Abstract
During infancy, sleep is at a lifetime maximum, and the maturation of sleep is one of the most important physiological processes occurring during the first year of life, particularly the first 6 months. Sleep has a marked effect on cardiorespiratory control which is also rapidly maturing during infancy. Immaturity of cardiorespiratory control frequently leads to respiratory instability and prolonged pauses in breathing as manifest in apnea of prematurity and periodic breathing. During infancy, central apneas are common and obstructive apnea is rare. Although currently believed to be benign during this early period of development, there is growing evidence that they may be associated with developmental deficits in neurocognition. A failure of cardiorespiratory control mechanisms, together with an impaired arousal from sleep response, is believed to play an important role in the final event of the sudden infant death syndrome (SIDS). The “triple-risk model” describes SIDS as an event that results from the intersection of three overlapping factors: (1) a vulnerable infant, (2) a critical developmental period in homeostatic control, and (3) an exogenous stressor. In an attempt to understand how the triple-risk hypothesis is related to infant cardiorespiratory physiology, many researchers have examined how the known risk and protective factors for SIDS alter infant physiology and arousal, particularly during sleep. This review discusses the association between the three components of the triple-risk hypothesis and major risk factors for SIDS, such as prone sleeping and maternal smoking, together with three “protective” factors, and cardiovascular control and arousability from sleep in infants, and discusses their potential involvement in SIDS.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Pediatric obstructive sleep apnea
- Periodic breathing
- Apnea of prematurity
- Sudden infant death syndrome
- Sleeping position
- Maternal smoking
- Prematurity
Development of Sleep
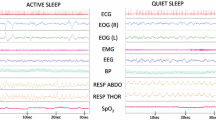
The maturation of sleep is one of the most important physiological processes occurring during the first year of life and is particularly rapid during the first 6 months after birth [1]. Behavioral states are defined by physiological and behavioral variables that are stable over time and occur repeatedly in an individual infant and also across infants [2]. The emergence of sleep states is dependent on the central nervous system and is a good and reliable indicator of normal and abnormal development [3]. Sleep states and sleep architecture in infants are quite different to those in adults. In infants, sleep states are defined as active sleep (AS) and quiet sleep (QS), which are the precursors of adult rapid eye movement sleep (REM sleep) and non-rapid eye movement sleep (NREM sleep), respectively. QS is characterized by high-voltage low-amplitude electroencephalogram activity, the absence of eye movements, and regular heart rate and respiration. In contrast, AS is characterized by low-amplitude high-frequency electroencephalogram activity, eye movements, and irregular heart rate and respiration (Fig. 8.1). In addition a third state, that of indeterminate sleep (IS), is defined when criteria for AS and QS are not met. IS is usually considered a sign of immaturity and the incidence decreases with increasing postnatal age.
Cardiorespiratory parameters in active and quiet sleep in an infant. ECG electrocardiograph, EOG electrooculograph, EMG electromyograph, EEG electroencephalograph, BP blood pressure, RESP ABDO abdominal respiratory effort, RESP THOR thoracic respiratory effort, SpO2 oxygen saturation, HR heart rate. Note regular breathing and heart rate in quiet sleep compared to active sleep
Rhythmic cyclical rest activity patterns can be observed in the human fetus from 28 weeks of gestation [4]. In infants born preterm, the infant sleep states cannot be distinguished in infants younger than 26 weeks of gestation [5]. By 28–30 weeks of gestation, AS can be recognized by the presence of eye movements, body movements, and irregular breathing and heart rate. At this gestational age, QS is difficult to identify as chin hypotonia is difficult to evaluate, and the majority of the sleep period is spent in AS. QS does not become clearly identifiable until about 36 weeks of gestational age [4]. The percentage of time spent in QS increases, and by term equal amounts of time are spent in both AS and QS with the two states alternating throughout each sleep period. The proportion of AS decreases across the first 6 months to make up approximately 25 % of total sleep time similar to that in adults [6]. In contrast, the proportion of QS increases with age to make up about 75 % of total sleep time by 6 months [6].
At term, infants sleep for about 16–17 h out of every 24 [4]. There is a gradual decrease in total sleep time with infants sleeping 14–15 h at 16 months of age and 13–14 h by 6–8 months of age. In the neonatal period, infants awaken every 2–6 h for feeding, regardless of the time of day, and stay awake for 1–2 h [7]. The major change in sleep/wake pattern occurs between 6 weeks and 3 months post term age [7]. During the first 6 months after term, consolidation and entrainment of sleep at night develops and sleep periods lengthen. At 3 weeks of age, the mean length of the longest sleep period has been reported to be 211.7 min, increasing to 358.0 min by 6 months of age [8]. The longest sleep period was randomly distributed between daytime and nighttime at 3 months but had moved to nighttime by 6 months [8].
Dramatic changes in the sleep electroencephalographic (EEG) patterns of infants occur during early infancy as the brain matures. The EEG patterns of QS and AS differ with a relatively continuous pattern in AS and a relatively discontinuous pattern in QS. A continuous pattern is defined by the presence of background activity throughout each 30 s epoch scored, and a discontinuous pattern is defined by the presence of higher amplitude EEG waves during <50 % of each epoch [9]. A semi-discontinuous EEG pattern of depressions and continuous delta activity during ≤70 % each epoch is called a tracé alternant pattern and can be identified at 32–34 weeks of gestational age [9]. This pattern is prominent in preterm infants but also occurs in infants born at term and disappears after 1 month after term equivalent age. Sleep spindles appear coincidentally with the disappearance of tracé alternant [10]. True continuous delta frequency does not appear until 8–12 weeks of age, and it is not until this age that adult criteria for determining the stages of NREM sleep can be used [11].
In summary, during infancy, sleep is at a lifetime maximum, and significant changes occur in the maturation of sleep which reflect maturation of the central nervous system. Sleep has a marked effect on cardiorespiratory control. Cardiorespiratory disturbances occur predominantly in AS sleep, so the predominance of AS in early infancy may increase the risk of cardiorespiratory disturbances during this period of development.
Apnea of Prematurity
One of the major problems facing preterm infants after birth is the immaturity of their cardiorespiratory system which often leads to repeated apneic events. Apnea of prematurity is defined as the cessation of breathing for >20 s, or if the breathing pause is shorter in duration, it is associated with bradycardia, cyanosis, marked pallor, or hypotonia [12]. Apnea of prematurity is extremely common, occurring in more than 85 % of infants born prior to 34 weeks of gestation. The incidence of apnea of prematurity is inversely related to gestational age: 3–5 % of term-born infants, 7 % of infants born at 34–35 weeks, 15 % of infants born at 32–33 weeks, 54 % of infants born at 30–31 weeks, and nearly 100 % of infants born less than 29 weeks experience episodes of apnea of prematurity [13, 14]. There are also marked changes in apnea frequency with postnatal age, with few events in the first week of life, then a progressive increase in weeks 2–3 which plateau in weeks 4–6, and then decrease in weeks 6–8 [15].
Frequently, the magnitude and frequency of the apneic events are underestimated due to the current clinical settings of pulse oximeter monitors, which often are set with long averaging times and to alarm at events longer than 20 s duration. In a study which used a 2 s averaging time and which counted apneas where oxygen saturation fell to ≤80 % for between 3 and 10 s, between 50 and 100 events/day were recorded [16]. It has recently been recommended that to take these frequent apneas which are associated with significant desaturation into account, that all events longer than 5 s should be recorded [17].
Studies have shown that excessive or persistent apnea and bradycardia are associated with long-term neurodevelopmental problems [18]. It is well known that obstructive sleep apnea in children and adults is associated with neurocognitive deficits, and the repetitive hypoxic events associated with this condition have been proposed as the primary mechanism. It is also possible that postnatal intermittent hypoxia can affect cardiovascular control beyond the neonatal period with studies in both rodent models [19] and human infants [20] demonstrating this.
Methylxanthines have been used since the 1970s for the treatment of apnea of prematurity and also to facilitate extubation and weaning off mechanical ventilation [21, 22]. Methylxanthines cross the blood-brain barrier [23], and their primary action is to antagonize the A1/A2a adenosine receptors in the CNS. Methylxanthines improve apnea of prematurity by increasing minute ventilation and improving both hypercapnic and hypoxic ventilatory drive [24, 25].
Today, caffeine is the most commonly used methylxanthine in neonatal units worldwide. Caffeine’s universal acceptance followed the 2006 CAP (caffeine for apnea of prematurity) randomized control trial, which compared caffeine citrate (20 mg/kg loading dose of caffeine citrate followed by 5 mg/kg/day) with placebo in very low birth weight preterm infants. The study demonstrated both significant short-term benefits of reduced incidence of bronchopulmonary dysplasia, medically and surgically treated ductus arteriosus, and long-term benefits of improved rates of survival without neurodevelopmental delay and significantly reduced incidences of cerebral palsy at 18–21 months [26, 27]. Improved microstructural development of white matter has been demonstrated in a subsample of these children who underwent brain magnetic resonance imaging (MRI) at term equivalent age, a finding which may explain the improved neurodevelopmental outcomes [28]. However, when reassessed at 5 years of age, there was no longer any difference in rate of survival without disability between children treated with caffeine and those that were not [29].
Apneas can occur in isolation or in a repetitive pattern termed periodic breathing. Repetitive short central apneas are termed periodic breathing (defined as three or more sequential central apneas each lasting ≥3 s) and are common in term babies in the first 2 weeks of life but significantly decrease with age [30]. In term babies, the frequency of periodic breathing is low, making up <1 % of total sleep time [30, 31]. Periodic breathing is significantly more prevalent in ex-preterm infants compared to term-born infants at term equivalent age [32]. Because of its high prevalence, and the fact that it is not usually associated with life-threatening hypoxia or bradycardia, the traditional view of periodic breathing is that it is simply due to immaturity of respiratory control and is benign [33]. However, recent studies have shown that periodic breathing can be associated with significant deficits in cerebral oxygenation [34] (Fig. 8.2), although any link to neurocognitive deficits has yet to be elucidated.
Polysomnographic example of the effects of periodic breathing in an infant born at 27 weeks of gestational age and studied at 2–4 weeks corrected age after discharge home. Periodic breathing is associated with repetitive oxygen desaturations, marked falls in cerebral tissue oxygenation index as measured with near-infrared spectroscopy, and repetitive bradycardias which worsen over time. This infant spent 28 % of his total sleep time in periodic breathing
Sleep Apnea in Infants
Apneas are characterized as central, obstructive, or mixed. Central apneas are defined as a cessation of nasal and oral airflow in conjunction with an absence of respiratory effort. Obstructive apneas are defined as the cessation of nasal and oral airflow in the presence of continued respiratory effort against airway obstruction. Central apneas are common in infancy and can occur spontaneously but occur more frequently after a movement [35, 36]. Traditionally, they are considered benign as they are not associated with significant desaturation and occur in healthy infants [36]. The frequency of central apneas declines with age. In a study by Brockmann et al., the median number of events per hour declined from 5.5 (minimum 0.9; maximum 44.3) at 1 month of age to 4.1 (minimum 1.2; maximum 27.3) at 3 months [31]. The authors suggested these high rates of central apnea may be simply due to the fact that the current definitions for central apneas used for older children are not appropriate for young infants.
Obstructive apneas are reported to be rare in infancy [31, 37]. However, snoring is reported to be common, with prevalence rates ranging from 5.6 to 26 % [38–41]. These wide ranges in prevalence may have been due to confounders, with some studies including infants with colds and others studying different ethnicities. In a study of healthy predominantly Caucasian children aged 0–3 months, a prevalence of 9 % has been reported [42]. A significantly greater proportion of 2–3-month-old infants were reported to snore habitually than 0–1-month-old infants [42]. Cognitive ability at 6 months of age was found to be lower in those infants who began snoring frequently (≥3 nights/week) within the first month of life [43].
In summary, central apnea is common in infants but obstructive apnea is rare. Both forms of apnea have been considered benign during infancy, but there is growing evidence that they may be associated with neurological deficits.
Sudden Infant Death Syndrome
Sudden infant death syndrome (SIDS) is defined as “the sudden and unexpected death of an infant under 1 year of age, with the onset of the lethal episode apparently occurring during sleep, that remains unexplained after a thorough investigation including performance of a complete autopsy and review of the circumstances of death” [44]. The incidence of SIDS was more than halved after public health campaigns publicized the known major risk factors of prone sleeping, maternal smoking, and overheating [45]. However, SIDS still remains the leading cause of unexpected death in infants in Western countries, contributing to almost 50 % of all postneonatal deaths [46, 47].
As SIDS is a diagnosis of exclusion, there has been considerable research into the underlying mechanisms which may underpin known risk factors. SIDS has long been believed to be multifactorial in origin. The triple-risk hypothesis [48] proposes that when a vulnerable infant, such as one born preterm or exposed to maternal smoking, is at a critical but unstable developmental period in homeostatic control and is exposed to an exogenous stressor, such as being placed prone to sleep, then SIDS may occur. The model proposes that infants will die of SIDS only if all three factors are present and that the vulnerability lies dormant until they enter the critical developmental period and are exposed to an exogenous stressor. SIDS usually occurs during sleep, and the peak incidence is between 2 and 4 months of age, when sleep patterns are rapidly maturing. The final pathway to SIDS is widely believed to involve immature cardiorespiratory control, in conjunction with a failure of arousal from sleep [45]. Support for this hypothesis comes from numerous physiological studies showing that the major risk factors for SIDS (prone sleeping, maternal smoking, prematurity, head covering) have significant effects on blood pressure and heart rate and their control [49] and impair arousal from sleep [50].
Vulnerable Infant
Neuropathologic findings from SIDS victims show significant deficits in brainstem and cerebellar structures involved in the regulation of respiratory drive, cardiovascular control, sleep/wake transition, and arousal from sleep [51–58]. Furthermore, genetic polymorphisms have been identified in SIDS victims which affect genes involved in autonomic function, neurotransmission, energy metabolism, and the response to infection [59–63].
Prenatal and/or postnatal exposure to cigarette smoke is one factor which increases infant vulnerability to SIDS [64, 65], with over 40 studies showing a positive association with risk ratios of between 0.7 and 4.85 [66–69]. This increased SIDS risk is likely to be due to the effects of nicotine exposure on autonomic control and arousal [58, 70–72]. In support of this idea, Duncan and colleagues [73] found that chronic exposure to nicotine in the prenatal baboon fetus altered serotonergic and nicotinic acetylcholine receptor binding in regions of the medulla, critical to cardiorespiratory control. Furthermore, they identified that these alterations were associated with abnormalities in fetal heart rate variability, indicating altered cardiovascular control [73]. Studies in infants exposed to maternal smoking have demonstrated altered heart rate and blood pressure control compared with control infants [74–80]. Maternal tobacco smoking also decreases both total arousability and the proportion of cortical arousals. Arousal impairment was observed for both spontaneous arousals from sleep and responses induced by various stimuli [81–87]. Few mothers change their smoking behavior postpartum [88]; therefore, it is difficult to ascertain whether these physiological effects are caused by prenatal or postnatal smoke exposure. Environmental smoke (in the same room) independently increases the risk of SIDS [89, 90]. Importantly, a recent study has shown that before discharge home from hospital, preterm infants of smoking mothers already exhibited disruptions in sleep patterns, prior to any postnatal smoke exposure [91]. Thus, there is considerable evidence from both animal and human studies suggesting that prenatal exposure to cigarette smoke has deleterious effects on the developing brain and cardiorespiratory system. It is suggested that these effects increase infant vulnerability to SIDS.
Maternal smoking may also be a confounding risk factor for SIDS due to its association with other risk factors, such as preterm birth and intrauterine growth restriction (IUGR) [92–95], which likely result from suboptimal intrauterine environments. Impaired heart rate control, manifest as shorter cardiac R-R intervals and higher resting sympathetic tone, has been reported in term-born IUGR infants when compared with infants of appropriate size for gestational age [96, 97]. Similarly, preterm infants demonstrated impaired autonomic control compared with term infants studied at or before term equivalent age, and this pattern was inversely related to gestational age at birth [98–103]. Longitudinal studies after term equivalent age have identified that preterm infants exhibited lower blood pressure, delayed blood pressure recovery following head-up tilting, and impaired baroreflex control of blood pressure and heart rate across the first 6 months corrected age, when compared with age-matched term infants [104–108]. Furthermore, maturation of baroreflex control of blood pressure during sleep is affected by gestational age at birth, with infants born very preterm (<32 weeks of gestation), having reduced increases in baroreflex sensitivity compared to both preterm and term infants [109]. Recently, studies have also identified that cerebral oxygenation is also lower in preterm compared to term infants across the first 6 months corrected age [110] and that cerebrovascular control after a head-up tilt is more variable [111], indicating immature or impaired control.
When compared with term infants at matched conceptional ages, preterm infants also exhibit decreased frequencies and durations of spontaneous arousals from sleep [112–114], together with decreased heart rate responses following arousal [115]. Furthermore, preterm infants exhibited longer arousal latencies after exposure to mild hypoxia (15 % inspired O2), reaching significantly lower oxygen saturations than term infants [116]. Cardiorespiratory complications commonly associated with prematurity, apnea, and bradycardia have also been shown to suppress total arousability when these infants were compared to preterm infants with no history of apnea [117].
In summary, these alterations in cardiorespiratory control and arousability during sleep support the classification of prenatal smoke exposure and preterm birth as factors strongly linked with the idea of a preexisting vulnerability to SIDS. Such physiological disturbances may be further exacerbated during a critical developmental period within infancy and by exposure to exogenous stressors.
Critical Developmental Period
Approximately 90 % of SIDS deaths occur in infants aged less than 6 months [45, 118]. During this period, the central nervous system undergoes dramatic maturational changes which are reflected in extensive alterations to sleep architecture, electroencephalogram characteristics, and autonomic control. The 2–4-month period, in particular, has been described as a “developmental window of vulnerability” [119, 120] and coincides with the age where a distinct peak in SIDS incidence occurs [45, 118].
A number of other significant developmental factors may make an infant more vulnerable to a cardiorespiratory challenge during this critical developmental period. Studies in both preterm [105, 110] and term [121] infants have identified a nadir in basal blood pressure during sleep at 2–4 months of age, when compared to both earlier (2–4 weeks) and later (5–6 months) ages studied; a nadir in physiological anemia also occurs at this age. Blood pressure responses to a cardiovascular challenge (head-up tilting) are also impaired at 2–4 months compared to younger (2–4 weeks) and older (5–6 months) ages [122]. The maturational reduction in cerebral oxygenation is most marked between 2–4 weeks and 2–4 months of age, which may be due to limited or inadequate flow-metabolism coupling at this age [123]. Thus, the 2–4-month age represents a critical time period when the effects of low blood pressure could accentuate decrements in oxygen-carrying capacity and delivery to critical organs [124]. These studies suggest that there is a postnatal age effect on cardiovascular control, with critical maturational changes occurring when the risk of SIDS is greatest.
Infant arousal responses from sleep are also affected by postnatal age, although these maturational effects are sleep state dependent. Previous studies have demonstrated that in response to respiratory (mild hypoxia), tactile (nasal air-jet), and auditory stimulation, total arousability is reduced with increasing age during quiet sleep while remaining unchanged in active sleep [124–126]. Following the introduction of standard scoring criteria for subcortical activation and cortical arousal as separate entities, a recent study noted that spontaneous subcortical activations decreased with increasing postnatal age, while cortical arousals increased [127]. Conversely, another study analyzed both spontaneous and nasal air-jet-induced arousability during supine sleep and found no change in the percentage of cortical arousals (from total responses) throughout the first 6 months of life [128]. Interestingly, when the same infants slept in the prone position, an increased propensity of cortical arousal was identified at 2–3 months, the age when SIDS is most common [87, 128]. This increase in cortical arousals may reflect an innate protective response to ensure an appropriate level of arousal for restoring homeostasis, not only during a vulnerable period of development but also in the presence of an exogenous stressor (e.g., the prone sleeping position).
Exogenous Stressor(s)
An exogenous stressor constitutes the third aspect of the triple-risk model for SIDS. Epidemiological studies have identified numerous factors common to SIDS victims, such as the prone sleeping position, overheating, and recent infection, which may disrupt homeostasis [45, 59, 129, 130].
The prone sleeping position has long been considered the major risk factor for SIDS [94, 131–134], with some studies suggesting a causal relation between prone sleep and SIDS [135, 136]. Several physiological changes ensue when infants sleep prone, including increased peripheral skin temperature and increased baseline heart rate, together with decreased heart rate variability [121, 137–145]. In an effort to identify changes in autonomic cardiovascular control with sleeping position, studies examining heart rate responses to auditory and nasal air-jet stimuli have suggested an increase in sympathetic and a decrease in parasympathetic tone in the prone sleeping position [146, 147]. Furthermore, sympathetic effects on blood pressure and vasomotor tone are decreased in the prone sleeping position. Lower resting blood pressure and altered cardiovascular responses to head-up tilting have also been identified in term infants when sleeping in the prone position, compared with the supine position [121, 122]. Furthermore, cerebral oxygenation is reduced and cerebrovascular control impaired in the prone position in both term [123, 148] and preterm infants [110, 149]. In addition, prone sleeping infants exhibit reduced cardiac and respiratory responses when arousing from sleep, when compared to sleeping in the supine position [146, 147]. Previous studies of both term and preterm infants have consistently identified increases in sleep time, with significant reductions in spontaneous arousability, associated with prone sleeping when compared with the supine position [150–153]. Furthermore, in other studies, the prone sleeping position depressed arousal responses provoked by postural change [137] and auditory [154] and somatosensory challenges [86, 138, 155]. It has been demonstrated that both spontaneous and induced arousal responses are similarly affected by sleep state and SIDS risk factors, suggesting that they are mediated through the same pathways [156]. Despite this well-documented decrease in total arousability, examining subcortical and cortical responses separately has produced conflicting results. Although one study reported a decreased frequency of spontaneous cortical arousals in the prone position [153], more recent studies have found an increased proportion of cortical arousals (of total responses) in both nonsmoking and smoking exposed infants when sleeping prone [87, 128]. This apparent promotion of full cortical arousal, demonstrated for both spontaneous and stimulus-induced responses, may protectively compensate against the threat of altered autonomic control and the already blunted total arousability imposed by the prone position.
The prone sleeping position also potentiates the risk of overheating, by reducing the exposed surface area available for radiant heat loss and reducing respiratory heat loss when the infants face is covered [157]. Both physiological studies in healthy infants and theoretical model studies of heat balance have observed a decreased ability to lose heat when in the prone position [158–160]. Early studies observed decreased variation in behavior and respiratory pattern, increased heart rate, and increased peripheral skin temperature during prone compared with supine sleep [159]. These studies suggest that infants are less able to maintain adequate respiratory and metabolic homoeostasis when sleeping prone.
Increased sweating occurs in SIDS victims, regardless of whether infants slept prone or supine; these cases were predominantly associated with a covered face [118, 161]. A history of profuse sweating in SIDS victims has been postulated to be a phenomenon representing an abnormality of function of the autonomic nervous system [162]. The involvement of thermal stress with SIDS is further supported by the finding of similar odds ratios for both too much and too little bedding [163] and the suggestion that future SIDS victims may have had atypical temperature regulation [164]. Infant arousability is also affected by body and room temperature; decreased sleep continuity and increased body movements have been associated with exposure to cooler temperatures [165], while infants sleeping in warmer environments (28 °C vs. 24 °C) exhibited increased arousal thresholds to auditory stimuli [166]. Furthermore, based on studies assessing blood pressure control in infants [139, 144], it has been suggested that in response to the increased peripheral skin temperature when infants sleep prone, thermoregulatory vasodilatation of the peripheral microvasculature occurs, resulting in a decrease in blood pressure and a reduction in vasomotor tone. Recent studies in preterm infants have shown that increased ambient temperature led to significant changes in autonomic control with elevated heart rates and lower heart rate variability compared to thermoneutral or cooler temperature [167].
Head covering has been identified as a major risk for SIDS with between 16 % and 28 % of SIDS infants found with their heads covered. Although a causal relationship with SIDS has not been established [168, 169], it appears likely that rebreathing and impaired arousal are involved. It has been suggested that the increased SIDS risk associated with head covering may result from hypoxia and hypercapnia via rebreathing of expired air [168, 170]. Head covering in healthy infants has profound effects on autonomic control during sleep [171]. Franco and colleagues [171] found that infants sleeping supine with their head covered by a bedsheet exhibited decreased parasympathetic activity, increased sympathetic activity, and increased body temperature when compared with head-free periods. In addition, arousal responses in active sleep were also depressed when the head was covered [172].
Bed-sharing or co-sleeping has also been reported to significantly increase the risk of SIDS, particularly when the mother smokes [118, 173–175] with more than 50 % of SIDS deaths occurring in this situation between 1997 and 2006 [176, 177]. There have been few studies investigating the physiology behind this risk factor. In infants from nonsmoking families who were studied on successive bed-sharing and solitary sleeping nights, bed-sharing was associated with increased awakenings and transient arousals during slow wave sleep compared to solitary nights [178]. In contrast, another study found that bed-sharing infants spent less time moving and were more likely to have their heads partially or fully covered by bedding than cot-sleeping infants [179]. Thus more studies are required to identify the exact physiological changes which occur during bed-sharing.
Other external stressors, such as infection, fever, and minor respiratory and gastrointestinal illnesses, commonly occur in the days to weeks preceding death of SIDS victims [180–182]. Although not identified as an independent risk factor for SIDS, minor infections have been associated with an increased likelihood of SIDS when combined with head covering or prone sleeping [183, 184]. In the prone sleeping position, minor infection, in combination with fever, could further exacerbate thermoregulatory effects on peripheral vasculature, which could increase the susceptibility of a hypotensive episode. Thus, hypotension, in combination with a decreased ability to arouse from sleep, which has been documented in term infants immediately following an infection [185], could potentially further impair an infant’s ability to appropriately respond to a life-threatening challenge such as circulatory failure or an asphyxial insult.
SIDS “Protective” Factors and Autonomic Control
Some studies have suggested that infant care practices, such as breastfeeding, dummy/pacifier use, and swaddling (tight wrapping), decrease the risk of SIDS. These potentially protective factors for SIDS have all been associated with alterations to both cardiovascular autonomic control and arousal responses during sleep. However, results are often inconsistent, and supporting evidence is less extensive than for the risk factors discussed above; thus, these potentially preventative factors remain controversial among researchers.
Breastfeeding
Breastfeeding reduces the incidence of SIDS by approximately half (OR 0.52, 95 % CI: 0.46–0.60), even after multivariate analyses accounted for potentially confounding socioeconomic factors [180, 186, 187]. This apparent protection may be a biological effect, given that breastfeeding has been associated with a decreased incidence of diarrhea, vomiting, colds, and other infections; in addition, breast milk is rich in antibodies and many micronutrients [180, 188, 189]. Only one study has assessed the effects of breastfeeding on the cardiovascular system during sleep in term infants, and this study found that heart rate was significantly lower in breast-fed infants when compared with formula-fed infants [190]. Although little is known about the effects of breastfeeding vs. formula feeding on cardiovascular control in infants, physiological studies have demonstrated an apparent promotion of arousal from sleep associated with breastfeeding. One study found that breast-fed infants spent more time awake during the night, thus requiring more frequent parental visits [191]. Another study showed that healthy breast-fed infants aroused more readily from active sleep than formula-fed infants in response to nasal air-jet stimulation at 2–3 months postnatal age [192]. Although there is a general consensus that breastfeeding should be encouraged, the relationship between breastfeeding for SIDS prevention remains unclear.
Pacifier/Dummy Use
The finding that the use of a dummy/pacifier has a protective effect for SIDS has consistently emerged from epidemiological studies, with significant associations being described for both usage during the final sleep and “dummy ever used” (OR: 0.46. CI 0.36–0.59) [118, 193–198]. Studies have suggested that a likely mechanism for this protection against SIDS is increased heart rate variability which has been demonstrated during sucking periods [199, 200]. Conversely, dummy sucking has also been shown to have no effect on heart rate, heart rate variability, respiratory frequency, or oxygen saturation in term infants [201, 202]. In addition, dummy sucking has been shown to elicit increases in blood pressure in quietly awake or sleeping term infants [203]. Another potential mechanism for the protective nature of dummy use against SIDS is an enhanced arousability from sleep. However, results of the few studies which have been conducted are conflicting, with one study reporting decreased arousal thresholds to auditory stimulation observed in infants who regularly used a dummy, when compared with those who did not use a dummy [204]. In contrast, other studies have reported no effect of dummy use on either the frequency or duration of spontaneous arousals in sleeping infants, when studied both with and without a dummy in the mouth [205, 206]. It has also been hypothesized that sucking on a dummy during sleep may assist in maintaining airway patency, thus preventing a pharyngeal vacuum and the consequent sealing of the airway [207, 208]. Thus, the risk of oropharyngeal obstruction may be reduced due to the forward positioning of the tongue when sucking on a dummy [208]. Although epidemiological studies have provided strong support for dummy use to be protective for SIDS, the physiological mechanisms responsible for this protection remain uncertain.
Swaddling
Swaddling, or firm wrapping, is a traditional infant care practice which, according to an extensive historical review, has been used in some form or another by various cultures since medieval times [209]. Low incidences of SIDS in populations where swaddling is common have led to the proposal that swaddling may be protective [210, 211], and on this basis, a number of SIDS prevention organizations recommend it. Several studies have documented a “tranquil” behavioral state with longer sleep periods in swaddled infants; therefore, despite a disparity between studies on the risk for SIDS [174, 183, 212], swaddling has become increasingly popular as a soothing technique throughout the world [213, 214]. Swaddling is a common practice in infants throughout the first 6 months of life, during the period of increased SIDS risk. The duration of swaddling and the age of initiation of the practice vary widely. Currently, it is unclear if swaddling is protective against SIDS or is indeed a risk. In the United Kingdom during the mid-1990s, swaddling during the last sleep was more common among SIDS infants than age-matched controls (14 % vs. 9 %); furthermore, a more recent study showed that this difference has since become more marked (19 % vs. 6 %) [174].
Studies investigating the effect of swaddling on cardiovascular control are limited. Swaddling elicits a mild increase in respiratory frequency, most likely due to restricted tidal volumes imposed by the firm wrapping [215–217]. No significant effects have been documented on baseline heart rate, skin temperature, or oxygen saturation in term infants when swaddled during sleep [216, 218]. Studies which compared infants who were routinely swaddled to those who were unused to this practice found that sleep time and heart rate variability were only altered in those naïve-to-swaddling infants [219]. Several studies investigated the effects of swaddling in relation to infant arousability; however, divergent results have been published. The commonly observed decreases in spontaneous movements and startle responses with swaddling are in contrast to effects of other protective factors for SIDS [209, 220]. One study reported that when infants were swaddled, fewer startle responses progressed to a full awakening, indicating an inhibition of the cortical arousal process [221]. More recent studies reported that swaddled infants exhibited increased arousal thresholds in response to nasal air-jet stimulation; furthermore, a decreased frequency of full cortical arousals was observed primarily in infants who were unaccustomed to being swaddled, at 3 months of age [216]. Spontaneous cortical arousals were also decreased in those infants unaccustomed to being swaddled, at 3 months of age [219]. These arousal differences between routinely swaddled and naïve-to-swaddling infants, only at this age of peak SIDS risk, may explain the contradictory findings of another group which found decreased auditory arousal thresholds in swaddled infants when compared to infants who were free to move [218]. The authors attributed these effects of swaddling on arousal to the greater autonomic changes found after auditory stimulation in swaddled conditions [222]. As with the other protective factors discussed above, the mechanisms whereby swaddling is protective for SIDS remain unclear, and further research is required.
Conclusions
In summary, the assessment of cardiovascular control and arousal processes during sleep is important in understanding sleep-related pathologies such as SIDS. In otherwise healthy infants, studies have demonstrated impairment of these physiological mechanisms in association with all three aspects of the triple-risk model, thus demonstrating the heterogeneous nature of SIDS. Altered cardiovascular and cerebrovascular control, in conjunction with a failure to arouse from sleep, could potentially impair an infant’s ability to appropriately compensate for life-threatening challenges, such as prolonged hypotension or asphyxia during sleep. The concept of a close relationship between SIDS and autonomic dysfunction becomes more compelling with the demonstration of an apparent promotion of arousal from sleep by protective factors for SIDS. Despite successful public awareness campaigns dramatically reducing SIDS rates, this decline in SIDS incidence may have stabilized [223–226]. Thus, further research is imperative to elucidate the exact mechanisms involved in the final events of SIDS, allowing identification of “at-risk” infants in the future. The ability to identify these infants would have the potential to increase awareness of both parents and clinicians while minimizing the incidence of SIDS with close monitoring and early intervention.
References
Gaultier C. Cardiorespiratory adaptation during sleep in infants and children. Pediatr Pulmonol. 1995;19:105–17.
Prechtl HF. The behavioural states of the newborn infant (a review). Brain Res. 1974;76:185–212.
Curzi-Dascalova L, Challamel M-J. Neurophysiological basis of sleep development. In: Loughlin GM, Carroll JL, Marcus CL, editors. Sleep and breathing in children: a developmental approach. New York: Marcel Dekker; 2000.
Parmelee AH, Stern E. Development of states in infants. In: Clemente CD, Purpura DP, Mayer FE, editors. Sleep and the maturing nervous system. Academic Press New York. 1972;199–228.
Dreyfus-Brisac C. Sleep ontogenesis in early human prematurity from 24 to 27 weeks conceptual age. Dev Psychobiol. 1968;1:162–9.
de Weerd AW, van den Bossche RA. The development of sleep during the first months of life. Sleep Med Rev. 2003;7:179–91.
Coons SC, Guilleminault C. Development of sleep-wake patterns and non-rapid eye movement sleep stages during the first six months of life in normal infants. Pediatrics. 1982;69:793–8.
Coons S. Development of sleep and wakefulness during the first 6 months of life. New York: Raven Press; 1987.
Curzi-Dascalova L, Mirmiran M. Manual of methods for recording and analysing sleep-wakefulness states in preterm and full term infants. Paris: Les Edition INSERM; 1996.
Metcalf D. The ontogenesis of sleep-awake states from birth to 3 months. Electroencephalogr Clin Neurophysiol. 1970;28:421.
Grigg-Damberger M, Gozal D, Marcus CL, Quan SF, Rosen CL, Chervin RD, Wise M, Picchietti DL, Sheldon SH, Iber C. The visual scoring of sleep and arousal in infants and children. J Clin Sleep Med. 2007;3:201–40.
National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring, Sept 29 to Oct 1, 1986. Pediatrics. 1987;79:292–9.
Henderson-Smart D. The effect of gestational age on the incidence and duration of recurrent apnoea in newborn babies. Aust Paediatr J. 1981;17:273–6.
Picone S, Bedetta M, Paolillo P. Caffeine citrate: when and for how long. A literature review. J Matern Fetal Neonatal Med. 2012;25 Suppl 3:11–4.
Martin RJ, di Fiore JM, Macfarlane PM, Wilson CG. Physiologic basis for intermittent hypoxic episodes in preterm infants. Adv Exp Med Biol. 2012;758:351–8.
di Fiore JM, Bloom JN, Orge F, Schutt A, Schluchter M, Cheruvu VK, Walsh M, Finer N, Martin RJ. A higher incidence of intermittent hypoxemic episodes is associated with severe retinopathy of prematurity. J Pediatr. 2010;157:69–73.
Elder DE, Whale J, Galletly D, Campbell AJ. Respiratory events in preterm infants prior to discharge: with and without clinically concerning apnoea. Sleep Breath. 2011;15:867–73.
Pillekamp F, Hermann C, Keller T, von Gontard A, Kribs A, Roth B. Factors influencing apnea and bradycardia of prematurity – implications for neurodevelopment. Neonatology. 2007;91:155–61.
Soukhova-O’Hare GK, Cheng ZJ, Roberts AM, Gozal D. Postnatal intermittent hypoxia alters baroreflex function in adult rats. Am J Physiol Heart Circ Physiol. 2006;290:H1157–64.
Cohen G, Lagercrantz H, Katz-Salamon M. Abnormal circulatory stress responses of preterm graduates. Pediatr Res. 2007;61:329–34.
Al-Saif S, Alvaro R, Manfreda J, Kwiatkowski K, Cates D, Qurashi M, Rigatto H. A randomized controlled trial of theophylline versus CO2 inhalation for treating apnea of prematurity. J Pediatr. 2008;153:513–8.
Henderson-Smart DJ, Steer P. Methylxanthine treatment for apnea in preterm infants. Cochrane Database Syst Rev. 2001;(3):CD000140.
McCall AL, Millington WR, Wurtman RJ. Blood-brain barrier transport of caffeine: dose-related restriction of adenine transport. Life Sci. 1982;31:2709–15.
Montandon G, Kinkead R, Bairam A. Adenosinergic modulation of respiratory activity: developmental plasticity induced by perinatal caffeine administration. Respir Physiol Neurobiol. 2008;164:87–95.
Chardon K, Bach V, Telliez F, Cardot V, Tourneux P, Leke A, Libert JP. Effect of caffeine on peripheral chemoreceptor activity in premature neonates: interaction with sleep stages. J Appl Physiol. 2004;96:2161–6.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, Solimano A, Tin W. Caffeine therapy for apnea of prematurity. NEJM. 2006;354:2112–21.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, Solimano A, Tin W. Long-term effects of caffeine therapy for apnea of prematurity. NEJM. 2007;357:1893–902.
Doyle LW, Cheong J, Hunt RW, Lee KJ, Thompson DK, Davis PG, Rees S, Anderson PJ, Inder TE. Caffeine and brain development in very preterm infants. Ann Neurol. 2010;68:734–42.
Schmidt B, Anderson PJ, Doyle LW, Dewey D, Grunau RE, Asztalos EV, Davis PG, Tin W, Moddemann D, Solimano A, Ohlsson A, Barrington KJ, Roberts RS. Survival without disability to age 5 years after neonatal caffeine therapy for apnea of prematurity. JAMA. 2012;307:275–82.
Kelly DH, Stellwagen LM, Kaitz E, Shannon DC. Apnea and periodic breathing in normal full-term infants during the first twelve months. Pediatr Pulmonol. 1985;1:215–9.
Brockmann PE, Poets A, Poets CF. Reference values for respiratory events in overnight polygraphy from infants aged 1 and 3months. Sleep Med. 2013;14:1323–7.
Albani M, Bentele KH, Budde C, Schulte FJ. Infant sleep apnea profile: preterm vs. term infants. Eur J Pediatr. 1985;143:261–8.
Edwards BA, Sands SA, Berger PJ. Postnatal maturation of breathing stability and loop gain: the role of carotid chemoreceptor development. Respir Physiol Neurobiol. 2013;185:144–55.
Decima PF, Fyfe KL, Odoi A, Wong FY, Horne RS. The longitudinal effects of persistent periodic breathing on cerebral oxygenation in preterm infants. Sleep Med. 2015;16:729–35.
Carskadon MA, Harvey K, Dement WC, Guilleminault C, Simmons FB, Anders TF. Respiration during sleep in children. West J Med. 1978;128:477–81.
Marcus CL, Omlin KJ, Basinki DJ, Bailey SL, Rachal AB, von Pechmann WS, Keens TG, Ward SL. Normal polysomnographic values for children and adolescents. Am Rev Respir Dis. 1992;146:1235–9.
Kato I, Scaillet S, Groswasser J, Montemitro E, Togari H, Lin J, Kahn A, Franco P. Spontaneous arousability in prone and supine position in healthy infants. Sleep. 2006;29:785–90.
Gislason T, Benediktsdottir B. Snoring, apneic episodes, and nocturnal hypoxemia among children 6 months to 6 years old. An epidemiologic study of lower limit of prevalence. Chest. 1995;107:963–6.
Kelmanson IA. Snoring, noisy breathing in sleep and daytime behaviour in 2-4-month-old infants. Eur J Pediatr. 2000;159:734–9.
Mitchell EA, Thompson JM. Snoring in the first year of life. Acta Paediatr. 2003;92:425–9.
Montgomery-Downs HE, Gozal D. Sleep habits and risk factors for sleep-disordered breathing in infants and young toddlers in Louisville, Kentucky. Sleep Med. 2006;7:211–9.
Piteo AM, Lushington K, Roberts RM, van den Heuvel CJ, Nettelbeck T, Kohler MJ, Martin AJ, Kennedy JD. Prevalence of snoring and associated factors in infancy. Sleep Med. 2011;12:787–92.
Piteo AM, Kennedy JD, Roberts RM, Martin AJ, Nettelbeck T, Kohler MJ, Lushington K. Snoring and cognitive development in infancy. Sleep Med. 2011;12:981–7.
Krous HF, Beckwith JB, Byard RW, Rognum TO, Bajanowski T, Corey T, Cutz E, Hanzlick R, Keens TG, Mitchell EA, Krous HF, Beckwith JB, Byard RW, Rognum TO, Bajanowski T, Corey T, Cutz E, Hanzlick R, Keens TG, Mitchell EA. Sudden infant death syndrome and unclassified sudden infant deaths: a definitional and diagnostic approach. Pediatrics. 2004;114:234–8.
Moon RY, Horne RS, Hauck FR. Sudden infant death syndrome. Lancet. 2007;370:1578–87.
Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber J, Jorch G, Schreuder P. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363:185–91.
Byard RW, Krous HF. Sudden infant death syndrome: overview and update. Pediatr Dev Pathol. 2003;6:112–27.
Filiano JJ, Kinney H. A perspective on neuropathologic findings in victims of the sudden infant death syndrome: the triple risk model. Biol Neonate. 1994;65:194–7.
Horne RS, Witcombe NB, Yiallourou SR, Scaillet S, Thiriez G, Franco P. Cardiovascular control during sleep in infants: implications for sudden infant death syndrome. Sleep Med. 2010;11:615–21.
Franco P, Kato I, Richardson HL, Yang JS, Montemitro E, Horne RS. Arousal from sleep mechanisms in infants. Sleep Med. 2010;11:603–14.
Paterson DS, Trachtenberg FL, Thompson EG, Belliveau RA, Beggs AH, Darnall BA, Chadwick AE, Krous HF, Kinney HC. Multiple serotonergic brainstem abnormalities in sudden infant death syndrome. JAMA. 2006;286:2124–32.
Kinney HC, Cryan JB, Haynes RL, Paterson DS, Haas EA, Mena OJ, Minter M, Journey KW, Trachtenberg FL, Goldstein RD, Armstrong DD. Dentate gyrus abnormalities in sudden unexplained death in infants: morphological marker of underlying brain vulnerability. Acta Neuropathol. 2015;129:65–80.
Kinney HC, Filiano JJ, Sleeper LA, Mandell F, Valdes-Dapena M, White WF. Decreased muscarinic receptor binding in the arcuate nucleus in sudden infant death syndrome. Science. 1995;269:1446–50.
Panigrahy A, Filiano J, Sleeper LA, Mandell F, Valdes-Dapena M, Krous HF, Rava LA, Foley E, White WF, Kinney HC. Decreased serotonergic receptor binding in rhombic lip-derived regions of the medulla oblongata in the sudden infant death syndrome. J Neuropathol Exp Neurol. 2000;59:377–84.
Panigrahy A, Filiano JJ, Sleeper LA, Mandell F, Valdes-Dapena M, Krous HF, Rava LA, White WF, Kinney HC. Decreased kainate receptor binding in the arcuate nucleus of the sudden infant death syndrome. J Neuropathol Exp Neurol. 1997;56:1253–61.
Machaalani R, Say M, Waters KA. Serotinergic receptor 1A in the sudden infant death syndrome brainstem medulla and associations with clinical risk factors. Acta Neuropathol. 2009;117:257–65.
Machaalani R, Waters KA. Neuronal cell death in the sudden infant death syndrome brainstem and associations with risk factors. Brain. 2008;131:218–28.
Machaalani R, Waters KA. Neurochemical abnormalities in the brainstem of the Sudden Infant Death Syndrome (SIDS). Paediatr Respir Rev. 2014;15:293–300.
Kinney HC, Thach BT. The sudden infant death syndrome. N Engl J Med. 2009;361:795–805.
Lavezzi AM, Casale V, Oneda R, Weese-Mayer DE, Matturri L. Sudden infant death syndrome and sudden intrauterine unexplained death: correlation between hypoplasia of raphe nuclei and serotonin transporter gene promoter polymorphism. Pediatr Res. 2009;66:22–7.
Weese-Mayer DE, Ackerman MJ, Marazita ML, Berry-Kravis EM. Sudden infant death syndrome: review of implicated genetic factors. Am J Med Genet. 2007;143A:771–88.
Filonzi L, Magnani C, Lavezzi AM, Rindi G, Parmigiani S, Bevilacqua G, Matturri L, Marzano FN. Association of dopamine transporter and monoamine oxidase molecular polymorphisms with sudden infant death syndrome and stillbirth: new insights into the serotonin hypothesis. Neurogenetics. 2009;10:65–72.
Courts C, Madea B. Genetics of the sudden infant death syndrome. Forensic Sci Int. 2010;203:25–33.
Mitchell E, Scragg R, Stewart AW, Becroft DMO, Taylor B, Ford RPK, Hassell B, Barry DMJ, Allen EM, Roberts AP. Results from the first year of the New Zealand cot death study. NZ Med J. 1991;104:71–6.
Matturri L, Ottaviani G, Lavezzi AM. Maternal smoking and sudden infant death syndrome: epidemiological study related to pathology. Virchows Arch. 2006;449:697–706.
Anderson HR, Cook DG. Passive smoking and sudden infant death syndrome: review of the epidemiological evidence. Thorax. 1997;52:1003–9.
Blair PS, Bensley D, Smith I, Bacon C, Taylor B, Berry J. Smoking and the sudden infant death syndrome: results from 1993–5 case-control study for confidential inquiry into stillbirths and deaths in infancy. BMJ. 1996;313:195–8.
Dwyer T, Ponsonby A, Couper D. Tobacco smoke exposure at one month of age and subsequent risk of SIDS – a prospective study. Am J Epidemiol. 1999;149:593–602.
Haglund B. Cigarette smoking and sudden infant death syndrome: some salient points in the debate. Acta Paediatr Suppl. 1993;389:37–9.
Machaalani R, Ghazavi E, Hinton T, Waters KA, Hennessy A. Cigarette smoking during pregnancy regulates the expression of specific nicotinic acetylcholine receptor (nAChR) subunits in the human placenta. Toxicol Appl Pharmacol. 2014;276:204–12.
Machaalani R, Say M, Waters KA. Effects of cigarette smoke exposure on nicotinic acetylcholine receptor subunits alpha7 and beta2 in the sudden infant death syndrome (SIDS) brainstem. Toxicol Appl Pharmacol. 2011;257:396–404.
Lavezzi AM, Mecchia D, Matturri L. Neuropathology of the area postrema in sudden intrauterine and infant death syndromes related to tobacco smoke exposure. Auton Neurosci. 2012;166:29–34.
Duncan JR, Garland M, Myers MM, Fifer WP, Yang M, Kinney HC, Stark RI. Prenatal nicotine-exposure alters fetal autonomic activity and medullary neurotransmitter receptors: implications for sudden infant death syndrome. J Appl Physiol. 2009;107:1579–90.
Browne CA, Colditz PB, Dunster KR. Infant autonomic function is altered by maternal smoking during pregnancy. Early Hum Dev. 2000;59:209–18.
Dahlstrom A, Ebersjo C, Lundell B. Nicotine in breast milk influences heart rate variability in the infant. Acta Paediatr. 2008;97:1075–9.
Fifer WP, Fingers ST, Youngman M, Gomez-Gribben E, Myers MM. Effects of alcohol and smoking during pregnancy on infant autonomic control. Dev Psychobiol. 2009;51:234–42.
Cohen G, Vella S, Jeffery H, Lagercrantz H, Katz-Salamon M. Cardiovascular stress hyperreactivity in babies of smokers and in babies born preterm. Circulation. 2008;118:1848–53.
Thiriez G, Bouhaddi M, Mourot L, Nobili F, Fortrat JO, Menget A, Franco P, Rednard J. Heart rate variability in preterm infants and maternal smoking during pregnancy. Clin Auton Res. 2009;19:149–56.
Viskari-Lahdeoja S, Hytinantti T, Andersson S, Kirjavainen T. Heart rate and blood pressure control in infants exposed to maternal cigarette smoking. Acta Paediatr. 2008;97:1535–41.
Franco P, Chabanski S, Szliwowski H, Dramaix M, Kahn A. Influence of maternal smoking on autonomic nervous system in healthy infants. Pediatr Res. 2000;47:215–20.
Sawnani H, Jackson T, Murphy T, Beckerman R, Simakajornboon N. The effect of maternal smoking on respiratory and arousal patterns in preterm infants during sleep. Am J Respir Crit Care Med. 2004;169:733–8.
Tirosh E, Libon D, Bader D. The effect of maternal smoking during pregnancy on sleep respiratory and arousal patterns in neonates. J Perinatol. 1996;16:435–138.
Franco P, Groswasser J, Hassid S, Lanquart J, Scaillet S, Kahn A. Prenatal exposure to cigarette smoking is associated with a decrease in arousal in infants. J Pediatr. 1999;135:34–8.
Chang AB, Wilson SJ, Masters IB, Yuill M, Williams G, Hubbard M. Altered arousal response in infants exposed to cigarette smoke. Arch Dis Child. 2003;88:30–3.
Lewis KW, Bosque EM. Deficient hypoxia awakening response in infants of smoking mothers: possible relationship to sudden infant death syndrome. J Pediatr. 1995;127:691–9.
Horne RSC, Ferens D, Watts A-M, Vitkovic J, Andrew S, Cranage SM, Chau B, Greaves R, Adamson TM. Effects of maternal tobacco smoking, sleeping position and sleep state on arousal in healthy term infants. Arch Dis Child Fetal Neonatal Ed. 2002;87:F100–5.
Richardson HL, Walker AM, Horne RSC. Maternal smoking impairs arousal patterns in sleeping infants. Sleep. 2009;32:515–21.
Johansson A, Halling A, Hermansson G. Indoor and outdoor smoking. Impact on children’s health. Eur J Public Health. 2003;13:61–6.
Schoendorf KC, Kiely JL. Relationship of sudden infant death syndrome to maternal smoking during and after pregnancy. Pediatrics. 1992;90:905–8.
Klonoff-Cohen HS, Edelstein SL, Lefkowitz ES, Srinivasan IP, Kaegi D, Chang JC, Wiley KJ. The effect of passive smoking and tobacco exposure through breast milk on sudden infant death syndrome. JAMA. 1995;273:795–8.
Stephan-Blanchard E, Telliez F, Leke A, Djeddi D, Bach V, Libert J, Chardon K. The influence of in utero exposure to smoking on sleep patterns in preterm neonates. Sleep. 2008;31:1683–9.
Andriessen P, Koolen AMP, Berendsen RCM, Wijn PFF, ten Broeke EDM, Oei SG, Blanco CE. Cardiovascular fluctuations and transfer function analysis in stable preterm infants. Pediatr Res. 2003;53:89–97.
Mitchell EA, Ford RPK, Stewart AW, Taylor BJ, Becroft DMO, Thompson JMD, Scragg R, Hassell IB, Barry DM, Allen EM, Roberts AP. Smoking and the sudden infant death syndrome. Pediatrics. 1993;91:893–6.
Brooke H, Gibson A, Tappin D, Brown H. Case control study of sudden infant death syndrome in Scotland, 1992–5. BMJ. 1997;314:1516–20.
Schellscheidt J, Oyen N, Jorch G. Interactions between maternal smoking and other perinatal risk factors for SIDS. Acta Paediatr. 1997;86:857–63.
Galland BC, Taylor B, Bolton DPG, Sayers RM. Heart rate variability and cardiac reflexes in small for gestational age infants. J Appl Physiol. 2006;100:933–9.
Spassov L, Curzi-Dascalova L, Clairambault J, Kauffmann F, Eiselt M, Medigue C, Periano P. Heart rate and heart rate variability during sleep in small-for-gestational age newborns. Pediatr Res. 1994;35:500–5.
Katona PG, Frasz A, Egbert J. Maturation of cardiac control in full-term and preterm infants during sleep. Early Hum Dev. 1980;4:145–59.
Eiselt M, Curzi-Dascalova L, Clairambault J, Kauffmann F, Medigue C, Peirano P. Heart rate variability in low-risk prematurely born infants reaching normal term: a comparison with full-term newborns. Early Hum Dev. 1993;32:183–95.
Eiselt M, Zwiener U, Witte H, Curzi-Dascalova L. Influence of prematurity and extrauterine development on the sleep state dependant heart rate patterns. Somnologie. 2002;6:116–23.
Patural H, Barthelemy JC, Pichot V, Mazzocchi C, Teyssier G, Damon G, Roche F. Birth prematurity determines prolonged autonomic nervous system immaturity. Clin Auton Res. 2004;14:391–5.
Patural H, Pichot V, Jaziri F, Teyssier G, Gaspoz JM, Roche F, Barthelemy JC. Autonomic cardiac control of very preterm newborns: a prolonged dysfunction. Early Hum Dev. 2008;84:681–7.
Longin E, Gerstner T, Schaible T, Lanz T, Konig S. Maturation of the autonomic nervous system: differences in heart rate variability in premature vs. term infants. J Perinat Med. 2006;34:303–8.
Witcombe NB, Yiallourou SR, Walker AM, Horne RSC. Delayed blood pressure recovery after head-up tilting during sleep in preterm infants. J Sleep Res. 2010;19:93–102.
Witcombe NB, Yiallourou SR, Walker AM, Horne RSC. Blood pressure and heart rate patterns during sleep are altered in preterm-born infants: implications for sudden infant death syndrome. Pediatrics. 2008;122:1242–8.
Witcombe NB, Yiallourou SR, Sands SA, Walker AM, Horne RS. Preterm birth alters the maturation of baroreflex sensitivity in sleeping infants. Pediatrics. 2012;129:e89–96.
Fyfe KL, Yiallourou SR, Wong FY, Odoi A, Walker AM, Horne RS. The effect of gestational age at birth on post-term maturation of heart rate variability. Sleep. 2015;38:1635.
Yiallourou SR, Witcombe NB, Sands SA, Walker AM, Horne RS. The development of autonomic cardiovascular control is altered by preterm birth. Early Hum Dev. 2013;89:145–52.
Fyfe KL, Yiallourou SR, Wong FY, Odoi A, Walker AM, Horne RS. Gestational age at birth affects maturation of baroreflex control. J Pediatr. 2015;166:559–65.
Fyfe KL, Yiallourou SR, Wong FY, Odoi A, Walker AM, Horne RS. Cerebral oxygenation in preterm infants. Pediatrics. 2014;134:435–45.
Fyfe K, Odoi A, Yiallourou SR, Wong F, Walker AM, Horne RS. Preterm infants exhibit greater variability in cerebrovascular control than term infants. Sleep. 2015;38:1411.
Horne RSC, Cranage SM, Chau B, Adamson TM. Effects of prematurity on arousal from sleep in the newborn infant. Pediatr Res. 2000;47:468–74.
Scher MS, Steppe DA, Dahl RE, Asthana S, Guthrie RD. Comparison of EEG sleep measures in healthy full-term and preterm infants at matched conceptional ages. Sleep. 1992;15:442–8.
Richardson HL, Horne RS. Arousal from sleep pathways are affected by the prone sleeping position and preterm birth: preterm birth, prone sleeping and arousal from sleep. Early Hum Dev. 2013;89:705–11.
Tuladhar R, Harding R, Adamson TM, Horne RSC. Comparison of postnatal development of heart rate responses to trigeminal stimulation in sleeping preterm and term infants. J Sleep Res. 2005;14:29–36.
Verbeek MMA, Richardson HL, Parslow PM, Walker AM, Harding R, Horne RSC. Arousal and ventilatory responses to mild hypoxia in sleeping preterm infants. J Sleep Res. 2008;17:344–53.
Horne RSC, Andrew S, Mitchell K, Sly DJ, Cranage SM, Chau B, Adamson TM. Apnoea of prematurity and arousal from sleep. Early Hum Dev. 2001;61:119–33.
Carpenter RG, Irgens LM, Blair PS, Fleming PJ, Huber J, Jorch G, Schreuder P. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363:185–91.
Kohyama J. Sleep as a window on the developing brain. Curr Probl Pediatr. 1998;28:69–92.
Carroll JL. Developmental plasticity in respiratory control. J Appl Physiol. 2003;94:375–89.
Yiallourou SR, Walker AM, Horne RSC. Effects of sleeping position on development of infant cardiovascular control. Arch Dis Child. 2008;93:868–72.
Yiallourou SR, Walker AM, Horne RSC. Prone sleeping impairs circulatory control during sleep in healthy term infants; implications for sudden infant death syndrome. Sleep. 2008;31:1139–46.
Wong FY, Witcombe NB, Yiallourou SR, Yorkston S, Dymowski AR, Krishnan L, Walker AM, Horne RS. Cerebral oxygenation is depressed during sleep in healthy term infants when they sleep prone. Pediatrics. 2011;127:e558–65.
Parslow PM, Harding R, Cranage SM, Adamson TM, Horne RSC. Ventilatory responses preceding hypoxia-induced arousal in infants: effects of sleep-state. Respir Physiol Neurobiol. 2003;136:235–47.
Trinder J, Newman NM, Le Grande M, Whitworth F, Kay A, Pirkis J, Jordan K. Behavioural and EEG responses to auditory stimuli during sleep in newborn infants and in infants aged 3 months. Biol Psychol. 1990;90:213–27.
Parslow PM, Harding R, Cranage SM, Adamson TM, Horne RSC. Arousal responses to somatosensory and mild hypoxic stimuli are depressed during quiet sleep in healthy term infants. Sleep. 2003;26:739–44.
Montemitro E, Franco P, Scaillet S, Kato I, Groswasser J, Villa MP, Kahn A, Sastre J, Ecochard R, Thiriez G, Lin J. Maturation of spontaneous arousals in healthy infants. Sleep. 2008;31:47–54.
Richardson HL, Walker AM, Horne RSC. Sleep position alters arousal processes maximally at the high-risk age for sudden infant death syndrome. J Sleep Res. 2008;17:450–7.
Blackwell C, Moscovis S, Hall S, Burns C, Scott RJ. Exploring the risk factors for sudden infant deaths and their role in inflammatory responses to infection. Front Immunol. 2015;6:44.
Galland BC, Elder DE. Sudden unexpected death in infancy: biological mechanisms. Paediatr Respir Rev. 2014;15:287–92.
Oyen H, Markstead T, Skjaerven R, Irgens LM, Helweg-Larsen K, Alm B, Norvenius G, Wennergren G. Combined effects of sleeping position and the perinatal risk factors in sudden infant death syndrome: the Nordic epidemiological study. Pediatrics. 1997;100:613–21.
Mitchell EA. Sleeping position of infants and the sudden infant death syndrome. Acta Paediatr. 1993;389:26–30.
Ponsonby AL, Dwyer T. The Tasmanian SIDS case-control study: univariate and multivariate risk factor analysis. Paediatr Perinat Epidemiol. 1995;9:256–72.
Taylor JA, Krieger JW, Reay DT, David RL, Harruff R, Cheney LK. Prone sleeping position and sudden infant death syndrome in King County, Washington: a case control study. Pediatrics. 1996;128:626–30.
Beal SM, Finch CF. An overview of retrospective case-control studies investigating the relationship between prone sleeping position and SIDS. J Paediatr Child Health. 1991;27:334–9.
Fleming PJ, Gilbert R, Azaz Y, Berry PJ, Rudd PT, Stewart A, Hall E. Interaction between bedding and sleeping position in the sudden infant death syndrome: a population based case-control study. BMJ. 1990;301:85–9.
Galland BC, Reeves H, Taylor B, Bolton DPG. Sleep position, autonomic function, and arousal. Arch Dis Child Fetal Neonatal Ed. 1998;78:189–94.
Horne R, Ferens D, Watts A, Vitkovic J, Lacey B, Andrew S, Cranage S, Chau B, Adamson T. The prone sleeping position impairs arousability in term infants. J Pediatr. 2001;138:811–6.
Galland B, Taylor B, Bolton D, Sayers R. Vasoconstriction following spontaneous sighs and head-up tilts in infants sleeping prone and supine. Early Hum Dev. 2000;58:119–32.
Ariagno RL, Mirmiran M, Adams MM, Saporito AG, Dubin AM, Baldwin RB. Effect of position on sleep, heart rate variability, and QT interval in preterm infants at 1 and 3 months’ corrected age. Pediatrics. 2003;111:622–5.
Sahni R, Schulz H, Kashyap S, Ohira-Kist K, Fifer WP, Myers MM. Postural differences in cardiac dynamics during quiet and active sleep in low birthweight infants. Acta Paediatr. 1999;88:1396–401.
Gabai N, Cohen A, Mahagney A, Bader D, Tirosh E. Arterial blood flow and autonomic function in full-term infants. Clin Physiol Funct Imaging. 2006;26:127–31.
Kahn A, Grosswasser J, Sottiaux M, Rebuffat E, Franco P, Dramaix M. Prone or supine body position and sleep characteristics in infants. Pediatrics. 1993;91:1112–5.
Chong A, Murphy N, Matthews T. Effect of prone sleeping on circulatory control in infants. Arch Dis Child. 2000;82:253–6.
Ammari A, Schulze KF, Ohira-Kist K, Kashyap S, Fifer WP, Myers MM, Sahni R. Effects of body position on thermal, cardiorespiratory and metabolic activity in low birth weight infants. Early Hum Dev. 2009;85:497–501.
Franco P, Grosswasser J, Sottiaux M, Broadfield E, Kahn A. Decreased cardiac responses to auditory stimulation during prone sleep. Pediatrics. 1996;97:174–8.
Tuladhar R, Harding R, Cranage SM, Adamson TM, Horne RSC. Effects of sleep position, sleep state and age on heart rate responses following provoked arousal in term infants. Early Hum Dev. 2003;71:157–69.
Wong F, Yiallourou SR, Odoi A, Browne P, Walker AM, Horne RS. Cerebrovascular control is altered in healthy term infants when they sleep prone. Sleep. 2013;36:1911–8.
Fyfe KL, Yiallourou SR, Wong FY, Horne RS. The development of cardiovascular and cerebral vascular control in preterm infants. Sleep Med Rev. 2014;18:299–310.
Ariagno R, van Liempt S, Mirmiran M. Fewer spontaneous arousals during prone sleep in preterm infants at 1 and 3 months corrected age. J Perinatol. 2006;26:306–12.
Goto K, Maeda T, Mirmiran M, Ariagno R. Effects of prone and supine position on sleep characteristics in preterm infants. Psychiatry Clin Neurosci. 1999;53:315–7.
Bhat RY, Hannam S, Pressler R, Rafferty GF, Peacock JL, Greenough A. Effect of prone and supine position on sleep, apneas, and arousal in preterm infants. Pediatrics. 2006;118:101–7.
Kato I, Franco P, Groswasser J, Kelmanson I, Togari H, Kahn A. Frequency of obstructive and mixed sleep apneas in 1,023 infants. Sleep. 2000;23:487–92.
Franco P, Pardou A, Hassid S, Lurquin P, Groswasser J, Kahn A. Auditory arousal thresholds are higher when infants sleep in the prone position. J Pediatr. 1998;132:240–3.
Horne RSC, Bandopadhayay P, Vitkovic J, Cranage SM, Adamson TM. Effects of age and sleeping position on arousal from sleep in preterm infants. Sleep. 2002;25:746–50.
Richardson HL, Walker AM, Horne R. Stimulus type does not affect infant arousal response patterns. J Sleep Res. 2010;19:111–5.
Ponsonby A, Dwyer T, Gibbons LE, Cochrane JA, Jones ME, McCall MJ. Thermal environment and sudden infant death syndrome: case-control study. BMJ. 1992;304:279–91.
Tuffnell CS, Peterson SA, Wailoo MP. Prone sleeping infants have a reduced ability to lose heat. Early Hum Dev. 1995;43:109–16.
Skadberg BT, Markstead T. Behaviour and physiological responses during prone and supine sleep in early infancy. Arch Dis Child. 1997;76:320–4.
Bolton DPG, Nelson EAS, Taylor BJ, Weatherall IL. Thermal balance in infants. J Appl Physiol. 1996;80:2234–42.
L’Hoir MP, Engelberts AC, van Well GTJ, McClelland S, Westers P, Dandachli T, Mellenbergh GJ, Wolters WHG, Huber J. Risk and preventive factors for cot death in The Netherlands, a low-incidence country. Eur J Pediatr. 1998;157:681–8.
Kahn A, Wachholder A, Winkler M, Rebuffat E. Prospective study on the prevalence of sudden infant death and possible risk factors in Brussels: preliminary results (1987–1988). Eur J Pediatr. 1990;149:284–6.
Williams SM, Taylor BJ, Mitchell EA, Other Members of the National Cot Death Study Group. Sudden infant death syndrome: insulation from bedding and clothing and its effect modifiers. Int J Epidemiol. 1996;25:366–75.
Naeye RL, Ladis B, Drage JS. Sudden infant death syndrome: a prospective study. Am J Dis Child. 1976;130:1207–10.
Bach V, Bouferrache B, Kremp O, Maingourd Y, Libert JP. Regulation of sleep and body temperature in response to exposure to cool and warm environments in neonates. Pediatrics. 1994;93:789–96.
Franco P, Scaillet S, Valente F, Chabanski S, Groswasser J, Kahn A. Ambient temperature is associated with changes in infants’ arousability from sleep. Sleep. 2001;24:325–9.
Stephan-Blanchard E, Chardon K, Leke A, Delanaud S, Bach V, Telliez F. Heart rate variability in sleeping preterm neonates exposed to cool and warm thermal conditions. PLoS One. 2013;8:e68211.
Blair PS, Mitchell EA, Heckstall-Smith EMA, Fleming PJ. Head covering a major modifiable risk factor for sudden infant death syndrome: a systematic review. Arch Dis Child. 2008;93:778–83.
Mitchell EA, Thompson JM, Becroft DM, Bajanowski T, Brinkmann B, Happe A, Jorch G, Blair PS, Sauerland C, Vennemann MM. Head covering and the risk for SIDS: findings from the New Zealand and German SIDS case-control studies. Pediatrics. 2008;121:e1478–83.
Paluszynska DA, Harris KA, Thach BT. Influence of sleep position experience on ability of prone-sleeping infants to escape from asphyxiating microenvironments by changing head position. Pediatrics. 2004;114:1634–9.
Franco P, Lipshut W, Valente F, Adams M, Grosswasser J, Kahn A. Cardiac autonomic characteristics in infants sleeping with their head covered by bedclothes. J Sleep Res. 2003;12:125–32.
Franco P, Lipshutz W, Valente F, Adams S, Scaillet S, Kahn A. Decreased arousals in infants who sleep with the face covered by bedclothes. Pediatrics. 2002;109:1112–7.
Carpenter R, McGarvey C, Mitchell EA, Tappin DM, Vennemann MM, Smuk M, Carpenter JR. Bed sharing when parents do not smoke: is there a risk of SIDS? An individual level analysis of five major case-control studies. BMJ Open. 2013 May 28;3(5). pii: e002299. doi: 10.1136/bmjopen-2012-002299.
Blair PS, Sidebotham P, Evason-Coombe C, Edmonds M, Heckstall-Smith EMA, Fleming P. Hazardous co-sleeping environments and risk factors amenable to change: case-control study of SIDS in south west England. BMJ. 2009;339:b3666.
Blair PS, Sidebotham P, Pease A, Fleming PJ. Bed-sharing in the absence of hazardous circumstances: is there a risk of sudden infant death syndrome? An analysis from two case-control studies conducted in the UK. PLoS One. 2014;9:e107799.
Escott AS, Elder ED, Zuccollo JM. Sudden unexpected infant death and bedsharing: referrals to the Wellington Coroner 1997–2006. N Z Med J. 2009;122:59–68.
Hauck FR, Signore C, Fein SB, Raju TNK. Infant sleeping arrangements and practices during the first year of life. Pediatrics. 2008;122:S113–20.
McKenna JJ, Mosko SS. Sleep and arousal synchrony and independence among mothers and infants sleeping apart and together (same bed): an experiment in evolutionary medicine. Acta Paediatr Suppl. 1994;397:94–102.
Baddock SA, Galland BC, Bolton DP, Williams SM, Taylor BJ. Differences in infant and parent behaviors during routine bed sharing compared with cot sleeping in the home setting. Pediatrics. 2006;117:1599–607.
Hoffman HJ, Damus K, Hillman L, Krongrad E. Risk factors for SIDS. Results of the National Institute of Child Health and Human Development SIDS Cooperative Epidemiological Study. Ann NY Acad Sci. 1988;533:13–30.
Leach CE, Blair PS, Fleming PJ, Smith IJ, Platt MW, Berry PJ, Golding J, Group., C. S. R. Epidemiology of SIDS and explained sudden infant deaths. Pediatrics. 1999;104:43–53.
Heininger U, Kleemann WJ, Cherry JD, Group., S. I. D. S. S. A controlled study of the relationship between bordetella pertussis infections and sudden unexplained deaths among German infants. Pediatrics. 2004;114:9–15.
Ponsonby A-L, Dwyer T, Gibbons LE, Cochrane JA, Wang Y-G. Factors potentiating the risk of sudden infant death syndrome associated with the prone position. N Engl J Med. 1993;329:377–82.
Hunt CE, Hauck FR. Sudden infant death syndrome. Can Med Assoc J. 2006;174:1861–9.
Horne RS, Osborne A, Vitkovic J, Lacey B, Andrew S, Chau B, Cranage SM, Adamson TM. Arousal from sleep in infants is impaired following an infection. Early Hum Dev. 2002;66:89–100.
Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Yucsesan K, Sauerland C, Mitchell EA, GeSID Study Group. Does breastfeeding reduce the risk of sudden infant death syndrome? Pediatrics. 2009;123:e406–10.
Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128:103–10.
Gordon AE, Saadi AT, Mackenzie DAC, Molony N, James VS, Weir DM, Busuttil A, Blackwell CC. The protective effect of breast feeding in relation to Sudden Infant Death Syndrome (SIDS): III. Detection of IgA antibodies in human milk that bind to bacterial toxins implicated in SIDS. FEMS Immunol Med Microbiol. 1999;25:175–82.
Mcvea KLSP, Turner PD, Peppler DK. The role of breastfeeding in sudden infant death syndrome. J Hum Lact. 2000;16:13–20.
Butte NF, Smith EO, Garza C. Heart rate of breast-fed and formula-fed infants. J Pediatr Gastroenterol Nutr. 1991;13:391–6.
Elias MF, Nicolson NA, Bora C, Johnston J. Sleep/wake patterns of breast-fed infants in the first 2 years of life. Pediatrics. 1986;77:322–9.
Horne R, Franco P, Adamson T, Grosswasser J, Kahn A. Influences of maternal cigarette smoking on infant arousability. Early Hum Dev. 2004;79:49–58.
Fleming PJ, Blair PS, Pollard K, Platt MW, Leach C, Smith I, Berry PJ, Golding J, CESDI SUDI Research Team. Pacifier use and sudden infant death syndrome: results from the CESDI/SUDI case control study. Arch Dis Child. 1999;81:112–6.
Hauck FR, Omojokun OO, Siadaty MS. Do pacifiers reduce the risk of sudden infant death syndrome? A meta-analysis. Pediatrics. 2005;116:e716–23.
Li D, Willinger M, Petiti DB, Odouli R, Liu L, Hoffman HJ. Use of a dummy (pacifier) during sleep and risk of Sudden Infant Death Syndrome (SIDS): population based case-control study. BMJ. 2006;332:18–22.
Mitchell EA, Blair PS, L’Hoir MP. Should pacifiers be recommended to prevent sudden infant death syndrome? Pediatrics. 2006;117:1755–8.
Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Sauerland C, Mitchell EA, Group, T. G. S. Sleep environment risk factors for sudden infant death syndrome: the German Sudden Infant Death Syndrome Study. Pediatrics. 2009;123:1162–70.
Horne RS, Hauck FR, Moon RY, L’Hoir MP, Blair PS, Physiology, Epidemiology Working Groups of the International Society for the, S., Prevention of, P. & Infant, D. Dummy (pacifier) use and sudden infant death syndrome: potential advantages and disadvantages. J Paediatr Child Health. 2014;50:170–4.
Franco P, Chabanski S, Scaillet S, Grosswasser J, Kahn A. Pacifier use modifies infant’s cardiac autonomic controls during sleep. Early Hum Dev. 2004;77:99–108.
Yiallourou SR, Poole H, Prathivadi P, Odoi A, Wong FY, Horne RS. The effects of dummy/pacifier use on infant blood pressure and autonomic activity during sleep. Sleep Med. 2014;15:1508–16.
Lappi H, Valkonen-Korhonen M, Georgiadis S, Tarvainen MP, Tarkka IM, Karjalainen PA, Lehtonen J. Effects of nutritive and non-nutritive sucking on infant heart rate variability during the first 6 months of life. Infant Behav Dev. 2007;30:546–56.
Hanzer M, Zotter H, Sauseng W, Pichler G, Mueller W, Kerbl R. Non-nutritive sucking habits in sleeping infants. Neonatology. 2010;97:61–6.
Cohen M, Brown DR, Myers MM. Cardiovascular responses to pacifier experience and feeding in newborn infants. Dev Psychobiol. 2001;39:34–9.
Franco P, Scaillet S, Wermenbol V, Valente F, Groswasser J, Kahn A. The influence of a pacifier on infants’ arousals from sleep. J Pediatr. 2000;136:775–9.
Hanzer M, Zotter H, Sauseng W, Pichler G, Pfurtscheller K, Mueller W, Kerbl R. Pacifier use does not alter the frequency or duration of spontaneous arousals in sleeping infants. Sleep Med. 2009;10:464–70.
Odoi A, Andrew S, Wong FY, Yiallourou SR, Horne RS. Pacifier use does not alter sleep and spontaneous arousal patterns in healthy term-born infants. Acta Paediatr. 2014;103:1244–50.
Tonkin SL, Lui D, Mcintosh CG, Rowley S, Knight DB, Gunn AJ. Effect of pacifier use on mandibular position in preterm infants. Acta Paediatr. 2007;96:1433–6.
Cozzi F, Albani R, Cardi E. A common pathophysiology for sudden cot death and sleep apnoea. “The vacuum-glossoptosis syndrome”. Med Hypotheses. 1979;5:329–38.
Lipton EL, Steinschneider A, Richmond JB. Swaddling, a child care practice: historical, cultural, and experimental observations. Pediatrics. 1965;35:521–67.
van Sleuwen BE, L’Hoir MP, Engleberts AC, Westers P, Schulpen TWJ. Infant care practices related to cot death in Turkish and Moroccan families in the Netherlands. Arch Dis Child. 2003;88:784–8.
Beal SM, Porter C. Sudden infant death syndrome related to climate. Acta Paediatr Scand. 1991;80:278–87.
Wilson CA, Taylor BJ, Laing RM, Williams SM, Mitchell EA. Clothing and bedding and its relevance to sudden infant death syndrome: further results from the New Zealand Cot Death Study. J Paediatr Child Health. 1994;30:506–12.
Karp H. The happiest baby on the block. New York: Bantam; 2002.
van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TWJ, L’Hoir MP. Swaddling: a systematic review. Pediatrics. 2007;120:e1097–106.
Gerard CM, Harris KA, Thach BT. Physiologic studies on swaddling: an ancient child care practice, which may promote the supine position for infant sleep. J Pediatr. 2002;141:398–403.
Richardson HL, Walker AM, Horne RSC. Minimizing the risk of sudden infant death syndrome: to swaddle or not to swaddle? J Pediatr. 2009;155:475. ePub August 2009.
Narangerel G, Pollock J, Manaseki-Holland S, Henderson J. The effects of swaddling on oxygen saturation and respiratory rate of healthy infants in Mongolia. Acta Paediatr. 2007;96:261–5.
Franco P, Seret N, van Hees J, Scaillet S, Grosswasser J, Kahn A. Influence of swaddling on sleep and arousal characteristics of healthy infants. Pediatrics. 2005;115:1307–11.
Richardson HL, Walker AM, Horne RS. Influence of swaddling experience on spontaneous arousal patterns and autonomic control in sleeping infants. J Pediatr. 2010;157:85–91.
Chisholm JS. Swaddling, cradleboards and the development of children. Early Hum Dev. 1978;2:255–75.
Gerard CM, Harris KA, Thach BT. Spontaneous arousals in supine infants while swaddled and unswaddled during rapid eye movement and quiet sleep. Pediatrics. 2002;110:70–6.
Franco P, Scaillet S, Grosswasser J, Kahn A. Increased cardiac autonomic responses to auditory challenges in swaddled infants. Sleep. 2004;27:1527–32.
Leiter JC, Bohm I. Mechanisms of pathogenesis in the sudden infant death syndrome. Respir Physiol Neurobiol. 2007;159:127–38.
Chang RR, Keens TG, Rodriguez S, Chen AY. Sudden infant death syndrome: changing epidemiologic patterns in California 1989–2004. J Pediatr. 2008;153:498–502.
Hauck FR, Tanabe KO. International trends in sudden infant death syndrome: stabilization of rates requires further action. Pediatrics. 2008;122:660–6.
Fleming PJ, Blair PS, Pease A. Sudden unexpected death in infancy: aetiology, pathophysiology, epidemiology and prevention in 2015. Arch Dis Child. 2015;100:984.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Horne, R.S.C. (2017). Sleep Disorders in Newborns and Infants. In: Nevšímalová, S., Bruni, O. (eds) Sleep Disorders in Children. Springer, Cham. https://doi.org/10.1007/978-3-319-28640-2_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-28640-2_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28638-9
Online ISBN: 978-3-319-28640-2
eBook Packages: MedicineMedicine (R0)