Abstract
Traumatic brain injury in the setting of polytrauma is associated with high morbidity and mortality. In particular, anemia, shock, hypoxia, and impaired cerebral autoregulation contribute to secondary brain injury. Treatment is focused on preservation of cerebral perfusion pressure with crystalloids and vasopressors while avoiding colloid solutions; and packed red blood cell transfusion for anemia. Raised intracranial pressure should be managed in a stepwise fashion. However, considerable knowledge gaps exist, and newer methods of monitoring brain injury, such as pressure reactivity index, partial pressure of brain oxygen, and microdialysis offer the potential for individualized patient care.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Epidemiology and Normal Physiology
Traumatic brain injury (TBI) is the leading cause of morbidity and mortality in the United States, especially in the young, affecting more than 1.4 million a year [1]. Serious major extracranial injury, or polytrauma, is commonly associated with TBI, occurring in up to 46 % of TBI patients [2]. Polytrauma is an independent predictor of poor outcome when compared to isolated TBI [3]. This is in part explained by the complications common to polytrauma, such as shock and anemia due to blood loss [4]. These complications contribute to reduced oxygen delivery resulting in delayed, or secondary, ischemic brain injury.
The effects of secondary brain injury are based on derangements in basic physiological principles of oxygen delivery. Normally, the human brain metabolizes oxygen (CMRO2) during oxidative phosphorylation of ATP production necessary for neuronal function. To assure a constant and adequate delivery of oxygen for metabolism, a constant cerebral blood flow (CBF) is necessary. CBF rate varies based on changes in CMRO2 or flow metabolic coupling. The high demand for oxygen, 20 % of the amount available to the whole body, makes the brain sensitive to changes in oxygen delivery (DO2) [5]. In the setting of polytrauma with TBI, DO2 can be perturbed due to shock, anemia, hypoxia, pain and agitation, and impaired cerebral autoregulation .
Mathematically, the relationship between DO2, CBF and cerebral perfusion pressure (CPP) are defined in the following equations:
Equation 1:
Equation 2:
Equation 3:
DO2, oxygen delivery (mL/min); CBF, cerebral blood flow (mL/100 gm brain tissue/min) Hb, hemoglobin (g/dL); SaO2, oxygen saturation (%); PaO2, partial pressure of oxygen (mm Hg); CPP, Cerebral perfusion pressure (mm Hg); r, vessel diameter; L, vessel length; η, viscosity; MAP, mean arterial pressure (mm Hg); ICP, intracranial pressure (mm Hg); IVP, intracranial venous pressure (mm Hg).
The focus of this chapter will be to review the clinical challenges in optimizing DO2 in the TBI patients with polytrauma. There will be a discussion on maintaining CPP with colloids, crystalloid, and vasopressor; as well as the current data on transfusing packed red blood cells. We will also briefly discuss intracranial pressure management and potential application of brain oxygen monitoring and cerebral microdialysis.
Cerebral Blood Flow
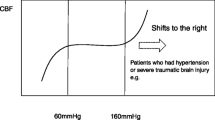
In healthy subjects, CBF is maintained at a constant flow despite fluctuations in blood pressure—mainly by modulating cerebral vessel size—a process known as autoregulation. As illustrated in Fig. 20.1, under normal physiological conditions, CBF remains relatively constant (about 50 mL/100 g/min) for a wide range of CPP (e.g., 60 and 150 mm Hg) [6].
Cerebral autoregulation, modified from [6, 127–129]. Under normal physiological conditions, CBF remains constant (about 50 mL/100 g/min) for a relatively wide CPP (e.g., 60–150 mm Hg), though age and chronic vascular disease may shift this range to the right; acute brain injury autoregulation is lost or narrow, such that the brain is susceptible to injury with CPP fluctuation. At low CPP (in figure above, <50 mm Hg), vascular tone collapses with resultant reduction in CBF and cerebral ischemia. Conversely, extremely high CPP (in figure above, CPP > 150 mm Hg), the myogenic vasoconstriction is overcome to the point of forced dilation and resultant increase in CBF with hyperemia, cerebral edema and intracranial hypertension. At these extreme pressures, cerebral autoregulation is lose, cerebral vascular tone and ICP are passive to CPP. This correlation between ICP and CPP is the basis for PRx [95]
In acute severe TBI, cerebral autoregulation is commonly lost, resulting in pressure dependent flow and increasing the risk for ischemia or hyperemia with relatively minor fluctuations in blood pressure. A reduction in CPP, especially when CPP < 50–60 mm Hg, can result in cerebral ischemia and worse outcomes; [7, 8] while higher perfusion pressure—CPP > 70 mm Hg or SBP > 120 mm Hg—has been associated with better outcomes [9, 10]. Yet, this finding is challenged by animal and human studies suggesting that higher CPP (e.g., CPP > 70 mm Hg), induced with vasopressors, are associated with cerebral edema, acute respiratory distress syndrome (ARDS) and worse outcomes [11–14]. Thus, the optimal CPP is likely within a narrow range, and is reflected in the National Brain Trauma foundation recommendation (Level III) of a CPP range between 50 and 70 mm Hg and SBP > 90 mm Hg, while avoiding a CPP > 70 mm Hg with pressors and fluids (Level II) [15]. For the polytrauma patient, increasing need for higher SBP goals, especially greater than 80–100 mm Hg, as might be necessary in a situation of raised ICP, must be balanced with the increased risk for extracranial bleeding [16, 17]. In order to achieve adequate perfusion goals, a combination of crystalloids or colloids and vasopressors are utilized.
Resuscitation with Crystalloids or Colloids
Patients with severe TBI often presented with concomitant polytrauma and may develop hypovolemic shock that requires early resuscitation. Resuscitation is commonly achieved with the administration of crystalloids or colloids, and vasopressors; with blood products reserved for hemorrhagic shock (discussed in later section). Rapid and adequate volume resuscitation is the first critical step in resuscitating TBI patients, as inadequate resuscitation is an independent predictor of worse outcomes in TBI patients [7], even when adjusted for blood pressure.
In choosing a resuscitation fluid, the general critical care literature lends considerable insight. When comparing crystalloids (e.g., normal saline or lactated ringer) to synthetic colloids (e.g., hydroxyethyl starch or pentastarch) or natural colloids (i.e., albumin) for resuscitation in critically ill populations, especially with sepsis, several large clinical trials have found either no benefit or harm with colloids [18–25]. In the TBI subgroup of the SAFE study, albumin was associated with intracranial hypertension, possibly through albumin extravasation into the brain, and death [20]. Given the clinical evidence against the use of colloids, guidelines recommend crystalloid for resuscitation in the trauma patient [26]. In this regard, the challenges in administering crystalloid will be determining adequacy of resuscitation without causing fluid overload.
Critical to the treatment of shock, regardless of etiology, is the rapid and adequate volume of the fluid. Much of literature on the dose of fluid resuscitation comes from non-trauma critical care studies, and has yielded mixed results. For example, in a mixed etiology ARDS study comparing two strategies, either liberal or restrictive fluid management over the first 7 days post injury, found the restrictive strategy resulted in a negative fluid balance, better oxygenation, reduced duration of mechanical ventilation and need for dialysis, but was equivocal with regards to the primary outcome of survival [27]. A secondary analysis of a septic shock study found higher mortality in the quartile with the greatest fluid balance after 4 days [28]. Conversely, in a recent prospective multicenter observational trial in septic shock patients, greater fluid volume was associated with a survival in patients with persistent shock [29]. Clearly, clinical equipoise persists regarding the effect of high-volume fluid administration in the setting of septic shock. Unfortunately, as a means of gauging the adequacy of volume resuscitation, traditional physiological variables, such as heart rate and blood pressure, are insensitive measures of ongoing hypoperfusion [30]. Initial arterial lactate level and clearance over time are prognostic, and thus could serve as a guide to resuscitation [31], but continuous real-time assessment of volume status is preferable. To this end, newer measures of fluid responsiveness, or need for additional fluid administration, using noninvasive or minimally invasive measures (e.g., straight leg raise or pulse pressure variability) have been studied in septic shock and show promise [32], but have not been studied in trauma and TBI patients.
Even if adequacy of volume resuscitation can be gauged accurately, it is important to note that the effect of fluid restriction may have heterogeneous systemic effect depending on the underlying pathology. For example, while the FACT trial found a negative fluid balance beneficial for lung function, a secondary analysis of the NABISH study (hypothermia in TBI) found that a negative fluid balance in severe TBI was associated with worse outcomes [7] Thus, what may be good for the lung may not be so for the brain, and generalization regarding volume status from non-TBI studies should be done with caution. In the setting of polytrauma with TBI, avoiding inadequate resuscitation may mitigate, to some extent, secondary brain injury.
The osmolality of the crystalloid fluid is also a critical factor in resuscitating the TBI patient. Compared to isotonic solutions, the use of hypotonic solutions (e.g., Ringer’s lactate) is associated with an increased risk of cerebral edema and intracranial hypertension [33, 34]. Surprisingly, the early administration of hypertonic saline has not been shown to be beneficial. In randomized controlled studies, the prehospital administration of hypertonic saline in hemodynamically stable or unstable TBI patients, while lowering ICP, did not improve long-term outcomes [35, 36], with some studies suggesting increased risk for hematoma expansion with hypertonic saline [37]. Clearly, the safety and efficacy of hypertonic saline in the setting of polytrauma needs more study. In conclusion, at a minimum, it seems reasonable to avoid hypotonic solutions while the administration of hypertonic saline should be reserved for treatment of intracranial hypertension.
Vasopressors
In polytrauma, shock is a serious life-threatening event that requires rapid treatment to prevent end-organ injury. In addition to hypovolemic shock, other etiologies include neurogenic, distributive, or hemorrhagic. Defining the etiology allows for definitive therapy (e.g., control of bleeding or chest tube for pneumothorax) if possible, or for initiating adjunct therapy (e.g., antibiotics). As the etiology of shock is being identified and treated, supportive measures may be necessary to normalize CPP, which is typically done with crystalloids, packed red blood cell transfusion, and vasopressors. With regards to vasopressors, optimal use depends on timing. Early initiation of vasopressors in trauma patients has been associated with increased risk of death [38, 39]. However, allowing shock to persist is similarly harmful, as suggested in an 8000 patient observational septic shock study [40]. Choosing an appropriate perfusion goal is also critical. Excessively high MAP to achieve a high CPP (i.e., >70 mm Hg) may contribute to cerebral edema and raised ICP, as well as ARDS [12]. However, in situations of raised ICP, administering vasopressors to achieve higher MAP, and thus adequate CPP, may be necessary to prevent ischemia [41]. Commonly used vasopressors in polytrauma patients include norepinephrine, phenylephrine, dopamine, and vasopressin [42]. It is not clear whether one vasopressors is superior to the rest [43], though animal data suggest a survival benefit with vasopressin in hemorrhagic shock [44], with human trials forthcoming [45]. From a practical standpoint, vasopressors need to be initiated as soon as necessary to maintain adequate CPP, and should be used in combination with crystalloids and packed red blood cells [46, 47].
Packed Red Blood Cell (pRBC) Transfusion
The transfusion of pRBC in trauma patients is critical for maintaining DO2, with there being two thresholds for transfusion based on hemodynamic status. The more obvious threshold for transfusion is in the treatment hemorrhagic shock, in conjunction with crystalloids, vasopressors and control of bleeding, as reviewed in guidelines [16]. The second threshold for pRBC transfusion is in the hemodynamically stable anemic TBI patient at risk for ongoing secondary brain injury. Regardless of hemodynamic stability, there is a threshold below which cerebral ischemia is likely to be exacerbated by anemia, if not treated with pRBC transfusion. Defining this threshold has been very challenging.
As noted in Eq. 1, it is clear that hemoglobin is a critical component of DO2. In healthy subjects, acute isovolemic anemia results in a reduction in oxygen content matched; which is compensated by an increase in CBF, mainly due to reduced viscosity and cerebral vasodilation, resulting in a constant oxygen delivery (DO2) [48]. This reserve is limited, however, and with severe enough isovolemic anemia (e.g., Hb < 6), reversible impairment in cognitive function can be noted on neurocognitive and electrophysiologic testing [49, 50]. Patients with cerebrovascular disease do not have the cerebrovascular reserve of healthy subject, and as a consequence, even mild anemia results in reduced oxygen delivery [51], and potentially secondary brain injury. More easily measurable than cognitive function and secondary brain injury is the overall functional status, which seems to be adversely affected with anemia in trauma [52], stroke [53] and severe TBI [54, 55].
The seemingly logical treatment of anemia in TBI with pRBC has not been proved in clinical trials of TBI without hemorrhagic shock. To begin with, pRBC transfusion is associated with severe side effects, including transfusion-associated circulatory overload, transfusion-related acute lung injury [56] and infection [57–60]. Perhaps as a consequence of these side effects, observational TBI studies have noted increased morbidity or mortality with pRBC transfusion [52, 61, 62]. However, such studies are limited through confounding by indication [63], whereby anemic TBI patients are likely sicker than those without anemia [64], and also more likely to receive pRBC; thus, making it difficult to differentiate the independent effect of pRBC on outcome from the natural history of the underlying disease. This notion is supported by the results of recent randomized clinical trials in non-TBI critically ill patients. In these studies of more than 4000 patient with sepsis or after cardiac surgery, a liberal transfusion goal resulted in more pRBC transfusions when compared to a restrictive transfusion practice, but did not result in increased harm [59, 60].
Specifically with regards to TBI, a randomized multicenter trial by Robertson et al., comparing a hemoglobin threshold of 7 versus 10 g/dL for transfusion in closed head injury TBI without life-threatening systemic injury, found no improvement in neurological outcome at 6 months as well as higher complication rate with the higher Hb threshold [65]. However, important baseline differences, such a higher rate of fixed pupils on presentation in the Hb 10 g/dL group, could have confounded results in favor of the lower Hgb group. In addition, a post hoc analysis suggested an interaction between the timing of injury (before or after 48 h) and Hb threshold (7 versus 10 g/dL) on outcome, with improved outcomes with higher Hb during the first 48 h, but harm thereafter [66]. This finding is in line with the observation that cerebral autoregulation and cerebral metabolic stress, as measured by cerebral microdialysis, are most abnormal during the initial 4 days after injury [67], suggesting this period to be one when pRBC is most likely to be beneficial.
Furthermore, anemia, independent of cerebral hypoxia, may not be a suitable indicator for pRBC transfusion. This is suggested in an observational study which noted worse outcomes in severe TBI patients with anemia only in the setting of coexistent cerebral hypoxia [68]. In another prospective study of moderate to severe TBI, brain hypoxia improved with pRBC only in the setting of concomitant cerebral metabolic stress, as determined with microdialysis [69]. Future studies will need to consider additional triggers (e.g., PbtO2), timing, and dose of pRBC, while minimizing confounding. In conclusion, in the polytrauma with TBI, it seems reasonable to aim for a higher Hb goal (Hb > 9–10 g/dL) [17], particularly during the first days after brain injury, and if possible, guided by multimodal monitoring (e.g., brain oxygen or microdialysis).
Intracranial Pressure
While the maintaining of adequate CPP is critical to the care of the TBI patient, intracranial pressure (ICP) is similarly a critical component in traditional management, and in effect, is integrally related to CPP (i.e., CPP = MAP − ICP). However, in clinical practice, ICP is considered a clinical endpoint for treatment and prognostication.
ICP is fundamentally a reflection of intracranial compliance governed by the Monro-Kellie hypothesis. Principally, this hypothesis states that the cranial vault is a rigid structure which encloses the brain, cerebrospinal fluid and blood, and all of which are maintained at a constant volume. Thus, additional volume in the form of bleeding or edema or hydrocephalus, must result in displacement of one of the three intracranial components. Initially, venous blood and cerebrospinal fluid are displaced into extracranial compartments (e.g., jugular vein or lumbar cisterns, respectively). If left unabated, increasing mass effect increases ICP to the point of eventually displacing brain tissue (i.e., brain herniation) and resulting in brain injury and ischemia (see Fig. 20.2) [70]. Measuring ICP is thus fundamental to identifying and treating reduced intracranial compliance prior to herniation. Typically, ICP monitoring is achieved with either intraparenchymal fiberoptic catheter or intraventricular fluid coupled drainage system, with the latter allowing for treatment of raised ICP by facilitating cerebrospinal fluid drainage. The risks of ICP monitor include bleeding during insertion, infection, device malfunction, inaccuracy, and complications related to treatment based on ICP values [71–75].
ICP-volume relationship and the concept of the intracranial compliance. Adapted from Avezaat et al. [130]. The ICP waveform is normally comprised of three waves. P1 is a percussion wave, derived from arterial pulsation; P2 is a tidal wave, derived from arterial blood volume load and reflective of intracranial compliance; and P3 is a dichotic wave, derived from aortic valve closure. Intracranial compliance is defined as the ratio of changes in volume over changes in pressure. Note, during normal ICP (waveform shown in a) P1 is greater than P2; but as ICP increases with greater volume, (ICP waveform in b) P2 becomes greater than P1
Indications for ICP monitoring, as per the BTF, are listed in Table 20.1. ICP greater than 20–25 mm Hg is associated with increased mortality [76–80] and morbidity [76, 81, 82], particularly when ICP is refractory to treatment [78]. While raised ICP is clearly associated with worse outcomes, the benefit of having an ICP monitor, and the resultant treatment, is less clear with some studies suggesting improved outcomes [83, 84] and other finding none [85]. A systematic review, consisting only of observational studies, found that ICP monitoring was not associated with lower mortality, though when considering only modern studies, there was in fact a benefit [86]. However, confounding variables, patient selection bias, study heterogeneity limit the generalizability of these data.
Given the clinical equipoise regarding ICP monitoring in isolated severe TBI, Chestnut et al. conduced the BEST-TRIP trial [87]. This study compared acute TBI care based on ICP monitor (ICP group) versus treatment based only on CT scan and clinical exam without an ICP monitor (ICE group). Treatment thresholds for raised ICP were based on TBF guidelines (e.g., CPP 50–70 mm Hg and ICP < 20 mm Hg). The primary outcome, functional outcome at six months, was not different between the groups. However, while 75 % of patients with ICP monitoring had at least one episode of ICP > 20 mm Hg, the median percent of hourly ICP > 20 mm Hg was only 5 %, suggesting an infrequent occurrence of raised ICP, which may explain the comparatively less frequent administration of hyperosmolar therapy in the ICP arm; while a greater administration of barbiturates and less use of hyperventilation in the ICP arm suggests a tailoring of advanced tier treatment only possible with ICP measurement. Given the low incidence of raised ICP, this study may have underpowered to assess the efficacy of ICP monitoring. This hypothesis is supported by a recent multicenter observational study that found ICP monitoring beneficial in patients with the most severe form of TBI (e.g., GCS 3–5) [86]. It is important to note that the treatments of raised ICP(see next paragraph) have not been found efficacious in clinical studies, further complicating the analysis of this study. Nonetheless, given the known association between raised ICP/low CPP and poor outcome, it seems prudent to continue to monitor and treat raised ICP, particularly in the setting of hemodynamic instability common to polytrauma.
The management of raised ICP involves a stepwise, multimodal approach (see Fig. 20.3) [88]. However, most of the treatments outlined in the figure have not been studied rigorously, and are applied with considerable physician variation [89]. Clinical data to help guide timing, duration, optimal combination, and triggers for escalating ICP treatment are lacking. Few clinical trials had studied the complex interaction of available treatments, and most trials attempt to measure the efficacy of a particular treatment, such as therapeutic hypothermia or decompressive hemicraniectomy, alone but not in combination. Even when studied in isolation, the few large randomized trials or systematic reviews conducted in severe TBI have shown harm with third tier treatments. For example, decompressive hemicraniectomy as a salvage treatment for refractory ICP [90], and therapeutic hypothermia (TH) as a prophylactic treatment or upon onset of raised ICP in severe TBI [91–93], have failed to show benefit. A Cochrane review of pentobarbital found no benefit to barbiturates with regards to ICP control or survival [94]. Furthermore, the added complexity of polytrauma necessitates an efficient treatment pathway that addresses brain injury unique to a particular patient’s physiology (i.e., with or without shock), rather than a one-size-fits-all approach. To achieve this goal, investigators have begun to analyze ICP in the context of other physiological variables, such as cerebral autoregulation , brain oxygen, and microdialysis.
Schematics illustrating the stepwise management of intracranial hypertension [88]
As mentioned previously, in normal brain, cerebral autoregulation maintains a constant CBF across a wide range of blood pressure. In acute TBI, however, cerebral autoregulation is blunted resulting in a narrower blood pressure range of constant CBF, beyond which ischemia or hyperemia can result. In clinical practice, direct measurement of cerebral autoregulation is difficult, but some groups have defined surrogate measures by correlating changes in MAP and ICP over time. One such measure is the pressure reactivity index (PRx), which is based on the idea that during impaired autoregulation, cerebral vessels dilate passively with increase in CPP. The dilated vessels increase cerebral blood volume and increase ICP—the correlation between ICP and CPP is thus positive (PRx > 0.2). Conversely, with preserved autoregulation, cerebral vessel constrict with CPP increase, resulting in a negative or zero PRx [95, 96]. The CPP range resulting in a low PRx, suggesting preserved autoregulation, is termed optimal CPP (CPPopt). Observational studies suggest that CPPopt varies between patients and over time, and that the magnitude of deviation between the actual CPP from the CPPopt correlates with poor outcome [97, 98]. Such real-time analysis, if validated, would provide a means of titrating ICP and CPP therapy based on individual patient’s physiology rather than the current one-size-fits-all strategy.
Brain Tissue Oxygen and Microdialysis
Normal brain oxygenation depends on adequate CBF and arterial oxygen content to match the needs of cerebral metabolic rate of oxygen consumption (CMRO2). Brain oxygenation is often altered following TBI due to reduced oxygen delivery secondary to (1) hypotension/shock; (2) acute anemia from blood loss; and (3) hypoxia often attributed to co-existing acute lung contusion in the setting of polytrauma, acute pulmonary edema caused by neurogenic stunned myocardium, aspiration pneumonia or ARDS. Alternatively, reduced brain oxygenation could also result from increased CMRO2 related to pain, agitation, pyrexia, or seizure.
Brain oxygenation is measured by one of the two ways, either by local white matter partial pressure of oxygen sampling or via a more global measure by sampling of jugular venous oxygen saturation. Passing a fiberoptic probe through a burr hole into the white matter allows for the measure of local tissue oxygen tension (PbtO2) within a small sampling area. PbtO2 is actually measuring the partial pressure of oxygen within the extracellular space, which equals the difference between oxygen that crosses into brain tissue (arterio-venous oxygen difference [AVDO2]x CBF) and CMRO2 [99]. Thus, reduction in CBF or oxygen content, or increase in CMRO2, can result in low PbtO2. The second and more global means of measuring brain oxygen, entails placing a fiberoptic catheter within the jugular vein at the level of the jugular bulb to measure jugular venous oxygen saturation (SjVO2) to derive oxygen extraction and AVO2. Brain hypoxia, as measured by either PbtO2 (<15–20 mm Hg) or SjVO2 (<55 %), is associated with worse outcomes in TBI patients [100–103]. Both techniques are relatively safe [104] with PbtO2 possibly being more accurate for a focal area of brain and more commonly used than SjVO2 [105–107].
Interestingly, ischemic PbtO2 values exist independent of ICP [108], making PbtO2 measurement in TBI a potentially useful add-on tool to standard ICP/CPP guided therapy. From a management perspective, low PbtO2 values may be treated by increasing the inspired fraction of oxygen (FIO2) and blood pressure with vasopressors or fluids; administering sedatives or paralytics; transfusing blood; or administering hypertonic saline [109, 110]. However, with randomized trials lacking, data from observational studies have shown mixed results of PbtO2 monitoring on outcomes [102, 111–118]. Increased fluids and vasopressor administration guided by PbtO2 monitoring may have contributed to worse outcomes, as suggested in one study [117]. In addition, given the small sampling area of PbtO2, catheter placement is of critical importance, with PbtO2 values near injured brain, but not from unaffected brain, being a better predictor of patient outcome and thus guide to therapy [119], though this has not been a consistent finding [66] and additional studies are needed. Other variables, such as extracellular brain pH [120], may interact with PbtO2 and serve to better discriminate treatment thresholds. Ongoing studies are addressing the utility and efficacy of PbtO2—guided treatment in TBI.
As with PbtO2, local sampling of metabolites of energy (e.g., lactate and pyruvate) or cell injury (e.g., glycerol) is possible by passing a microdialysis (MCD) catheter through a burr hole and into the white matter. MCD can be used to measure extracellular cerebral glycolysis, as represented by the ratio of lactate to pyruvate (LPR). Several studies have found an association between elevated LPR (>25–40), or metabolic crisis, and poor outcomes [121]. In particular, LPR values are elevated during cerebral hypoxia [120], low CPP (<50 mm Hg) [122] as well as high CPP (>70 mm Hg) [123]. Concomitant MCD and PET scan measured CMRO2, LPR > 40 is seen in 25 % of severe TBI patients, but only a small fraction (2.4 %) have concomitant ischemia, suggesting cerebral metabolic stress, and thus injury, occurs by mechanism other than just cerebral hypoxia [124]. Other studies suggest 75 % of moderate to severe TBI patients develop metabolic crisis (LRP > 25 and low glucose) within the first 72 h after brain injury, despite adequate resuscitation and ICP control, with longer duration of metabolic crisis associated with unfavorable outcome [125]. Thus, MCD uniquely offers insight into nonischemic mechanism of brain injury, such as mitochondrial dysfunction [126], offering the potential to identify new therapies for mitigating secondary brain injury.
In conclusion, the management of TBI with polytrauma is challenging given the complexity of secondary brain injury, which is incompletely understood and not easily measurable in clinical practice. Nonetheless, current care is focused on maintaining adequate oxygen delivery by: (1) aiming for a narrow CPP range (e.g., CPP 60–80 mm Hg) with the use of crystalloids and vasopressors; (2) avoiding excessive anemia by pRBC transfuson; and (3) Aggressively treating ICP in a stepwise approach. Studies are ongoing to better define therapeutic thresholds, particularly with the advent of new of technologies.
References
Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury. J Head Trauma Rehabil. 2006;21(5):375–8. doi:10.1097/00001199-200609000-00001.
van Leeuwen N, Lingsma HF, Perel P, et al. Prognostic value of major extracranial injury in traumatic brain injury. Neurosurgery. 2012;70(4):811–8. doi:10.1227/NEU.0b013e318235d640.
Tortella FC, Leung LY. TBI and polytrauma in theatres of combat: the case for neurotrauma resuscitation? Shock. 2015;. doi:10.1097/SHK.0000000000000380.
Pape H-C, Lefering R, Butcher N, et al. The definition of polytrauma revisited: an international consensus process and proposal of the new “Berlin definition”. J Trauma Acute Care Surg. 2014;77(5):780–6. doi:10.1097/TA.0000000000000453.
Clarke DD, Sokoloff L. Regulation of Cerebral Metabolic Rate. Lippincott-Raven; 1999. http://www.ncbi.nlm.nih.gov/books/NBK28194/. Accessed June 6, 2015.
Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 1990;2(2):161–92. http://www.ncbi.nlm.nih.gov/pubmed/2201348.
Clifton GL, Miller ER, Choi SC, Levin HS. Fluid thresholds and outcome from severe brain injury. Crit Care Med. 2002;30(4):739–45. http://www.ncbi.nlm.nih.gov/pubmed/11940738.
Butcher I, Maas AIR, Lu J, et al. Prognostic value of admission blood pressure in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24(2):294–302. doi:10.1089/neu.2006.0032.
Griesdale DEG, Örtenwall V, Norena M, et al. Adherence to guidelines for management of cerebral perfusion pressure and outcome in patients who have severe traumatic brain injury. J Crit Care. 2015;30(1):111–5. doi:10.1016/j.jcrc.2014.07.026.
Brenner M, Stein DM, Hu PF, Aarabi B, Sheth K, Scalea TM. Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. J Trauma Acute Care Surg. 2012;72(5):1135–9. doi:10.1097/TA.0b013e31824af90b.
Robertson CS, Valadka AB, Hannay HJ, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999;27(10):2086–95. doi:10.1097/00003246-199910000-00002.
Contant CF, Valadka AB, Gopinath SP, Hannay HJ, Robertson CS. Adult respiratory distress syndrome: a complication of induced hypertension after severe head injury. J Neurosurg. 2001;95(4):560–8. doi:10.3171/jns.2001.95.4.0560.
Elf K, Nilsson P, Ronne-Engström E, Howells T, Enblad P. Cerebral perfusion pressure between 50 and 60 mm Hg may be beneficial in head-injured patients: a computerized secondary insult monitoring study. Neurosurgery. 2005;56(5):962–71; discussion 962–971. http://www.ncbi.nlm.nih.gov/pubmed/15854244.
Sellmann T, Miersch D, Kienbaum P, et al. The impact of arterial hypertension on polytrauma and traumatic brain injury. Dtsch Arztebl Int. 2012;109(49):849–56. doi:10.3238/arztebl.2012.0849.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, et al. Guidelines for the management of severe traumatic brain injury. IX. Cerebral perfusion thresholds. J Neurotrauma. 2007;24 Suppl 1:S59–S64. doi:10.1089/neu.2007.9987.
Rossaint R, Bouillon B, Cerny V, et al. Management of bleeding following major trauma: an updated European guideline. Crit Care. 2010;14(2):R52. doi:10.1186/cc8943.
Bougle A, Harrois A, Duranteau J. Resuscitative strategies in traumatic hemorrhagic shock. Ann Intensive Care. 2013;3(1):1. doi:10.1186/2110-5820-3-1.
Annane D, Siami S, Jaber S, et al. Effects of fluid resuscitation with colloids vs. crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013;310(17):1809–17. doi:10.1001/jama.2013.280502.
Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367(2):124–34. doi:10.1056/NEJMoa1204242.
SAFE Study Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group, Australian Red Cross Blood Service, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357(9):874–84. doi:10.1056/NEJMoa067514.
Caironi P, Tognoni G, Masson S, et al. Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med. 2014;370(15):1412–21. doi:10.1056/NEJMoa1305727.
Perel P, Roberts I, Ker K. Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev. 2013;2:CD000567. doi:10.1002/14651858.CD000567.pub6.
Patel A, Laffan MA, Waheed U, Brett SJ. Randomised trials of human albumin for adults with sepsis: systematic review and meta-analysis with trial sequential analysis of all-cause mortality. BMJ. 2014;349:g4561. doi:10.1136/bmj.g4561.
Haase N, Perner A, Hennings LI, et al. Hydroxyethyl starch 130/0.38-0.45 versus crystalloid or albumin in patients with sepsis: systematic review with meta-analysis and trial sequential analysis. BMJ. 2013;346:f839. doi:10.1136/bmj.f839.
Schortgen F, Lacherade JC, Bruneel F, et al. Effects of hydroxyethylstarch and gelatin on renal function in severe sepsis: a multicentre randomised study. Lancet. 2001;357(9260):911–6. doi:10.1016/S0140-6736(00)04211-2.
Advanced Trauma Life Support. American College of Surgeons. https://www.facs.org/quality%20programs/trauma/atls. Accessed Nov 24, 2015.
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75. doi:10.1056/NEJMoa062200.
Boyd JH, Forbes J, Nakada T-A, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39(2):259–65. doi:10.1097/CCM.0b013e3181feeb15.
Smith SH, Perner A. Higher vs. lower fluid volume for septic shock: clinical characteristics and outcome in unselected patients in a prospective, multicenter cohort. Crit Care. 2012;16(3):R76. doi:10.1186/cc11333.
Scalea TM, Maltz S, Yelon J, Trooskin SZ, Duncan AO, Sclafani SJ. Resuscitation of multiple trauma and head injury: role of crystalloid fluids and inotropes. Crit Care Med. 1994;22(10):1610–15. http://www.ncbi.nlm.nih.gov/pubmed/7924373.
Odom SR, Howell MD, Silva GS, et al. Lactate clearance as a predictor of mortality in trauma patients. J Trauma Acute Care Surg. 2013;74(4):999–1004. doi:10.1097/TA.0b013e3182858a3e.
Pinsky MR. Functional haemodynamic monitoring. Curr Opin Crit Care. 2014;20(3):288–93. doi:10.1097/MCC.0000000000000090.
Shackford SR, Zhuang J, Schmoker J. Intravenous fluid tonicity: effect on intracranial pressure, cerebral blood flow, and cerebral oxygen delivery in focal brain injury. J Neurosurg. 1992;76(1):91–8. doi:10.3171/jns.1992.76.1.0091.
Simma B, Burger R, Falk M, Sacher P, Fanconi S. A prospective, randomized, and controlled study of fluid management in children with severe head injury: lactated Ringer’s solution versus hypertonic saline. Crit Care Med. 1998;26(7):1265–70. http://www.ncbi.nlm.nih.gov/pubmed/9671379.
Bulger EM, May S, Brasel KJ, et al. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA. 2010;304(13):1455–64. doi:10.1001/jama.2010.1405.
Cooper DJ, Myles PS, McDermott FT, et al. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: a randomized controlled trial. JAMA. 2004;291(11):1350–7. doi:10.1001/jama.291.11.1350.
Bulger EM, May S, Kerby JD, et al. Out-of-hospital hypertonic resuscitation after traumatic hypovolemic shock: a randomized, placebo controlled trial. Ann Surg. 2011;253(3):431–41. doi:10.1097/SLA.0b013e3181fcdb22.
Sperry JL, Minei JP, Frankel HL, et al. Early use of vasopressors after injury: caution before constriction. J Trauma. 2008;64(1):9–14. doi:10.1097/TA.0b013e31815dd029.
Plurad DS, Talving P, Lam L, Inaba K, Green D, Demetriades D. Early vasopressor use in critical injury is associated with mortality independent from volume status. J Trauma. 2011;71(3):565–70; discussion 570–572. doi:10.1097/TA.0b013e3182213d52.
Beck V, Chateau D, Bryson GL, et al. Timing of vasopressor initiation and mortality in septic shock: a cohort study. Crit Care. 2014;18(3):R97. doi:10.1186/cc13868.
Young JS, Blow O, Turrentine F, Claridge JA, Schulman A. Is there an upper limit of intracranial pressure in patients with severe head injury if cerebral perfusion pressure is maintained? Neurosurg Focus. 2003;15(6):E2. http://www.ncbi.nlm.nih.gov/pubmed/15305838.
Sookplung P, Siriussawakul A, Malakouti A, et al. Vasopressor use and effect on blood pressure after severe adult traumatic brain injury. Neurocrit Care. 2011;15(1):46–54. doi:10.1007/s12028-010-9448-9.
Havel C, Arrich J, Losert H, Gamper G, Müllner M, Herkner H. Vasopressors for hypotensive shock. Cochrane Database Syst Rev. 2011;(5):CD003709. doi:10.1002/14651858.CD003709.pub3.
Cossu AP, Mura P, De Giudici LM, et al. Vasopressin in hemorrhagic shock: a systematic review and meta-analysis of randomized animal trials. Biomed Res Int. 2014;2014:421291. doi:10.1155/2014/421291.
Lienhart HG, Wenzel V, Braun J, et al. [Vasopressin for therapy of persistent traumatic hemorrhagic shock: The VITRIS. at study]. Anaesthesist. 2007;56(2):145–8, 150. doi:10.1007/s00101-006-1114-4.
Feinstein AJ, Patel MB, Sanui M, Cohn SM, Majetschak M, Proctor KG. Resuscitation with pressors after traumatic brain injury. J Am Coll Surg. 2005;201(4):536–45. doi:10.1016/j.jamcollsurg.2005.05.031.
Beloncle F, Meziani F, Lerolle N, Radermacher P, Asfar P. Does vasopressor therapy have an indication in hemorrhagic shock? Ann Intensive Care. 2013;3(1):13. doi:10.1186/2110-5820-3-13.
Henriksen L, Paulson OB, Smith RJ. Cerebral blood flow following normovolemic hemodilution in patients with high hematocrit. Ann Neurol. 1981;9(5):454–7. doi:10.1002/ana.410090507.
Weiskopf RB, Toy P, Hopf HW, et al. Acute isovolemic anemia impairs central processing as determined by P300 latency. Clin Neurophysiol. 2005;116(5):1028–32. doi:10.1016/j.clinph.2004.12.009.
Weiskopf RB, Kramer JH, Viele M, et al. Acute severe isovolemic anemia impairs cognitive function and memory in humans. Anesthesiology. 2000;92(6):1646–52. http://www.ncbi.nlm.nih.gov/pubmed/10839915.
Kusunoki M, Kimura K, Nakamura M, Isaka Y, Yoneda S, Abe H. Effects of hematocrit variations on cerebral blood flow and oxygen transport in ischemic cerebrovascular disease. J Cereb Blood Flow Metab. 1981;1(4):413–7. doi:10.1038/jcbfm.1981.45.
Malone DL, Dunne J, Tracy JK, Putnam AT, Scalea TM, Napolitano LM. Blood transfusion, independent of shock severity, is associated with worse outcome in trauma. J Trauma. 2003;54(5):898–905; discussion 905–7. doi:10.1097/01.TA.0000060261.10597.5C.
Kellert L, Schrader F, Ringleb P, Steiner T, Bösel J. The impact of low hemoglobin levels and transfusion on critical care patients with severe ischemic stroke: STroke: RelevAnt Impact of HemoGlobin, Hematocrit and Transfusion (STRAIGHT)–an observational study. J Crit Care. 2014;29(2):236–40. doi:10.1016/j.jcrc.2013.11.008.
Sekhon MS, McLean N, Henderson WR, Chittock DR, Griesdale DEG. Association of hemoglobin concentration and mortality in critically ill patients with severe traumatic brain injury. Crit Care. 2012;16(4):R128. doi:10.1186/cc11431.
Griesdale DE, Sekhon MS, Menon DK, et al. Hemoglobin Area and Time Index Above 90 g/L are Associated with Improved 6-Month Functional Outcomes in Patients with Severe Traumatic Brain Injury. Neurocrit Care. 2014;. doi:10.1007/s12028-014-0096-3.
Retter A, Wyncoll D, Pearse R, et al. Guidelines on the management of anaemia and red cell transfusion in adult critically ill patients. Br J Haematol. 2013;160(4):445–64. doi:10.1111/bjh.12143.
Claridge JA, Sawyer RG, Schulman AM, McLemore EC, Young JS. Blood transfusions correlate with infections in trauma patients in a dose-dependent manner. Am Surg. 2002;68(7):566–72. http://www.ncbi.nlm.nih.gov/pubmed/12132734.
Rohde JM, Dimcheff DE, Blumberg N, et al. Health care-associated infection after red blood cell transfusion: a systematic review and meta-analysis. JAMA. 2014;311(13):1317–26. doi:10.1001/jama.2014.2726.
Murphy GJ, Pike K, Rogers CA, et al. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med. 2015;372(11):997–1008. doi:10.1056/NEJMoa1403612.
Holst LB, Wetterslev J, Perner A. Hemoglobin threshold for transfusion in septic shock. N Engl J Med. 2015;372(1):91–2. doi:10.1056/NEJMc1413474.
Moore FA, Moore EE, Sauaia A. Blood transfusion. An independent risk factor for postinjury multiple organ failure. Arch Surg. 1997;132(6):620–4; discussion 624–625. http://www.ncbi.nlm.nih.gov/pubmed/9197854.
Dunne JR, Malone DL, Tracy JK, Napolitano LM. Allogenic blood transfusion in the first 24 hours after trauma is associated with increased systemic inflammatory response syndrome (SIRS) and death. Surg Infect. 2004;5(4):395–404. doi:10.1089/sur.2004.5.395.
Middelburg RA, van de Watering LMG, van der Bom JG. Blood transfusions: good or bad? Confounding by indication, an underestimated problem in clinical transfusion research. Transfusion. 2010;50(6):1181–3. doi:10.1111/j.1537-2995.2010.02675.x.
Salim A, Hadjizacharia P, DuBose J, et al. Role of anemia in traumatic brain injury. J Am Coll Surg. 2008;207(3):398–406. doi:10.1016/j.jamcollsurg.2008.03.013.
Robertson CS, Hannay HJ, Yamal J-M, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312(1):36–47. doi:10.1001/jama.2014.6490.
Yamal J-M, Rubin ML, Benoit JS, et al. Effect of hemoglobin transfusion threshold on cerebral hemodynamics and oxygenation. J Neurotrauma. 2015;. doi:10.1089/neu.2014.3752.
Yokobori S, Watanabe A, Matsumoto G, et al. Time course of recovery from cerebral vulnerability after severe traumatic brain injury: a microdialysis study. J Trauma. 2011;71(5):1235–40. doi:10.1097/TA.0b013e3182140dd7.
Oddo M, Levine JM, Kumar M, et al. Anemia and brain oxygen after severe traumatic brain injury. Intensive Care Med. 2012;38(9):1497–504. doi:10.1007/s00134-012-2593-1.
Zygun DA, Nortje J, Hutchinson PJ, Timofeev I, Menon DK, Gupta AK. The effect of red blood cell transfusion on cerebral oxygenation and metabolism after severe traumatic brain injury. Crit Care Med. 2009;37(3):1074–8. doi:10.1097/CCM.0b013e318194ad22.
Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001;56(12):1746–8. http://www.ncbi.nlm.nih.gov/pubmed/11425944.
Muralidharan R. External ventricular drains: Management and complications. Surg Neurol Int. 2015;6(Suppl 6):S271–4. doi:10.4103/2152-7806.157620.
Poca M-A, Sahuquillo J, Arribas M, Báguena M, Amorós S, Rubio E. Fiberoptic intraparenchymal brain pressure monitoring with the Camino V420 monitor: reflections on our experience in 163 severely head-injured patients. J Neurotrauma. 2002;19(4):439–48. doi:10.1089/08977150252932398.
Martínez-Mañas RM, Santamarta D, de Campos JM, Ferrer E. Camino intracranial pressure monitor: prospective study of accuracy and complications. J Neurol Neurosurg Psychiatry. 2000;69(1):82–6. http://www.ncbi.nlm.nih.gov/pubmed/10864608.
Bauer DF, Razdan SN, Bartolucci AA, Markert JM. Meta-analysis of hemorrhagic complications from ventriculostomy placement by neurosurgeons. Neurosurgery. 2011;69(2):255–60. doi:10.1227/NEU.0b013e31821a45ba.
Mayhall CG, Archer NH, Lamb VA, et al. Ventriculostomy-related infections. A prospective epidemiologic study. N Engl J Med. 1984;310(9):553–9. doi:10.1056/NEJM198403013100903.
Badri S, Chen J, Barber J, et al. Mortality and long-term functional outcome associated with intracranial pressure after traumatic brain injury. Intensive Care Med. 2012;38(11):1800–9. doi:10.1007/s00134-012-2655-4.
Balestreri M, Czosnyka M, Hutchinson P, et al. Impact of intracranial pressure and cerebral perfusion pressure on severe disability and mortality after head injury. Neurocrit Care. 2006;4(1):8–13. doi:10.1385/NCC:4:1:008.
Farahvar A, Gerber LM, Chiu Y-L, et al. Response to intracranial hypertension treatment as a predictor of death in patients with severe traumatic brain injury. J Neurosurg. 2011;114(5):1471–8. doi:10.3171/2010.11.JNS101116.
Lannoo E, Van Rietvelde F, Colardyn F, et al. Early predictors of mortality and morbidity after severe closed head injury. J Neurotrauma. 2000;17(5):403–14. http://www.ncbi.nlm.nih.gov/pubmed/10833059.
Bremmer R, de Jong BM, Wagemakers M, Regtien JG, van der Naalt J. The course of intracranial pressure in traumatic brain injury: relation with outcome and CT-characteristics. Neurocrit Care. 2010;12(3):362–8. doi:10.1007/s12028-009-9329-2.
Stein DM, Hu PF, Brenner M, et al. Brief episodes of intracranial hypertension and cerebral hypoperfusion are associated with poor functional outcome after severe traumatic brain injury. J Trauma. 2011;71(2):364–73; discussion 373–374. doi:10.1097/TA.0b013e31822820da.
Stein DM, Brenner M, Hu PF, et al. Timing of intracranial hypertension following severe traumatic brain injury. Neurocrit Care. 2013;18(3):332–40. doi:10.1007/s12028-013-9832-3.
Alali AS, Fowler RA, Mainprize TG, et al. Intracranial pressure monitoring in severe traumatic brain injury: results from the American College of Surgeons Trauma Quality Improvement Program. J Neurotrauma. 2013;30(20):1737–46. doi:10.1089/neu.2012.2802.
Talving P, Karamanos E, Teixeira PG, et al. Intracranial pressure monitoring in severe head injury: compliance with Brain Trauma Foundation guidelines and effect on outcomes: a prospective study. J Neurosurg. 2013;119(5):1248–54. doi:10.3171/2013.7.JNS122255.
Cremer OL, van Dijk GW, van Wensen E, et al. Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med. 2005;33(10):2207–13. doi:10.1097/01.CCM.0000181300.99078.B5.
Yuan Q, Wu X, Sun Y, et al. Impact of intracranial pressure monitoring on mortality in patients with traumatic brain injury: a systematic review and meta-analysis. J Neurosurg. 2015;122(3):574–87. doi:10.3171/2014.10.JNS1460.
Chesnut RM, Temkin N, Carney N, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367(26):2471–81. doi:10.1056/NEJMoa1207363.
Stevens RD, Huff JS, Duckworth J, Papangelou A, Weingart SD, Smith WS. Emergency neurological life support: intracranial hypertension and herniation. Neurocrit Care. 2012;17(Suppl 1):S60–5. doi:10.1007/s12028-012-9754-5.
Hays AN, Lazaridis C, Neyens R, Nicholas J, Gay S, Chalela JA. Osmotherapy: use among neurointensivists. Neurocrit Care. 2011;14(2):222–8. doi:10.1007/s12028-010-9477-4.
Cooper DJ, Rosenfeld JV, Murray L, et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364(16):1493–502. doi:10.1056/NEJMoa1102077.
Clifton GL, Miller ER, Choi SC, et al. Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med. 2001;344(8):556–63. doi:10.1056/NEJM200102223440803.
Clifton GL, Valadka A, Zygun D, et al. Very early hypothermia induction in patients with severe brain injury (the National Acute Brain Injury Study: Hypothermia II): a randomised trial. Lancet Neurol. 2011;10(2):131–9. doi:10.1016/S1474-4422(10)70300-8.
Andrews PJD, Sinclair HL, Rodriguez A, et al. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. N Engl J Med. 2015;. doi:10.1056/NEJMoa1507581.
Roberts I, Sydenham E. Barbiturates for acute traumatic brain injury. Cochrane Database Syst Rev. 2012;12:CD000033. doi:10.1002/14651858.CD000033.pub2.
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD. Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery. 1997;41(1):11–17; discussion 17–19. http://www.ncbi.nlm.nih.gov/pubmed/9218290.
Czosnyka M, Smielewski P, Kirkpatrick P, Piechnik S, Laing R, Pickard JD. Continuous monitoring of cerebrovascular pressure-reactivity in head injury. Acta Neurochir Suppl. 1998;71:74–7. http://www.ncbi.nlm.nih.gov/pubmed/9779149.
Dias C, Silva MJ, Pereira E, et al. Optimal cerebral perfusion pressure management at bedside: a single-center pilot study. Neurocrit Care. 2015;. doi:10.1007/s12028-014-0103-8.
Aries MJH, Czosnyka M, Budohoski KP, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40(8):2456–63. doi:10.1097/CCM.0b013e3182514eb6.
Rosenthal G, Hemphill JC 3rd, Sorani M, et al. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2008;36(6):1917–24. doi:10.1097/CCM.0b013e3181743d77.
Gopinath SP, Robertson CS, Contant CF, et al. Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psychiatry. 1994;57(6):717–23. http://www.ncbi.nlm.nih.gov/pubmed/8006653.
Fandino J, Stocker R, Prokop S, Trentz O, Imhof HG. Cerebral oxygenation and systemic trauma related factors determining neurological outcome after brain injury. J Clin Neurosci. 2000;7(3):226–33. doi:10.1054/jocn.1999.0202.
Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009;111(4):672–82. doi:10.3171/2009.4.JNS081150.
Maloney-Wilensky E, Gracias V, Itkin A, et al. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review*. Crit Care Med. 2009;37(6):2057–63. doi:10.1097/CCM.0b013e3181a009f8.
Oddo M, Bösel J, Participants in the International Multidisciplinary Consensus Conference on Multimodality Monitoring. Monitoring of brain and systemic oxygenation in neurocritical care patients. Neurocrit Care. 2014;21 Suppl 2:S103–S120. doi:10.1007/s12028-014-0024-6.
Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR. Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg. 1996;85(5):751–7. doi:10.3171/jns.1996.85.5.0751.
Filippi R, Reisch R, Mauer D, Perneczky A. Brain tissue pO2 related to SjvO2, ICP, and CPP in severe brain injury. Neurosurg Rev. 2000;23(2):94–7. http://www.ncbi.nlm.nih.gov/pubmed/10926102.
Gupta AK, Hutchinson PJ, Al-Rawi P, et al. Measuring brain tissue oxygenation compared with jugular venous oxygen saturation for monitoring cerebral oxygenation after traumatic brain injury. Anesth Analg. 1999;88(3):549–53. http://www.ncbi.nlm.nih.gov/pubmed/10072004.
Chang JJJ, Youn TS, Benson D, et al. Physiologic and functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37(1):283–90. doi:10.1097/CCM.0b013e318192fbd7.
Rockswold GL, Solid CA, Paredes-Andrade E, Rockswold SB, Jancik JT, Quickel RR. Hypertonic saline and its effect on intracranial pressure, cerebral perfusion pressure, and brain tissue oxygen. Neurosurgery. 2009;65(6):1035–41; discussion 1041–1042. doi:10.1227/01.NEU.0000359533.16214.04.
Rockswold SB, Rockswold GL, Zaun DA, et al. A prospective, randomized clinical trial to compare the effect of hyperbaric to normobaric hyperoxia on cerebral metabolism, intracranial pressure, and oxygen toxicity in severe traumatic brain injury. J Neurosurg. 2010;112(5):1080–94. doi:10.3171/2009.7.JNS09363.
Spiotta AM, Stiefel MF, Gracias VH, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113(3):571–80. doi:10.3171/2010.1.JNS09506.
Stiefel MF, Spiotta A, Gracias VH, et al. Reduced mortality rate in patients with severe traumatic brain injury treated with brain tissue oxygen monitoring. J Neurosurg. 2005;103(5):805–11. doi:10.3171/jns.2005.103.5.0805.
Nangunoori R, Maloney-Wilensky E, Stiefel M, et al. Brain tissue oxygen-based therapy and outcome after severe traumatic brain injury: a systematic literature review. Neurocrit Care. 2012;17(1):131–8. doi:10.1007/s12028-011-9621-9.
Green JA, Pellegrini DC, Vanderkolk WE, Figueroa BE, Eriksson EA. Goal directed brain tissue oxygen monitoring versus conventional management in traumatic brain injury: an analysis of in hospital recovery. Neurocrit Care. 2013;18(1):20–5. doi:10.1007/s12028-012-9797-7.
Martini RP, Deem S, Yanez ND, et al. Management guided by brain tissue oxygen monitoring and outcome following severe traumatic brain injury. J Neurosurg. 2009;111(4):644–9. doi:10.3171/2009.2.JNS08998.
Adamides AA, Cooper DJ, Rosenfeldt FL, et al. Focal cerebral oxygenation and neurological outcome with or without brain tissue oxygen-guided therapy in patients with traumatic brain injury. Acta Neurochir. 2009;151(11):1399–409. doi:10.1007/s00701-009-0398-y.
Fletcher JJ, Bergman K, Blostein PA, Kramer AH. Fluid balance, complications, and brain tissue oxygen tension monitoring following severe traumatic brain injury. Neurocrit Care. 2010;13(1):47–56. doi:10.1007/s12028-010-9345-2.
McCarthy MC, Moncrief H, Sands JM, et al. Neurologic outcomes with cerebral oxygen monitoring in traumatic brain injury. Surgery. 2009;146(4):585–90; discussion 590–591. doi:10.1016/j.surg.2009.06.059.
Ponce LL, Pillai S, Cruz J, et al. Position of probe determines prognostic information of brain tissue PO2 in severe traumatic brain injury. Neurosurgery. 2012;70(6):1492–502; discussion 1502–1503. doi:10.1227/NEU.0b013e31824ce933.
Timofeev I, Nortje J, Al-Rawi PG, Hutchinson PJA, Gupta AK. Extracellular brain pH with or without hypoxia is a marker of profound metabolic derangement and increased mortality after traumatic brain injury. J Cereb Blood Flow Metab. 2013;33(3):422–7. doi:10.1038/jcbfm.2012.186.
Timofeev I, Carpenter KLH, Nortje J, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134(Pt 2):484–94. doi:10.1093/brain/awq353.
Nordström C-H, Reinstrup P, Xu W, Gärdenfors A, Ungerstedt U. Assessment of the lower limit for cerebral perfusion pressure in severe head injuries by bedside monitoring of regional energy metabolism. Anesthesiology. 2003;98(4):809–14. http://www.ncbi.nlm.nih.gov/pubmed/12657839.
Ståhl N, Ungerstedt U, Nordström CH. Brain energy metabolism during controlled reduction of cerebral perfusion pressure in severe head injuries. Intensive Care Med. 2001;27(7):1215–23. http://www.ncbi.nlm.nih.gov/pubmed/11534571.
Vespa P, Bergsneider M, Hattori N, et al. Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metab. 2005;25(6):763–74. doi:10.1038/sj.jcbfm.9600073.
Stein NR, McArthur DL, Etchepare M, Vespa PM. Early cerebral metabolic crisis after TBI influences outcome despite adequate hemodynamic resuscitation. Neurocrit Care. 2012;17(1):49–57. doi:10.1007/s12028-012-9708-y.
Verweij BH, Muizelaar JP, Vinas FC, Peterson PL, Xiong Y, Lee CP. Impaired cerebral mitochondrial function after traumatic brain injury in humans. J Neurosurg. 2000;93(5):815–20. doi:10.3171/jns.2000.93.5.0815.
Kontos HA, Wei EP, Navari RM, Levasseur JE, Rosenblum WI, Patterson JL Jr. Responses of cerebral arteries and arterioles to acute hypotension and hypertension. Am J Physiol. 1978;234(4):H371–H383. http://www.ncbi.nlm.nih.gov/pubmed/645875.
Hossmann KA. Viability thresholds and the penumbra of focal ischemia. Ann Neurol. 1994;36(4):557–65. doi:10.1002/ana.410360404.
Osol G, Brekke JF, McElroy-Yaggy K, Gokina NI. Myogenic tone, reactivity, and forced dilatation: a three-phase model of in vitro arterial myogenic behavior. Am J Physiol Heart Circ Physiol. 2002;283(6):H2260–7. doi:10.1152/ajpheart.00634.2002.
Avezaat CJ, van Eijndhoven JH, Wyper DJ. Cerebrospinal fluid pulse pressure and intracranial volume-pressure relationships. J Neurol Neurosurg Psychiatry. 1979;42(8):687–700. http://www.ncbi.nlm.nih.gov/pubmed/490174.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons, et al. Guidelines for the management of severe traumatic brain injury. VII. Intracranial pressure monitoring technology. J Neurotrauma. 2007;24 Suppl 1(supplement 1):S45–S54. doi:10.1089/neu.2007.9989.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wang, J., Altaweel, L. (2017). Hemodynamic Considerations in the Polytrauma Patient with Traumatic Brain Injury (TBI). In: Ecklund, J., Moores, L. (eds) Neurotrauma Management for the Severely Injured Polytrauma Patient. Springer, Cham. https://doi.org/10.1007/978-3-319-40208-6_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-40208-6_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40206-2
Online ISBN: 978-3-319-40208-6
eBook Packages: MedicineMedicine (R0)