Abstract
Early laparoscopic cholecystectomy (LC) after endoscopic retrograde cholangio-pancreaticography (ERCP) is beneficial for patients with gall stone disease (GSD) and common bile duct (CBD) stones. However, there are no clear guidelines for the optimal timing of surgical intervention. This study aimed to assess the feasibility and clinical outcomes of the same-day sequential approach—ERCP followed by LC for management of choledocholithiasis and concomitant cholelithiasis. Between March 2018 and November 2019, 24 patients diagnosed with choledocholithiasis and concomitant cholelithiasis underwent ERCP-guided biliary clearance followed by LC sequentially on the same day. ERCP was done in the endoscopy suite and followed by LC in the operation theatre. Both procedures were performed by the same endoscopist-cum-laparoscopic surgeon proficient in advanced endoscopy and laparoscopy. Success rate, ERCP findings, operative findings, logistic issues, and complications were recorded and analysed. Technical success for ERCP and LC, both were 100%. No major complications like bleeding, perforation, pancreatitis, or mortality were encountered post-ERCP. The rate of conversion to open cholecystectomy was 0%. Post-operative self-resolving minor bile leak was encountered in 1 patient (4.1%) who was managed conservatively. The mean time for ERCP and LC was 33.33 min and 80.4 min, respectively. The mean time interval between the two procedures was 51 min. The mean post-procedure hospital stay was 3.7 days. This study demonstrated a safe, effective, and feasible same-day sequential approach—ERCP-guided biliary clearance followed by LC—in selected patients with choledocholithiasis with concomitant cholelithiasis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Symptomatic gallstone disease is one of the most common gastrointestinal surgical problems faced worldwide, and about 10–18% of patients with gallbladder stones have common bile duct (CBD) stones at the time of cholecystectomy [1, 2]. While various minimally invasive approaches have been described, there is no consensus on the optimum strategy for the management of gallbladder stones with concomitant CBD stones. Minimally invasive surgery offers faster recovery, lesser post-operative pain, and a shorter length of hospital stay. Reducing the length of stay (LOS) in hospitals perhaps remains one of the most cost-effective approaches to reducing the healthcare expenditure of patients. ERCP followed by LC is the most commonly practised method in most hospitals worldwide [3]. Traditionally, these procedures were performed on different days and often with an unnecessary delay. This was in lieu of the anticipated fear arising from post-ERCP-related complications including pancreatitis. However, advanced technology and endoscopic expertise have reduced the rate of such complications. Performing ERCP and LC on the same day is one potential method of decreasing LOS and potentially reducing healthcare expenditures. The benefits of a single-stage approach in the management of cholelithiasis and choledocholithiasis have been studied concerning laparoscopic CBD exploration (LCBDE), or LC with intra-operative ERCP [4,5,6], but the clinical application of a same-day sequential approach—ERCP followed by LC— has not been adequately analysed. Such a method may provide an alternative approach to managing gallstones and CBD stones, especially in centres where performing laparoscopic CBD exploration or intra-operative ERCP during LC may still not be feasible.
This study aimed to assess the feasibility and clinical outcomes of the same-day sequential approach—ERCP-guided biliary clearance followed by LC in the management of choledocholithiasis with concomitant cholelithiasis. Special emphasis was laid on evaluating the intra-procedural difficulties faced, post-operative complications, and logistical issues encountered in conducting these same-day sequential interventions.
Patients and Methods
This case series analysis was conducted in the Department of Surgery at MGM Medical College and Hospital (Aurangabad, India) between March 2018 and November 2019. Appropriate clearances and approvals were sought from the Institutional Ethics Committee.
Patients presenting to the hospital with choledocholithiasis and concomitant cholelithiasis on an accrual basis were evaluated clinically and with radiological and biochemical investigations. A liver function test was part of the routine biochemical workup. Diagnostic ultrasonography of the abdomen (USG) was performed in all patients, whereas contrast-enhanced computed tomography (CECT), magnetic resonance imaging cholangiopancreatography (MRCP), or endoscopic ultrasound (EUS) were done selectively, for further assessment as clinically warranted.
After obtaining written informed consent, the patients satisfying the inclusion criteria were included in the study. The sole inclusion criterion was the presence of stone in the CBD as evidenced by imaging modalities in patients with symptomatic gallstone disease. Gallbladder wall thickness was measured in millimetres using transabdominal USG preoperatively.
Patients with severe cholangitis, large CBD stones (> 2 cm), complicated cholecystitis, gallstone pancreatitis, and unfit for general anaesthesia (GA) were excluded from the study.
The selected patients underwent ERCP followed by LC on the same day. ERCP was performed in the endoscopy suite, in the left semi-prone position under propofol sedation and CO2 insufflation. Guidewire-assisted technique was used for selective biliary cannulation. Various parameters including the duration of the procedure (time interval between scope-in and scope-out), number of attempts at guidewire insertion, inadvertent pancreatic duct cannulation, difficulties encountered, and complications were recorded. Once the biliary stone extraction was successful, a CBD stent was placed, and the patient was shifted to the operation theatre for LC. The patient’s condition during transport and the time interval between the two procedures were monitored. LC was performed using the standard 4-port technique under general anaesthesia. The total time of surgery was recorded from the time of intubation till the time of extubation. Other parameters like intra-operative difficulties faced, presence of bowel distension or adhesions, use of drains, and conversions to open cholecystectomy or any complications were noted.
A standardised post-operative care protocol was followed for all patients. An oral diet was resumed after 6 h. Serum amylase level was done 4-h post-ERCP to evaluate for pancreatitis. Complications like biliary leaks, haemorrhage, pancreatitis, and bowel injury were recorded if present. Total and post-operative hospital length of stay (LOS) was recorded.
Patients were followed up at 1-week, 4-week, and 28-week intervals. Recurrent biliary events and other complications were noted. CBD stents, if placed, were removed after 4 weeks of surgery, after excluding any residual stones on ultrasonography.
The primary outcome was studied based on parameters like the average time for ERCP and LC, the average time interval between the procedures, ERCP and LC findings, post-ERCP and post-LC complications, perioperative logistical difficulties, total and post-operative LOS (mean no. of days), and follow-up evaluation.
Results
A total of 24 patients (10 men and 14 women) underwent ERCP followed by LC by same-day sequential approach. The average age was 48.88 SD16.29 years, with 25% (n = 06) of patients belonging to the elderly age group (age > 65 years), all of whom underwent both procedures safely.
Abdominal pain was the presenting complaint in 100% of patients, whereas jaundice and fever were recorded in 62.5%, and 25% of patients, respectively. The average total bilirubin was 2.65 SD2.24 mg/dL, and the average direct bilirubin was 1.89 SD1.87 mg/dL. The largest CBD stone size in our study was 16 mm, while the average CBD stone size was 8.26 SD3.28 mm, and the average CBD diameter was 10.12 SD3.54 mm. The average GB wall thickness was calculated at 4.90 SD2.24 mm.
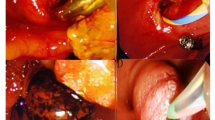
During ERCP, selective CBD cannulation and stone extraction were achieved in all the patients (100%). CBD stents were placed in all 24 patients. The average time taken for ERCP was 33.33 SD15.79 min. No major complications (bleeding, perforation, or pancreatitis) were encountered following ERCP. Asymptomatic hyperamylasaemia (Sr. amylase > 100 U/L) was noted in 5 patients, which settled spontaneously without any further intervention. Inadvertent pancreatic duct cannulation occurred in 2 patients (8.3%) with an uneventful post-ERCP course. We also studied the correlation between the number of attempts at guidewire insertion and post-procedure serum amylase levels and found a positive correlation (p = 0.024). This suggested that the more the number of guidewire insertions, the higher the possibility of hyperamylaesemia (Fig. 1). The average post-procedure serum amylase level was 74.29 SD47.93 U/L. No major logistical difficulties were encountered as both procedures were performed in the same centre and by the same surgeon. Additionally, careful patient selection and the use of CO2 insufflation reduced the occurrence of abdominal distension facilitating LC.
The average time interval between the two procedures (ERCP and LC) was 51.25 SD22.47 min. All patients were clinically monitored between the procedures and were stable.
The average time taken for LC was 80.42 SD47.82 min. The rate of conversion to open cholecystectomy was 0%. Bowel distension was also not seen in any patient (0%). Drains were placed in 9 patients (37.5%) based on intra-operative findings. One patient had a complication of a minor bile leak from the cystic duct stump which was self-limiting and managed conservatively.
Additionally, the correlation between the gallbladder wall thickness on preoperative imaging and the time taken for LC was analysed, and a positive correlation was noted (p = 0.013), indicating that increased wall thickness could contribute to longer operative times (Fig. 2).
This finding, although positive, needs to be considered in light of various confounding factors of operative time like duration, the number of attacks of cholecystitis, biliary anatomy, condition of the liver, location of stone in the gallbladder, and length of the cystic duct.
The average post-procedure LOS was 3.71 SD1.58 days. A 28-week follow-up of all the patients was recorded. There were no recurrent biliary episodes, and CBD stents were removed at 4 weeks after the procedure.
Discussion
Laparoscopic cholecystectomy for GSD is the most common surgery performed worldwide, and about 10–18% of patients undergoing LC have concomitant CBD stones [1]. The appropriate management for these patients involves clearance of the CBD stones, in addition to removal of the gallbladder to prevent recurrent biliary events. The appropriate method of dealing with CBD stones largely rests on the availability of local resources and the technical skills of the surgeon and endoscopist. Therapeutic options range from open CBD exploration to the minimally invasive laparoscopic CBD exploration (LCBDE) and the widely used ERCP. While LCDBE offers a single-stage therapy, it requires considerable surgical skill in laparoscopic suturing and additional resources [7, 8]. ERCP on the other hand is widely practised and is the most common method of dealing with choledocholithiasis worldwide [9]. Studies have shown an early LC following ERCP to be beneficial when the surgery is done before the onset of inflammation in the hepatoduodenal region. Still, no guidelines as to when the surgery should be performed have been established [10, 11]. Although same-day ERCP and LC does not take away the need for CBD exploration, it can offer the benefits of a single-stage procedure, and reduce hospital stay and costs, in patients whose CBD stones can be dealt with endoscopically [12,13,14,15].
While some authors have advocated intra-operative ERCP and LC done under the same general anaesthesia as an option, it is worthwhile to note that this method has several logistical drawbacks. It might not always be feasible to have the endoscopy team in the operating theatre, and performing ERCP on a supine patient can be technically challenging even for an experienced endoscopist [16, 17]. To overcome these challenges, we adopted an alternative same-day sequential approach—ERCP preoperatively in the endoscopy suite under propofol sedation, followed by LC in the operation theatre under general anaesthesia. This method offered several advantages—the ERCP could be performed in a comfortable semi-prone position, making cannulation easier, as we reported successful CBD cannulation in all our patients. There were no instances of post-ERCP pancreatitis, although self-resolving asymptomatic hyperamylasemia was seen in 5 patients which was probably related to inadvertent pancreatic duct cannulation and multiple attempts at guidewire insertion, as has been noted in other studies as well [11, 12, 14]. The decision to exclude patients with large CBD stones (> 2 cm) from our study could have contributed to our success in achieving complete CBD clearance in all the patients. The mean total procedure time for ERCP was 33.3 min and was comparable to that of other studies found in the literature [11, 12, 15].
Our study involved immediate shifting of patients from the endoscopy suite to the operating theatre, and the average time interval between the two procedures was only 51 min, which was much less compared to other similar studies [12, 14, 15].
Successful ERCP-guided CBD clearance and the absence of any immediate post-procedure complications enabled us to proceed with LC safely. There was no need for intra-operative cholangiography, as CBD clearance had been documented. Complete CBD clearance must be achieved endoscopically before proceeding with laparoscopic cholecystectomy, as just stenting may add to overconfidence and can lead to CBD injuries. ERCP complications may complicate laparoscopic cholecystectomy. Bowel distension has been reported in the literature to be a problem during LC after ERCP; however, the use of CO2 for insufflation during ERCP helped us to prevent any bowel distension in our study [11, 13, 14]. Laparoscopic cholecystectomy was completed safely without conversion in all the patients, which reflected results in other studies [11,12,13,14,15]. The mean operating time of 80.4 min was comparable to the literature reviewed [11,12,13,14,15]. Only 1 patient had a complication of a post-operative biliary leak which was self-limiting and managed conservatively. The average post-procedure LOS of 3.7 days was similar to other studies that had performed single-stage procedures [11, 14]. This translates into decreased hospital stay and reduced healthcare expenses as demonstrated in other similar studies [14, 15]. The absence of any mortality or long-term complications further assured us of the feasibility and safety of this novel approach. Another lesson learnt from this case series is that serum amylase may be raised without much implication to the difficulty in cholecystectomy, but if the GB wall thickness is much more, one may wait for 4 to 6 weeks and delay the cholecystectomy.
A few limitations to our study must be kept in mind. The study population was small, it was a single-centre study, and there was no control group. Larger, multi-institutional, randomised controlled trials with a wider range of inclusion criteria are needed before adopting this method as a standard of care. We also feel that further studies need to be done comparing this method to LCBDE or with LC and intra-operative ERCP before this is widely adopted.
Conclusion
In 24 patients with cholelithiasis and choledocholithiasis, endoscopic bile duct clearance followed by same-day laparoscopic cholecystectomy was performed successfully, with minimal complications and no mortality. The success of performing follow on cholecystectomy within a few hours of endo-biliary stone clearance is dependent on the hospital’s functionality. While it is preferable that biliary clearance and laparoscopic cholecystectomy are both performed on the same working day, if however, the biliary clearance is achieved during later hours of a working day, and then, cholecystectomy may be performed on the next working day within 24 h. Additionally, other parameters like increased gallbladder wall thickness, suspicion of malignancy, or lack of expert surgeons may require a delayed cholecystectomy.
References
Martin DJ, Vernon DR, and Toouli J (2006) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev (2):CD003327. https://doi.org/10.1002/14651858.CD003327.pub2
Gupta P, Bhartia VK (2005) Laparoscopic management of common bile duct stones: Our experience. Indian J Surg 67(2):94–99
Williams EJ, Green J, Beckingham I et al (2008) Guidelines on the management of common bile duct stones (CBDS). Gut 57(7):1004–1021. https://doi.org/10.1136/gut.2007.121657
Liverani A, Muroni M, Santi F et al (2013) One-step laparoscopic and endoscopic treatment of gallbladder and common bile duct stones: our experience of the last 9 years in a retrospective study. Am Surg 79(12):1243–1247
Saccomani G, Durante V, Magnolia MR et al (2005) Combined endoscopic treatment for cholelithiasis associated with choledocholithiasis. Surg Endosc 19(7):910–914. https://doi.org/10.1007/s00464-003-9314-3
Rábago LR, Vicente C, Soler F et al (2006) Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy 38(8):779–786. https://doi.org/10.1055/s-2006-944617
Rojas-Ortega S, Arizpe-Bravo D, Marín López ER et al (2003) Transcystic common bile duct exploration in the management of patients with choledocholithiasis. World J Gastrointest Surg 7(4):492–496. https://doi.org/10.1016/s1091-255x(03)00026-x
Poulose BK, Speroff T, Holzman MD (2007) Optimizing choledocholithiasis management: a cost-effectiveness analysis. Arch Surg 142(1):43–49. https://doi.org/10.1001/archsurg.142.1.43
Maple JT, Ikenberry SO, Anderson MA, ASGE Standards of Practice Committee et al (2011) The role of endoscopy in the management of choledocholithiasis. Gastrointest Endosc 74(4):731–744. https://doi.org/10.1016/j.gie.2011.04.012
Friis C, Rothman JP, Burcharth J, Rosenberg J (2018) Optimal timing for laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreatography: a systematic review. Scand J Surg 107(2):99–106. https://doi.org/10.1177/1457496917748224
Zang JF, Zhang C, Gao JY (2013) Endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy during the same session: feasibility and safety. World J Gastroenterol 19(36):6093–6097. https://doi.org/10.3748/wjg.v19.i36.6093
Akaraviputh T, Rattanapan T, Lohsiriwat V et al (2009) A same day approach for choledocholithiasis using endoscopic stone removal followed by laparoscopic cholecystectomy: a retrospective study. J Med Assoc Thai 92(1):8–11
Wild JL, Younus MJ, Torres D et al (2015) Same-day combined endoscopic retrograde cholangiopancreatography and cholecystectomy: achievable and minimizes costs. J Trauma Acute Care Surg 78(3):503–509. https://doi.org/10.1097/TA.0000000000000552
Borreca D, Bona A, Bellomo MP et al (2015) “Ultra-rapid” sequential treatment in cholecystocholedocholithiasis: alternative same-day approach to laparoendoscopic rendezvous. Updates Surg 67:449–454. https://doi.org/10.1007/s13304-015-0339-7
Mallick R, Rank K, Ronstrom C et al (2016) Single-session laparoscopic cholecystectomy and ERCP: a valid option for the management of choledocholithiasis. Gastrointest Endosc 84(4):639–645. https://doi.org/10.1016/j.gie.2016.02.050
Cavina E, Franceschi M, Sidoti F et al (1998) Laparo-endoscopic “rendezvous”: a new technique in the choledocholithiasis treatment. Hepatogastroenterology 45(23):1430–1435
ElGeidie AA (2014) Single-session minimally invasive management of common bile duct stones. World J Gastroenterol 20(41):15144–15152. https://doi.org/10.3748/wjg.v20.i41.15144
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The questionnaire and methodology for this study were approved by the Ethics Committee for Research on Human Subjects (ECRHS) of MGM’s Medical College Aurangabad (MGM-ECRHS/2018/19).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tantia, M., Suryawanshi, P. & Gandhi, A. Endoscopic Bile Duct Clearance Followed by Same-Day Cholecystectomy: a Case Series Analysis. Indian J Surg 85, 854–858 (2023). https://doi.org/10.1007/s12262-022-03597-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03597-9