Abstract
The advantages of laparoscopic (LPS) surgery have made it increasingly attractive as an alternative to traditional approaches for treatment of gynaecologic malignancies, especially endometrial cancers.
Many patients with gynaecologic disorders present with co-morbidity such as obesity, hypertension, and diabetes.
Abdominal surgery (LPT) is therefore exposing patients into increased risk of complications. Vaginal hysterectomy has been demonstrated as an attractive alternative for these patients, but this approach does not allow exploration of the abdominal cavity, peritoneal washing, and lymph node dissection.
Laparoscopic technique seems to overcome these disadvantages especially in extremely obese women.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Several studies showed that LPS treatment of obese women with endometrial pathologies offers many advantages compared to the open approach [1–4] primarily considering the less postoperative pain, better visibility of the operative field, and shorter hospital stay as the main benefit [5, 6]; post-operative complications after LPS treatment seems to be reduced or similar [1, 3], likely related to the laparoscopic expertise of the operating surgeons and the patient’s co-morbidities.
However, this procedure does not seem to modify the incidence of intra-operative and post-operative complications [3, 7].
It appears from data of several studies that LPS hysterectomy may offer significant advantages over LPT in the comprehensive surgical management of extremely obese women, but it should be performed by advanced laparoscopic gynaecologic surgeons [7].
Surgical Technique of Laparoscopic Hysterectomy
After dilatation with a Hegar dilator (no. 7.5), an uterine manipulator (Clermont-Ferrand, Karl Storz, Tuttlingen, Germany) is inserted.
A 11 mm Endopath XCEL® trocar (Ethicon, Johnson & Johnson, USA) that incorporates the zero-degree laparoscope (Karl Storz, Tuttlingen, Germany) was inserted through an umbilical vertical incision, after pneumoperitoneum by Veress needle (Covidien Cares, Minneapolis, MN) has been induced at the level of umbilicus.
Difficulties of entry into the abdomen in obese patients are often associated with the expanded thick fatty layer of the abdominal wall, especially with translocation of the umbilicus which is more caudal to the normal umbilical site and just below the aortic bifurcation.
In our technique, an 11 mm skin incision is created at the superior crease of the umbilical fold, and the underlying subcutaneous adipose tissue is bluntly dissected using the tip of a fine clamp until the umbilical stalk is isolated at the inferior and central part of the incision.
There is a concern that rare but life-threatening complications can occur, including severe bleeding due to damages of major abdominal vessels, as well as other injuries related to bowel and bladder trauma, subcutaneous emphysema and postsurgical infections.
To prevent these complications and risks, the abdominal wall is elevated by upward traction. In obese patients the Veress needle is then inserted nearly perpendicular to the incision and turned toward the pelvis “immediately” after resistance to the needle has been lost.
Three suprapubic ancillary trocars were used: one 5 mm Endopath XCEL® trocar (Ethicon, Johnson & Johnson, USA) trocar was inserted in the midline 3 cm under the umbilicus, and one in each iliac fossa (11 mm on the left side and 5 mm on the right size) laterally to inferior epigastric vessels, respectively.
Before the operative procedure, all the pelvic structures are inspected and the abdomen explored through the laparoscope in a clockwise fashion.
Laparoscopic hysterectomy is performed with the patient in an approximately 30 ° Trendelenburg position to facilitate retroperitoneal exposure by retaining the small intestine in the mid and upper abdomen using gravity and gentle instrumentation. In patients with a prior midline incision, the initial entry into the abdominal cavity was made approximately 2 cm below the left costal margin at the level of the midclavicular line to avoid injury to bowel adherent to the anterior abdominal wall.
A MiniPort 2 mm single use introducer (MiniPort-Auto-Suture, USSC, Norwalk, CT) and a stopcock for insufflation and desufflation were used to establish the pneumoperitoneum.
The obturator had a spring-loaded, blunt stylet similar in function to a Veress needle. A circular adjustable stopper located on the sleeve of the miniport allowed for adjustment of depth in the cavity. The system was used to establish and maintain the pneumoperitoneum in the abdomen while providing access for a minilaparoscope with a diameter of 1.9 mm and a length of 10 or 12 cm (Karl Storz, Tuttlingen, Germany).
The round ligament is coagulated and transected with endoscopic shears (Fig. 49.1). The vesico-uterine fold is grasped and incised (Fig. 49.2) while the bladder is isolated: after dividing the vesico-uterine fold (Fig. 49.3, the suction-irrigator probe pushes the bladder completely from the upper vagina (Fig. 49.4).
The anterior and posterior peritoneal layers of the broad ligament are opened and the ureter is identified at the pelvic brim, traced into the pelvis and freed from the posterior leaf of the broad ligament. The ovarian ligament is coagulated (Fig. 49.5) with bipolar forceps and transacted with scissors. The uterine vessels are identified allowing an excellent skeletonization of the obliterated artery by preparing the anterior and posterior web. The uterine artery is coagulated and transected.
The vagina is visualized and the vaginal cuff around the cervix is transected with the monopolar needle (Fig. 49.6), incising the vagina circumferentially using the porcelain-valve of the uterine manipulator as a guide; the uterus is removed vaginally. The vaginal vault is closed with continuous 0-polysorb sutures by laparoscopic access and after the laparoscopic control of the haemostasis is performed (Fig. 49.7). The 5- and 10-mm incisions are closed with mattress sutures of 2–0 Rapide Vycril. At the conclusion of the surgical procedure we deflated the abdomen before removing the trocars.
During laparoscopic surgery in obese patients, sufficient intraabdominal workspace is important for the surgeon. Therefore, most surgeons request that their patients be placed in an adequate Trendelenburg position to facilitate retroperitoneal exposure in the case of lymphadenectomy. This leads to retention of the small intestine in the mid and upper abdomen using gravity and gentle instrumentation and reduces bowel injury; however, the effect of an increased workspace is not always sufficient.
Discussion
Obese patients with endometrial cancer patients exhibit a large accumulation and abnormal distribution of abdominal fat; these characteristics seriously affect the exposure of the operative field. In addition, perivascular fat parcels and lipid deposition on vascular walls lead to increased vascular fragility; as a result, slight stretching of blood vessels can easily lead to vascular rupture and bleeding, which severely affect the surgical process and increase surgical difficulty and risk. Furthermore, obesity is frequently associated with many cardiopulmonary and other chronic diseases that decrease operational tolerance.
Many patients with gynaecologic pathologies present with co-morbidity such as obesity, hypertension, and diabetes [8]. Abdominal surgery is therefore exposing patients into increased risk of complications [9].
The role of minimally invasive surgical staging in the management of extremely obese patients with gynaecologic pathologies continues to evolve. Recently, several studies concluded, as others, that the post-operative complications after LPS treatment are reduced or similar [5, 9–12].
Brezina et al. compared the surgical outcomes of 293 obese women undergoing hysterectomy (LPT, vaginal, or LPS). No significant difference was found in obese women between LPS and LPT hysterectomy for operative time and anaesthesia. They concluded that in obese patients for whom vaginal hysterectomy is not possible, LPS hysterectomy should be considered before LPT hysterectomy because the LPS route reduced hospital time and blood loss [13].
Nawfal et al. estimated the impact of body mass index (BMI) on the surgical outcomes of 135 patients undergoing robotic-assisted total LPS hysterectomy for benign indications. They concluded that BMI is not associated with blood loss, duration of surgery, length of stay, or complication rates in patients undergoing robotic-assisted total LPS hysterectomy. Robotic assistance may help surgeons overcome adverse outcomes sometimes found in obese patients [14].
Bardens et al. investigated the influence of the body mass index (BMI) on 200 patients who underwent LPS hysterectomy for benign disease. The group of overweight women had the highest rate of complications and the group of obese women had the lowest. However, the rate of women who required readmission and reoperation was not elevated in the overweight group. They concluded that LPS hysterectomy is a safe and feasible method even in obese and morbidly obese patients. Overweight and obesity increase the time needed to perform LPS hysterectomy but do not seem to relevantly influence the rate of major intra and postoperative complications [15].
Harmanli et al. compared the effect of obesity on perioperative outcomes in women undergoing LPS supracervical hysterectomy (LSH) or LPS total hysterectomy (TLH) for benign conditions in obese (body mass index > or = 30 kg/m2) and non-obese women. The rates of urinary tract injury, vaginal cuff dehiscence, postoperative fever, and ileus were similar between the groups. Of all seven cuff dehiscences, 5 (71 %) occurred in non-obese women undergoing TLH. They concluded that obesity increased the risk of bleeding requiring transfusion and conversion to laparotomy but did not influence the other perioperative complications. LSH in non-obese women seems to result in best outcomes [16].
In a recent study by Fanfani et al. they analysed perioperative outcomes of Laparo-Endoscopic Single-Site (LESS) hysterectomy in obese and non-obese women in a multicentric retrospective case-control study on 115 women who underwent LESS hysterectomy and were divided into two groups: obese (n = 43, BMI ≥ 30 kg/m2) and non-obese (n = 72, BMI < 30 kg/m2). No statistical differences regarding perioperative outcomes were observed between the two groups. Conversion to laparotomy occurred in 1 obese (2.3 %) and 3 (4.2 %) non-obese women. Intraoperative complication rate was 11.6 % and 9.6 % in obese and non-obese women, respectively. The early postoperative complication rate was 6.9 % in obese and 4.1 % in non-obese women. This study suggested that obesity (BMI ≥ 30) does not preclude successful completion of total LESS hysterectomy [17].
In a recent retrospective study Tinelli et al. compared the safety, complication and recurrence rate after total LPS hysterectomy with lymphadenectomy and LPT hysterectomy with lymphadenectomy for early stage endometrial carcinoma in a series of 75 extremely obese women (BMI > 35).
They performed a multicenter study of all the complications after treatment of 75 consecutive extremely obese patients with clinical stage I endometrial cancer who underwent LPS hysterectomy (45 cases) or LPT hysterectomy (30 cases) with pelvic and aortic lymph node dissection.
According to the FIGO staging system, all the patients underwent surgical staging consisting of total hysterectomy, bilateral salpingo-oophorectomy, and in all cases systematic bilateral pelvic lymphadenectomy was performed. In three patients of the LPT group they observed a dehiscence of the abdominal suture with surgical site infection in the first week after surgery that was resutured with interrupted sutured with no sequelae. Postoperative fever was reported in 6 (20 %) patients of the LPT group and in 2 patient of LPS (4.4 %) group.
No case of port-site metastasis, no vascular injury and no wound complications were detected.
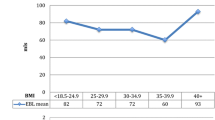
In all cases the LPS procedures were successfully completed without conversion to LPT and no patient of the two groups required an intra-operative or postoperative blood transfusion (Fig. 49.8).
One case of bladder injury occurred in the LPS group at the time of utero-vesical fold incision that was laparoscopically sutured.
In this multicentre study, no significant difference in intra-operative complications was observed between groups, whereas postoperative were significantly less common in the LPS than in the LPT group.
We can speculate that LPS hysterectomy in extremely obese women is associated with safety and efficacy outcomes that are similar to those that have been reported for LPT hysterectomy for the treatment of endometrial pathologies [18, 19].
In fact, in almost cases the LPS procedures were successfully completed without conversion to LPT and no patient of the two groups required an intra-operative or postoperative blood transfusion.
Therefore, it appears from data of our studies that LPS hysterectomy may offer significant advantages over LPT in the comprehensive surgical management of extremely obese women, but it should be performed by advanced laparoscopic gynaecologic surgeons.
In fact, a totally LPS hysterectomy is more difficult in the morbidly obese and other patient factors such as associated co-morbidities, adhesive disease, large uteri, fatty mesentery, and inability to tolerate steep Trendelenburg have limited widespread use of this approach in the treatment of uterine pathologies [3–7, 20].
The obese patients with associated co-morbidities had the most to gain from a successfully completed minimally invasive procedure, but also offered the surgeon the greatest challenges to complete the case [21–24].
Moreover, the LPS permits a better exposure of the operative field in association with the advancement of the LPS techniques allowing better dissection of the pelvic spaces; however, it should be outlined that LPS procedures have to be always performed by the same surgical team [4, 7, 12].
Several studies confirm that LPS hysterectomy remains, in expert hands, the procedure better related to the best short-term outcomes in obese women [13–19, 25].
In fact, LPS hysterectomy was associated with a shorter time of post-operative ileus, shorter hospitalization, lower cases of dehiscence of the suture with surgical site infection, reduced cases of postoperative fever, and a reduced time of discharge when compared with LPT fever reducing the costs.
Conclusion
Our data confirm that LPS hysterectomy in extremely obese women improves quality of life in the postoperative period with reduced time of discharge.
The low intra-operative and post-operative complications rate observed in the LPS group highlights the feasibility, safety and efficacy of this surgical approach for the obese patients.
LPS hysterectomy can be considered a safe and effective therapeutic approach for management of e obese women with a better visibility of the operative field, lower postoperative pain, and a significantly lower blood loss, although multicentre randomized trials, long-term follow-up and cost-benefit analyses are required to determine if the use of LPS improves outcomes over standard LPT in obese women and if the advantages of this technique could be extended to a larger proportion of patients.
References
Ghezzi F, Cromi A, Bergamini V, Uccella S, Beretta P, Franchi M, Bolis P. Laparoscopic management of endometrial cancer in nonobese and obese women: a consecutive series. J Minim Invasive Gynecol. 2006;13:269–75.
Malur S, Possover M, Michels W, Schneider A. Laparoscopic-assisted vaginal versus abdominal surgery in patients with endometrial cancer: a prospective randomized trial. Gynecol Oncol. 2001;80:239–44.
Malzoni M, Tinelli R, Cosentino F, Perone C, Rasile M, Iuzzolino D, Malzoni C, Reich H. Total laparoscopic hysterectomy versus abdominal hysterectomy with lymphadenectomy for early-stage endometrial cancer: a prospective randomized study. Gynecol Oncol. 2009;112:126–33.
Palomba S, Falbo A, Mocciaro R, Russo T, Zullo F. Laparoscopic treatment for endometrial cancer: a meta-analysis of randomized controlled trials (RCTs). Gynecol Oncol. 2009;112:415–21.
Galaal K, Bryant A, Fisher AD, Al-Khaduri M, Kew F, Lopes AD. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev 2012;(9):CD 006655.
Perrone AM, Di Marcoberardino B, Rossi M, Pozzati F, Pellegrini A, Procaccini M, Santini D, De Iaco P. Laparoscopic versus laparotomic approach to endometrial cancer. Eur J Gynaecol Oncol. 2012;33:376–81.
Litta P, Merlin F, Saccardi C, Pozzan C, Sacco G, Fracas M, Capobianco G, Dessole S. Role of hysteroscopy with endometrial biopsy to rule out endometrial cancer in postmenopausal women with abnormal uterine bleeding. Maturitas. 2005;50:117–23.
Kalogiannidis I, Lambrechts S, Amant F, Neven P, Van Gorp T, Vergote I. Laparoscopy-assisted vaginal hysterectomy compared with abdominal hysterectomy in clinical stage I endometrial cancer: safety, recurrence, and long-term outcome. Am J Obstet Gynecol. 2007;196:248.
Litta P, Bartolucci C, Saccardi C, Codroma A, Fabris A, Borgato S, Conte L. Atypical endometrial lesions: hysteroscopic resection as an alternative to hysterectomy. Eur J Gynaecol Oncol. 2013;34:51–3.
Mariani A, Webb MJ, Galli L, Podratz KC. Potential therapeutic role of para-aortic lymphadenectomy in node-positive endometrial cancer. Gynecol Oncol. 2000;76:348–56.
Lu Q, Liu H, Liu C, Wang S, Li S, Guo S, Lu J, Zhang Z. Comparison of laparoscopy and laparotomy for management of endometrial carcinoma: a prospective randomized study with 11-year experience. J Cancer Res Clin Oncol. 2013;139:1853–9.
Walker JL, Piedmonte MR, Spirtos NM, Eisenkop SM, Schlaerth JB, Mannel RS, Spiegel G, Barakat R, Pearl ML, Sharma SK. Laparoscopy compared with laparotomy for comprehensive surgical staging of uterine cancer: Gynecologic Oncology Group Study LAP2. J Clin Oncol. 2009;27:5331–6.
Brezina PR, Beste TM, Nelson KH. Does route of hysterectomy affect outcome in obese and nonobese women? JSLS. 2009;13:358–63.
Nawfal AK, Orady M, Eisenstein D, Wegienka G. Effect of body mass index on robotic-assisted total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2011;18:328–32.
Bardens D, Solomayer E, Baum S, Radosa J, Gräber S, Rody A, Juhasz-Böss I. The impact of the body mass index (BMI) on laparoscopic hysterectomy for benign disease. Arch Gynecol Obstet. 2014;289:803–7.
Harmanli O, Esin S, Knee A, Jones K, Ayaz R, Tunitsky E. Effect of obesity on perioperative outcomes of laparoscopic hysterectomy. J Reprod Med. 2013;58:497–503.
Fanfani F, Boruta DM, Fader AN, Vizza E, Growdon WB, Kushnir CL, Corrado G, Scambia G, Turco LC, Fagotti A. Feasibility and surgical outcome in obese vs. non-obese patients undergoing Laparo-Endoscopic Single-Site (LESS) hysterectomy: a multicenter case-control study. J Minim Invasive Gynecol. 2014;12:401–10.
Barakat RR, Lev G, Hummer AJ, Sonoda Y, Chi DS, Alektiar KM, Abu-Rustum NR. Twelve-year experience in the management of endometrial cancer: a change in surgical and postoperative radiation approaches. Gynecol Oncol. 2007;105:150–6.
Seamon LG, Cohn DE, Henretta MS, Kim KH, Carlson MJ, Phillips GS, Fowler JM. Minimally invasive comprehensive surgical staging for endometrial cancer: robotics or laparoscopy? Gynecol Oncol. 2009;113:36–41.
Tinelli R, Malzoni M, Cicinelli E, Fiaccavento A, Zaccoletti R, Barbieri F, Tinelli A, Perone C, Cosentino F. Is early stage endometrial cancer safely treated by laparoscopy? Complications of a multicenter study and review of recent literature. Surg Oncol. 2011;20:80–7.
Malzoni M, Tinelli R, Cosentino F, Fusco A, Malzoni C. Total laparoscopic radical hysterectomy versus abdominal radical hysterectomy with lymphadenectomy in patients with early cervical cancer: our experience. Ann Surg Oncol. 2009;16:1316–23.
Malzoni M, Tinelli R, Cosentino F, Perone C, Vicario V. Feasibility, morbidity, and safety of total laparoscopic radical hysterectomy with lymphadenectomy: our experience. J Minim Invasive Gynecol. 2007;14:584–90.
Palomba S, Ghezzi F, Falbo A, Mandato VD, Annunziata G, Lucia E. Laparoscopic versus abdominal approach to endometrial cancer: a 10-year retrospective multicenter analysis. Int J Gynecol Cancer. 2012;22:425–33.
Tinelli R, Malzoni M, Cosentino F, Perone C, Fusco A, Cicinelli E, Nezhat F. Robotics versus laparoscopic radical hysterectomy with lymphadenectomy in patients with early cervical cancer: a multicenter study. Ann Surg Oncol. 2011;18:2622–8.
Tinelli R, Litta P, Meir Y, Surico D, Leo L, Fusco A, Angioni S, Cicinelli E. Advantages of laparoscopy versus laparotomy in extremely obese women (BMI > 35) with early-stage endometrial cancer: a multicenter study. Anticancer Res. 2014;34:2497–502.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Tinelli, R., Cicinelli, E. (2018). Laparoscopic Hysterectomy (TLH) in Obese Patients. In: Alkatout, I., Mettler, L. (eds) Hysterectomy. Springer, Cham. https://doi.org/10.1007/978-3-319-22497-8_49
Download citation
DOI: https://doi.org/10.1007/978-3-319-22497-8_49
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22496-1
Online ISBN: 978-3-319-22497-8
eBook Packages: MedicineMedicine (R0)