Abstract
Electrical stimulation is a tool that applies low-energy electrical pulses to artificially generate muscle contractions. If electrical stimulation is used to enable functional movements, such as walking and grasping, then this intervention is called functional electrical stimulation (FES). When FES is used as a therapy instead of being used as an orthosis, it is called FES therapy or FET. In this chapter, we introduce recent findings and advances in the field of FET. The findings to date clearly show that FET for reaching and grasping is a therapeutic modality that should be implemented in every rehabilitation institution that is treating patients with stroke and SCI. There is also considerable evidence to support the use of FET as a therapeutic modality to treat drop-foot problem in both stroke and incomplete spinal cord injury (SCI) populations. Although phase I randomized control trials have been completed with chronic SCI population using this new FET technology and preliminary findings are encouraging, further R&D is required before the multichannel FET for walking will be ready for prime time clinical implementation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Functional electrical stimulation (FES)
- Therapy
- FES therapy
- Spinal cord injury
- Stroke
- Rehabilitation
- Neuroprosthesis
- Neurorehabilitation
- Restoration of voluntary function
1 Introduction
Functional electrical stimulation (FES) is a technology one can use to artificially generate body movements in individuals who have paralyzed muscles due to injury to the central nervous system. More specifically, FES can be used to generate functions such as grasping and walking in individuals with spinal cord injury (SCI) and stroke. This technology was originally used to develop neuroprostheses that were implemented to permanently substitute impaired functions such as bladder voiding, grasping, and walking. In other words, a consumer would use the device each time she/he wanted to generate a desired function. In recent years FES technology has been used to deliver therapies to retrain voluntary motor functions such as grasping, reaching, and walking. In this embodiment, FES is used as a short-term therapy, the objective of which is restoration of voluntary function and not lifelong dependence on the FES device, hence the name FES therapy or FET. In other words, FET is used as a short-term intervention to help the central nervous system of the consumer to relearn how to execute impaired functions, instead of making the consumer dependent on neuroprostheses for the rest of her/his life. In this chapter, we introduce recent findings and advances in the field of FET.
2 Functional Electrical Stimulation (FES)
2.1 Definitions
Individuals with SCI and stroke have injuries that prevent the central nervous system from generating a desired motor command and/or transmitting the desired motor command to the parts of the peripheral nervous system that innervate muscles. As a result, these individuals are frequently unable to voluntarily move different body parts and perform functions such as sitting, standing, reaching, grasping, and bladder voiding. However, as long as the nerves innervating the muscles, the muscles themselves, and the joints and soft tissues supporting the muscle-joint structures are intact, the electrical stimulation can be used to generate joint movements by contracting the muscles that actuate them. The electrical stimulation used for this purpose is called neuromuscular electrical stimulation (NMES). An organized and patterned NMES that aims to generate coordinated limb or body movements, instead of isolated muscle contractions, is called functional electrical stimulation (FES). One of the possible applications of FES technology is to artificially generate body movements such as grasping, standing, and walking. In such a context, the FES technology is used as a prosthetic/orthotic device. In literature, this use of FES technology is referred to as neuroprosthesis or neuroprosthetics.
2.2 Physiology
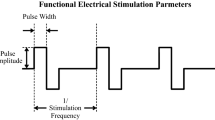
In nerve cells, information is coded and transmitted as a series of electrical impulses called action potentials, which represent a brief change in cell electric potential of approximately 80–90 mV. Nerve signals are frequency modulated; that is, the number of action potentials that occur in a unit of time is proportional to the intensity of the transmitted signal. Typical action potential frequency is between 4 and 12 Hz. An electrical stimulation can artificially elicit this action potential by changing the electric potential across a nerve cell membrane (this also includes the nerve axon) by inducing electrical charge in the immediate vicinity of the outer membrane of the cell (Fig. 25.1).
A schematic representation of the surface functional electrical stimulation (FES) system. The FES system causes a muscle contraction by electrically stimulating the motor axons that are connected to the muscles. The electrical stimulation generates action potentials in the motor neurons, which propagate along the motor neurons toward the muscle. When the action potentials reach the muscle, they cause the muscle to contract
The stimulated nerve bundle includes motor nerves (efferent nerves—descending nerves from the central nervous system to muscles) and sensory nerves (afferent nerves—ascending nerves from sensory organs to the central nervous system). In some applications, FES can be used to directly stimulate muscles, if their peripheral nerves have been severed or damaged (i.e., denervated muscles) [1]. However, the majority of the FES systems used today stimulate the nerves or the points where the junction occurs between the nerve and the muscle. The main reason is the fact that direct muscle stimulation requires considerably more energy to generate contractions (at least three orders of magnitude more [2]), which makes these systems more challenging to implement at home and in clinical settings. Nevertheless, it should be noted that an electric stimulator that has been purposefully designed to generate contractions in denervated muscles is currently commercially available. Its name is Stimulette den2x, and it is manufactured by Dr. Schuhfried, Medical technology, Austria (www.schuhfriedmed.at/en/). In the remainder of this document, we will only discuss FES systems that have been developed to stimulate innervated muscles.
The electrical charge can stimulate both motor and sensory nerves. In some applications, the nerves are stimulated to generate localized muscle activity, i.e., the stimulation is aimed at generating direct muscle contraction. In other applications, stimulation is used to activate simple or complex reflexes. In other words, the afferent nerves are stimulated to evoke a reflex, which is typically expressed as a coordinated contraction of one or more muscles in response to the sensory nerve stimulation.
When a nerve is stimulated, i.e., when sufficient electrical charge is provided to a nerve cell, a localized depolarization of the cell wall occurs resulting in an action potential that propagates toward both ends of the axon. Typically, one “wave” of action potentials will propagate along the axon toward the muscle (orthodromic propagation), and concurrently, the other “wave” of action potentials will propagate toward the cell body in the central nervous system (antidromic propagation). While the direction of propagation in case of the antidromic stimulation and the sensory nerve stimulation is the same, i.e., toward the central nervous system, their end effects are very different. The antidromic stimulus has been considered an irrelevant side effect of FES. According to Rushton [3], repeated antidromic stimulation through Hebb-type processes may over time enable week/sparse supraspinal commands to activate anterior motor neuron and enable it to produce desired muscle contraction(s). Typically, FES is concerned with orthodromic stimulation and uses it to generate coordinated muscle contractions.
In the case where sensory nerves are stimulated, the reflex arcs are triggered by the stimulation of sensory nerve axons at specific peripheral sites. One example of such a reflex is the flexor withdrawal reflex. The flexor withdrawal reflex occurs naturally when a sudden, painful sensation is applied to the sole of the foot. It results in flexion of the hip, knee, and ankle of the affected leg and extension of the contralateral leg in order to get the foot away from the painful stimulus as quickly as possible. The sensory nerve stimulation can be used to generate desired motor tasks, such as evoking flexor withdrawal reflex to facilitate walking in individuals following stroke, or they can be used to alter reflexes or the function of the central nervous system. In the later case, the electrical stimulation is commonly described by the term neuromodulation.
2.3 Technology
Nerves can be stimulated using either surface (transcutaneous) or subcutaneous (percutaneous or implanted) electrodes. The surface electrodes are placed on the skin surface above the nerve or muscle that needs to be “activated.” They are noninvasive, easy to apply, and generally inexpensive. Until recently the common belief in the FES field has been that due to the electrode-skin contact impedance, skin and tissue impedance, and current dispersion during stimulation, much higher-intensity pulses are required to stimulate nerves using surface stimulation electrodes as compared to the subcutaneous electrodes. This statement is correct for all commercially available stimulators except MyndMove® stimulator (Fig. 25.2), which is manufactured by a Canadian company MyndTec (www.myndtec.com). MyndMove® has implemented a new stimulation pulse that allows the stimulator to generate muscle contractions using electrical pulses, which amplitudes are 10–15 times lower in intensity then those required by other transcutaneous electrical stimulation systems. The key aspects of this new technology are stimulation pulses that have very fast slew rate (US Patent 20130090712) and are able to rapidly engage Aα efferent nerve fibers (i.e., descending nerves from the central nervous system to muscles) using very low stimulation amplitudes and at the same time minimize engagement of afferent Aδ and C nerve fibers responsible for transmission of pain sensation. This new technology not only reduces the intensity of stimulation, but it also reduces discomfort during stimulation, which is a common problem with commercially available transcutaneous electrical stimulation systems.
A major limitation of the transcutaneous electrical stimulation is that some nerves, for example, those innervating the hip flexors, are too deep to be stimulated using surface electrodes. This limitation can be partly addressed by using arrays of electrodes, which can use several electrical contacts to increase selectivity [4–6].
Subcutaneous electrodes can be divided into percutaneous and implanted electrodes. The percutaneous electrodes consist of thin wires inserted through the skin and into muscular tissue close to the targeted nerve. These electrodes typically remain in place for a short period of time and are only considered for short-term FES interventions. However, it is worth mentioning that some groups, such as Cleveland FES Center, have been able to safely use percutaneous electrodes with individual patients for months and years at a time. One of the drawbacks of using the percutaneous electrodes is that they are prone to infection, and special care has to be taken to prevent such events.
The other class of subcutaneous electrodes is implanted electrodes. These are permanently implanted in the consumer’s body and remain in the body for the remainder of the consumer’s life. Compared to surface stimulation electrodes, implanted and percutaneous electrodes potentially have higher stimulation selectivity, which is a desired characteristics of FES systems. To achieve higher selectivity while applying lower stimulation amplitudes, it is recommended that both cathode and anode are in the vicinity of the nerve that is stimulated [7]. The drawbacks of the implanted electrodes are they require an invasive surgical procedure to install, and, as is the case with every surgical intervention, there exists a possibility of infection following implantation.
3 FES Therapy (FET)
3.1 Definition
FES can be used for neuroprosthetic and therapeutic purposes. If FES is used as a neuroprosthesis, the purpose of this device is to generate a body function that the consumer is unable to perform alone, such as walking, biking, bladder voiding, grasping, etc. In this application the FES system needs to be worn or used each and every time the consumer needs to perform the desired function. In essence, the consumer uses the FES device as a permanent orthotic system.
The use of neuroprostheses as a means of providing short-term therapeutic intervention for improving and restoring voluntary function has been termed FES therapy or FET [8]. When the FES technology is used to deliver FET, the purpose of that intervention is to restore voluntary function. In other words, FES is used only temporarily as a short-term intervention with the objective of helping the neuromuscular system relearn to execute a function impaired due to neurological injury or disorder. In this application the ultimate goal of the FES intervention is for the consumer to recover voluntary function, as much as possible, so the consumer does not need to use the FES system for the rest of her/his life. In this application, the central nervous system essentially relearns how to control the impaired muscles and how to contract them in a temporarily appropriate manner to generate the desired body function. Since FET systems are generally noninvasive and are used to produce diverse upper or lower limb movements/therapies, FET-dedicated systems can have many more stimulation protocols (e.g., ten or more for upper limb FET) that at times target different muscle groups and can be used with a single consumer. However, the neuroprostheses that are used as permanent orthotic systems often target one set of muscles or muscle groups and have one or at best two/three consumer-specific stimulation protocols.
Some neuroprosthetic systems are also used for cardiovascular conditioning and muscle strengthening. Although the ultimate goal of this type of application is therapeutic, this is not FET. Good examples of these FES systems are neuroprostheses for rowing and biking. Each time the consumer wants to row or bike she/he needs to use the neuroprosthetic system, without which she/he would not be able to perform this task at all. Good examples of such technologies that are commercially available are RT300 FES bike from Restorative Therapies (www.restorative-therapies.com) and RehaBike by Hasomed (www.hasomed.de).
The implanted FES systems are primarily used as permanent neuroprostheses. However, some attempts have been made to use the BION implantable FES system for FET [9]. On the other hand, the surface FES systems have been used equally well as neuroprostheses and platforms to deliver FET. In the past, the main focus of the FES field was on developing neuroprosthetic systems, in particular those that patients had to use daily. In recent years, the advances made in the field of FET and the use of neuroprostheses for muscle strengthening and cardiovascular exercises have shifted the focus of the FES field, at least partially, toward the use of surface FES systems. As a result, a number of commercially available surface FES systems have been developed in last decade.
3.2 Neuroplasticity Effect
Since the 1970s, some researchers and practitioners in the field of FES have observed that many patients who use FES on a regular basis experience significant carry-over in function that persists even when the device is not in use. This “enigma” of “carry-over effect” has interested researchers [10], even though most of these reports were anecdotal in nature at the beginning.
One of the first papers that specifically discussed this phenomenon was an article authored by Merletti et al. in 1975 [11]. They investigated the carry-over effect of FES on hand opening and elbow extension functions for stroke patients. Three of five patients showed the carry-over effects after a 2-month training period, i.e., after the FES intervention session, functional tasks such as the shifting of an object between two specified areas on a desk were improved even without wearing the FES device. The observed carry-over effect supported the potential role of neuroprostheses as therapeutic interventions in clinical practice. Despite the fact that FES-related carry-over results were observed as early as the 1970s, a rigorous investigation of FES carry-over effect started only recently.
4 Current Evidences of FET
It took almost two decades before the carry-over effect started being examined seriously. As describe next, it was first examined with the drop-foot FES systems, where scientists explored the ability of the system to restore voluntary walking function in individuals with stroke. These studies were then followed by studies examining the use of a neuroprosthesis for grasping and, later, neuroprostheses for reaching and grasping for restoring voluntary arm and hand functions in individuals with stroke and SCI. Finally, the neuroprosthesis for walking was used to investigate restoration of voluntary walking function in individuals with incomplete SCI.
Initially, FET did not exist as a field on its own, and the first FET studies were essentially examining carry-over effect of the neuroprostheses. Once, it become clear that FET is actually helping reprogram the central nervous system and that the carry-over effect is not due to the muscle strengthening (which was initially suspected [12]) but was due to neuroplasticity, the FET field has been established and FET-dedicated systems started being developed. The systems used to test FET concept were originally neuroprostheses that were normally used as orthoses. Today we are experiencing the development of FET-dedicated systems, which design requirements are very different from the “garden variety” neuroprosthetic systems developed for orthotic applications.
4.1 FET for Restoration of Lower Limb Function Following Stroke
Among stroke patients, the drop-foot is a common symptom, characterized by a lack of dorsiflexion during the swing phase of gait, resulting in short, shuffling strides. It has been shown that the drop-foot stimulator effectively compensates for the drop-foot during the swing phase of the gait. At the moment just before a heel off phase of the gait occurs, the drop-foot stimulator induces a stimulus at the common peroneal nerve, which results in contraction of the muscles responsible for dorsiflexion (Fig. 25.3). There are a number of drop-foot stimulators, which use surface FES technology and have been FDA (US Food and Drug Administration) approved, that have been developed to date: the Odstock® Dropped Foot Stimulator (ODFS® Pace) by Odstock Medical (www.odstockmedical.com) [13], the WalkAide® by Innovative Neurotronics (www.walkaide.com) [14], and the NESS L300 for Foot Drop by Bioness (www.bioness.com) [15]. The ActiGait® by Ottobock (www.ottobock.com) [16] and the STIMuSTEP® by Finetech Medical (www.finetech-medical.co.uk) [17] are implantable drop-foot stimulators that are also commercially available and have the CE mark in Europe. Drop-foot stimulators are one of the most successful neuroprostheses to date after cochlear implants. Overall, consumer perception of the drop-foot stimulators is they are superior to the ankle-foot orthosis [18].
There has been a great deal of evidence showing the benefits of the drop-foot FES for the lower limbs of stroke patients. In most of the studies, the effect of the drop-foot stimulator as an orthosis has been studied. Only few studies have investigated the FET effect in stroke patients with drop-foot problem (e.g. [19]). In the early phase, some studies showed a negative result with respect to the FET effect [20, 21], while other studies showed positive effect on the FET effect [13]. For example, Granat et al. [21] investigated the effect of a drop-foot stimulator on hemiplegic patients (n = 19) in a two-period crossover study design (4-week control period followed by 4-week FES treatment period). The results demonstrated that there was a significant orthotic effect (positive effect when the subject was using the FES system) in inversion of ankle, while the same study did not show a therapeutic effect (positive effect when the subjects was not using the FES system, i.e., FET effect). In a randomized controlled trial, Burridge et al. [20] investigated the effect of a drop-foot stimulator on individuals with stroke. The intervention group (n = 16) received conventional physiotherapy and FES treatment, while the control group (n = 16) received conventional physiotherapy alone. They demonstrated that the mean increase in walking speed was 20.5 % in the intervention group when the subjects in that group used the drop-foot stimulator as an orthosis. The control group showed only a 5.2 % increase in mean walking speed. The physiological cost index (PCI) was reduced 24.9 % in the intervention group when they were using the drop-foot stimulator as an orthosis and was reduced 1 % in the control group. However, the same study did not show any improvements in the intervention group when the drop-foot stimulator was removed. In other words, they were not able to demonstrate the drop-foot stimulator’s FET effect. Taylor et al. [13] investigated the effect of a drop-foot stimulator in stroke (n = 9) and multiple sclerosis (MS) (n = 2) patients. Stroke patients showed a mean increase in walking speed of 27 % and a reduction in PCI of 31 % when the system was used as an orthosis. However, the same study showed a 14 % increase in walking speed and a 19 % reduction in PCI, when the stimulator was removed from the patients, i.e., FET effect. The MS patients showed similar benefits when they used the drop-foot stimulator as an orthosis, with no noticeable FET effects.
Recently, in a relatively larger population study, Stein et al. [14] investigated the effect of a drop-foot stimulator in stroke (n = 41) and MS (n = 32) patients. They demonstrated that both stroke and MS patients showed increased walking speed when the system is used as therapeutic and orthotic devices. After 3 months of drop-foot stimulator training, both groups had a similar and significant orthotic (increments of 5.0 % and 5.7 % for stroke and MS patients, respectively) and FET (17.8 % and 9.1 % for stroke and MS patients, respectively) effects on walking speed, during over ground figure-8 walking. After 11 months of following the baseline, the FET effect on figure-8 speed diverged between the two groups to 28.0 % and 7.9 % for stroke and MS patients, respectively. Overall, PCI showed a decreasing trend. They concluded that both subject groups had an orthotic benefit from FES up to 11 months. The FET effect increased up to 11 months in stroke patients, which is a nonprogressive neurologic disorder, while in the MS patients, as expected, the therapeutic effect increased only in the first 3 months following the baseline.
In summary, there is considerable evidence that the drop-foot stimulators, if they are used to deliver FET, produce lasting positive changes in gait in individuals with stroke.
4.2 FET for Restoration of Lower Limb Function Following SCI
Impairment in lower limb function is a common symptom following SCI. Various FES systems have been developed to help individuals with SCI to improve walking function. In individuals with SCI, the scope of impairment is not limited to the ankle joint, as is the case with many stroke individuals, but rather affects many muscles in the legs, pelvis, and trunk. Thus, the FES technology for walking for individuals with SCI is more diverse and targets the muscles of the entire lower limb. However, it is not uncommon that in some individuals with SCI, the above discussed drop-foot stimulators have been also used as a means to assist with gait.
As early as the 1960s, Kantrowitz demonstrated paraplegic standing by applying continuous electrical stimulation to the quadriceps and gluteus maximus muscles of a patient with complete SCI, using surface FES technology [22]. This earliest neuroprosthesis for paraplegic “gait” provided continuous stimulation to the quadriceps to produce a mode of gait similar to long leg-brace walking, by inducing stiffened legs. Later systems used alternating bilateral quad/glut stimulation (during stance phase) out of phase with peroneal nerve stimulation to induce the flexor withdrawal reflex (during swing phase) [23]. Following that, Kralj et al. described a technique for paraplegic gait using surface electrical stimulation, which remains the most popular method in use today [24]. Electrodes are placed over the quadriceps muscles and peroneal nerves bilaterally. The user controls the neuroprosthesis with two pushbuttons attached to the left and right handles of a walking frame, or on canes, or crutches. When the neuroprosthesis is turned on, both quadriceps muscles are stimulated to provide a standing posture. The left button initiates the swing phase in the left leg by briefly stopping stimulation of the left quadriceps and stimulating the peroneal nerve. This stimulation is applied suddenly, so as to trigger the flexor withdrawal reflex, resulting in simultaneous hip and knee flexion, as well as dorsiflexion. After a fixed period of time, peroneal nerve stimulation is stopped, and quadriceps stimulation is initiated, while the reflex is still active to complete the stride. Similarly, the right button initiates swing phase in the right leg. Many current FES systems for walking have employed this technique as the basic concept.
As microprocessor technology developed, neuroprostheses for walking became more portable and flexible. Examples of this type of neuroprosthesis are Parastep [25, 26], HAS [27], and RGO [28] and the Case Western Reserve University (CWRU)/VA neuroprosthesis [29–32]. The Parastep system is one of most popular products and uses Kralj’s technique [25, 26] (Fig. 25.4). The HAS and the RGO walking neuroprostheses are devices that, in addition to FES, also apply active and passive braces, respectively. The braces were introduced to provide additional stability during standing and walking and to conserve the user’s energy. CWRU/VA neuroprosthesis is an implant system [29–32]. Parastep, HAS, and RGO systems were designed for orthotic use; however, they could be potentially implemented as FET devices as well.
The above neuroprostheses for walking apply the flexor withdrawal reflex to generate stepping movement during the walking cycle. There is a disadvantage in using this approach as the flexor withdrawal reflex is highly variable and is subject to rapid habituation. However, there are systems that do not use the flexor withdrawal reflex, instead they stimulate muscles in a manner that is as close as possible to the physiologically correct muscle activation pattern that generates the bipedal walking cycle. Good examples of such systems are the Case Western Reserve University (CWRU)/VA neuroprosthesis [29–32], Praxis [33], and Compex Motion neuroprosthesis for walking [34, 35]. The Praxis and CWRU/VA neuroprosthesis are implantable FES device systems that have 22 and 8–16 stimulation channels, respectively. They are able to generate sit-to-stand, walking, and stand-to-sit functions and are suitable to orthotic applications. However, recently the Cleveland team tested the therapeutic effects of their implantable system in a single-subject study [29].
Compex Motion neuroprosthesis for walking is an 8–16 channel surface FES system used to restore walking in stroke and SCI individuals [34]. The system uses a push button control strategy, similar to the one used in the Parastep system, and a gate phase detection sensor [36] to trigger the FES sequences. What is unique about this FES system is that it was specifically developed for FET applications. The benefits of FES for lower limbs of individuals with incomplete SCI were discussed in a review by Bajd et al. [37]. The review concluded that there are various benefits including therapeutic effect of FES for individuals with SCI and of strength training, drop-foot stimulator, and plantar flexor stimulation during gait phase.
In addition to those studies, Wieler et al. [38] investigated, in a multicenter study, the effect of a drop-foot stimulator and a withdrawal reflex stimulator on individuals with SCI (n = 31) and with cerebral impairment (n = 9). The results showed that the walking speed increased by approximately 40 % when the drop-foot stimulator was used as an orthotic device and 20 % as when it was used as FET device. Similar findings have been published by Field-Fote and her team [39, 40].
Thrasher et al. [35] hypothesized that direct muscle stimulation would have greater rehabilitative potential than the stimulation of flexor withdrawal reflexes. They investigated the effect of a gait-patterned multichannel FES in five individuals with chronic, incomplete SCI. These subjects were trained for 12–18 weeks using Compex Motion multichannel neuroprosthesis for walking. All subjects demonstrated significant improvements in walking function over the training period. Four of the subjects achieved significantly increased walking speeds, which were due to increases in both stride length and step frequency. The fifth subject experienced a significant reduction in preferred assistive devices. The results suggest that the proposed FES-based gait training regimen was effective for improving voluntary walking function in a population for whom significant functional changes are not expected and that this application of FET is viable for restoration of voluntary gait in incomplete SCI.
Inspired by Thrasher et al. [35] results, Toronto team carried out phase I randomized control trial in which they compared the gait-patterned multichannel FET against equal dose of convectional exercise [41–43]. Patient population was incomplete chronic SCI individuals. The results of the study suggested that 40 h of exercise and 40 h of multichannel FET both generated clinically meaningful improvements in this patient population. At the same time, the differences between the two groups were minimal, meaning that FET in this patient population did not generate superior outcomes compared to the control group. However, it should be noted that the Spinal Cord Independence Measure (SCIM) Mobility Subscore improved in FET group significantly more than in the control group [43].
In summary, there is mounting evidence that, in individuals with incomplete SCI, neuroprostheses for walking can be used as FET devices to improve voluntarily walking function. Most of the work has been done using drop-foot stimulators. However, more complex gait-patterned multichannel FES systems have been recently tested as FET systems and have shown encouraging results with respect to improving voluntary walking function in more severely disable individuals with SCI.
4.3 FET for Restoration of Upper Limb Function Following Stroke
Impaired reaching and grasping functions are common symptoms among stroke patients. Numerous neuroprostheses have been designed to compensate for lost grasping [44–55] and grasping and reaching [8, 34, 52, 56, 57] functions in stroke patients.
Some notable grasping and/or reaching neuroprostheses are the Freehand system [7], the NESS H200 for Hand Paralysis by Bioness (www.bioness.com) [48] (Fig. 25.5), the Bionic Glove [49, 52, 58], the ETHZ-ParaCare neuroprosthesis for grasping [34, 59, 92], the systems developed by Rebersek and Vodovnik [53], the Belgrade Grasping-Reaching System [60], Compex Motion neuroprosthesis for reaching and grasping [34], the percutaneous systems by Chae et al. [45, 46], and recently MyndMove® by MyndTec (www.myndtec.com). The above neuroprostheses for grasping were shown to restore the power grasp and the precision grip. The power grasp is used to hold larger and heavier objects between the palm of the hand and the four fingers. During a power grasp, the object is held in a clamp formed by partly flexed fingers and the palm counter pressure being applied by the thumb lying more or less in the plane of the palm. Precision grip is used to hold smaller and thinner objects, such as keys and paper, between the thumb and forefinger. The precision grip is generated by flexing the fingers followed by opposition of the thumb. In addition to these two grasping styles, Compex Motion neuroprosthesis and MyndMove® system offer variety of additional grasping styles, such as pinch grasp, lumbrical grasp, tripod grasp, and proper hand opening that involves activation of the intrinsic muscles of the hand. The Belgrade Grasping-Reaching System, Freehand system, Compex Motion system, and MyndMove® also offer reaching capabilities. Of these systems MyndMove® offers the largest diversity of grasping and/or reaching tasks that can be performed with a single FES system. The Freehand system is an implantable FES system designed for individuals with SCI, while the remaining devices are surface FES systems that can be used to deliver FET.
The use of FES as means of improving hand function following stroke has been intensively studied for a long time. A meta-analysis in 1996 already proved that FES is effective in recovery of muscle strength after stroke [61]. Recent studies that have specifically examined FET have suggested positive outcomes in acute [8, 49, 50, 56] and chronic [48, 54, 55, 58] stroke patients. These were then followed by randomized control trials that confirmed the positive outcomes of FET in acute [44, 57, 62] and chronic [45, 57] stroke patients. In most of discussed studies, surface FES technology has been used to deliver FET, while a percutaneous FES system has been used in studies published by Chae et al. [45, 46]. In most studies the upper limb FET has been delivered in a clinical setting with the assistance of therapists. However, a self-administered FET intervention, i.e., those that were conducted at home, has been recently explored using the NESS system [6] and a new version of the Bionic Glove [49, 58, 63].
It is important to mention that, to date, most of the clinical trials conducted using FET for grasping in the stroke population targeted individuals who had partially preserved reaching and/or grasping functions. Namely, the targeted patients typically had Chedoke McMaster Stages of Motor Recovery scores 4 and 5 or Upper Extremity Fugl-Meyer Assessment Score greater then 30, which means that they were able to place the hand voluntarily within at least 20–30 % of the hand/arm workspace and were able to initiate some or many wrist, hand, and finger movements. However, recently in randomized controlled trials, Popovic and colleagues [56, 57] investigated the use of FET for reaching and grasping in severe stroke patients, i.e., stroke patients who had Chedoke McMaster Stages of Motor Recovery scores 1 and 2 or Upper Extremity Fugl-Meyer Assessment Score ≤15. These individuals were unable to initiate or execute voluntarily any component of reaching or grasping function. Popovic et al. have shown that the FET is able to improve both reaching and grasping functions in severe stroke patients [57]. The median improvement achieved in this study in the FET group was 24.5 points on the Upper Extremity Fugl-Meyer Assessment, while the median improvement in the control group was 0 [57].
It is worth mentioning that a small study with chronic pediatric stroke patients has been carried out where FET was used to improve reaching and grasping function in this patient population [64]. Although only four individuals participated in this pilot study, the outcomes achieved were very encouraging, and they indicated that FET for upper limb could be effectively delivered in pediatric patients.
In summary, there is mounting evidence that in individuals with moderate and severe upper limb deficit, which results from stroke, FET can enable substantial improvement in their voluntary upper limb function. Also, these studies suggested that the improvements achieved are long lasting.
4.4 FET for Restoration of Upper Limb Function Following SCI
A SCI at a T1 level or above frequently results in a partial or complete loss of grasping and reaching functions. Various therapies, surgical interventions, and/or devices have been proposed to help improve those functions in individuals with SCI. Among these interventions, FES devices have shown the most promise [65]. The same neuroprostheses for grasping and reaching as discussed above have been used with the SCI population. However, almost all these devices, except for Bionic Glove, ETHZ-ParaCare neuroprosthesis, Compex Motion system, and MyndMove®, have been used with SCI subjects almost exclusively as orthotic systems and were all efficacious as orthoses.
While the benefit of FET has been intensively investigated with stroke patients, it has not been investigated as intensely with individuals who have SCI. From the above-listed FES systems that were used to deliver FET in individuals with SCI, ETHZ-ParaCare and Compex Motion systems were able to deliver both palmar and lateral grasps using the same electrode configuration. The ETHZ-ParaCare grasping neuroprosthesis was primarily used as an orthotic system. However, Mangold et al. [66] provided some evidence that a few of the SCI patients who used the device experienced a weak FET effect. A clinical trial using Bionic Grove showed that the Bionic Glove can considerably improve upper limb function in individuals with C5–C7 SCI. This study was conducted by Popovic et al. (not the author of this article) and presents the first concrete evidence that FET for grasping could be effective in SCI population [64].
In 2006, the first randomized controlled trial was carried out carefully examining the impact of FET on grasping function in individuals with traumatic C4–C7 SCI [67]. In this study, the individuals received 40 1-h FET treatments (intervention group) or 40 1-h conventional occupational therapy treatments (control group). The therapy was tested on individuals with complete and incomplete subacute (<6 months) SCI. Although this particular study was underpowered, it provided clear evidence that both individuals with complete and incomplete subacute SCI greatly benefited from the FET for grasping. This study was then followed by another phase II randomized controlled trial; FET for grasping was evaluated in individuals with incomplete, traumatic subacute C3–C7 SCI [68]. What is relevant to mention is that this was a very conservative study with respect to FET. In this study, both control and intervention groups received 1 h of conventional occupational therapy daily, as described in [67]. Then both groups were given at least a 2-h break followed by another dose of therapy where the control group got 1 h of conventional occupational therapy, and the intervention group received 1 h of FET for grasping. Both groups received therapy 5 days a week (working days) for 8 weeks (40 session days in total). At the end of the study, there were 12 subjects in the intervention group and nine in the control group. The results obtained were statistically significant and have revealed that FET dramatically improved hand function in this patient population. Also, the long-term follow-up in this study has shown that 6 months after the baseline assessment, both control and intervention groups maintained or further improved their hand function as compared to the assessments performed at discharge from the study [69]. In other words, this study suggests that the changes in the hand function produced by FET are dramatic, and they persist over time. Recently, a phase I randomized control trial study was performed using FET for grasping in chronic (>24 months) incomplete SCI individuals [70]. Forty 1-h sessions of FET (intervention group) were compared against 40 1-h sessions of conventional occupational therapy (control group). The results of the study showed that the individuals who received FET improved considerably better then the individuals who had the same dose of conventional occupational therapy.
In summary, there is mounting evidence that individuals with incomplete C3–C7 SCI, both chronic and subacute, can benefit from the FET for grasping. The existing studies also suggest that early engagement in the FET would result in better outcomes compared to later engagement. Also, a recently published study suggested that simple increase in intensity of conventional therapy is not able to match outcomes that were achieved with FET [71], further confirming that FET for grasping should be considered the new best practice with respect to incomplete SCI population. As for the complete SCI individuals, there is weak evidence that FET is beneficial for that population as well, if it is used early during subacute phase of rehabilitation.
4.5 Hybrid FET with Orthoses or Robotic Devices
In the past, it has been shown that FES-assisted walking has several limitations such as muscle fatigue, reduced joint torques generated using FES alone as compared to volitionally activated torques in healthy subjects, modified reflex activities, and spasticity [72]. To overcome these limitations, a combined use of FES and a mechanical brace or an orthosis has been suggested. These systems are better known as hybrid assistive systems (HAS) or hybrid orthotic systems (HOS) [27, 73, 74]. Such mechanical supports have been used mainly for safety and prevention of adverse events during standing and gait [72].
In recent years the rehabilitation robotics field has experienced rapid growth. Instead of being passive orthotic systems or braces, rehabilitation robots now have active joints and are used to help move upper and lower limbs in a physiologically correct manner, mimicking proper reaching and walking functions, respectively. Similarly, FET has been used to allow patients to execute various repetitive upper and lower limb tasks. Since both technologies have advantages and disadvantages, it was only natural to consider merging these technologies as means to overcome the disadvantages and benefit from the advantages that these two technologies offer. For example, FES systems are currently unable to generate very accurate limb movements but are able to engage flaccid and spastic muscles in task execution and generate much more significant proprioceptive and sensory feedback, which is critical for retraining the neuromuscular system. Specifically, Takeoka et al. [75] recently demonstrated that muscle spindle feedback is critical and probably essential for the functional recovery following SCI. On the other hand, robotic systems are very good in executing accurate limb movements, but, in general, these systems themselves do not generate muscle activations. However, in order for the muscles to produce proper afferent feedback, in particular proper muscle spindle feedback, they need to be contracted at a proper level of muscle tension, and the their tension needs to be regulated according to the join angle. The FES systems are able to achieve that, although not as good as the intact central nervous system does. The robotic systems, because of the nature of this technology, have neither capability to produce desired muscle tension nor are able to regulate muscle tension as a function of joint angle. In robotic systems, the more substantial afferent feedback can be produced if the consumer has tone. However, it is not clear if the afferent feedback produced under such circumstances matches the one that the intact central nervous system would naturally produce. Therefore, it has been suggested that the combination of FES with robotic devices will enhance the therapeutic effects of both interventions. A recent study by Freeman et al. [76] has proposed a robotic device for reaching movement with upper limbs that can be combined with FES. The study tested and confirmed the accuracy of the trajectory that the robotic system executed with 18 healthy subjects using FES applied to the triceps muscle. The results confirmed the efficacy of a combined robotic device and FES system and showed the feasibility of the proposed device. The same authors started to test the system with five stroke patients in treatment sessions comprised of up to 25 1-h visits. For walking, Stauffer et al. [77] developed a hybrid robotic and FES system (WalkTrainer). The robotic device consisted of leg and pelvic orthoses, active bodyweight support, and a mobile frame that allowed the user to perform walking therapy during overground walking. The system also had a closed-loop controlled FES system. This system was tested with six paraplegic patients, and its feasibility as a rehabilitation tool was confirmed.
Very recently, a new hybrid robotics-FET system has been proposed for the restoration of grasping and reaching after stroke [78]. The system combines ALEX (an upper limb exoskeleton), which provides the reaching support [79], together with a FES system that uses electrode arrays to provide grasp control. Real reaching and grasping tasks can be achieved by using a satellite robot, which presents the objects to be grasped. Specific rehabilitation tasks can be implemented by taking advantage of the possibility to quantify the support needed by patients and to modulate both the mechanical and FES support over the reachable workspace.
Hybrid rehabilitation systems, consisting of a robotic device and an FES system, are not a new idea. However, this idea has become a more attractive and realistic solution in recent years. It is very likely that in the near future, we will see more devices that are combining FES and robotic technologies to develop advanced neurorehabilitation tools and interventions.
5 Potential Mechanisms of FET
At the present time, the exact mechanisms responsible for the observed FET effect are not known. However, a few hypotheses have been proposed that may provide at least a partial explanation of the FET effect.
Three possible “peripheral” mechanisms might be considered. At first, FET may improve the muscle functions in the remaining motor units through muscle training and strengthening. However, this does not necessarily happen only during FET; other training mechanisms can be used to improve muscle strength and endurance. Second, FET may improve the flexibility and range of motion of the affected limb/joints, and as a consequence, the voluntary function may be improved. However, stretching during physiotherapy should be able to generate similar results. Third, FET reduces the amount of spasticity in the affected limb, and by doing so it may improve the motor function. Although it has been shown in the past that FET does improve the spasticity [80, 81], the FET effect has been observed even in the affected limbs that did not have spasticity. Thus, although all three above-listed mechanisms may be possible, they alone could not account for the observed FET effect.
It has been reported that cortical reorganization can occur following stroke recovery [82]. As FES activates both motor and sensory nerve fibers, high-frequency sensory stimulation may be capable of modifying cortical connectivity [83]. Thus, through forced repetitive movements, FET may promote the neuroplasticity in the central nervous system through sensory nerve stimulation [84].
In addition to the cortical reorganization mechanism, Rushton [3] suggested a hypothesis that accounts for the neuroplasticity effect as uniquely due to FES. Electrical stimulation of a motor nerve fiber generates both an orthodromic (centrifugal) and an antidromic (centripetal) impulse. When the voluntary, descending command comes down from the brain to the spinal motor neuron, it can meet the antidromic impulse at the motor neuron during FES. This coincidence of two impulses at the spinal motor neuron can strengthen the synaptic connection via Hebb’s rule. This enhancement of the synaptic connection would increase the efficacy of the voluntary, descending command to activate impaired muscle in individuals with stroke and SCI. Recent results that showed a facilitation of motor evoked potential using TMS after FES support this hypothesis [85, 86]. However, it should be noted that a facilitation of motor evoked potential using simultaneous TMS and FES (i.e., spinal paired associative stimulation) is not always guaranteed [87] and that the above Rushton’s hypothesis yet needs to be confirmed.
Another hypothesis that could also explain the mechanisms behind FET is the one proposed by Popovic et al. [34–57, 67–69]. If a subject, who attempts to execute a motor task, is assisted with the FET to carry out that task, she/he is effectively voluntarily generating the motor command (desire to move the arm, leg, etc.; i.e., command input). In this situation, FET is providing afferent feedback (system’s output), indicating that the command was executed successfully. By providing both the command input and system’s output to the central nervous system repetitively for prolonged periods of time, this type of treatment facilitates functional reorganization and retraining of intact parts of the central nervous system and allows them to take over the function of the damaged part of the central nervous system. It is important to add that during the FET, the subjects perform motor tasks repetitively. The combination of performing diverse and meaningful tasks with high repetition and with a subject’s persistent active engagement (i.e., the subject has to devote 100 % of her/his attention to the tasks performed) may play a critical role in retraining voluntary motor function. This hypothesis and use of FET are fully in tune with recent findings in the field of neuroplasticity and suggest that FET is potentially another effective method that can be used to retrain the neuromuscular system.
Recently a study by Takeoka et al. [75] demonstrated very elegantly that muscle spindle feedback is critical and probably essential for the functional recovery following SCI. They have shown that if muscle spindles are “removed out of the rehabilitation process” that the animal trained is unable to recover its function. Since FET fully engages muscle spindle feedback system during therapy, it is very likely that the high intensity muscle spindle feedback produced by the FET is contributing to the process of recovery of voluntary function. Please note that in the past, it has been frequently suggested that the FES/FET does not activate muscle fibers in physiologically correct manner, i.e., that the fast-twitch muscle fibers are recruited first followed by the slow-twitch muscle fibers [88]. This reverse order of muscle fiber activation could impact the order in which muscle spindle feedback is presented to the central nervous system following FET. However, recent experiments have shown that this notion of reverse muscle fiber recruitment during FES/FET is incorrect [88], suggesting that the order in which muscle spindle feedback is delivered to the central nervous system should be reasonably close to the natural one. More comprehensive discussion about the sensory feedback systems that may be engaged during FET and how they may contribute to the improvement in the voluntary function following FET can be found in Prochazka’s recent article [89].
The final hypothesis that Popovic and his team in Toronto proposed previously suggests that it is possible that the phylogenetically older brain structures, which are equally able of control limbs, may be engaged during FET training. Specifically, he hypothesized that FET for reaching and grasping, when it is applied to stroke patients, engages phylogenetically older brain structures and retrains them to perform reaching and grasping tasks, instead of retraining the cortical structures. Recently, Kawai et al. [90] actually demonstrated in rodents that the motor cortex is required for learning new tasks, but that it is not required for execution of already mastered forelimb motor tasks. This finding suggests that Popovic’s hypothesis may be correct, but this hypothesis still needs to be properly verified.
In any event, the carry-over effect is probably multifactorial and needs to be fully examined. However, what is certain is that the FET is an effective method for restoring voluntary upper and lower limb functions in individuals following stroke and SCI. It is our impression that the FET is a very promising intervention that is only now being seriously examined and has the potential to revolutionize the way we rehabilitate individuals with diverse neuromuscular disorders.
6 Comparison of FET and Robotic Therapies
To the best of our knowledge, a proper comparison of the FET and robotic therapy was not conducted to date. The only comparison that we are aware of is the one conducted by Hess at al. [91], where Bi-Many-Track system (Reha-Stim, Germany) (www.reha-stim.de) was compared to electrical stimulation of the wrist extensor muscles. The study was performed in subacute stroke individuals (between 4 and 8 weeks following stroke) patients, which Upper Extremity Fugl-Meyer scores were less than 18. Bi-Many-Track was used to deliver therapy to the wrist (flexion/extension and pronation/supination), elbow (flexion/extension), and indirectly to shoulder (flexion/extension). The electrical stimulation was delivered to wrist extensors only and was activated manually or using biofeedback approach. Although both therapies were delivered over 30 sessions that were 20 min long (10 h of therapy in total), Bi-Many-Track delivered between 12,000 and 24,000 movement repetitions (spread over different joints) and electrical stimulation delivered between 1,800 and 2,400 wrist flexion/extension repetitions. Please note that the electrical stimulation intervention used in this study does not belong to the FET variety of therapies but rather to a muscle strengthening type of interventions. The study results suggest that at discharge, participants who received Bi-Many-Track had improvement in Upper Extremity Fugl-Meyer scores of 16.7 points, while the participants who received electrical stimulation had improvement in Upper Extremity Fugl-Meyer scores of 3.1 points.
We are hopeful that this study will inspire the research community to start comparing equal dose FET and robotic therapy, which are training the same joints and muscle groups, and are delivering equal dose/intensity of intervention.
7 Limitations and Perspectives
This chapter summarizes the research findings regarding the effects of FET in individuals with stroke and SCI. The findings to date clearly show that FET for reaching and grasping is a therapeutic modality that should be implemented in every rehabilitation institution that is treating patients with stroke and SCI. The results obtained in a number of randomized control trials to date clearly point out that FET for upper limb should not be ignored any longer. There is also considerable evidence to support the use of FET as a therapeutic modality to treat drop-foot problem in both stroke and incomplete SCI populations. There are a couple of FES systems on the market that can be used to deliver FET for drop-foot and grasping, and physiotherapists and occupational therapists should take advantage of this technology. Presently, few teams in the world are investigating use of more complex FES systems (6–16 channels FES systems that stimulate muscles in one of both legs in a physiologically appropriate manner) for retraining voluntary walking function in stroke and incomplete SCI populations. Although comprehensive randomized control trials have not been completed yet with either patient population, preliminary findings are encouraging.
The results obtained to date suggest that FET can be used effectively with both chronic and subacute stroke and SCI patients. However, the results published to date suggest that FET produces better results if it is applied during early rehabilitation, i.e., during subacute phase following injury. Further, the effect of FET has shown good results in individuals with chronic complete and incomplete SCI and stroke subjects. However, to date, statistically significant results have only been obtained with chronic stroke and incomplete SCI patients. It should be noted that FET therapy does not require any voluntary movement in the affected limb as an indication for the therapy. In other words, FET can be applied to individuals who are profoundly paralyzed (i.e., cannot move the limb at all), and one can expect to see at least partial recovery of the limb function at the end of the FET.
As the surface FES technology is continuously improving and delivery methods for FET are evolving due to system’s miniaturization, better stimulation electrodes, and better stimulation protocols, it is foreseeable that, in next 10–15 years, FET will become one of the dominant interventions for upper and lower limb rehabilitation. Many FET systems are already commercialized, and many more are in the process of being developed and/or commercialized. Thus, we feel very confident that FET filed is only beginning to evolve, and that, in the future, it may become one of the key therapeutic interventions not only for patients with stroke and SCI but also for patients with other neuromuscular disorders.
References
Reichel M, Breyer T, Mayr W, Rattay F. Simulation of the three-dimensional electrical field in the course of functional electrical stimulation. Artif Organs. 2002;26:252–5.
Kern H, Hofer C, Mödlin M, Forstner C, Raschka-Högler D, Mayr W, Stöhr H. Denervated muscles in humans: limitations and problems of currently used functional electrical stimulation training protocols. Artif Organs. 2002;26:216–8.
Rushton D. Functional electrical stimulation and rehabilitation—an hypothesis. Med Eng Phys. 2003;25:75–8.
Kuhn A, Keller T, Micera S, Morari M. Array electrode design for transcutaneous electrical stimulation: a simulation study. Med Eng Phys. 2009;31:945–51.
Micera S, Keller T, Lawrence M, Morari M, Popović DB. Wearable neural prostheses. Restoration of sensory-motor function by transcutaneous electrical stimulation. IEEE Eng Med Biol Mag. 2010;29:64–9.
Popović DB, Popović MB. Automatic determination of the optimal shape of a surface electrode: selective stimulation. J Neurosci Methods. 2009;178:174–81.
Smith B, Tang Z, Johnson MW, Pourmehdi S, Gazdik MM, Buckett JR, Peckham PH. An externally powered, multichannel, implantable stimulator-telemeter for control of paralyzed muscle. IEEE Trans Biomed Eng. 1998;45:463–75.
Popovic MB, Popovic DB, Sinkjaer T, Stefanovic A, Schwirtlich L. Restitution of reaching and grasping promoted by functional electrical therapy. Artif Organs. 2002;26:271–5.
Davis R, Sparrow O, Cosendai G, Burridge JH, Turk R, Wulff C, Schulman J. Post-stroke arm rehabilitation using 5–7 implanted microstimulators: implantation procedures, safety and efficacy. 12th Ann Conf Int FES Soc, Nov 2007, Philadelphia.
Waters RL. The enigma of “carry-over”. Int Rehabil Med. 1984;6:9–12.
Merletti R, Acimovic R, Grobelnik S, Cvilak G. Electrophysiological orthosis for the upper extremity in hemiplegia: feasibility study. Arch Phys Med Rehabil. 1975;56:507–13.
Popovic MR, Popovic DB, Keller T. Neuroprostheses for grasping. Neurol Res. 2002;24:443–52.
Taylor PN, Burridge JH, Dunkerley AL, Wood DE, Norton JA, Singleton C, Swain ID. Clinical use of the Odstock dropped foot stimulator: its effect on the speed and effort of walking. Arch Phys Med Rehabil. 1999;80:1577–83.
Stein RB, Everaert DG, Thompson AK, Chong SL, Whittaker M, Robertson J, Kuether G. Long-term therapeutic and orthotic effects of a foot drop stimulator on walking performance in progressive and nonprogressive neurological disorders. Neurorehabil Neural Repair. 2010;24:152–67.
Hausdorff JM, Ring H. Effects of a new radio frequency-controlled neuroprosthesis on gait symmetry and rhythmicity in patients with chronic hemiparesis. Am J Phys Med Rehabil. 2008;87:4–13.
Burridge JH, Haugland M, Larsen B, Svaneborg N, Iversen HK, Christensen PB, Pickering RM, Sinkjaer T. Patients’ perceptions of the benefits and problems of using the ActiGait implanted drop-foot stimulator. J Rehabil Med. 2008;40:873–5.
Kenney L, Bultstra G, Buschman R, Taylor P, Mann G, Hermens H, Holsheimer J, Nene A, Tenniglo M, van der Aa H, Hobby J. An implantable two channel drop foot stimulator: initial clinical results. Artif Organs. 2002;26:267–70.
van Swigchem R, Vloothuis J, den Boer J, Weerdesteyn V, Geurts ACH. Is transcutaneous peroneal stimulation beneficial to patients with chronic stroke using an ankle-foot orthosis? A within-subjects study of patients’ satisfaction, walking speed and physical activity level. J Rehabil Med. 2010;42:117–21.
Daly JJ, Roenigk K, Holcomb J, Rogers JM, Butler K, Gansen J, McCabe J, Fredrickson E, Marsolais EB, Ruff RL. A randomized controlled trial of functional neuromuscular stimulation in chronic stroke subjects. Stroke. 2006;37:172–8.
Burridge JH, Taylor PN, Hagan SA, Wood DE, Swain ID. The effects of common peroneal stimulation on the effort and speed of walking: a randomized controlled trial with chronic hemiplegic patients. Clin Rehabil. 1997;11:201–10.
Granat MH, Maxwell DJ, Ferguson AC, Lees KR, Barbenel JC. Peroneal stimulator; evaluation for the correction of spastic drop foot in hemiplegia. Arch Phys Med Rehabil. 1996;77:19–24.
Kantrowitz A. Electronic physiological aids: A report of the Maimonides Hospital. Maimonides Hospital, Brooklyn. 1960.
Strojnik P, Kralj A, Ursic I. Programmed six-channel electrical stimulator for complex stimulation of leg muscles during walking. IEEE Trans Biomed Eng. 1979;26:112–6.
Kralj A, Bajd T, Turk R. Enhancement of gait restoration in spinal injured patients by functional electrical stimulation. Clin Orthop Relat Res. 1988;233:34–43.
Graupe D, Davis R, Kordylewski H, Kohn K. Ambulation by traumatic T4–12 paraplegics using functional neuromuscular stimulation. Crit Rev Neurosurg. 1998;8:221–31.
Graupe D, Kohn KH. Functional neuromuscular stimulator for short-distance ambulation by certain thoracic-level spinal-cord-injured paraplegics. Surg Neurol. 1998;50:202–7.
Popovic D, Tomović R, Schwirtlich L. Hybrid assistive system—the motor neuroprosthesis. IEEE Trans Biomed Eng. 1989;36:729–37.
Solomonow M, Baratta R, Hirokawa S, Rightor N, Walker W, Beaudette P, Shoji H, D’Ambrosia R. The RGO generation II: muscle stimulation powered orthosis as a practical walking system for thoracic paraplegics. Orthopedics. 1989;12:1309–15.
Bailey SN, Hardin EC, Kobetic R, Boggs LM, Pinault G, Triolo RJ. Neurotherapeutic and neuroprosthetic effects of implanted functional electrical stimulation for ambulation after incomplete spinal cord injury. J Rehabil Res Dev. 2010;47:7–16.
Davis JA, Triolo RJ, Uhlir J, Bieri C, Rohde L, Lissy D, Kukke S. Preliminary performance of a surgically implanted neuroprosthesis for standing and transfers—where do we stand? J Rehabil Res Dev. 2001;38:609–17.
Davis JA, Triolo RJ, Uhlir JP, Bhadra N, Lissy DA, Nandurkar S, Marsolais EB. Surgical technique for installing an eight-channel neuroprosthesis for standing. Clin Orthop Relat Res. 2001;385:237–52.
Hardin E, Kobetic R, Murray L, Corado-Ahmed M, Pinault G, Sakai J, Bailey SN, Ho C, Triolo RJ. Walking after incomplete spinal cord injury using an implanted FES system: a case report. J Rehabil Res Dev. 2007;44:333–46.
Johnston TE, Betz RR, Smith BT, Benda BJ, Mulcahey MJ, Davis R, Houdayer TP, Pontari MA, Barriskill A, Creasey GH. Implantable FES system for upright mobility and bladder and bowel function for individuals with spinal cord injury. Spinal Cord. 2005;43:713–23.
Popovic MR, Keller T. Modular transcutaneous functional electrical stimulation system. Med Eng Phys. 2005;27:81–92.
Thrasher TA, Flett HM, Popovic MR. Gait training regimen for incomplete spinal cord injury using functional electrical stimulation. Spinal Cord. 2006;44:357–61.
Pappas IP, Popovic MR, Keller T, Dietz V, Morari M. A reliable gait phase detection system. IEEE Trans Neural Sys Rehabil Eng. 2001;9:113–25.
Bajd T, Kralj A, Stefancic M, Lavrac N. Use of functional electrical stimulation in the lower extremities of incomplete spinal cord injured patients. Artif Organs. 1999;23:403–9.
Wieler M, Stein R, Ladouceur M, Whittaker M, Smith A, Naaman S, Barbeau H, Bugaresti J, Aimone E. Multicenter evaluation of electrical stimulation systems for walking. Arch Phys Med Rehabil. 1999;80:495–500.
Field-Fote EC, Roach KE. Influence of a locomotor training approach on walking speed and distance in people with chronic spinal cord injury: a randomized clinical trial. Phys Ther. 2011;91(1):48–60.
Field-Fote EC, Lindley SD, Sherman AL. Locomotor training approaches for individuals with spinal cord injury: a preliminary report of walking-related outcomes. J Neurol Phys Ther. 2005;29(3):127–37.
Giangregorio L, Craven BC, Richards K, Kapadia N, Hitzig SL, Masani K, Popovic MR. A randomized trial of functional electrical stimulation for walking in incomplete spinal cord injury: effects on body composition. J Spinal Cord Med. 2012;35(5):351–60.
Hitzig SL, Craven BC, Panjwani A, Kapadia N, Giangregorio LM, Richards K, Masani K, Popovic MR. A randomized trial of functional electrical stimulation therapy for walking in incomplete spinal cord injury: effects on quality of life and community participation. Top Spinal Cord Inj Rehabil. 2013;19(4):245–58.
Kapadia N, Masani K, Craven BC, Giangregorio LM, Hitzig SL, Richards K, Popovic MR. A randomized trial of functional electrical stimulation for walking in incomplete spinal cord injury: effects on walking competency. J Spinal Cord Med. 2014;37(5):511–24.
Chae J, Bethoux F, Bohine T, Dobos L, Davis T, Friedl A. Neuromuscular stimulation for upper extremity motor and functional recovery in acute hemiplegia. Stroke. 1998;29:975–9.
Chae J, Harley M, Hisel T, Corrigan C, Demchak J, Wong Y-T, Fang Z-P. Intramuscular electrical stimulation for upper limb recovery in chronic hemiparesis: an exploratory randomized clinical trial. Neurorehabil Neural Repair. 2009;23:569–78.
Chae J, Hart R. Intramuscular hand neuroprosthesis for chronic stroke survivors. Neurorehabil Neural Repair. 2003;17:109–17.
Francisco G, Chae J, Chawla H, Kirshblum S, Zorowitz R, Lewis G, Pang S. Electromyogram-triggered neuromuscular stimulation for improving the arm function of acute stroke survivors: a randomized pilot study. Arch Phys Med Rehabil. 1998;79:570–5.
Hendricks HT, IJzerman MJ, de Kroon JR, in’t Groen FA, Zilvold G. Functional electrical stimulation by means of the ‘Ness Handmaster Orthosis’ in chronic stroke patients: an exploratory study. Clin Rehabil. 2001;15:217–20.
Kowalczewski J, Gritsenko V, Ashworth N, Ellaway P, Prochazka A. Upper-extremity functional electric stimulation-assisted exercises on a workstation in the subacute phase of stroke recovery. Arch Phys Med Rehabil. 2007;88:833–9.
Popovic D, Popovic M, Sinkjaer T, Stefanovic A, Schwirtlich L. Therapy of paretic arm in hemiplegic subjects augmented with a neural prosthesis: a cross-over study. Can J Physiol Pharmacol. 2004;82:749–56.
Popović D, Stojanović A, Pjanović A, Radosavljević S, Popović M, Jović S, Vulović D. Clinical evaluation of the bionic glove. Arch Phys Med Rehabil. 1999;80:299–304.
Prochazka A, Gauthier M, Wieler M, Kenwell Z. The bionic glove: an electrical stimulator garment that provides controlled grasp and hand opening in quadriplegia. Arch Phys Med Rehabil. 1997;78:608–14.
Rebersek S, Vodovnik L. Proportionally controlled functional electrical stimulation of hand. Arch Phys Med Rehabil. 1973;54:378–82.
Sullivan JE, Hedman LD. A home program of sensory and neuromuscular electrical stimulation with upper-limb task practice in a patient 5 years after a stroke. Phys Ther. 2004;84:1045–54.
Sullivan JE, Hedman LD. Effects of home-based sensory and motor amplitude electrical stimulation on arm dysfunction in chronic stroke. Clin Rehabil. 2007;21:142–50.
Popovic MR, Thrasher TA, Zivanovic P, Takaki M, Hajek P. Neuroprosthesis for retraining reaching and grasping functions in severe hemiplegic patients. Neuromodulation. 2005;8:58–72.
Thrasher TA, Zivanovic V, McIlroy W, Popovic MR. Rehabilitation of reaching and grasping function in severe hemiplegic patients using functional electrical stimulation therapy. Neurorehabil Neural Repair. 2008;22:706–14.
Gritsenko V, Prochazka A. A functional electric stimulation-assisted exercise therapy system for hemiplegic hand function. Arch Phys Med Rehabil. 2004;85:881–5.
Popovic MR, Keller T, Pappas IP, Dietz V, Morari M. Surface-stimulation technology for grasping and walking neuroprosthesis. IEEE Eng Med Biol Mag. 2001;20:82–93.
Popović MB. Control of neural prostheses for grasping and reaching. Med Eng Phys. 2003;25:41–50.
Glanz M, Klawansky S, Stason W, Berkey C, Chalmers TC. Functional electrostimulation in poststroke rehabilitation: a meta-analysis of the randomized controlled trials. Arch Phys Med Rehabil. 1996;77:549–53.
Cauraugh JH, Kim S. Two coupled motor recovery protocols are better than one: electromyogram-triggered neuromuscular stimulation and bilateral movements. Stroke. 2002;33:1589–94.
Ring H, Rosenthal N. Controlled study of neuroprosthetic functional electrical stimulation in sub-acute post-stroke rehabilitation. J Rehabil Med. 2005;37:32–6.
Kapadia NM, Nagai MK, Zivanovic V, Bernstein J, Woodhouse J, Rumney P, Popovic MR. Functional electrical stimulation therapy for recovery of reaching and grasping in severe chronic paediatric stroke patients. J Child Neurol. 2014;29(4):493–9.
Popovic MR, Thrasher TA. Neuroprostheses, Encyclopedia of biomaterials and biomedical engineering. New York: Marcel Dekker Inc.; 2004. p. 1056–65.
Mangold S, Keller T, Curt A, Dietz V. Transcutaneous functional electrical stimulation for grasping in subjects with cervical spinal cord injury. Spinal Cord. 2005;43:1–13.
Popovic MR, Thrasher TA, Adams ME, Takes V, Zivanovic V, Tonack MI. Functional electrical therapy: retraining grasping in spinal cord injury. Spinal Cord. 2006;44:143–51.
Popovic MR, Kapadia N, Zivanovic V, Furlan J, Craven C, McGillivray C. Functional electrical stimulation therapy for restoring voluntary grasping function in patietns with sub-acute incomplete tetraplegia: a randomized single-blind clinical trial. Neurorehabil Neural Repair. 2011;25(5):433–42.
Kapadia NM, Zivanovic V, Furlan J, Craven BC, McGillivray C, Popovic MR. Toronto Rehabilitation Institute’s functional electrical stimulation therapy for grasping in traumatic incomplete spinal cord injury: randomized control trial. Artif Organs. 2011;35(3):212–6.
Kapadia N, Zivanovic V, Popovic MR. Restoring voluntary grasping function in individuals with incomplete chronic spinal cord injury: pilot study. Top Spinal Cord Inj Rehabil. 2013;19(4):279–87.
Desai N, Bagher S, Popovic MR. Influence of different rehabilitation therapy models on patient outcomes: hand functiontherapy in individuals with incomplete SCI. J Spinal Cord Med. 2014;37(6):734–43.
Tomović R, Popović D. Nonanalytical methods for motor control. World Scientific Publishing Company; Singapore; 1995.
Andrews BJ, Baxendale RH, Barnett R, Phillips GF, Yamazaki T, Paul JP, Freeman PA. Hybrid FES orthosis incorporating closed loop control and sensory feedback. J Biomed Eng. 1988;10:189–95.
Solomonow M. Biomechanics and physiology of a practical powered walking orthosis for paraplegics. In: Stein RB, Peckham P, Popovic D, editors. Neural prostheses: replacing motor function after disease or disability. Oxford University Press; London; 1992. p. 202–32.
Takeoka A, Vollenweider I, Courtine G, Arber S. Muscle spindle feedback directs locomotor recovery and circuit reorganization after spinal cord injury. Cell. 2014;159(7):1626–39.
Freeman C, Hughes A, Burridge J, Chappell P, Lewin P, Rogers E. Iterative learning control of FES applied to the upper extremity for rehabilitation. Control Eng Pract. 2009;17:368–81.
Stauffer Y, Allemand Y, Bouri M, Fournier J, Clavel R, Metrailler P, Brodard R, Reynard F. The WalkTrainer—a new generation of walking reeducation device combining orthoses and muscle stimulation. IEEE Trans Neural Sys Rehabil Eng. 2009;17:38–45.
Crema A, Mancuso M, Frisoli A, Salsedo F, Raschellà F, Micera S. A hybrid NMES-exoskeleton for real objects interaction. IEEE Neural Eng Conference. 2015.
Bergamasco M. An exoskeleton structure for physical interaction with a human being. PCT Application N. W02013186701 (A1). 2013.
Granat MH, Ferguson AC, Andrews BJ, Delargy M. The role of functional electrical stimulation in the rehabilitation of patients with incomplete spinal cord injury—observed benefits during gait studies. Paraplegia. 1993;31:207–15.
Kawashima N, Popovic MR, Zivanovic V. Effect of intensive functional electrical stimulation therapy on the upper limb motor recovery after stroke: single case study of a chronic stroke patient. Physiother Can. 2013;65(1):20–8.
Weiller C, Ramsay SC, Wise RJ, Friston KJ, Frackowiak RS. Individual patterns of functional reorganization in the human cerebral cortex after capsular infarction. Ann Neurol. 1993;33:181–9.
Ridding MC, Brouwer B, Miles TS, Pitcher JB, Thompson PD. Changes in muscle responses to stimulation of the motor cortex induced by peripheral nerve stimulation in human subjects. Exp Brain Res. 2000;131:135–43.
Chae J, Yu D. Neuromuscular stimulation for motor relearning in hemiplegia. Crit Rev Phys Rehabil Med. 1999;11:208–29.
Thompson A, Doran B, Stein R. Short-term effects of functional electrical stimulation on spinal excitatory and inhibitory reflexes in ankle extensor and flexor muscles. Exp Brain Res. 2006;170:216–26.
Thompson AK, Stein R. Short-term effects of functional electrical stimulation on motor-evoked potentials in ankle flexor and extensor muscles. Exp Brain Res. 2004;159:491–500.
McGie SC, Masani K, Popovic MR. Failure of spinal paired associative stimulation to induce neuroplasticity in the human corticospinal tract. J Spinal Cord Med. 2014;37(5):565–74.
Gregory CM, Bickel CS. Recruitment patterns in human skeletal muscle during electrical stimulation. Phys Ther. 2005;85(4):358–64.
Prochazka A. Sensory control of normal movement and of movement aided by neural prostheses. J Anat. 2015;227(2):167–77.
Kawai R, Markman T, Poddar R, Ko R, Fantana AL, Dhawale AK, Kampff AR, Ölveczky BP. Motor cortex is required for learning but not for executing a motor skill. Neuron. 2015;86(3):800–12.
Hesse S, Werner C, Pohl M, Rueckriem S, Mehrholz J, Lingnau ML. Computerized arm training improves the motor control of the severely affected arm after stroke: a single-blinded randomized trial in two centers. Stroke. 2005;36:1960–6.
Popovic MR, Curt A, Keller T, Dietz V. Functional electrical stimulation for grasping and walking: indications and limitations. Spinal Cord. 2001;39:403–12.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing
About this chapter
Cite this chapter
Popovic, M.R., Masani, K., Micera, S. (2016). Functional Electrical Stimulation Therapy: Recovery of Function Following Spinal Cord Injury and Stroke. In: Reinkensmeyer, D., Dietz, V. (eds) Neurorehabilitation Technology. Springer, Cham. https://doi.org/10.1007/978-3-319-28603-7_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-28603-7_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-28601-3
Online ISBN: 978-3-319-28603-7
eBook Packages: MedicineMedicine (R0)