Abstract
Background
Cerebral edema and raised intracranial pressure are common problems in neurological intensive care. Osmotherapy, typically using mannitol or hypertonic saline (HTS), has become one of the first-line interventions. However, the literature on the use of these agents is heterogeneous and lacking in class I studies. The authors hypothesized that clinical practice would reflect this heterogeneity with respect to choice of agent, dosing strategy, and methods for monitoring therapy.
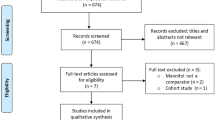
Methods
An on-line survey was administered by e-mail to members of the Neurocritical Care Society. Multiple-choice questions regarding use of mannitol and HTS were employed to gain insight into clinician practices.
Results
A total of 295 responses were received, 79.7% of which were from physicians. The majority (89.9%) reported using osmotherapy as needed for intracranial hypertension, though a minority reported initiating treatment prophylactically. Practitioners were fairly evenly split between those who preferred HTS (54.9%) and those who preferred mannitol (45.1%), with some respondents reserving HTS for patients with refractory intracranial hypertension. Respondents who preferred HTS were more likely to endorse prophylactic administration. Preferred dosing regimens for both agents varied considerably, as did monitoring parameters.
Conclusions
Treatment of cerebral edema using osmotically active substances varies considerably between practitioners. This variation could hamper efforts to design and implement multicenter trials in neurocritical care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral edema is a pervasive problem in neurocritical care. It is an inevitable consequence of acute brain injury, including ischemic stroke, intracranial hemorrhage (ICH), traumatic brain injury (TBI), subarachnoid hemorrhage (SAH), CNS infections, and intracranial neoplasms. It is widely recognized as one of the underlying causes of secondary brain injury contributing to poor patient outcome in many of these disease states. Unchecked brain edema has potentially devastating consequences, including intracranial hypertension, cerebral ischemia, herniation, and eventual progression to death. Consequently, early recognition and treatment are critical.
Use of osmotically active substances is the mainstay of therapy for cerebral edema, with or without associated intracranial hypertension [1]. Mannitol and hypertonic saline have gained widespread acceptance; however, little clinical data inform their use. Current practice guidelines for ICH, ischemic stroke, and TBI acknowledge that osmotically active substances may play a useful role, but have been unable to provide detailed recommendations regarding clinical applications secondary to a lack of high quality clinical trials [2–4].
In the absence of applicable large-scale randomized controlled trials, we hypothesized that the indications for osmotherapy, choice of agent, dosing regimen, and method for monitoring therapy would vary considerably between practitioners and institutions. If true, this heterogeneity could significantly undermine efforts to design multicenter trials in the neurocritical care community. Consequently, we designed a survey in an effort to better understand the practice patterns governing the use of these agents in the neurocritical care community. The authors also sought to explore the impact of physician training on use of osmotically active substances.
Materials and Methods
Survey Development and Administration
After obtaining approval from the Institutional Review Board, an on-line survey consisting of 20 multiple-choice questions was generated using a commercial service. The survey was developed by an interdisciplinary team of neurocritical care clinicians, all of whom had considerable experience managing patients with cerebral edema and intracranial hypertension. The survey addressed demographics, indications for the use of osmotherapy, choice of agent, dosing strategy, and criteria for discontinuation of therapy. Several items permitted multiple responses, and some provided the opportunity for open-ended responses. The survey was approved for distribution by the Neurocritical Care Society Board of Directors, and the members of the Society were invited to participate by e-mail. Responses were anonymous. The initial invitation was distributed on January 12, 2009, with a second request issued to the same recipients approximately 6 weeks later.
Data Analysis
Response rates were calculated as a percentage of those who responded to a given question, as opposed to a percentage of all survey respondents. Certain questions were directed at a designated subset of survey takers; i.e., physicians; consequently, the number of respondents varied between items. In some cases, more than one response was permitted; in those instances, the survey responses will exceed 100%.
Results
Demographics
Members of the Neurocritical Care Society were sent invitations to participate in this survey via e-mail in January, 2009. A total of 295 responses were received, 279 (94.6%) of which were complete. The majority of respondents (79.7%) were physicians; physician assistants, and nurse practitioners comprised 8.8% of the sample, followed by clinical pharmacists (7.5%), and registered nurses (4.1%). Among physicians, 58.3% listed neurology as their primary specialty (see Fig. 1), and 59.6% reported fellowship training in neurocritical care.
Indications for Osmotherapy
Clinicians reported using osmotherapy in a wide range of disease states, including TBI (89.1%), SAH (67.3%), ICH (68.3%), and ischemic stroke (62.7%). The majority of survey respondents reported using osmotherapy on an as-needed basis, either for intracranial hypertension (89.9%) or for cerebral edema as noted on imaging studies (58.7%). A similar proportion employed osmotically active substances empirically for patients with declining exams (54.9%). Only a small minority reported using osmotherapy prophylactically, either for edema (17.8%) or for intracranial hypertension (16.8%). Clinicians who indicated a preference for HTS were more likely to endorse prophylactic osmotherapy (49.4 vs. 16.4% of those who prefer mannitol). Responses were consistent across disciplines and physician specialties.
Choice of Agent
A slight majority of survey respondents favored the use of HTS (54.9%) over mannitol (45.1%). Among those that preferred HTS (Table 1), the most commonly cited reasons were less rebound edema (43.8%), duration of benefit (42.6%), and lack of systemic side effects (39.4%). Several clinicians (15.6% of those who responded to this item) commented that they chose HTS in patients who would be expected to benefit from volume expansion as opposed to osmotic diuresis. Of those who preferred mannitol (Table 2), 35.0% attributed their preference to greater experience; the next most commonly stated reason was the lack of need for central access (17.1%). A subset of those who employ mannitol noted that their institutions either had not yet approved, or did not carry hypertonic saline. Others described using mannitol preferentially for acute decompensation, and reserving HTS for patients with persistent intracranial hypertension. A greater proportion of neurosurgeons (61.9%) than neurologists (44.9%) reported a preference for mannitol, but this difference was not statistically significant.
Mannitol: Use in Clinical Practice
Ninety-five percent (95.4%) of survey participants use mannitol in their clinical practice. The majority reported using bolus doses delivered for the treatment of elevated intracranial pressure or decline in exam (83.0%). Twenty-eight percent reported using scheduled dosing for patients without intracranial pressure (ICP) monitors, and 1.8% reported using continuous infusions. Eighty percent (80.2%) of respondents routinely monitor serum osmolality in patients receiving mannitol, 31.3% track serum sodium levels, and only 22.5% report monitoring the osmolal gap. Interestingly, a higher proportion of neurosurgeons than neurologists reported following sodium levels (57.1 vs. 24.4%). Twenty-two clinicians reported relying on the clinical exam and/or ICP alone, and one neurologist described following the ratio of blood urea nitrogen to serum creatinine for evidence of intravascular volume depletion. For those that do routinely monitor serum osmolality, 320 mOsms was the cutoff chosen by the majority of respondents (57.8%); a minority (19.6%) selected a cutoff of 340 mOsms. Physicians with training in neurocritical care were somewhat less likely to monitor serum osmolality than those without (66.4 vs. 75.3%), but the target values did not differ between groups. More than half of study participants (58.8%) also reported following serum sodium levels as a means to guide therapy, though a wide range of target values were reported. Most responses (69.2%, or 39.4% of all respondents) fell within the 150–160 range, with some clinicians commenting that they will tolerate higher values if alternative interventions have been exhausted.
Hypertonic Saline: Use in Clinical Practice
Eighty-nine percent of sampled clinicians reported using HTS for management of cerebral edema or ICH. Patterns of administration varied considerably. Approximately, a third of respondents (79, or 28.1%) reported using continuous infusion exclusively; an additional quarter (74, or 26.6%) exclusively used bolus doses for intracranial hypertension; and several others (53, or 18.9%) reported using both strategies. A minority (43, or 15.3%) reported using scheduled bolus doses, with or without ICP monitoring. Among those who employ continuous infusions, 65.9% prefer 3% normal saline; however, clinicians reported using a variety of formulations ranging from 1.5% to 14.6%. A subset of practitioners (91, or 33.2%) reported adding sodium acetate to their infusions in order to prevent or treat hyperchloremic metabolic acidosis. This practice was significantly more widespread among fellowship-trained neurointensivists, with 50.0% versus 28.6% reporting some acetate use (P = 0.03). In the open-ended response section, 3 clinicians (1.1%) indicated that they use sodium bicarbonate for this purpose. Virtually all clinicians who reported using HTS also reported monitoring serum sodium levels; 30.1% also follow serum osmolality. Once again, most respondents titrated to a sodium level between 150 and 160 (67.0%), with 10.2% being willing to tolerate sodium levels as high as 165. Several practitioners commented that the target sodium level varies according to the clinical situation, with two noting that the rate of change is an important factor. Of those who took serum osmolality into account, 64 out of 104 (61.2%) selected 320 mOsms as the most appropriate cutoff.
Discontinuation of Osmotherapy
Respondents cited a number of criteria for use in determining when to discontinue osmotherapy. The majority (87.7%) reported that normalization of intracranial pressure was a necessary precondition. Sixty-one respondents (22.0%) listed intracranial pressure as the only consideration, 154 clinicians (55.6%) also reported taking the patient’s clinical exam into account. Radiographic findings were considered important by 99 respondents (35.7%), though no one listed radiographic improvement as the sole criteria for discontinuation of therapy. Seventy-three individuals (26.4%) felt that the time course of the patient’s disease process was an important consideration, with 29 (10.4%) listing clinical considerations as the only relevant factors in the decision to withdraw osmotherapy. Two respondents reported that measures of cerebral perfusion and vasomotor reactivity factored into their decisions as well.
Discussion
Prevention of secondary brain injury is one of the primary goals of the clinician; efforts to do so often center on the management of cerebral edema and intracranial hypertension. Mannitol has been used for this purpose since the 1960s [5, 6]. In addition to establishing an osmotic gradient across the blood–brain barrier, experimental data indicate that mannitol has rheological effects that contribute to ICP reduction and can affect cerebral blood flow (CBF) both regionally and at the level of the microcirculation [6–10]. In the presence of preserved cerebral autoregulation, mannitol infusion induces transient vasoconstriction. This has been explained alternately as a response to increased cerebral perfusion pressure (CPP) resulting from volume expansion, or as a response to increased CBF resulting from decreased blood viscosity [10, 11]. Studies evaluating the clinical effect of mannitol on blood flow and oxygenation have been inconsistent. Mannitol has been shown to transiently increase CBF in several small studies of patients with a variety of diagnoses, [7–9] but this finding could not be confirmed in a group of patients with ICH [12]. Similarly, data regarding the effect of mannitol on cerebral oxygenation in TBI have been conflicting [13–16]. There is also experimental evidence that mannitol functions as a free-radical scavenger and inhibits programmed cell death, leading to speculation that it may have neuroprotective effects [10, 17, 18].
Hypertonic saline solution was found to reduce the volume of brain tissue in experimental models almost a century ago, but interest in the use of HTS solutions for brain injured patients lagged until the 1980s and 1990s [1]. At that time, reports emerged that HTS resuscitation may convey a survival benefit in hemorrhagic shock patients with coexisting TBI[19]; however, this could not be confirmed in a later trial [20]. Hypertonic saline has been proven effective in reducing ICP in a number of clinical scenarios, including those in which intracranial hypertension had proven refractory to mannitol [21–24]. Unlike mannitol, it is a very effective volume expander, and has been shown to improve cardiac output, systemic tissue perfusion, and mean arterial pressure in trauma patients [1, 25, 26]. It has proven to be effective in increasing CBF in patients with poor-grade subarachnoid hemorrhage, regardless of the intracranial pressure. It has rheological effects similar to those observed with mannitol [27], and additionally has immunomodulatory effects which have been demonstrated both in trauma and in sepsis (see Table 3) [28, 29].
Though both agents are relatively safe in clinical practice, a variety of complications have been described. Hypertonic saline is known to cause venous sclerosis [30], and concentrations above 2% are best administered via central venous catheter. Other reported adverse effects have included acute kidney injury, coagulopathy, exacerbation of congestive heart failure, hypokalemia, and seizure [25, 31]. Central pontine myelinolysis is a potential risk, though it has never been reported in patients receiving HTS for treatment of cerebral edema. Recognition of the effect of HTS on neutrophil function led to speculation that administration may increase susceptibility to infection, but a recent observational study failed to substantiate this concern [32]. The most common side effects observed with mannitol administration are hypovolemia, hyperkalemia, pulmonary edema, and renal insufficiency [1, 10]. Both agents produce hypernatremia, which has been associated with increased mortality and renal failure in critically ill patients with and without neurological disease [33]. To some extent, these findings may be confounded by disease severity; however, the upper limit of mannitol/HTS dose remains to be defined. Perhaps the most significant question surrounding the use of osmotically active agents is the possibility of rebound cerebral edema. Prolonged exposure to a hypertonic environment leads to increases in intracellular concentrations of electrolytes and organic osmoles in neuronal tissue [10]. Subsequent administration of relatively hypo-osmolal fluids can result in influx of water into the intracellular space, potentially increasing cerebral edema and intracranial pressure. Furthermore, the reduction in brain water content resulting from use of osmotherapy is dependent upon the integrity of the blood–brain barrier. In regions where the barrier has been disrupted, osmotically active agents can diffuse into the brain parenchyma. Mannitol accumulation within edematous brain tissue has been demonstrated in patients with primary brain tumors [34, 35], and in at least one patient with an ischemic stroke [36], though the clinical relevance of this phenomenon remains uncertain. Though tissue accumulation of sodium chloride has not been demonstrated, clinically significant rebound edema has been described in ICH patients after treatment with infusions of HTS [37].
We have reported a preference of practitioners for HTS over mannitol. We believe the above comparative discussion of pros and cons highlights the main reasons employed by the surveyed practitioners. Namely, these are: a decreased likelihood for rebound cerebral edema, longer duration of clinical benefit, safer systemic side-effect profile, and volume expansion. Despite decades of experience, clinical trials pertaining to the use of these agents are few in number. A recent review revealed only nine clinical trials of HTS solutions in neurosurgical practice; the majority of these included fewer than 30 patients [21]. Some trials described the use of continuous infusions, whereas others employed bolus doses in response to elevated intracranial pressure. Clinical practice among neurointensivists, as reflected in our survey, follows the same pattern with a third of clinicians using continuous infusion to establish and maintain a prespecified sodium level, a third using bolus, as needed, doses and another third combining the two strategies. This survey does not provide insight into the underlying rationale for these choices. We speculate that in the absence of scientific evidence practitioners follow local patterns of experience.
The doses described in the literature vary widely, with relatively few studies relying on weight-based dosing. The literature on the use of mannitol displays similar variability, with bolus doses ranging from 0.5 g/kg to 1.4 g/kg, and continuous infusions reported in a minority of studies [24, 38–43]. Only three direct comparisons have been reported, all of which were limited by small sample sizes [7, 24, 39]. Vialet et al. randomized trauma patients with refractory intracranial hypertension to 2 ml/kg of either 7.5% HTS (2400 mOsm/kg/H2O) or 20% mannitol (1160 mOsm/kg/H2O) over a period of several days and found that patients receiving HTS required fewer interventions for elevated ICP [24]. Two small trials have evaluated equimolar doses of HTS and 20% mannitol, and found equal efficacy in reducing ICP [7] and producing intraoperative brain relaxation [39]. However, no trial to date has compared mannitol and HTS with respect to patient outcome.
We inquired on the monitoring targets used by practitioners during osmotherapy. According to our results, HTS therapy is guided heavily by sodium levels and to a lesser extent by serum osmolality. The reverse applies to the use of mannitol. For either agent the numbers indicated by our responders are Na levels of 150–160 mEq/l and a serum osmolality ≤320 mOsm/l. Evidence for these target ranges is sparse. Aiyagari et al. have reported an independent association between Na exceeding 160 and mortality [33]. Regarding mannitol use, and as suggested by Diringer and Zazulia, we often exceed the 320 threshold. Monitoring the osmolar gap as an index of renal mannitol clearance to avoid nephrotoxicity has been suggested, but only 1 out of 5 practitioners in our sample report doing so routinely [10].
To our knowledge, this is the first attempt to characterize the clinical application of osmotherapy within the neurocritical care community. Our results confirm that clinician practice differs widely with respect to the use of osmotherapy, as would be expected given the absence of high quality clinical trials. This study has several limitations, the most obvious of which is that the study population does not accurately represent the range of practitioners who may find themselves managing patients with cerebral edema. By targeting members of the Neurocritical Care Society, we selected a population of individuals with demonstrated interest and expertise in this patient population. We hope that besides the mere recording of practice and despite the significant variability, our data may serve as an osmotherapy guide for practitioners beyond specialized neurointensivists. It is likely that our results underestimate the degree of heterogeneity which exists in the community at large. The need for large, randomized trials in neurocritical care is widely recognized; however, lack of consensus among experts regarding treatment of cerebral edema has the potential to undermine these efforts.
Conclusions
The use of mannitol and HTS in neurocritical care patients varies considerably. Due to the different mechanisms of action and side-effect profiles of these agents, it is reasonable to hypothesize that these practice variations could impact patient outcomes. As a consequence, the lack of consensus could undermine efforts to conduct multicenter, randomized trials in neuroscience intensive care units. A large-scale randomized trial of mannitol versus HTS will be necessary to resolve these inconsistencies.
References
Bhardwaj A. Osmotherapy in neurocritical care. Curr Neurol Neurosci Rep. 2007;7:513–21.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. II. Hyperosmolar therapy. J Neurotrauma. 2007;24(Suppl 1):S14–20.
Harold P, Adams J, Zoppo Gd, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke. Stroke. 2007;38:1655–711.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update. Stroke. 2007;38:2001–23.
Wise BL, Chater N. The value of hypertonic mannitol solution in decreasing brain mass and lowering cerebrospinal fluid pressure. J Neurosurg. 1962;19:1038–43.
Paczynski RP. Osmotherapy. Basic concepts and controversies. Crit Care Clin. 1997;13:105–29.
Francony G, Fauvage B, Falcon D, et al. Equimolar doses of mannitol and hypertonic saline in the treatment of increased intracranial pressure. Crit Care Med. 2008;36:795–800.
Lee SC, Chen JF, Lee ST. Continuous regional cerebral blood flow monitoring in the neurosurgical intensive care unit. J Clin Neurosci. 2005;12:520–3.
Hartmann A, Dettmers C, Schott H, Beyenburg S. Cerebral blood flow and rheologic alterations by hyperosmolar therapy in patients with brain edema. Acta Neurochir Suppl. (Wien). 1990;51:168–9.
Diringer MN, Zazulia AR. Osmotic therapy: fact and fiction. Neurocrit Care. 2004;1:219–33.
Rangel-Castillo L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 2008;26:521–41.
Kalita J, Misra UK, Ranjan P, Pradhan PK, Das BK. Effect of mannitol on regional cerebral blood flow in patients with intracerebral hemorrhage. J Neurol Sci. 2004;224:19–22.
Oddo M, Levine JM, Frangos S, et al. Effect of mannitol and hypertonic saline on cerebral oxygenation in patients with severe traumatic brain injury and refractory intracranial hypertension. J Neurol Neurosurg Psychiatry. 2009;80:916–20.
Sakowitz OW, Stover JF, Sarrafzadeh AS, Unterberg AW, Kiening KL. Effects of mannitol bolus administration on intracranial pressure, cerebral extracellular metabolites, and tissue oxygenation in severely head-injured patients. J Trauma. 2007;62:292–8.
Gasco J, Sendra J, Lim J, Ng I. Linear correlation between stable intracranial pressure decrease and regional cerebral oxygenation improvement following mannitol administration in severe acute head injury patients. Acta Neurochir Suppl. 2005;95:73–7.
Hartl R, Bardt TF, Kiening KL, Sarrafzadeh AS, Schneider GH, Unterberg AW. Mannitol decreases ICP but does not improve brain-tissue pO2 in severely head-injured patients with intracranial hypertension. Acta Neurochir Suppl. 1997;70:40–2.
Alvarez B, Ferrer-Sueta G, Radi R. Slowing of peroxynitrite decomposition in the presence of mannitol and ethanol. Free Radic Biol Med. 1998;24:1331–7.
Korenkov AI, Pahnke J, Frei K, et al. Treatment with nimodipine or mannitol reduces programmed cell death and infarct size following focal cerebral ischemia. Neurosurg Rev. 2000;23:145–50.
Wade CE, Grady JJ, Kramer GC, Younes RN, Gehlsen K, Holcroft JW. Individual patient cohort analysis of the efficacy of hypertonic saline/dextran in patients with traumatic brain injury and hypotension. J Trauma. 1997;42:S61–5.
Cooper DJ, Myles PS, McDermott FT, et al. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: a randomized controlled trial. JAMA. 2004;291:1350–7.
Ogden AT, Mayer SA, Sander Connolly E Jr. Hyperosmolar agents in neurosurgical practice: the evolving role of hypertonic saline. Neurosurgery. 2005;57:207–15.
Schwarz S, Georgiadis D, Aschoff A, Schwab S. Effects of hypertonic (10%) saline in patients with raised intracranial pressure after stroke. Stroke. 2002;33:136–40.
Schwarz S, Schwab S, Bertram M, Aschoff A, Hacke W. Effects of hypertonic saline hydroxyethyl starch solution and mannitol in patients with increased intracranial pressure after stroke. Stroke. 1998;29:1550–5.
Vialet R, Albanese J, Thomachot L, et al. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 ml/kg 7.5% saline is more effective than 2 ml/kg 20% mannitol. Crit Care Med. 2003;31:1683–7.
Ziai WC, Toung TJ, Bhardwaj A. Hypertonic saline: first-line therapy for cerebral edema? J Neurol Sci. 2007;261:157–66.
Mattox KL, Maningas PA, Moore EE, et al. Prehospital hypertonic saline/dextran infusion for post-traumatic hypotension. The U.S.A. Multicenter Trial. Ann Surg. 1991;213:482–91.
Shackford SR, Norton CH, Todd MM. Renal, cerebral, and pulmonary effects of hypertonic resuscitation in a porcine model of hemorrhagic shock. Surgery. 1988;104:553–60.
Rizoli SB, Rhind SG, Shek PN, et al. The immunomodulatory effects of hypertonic saline resuscitation in patients sustaining traumatic hemorrhagic shock: a randomized, controlled, double-blinded trial. Ann Surg. 2006;243:47–57.
Poli-de-Figueiredo LF, Cruz RJ Jr, Sannomiya P, Rocha ESM. Mechanisms of action of hypertonic saline resuscitation in severe sepsis and septic shock. Endocr Metab Immune Disord Drug Targets. 2006;6:201–6.
Sadick NS. Sclerotherapy of varicose and telangiectatic leg veins. Minimal sclerosant concentration of hypertonic saline and its relationship to vessel diameter. J Dermatol Surg Oncol. 1991;17:65–70.
Himmelseher S. Hypertonic saline solutions for treatment of intracranial hypertension. Curr Opin Anaesthesiol. 2007;20:414–26.
Froelich M, Ni Q, Wess C, Ougorets I, Hartl R. Continuous hypertonic saline therapy and the occurrence of complications in neurocritically ill patients. Crit Care Med. 2009;37:1433–41.
Aiyagari V, Deibert E, Diringer MN. Hypernatremia in the neurologic intensive care unit: how high is too high? J Crit Care. 2006;21:163–72.
Sankar T, Assina R, Karis JP, Theodore N, Preul MC. Neurosurgical implications of mannitol accumulation within a meningioma and its peritumoral region demonstrated by magnetic resonance spectroscopy: case report. J Neurosurg. 2008;108:1010–3.
Palma L, Bruni G, Fiaschi AI, Mariottini A. Passage of mannitol into the brain around gliomas: a potential cause of rebound phenomenon. A study on 21 patients. J Neurosurg Sci. 2006;50:63–6.
Maioriello AV, Chaljub G, Nauta HJ, Lacroix M. Chemical shift imaging of mannitol in acute cerebral ischemia Case report. J Neurosurg. 2002;97:687–91.
Qureshi AI, Suarez JI, Bhardwaj A. Malignant cerebral edema in patients with hypertensive intracerebral hemorrhage associated with hypertonic saline infusion: a rebound phenomenon? J Neurosurg Anesthesiol. 1998;10:188–92.
Soustiel JF, Mahamid E, Chistyakov A, Shik V, Benenson R, Zaaroor M. Comparison of moderate hyperventilation and mannitol for control of intracranial pressure control in patients with severe traumatic brain injury—a study of cerebral blood flow and metabolism. Acta Neurochir. (Wien). 2006;148:845–51. discussion 51.
Rozet I, Tontisirin N, Muangman S, et al. Effect of equiosmolar solutions of mannitol versus hypertonic saline on intraoperative brain relaxation and electrolyte balance. Anesthesiology. 2007;107:697–704.
Harutjunyan L, Holz C, Rieger A, Menzel M, Grond S, Soukup J. Efficiency of 7.2% hypertonic saline hydroxyethyl starch 200/0.5 versus mannitol 15% in the treatment of increased intracranial pressure in neurosurgical patients—a randomized clinical trial [ISRCTN62699180]. Crit Care. 2005;9:R530–40.
Battison C, Andrews PJ, Graham C, Petty T. Randomized, controlled trial on the effect of a 20% mannitol solution and a 7.5% saline/6% dextran solution on increased intracranial pressure after brain injury. Crit Care Med. 2005;33:196–202. discussion 57–8.
Cruz J, Minoja G, Okuchi K, Facco E. Successful use of the new high-dose mannitol treatment in patients with Glasgow Coma Scale scores of 3 and bilateral abnormal pupillary widening: a randomized trial. J Neurosurg. 2004;100:376–83.
Cruz J, Minoja G, Okuchi K. Major clinical and physiological benefits of early high doses of mannitol for intraparenchymal temporal lobe hemorrhages with abnormal pupillary widening: a randomized trial. Neurosurgery. 2002;51:628–37. discussion 37–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hays, A.N., Lazaridis, C., Neyens, R. et al. Osmotherapy: Use Among Neurointensivists. Neurocrit Care 14, 222–228 (2011). https://doi.org/10.1007/s12028-010-9477-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9477-4