Abstract
The use of positron-emitting and high-energy gamma photon-emitting radiopharmaceuticals, like fluorine-18 fluorodeoxyglucose (18F-FDG), for real-time cancer detection and surgical guidance within the operating room and for real-time guidance of diagnostic and therapeutic interventional procedures within the interventional radiology suite, has great clinical potential. This technology may allow for (1) real-time intraoperative staging of the extent of disease; (2) real-time intraoperative surgical planning and execution of the necessary and most appropriate operation, determination of the extent of surgical resection, and determination of the completeness of surgical resection; (3) real-time pathologic evaluation of intact surgical resected specimens for the confirmation of completeness of surgical resection and for surgical margin assessment; (4) real-time pathologic evaluation of diagnostically biopsied tissues for confirmation of correctness of tissue diagnosis; and (5) real-time guidance of diagnostic and therapeutic interventional procedures within the interventional radiology suite. This chapter discusses (1) the history and development of positron imaging and detection, (2) the fundamental basis for the use of 18F-FDG in positron imaging and detection strategies, (3) the inherent limitations of 18F-FDG in positron imaging and detection strategies, (4) radiation detection devices utilized during 18F-FDG-directed surgery, (5) the clinical applications of real-time 18F-FDG-directed surgery and real-time 18F-FDG-directed interventional procedures, (6) timing issues related to 18F-FDG-directed surgery, (7) the inherent challenge of in situ detection of 18F-FDG with a gamma photon detection device, and (8) occupational radiation exposure during 18F-FDG radioguided surgical procedures.
Portions of the contents of this chapter are adapted from 5 prior Open Access articles:
1. Povoski et al.: A comprehensive overview of radioguided surgery using gamma detection probe technology. World Journal of Surgical Oncology, 2009, 7:11.; doi:10.1186/1477-7819-7-11; http://www.wjso.com/content/pdf/1477-7819-7-11.pdf; © 2009 Povoski et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
2. Povoski et al.: Multimodal imaging and detection approach to 18F-FDG-directed surgery for patients with known or suspected malignancies: a comprehensive description of the specific methodology utilized in a single-institution cumulative retrospective experience. World Journal of Surgical Oncology, 2011, 9:152.; doi:10.1186/1477-7819-9-152; http://www.wjso.com/content/pdf/1477-7819-9-152.pdf; © 2011 Povoski et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
3. Povoski et al.: 18F-FDG PET/CT oncologic imaging at extended injection-to-scan acquisition time intervals derived from a single institution 18F-FDG-directed surgery experience: feasibility and quantification of 18F-FDG accumulation within 18F-FDG-avid lesions and background tissues. BMC Cancer 2014 14:453.; doi:10.1186/1471-2407-14-453; http://www.biomedcentral.com/content/pdf/1471-2407-14-453.pdf; © 2014 Povoski et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
4. Chapman et al.: Comparison of two threshold detection criteria methodologies for determination of probe positivity for intraoperative in situ identification of presumed abnormal 18F-FDG avid tissue sites during radioguided oncologic surgery. BMC Cancer. 2014 14:667.; doi:10.1186/1471-2407-14-667; http://www.biomedcentral.com/content/pdf/1471-2407-14-667.pdf; © 2014 Chapman et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
5. Povoski et al.: Feasibility of a multimodal 18F-FDG-directed lymph node surgical excisional biopsy approach for appropriate diagnostic tissue sampling in patients with suspected lymphoma. BMC Cancer 2015 15:378.; doi: 10.1186/s12885-015-1381-z; http://www.biomedcentral.com/content/pdf/s12885-015-1381-z.pdf; © 2015 Povoski et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Fluorine-18 fluorodeoxyglucose
- 18F-FDG
- Positron
- High-energy gamma photon
- Electron-positron annihilation
- Gamma photon detection
- Beta plus decay detection
- Radioguided surgery
- 18F-FDG-directed surgery
- 18F-FDG-directed interventional procedure
- Real time
- Target-to-background ratio
- Tumor-to-background ratio
- Occupational radiation exposure
1 The History of the Development of Positron Imaging and Detection
The theoretical physics framework behind the implementation of positron imaging and detection is the basic concept of electron-positron annihilation [1–6], which was first realized in the 1930s. Within any given biological system, electron-positron annihilation results when a positron (i.e., a positively charged antimatter counterpart of an electron), emitted from the nucleus of a radionuclide and travels only a few millimeters, collides with an electron (i.e., a negative charged particle) within a biological tissue and generates two resultant high-energy 511 keV gamma photons traveling in opposite directions.
The development of clinical applications of positron imaging and detection has its origins in the early 1950s [7, 8] and occurred far before the subsequent availability of fluorine-18 fluorodeoxyglucose (18F-FDG) in the late 1970s [9, 10]. The first reported clinical application of positron imaging technology in humans was published by Gordon L. Brownell and William H. Sweet at the Massachusetts General Hospital (Boston, Massachusetts, USA) in 1953 and consisted of the collection of three-dimensional data using a prototype positron imaging device on patients with brain tumors who were intravenously injected with arsenic-74 [7, 8]. Subsequent technologic advancements over the ensuing two decades culminated in the development of the first commercially available positron emission tomography (PET) device by the early 1970s for generating whole-body positron transaxial tomographs [7, 11–14], thus representing the antecedent of current-day PET imaging devices.
Currently, positron imaging and detection, in the specific form of 18F-FDG PET imaging, is a well-established cancer imaging modality that is routinely used in the clinical management of a wide variety of solid malignancies [6, 15–25]. 18F-FDG PET is generally combined with “anatomical” imaging, by way of computed tomography (CT), for attempting to maximize the geographic localization and spatial recognition of sites of 18F-FDG avidity to corresponding anatomic structures. A wide range of diagnostic utilities of 18F-FDG PET/CT have been clinically investigated and implemented [6, 15–25]. Those diagnostic clinical applications include (1) initial cancer diagnosis, (2) initial cancer staging, (3) subsequent cancer restaging, (4) therapy planning, (5) monitoring therapy response, (6) surveillance for cancer survivors, and (7) cancer screening for at-risk populations. As a step beyond these diagnostic clinical cancer imaging utilities, there has been emergent interest in the feasibility of utilizing 18F-FDG for real-time cancer detection and surgical guidance within the operating room [6, 26–76] and for real-time guidance of diagnostic and therapeutic interventional procedures within the interventional radiology suite [6, 77–95].
2 The Fundamental Basis for the Use of 18F-FDG in Positron Imaging and Detection Strategies
The radionuclide 18F has a relatively short physical half-life of approximately 110 min [6, 96, 97]. The radioactive decay pattern of 18F is predominantly (97 %) by way of positron emission (i.e., beta plus decay emission). The maximum positron radiation emission energy of 18F is approximately 635 keV, giving 18F a relatively low maximum positron radiation emission energy level as compared to other positron-emitting radionuclides. As a result, the positron emitted from the nucleus of 18F travels only a very short distance (i.e., approximately 1–2 mm) within a biological tissue before interacting/colliding with an electron (i.e., a negative charged particle). This interaction/collision of the emitted positron with the electron and the resultant electron-positron annihilation within a biological tissue generates two resultant high-energy 511 keV gamma photons traveling in opposite directions [1–6, 96, 97]. These resultant high-energy 511 keV gamma photons can travel many, many centimeters within a biological tissue. As based upon the initial positron emission and subsequent electron-positron annihilation process which occurs by 18F, the detection of 18F within biological tissues can potentially be accomplished by one of two mechanisms: (1) a direct mechanism of detection of positron emissions (i.e., beta plus decay emissions) using a beta plus detection device or (2) an indirect mechanism of detection of the resultant high-energy 511 keV gamma photons arising from electron-positron annihilation process using a gamma photon detection device [6].
Dating back to the work of Otto Heinrich Warburg in the early 1930s from the Kaiser-Wilhelm-Gesellschaft zur Förderung der Wissenschaften (Berlin-Dahlem, Germany), it has long been recognized that malignant tumors have an accelerated rate of glucose metabolism and have an increased rate of glucose transport and glucose utilization [6, 98–101]. The biochemical transport and processing mechanisms related to 18F-FDG, a non-physiologic 18F-labeled analog of glucose, within malignant cells are also well described within the scientific literature [6, 102–104]. 18F-FDG within the circulatory system is transported into cells (both malignant cells and normal cells) by a facilitated diffusion mechanism involving specific glucose transporters (i.e., GLUT transporters). Once it is within the cell, 18F-FDG is phosphorylated to 18F-FDG-6-phosphate by the enzyme hexokinase. However, unlike 18F-FDG, 18F-FDG-6-phosphate cannot be readily transported across the cellular membrane of either malignant cells or normal cells, thus essentially entrapping the 18F-FDG-6-phosphate within those cells. The enzyme glucose-6-phosphatase is responsible for dephosphorylating 18F-FDG-6-phosphate back to 18F-FDG within the intracellular environment and is present in relatively lower levels within malignant cells as opposed to normal cells. Additionally, unlike glucose-6-phosphate, 18F-FDG-6-phosphate cannot be utilized as a substrate in the metabolic steps of glycolysis, hence attributing to the further accumulation of 18F-FDG-6-phosphate within those cells. This overall process which results in the intracellular accumulation 18F-FDG-6-phosphate is thought to occur more readily in malignant cells than in normal cells secondary to the combination of the overexpression of the glucose transporters GLUT 1 and GLUT 3 by malignant cells, the higher level of hexokinase within malignant cells, and the lower level of glucose-6-phosphatase within malignant cells, thus leading to proportionally greater accumulation of 18F-FDG-6-phosphate within malignant cells as compared to normal cells. This elegantly elucidated biochemical transport and processing mechanism represents the fundamental basis behind the clinical application of 18F-FDG for the detection of malignant tumor using positron imaging and detection strategies (i.e., diagnostic PET imaging technology and various radiation detection probe technologies) [6, 98–104].
3 Inherent Limitations for the Use of 18F-FDG in Positron Imaging and Detection Strategies
Despite the fact that these biochemical transport and processing mechanisms lead to the greater accumulation of the phosphorylated form of 18F-FDG within malignant cells as compared to normal cells, there are several inherent limitations regarding the utilization of 18F-FDG for the detection of malignant tumor using positron imaging and detection strategies [6, 75, 102, 105–107]. First, 18F-FDG can readily accumulate within various normal tissues (i.e., brain, heart, mucosa and smooth muscle of the stomach, small intestines and colon, thyroid, liver, spleen, and brown fat) which typically have physiologic propensity for 18F-FDG accumulation. Second, 18F-FDG can also readily accumulate within tissues representing benign disease processes (i.e., infection, inflammation, and trauma). The basis for these first two limitations is the fact that 18F-FDG is not a cancer-specific imaging and detection agent. Third, 18F-FDG is excreted by way of the urinary tract (kidneys, ureters, and bladder), thus leading to accumulation within those structures. Fourth, alterations in tissue uptake of 18F-FDG can occur in patients with elevated blood glucose levels/impaired glucose metabolism, in patients receiving insulin, and in obese patients. An accumulation of 18F-FDG within normal tissues leads to intrinsically higher background levels of 18F-FDG activity within normal tissues located in proximity to adjacent sites of elevated 18F-FDG activity representing malignant tumor. This may be particularly challenging when the malignant tumor site itself has a relatively low level of 18F-FDG activity, leading to a relatively low target-to-background ratio (i.e., low tumor-to-background ratio) of the radiation emissions of 18F-FDG.
4 Radiation Detection Devices Utilized during 18F-FDG-Directed Surgery: Mechanisms for the Detection of 18F-FDG and Device Specifications
4.1 General Considerations
As previously mentioned, there are two mechanisms for how 18F-FDG within biological tissues can be detected by a radiation detection device: (1) the direct detection of positron emissions (i.e., beta plus decay emissions) using a beta plus detection device and (2) the detection of the resultant high-energy 511 keV gamma photons arising from electron-positron annihilation process using a gamma photon detection device [6]. The ability to successfully detect 18F-FDG within a site of suspected malignancy is highly dependent upon the specific type of radiation detection device utilized and its performance parameters [6, 108]. The most important performance parameters for any given radiation detection device are (1) overall sensitivity (i.e., efficiency, detected count rate per unit of activity), (2) spatial selectivity (i.e., radial sensitivity distribution), (3) spatial resolution (i.e., lateral sensitivity distribution), (4) energy resolution (i.e., spectral discrimination), and (5) contrast.
Radiation detection devices are categorized as either scintillation detectors or semiconductor ionization detectors [6, 108]. The basis for how a scintillation-type detection system works is that the radiation emitted from the radionuclide excites atoms within the scintillation crystal, producing visible light in proportion to the energy absorbed, and for which a photomultiplier enhances the resultant visible light and converts it into an electrical pulse which is quantified by a detection unit. Examples of inorganic scintillation materials used in scintillation detectors include thallium-activated sodium iodide (NaI[Tl]), thallium-activated cesium iodide (CsI[Tl]), sodium-activated cesium iodide (CsI[Na]), samarium-activated lutetium orthooxysilicate (LSO), bismuth germanate (BGO), cerium-activated gadolinium orthosilicate (GSO[Ce]), cerium-activated lutetium yttrium orthosilicate (LYSO[Ce]), and cerium-activated lutetium gadolinium oxyorthosilicate (LGSO[Ce]). Examples of organic (“plastic”) scintillation materials used in scintillation detectors include anthracene (C14H10), stilbene (C14H12), and naphthalene (C10H8). The basis for how a semiconductor ionization-type detection system works is that the radiation emitted from the radionuclide produces free electrons as it passes through and ionizes the semiconductor crystal, creating an electrical pulse which is quantified by a detection unit. Examples of crystalline materials used in semiconductor ionization detectors include cadmium telluride (CdTe), cadmium zinc telluride (CdZnTe), mercuric iodide (HgI2), and silicon.
There are advantageous and disadvantageous features to both the scintillation-type detection system design and the semiconductor ionization-type detection system design [6, 108]. On one hand, scintillation-type detection systems have higher sensitivity (especially for medium-energy to high-energy gamma photons) but have poorer energy resolution and scatter rejection. Likewise, scintillation-type detection probes tend to have a much bulkier and heavier probe head profile. On the other hand, semiconductor ionization-type detection systems have higher-energy resolution and scatter rejection but have lower sensitivity (especially for medium-energy to high-energy gamma photons). Likewise, semiconductor ionization-type detection probes tend to have a much more compact and light-weight probe head profile.
4.2 Gamma Photon Detection
The detector component of a gamma detection probe generally consists of an inorganic scintillator detector or a semiconductor ionization detector [6, 108]. Most commercially available handheld gamma detection probes are generally designed for detecting radioisotopes of gamma-ray energies in the low-energy emission (0–150 keV) range and medium-energy emission (150–400 keV) range, thus allowing successful detection of radioisotopes such as technetium-99 m (99mTc; 140 keV and 142 keV), indium-111 (111In; 171 keV and 247 keV), iodine-123 (123I; 159 keV), and iodine-125 (125I; 35 keV) [6, 76, 108]. However, most commercially available handheld gamma detection probes are not specifically designed for detecting resultant high-energy 511 keV gamma emissions emanating from the electron-positron annihilation process that is characteristic of high-energy gamma photon-emitting radionuclides, like 18F. As a result, there has been a recent appearance of commercially available handheld gamma detection probes that are specifically intended for attempting to detect high-energy 511 keV gamma emissions, and for which these high-energy gamma detection probes have been designated as “PET” probes. The overall weight and physical dimensions of any such “PET” probe is generally a function of the thickness of side and back shielding (with materials like lead, tungsten, gold, or platinum) and the length of collimation (i.e., extension of shielding in a forward direction beyond the distal face of the detector in the direction of the radiation source being counted) that is thought to be necessary to block adjacent background radiation, to limit the field-of-view, and to collimate the head of the probe, with the intention of limiting the area of tissue contributing to the probe count rate and of providing better spatial resolution between areas of tissue of differing radioactivity levels [6, 73, 108, 109]. All conventional attempts to improve upon the current “PET” probe design by further increasing the degree of side/back shielding or the collimation length to further block adjacent background radiation, or by increasing crystal diameter/thickness to capture a greater percentage of 511 keV gamma emissions, are generally counterproductive, as such conventional approaches will simply result in a “PET” probe configuration that is prohibitively too large in physical size, too heavy in weight, and potentially of significant greater cost. Alternatively, in order to attempt to bypass these physical barriers related to the degree of side and back shielding, collimation, and crystal diameter/thickness in designing handheld gamma detection probes specifically intended for the detection of 511 KeV gamma emissions, efforts have been redirected toward engineering more novel “PET” probe designs for which their efficacy is not dependent upon side and back shielding, collimation, or crystal diameter/thickness. Several examples of alternative design concepts for “PET” probe include secondary K-alpha x-ray fluorescence [73, 76, 109], active electronic collimation [39, 61, 64, 66, 70, 76, 110–112], and other crystal geometry designs using multiple small crystals with specific novel geometric configurations [76, 113, 114] for optimizing and maximizing background rejection capabilities. These innovative alternative design concepts for improving the efficacy of detection of high-energy gamma photon-emitting/positron-emitting radionuclides, some of which have already been successfully applied to handheld gamma detection probe systems, are also the focus of current preclinical research that is actively looking at developing small platform, portable perioperative and intraoperative patient and ex vivo surgical specimen imaging devices which possess similar capabilities for detecting high-energy gamma photon-emitting/positron-emitting radionuclides [76]. However, such small platform, portable perioperative and intraoperative patient and ex vivo surgical specimen imaging devices have not yet been fully realized or made commercially available for use in the setting of clinical medicine.
4.3 Beta plus Decay (i.e., Positron) Detection
The detector component of a beta plus detection probe generally consists of a semiconductor ionization detector or an organic (“plastic”) scintillator detector but for which an inorganic scintillator detector can also be utilized [6, 45, 52, 108, 115–127]. As previously mentioned, whereas high-energy 511 keV gamma photons can travel many, many centimeters within biological tissues, positrons travels only very short distances (i.e., approximately 1–2 mm) within biological tissues before they are annihilated. This difference in the distances traveled by positrons as opposed to resultant high-energy 511 keV gamma photons within biologic tissues contributes to both the advantages and disadvantages of direct detection of positrons by a handheld beta plus detection probe. Thus, handheld beta plus detection probes can be small in physical size and light in weight secondary to the fact that whereas gamma photon detection of high-energy 511 keV gamma photons relies heavily on the thickness of side and back shielding and the length of collimation, beta plus decay detection of positrons does not require any significant degree of side and back shielding or collimation. However, whereas gamma photon detection of high-energy 511 keV gamma photons is less effected by the distance from the source of 511 keV gamma emissions to the proximity of the head of the handheld gamma detection probe, beta plus decay detection requires close apposition of the head of the handheld beta plus detection probe to the source of the positrons emitted from the biologic tissue. As a result, if the head of the handheld beta plus detection probe is not in direct contact with the biologic tissue emitting positrons, or if the source of the positrons emitted from the biologic tissue is located several millimeters below of the surface of that biologic tissue, the handheld beta plus detection probe will be unable to detect such 18F-FDG-avid tissues. Along similar lines, the simple placement of a sterile disposable barrier sheath over the handheld beta plus detection probe significantly reduces the overall sensitivity for the detection of 18F-FDG-avid tissues by such a device.
5 Clinical Applications of Real-Time 18F-FDG-Directed Surgery and Real-Time 18F-FDG-Directed Interventional Procedures (Tables 25.1 and 25.2)
The principal motivation behind the use of 18F-FDG for providing for real-time cancer detection and guidance within the operating room has been multifactorial, including exploring its applicability for real-time intraoperative staging, surgical planning and execution, and determination of completeness of surgical resection [6]. The clinical application of 18F-FDG-directed surgery was first described in 1999 by Desai et al. from the Ohio State University (Columbus, Ohio, USA) for colorectal cancer [6, 26, 27]. In this first clinical description of 18F-FDG-directed surgery, a total of 15 colorectal cancer patients received an intravenous injection of 4.0–5.7 mCi (148–211 MBq) of 18F-FDG at a time of 58–110 min prior to intraoperative evaluation with a commercially available gamma detection probe. Fourteen of these 15 patients had undergone a prior preoperative diagnostic 18F-FDG PET scan. A single or multiple tumor foci were identified with the gamma detection probe as 18F-FDG-avid tissue in 14 of the 15 patients receiving an intravenous injection of 18F-FDG on the day of surgery. Likewise, a single or multiple tumor foci were correctly identified with the gamma detection probe as 18F-FDG-avid tissue in 13 of 14 patients undergoing a prior preoperative diagnostic 18F-FDG PET scan, correctly correlating to the sites of hypermetabolic activity seen on the prior preoperative diagnostic 18F-FDG PET imaging.
Subsequent to the first report of 18F-FDG-directed surgery in 1999 [6, 26, 27], multiple groups of investigators from across the globe have collectively investigated the utility of real-time 18F-FDG-directed surgery and real-time 18F-FDG-directed diagnostic and therapeutic interventional procedures in regard to a wide range of solid malignancies, including colorectal cancer, gastric cancer, gastroesophageal cancer, pancreatic cancer, melanoma, lymphoma, breast cancer, ovarian cancer, endometrial cancer, cervical cancer, vulvar cancer, testicular cancer, prostate cancer, head and neck malignancies (squamous cell cancer of the oral cavity, oropharynx, hypopharynx, and laryngeal regions, iodine-negative recurrent papillary thyroid cancer, and recurrent medullary thyroid cancer), lung cancer, squamous cell cancer of the skin, GIST (gastrointestinal stromal tumor tumors), sarcoma, adrenocortical carcinoma, and carcinoma of unknown primary [6, 28–95]. Table 25.1 summarizes all reported real-time 18F-FDG-directed surgery series in the literature [6, 26–76]. Table 25.2 summarizes all reported real-time 18F-FDG-directed diagnostic and therapeutic interventional procedure series in the literature [6, 77–95]. It is worth noting a substantial portion of the clinical investigations into the use of 18F-FDG for real-time detection and guidance during cancer surgery for a variety of solid malignancies have been conducted at the Ohio State University (Columbus, Ohio, USA) [6, 26–28, 44, 46–51, 53, 54, 56, 59, 67, 71–76].
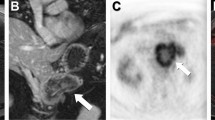
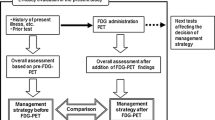
Our own experience with utilizing 18F-FDG for real-time cancer detection and guidance within the operating room at the Ohio State University (Columbus, Ohio, USA) [6, 26–28, 44, 46–51, 53, 54, 56, 59, 67, 71–76] has strengthened our long-standing contention regarding the importance of implementing a multimodal imaging and detection approach to 18F-FDG-directed surgery [50, 67, 74, 76]. Since 2005, the general structure of this multimodal approach has incorporated various components, including (1) same-day preoperative patient diagnostic whole-body PET/CT imaging, (2) intraoperative gamma detection probe assessment, (3) specimen imaging of surgically resected specimens with both a clinical PET/CT unit and a micro PET/CT unit, (4) radioactivity counting of selected portion of surgically resected specimens by an automatic gamma well counter, and (5) same-day postoperative patient diagnostic limited field-of-view PET/CT imaging [67].
On the day of the anticipated 18F-FDG-directed surgery procedure, patients fasted for a minimum of 6 h before undergoing the same-day preoperative diagnostic whole-body 18F-FDG PET/CT scan [67, 74]. Each patient received a same-day, single-dose, preoperative, intravenous injection of 18F-FDG, consisting of an averaged recommended dose in the range of approximately 15 mCi (555 MBq). The 18F-FDG dosing at the Ohio State University (Columbus, Ohio, USA) was based upon the standard-of-care practice guidelines set in the USA by the Society of Nuclear Medicine, the American College of Radiology, and the Society for Pediatric Radiology for diagnostic 18F-FDG PET/CT image acquisition (i.e., 10–20 mCi (370–740 MBq) of 18F-FDG in adults) [128, 129]. The same-day, single-dose, preoperative, intravenous dose of 18F-FDG was generally administered approximately 75 min prior to the planned time of the same-day preoperative diagnostic whole-body 18F-FDG PET/CT scan, which was performed within the time frame recognized by the standard-of-care practice guidelines set in the USA by the Society of Nuclear Medicine, the American College of Radiology, and the Society for Pediatric Radiology for diagnostic 18F-FDG PET/CT image acquisition [128, 129]. The same-day preoperative diagnostic whole-body 18F-FDG PET/CT scan usually consisted of 6–8 field-of-view PET bed positions and with 2 min of PET imaging for each field-of-view PET bed position. Patients then proceeded to the operating room for their anticipated surgical procedure and completed standard postoperative recovery in the postanesthesia care unit. The same-day postoperative diagnostic limited field-of-view 18F-FDG PET/CT scan was generally restricted to those field-of-view PET bed positions encompassing the immediate area of the surgical field (usually consisting of 1–3 field-of-view PET bed positions, in order to limit overall patient radiation exposure for the CT portion of the PET/CT, and with 10 min of PET imaging for each field-of-view PET bed position).
Our multimodal imaging and detection approach to 18F-FDG-directed surgery at the Ohio State University (Columbus, Ohio, USA) [50, 67, 74, 76] demonstrated technical and logistical feasibility for coordination of services by the surgeon, nuclear medicine physician, and pathologist in a same-day fashion. It allowed for (1) real-time intraoperative staging of the extent of disease; (2) real-time intraoperative surgical planning and execution of the necessary and most appropriate operation, determination of the extent of surgical resection, and determination of the completeness of surgical resection; (3) real-time pathologic evaluation of intact surgical resected specimens for the confirmation of completeness of surgical resection and for surgical margin assessment; and (4) real-time pathologic evaluation of diagnostically biopsied tissues for confirmation of correctness of tissue diagnosis.
6 Timing Issues Related to 18F-FDG-Directed Surgery: Impact of Length of Time from Injection of 18F-FDG to the Performance of Intraoperative Gamma Detection Probing
Numerous investigators have evaluated the concept of delayed phase and dual-time-point diagnostic 18F-FDG PET imaging [74] in which a portion of the diagnostic 18F-FDG PET imaging sequence is extended temporally out further than is generally recommended by the standard-of-care practice guidelines for diagnostic 18F-FDG PET/CT image acquisition [128, 129]. Remarkably, several of these groups of investigators have performed delayed phase diagnostic 18F-FDG PET imaging out to ultra-extended injection-to-scan acquisition time intervals ranging to 6–9 h after the initial 18F-FDG injection dose is administered [31, 74, 130–134].
In contrast to the innumerous work done on extended injection-to-scan acquisition time intervals for diagnostic 18F-FDG PET imaging, there has been very little data or discussion in the literature regarding the equivalent scenario of extended injection-to-probing time intervals as it pertains to gamma detection probing of patients intravenously injected with 18F-FDG [31, 38, 42, 43, 74]. Therefore, it is reasonable to say that the optimal length of time from the injection of 18F-FDG to the performance of intraoperative gamma detection probing has yet to be determined.
In 2004, Higashi et al. [31, 74] examined the question of “appropriate timing” for “postinjection” gamma detection probing using phantom studies and a limited series of 3 patients with “superficially located malignant lesions.” For the phantom studies, they used 5 liter plastic barrels filled with saline containing varying-dose “background” 18F-FDG as the “body trunk” phantom, 0.2 liter plastic bottles filled with saline containing varying-dose 18F-FDG as the “kidney” phantom, and 2 fixed-dose 18F-FDG sources to simulate “superficially located tumor nodules.” For the 3 patients with “superficially located malignant lesions,” they performed “preoperative” gamma detection probing at the skin surface at 1, 3, 5, 6, and/or 7 h after receiving an intravenous injection of 2–10 mCi (74–370 MBq) of 18F-FDG (and for which no intraoperative gamma detection probing was undertaken). In their limited patient data set, they showed that the tumor-to-background ratios of 18F-FDG by gamma detection probing at the skin surface remained relatively stable at the measured time intervals and remained relatively stable up to the 7-h postinjection time interval. However, they were concerned that the overall lower 18F-FDG count rates encountered at time intervals of 6–7 h postinjection of 18F-FDG, secondary to the normal physical decay pattern of 18F-FDG, “would be problematic” when applied to a clinical application of intraoperative gamma detection probing. Therefore, they concluded that the clinical application of intraoperative gamma detection probing was “more suitable” at 1–3 h postinjection of 18F-FDG as compared to 6–7 h postinjection of 18F-FDG.
In 2006 and 2007, Gulec et al. [38, 42, 43, 74] reported on two consecutive series of patients, including 40 patients undergoing intraoperative gamma detection probing after receiving an intravenous injection of 7–10 mCi (259–370 MBq) of 18F-FDG [38] and 25 patients undergoing intraoperative gamma detection probing after receiving an intravenous injection of 5–15 mCi (185–555 MBq) of 18F-FDG [42]. In both series, Gulec et al. [38, 42, 43] reported observing a nonsignificant trend toward an increased tumor-to-background ratio of 18F-FDG as the duration of time from the 18F-FDG injection to performing intraoperative gamma detection probing increased, with satisfactory count rates and lesion detection capabilities up to 6 h of time after injection of 18F-FDG. Therefore, regarding intraoperative gamma detection probing during 18F-FDG-directed surgery, they concluded that longer injection-to-probing time intervals “accentuated” the tumor-to-background ratio of 18F-FDG and resulted in “better lesion detection” [38, 42]. However, they also stated that “more delayed intervals between FDG injection and imaging might compromise image quality as a result of lower count rates” [42].
Most recently, in 2014, our group at the Ohio State University (Columbus, Ohio, USA) [74] examined the question of extended injection-to-scan acquisition time intervals in a retrospective data analysis of a subset of patients undergoing 18F-FDG-directed surgery. This data analysis specifically looked at preoperative 18F-FDG PET/CT imaging and postoperative 18F-FDG PET/CT imaging of 32 individual 18F-FDG-avid lesions (from among a total of 7 patients) which were not surgically manipulated or altered during 18F-FDG-directed surgery, and, for which, all of these 32 individual 18F-FDG-avid lesions were visualized on both same-day preoperative 18F-FDG PET/CT imaging and same-day postoperative 18F-FDG PET/CT imaging. In this retrospective data analysis, both 18F-FDG-avid lesions and their corresponding background tissues were assessed on same-day preoperative and postoperative 18F-FDG PET/CT scans. This data analysis demonstrated several important time-dependent observations. First, 18F-FDG PET/CT imaging performed at extended injection-to-scan acquisition times of up to a mean time of 530 min (i.e., approximately five half-lives for 18F-FDG) was able to maintain a designation of good/adequate diagnostic image quality deemed necessary for clinical interpretation. Second, the mean 18F-FDG-avid lesion SUVmax value increased significantly from preoperative to postoperative 18F-FDG PET/CT imaging (mean 18F-FDG-avid lesion SUVmax value; 7.7 preoperative to 11.3 postoperative; P <0.001). Third, mean background SUVmax value decreased significantly from preoperative to postoperative 18F-FDG PET/CT imaging (mean background SUVmax value; 2.3 preoperative to 2.1 postoperative; P = 0.017). Fourth, the mean lesion-to-background SUVmax ratio increased significantly from preoperative to postoperative 18F-FDG PET/CT imaging (mean lesion-to-background SUVmax ratio; 3.7 preoperative to 5.8 postoperative; P <0.001).
The far-reaching implications of these collective time-dependent observations [74] appear highly influential for guiding future direction in 18F-FDG-directed procedural and surgical applications, as well as 18F-FDG PET/CT oncologic imaging. First and foremost, these time-dependent observations justify the more widespread and integrated, real-time use of diagnostic 18F-FDG PET/CT imaging in conjunction with 18F-FDG-directed interventional radiology diagnostic biopsy procedures and therapeutic ablation procedures, as well as with 18F-FDG-directed surgical procedures. These sorts of integrated, real-time utilities for diagnostic 18F-FDG PET/CT imaging would facilitate periprocedural verification of appropriate tissue targeting during 18F-FDG-directed interventional radiology diagnostic biopsy procedures and therapeutic ablation procedures and for perioperative verification of appropriate tissue targeting and completeness of resection during 18F-FDG-directed surgical procedures. Secondly but still importantly, these time-dependent observations could have far-reaching impact on potentially reshaping future thinking regarding what represents the “most optimal” injection-to-scan acquisition time interval for all routine diagnostic 18F-FDG PET/CT oncologic imaging.
7 Inherent Challenge of In Situ Detection of 18F-FDG with a Gamma Photon Detection Device When Encountering a Low Target-to-Background Ratio of 18F-FDG and the Impact of Threshold Detection Criteria Methodology on the Determination of Gamma Detection Probe Positivity for Intraoperative In Situ Identification of 18F-FDG-Avid Tissue Sites during 18F-FDG-Directed Surgery
A significant challenge faced during attempted intraoperative in situ identification of 18F-FDG-avid tissue sites with a gamma photon detection device during 18F-FDG-directed surgery is a scenario in which a low target-to-background ratio (i.e., low tumor-to-background ratio) of high-energy 511 keV gamma photon emissions is encountered within the surgical field [6, 31, 38, 42, 43, 45, 52, 73, 75, 115–126]. As previously discussed, a low target-to-background ratio of high-energy 511 keV gamma photon emissions can results from a multitude of factors, including the marginal 18F-FDG uptake by certain tumor-bearing tissues, the distribution and degree of intrinsic physiologic background 18F-FDG activity within adjacent surrounding tissues which do not represent tumor-bearing tissues, and innumerable factors related to the technical specifications of the specific gamma photon detection device used for generating the counts per second measurements [75]. In this regard, some investigators have suggested that a minimum in situ target-to-background ratio of 1.5-to-1 for 18F-FDG is necessary for allowing the surgeon to comfortably differentiate tumor-bearing tissues from normal tissue during 18F-FDG-directed surgery [38, 42, 43, 73, 75]. However, a target-to-background ratio of 1.5-to-1 simply represents an arbitrary and fixed ratio determination.
Our personal experience with 18F-FDG-directed surgery at the Ohio State University (Columbus, Ohio, USA) [6, 26–28, 44, 46–51, 53, 54, 56, 59, 67, 71–76] clearly indicates that the observed in situ target-to-background ratio of 18F-FDG-avid tissue sites is frequently less than 1.5-to-1 and is highly dependent upon the specific gamma photon detection device utilized. Resultantly, when intraoperative detection of in situ 18F-FDG-avid tissue sites relies solely on a fixed target-to-background ratio (i.e., a ratiometric threshold method) as the threshold for probe positivity, the success of intraoperative detection can be limited and provide unsatisfactory results to the surgeon [73, 75]. Therefore, our own group has long contended that improved intraoperative in situ identification of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery can be better accomplished by the use of the three-sigma statistical threshold criteria method for determination of gamma detection probe positivity. The three-sigma statistical threshold criteria defines any given tissue as being probe positive when the count rate in that tissue exceeds three standard deviations above the mean count rate detected within normal adjacent tissue.
In order to comparatively assess the efficacy of the 1.5-to-1 ratiometric threshold criteria method and the three-sigma statistical threshold criteria method for determination of gamma detection probe positivity for intraoperative in situ detection of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery, we evaluated a total of 401 intraoperative gamma detection probe measurement sets of in situ counts per second measurements collected from our prospective, pilot study database and performed our analysis in a manner that was completely independent of the specific type of gamma detection probe system that was used for determination of the counts per second measurements [75]. Our data analysis demonstrated that the three-sigma statistical threshold criteria method was significantly better than the 1.5-to-1 ratiometric threshold criteria method (P <0.001) for determining gamma detection probe positivity for intraoperative in situ detection of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery. Likewise, the three-sigma statistical threshold criteria method was able to detect true positive results at target-to-background counts ratios that were much lower than could be detected by a ratiometric threshold criteria method that set the target-to-background count ratio cutoff at 1.5-to-1. Thus, if a surgeon utilized a gamma detection probe system with high count rate sensitivity, it was theoretically feasible that target-to-background count ratios as low as 1.1-to-1 could be identified as in situ probe positive when applying the three-sigma statistical threshold criteria method. Therefore, use of the three-sigma statistical threshold criteria for determination of gamma detection probe positivity for intraoperative in situ detection of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery proved instrumental for overcoming the commonly encountered scenario of a low target-to-background ratio (i.e., low tumor-to-background ratio).
8 Occupational Radiation Exposure to Intraoperative and Perioperative Personnel from 18F-FDG Radioguided Surgical Procedures
Occupational radiation exposure incurred by intraoperative and perioperative personnel participating in surgical cases has been previously evaluated by several groups of investigators [37, 41, 44–46, 52, 54, 55, 57, 60, 61, 64, 67, 135–137]. These investigators have reported data based upon several different study-design scenarios, including utilizing simulated surgical cases [46, 135, 136], surgical cases in which the patient was injected with 18F-FDG but in which actual 18F-FDG-directed surgery with intraoperative utilization of radiation detection probes was not undertaken for assisting in the surgical procedure [55, 57, 137], and actual 18F-FDG-directed surgery cases [37, 41, 44, 45, 52, 54, 60, 61, 64, 67].
The most comprehensive evaluation of occupational radiation exposure to intraoperative and perioperative personnel participating in 18F-FDG-directed surgery cases was published in 2008 by our group at the Ohio State University (Columbus, Ohio, USA) [54, 67]. In this comprehensive study, 10 actual 18F-FDG-directed surgery cases were evaluated. A mean dose of 18.9 mCi (699 MBq) of 18F-FDG was intravenously injected at a mean time of 142 min prior to surgery. The resultant mean deep dose equivalent per case for the surgeon, anesthetist, scrub technologist, postoperative nurse, circulating nurse, and preoperative nurse was 164, 119, 92, 63, 54, and 48 μSv, respectively.
The results of this comprehensive evaluation were used to determine the estimated number of 18F-FDG-directed surgery cases per year and the estimated number of hours of exposure per year that could be theoretically incurred by the surgeon, anesthetist, scrub technologist, postoperative nurse, circulating nurse, and preoperative nurse in both the USA and internationally [54, 67]. Based upon the established annual occupational exposure limit for adults within the USA of a total effective dose equivalent of 50,000 μSv (as defined by the US Nuclear Regulatory Commission) [54, 138], the estimated number of 18F-FDG-directed surgery cases per year and the estimated number of hours of exposure per year that could be theoretically incurred by the surgeon, anesthetist, scrub technologist, postoperative nurse, circulating nurse, and preoperative nurse were 305 cases and 820 h, 420 cases and 1020 h, 543 cases and 2083 h, 794 cases and 1471 h, 926 cases and 2941 h, and 1042 cases and 602 h, respectively [54]. In contrast to the annual occupational exposure limit for adults within the USA, the annual occupational exposure limit for the adult international community outside the USA (as defined by the International Commission on Radiological Protection (ICRP)) is more stringent and complex, with the annual occupational exposure limit for adults to be a total effective dose equivalent of 20,000 μSv per year, averaged over a 5-year period (100,000 μSv in 5 years), with further provision that the total effective dose equivalent should not exceed 50,000 μSv in any single year [54, 139, 140]. Based upon the established annual occupational exposure limit for the adult international community outside the USA defined by the International Commission on Radiological Protection (ICRP), the estimated number of 18F-FDG-directed surgery cases per year and the estimated number of hours of exposure per year that could be theoretically incurred by the surgeon, anesthetist, scrub technologist, postoperative nurse, circulating nurse, and preoperative nurse were 122 cases and 328 h, 168 cases and 408 h, 217 cases and 833 h, 317 cases and 588 h, 370 cases and 1176 h, and 417 cases and 241 h, respectively [54]. The data outlined in this comprehensive evaluation [54, 67] clearly illustrated that the absorbed radiation dose received by both intraoperative and perioperative personnel involved in 18F-FDG-directed surgery cases was relatively low per case and allows for all such personnel to participate in multiple cases and still remain well below regulatory standards set for occupational radiation exposure limits.
9 Concluding Remarks
The use of positron-emitting and high-energy gamma photon-emitting radiopharmaceuticals, like 18F-FDG, for real-time cancer detection and surgical guidance within the operating room and for real-time guidance of diagnostic and therapeutic interventional procedures within the interventional radiology suite, has great clinical potential. When a multimodal imaging and detection approach to 18F-FDG-directed surgery is utilized, thus coordinating of services provided by the surgeon, nuclear medicine physician, and pathologist, this integrated approach has the potential for allowing (1) real-time intraoperative staging of the extent of disease; (2) real-time intraoperative surgical planning and execution of the necessary and most appropriate operation, determination of the extent of surgical resection, and determination of the completeness of surgical resection; (3) real-time pathologic evaluation of intact surgical resected specimens for the confirmation of completeness of surgical resection and for surgical margin assessment; (4) real-time pathologic evaluation of diagnostically biopsied tissues for confirmation of correctness of tissue diagnosis; and (5) real-time guidance of diagnostic and therapeutic interventional procedures within the interventional radiology suite. However, major hurdles still exist for maximizing the clinical potential of these technologies. The greatest challenges that remain involve the need for the development of more technically optimized handheld radiation detection probes for positron-emitting and high-energy gamma photon-emitting radiopharmaceuticals, like 18F-FDG, as well as the need for the development of portable positron and high-energy gamma photon imaging devices that can be fully integrated into the operative/perioperative arena for real-time intraoperative/perioperative patient and specimen imaging. If these hurdles can be overcome, the use of positron-emitting and high-energy gamma photon-emitting radiopharmaceuticals for real-time cancer detection and surgical guidance within the operating room and for real-time guidance of diagnostic and therapeutic interventional procedures within the interventional radiology suite can become more fully realized and potentially impactful upon the long-term outcome for cancer patients.
References
Joliot F. Preuve expérimentale de lʹannihilation des electrons positifs. CR Acad Sci. 1933;197:1622–5.
Thibaud J. Lʹannihilation des positrons au contact de la matière et la radiation quʹen resulte. CR Acad Sci. 1933;197:1629–32.
Klemperer O. On the annihilation radiation of the positron. Math Proc Camb Phil Soc. 1934;30:347–54.
Berriger R, Montgomery CG. The angular distribution of positron annihilation radiation. Phys Rev. 1942;61:222–4.
Wrenn Jr FR, Good ML, Handler P. The use of positron-emitting radioisotopes for the localization of brain tumors. Science. 1951;113(2940):525–7.
Povoski SP, Neff RL, Mojzisik CM, O’Malley DM, Hinkle GH, Hall NC, Murrey Jr DA, Knopp MV, Martin Jr EW. A comprehensive overview of radioguided surgery using gamma detection probe technology. World J Surg Oncol. 2009;7:11.
Brownell GL. A history of positron imaging. October 15, 1999. http://neurosurgery.mgh.harvard.edu/docs/PEThistory.pdf.
Brownell GL, Sweet WH. Localization of brain tumors with positron emitters. Nucleonics. 1953;11:40–5.
Gallagher BM, Ansari A, Atkins H, Casella V, Christman DR, Fowler JS, Ido T, MacGregor RR, Som P, Wan CN, Wolf AP, Kuhl DE, Radiopharmaceuticals RM, XXVII. 18F-labeled 2-deoxy-2-fluoro-d-glucose as a radiopharmaceutical for measuring regional myocardial glucose metabolism in vivo: tissue distribution and imaging studies in animals. J Nucl Med. 1977;18:990–6.
Ido T, Wan CN, Casella V, Fowler JS, Wolf AP, Reivich M, Kuhl DE. Labeled 2-deoxy-D-glucose analogs: 18F-labeled 2-deoxy-2-fluoro-D-glucose, 2-deoxy-2-fluoro-D-mannose and 14C-2-deoxy-2-fluoro-D-glucose. J Label Compd Radiopharm. 1978;24:174–83.
Chesler DA. Three-dimensional activity distribution from multiple positron scintigraphs. J Nucl Med. 1971;12:347–8 [Abstract].
Chesler DA. Positron tomography and three-dimensional reconstruction technique. In: Freedman GS, editor. Tomographic imaging in nuclear medicine. 1st ed. New York, NY: Society of Nuclear Medicine; 1973. p. 176–83.
Ter-Pogossian MM, Phelps ME, Hoffman EJ, Mullani NA. A positron-emission transaxial tomograph for nuclear imaging (PETT). Radiology. 1975;114:89–98.
Hoffmann EJ, Phelps ME, Mullani NA, Higgins CS, Ter-Pogossian MM. Design and performance characteristics of a whole-body positron transaxial tomograph. J Nucl Med. 1976;17:493–502.
Hillner BE, Siegel BA, Liu D, Shields AF, Gareen IF, Hanna L, Stine SH, Coleman RE. Impact of positron emission tomography/computed tomography and positron emission tomography (PET) alone on expected management of patients with cancer: initial results from the National Oncologic PET Registry. J Clin Oncol. 2008;26:2155–61.
Hillner BE, Siegel BA, Shields AF, Liu D, Gareen IF, Hanna L, Stine SH, Coleman RE. The impact of positron emission tomography (PET) on expected management during cancer treatment: findings of the National Oncologic PET Registry. Cancer. 2009;115:410–8.
Poeppel TD, Krause BJ, Heusner TA, Boy C, Bockisch A, Antoch G. PET/CT for the staging and follow-up of patients with malignancies. Eur J Radiol. 2009;70:382–92.
Stroobants S. To PET or not to PET: what are the indications? Eur J Cancer. 2011;47 Suppl 3:S304–5.
Czernin J, Allen-Auerbach M, Nathanson D, Herrmann K. PET/CT in oncology: current status and perspectives. Curr Radiol Rep. 2013;1:177–90.
Schöder H, Gönen M. Screening for cancer with PET and PET/CT: potential and limitations. J Nucl Med. 2007;48 Suppl 1:4S–18.
Kojima S, Zhou B, Teramukai S, Hara A, Kosaka N, Matsuo Y, Suzuki H, Torigoe S, Suzuki T, Uno K, Fukushima M. Cancer screening of healthy volunteers using whole-body 18F-FDG-PET scans: The Nishidai clinic study. Eur J Cancer. 2007;43:1842–8.
Minamimoto R, Senda M, Uno K, Jinnouchi S, Iinuma T, Ito K, Okuyama C, Oguchi K, Kawamoto M, Suzuki Y, Tsukamoto E, Terauchi T, Nakashima R, Nishio M, Nishizawa S, Fukuda H, Yoshida T, Inoue T. Performance profile of FDG-PET and PET/CT for cancer screening on the basis of a Japanese Nationwide Survey. Ann Nucl Med. 2007;21:481–98.
Terauchi T, Murano T, Daisaki H, Kanou D, Shoda H, Kakinuma R, Hamashima C, Moriyama N, Kakizoe T. Evaluation of whole-body cancer screening using 18F-2-deoxy-2-fluoro-D-glucose positron emission tomography: a preliminary report. Ann Nucl Med. 2008;22:379–85.
Lee JW, Kang KW, Paeng JC, Lee SM, Jang SJ, Chung JK, Lee MC, Lee DS. Cancer screening using 18F-FDG PET/CT in Korean asymptomatic volunteers: a preliminary report. Ann Nucl Med. 2009;23:685–91.
Nishizawa S, Kojima S, Teramukai S, Inubushi M, Kodama H, Maeda Y, Okada H, Zhou B, Nagai Y, Fukushima M. Prospective evaluation of whole-body cancer screening with multiple modalities including [18F]fluorodeoxyglucose positron emission tomography in a healthy population: a preliminary report. J Clin Oncol. 2009;27:1767–73.
Desai D, Arnold M, Saha S, Hinkle G, Soble D, Frye J, DePalatis L, Mantil J, Satter M, Martin E. Intraoperative gamma detection of FDG distribution in colorectal cancer. Clin Positron Imaging. 1999;2:325.
Desai DC, Arnold M, Saha S, Hinkle G, Soble D, Fry J, DePalatis LR, Mantil J, Satter M, Martin EW. Correlative whole-body FDG-PET and intraoperative gamma detection of FDG distribution in colorectal cancer. Clin Positron Imaging. 2000;3:189–96.
Zervos EE, Desai DC, DePalatis LR, Soble D, Martin EW. 18F-labeled fluorodeoxyglucose positron emission tomography-guided surgery for recurrent colorectal cancer: a feasibility study. J Surg Res. 2001;97:9–13.
Essner R, Hsueh EC, Haigh PI, Glass EC, Huynh Y, Daghighian F. Application of an [(18)F]fluorodeoxyglucose-sensitive probe for the intraoperative detection of malignancy. J Surg Res. 2001;96:120–6.
Essner R, Daghighian F, Giuliano AE. Advances in FDG PET probes in surgical oncology. Cancer J. 2002;8:100–8.
Higashi T, Saga T, Ishimori T, Mamede M, Ishizu K, Fujita T, Mukai T, Sato S, Kato H, Yamaoka Y, Matsumoto K, Senda M, Konishi J. What is the most appropriate scan timing for intraoperative detection of malignancy using 18F-FDG-sensitive gamma probe? Preliminary phantom and preoperative patient study. Ann Nucl Med. 2004;18:105–14.
Yen TC, See LC, Lai CH, Yah-Huei CW, Ng KK, Ma SY, Lin WJ, Chen JT, Chen WJ, Lai CR, Hsueh S. 18F-FDG uptake in squamous cell carcinoma of the cervix is correlated with glucose transporter 1 expression. J Nucl Med. 2004;45:22–9.
Yap JT, Carney JP, Hall NC, Townsend DW. Image-guided cancer therapy using PET/CT. Cancer J. 2004;10:221–33.
Barranger E, Kerrou K, Petegnief Y, David-Montefiore E, Cortez A, Daraï E. Laparoscopic resection of occult metastasis using the combination of FDG-positron emission tomography/computed tomography image fusion with intraoperative probe guidance in a woman with recurrent ovarian cancer. Gynecol Oncol. 2005;96:241–4.
Carrera D, Fernandez A, Estrada J, Martin-Comin J, Gamez C. [Detection of occult malignant melanoma by 18F-FDG PET-CT and gamma probe]. Rev Esp Med Nucl. 2005;24:410–3. [Spanish].
Franc BL, Mari C, Johnson D, Leong SP. The role of a positron- and high-energy gamma photon probe in intraoperative localization of recurrent melanoma. Clin Nucl Med. 2005;30:787–91.
Kraeber-Bodéré F, Cariou B, Curtet C, Bridji B, Rousseau C, Dravet F, Charbonnel B, Carnaille B, Le Néel JC, Mirallié E. Feasibility and benefit of fluorine 18-fluoro-2-deoxyglucose-guided surgery in the management of radioiodine-negative differentiated thyroid carcinoma metastases. Surgery. 2005;138:1176–82.
Gulec SA, Daghighian F, Essner R. PET-Probe. Evaluation of technical performance and clinical utility of a handheld high-energy gamma probe in oncologic surgery. Ann Surg Oncol. 2006 [Epub ahead of print].
Meller B, Sommer K, Gerl J, von Hof K, Surowiec A, Richter E, Wollenberg B, Baehre M. High energy probe for detecting lymph node metastases with 18F-FDG in patients with head and neck cancer. Nuklearmedizin. 2006;45:153–9.
Nwogu C, Fischer G, Tan D, Glinianski M, Lamonica D, Demmy T. Radioguided detection of lymph node metastasis in non-small cell lung cancer. Ann Thorac Surg. 2006;82:1815–20; discussion 1820.
Curtet C, Carlier T, Mirallié E, Bodet-Milin C, Rousseau C, Barbet J, Kraeber-Bodéré F. Prospective comparison of two gamma probes for intraoperative detection of 18F-FDG: in vitro assessment and clinical evaluation in differentiated thyroid cancer patients with iodine-negative recurrence. Eur J Nucl Med Mol Imaging. 2007;34:1556–62.
Gulec SA, Hoenie E, Hostetter R, Schwartzentruber D. PET probe-guided surgery: applications and clinical protocol. World J Surg Oncol. 2007;5:65.
Gulec SA. PET probe-guided surgery. J Surg Oncol. 2007;96:353–7.
Hall NC, Povoski SP, Murrey DA, Knopp MV, Martin EW. Combined approach of perioperative 18F-FDG PET/CT imaging and intraoperative 18F-FDG handheld gamma probe detection for tumor localization and verification of complete tumor resection in breast cancer. World J Surg Oncol. 2007;5:143.
Piert M, Burian M, Meisetschlager G, Stein HJ, Ziegler S, Nahrig J, Picchio M, Buck A, Siewert JR, Schwaiger M. Positron detection for the intraoperative localisation of cancer deposits. Eur J Nucl Med Mol Imaging. 2007;34:1534–44.
Sarikaya I, Povoski SP, Al-Saif OH, Kocak E, Bloomston M, Marsh S, Cao Z, Murrey DA, Zhang J, Hall NC, Knopp MV, Martin EW. Combined use of preoperative 18F FDG-PET imaging and intraoperative gamma probe detection for accurate assessment of tumor recurrence in patients with colorectal cancer. World J Surg Oncol. 2007;5:80.
Sun D, Bloomston M, Hinkle G, Al-Saif OH, Hall NC, Povoski SP, Arnold MW, Martin EW. Radioimmunoguided surgery (RIGS), PET/CT image-guided surgery, and fluorescence image-guided surgery: past, present, and future. J Surg Oncol. 2007;96:297–308.
Agrawal A, Hall NC, Ringel MD, Povoski SP, Martin Jr EW. Combined use of perioperative TSH-stimulated 18F-FDG PET/CT imaging and gamma probe radioguided surgery to localize and verify resection of iodine scan-negative recurrent thyroid carcinoma. Laryngoscope. 2008;118:2190–4.
Cohn DE, Hall NC, Povoski SP, Seamon LG, Farrar WB, Martin Jr EW. Novel perioperative imaging with 18F-FDG PET/CT and intraoperative 18F-FDG detection using a handheld gamma probe in recurrent ovarian cancer. Gynecol Oncol. 2008;110:152–7.
Hall NC, Povoski SP, Murrey DA, Knopp MV, Martin EW. Bringing advanced medical imaging into the operative arena could revolutionize the surgical care of cancer patients. Expert Rev Med Devices. 2008;5:663–7.
Moffatt-Bruce SD, Povoski SP, Sharif S, Hall NC, Ross Jr P, Johnson MA, Martin Jr EW. A novel approach to positron emission tomography in lung cancer. Ann Thorac Surg. 2008;86:1355–7.
Piert M, Carey J, Clinthorne N. Probe-guided localization of cancer deposits using [(18)F]fluorodeoxyglucose. Q J Nucl Med Mol Imaging. 2008;52:37–49.
Povoski SP, Hall NC, Martin EW, Walker MJ. Multimodality approach of perioperative 18F-FDG PET/CT imaging, intraoperative 18F-FDG handheld gamma probe detection, and intraoperative ultrasound for tumor localization and verification of resection of all sites of hypermetabolic activity in a case of occult recurrent metastatic melanoma. World J Surg Oncol. 2008;6:1.
Povoski SP, Sarikaya I, White WC, Marsh SG, Hall NC, Hinkle GH, Martin Jr EW, Knopp MV. Comprehensive evaluation of occupational radiation exposure to intraoperative and perioperative personnel from 18F-FDG radioguided surgical procedures. Eur J Nucl Med Mol Imaging. 2008;35:2026–34.
van Baardwijk A, Bosmans G, van Suylen RJ, van Kroonenburgh M, Hochstenbag M, Geskes G, Lambin P, De Ruysscher D. Correlation of intra-tumour heterogeneity on 18F-FDG PET with pathologic features in non-small cell lung cancer: a feasibility study. Radiother Oncol. 2008;87:55–8.
Murrey Jr DA, Bahnson EE, Hall NC, Povoski SP, Mojzisik CM, Young DC, Sharif S, Johnson MA, Abdel-Misih S, Martin Jr EW, Knopp MV. Perioperative (18)F-fluorodeoxyglucose-guided imaging using the becquerel as a quantitative measure for optimizing surgical resection in patients with advanced malignancy. Am J Surg. 2009;198:834–40.
Gollub MJ, Akhurst TJ, Williamson MJ, Shia J, Humm JL, Wong WD, Paty PB, Guillem JG, Weiser MR, Temple LK, Dauer LT, Jhanwar SC, Kronman RE, Montalvo CV, Miller AR, Larson SM, Margulis AR. Feasibility of ex vivo FDG PET of the colon. Radiology. 2009;252:232–9.
Molina MA, Goodwin WJ, Moffat FL, Serafini AN, Sfakianakis GN, Avisar E. Intra-operative use of PET probe for localization of FDG avid lesions. Cancer Imaging. 2009;9:59–62.
Hall NC, Povoski SP, Murrey DA, Martin Jr EW, Knopp MV. Ex vivo specimen FDG PET/CT imaging for oncology. Radiology. 2010;255:663–4.
Nalley C, Wiebeck K, Bartel TB, Bodenner D, Stack Jr BC. Intraoperative radiation exposure with the use of (18)F-FDG-guided thyroid cancer surgery. Otolaryngol Head Neck Surg. 2010;142:281–3.
de Jong JS, van Ginkel RJ, Slart RH, Lemstra CL, Paans AM, Mulder NH, Hoekstra HJ. FDG-PET probe-guided surgery for recurrent retroperitoneal testicular tumor recurrences. Eur J Surg Oncol. 2010;36:1092–5.
Lee GO, Costouro NG, Groome T, Kashani-Sabet M, Leong SPL. The use of intraoperative PET probe to resect metastatic melanoma. BMJ Case Reports. 2010. doi:10.1136/bcr.12.2009.2593.
Hartemink KJ, Muller S, Smulders YM, Petrousjkavandentol M, Comans EF. [Fluorodeoxyglucose F18(FDG)-probe guided biopsy]. Ned Tijdschr Geneeskd. 2010;154:A1884. [Dutch].
García JR, Fraile M, Soler M, Bechini J, Ayuso JR, Lomeña F. [PET/CT-guided salvage surgery protocol. Results with ROLL Technique and PET probe]. Rev Esp Med Nucl. 2011;30:217–22. [Spanish].
Kim WW, Kim JS, Hur SM, Kim SH, Lee SK, Choi JH, Kim S, Choi JY, Lee JE, Kim JH, Nam SJ, Yang JH, Choe JH. Radioguided surgery using an intraoperative PET probe for tumor localization and verification of complete resection in differentiated thyroid cancer: A pilot study. Surgery. 2011;149:416–24.
Manca G, Biggi E, Lorenzoni A, Boni G, Roncella M, Ghilli M, Volterrani D, Mariani G. Simultaneous detection of breast tumor resection margins and radioguided sentinel node biopsy using an intraoperative electronically collimated probe with variable energy window: a case report. Clin Nucl Med. 2011;36:e196–8.
Povoski SP, Hall NC, Murrey Jr DA, Chow AZ, Gaglani JR, Bahnson EE, Mojzisik CM, Kuhrt MP, Hitchcock CL, Knopp MV, Martin Jr EW. Multimodal imaging and detection approach to 18F-FDG-directed surgery for patients with known or suspected malignancies: a comprehensive description of the specific methodology utilized in a single-institution cumulative retrospective experience. World J Surg Oncol. 2011;9:152.
Francis CL, Nalley C, Fan C, Bodenner D, Stack Jr BC. 18F-fluorodeoxyglucose and 131I Radioguided Surgical Management of Thyroid Cancer. Otolaryngol Head Neck Surg. 2012;146:26–32.
Bains S, Reimert M, Win AZ, Khan S, Aparici CM. A patient with psoriatic arthritis imaged with FDG-PET/CT demonstrated an unusual imaging pattern with muscle and fascia involvement: a case report. Nucl Med Mol Imaging. 2012;46:138–43.
Vos CG, Hartemink KJ, Muller S, Oosterhuis JW, Meijer S, van den Tol MP, Comans EF. Clinical applications of FDG-probe guided surgery. Acta Chir Belg. 2012;112:414–8.
Hall N, Murrey D, Povoski S, Barker D, Zhang J, Bahnson E, Chow A, Martin EW, Knopp MV. Evaluation of 18FDG PET/CT image quality with prolonged injection-to-scan times. Mol Imaging Biol. 2012;14(2, supplement):P610.
Hall NC, Povoski SP, Zhang J, Knopp MV, Martin Jr EW. Use of intraoperative nuclear medicine imaging technology: strategy for improved patient management. Expert Rev Med Devices. 2013;10:149–52.
Povoski SP, Chapman GJ, Murrey Jr DA, Lee R, Martin Jr EW, Hall NC. Intraoperative detection of 18F-FDG-avid tissue sites using the increased probe counting efficiency of the K-alpha probe design and variance-based statistical analysis with the three-sigma criteria. BMC Cancer. 2013;13:98.
Povoski SP, Murrey Jr DA, Smith SM, Martin Jr EW, Hall NC. 18F-FDG PET/CT oncologic imaging at extended injection-to-scan acquisition time intervals derived from a single-institution 18F-FDG-directed surgery experience: feasibility and quantification of 18F-FDG accumulation within 18F-FDG-avid lesions and background tissues. BMC Cancer. 2014;14:453.
Chapman GJ, Povoski SP, Hall NC, Murrey Jr DA, Lee R, Martin Jr EW. Comparison of two threshold detection criteria methodologies for determination of probe positivity for intraoperative in situ identification of presumed abnormal 18F-FDG-avid tissue sites during radioguided oncologic surgery. BMC Cancer. 2014;14:667.
Povoski SP, Hall NC, Murrey Jr DA, Wright CL, Martin Jr EW. Feasibility of a multimodal 18F-FDG-directed lymph node surgical excisional biopsy approach for appropriate diagnostic tissue sampling in patients with suspected lymphoma. BMC Cancer. 2015;15:378.
Prior JO, Kosinski M, Delaloye AB, Denys A. Initial report of PET/CT-guided radiofrequency ablation of liver metastases. J Vasc Interv Radiol. 2007;18:801–3.
Mallarajapatna GJ, Kallur KG, Ramanna NK, Susheela SP, Ramachandra PG. PET/CT-guided percutaneous biopsy of isolated intramuscular metastases from postcricoid cancer. J Nucl Med Technol. 2009;37:220–2.
Klaeser B, Mueller MD, Schmid RA, Guevara C, Krause T, Wiskirchen J. PET-CT-guided interventions in the management of FDG-positive lesions in patients suffering from solid malignancies: initial experiences. Eur Radiol. 2009;19:1780–5.
Klaeser B, Wiskirchen J, Wartenberg J, Weitzel T, Schmid RA, Mueller MD, Krause T. PET/CT-guided biopsies of metabolically active bone lesions: applications and clinical impact. Eur J Nucl Med Mol Imaging. 2010;37:2027–36.
Tatli S, Gerbaudo VH, Feeley CM, Shyn PB, Tuncali K, Silverman SG. PET/CT-guided percutaneous biopsy of abdominal masses: initial experience. J Vasc Interv Radiol. 2011;22:507–14.
Shyn PB, Tatli S, Sainani NI, Morrison PR, Habbab F, Catalano P, Silverman SG. Minimizing image misregistration during PET/CT-guided percutaneous interventions with monitored breath-hold PET and CT acquisitions. J Vasc Interv Radiol. 2011;22:1287–92.
Sainani NI, Shyn PB, Tatli S, Morrison PR, Tuncali K, Silverman SG. PET/CT-guided radiofrequency and cryoablation: is tumor fluorine-18 fluorodeoxyglucose activity dissipated by thermal ablation? J Vasc Interv Radiol. 2011;22:354–60.
Werner MK, Aschoff P, Reimold M, Pfannenberg C. FDG-PET/CT-guided biopsy of bone metastases sets a new course in patient management after extensive imaging and multiple futile biopsies. Br J Radiol. 2011;84:e65–7.
Schoellnast H, Larson SM, Nehmeh SA, Carrasquillo JA, Thornton RH, Solomon SB. Radiofrequency ablation of non-small-cell carcinoma of the lung under real-time FDG PET CT guidance. Cardiovasc Intervent Radiol. 2011;34 Suppl 2:S182–5.
Ryan ER, Sofocleous CT, Schöder H, Carrasquillo JA, Nehmeh S, Larson SM, Thornton R, Siegelbaum RH, Erinjeri JP, Solomon SB. Split-dose technique for FDG PET/CT-guided percutaneous ablation: a method to facilitate lesion targeting and to provide immediate assessment of treatment effectiveness. Radiology. 2013;268:288–95.
Cerci JJ, Pereira Neto CC, Krauzer C, Sakamoto DG, Vitola JV. The impact of coaxial core biopsy guided by FDG PET/CT in oncological patients. Eur J Nucl Med Mol Imaging. 2013;40:98–103.
Win AZ, Aparici CM. Real-time FDG PET/CT-guided bone biopsy in a patient with two primary malignancies. Eur J Nucl Med Mol Imaging. 2013;40:1787–8.
Shyn PB. Interventional positron emission tomography/computed tomography: state-of-the-art. Tech Vasc Interv Radiol. 2013;16:182–90.
Shyn PB, Tatli S, Sahni VA, Sadow CA, Forgione K, Mauri G, Morrison PR, Catalano PJ, Silverman SG. PET/CT-guided percutaneous liver mass biopsies and ablations: targeting accuracy of a single 20 s breath-hold PET acquisition. Clin Radiol. 2014;69:410–5.
Cerci JJ, Huber FZT, Bogoni M. PET/CT-guided biopsy of liver lesions. Clin Transl Imaging. 2014;2:157–63.
Aparici CM, Win AZ. Use of positron emission tomography/CT to perform biopsy of a mesenteric mass. J Vasc Interv Radiol. 2014;25:1609.
Aparici CM, Aslam R, Win AZ. Initial experience of utilizing real-time intra-procedural PET/CT biopsy. J Clin Imaging Sci. 2014:4:54.
Chakraborty PS, Dhull VS, Karunanithi S, Verma S, Kumar R. Malignant melanoma with cavitary pulmonary metastasis: Diagnostic dilemma resolved by FDG PET/CT guided biopsy. Indian J Nucl Med. 2014;29:196–7.
Cornelis F, Silk M, Schoder H, Takaki H, Durack JC, Erinjeri JP, Sofocleous CT, Siegelbaum RH, Maybody M, Solomon SB. Performance of intra-procedural 18-fluorodeoxyglucose PET/CT-guided biopsies for lesions suspected of malignancy but poorly visualized with other modalities. Eur J Nucl Med Mol Imaging. 2014;41:2265–72.
Syder SE, Kilbourne MR. Chemistry of fluorine-18 radiopharmaceuticals. In: Welch MJ, Redvanly CS, editors. Handbook of radiopharmaceuticals: radiochemistry and applications. 1st ed. Hoboken: John Wiley and Sons, Ltd; 2003. p. 195–228.
Fowler JS, Fowler JS, Ido T. Design and synthesis of 2-deoxy-2-[18F] fluoro-D-glucose (18FDG). In: Welch MJ, Redvanly CS, editors. Handbook of radiopharmaceuticals: radiochemistry and applications. 1st ed. Hoboken: John Wiley and Sons, Ltd; 2003. p. 307–22.
Warburg O, Posener K, Negelein E. The metabolism of the carcinoma cell. In: Warburg O, editor. The mechanism of tumors. 1st ed. New York: Richard R. Smith, Inc; 1931. p. 129–69.
Warburg O. On the origin of cancer cells. Science. 1956;123(3191):309–14.
Weber G. Enzymology of cancer cells. N Engl J Med. 1977;296:486–93.
Merrall NW, Plevin R, Gould GW. Growth factors, mitogens, oncogenes and the regulation of glucose transport. Cell Signal. 1993;5:667–75.
Pauwels EK, Ribeiro MJ, Stoot JH, McCready VR, Bourguignon M, Mazière B. FDG accumulation and tumor biology. Nucl Med Biol. 1998;25:317–22.
Gambhir SS. Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer. 2002;2:683–93.
Buck AK, Reske SN. Cellular origin and molecular mechanisms of 18F-FDG uptake: is there a contribution of the endothelium? J Nucl Med. 2004;45:461–3.
Otsuka H, Graham M, Kubo A, Nishitani H. Clinical utility of FDG PET. J Med Invest. 2004;51:14–9.
Otsuka H, Morita N, Yamashita K, Nishitani H. FDG-PET/CT for cancer management. J Med Invest. 2007;54:195–9.
Büsing KA, Schönberg SO, Brade J, Wasser K. Impact of blood glucose, diabetes, insulin, and obesity on standardized uptake values in tumors and healthy organs on 18F-FDG PET/CT. Nucl Med Biol. 2013;40:206–13.
Heller S, Zanzonico P. Nuclear probes and intraoperative gamma cameras. Semin Nucl Med. 2011;41:166–81.
Martin EW, Chapman GJ, Subramaniam VV, Povoski SP. Intraoperative detection of gamma emissions using K-alpha X-ray fluorescence. Expert Rev Med Devices. 2010;7:431–4.
GFE Gesellschaft für Forschungs und Entwicklungsservice mbH; Gamma Locator DXI. http://www.gfe-service.de/en/ylocator.php.
Gerl J, Ameil F, Kojouharov Z, Surowiec D. High energy gamma probe with position sensing capability. European Patent EP 1 596 223 B1; Filed May 10, 2005; Published January 21, 2009.
Gerl J. Kojouharov Z, Ameil E, Surowiec D. High energy gamma probe with position sensing capability. United States Patent US 7,312,460 B2; Filed May 10, 2005; Published December 25, 2007.
Lecomte R, Schmitt D, Lamoureux G. Geometry study of a high resolution PET detection system using small detectors. IEEE Trans Nucl Sci. 1984;31:556–61.
Levin CS. New imaging technologies to enhance the molecular sensitivity of positron emission tomography. Proc IEEE. 2008;96:439–67.
Raylman RR, Wahl RL. A fiber-optically coupled positron-sensitive surgical probe. J Nucl Med. 1994;35:909–13.
Daghighian F, Mazziotta JC, Hoffman EJ, Shenderov P, Eshaghian B, Siegel S, Phelps ME. Intraoperative beta probe: a device for detecting tissue labeled with positron or electron emitting isotopes during surgery. Med Phys. 1994;21:153–7.
Raylman RR, Fisher SJ, Brown RS, Ethier SP, Wahl RL. Fluorine-18-fluorodeoxyglucose-guided breast cancer surgery with a positron-sensitive probe: validation in preclinical studies. J Nucl Med. 1995;36:1869–74.
Raylman RR, Wahl RL. Evaluation of ion-implanted-silicon detectors for use in intraoperative positron-sensitive probes. Med Phys. 1996;23:1889–95.
Raylman RR. A solid-state intraoperative beta probe system. (Nuclear Science) IEEE Trans Nucl Sci. 2000;47:1696–703.
Yasuda S, Makuuchi H, Fujii H, Nakasaki H, Mukai M, Sadahiro S, Tajima T, Ide M, Shohtsu A, Suzuki Y. Evaluation of a surgical gamma probe for detection of 18F-FDG. Tokai J Exp Clin Med. 2000;25:93–9.
Raylman RR. Performance of a dual, solid-state intraoperative probe system with 18F, 99mTc, and (111)In. J Nucl Med. 2001;42:352–60.
Raylman RR, Srinivasan A. Endoprobe: a system for radionuclide-guided endoscopy. Med Phys. 2004;31:3306–13.
Yamamoto S, Matsumoto K, Senda M. Optimum threshold setting for a positron-sensitive probe with background rejection capability. Ann Nucl Med. 2004;18:251–6.
Yamamoto S, Matsumoto K, Sakamoto S, Tarutani K, Minato K, Senda M. An intra-operative positron probe with background rejection capability for FDG-guided surgery. Ann Nucl Med. 2005;19:23–8.
Yamamoto S, Higashi T, Matsumoto K, Senda M. Development of a positron-imaging detector with background rejection capability. Ann Nucl Med. 2006;20:655–62.
Strong VE, Galanis CJ, Riedl CC, Longo VA, Daghighian F, Humm JL, Larson SM, Fong Y. Portable PET probes are a novel tool for intraoperative localization of tumor deposits. Ann Surg Innov Res. 2009;3:2.
Singh B, Stack Jr BC, Thacker S, Gaysinskiy V, Bartel T, Lowe V, Cool S, Entine G, Nagarkar V. A hand-held beta imaging probe for FDG. Ann Nucl Med. 2013;27:203–8.
Delbeke D, Coleman RE, Guiberteau MJ, Brown ML, Royal HD, Siegel BA, Townsend DW, Berland LL, Parker JA, Hubner K, Stabin MG, Zubal G, Kachelriess M, Cronin V, Holbrook S. Procedure guideline for tumor imaging with 18F-FDG PET/CT 1.0. J Nucl Med. 2006;47:885–95.
American College of Radiology (ACR) and the Society for Pediatric Radiology (SPR) Practice Parameter for Performing FDG-PET/CT in Oncology, Res. 24 – 2012, Amended 2014 (Res. 39). http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/FDG_PET_CT.pdf.
Lodge MA, Lucas JD, Marsden PK, Cronin BF, O’Doherty MJ, Smith MA. A PET study of 18FDG uptake in soft tissue masses. Eur J Nucl Med. 1999;26:22–30.
Spence AM, Muzi M, Mankoff DA, O’Sullivan SF, Link JM, Lewellen TK, Lewellen B, Pham P, Minoshima S, Swanson K, Krohn KA. 18F-FDG PET of gliomas at delayed intervals: improved distinction between tumor and normal gray matter. J Nucl Med. 2004;45:1653–9.
Basu S, Kung J, Houseni M, Zhuang H, Tidmarsh GF, Alavi A. Temporal profile of fluorodeoxyglucose uptake in malignant lesions and normal organs over extended time periods in patients with lung carcinoma: implications for its utilization in assessing malignant lesions. Q J Nucl Med Mol Imaging. 2009;53:9–19.
Horky LL, Hsiao EM, Weiss SE, Drappatz J, Gerbaudo VH. Dual phase FDG-PET imaging of brain metastases provides superior assessment of recurrence versus post-treatment necrosis. J Neurooncol. 2011;103:137–46.
Prieto E, Martí-Climent JM, Domínguez-Prado I, Garrastachu P, Díez-Valle R, Tejada S, Aristu JJ, Peñuelas I, Arbizu J. Voxel-based analysis of dual-time-point 18F-FDG PET images for brain tumor identification and delineation. J Nucl Med. 2011;52:865–72.
Heckathorne E, Dimock C, Dahlbom M. Radiation dose to surgical staff from positron-emitter-based localization and radiosurgery of tumors. Health Phys. 2008;95:220–6.
Heckathorne E, Dimock C, Dahlbom M, Daghighian F. Radiation dose to surgical staff from PET-based localization and radiosurgery of tumors. Health Phys. 2007;93:S45.
Andersen PA, Chakera AH, Klausen TL, Binderup T, Grossjohann HS, Friis E, Palnaes Hansen C, Schmidt G, Kjaer A, Hesse B. Radiation exposure to surgical staff during F-18-FDG-guided cancer surgery. Eur J Nucl Med Mol Imaging. 2008;35:624–9.
United States Nuclear Regulatory Commission (1991). Section 20.1201 – occupational dose limits for adults, subpart C – occupational dose limits, part 20 – Standards for Protection Against Radiation, Chapter I – Nuclear Regulatory Commission, NRC Regulations Title 10 of the Code of Federal Regulations. http://www.nrc.gov/reading-rm/doc-collections/cfr/part020/full-text.html.
ICRP. Publication 60. The 1990 recommendations of the international commission on radiological protection. Ann ICRP. 1991;21(1–3):1–201.
ICRP. Publication 103. The 2007 recommendations of the international commission on radiological protection (chapters 5 and 6). Ann ICRP. 2007;37(2-4):81–123.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Povoski, S.P., Murrey, D.A., Hall, N.C. (2016). 18F-FDG-Directed Surgery and 18F-FDG-Directed Interventional Procedures. In: Herrmann, K., Nieweg, O., Povoski, S. (eds) Radioguided Surgery. Springer, Cham. https://doi.org/10.1007/978-3-319-26051-8_25
Download citation
DOI: https://doi.org/10.1007/978-3-319-26051-8_25
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26049-5
Online ISBN: 978-3-319-26051-8
eBook Packages: MedicineMedicine (R0)