quaternary ammonium salt from the group of isoquinoline alkaloids (2,3–methylenedioxy-9,10-dimethoxyprotoberberine chloride; C20H18NO4 +) with a molar mass of 336.36122 g/mol [11]. It is highly concentrated in the roots, rhizomes and stem bark of various plants including Coptis chinensis, Rhizoma coptidis, Hydrastis canadensis, Berberis aquifolium, Berberis vulgaris, Berberis aristata, Tinospora cordifolia, Arcangelisia flava and Cortex rhellodendri [12]. Berberine is strongly yellow coloured, which explains the fact that in the past berberis species were used to dye wool, leather and wood. Under ultraviolet light, berberine shows a strong yellow fluorescence with a Colour Index of 75,160 [13].
Berberis vulgaris as well as other berberine-containing plants [14] are used medicinally in virtually all-traditional medical systems, and have a history of usage in Ayurvedic, Iranian and Chinese medicine dating back at least 3000 years [16]. Ancient Egyptians used barberry fruit with fennel seeds to ward off pestilent fevers [15]. Indian Ayurvedic physicians used barberry in the treatment of dysentery and traditional Iranian medicine uses its fruit as a sedative [15, 17]. In northern Europe, barberry was used to treat gall bladder and liver problems, while it was used in the treatment of abnormal uterine bleeds and rheumatism in Russia and Bulgaria [18, 19]. In North America, the Eclectics used barberry for treatment of malaria and as a general tonic [20]. Also, the American Indians found it effective in improving appetite and used its dried fruit as a gargle [21, 22].
Medicinal properties for all parts of the plant have been reported, including tonic, antimicrobial, antiemetic, antipyretic, antipruritic, antioxidant, anti-inflammatory, hypotensive, antiarrhythmic, sedative, antinociceptive, anticholinergic and cholagogue actions, and it has been used in some cases like cholecystitis, cholelithiasis, jaundice, dysentery, leishmaniasis, malaria and gall stones [23]. Furthermore, berberine has been used for treating diarrhoea and gastrointestinal disorders for a long time [24, 25]. It has multiple pharmacological effects including; antimicrobial activity against 54 microorganisms [26], inhibition of intestinal ion secretion and smooth muscle contraction, inhibition of ventricular tachyarrhythmia, reduction of inflammation, stimulation of bile secretion and bilirubin discharge [27].
Berberine has low bioavailability and poor absorption through the gut wall (<5 %) and bowel P-glycoprotein contributes to that, actively expelling the alkaloid from the lumen mucosal cells [28].
In a rat noncompartmental model [29], unbound berberine is transported to bile through active transportation and it is metabolized by P450 enzyme system in liver, with phase I demethylation and phase II glucuronidation. Berberine has four main metabolites identified in rats: berberrubine, thalifendine, demethyleneberberine and jatrorrhizine, and all of them have glucuronide conjugates [30]. Intestinal bacterial flora takes role in enterohepatic circulation of berberine and its conjugated metabolites [28]. On the other hand, very small amount of unchanged berberine is eliminated in urines [31].
As other alkaloids are present in H. canadensis extracts (i.e. hydrastine and canadine), berberine may inhibit cytochrome P450 2E1 (CYP2E1) [32] and 1A2 (CYP1A2) [33]. This inhibition is not related to a significant increase in pharmacological interactions since the largest part of the available drugs is not metabolized by these enzymatic systems.
2.1.2 Berberine Modulation of Cell Signalling Pathways
Berberine is a potent antioxidant and anti-inflammatory agent: these properties could be particularly relevant in the management of type 2 diabetes and cardiovascular diseases.
In metabolic disorders, as obesity and type 2 diabetes, increased oxidative stress is a common feature [34, 35]. It could induce or deteriorate insulin resistance and diabetes through multiple mechanisms. In the process of oxidative stress, excessive reactive oxygen species (ROS) are produced, mainly by mitochondria [36, 37]. They could cause damage and apoptosis of pancreatic islet β-cells and reduction of insulin secretion [38]. ROS also activate c-Jun N-terminal kinase (JNK), protein kinase C (PKC) and nuclear factor-κB (NF-κB), interfering with the insulin signalling pathway and causing insulin resistance [39–41]. In addition, oxidative stress also contributes to the development of chronic complications of diabetes, such as diabetic nephropathy, retinopathy and neuropathy [37].
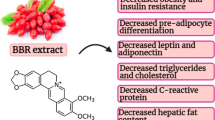
Molecular mechanisms of berberine in reducing oxidative stress seem to be related with multiple cellular pathways (Fig. 2.1).
Schematic illustration of the molecular mechanisms and pathways of Berberine in reducing oxidative stress and inflammation. 1 Berberine could inhibit oxidative stress by upregulation of SOD, and downregulation of NADPH oxidase expression. 2 Berberine administration induces the activation of the Nrf2 transcription. The effect of berberine on Nrf2 relies on the activation of AMPK, and P38 pathways. 3 Berberine could suppress inflammation by blocking the MAPK pathways in an AMPK-dependent manner, inhibiting the classic NF-κB transcription; inhibiting the Rho GTPase pathway, which plays a role in NF-κB regulation, and attenuating the transcription activity of AP-1, which was possible to be mediated by PPARγ activation
The NOX family of ROS-generating NADPH oxidases, a family of membrane-associated enzymatic complexes, is one of the major sources of ROS production in cells [42]; its activation is often associated to high levels of fatty acids, cholesterol, glucose or advanced glycation end products (AGEs) [43–45]. Among various NOX isoforms, berberine was reported to suppress the overexpression of NOX 2,4 and to decrease ROS production in macrophages and endothelial cells upon stimulation with inflammatory stimuli [46, 47]. In endothelial cells, berberine attenuated LDL oxidation induced by ROS and reduces the collapse of mitochondrial membrane potential, the chromosome condensation, the cytochrome C release and the caspase-3 activation [48]. Circulating endothelial microparticles, vesicular structures found in plasma from patients with vascular diseases so utilized as a surrogate marker of endothelial dysfunction, are oxidative stress inducers; they promote upregulation of NOX4 expression and ROS production. It has been reported that berberine reversed NOX4-derived ROS production in human umbilical vein endothelial cells (HUVECs) [46].
NOX could be negatively regulated by adenosine monophosphate-activated protein kinase (AMPK) activation [49, 50]; in fact AMPK activators, such as metformin, may exert their cardiovascular protective function through NOX inhibition [51]. AMPK pathway is activated by berberine [52] and it seems to play a pivotal role in mediating its antioxidant activity [53, 54].
The AMPK is a ubiquitously expressed cellular energy sensor and an essential component of the adaptive response to cardiomyocyte stress that occurs during ischemia. AMPK plays also an important role in regulating function of NO synthesis in endothelial cells. In fact, AMPK is an upstream kinase of endothelial nitric oxide synthase (eNOS) which promotes the phosphorylation of eNOS at Ser1177 site as well as the formation of eNOS and HSP90 complex and NO production [55]. Zhang et al. [56] observed that in HUVECs berberine ameliorated palmitate-induced endothelial dysfunction by upregulating eNOS and downregulating of NOX4 through the activation of AMPK. In both cultured endothelial cells and blood vessels isolated from rat aorta berberine enhanced eNOS phosphorylation and attenuated high glucose-induced generation of ROS, cellular apoptosis, NF-κB activation and expression of adhesion molecules through AMPK signalling cascade activation, a key event in preventing oxidative and inflammatory signalling [57].
Besides NADPH oxidase downregulation and NO production, AMPK activation has been linked to upregulation of the antioxidant enzyme superoxide dismutase (SOD) [58, 59], which is dismutated to hydrogen peroxide. It was observed an increased SOD expression in berberine treated diabetic mice [60, 61]. Glutathione (GSH) is another antioxidant molecule which helps to maintain the balance of redox state in organisms and acting asco-substrate of glutathione peroxidase (GSH-Px) in the clearance of peroxides [62]. Berberine treatment promoted a GSH-Px and SOD hyperactivation in the liver of mice [63], attenuated ROS production and increased detoxifying enzymes GSH-Px and SOD in NSC34 motor neuron-like cells [64].
Recent studies revealed that berberine suppressed oxidative stress through induction of the nuclear factor erythroid-2-related factor-2 (Nrf2) pathway [65–67]. Nrf2 is a transcription factor which binds to antioxidative response elements (ARE) in DNA, leading to transcription of phase II enzymes and cytoprotective proteins genes such as NAD(P)H quinone oxidoreductase-1 (NQO-1) and heme oxygenase-1 (HO-1) with a wide range of activities in regulating redox state and energy metabolism in cells [68]. Now, Nrf2 is recognized as an important mediator of berberine in reducing oxidative stress, as blocking Nrf2 abolishes the antioxidant activity of berberine in macrophages and nerve cells [65–67]. The activation of AMPK, phosphatidylinositol 3-kinase (PI3K)/Akt and p38 kinase cellular pathways is involved in the effect of berberine on Nrf2, since the block of these pathways diminishes the stimulating effect of berberine on Nrf2 [65–67].
The anti-inflammatory activity of berberine was observed both in vitro and in vivo and was noted by the reduction of proinflammatory cytokines as well as acute phase proteins [69–78].
In cultured metabolically active cells (adipocytes and liver cells), immunocytes (macrophages and splenocytes) or pancreatic β-cells, berberine treatment reduced the production of TNF-α, IL-6, IL-1β, matrix metalloprotease 9 (MMP9), cyclooxygenase-2 (COX2), inducible NOS (iNOS), monocyte chemoattractant protein 1 (MCP-1) and C-reactive protein (CRP) and haptoglobin (HP) [70–100]. In insulin-resistant HepG2 cells, the anti-inflammatory activity of berberine was associated with its insulin-sensitizing effect. Berberine administration significantly decreased cytokine production, and reduced serine phosphorylation but increased insulin-mediated tyrosine phosphorylation of IRS in HepG2 cells treated with palmitate [71].
Berberine could reduce proinflammatory cytokines, acute phase protein and infiltration of inflammatory cells in animals with diabetes mellitus or insulin resistance, either induced by streptozocin injection/high-fat diet (HFD) feeding or spontaneously happened [69, 72, 74–76]. In these animal models, the anti-inflammatory activity of berberine was observed in different tissues like serum, liver, adipose tissue, and kidney and was associated with its effect against insulin resistance or diabetes mellitus [69, 72, 74–76]. Besides evidences from cultured cells and diabetic animal models, the anti-inflammatory effect of berberine was also observed in humans: the berberine dose of 1 g/day for 3 months significantly reduced the serum hsCRP and IL-6 level in patients with acute coronary syndrome following percutaneous coronary intervention [80].
Berberine suppresses inflammation through complex mechanisms. In addition to antioxidant activity, the AMPK pathway was also crucial for the anti-inflammatory efficacy of berberine [72]. Blocking AMPK could abolish the inhibitory effect of berberine on the production of proinflammatory cytokines, like inducible nitric oxide synthase (iNOS) and COX2 in macrophages [72]. Excessive iNOS in cells could cause overproduction of NO and had close relationship with the development of insulin resistance [82]. COX2 is a key enzyme for the synthesis of prostaglandins [81], which are important mediators for the pathogenesis of diabetes mellitus and diabetic nephropathy [82].
The anti-inflammatory activity of berberine was also associated with its inhibitory effect on the mitogen-activated protein kinase (MAPK) signalling pathways, which were activated by inflammatory stimuli [72, 83, 84]. The inhibitory effect of berberine on MAPKs was dependent on AMPK activation in macrophages [72]. It seems that conflicting results exist concerning the regulatory effect of berberine on MAPK signalling. Although some results suggested that berberine suppressed the inflammation through inhibiting MAPKs [72, 83, 84], others indicated that p38 kinase was activated by berberine which was considered important for berberine’s efficacy against oxidative stress and inflammation [65–67].
The NF-κB pathway plays a key role in controlling inflammation [85]. In NF-κB signalling pathway, IκB kinase-β (IKK-β) could be activated by inflammatory stimuli like TNF-α, as well as nutritional factors like glucose and FFA [86]. The activation of IKK-β required phosphorylation of the serine residue at position 181 [87, 88]. In insulin-resistant 3T3-L1 adipocytes [89] and liver/adipose tissues from obese mice feed with HFD [74], berberine administration greatly reduced phosphorylation of ser181 and activation of IKK-β. In addition, the inhibitory effect of berberine on IKK-β required a cysteine residue at position 179 of IKK-β [89].
Recent studies proved that berberine could reduce renal inflammation in diabetic rats through inhibiting the Rho GTPase signalling pathway [69]. Rho GTPase is a member of the superfamily of small GTP binding proteins with multiple biological functions [90]; it was proven to positively regulate the NF-κB signalling pathway in diabetic rats [91]. Therefore, in addition to regulation of the classic NF-κB signalling pathway, berberine could inhibit NF-κB by suppressing Rho GTPase [69, 92]. Furthermore, the inhibitory effect of berberine on Rho GTPase relied on its antioxidant activity [69].
In addition to NF-κB, transcription factor activator protein 1 (AP-1) also played a role in the anti-inflammatory activity of berberine [93, 94]. Administration of berberine to macrophages or epithelial cells greatly attenuated the DNA binding activity of AP-1 and reduced the production of cytokines like MCP-1 and COX2 [93]. There were reports that the transcription stimulating activity of AP-1 and NF-κB could be inhibited by activation of peroxisome proliferator-activated receptor γ (PPARγ) [95–99].
2.1.2.1 Berberine Effects on Glucose Metabolism
In general, there are two distinct pathways to activate glucose uptake in peripheral tissues; one stimulated by insulin through the IRS-1/PI 3-kinase and the other by exercise or hypoxia via activation of AMP activated protein kinase (AMPK). In muscle, which is the major tissue responsible for whole body glucose disposal after liver, both pathways stimulate the translocation of glucose transporter-4 (GLUT4) to the cell membrane which accounts for the enhanced glucose uptake [100].
Current data suggest that the berberine effects are complex and may activate portions of both the insulin and the exercise-induced glucose uptake pathways [101]. In addition, berberine inhibits intestinal absorption of glucose, which also contributes to berberine glucose-lowering effect [102].
There is increasing evidence that the most widely expressed GLUT1, initially thought to be responsible only for basal glucose uptake, can be acutely activated by cell stressors such as azide [103, 104], osmotic stress [105, 106], methylene blue [107] and glucose deprivation [108, 109]. In particular, the acute activation of GLUT1 by hypoxia or azide has been attributed to activation of AMPK [110, 111]. In addition, it has been recently shown that peptide C activates GLUT1 transport activity in erythrocytes, establishing a potential link between GLUT1 activity and diabetes [112].
In cultured human liver cells and rat skeletal muscle, berberine increases insulin receptor mRNA expression through Protein kinase C-dependent activation of its promoter [113].
Since berberine was observed to act as an insulin-sensitizing agent in cultured cells [114], its activity has been compared with that of metformin in different animal models. In rat models of type 2 diabetes (T2DM), berberine shows to have equal or better fasting plasma glucose (FPG), insulin-resistance and low-density lipoprotein cholesterol (LDL-C) lowering activity than metformin by a mechanism involving retinol binding protein-4 (RBP-4) and (GLUT-4) [115, 116].
Berberine exhibited a high hypoglycemic potential; it has been shown that berberine activates AMPK with subsequent induction of glycolysis [117]. AMPK, as an intracellular energy receptor, has attracted more attention and become a new target for the treatment of diabetes and its cardiovascular complications due to its regulatory effect on endothelial cell function and energy homeostasis. In H9c2 myoblast cell line treated with insulin to induce insulin resistance, berberine attenuated the reduction in glucose consumption and glucose uptake at least in part via stimulation of AMPK activity [118]. berberine enhanced acute insulin-mediated GLUT4 translocation and glucose transport in insulin-resistant myotubes through activation of AMPK and PI3K pathway [119] (Fig. 2.2).
In a clinical study, the same group observed that berberine significantly lowered FPG, hemoglobin A1c, triglycerides and insulin levels in patients with T2DM as well as metformin and rosiglitazone (a combination commonly used for the T2DM therapy); the percentages of peripheral blood lymphocytes expressing InsR were significantly elevated after therapy [120].
In a recent meta-analysis of randomized clinical trials, berberine resulted to be safe and effective in the treatment of patients with T2DM [121].
2.1.2.2 Berberine Effects on Lipid Metabolism and Vascular Health
The cholesterol and triglycerides lowering effect of berberine has been clearly demonstrated by a recent meta-analysis of randomized clinical trials [122]. The lipid-lowering activity of berberine, in association with other nutraceuticals, has been also clearly confirmed in a relatively large number of randomized clinical trials [123, 124].
The supposed mechanism of action is the increased expression of the liver receptor for LDL mediated by the inhibition of the Pro-protein-convertase-subtilisin-kexin-9 (PCSK9) activity [125]. Besides its upregulation effect on the LDL receptor, berberine could also reduce triglycerides by AMP kinase activation and MAPK/ERK pathway blocking [126] (Fig. 2.3).
High levels of LDL and their oxidized counterpart, oxidized LDL (oxLDL), in the blood vessels represent a major risk factor for endothelial dysfunction and atherosclerosis [127]. Inactivity of LDL receptor (LDLR) or its low-level expression initiates accumulation of LDL in blood vessels [128]. On the other hand, the receptor of oxLDL, lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1) identified as the main endothelial receptor for oxLDL also present in macrophages and smooth muscle cells (SMC), activates a proatherogenic cascade by inducing endothelial dysfunction, SMC proliferation, apoptosis and the transformation of macrophages into foam cells and platelet activation via NF-κB activation [129]. LOX-1 contains a lectin-like extracellular C-terminal domain which interacts with oxLDL, proteolytically cleaved and released as a soluble circulating form (sLOX-1) that reflects the increased expression of membrane-bound receptors and disease activities [130].
In human macrophage-derived foam cells treated with oxLDL, berberine inhibits the expression of LOX-1 [131] as well as the oxLDL uptake of macrophages and reduces foam cell formation in a dose-dependent manner [132] by activating the AMPK-SIRT1-PPARγ pathway [133]. Chi and colleagues demonstrated that berberine combined with atorvastatin is more effective in diminishing LOX‑1 expression than atorvastatin alone in monocyte-derived macrophages both in vitro and in rats through modulation of endothelin-1 receptor [134].
Berberine improves also the survival of TNFα-treated endothelial progenitor cells (EPCs) via the activation of PI3K/AKT/eNOS transcription factor [135] possibly through AMPK activation. Wu and colleagues showed, both in vitro and in vivo that berberine reduces the leukocyte-endothelium adhesion and vascular cell adhesion molecule-1 (VCAM-1) expression induced by LPS. Berberine was further confirmed to inhibit the nuclear translocation and DNA binding activity of LPS-activated NF-κB signalling pathway [136].
2.1.2.3 Berberine and Central Nervous System Disorders
A large number of preclinical evidence support a possible role of berberine in the management of Alzheimer’s disease, cerebral ischemia, mental depression, schizophrenia and anxiety, however the most part of these data have been obtained in purely experimental models [137]. Of particular interest is the potential antidepressant effect of berberine.
Berberine inhibited the immobility period in mice in both forced swim and tail-suspension test, two animal models of depression, in a dose independent manner [138, 139]. Among the reported bioactivities of berberine, there is the inhibition of monoamino oxidase (MAO)-A activity, [140] an enzyme catalyzing the oxidative deamination of catecholamines, and thus inhibiting degradation of these neurotransmitters. In fact acute and chronic administration of berberine in mice resulted in increased levels of norepinephrine, serotonin and dopamine, neurotransmitters induced by MAO-A enzyme [140]. In accordance with Kulkarni and colleagues data, Arora and Chopra [138] showed the protective antidepressant-like effect of berberine against the reserpine-induced biogenic amine depletion (a monoamine depletor commonly used to induce depression in animals. However, at the best of our knowledge, there are no available data on the evaluation of the potential antidepressant effects of berberine in humans [141].
2.1.2.4 Tolerability and Safety
Highly purified and concentrated berberine is safe, in fact, its Lethal Dose 50 (LD50) in mice is 25 mg/kg in mice [131].
Standard doses of berberine are usually well tolerated and adverse events are rare and mild. The most studied side effects are those on the gastrointestinal system. In fact, berberine and its derivatives can produce gastric lesions in animal models [142]. As shown by the determination of small intestinal transit time measurements by sorbitol and breath hydrogen test, berberine delays small intestinal transit time, and this may account for a part of its gastrointestinal side effects (but also of its antidiarrhoeal one) [143].
The main safety issue of berberine involves the risk of pharmacological interactions. In fact, berberine displaces bilirubin from albumin about tenfold more than phenylbutazone, thus any herb containing large amounts of berberine should be avoided in jaundiced infants and pregnant women [144]. Berberine also displaces warfarin, thiopental and tolbutamide from their protein binding sites, increasing their plasma levels [145].
Then, berberine can markedly increase blood levels of cyclosporine A because of CYP3A4 and P-glycoprotein inhibition in liver and gut wall, respectively, and because of the increase in gastric emptying time, thus causing increased cyclosporine A bioavailability and reduced metabolism [146]. In renal transplant recipients who take cyclosporine 3 mg/kg twice daily, the coadministration of berberine (0.2 g/day for three times a day for 3 months) increased the mean cyclosporine A AUC of 34.5 % and its mean half-life of 2.7 h [147].
Even if the main mechanism of berberine pharmacological interaction involves CYP3A4 and intestinal P-glycoprotein, it also inhibits CYP1A1, potentially interacting with drugs metabolized by this cytochrome isophorm as well. The impact of this observation in clinical practise has yet to be evaluated since the CYP1A1 metabolized drugs are relatively rare [148].
Overall, the assumption of berberine in dosages of 500–1000 mg/day has to be considered safe for the most part of subjects and the risk of clinically relevant pharmacological interaction is limited to cyclosporine and warfarin.
2.2 Conclusion
Berberine is a natural alkaloid with proven antioxidant, anti-inflammatory, glucose-lowering and lipid-lowering actions, both in animal models and in humans. Altogether, these effects support the need to study the effects of the long-term exposition to berberine for the management and prevention of numerous chronic diseases such as type 2 diabetes and atherosclerosis.
References
Banegas JR, López-García E, Dallongeville J et al (2011) Achievement of treatment goals for primary prevention of cardiovascular disease in clinical practice across Europe: the EURIKA study. Eur Heart J 32:2143–2152
Saha S, Gerdtham UG, Johansson P (2010) Economic evaluation of lifestyle interventions for preventing diabetes and cardiovascular diseases. Int J Environ Res Public Health 7:3150–3195
King DE, Mainous AG, Matheson EM, Everett CJ (2013) Impact of healthy lifestyle on mortality in people with normal blood pressure, LDL cholesterol, and C-reactive protein. Eur J Cardiovasc Prev Rehabil 20(1):73–79
Cicero AF, Derosa G, D’angelo A et al (2009) Gender-specific haemodynamic and metabolic effects of a sequential training programme on overweight-obese hypertensives. Blood Press 18:111–116
Cicero AF, Ertek S (2008) Natural sources of antidyslipidaemic agents: is there an evidence-based approach for their prescription? Med J Nutr Metab 2:85–93
NCEP Expert Panel (2001) Expert Panel on detection, evaluation and treatment of high blood cholesterol in adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) (Adult Treatment Panel III). J Am Med Assoc 285:2486–2497
Catapano AL, Reiner Z, De Backer G et al (2011) European Society of Cardiology (ESC); European Atherosclerosis Society (EAS). ESC/EAS Guidelines for the management of dyslipidaemias The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis 217:3–46
Hasani-Ranjbar S, Nayebi N, Moradi L et al (2010) The efficacy and safety of herbal medicines used in the treatment of hyperlipidemia: a systematic review. Curr Pharm Res 16:2935–2947
McGowan MP, Proulx S (2009) Nutritional supplements and serum lipids: does anything work? Curr Atheroscler Rep 11:470–476
Kim JY, Kwon O (2011) Culinary plants and their potential impact on metabolic overload. Ann NY Acad Sci 1229:133–139
Xia X, Weng J (2010) Targeting metabolic syndrome: candidate natural agents. J Diabetes 2:243–249
Birdsall TC, Kelly GS (1997) Berberine: therapeutic potential of an alkaloid found in several medicinal plants. Altern Med Rev 2:94–103
Vuddanda PR, Chakraborty S, Singh S (2010) Berberine: a potential phytochemical with multispectrum therapeutic activities. Expert Opin Investig Drugs 19:1297–1307
Souri E, Dehmobed-Sharifabadi A, Nazifia A, Farsam H (2004) Antioxidant activity of sixty plants from Iran. Iran J Pharm Res 13:55–59
Chevallier A (2001) The encyclopedia of medicinal plants. Dorling Kindersley, St Leonards, pp 234–237
Timothy CBN, Gregory S, Kelly ND (1997) Berberine: therapeutic potential of an alkaloid found in several medicinal plants. Altern Med Rev 13:94–103
Kunwar RM, Nepal BK, Kshhetri HB et al (2006) Ethnomedicine in Himalaya: a case study from Dolpa, Humla, Jumla and Mustang districts of Nepal. J Ethnobiol Ethnomed 13:27
Fatehi-Hassanabad Z, Jafarzadeh M, Tarhini A, Fatehi M (2005) The antihypertensive and vasodilator effects of aqueous extract from Berberis vulgaris fruit on hypertensive rats. Phytother Res 13(3):222–225
Ivanovska N, Philipov S (1996) Study on the anti-inflammatory action of Berberis vulgaris root extract, alkaloid fractions and pure alkaloids. Int J Immunopharmacol 13(10):553–561
Imanshahidi M, Hosseinzadeh H (2008) Pharmacological and therapeutic effects of Berberis vulgaris and its active constituent, Berberine. Phytother Res 13:999–1012
Mills S, Bone K (2000) Principals and practice of phytotherapy. Churchill Livingstone, Edinburgh, pp 338–341
Bone K (2003) A clinical guide to blending liquid herbs: herbal formulations for the individual patient. Churchill Livingstone, St Louis, pp 422–429
Khosrokhavar R, Ahmadiani AS (2010) Antihistaminic and anticholinergic activity of methanolic extract of barberry fruit (Berberis vulgaris) in the Guinea-Pig Ileum. J Med Plants 13:99–105
Akhter MH, Sabir M, Bhide NK (1979) Possible mechanism of antidiarrheal effect of berberine. Indian J Med Res 13:233–241
Rabbani GHBT, Knight J, Sanyal SC, Alam K (1987) Randomized controlled trial of berberine sulfate therapy for diarrhea due to enterotoxigenic Escherichia coli and Vibrio cholera. J Infect Dis 13:979–984
Amin AH, Subbaiah TV, Abbasi KM (1969) Berberine sulfate: antimidrobial activity, bioassay, and mode of action. Can J Microbiol 13:1067–1076
Sabir M (1971) Study of some pharmacological actions of berberine. Indian J Physiol Pharmacol 13:111–132
Pan GY, Wang GJ, Liu XD, Fawcett JP, Xie YY (2002) The involvement of P-glycoprotein in berberine absorption. Pharmacol Toxicol 91:193–197
Tsai PL, Tsai TH (2003) Hepatobiliary excretion of berberine. Drug Metab Dispos 32:405–412
Zuo F, Nakamura N, Akao T, Hattori M (2006) Pharmacokinetics of berberine and its main metabolites in conventional and pseudo germ-free rats determined by liquid chromatography/ion trap mass spectrometry. Drug Metab Dispos 34:2064–2072
Chen CM, Chang HC (1995) Determination of berberine in plasma, urine and bile by high performance liquid chromatograpy. J Chromatogr 665:117–123
Raner GM, Cornelious S, Moulick K et al (2007) Effects of herbal products on human cytochrome P450(2E1) activity. Food Chem Tox 45:2359–2365
Zhao X, Zhang JJ, Wang X et al (2008) Effect of berberine on hepatocyte proliferation inducible nitric oxide synthase expression, cytochrome 450 2E1 and 1A2 activities in diethylnitrosamine- and Phenobarbital-treated rats. Biomed Pharmacother 62:567–572
Furukawa S, Fujita T, Shimabukuro M et al (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Investig 114(12):1752–1761
Bonnefont-Rousselot D (2002) Glucose and reactive oxygen species. Curr Opin Clin Nutr Metab Care 5(5):561–568
Alberici LC, Vercesi AE, Oliveira HC (2011) Mitochondrial energy metabolism and redox responses to hypertriglyceridemia. J Bioenerg Biomembr 43(1):19–23
Rösen P, Nawroth PP, King G et al (2001) The role of oxidative stress in the onset and progression of diabetes and its complications: a summary of a congress series sponsored by UNESCO-MCBN, the American diabetes association and the German diabetes society. Diab Metab Res Rev 17(3):189–212
Evans JL, Goldfine ID, Maddux BA, Grodsky GM (2003) Are oxidative stress—activated signaling pathways mediators of insulin resistance and β-cell dysfunction? Diabetes 52(1):1–8
Kaneto H, Xu G, Fujii N, Bonner-Weir S, Weir GC (2002) Involvement of c-Jun N-terminal kinase in oxidative stress-mediated suppression of insulin gene expression. J Biol Chem 277(33):30010–30018
Scivittaro V, Ganz MB, Weiss MF (2000) AGEs induce oxidative stress and activate protein kinase C-β(II) in neonatal mesangial cells. Am J Physiol 278(4):F676–F683
Goldin A, Beckman JA, Schmidt AM, Creager MA (2006) Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation 114(6):597–605
Frey RS, Ushio-Fukai M, Malik AB (2009) NADPH oxidase-dependent signaling in endothelial cells role in physiology and pathophysiology. Antioxid Redox Signal 11:791–810
Furukawa S, Fujita T, Shimabukuro M et al (2004) Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Investig 114:1752–1761
Maiese K (2015) New insights for oxidative stress and diabetes mellitus. Oxid Med Cell Longev 2015:875961
Wu XD, Liu WL, Zeng K et al (2014) Advanced glycation end products activate the miRNA/RhoA/ROCK2 pathway in endothelial cells. Microcirculation 21(2):178–186
Cheng F, Wang Y, Li J et al (2013) Berberine improves endothelial function by reducing endothelial microparticles-mediated oxidative stress in humans. Int J Cardiol 167:936–942
Sarna LK, Wu N, Hwang SY, Siow YL, O K (2010) Berberine inhibits NADPH oxidase mediated superoxide anion production in macrophages. Can J Physiol Pharmacol 88:369–378
Hsieh S, Kuo WH, Lin TW et al (2007) Protective effects of berberine against low-density lipoprotein (LDL) oxidation and oxidized LDL-induced cytotoxicity on endothelial cells. J Agric Food Chem 55:10437–10445
Kim JE, Kim YW, Lee IK et al (2008) AMP-activated protein kinase activation by 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR) inhibits palmitate-induced endothelial cell apoptosis through reactive oxygen species suppression. J Pharmacol Sci 106:394–403
Wang S, Zhang M, Liang B et al (2010) AMPKα2 deletion causes aberrant expression and activation of NAD(P)H oxidase and consequent endothelial dysfunction in vivo: role of 26S proteasomes. Circ Res 106:1117–1128
Ceolotto G, Gallo A, Papparella I et al (2007) Rosiglitazone reduces glucose-induced oxidative stress mediated by NAD(P)H oxidase via AMPK-dependent mechanism. Arterioscler Thromb Vasc Biol 27:2627–2633
Lee KH, Lo HL, Tang WC et al (2014) A gene expression signature-based approach reveals the mechanisms of action of the Chinese herbal medicine berberine. Sci Rep 4:6394
Turner N, Li JY, Gosby A, To SW, Cheng Z, Miyoshi H et al (2008) Berberine and its more biologically available derivative, dihydroberberine, inhibit mitochondrial respiratory complex I: a mechanism for the action of berberine to activate AMP-activated protein kinase and improve insulin action. Diabetes 57(5):1414–1418
Li Z, Geng YN, Jiang JD, Kong WJ (2014) Antioxidant and anti-inflammatory activities of berberine in the treatment of diabetes mellitus. Evid Based Complement Alternat Med 2014:289264
Morrow VA, Foufelle F, Connell JM et al (2003) Direct activation of AMP-activated protein kinase stimulates nitric-oxide synthesis in human aortic endothelial cells. J Biol Chem 278:31629–31639
Zhang ZM, Jiang B, Zheng XX (2005) Effect of l-tetrahydropalmatine on expression of adhesion molecules induced by lipopolysaccharides in human umbilical vein endothelium cell. Zhongguo Zhong Yao Za Zhi 30(11):861–864
Wang Y, Huang Y, Lam KS et al (2009) Berberine prevents hyperglycemia-induced endothelial injury and enhances vasodilatation via adenosine monophosphate-activated protein kinase and endothelial nitric oxide synthase. Cardiovasc Res 82(3):484–492
Kukidome D, Nishikawa T, Sonoda K et al (2006) Activation of AMP-activated protein kinase reduces hyperglycemia-induced mitochondrial reactive oxygen species production and promotes mitochondrial biogenesis in human umbilical vein endothelial cells. Diabetes 55:120–127
Xie Z, Zhang J, Wu J, Viollet B, Zou MH (2008) Upregulation of mitochondrial uncoupling protein-2 by the AMP-activated protein kinase in endothelial cells attenuates oxidative stress in diabetes. Diabetes 57(12):3222–3230
Chatuphonprasert W, Lao-ong T, Jarukamjorn K (2013) Improvement of superoxide dismutase and catalase in streptozotocin-nicotinamide-induced type 2-diabetes in mice by berberine and glibenclamide. Pharm Biol (Epub ahead of print). doi:10.3109/13880209.2013.839714
Lao-ong T, Chatuphonprasert W, Nemoto N, Jarukamjorn K (2012) Alteration of hepatic glutathione peroxidase and superoxide dismutase expression in streptozotocin-induced diabetic mice by berberine. Pharm Biol 50(8):1007–1012
Ceballos-Picot I, Witko-Sarsat V, Merad-Boudia M et al (1996) Glutathione antioxidant system as a marker of oxidative stress in chronic renal failure. Free Radic Biol Med 21:845–853
Abd El-Wahab AE, Ghareeb DA, Sarhan EE et al (2013) In vitro biological assessment of Berberis vulgaris and its active constituent, berberine: antioxidants, anti-acetylcholinesterase, anti-diabetic and anticancer effects. BMC Complement Altern Med 13:218
Hsu YY, Chen CS, Wu SN, Jong YJ, Lo YC (2012) Berberine activates Nrf2 nuclear translocation and protects against oxidative damage via a phosphatidylinositol 3-kinase/Akt-dependent mechanism in NSC34 motor neuron-like cells. Eur J Pharm Sci 46:415–425
Mo C, Wang L, Zhang J et al (2014) The crosstalk between Nrf2 and AMPK signal pathways is important for the anti-inflammatory effect of berberine in LPS-stimulated macrophages and endotoxin-shocked mice. Antioxid Redox Signal 20(4):574–588
Hsu YY, Tseng YT, Lo YC (2013) Berberine, a natural antidiabetes drug, attenuates glucose neurotoxicity and promotes Nrf2-related neurite outgrowth. Toxicol Appl Pharmacol 272(3):787–796
Bae J, Lee D, Kim YK et al (2013) Berberine protects 6-hydroxydopamine-induced human dopaminergic neuronal cell death through the induction of heme oxygenase-1. Mol Cells 35(2):151–157
Vomhof-Dekrey EE, PickloSr MJ (2012) The Nrf2-antioxidant response element pathway: a target for regulating energy metabolism. J Nutr Biochem 23(10):1201–1206
Xie X, Chang X, Chen L et al (2013) Berberine ameliorates experimental diabetes-induced renal inflammation and fibronectin by inhibiting the activation of RhoA/ROCK signaling. Mol Cell Endocrinol 381(1–2):56–65
Choi B-H, Ahn I-S, Kim Y-H et al (2006) Berberine reduces the expression of adipogenic enzymes and inflammatory molecules of 3T3-L1 adipocyte. ExpMol Med 38(6):599–605
Lou T, Zhang Z, Xi Z et al (2011) Berberine inhibits inflammatory response and ameliorates insulin resistance in hepatocytes. Inflammation 34(6):659–667
Jeong HW, Hsu KC, Lee JW et al (2009) Berberine suppresses proinflammatory responses through AMPK activation in macrophages. Am J Physiol Endocrinol Metab 296(4):E955–E964
Lin W-C, Lin JY (2011) Five bitter compounds display different anti-inflammatory effects through modulating cytokine secretion using mouse primary splenocytes in vitro. J Agric Food Chem 59(1):184–192
Shang W, Liu J, Yu X, Zhao J (2010) Effects of berberine on serum levels of inflammatory factors and inflammatory signaling pathway in obese mice induced by high fat diet. Zhongguo Zhong Yao Za Zhi 35(11):1474–1477
Chen Y, Wang Y, Zhang J, Sun C, Lopez A (2011) Berberine improves glucose homeostasis in streptozotocin-induced diabetic rats in association with multiple factors of insulin resistance. ISRN Endocrinol 2011:519371
Xing L-J, Zhang L, Liu T (2011) Berberine reducing insulin resistance by up-regulating IRS-2 mRNA expression in nonalcoholic fatty liver disease (NAFLD) rat liver. Eur J Pharmacol 668(3):467–471
Cui G, Qin X, Zhang Y et al (2009) Berberine differentially modulates the activities of ERK, p 38 MAPK, and JNK to suppress Th17 and Th1 T cell differentiation in type 1 diabetic mice. J Biol Chem 284(41):28420–28429
Chueh WH, Lin JY (2012) Protective effect of isoquinoline alkaloid berberine on spontaneous inflammation in the spleen, liver and kidney of non-obese diabetic mice through downregulating gene expression ratios of pro-/anti-inflammatory and Th1/Th2 cytokines. Food Chem 131(4):1263–1271
Zhang Y, Li X, Zou D et al (2008) Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J Clin Endocrinol Metab 93(7):2559–2565
Meng S, Wang LS, Huang ZQ et al (2012) Berberine ameliorates inflammation in patients with acute coronary syndrome following percutaneous coronary intervention. Clin Exp Pharmacol Physiol 39(5):406–411
Dubois RN, Abramson SB, Crofford L (1998) Cyclooxygenase in biology and disease. FASEB J 12(12):1063–1073
Mima A (2013) Inflammation and oxidative stress in diabetic nephropathy: new insights on its inhibition as new therapeutic targets. J Diab Res 2013:248563
Lee D, Bae J, Kim YK et al (2013) Inhibitory effects of berberine on lipopolysaccharide-induced inducible nitric oxide synthase and the high-mobility group box 1 release in macrophages. Biochem Biophys Res Commun 431(3):506–511
Zhou Y, Liu SQ, Yu L et al (2015) Berberine prevents nitric oxide-induced rat chondrocyte apoptosis and cartilage degeneration in a rat osteoarthritis model via AMPK and p38 MAPK signaling. Apoptosis 20(9):1187–1199
Gratas-Delamarche A, Derbré F, Vincent S, Cillard J (2014) Physical inactivity, insulin resistance, and the oxidative-inflammatory loop. Free Rad Res 48(1):93–108
Solinas G, Karin M (2010) JNK1 and IKKbeta: molecular links between obesity and metabolic dysfunction. FASEB J 24(8):2596–2611
Karin M (1999) Positive and negative regulation of IκB kinase activity through IKKβ subunit phosphorylation. Science 284(5412):309–313
Yi P, Lu FE, Xu LJ et al (2008) Berberine reverses free-fatty-acid-induced insulin resistance in 3T3-L1 adipocytes through targeting IKKβ. World J Gastroenterol 14(6):876–883
Pandey MK, Sung B, Kunnumakkara AB et al (2008) Berberine modifies cysteine 179 of IκBα kinase, suppresses nuclear factor-κB-regulated antiapoptotic gene products, and potentiates apoptosis. Cancer Res 68(13):5370–5379
Shi J, Wei L (2013) Rho kinases in cardiovascular physiology and pathophysiology: the effect of fasudil. J Cardiovasc Pharmacol 62(4):341–354
Xie X, Peng J, Chang X et al (2013) Activation of RhoA/ROCK regulates NF-κB signaling pathway in experimental diabetic nephropathy. Mol Cell Endocrinol 369(1–2):86–97
Remppis A, Bea F, Greten HJ et al (2010) Rhizoma Coptidis inhibits LPS-induced MCP-1/CCL2 production in murine macrophages via an AP-1 and NFκB-dependent pathway. Mediat Inflamm 2010:194896
Kuo CL, Chi CW, Liu TY (2004) The anti-inflammatory potential of berberine in vitro and in vivo. Cancer Lett 203(2):127–137
Schonthaler HB, Guinea-Viniegra J, Wagner EF (2011) Targeting inflammation by modulating the Jun/AP-1 pathway. Ann Rheum Dis 70(1):i109–i112
Ricote M, Li AC, Willson TM et al (1998) The peroxisome proliferator-activated receptor-γ is a negative regulator of macrophage activation. Nature 391(6662):79–82
Delerive P, Martin-Nizard F, Chinetti G et al (1999) Peroxisome proliferator-activated receptor activators inhibit thrombin-induced endothelin-1 production in human vascular endothelial cells by inhibiting the activator protein-1 signaling pathway. Circ Res 85(5):394–402
Pasceri V, Wu HD, Willerson JT, Yeh ETH (2000) Modulation of vascular inflammation in vitro and in vivo by peroxisome proliferator-activated receptor-γ activators. Circulation 101(3):235–238
Chen FL, Yang ZH, Liu Y et al (2008) Berberine inhibits the expression of TNFα, MCP-1, and IL-6 in AcLDL-stimulated macrophages through PPARγ pathway. Endocrine 33(3):331–337
Feng AW, Gao W, Zhou GR et al (2012) Berberine ameliorates COX-2 expression in rat small intestinal mucosa partially through PPARγ pathway during acute endotoxemia. Int Immunopharmacol 12(1):182–188
Krook A, Wallberg-Henriksson H, Zierath JR (2004) Sending the signal: molecular mechanisms regulating glucose uptake. Med Sci Sports Exerc 36:1212–1217
Kim SH, Shin EJ, Kim ED (2007) Berberine activates GLUT1-mediated glucose uptake in 3T3-L1 adipocytes. Biol Pharm Bull 30:2120–2125
Pan GY, Huang ZJ, Wang GJ et al (2003) The antihyperglycaemic activity of berberine arises from a decrease of glucose absorption. Planta Med 69:632–636
Shetty M, Loeb JN, Vikstrom K, Ismail-Beigi F (1993) Rapid activation of GLUT-1 glucose transporter following inhibition of oxidative phosphorylation in clone 9 cells. J Biol Chem 268:17225–17232
Rubin D, Ismail-Beigi F (2003) Distribution of Glut1 in detergent-resistant membranes (DRMs) and non-DRM domains: effect of treatment with azide. Am J Physiol Cell Physiol 285:C377–C383
Barnes K, Ingram JC, Porras OH et al (2002) Activation of GLUT1 by metabolic and osmotic stress: potential involvement of AMP-activated protein kinase (AMPK). J Cell Sci 115:2433–2442
Barros LF, Barnes K, Ingram JC et al (2001) Hyperosmotic shock induces both activation and translocation of glucose transporters in mammalian cells. Pflugers Arch 442:614–621
Louters LL, Dyste SG, Frieswyk D et al (2006) Methylene blue stimulates 2-deoxyglucose uptake in L929 fibroblast cells. Life Sci 78:586–591
Kumar A, Xiao YP, Laipis PJ (2004) Glucose deprivation enhances targeting of GLUT1 to lipid rafts in 3T3-L1 adipocytes. Am J Physiol Endocrinol Metab 286:E568–E576
Roelofs B, Tidball A, Lindborg AE et al (2006) Acute activation of glucose uptake by glucose deprivation in L929 fibroblast cells. Biochimie 88:1941–1946
Jing M, Ismail-Beigi F (2007) Critical role of 5′-AMP-activated protein kinase in the stimulation of glucose transport in response to inhibition of oxidative phosphorylation. Am J Physiol Cell Physiol 292:C477–C487
Jing M, Cheruvu VK, Ismail-Beigi F (2008) Stimulation of glucose transport in response to activation of distinct AMPK signaling pathways. Am J Physiol Cell Physiol 295:C1071–C1082
Meyer JA, Froelich JM, Reid GE, Karunarathne WK, Spence DM (2008) Metal-activated C-peptide facilitates glucose clearance and the release of a nitric oxide stimulus via the GLUT1 transporter. Diabetologia 51:175–182
Kong WJ, Zhang H, Song DQ et al (2009) Berberine reduces insulin resistance through protein kinase C-dependent up-regulation of insulin receptor expression. Metabolism 58:109–119
Ko BS, Choi SB, Park SK et al (2005) Insulin sensitizing and insulin otropic action of berberine from Cortidis rhizoma. Biol Pharm Bull 28:1431–1437
Zhang W, Xu YC, Guo FJ, Meng Y, Li ML (2008) Antidiabetic effects of cinnamaldehyde and berberine and their impacts on retinol binding protein 4 expression in rats with type 2 diabetes mellitus. Chin Med J121:2124–2128
Ni WJ, Ding HH, Tang LQ (2015) Berberine as a promising anti-diabetic nephropathy drug: An analysis of its effects and mechanisms. Eur J Pharmacol 760:103–112
Yin J, Gao Z, Liu D, Liu Z, Ye J (2008) Berberine improves glucose metabolism through induction of glycolysis. Am J Physiol Endocrinol Metab 294:E148–E156
Chang W, Zhang M, Li J et al (2013) Berberine improves insulin resistance in cardiomyocytes via activation of 5′-adenosine monophosphate-activated protein kinase. Metabolism 62(8):1159–1167
Liu LZ, Cheung SC, Lan LL et al (2010) Berberine modulates insulin signaling transduction in insulin-resistant cells. Mol Cell Endocrinol 317(1–2):148–153
Zhang H, Wei J, Xue R et al (2010) Berberine lowers blood glucose in type 2 diabetes mellitus patients through increasing insulin receptor expression. Metabolism 59(2):285–292
Dong H, Wang N, Zhao L, Lu F (2012) Berberine in the treatment of type 2 diabetes mellitus: a systemic review and meta-analysis. Evidence-Based Complement Altern Med 2012:591654
Dong H, Zhao Y, Zhao L, Lu F (2013) The effects of berberine on blood lipids: a systemic review and meta-analysis of randomized controlled trials. Planta Med 79(6):437–446
Cicero AF, Tartagni E, Ertek S (2014) Nutraceuticals for metabolic syndrome management: from laboratory to benchside. Curr Vasc Pharmacol 12:565–571
Cianci A, Cicero AF, Colacurci N, Matarazzo MG, De Leo V (2012) Activity of isoflavones and berberine on vasomotor symptoms and lipid profile in menopausal women. Gynecol Endocrinol 28:699–702
Dong B, Li H, Singh AB, Cao A, Liu J (2015) Inhibition of PCSK9 transcription by berberine involves down-regulation of hepatic HNF1α protein expression through the ubiquitin-proteasome degradation pathway. J Biol Chem 290(7):4047–4058
Kong W, Wei J, Abidi P et al (2004) Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat Med 10:1344–1351
Lubrano V, Balzan S (2014) LOX-1 and ROS, inseparable factors in the process of endothelial damage. Free Radic Res 48:841–848
Kong WJ, Liu J, Jiang JD (2006) Human low-density lipoprotein receptor gene and its regulation 4. J Mol Med 84:29–36
Cominacini L, Anselmi M, Garbin U et al (2005) Enhanced plasma levels of oxidized low-density lipoprotein increase circulating nuclear factor-kappa B activation in patients with unstable angina. J Am Coll Cardiol 46:799–806
Pirillo A, Catapano AL (2013) Soluble lectin-like oxidized low density lipoprotein receptor-1 as a biochemical marker for atherosclerosis-related diseases. Dis Markers 35:413–418
Guan S, Wang B, Li W, Guan J, Fang X (2010) Effects of berberine on expression of LOX-1 and SR-BI in human macrophage-derived foam cells induced by ox-LDL. Am J Chin Med 38:1161–1169
Huang Z, Dong F, Li S et al (2012) Berberine-induced inhibition of adipocyte enhancer-binding protein 1 attenuates oxidized low-density lipoprotein accumulation and foam cell formation in phorbol 12-myristate 13-acetate-induced macrophages. Eur J Pharmacol 690(1–3):164–169
Chi L, Peng L, Pan N, Hu X, Zhang Y (2014) The anti-atherogenic effects of berberine on foam cell formation are mediated through the upregulation of sirtuin 1. Int J Mol Med 34(4):1087–1093
Chi L, Peng L, Hu X, Pan N, Zhang Y (2014) Berberine combined with atorvastatin downregulates LOX-1 expression through the ET-1 receptor in monocyte/macrophages. Int J Mol Med 34(1):283–290
Xiao M, Men LN, Xu MG et al (2014) Berberine protects endothelial progenitor cell from damage of TNF-α via the PI3K/AKT/eNOS signaling pathway. Eur J Pharmacol 743:11–16
Wu YH, Chuang SY, Hong WC et al (2012) Berberine reduces leukocyte adhesion to LPS-stimulated endothelial cells and VCAM-1 expression both in vivo and in vitro. Int J Immunopathol Pharmacol 25:741–750
Kulkarni SK, Dhir A (2010) Berberine: a plant alkaloid with therapeutic potential for central nervous system disorders. Phytother Res 24(3):317–324
Kulkarni SK, Dhir A (2008) On the mechanism of antidepressant-like action of berberine chloride. Eur J Pharmacol 589:163–172
Peng WH, Lo KL, Lee YH, Hung TH, Lin YC (2007) Berberine produces antidepressant-like effects in the forced swim test and in the tail suspension test in mice. Life Sci 81:933–938
Kong LD, Cheng CH, Tan RX (2001) Monoamine oxidase inhibitors from rhizoma of Coptis chinensis. Planta Med 67:74–76
Kumar A, Ekavali Chopra K et al (2015) Current knowledge and pharmacological profile of berberine: an update. Eur J Pharmacol 761:288–297
Kupeli E, Kosar M, Yesilada E, Hüsnü K, Başer C (2002) A comparative study on the anti-inflammatory, antinociceptive and antipyretic effects of isoquinoline alkaloids from the roots of Turkish berberis species. Life Sci 72:645–657
Chen C, Yu Z, Li Y, Fichna J, Storr M (2014) Effects of berberine in the gastrointestinal tract—a review of actions and therapeutic implications. Am J Chin Med 42(5):1053–1070
Chan E (1993) Displacement of bilirubin from albumin by berberine. Biol Neonat 63:201–208
Tan YZ, Wu AC, Tan BY et al (2002) Study on the interactions of berberine displace other drug from their plasma proteins binding sites. Chin Pharmacol Bull 18:576–578
Xin HW, Wu XC, Li Q et al (2006) The effects of berberine on the pharmacokinetics of cyclosporine A in healthy volunteers. Methods Find Exp Clin Pharmacol 28:25–29
Wu X, Lu Q, Xin H, Zhong M (2005) Effects of berberine on the blood concentration of cyclosporine A in renal transplanted recipients: clinical and pharmacokinetic study. Eur J Clin Pharmacol 61:567–572
Cicero AF, Tartagni E, Ertek S (2014) Safety and tolerability of injectable lipid-lowering drugs: a review of available clinical data. Expert Opin Drug Saf 13(8):1023–1030
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Cicero, A.F.G., Baggioni, A. (2016). Berberine and Its Role in Chronic Disease. In: Gupta, S., Prasad, S., Aggarwal, B. (eds) Anti-inflammatory Nutraceuticals and Chronic Diseases. Advances in Experimental Medicine and Biology, vol 928. Springer, Cham. https://doi.org/10.1007/978-3-319-41334-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-41334-1_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-41332-7
Online ISBN: 978-3-319-41334-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)