Abstract
Obesity is having an increasingly significant impact on health care services across the developed world. Although initially laparoscopic surgery was thought to be contraindicated in cases of obesity, surgeons, including gynaecologists, are now routinely performing laparoscopic surgery on obese patients. Limited research has been conducted into the effect of obesity on outcomes of major laparoscopic pelvic surgery. Some authors report worsening outcomes in obese women having laparoscopic hysterectomies; others suggest that complication rates do not increase, but operating times are longer. Here, we report our experience from 250 total laparoscopic hysterectomies performed for benign, malignant and pre-malignant conditions, and we compare outcomes among normal, overweight, obese and morbidly obese patients. We used a composite score index calculated on the basis of operating and theatre times, estimated blood loss, length of stay and number and severity of complications for our comparisons. Our conclusions suggest that meticulous, consistent surgical technique may produce similar outcomes in normal and obese patients having total laparoscopic hysterectomy, with longer operating/theatre times noted only at BMI levels >40.
Similar content being viewed by others
Background
According to the Health Survey for England for 2013, 33 % of women were overweight and 24 % were obese [1]. Put together, these numbers suggest that more than half of the women in England have a body mass index (BMI) above 25, the upper normal limit according to the World Health Organisation (WHO) classification. The impact on health care services across the country has grown exponentially in the recent years. Estimates of the direct costs to the NHS for treating overweight and obese patients, and related morbidity in England, have ranged from approximately UK£500 million in 1998 to UK£4.2 billion in 2007 [2]. Surgical teams caring for these patients account for a large part of this burden. Obesity is an independent risk factor for peri-operative surgical morbidity across surgical specialties [3] and was initially considered a contra-indication to laparoscopic surgery. It is now well established that obese patients undergoing laparoscopic surgery benefit from the shorter hospital stays, less post-operative pain and fewer wound infections when compared with obese patients who undergo laparotomy [4]. Few studies have examined the relationship between obesity and outcomes of major pelvic laparoscopic surgery, such as laparoscopic hysterectomy. The majority of these studies include data from a mixture of laparoscopic-assisted vaginal hysterectomies and subtotal and total laparoscopic hysterectomies (TLH). Some authors report that compared to normal-weight patients, obese women tend to have worse peri- and post-operative outcomes [5]. Others suggest that complication rates do not increase, but that operating times are longer [6, 7]. Here, we compared the outcomes of women of different BMI groups undergoing TLH in our department over a period of 3 years.
Materials and methods
The electronic and paper notes of 250 patients who had TLH from June 2011 to May 2014 in our unit were reviewed retrospectively. Three laparoscopic gynaecological surgeons operated the patients (Table 1). Demographic and surgical details were recorded on Excel sheets. The surgical data extracted included surgical indication and procedure, operating and theatre time, estimated blood loss (EBL), length of stay (LOS) recorded in number of nights stayed in hospital, intra-operative and post-operative complications, readmissions, conversion to laparotomy and return to theatre rates.
The indications for TLH included benign conditions (pelvic pain/endometriosis, dysfunctional uterine bleeding, fibroids), gynaecological cancers or potential for cancer (early stage cervical or endometrial cancer, ovarian masses with no evidence of metastatic disease, endometrial hyperplasia with atypia, cervical intra-epithelial and glandular intra-epithelial neoplasia—CIN/CGIN) and patients with genetic pre-disposition for gynaecological cancer (prophylactic TLH and bilateral salpingo-oophorectomy).
The BMI was calculated according to the formula of weight (Kg)/height (m)2. The WHO BMI categorisation was used with the exception of the under-weight and normal-weight patients being grouped in the same category (BMI < 25) as we only had two under-weight patients.
To measure our primary outcome, we used a composite surgical outcome index, which has been described by Siedhoff et al. [5]. The method produces a score for each patient, i.e. a single number which represents the patient’s surgical outcome, through a point system which takes into account a number of features as shown in Table 2. The classification of complication severity follows the previously validated Clavien-Dindo classification of surgical complications [8].
Statistical analysis
The SPSS software was used for statistical analysis. The data failed to meet the specifications of a normal distribution. A non-parametric Kruskal-Wallis ANOVA was performed across the BMI categories to examine differences among their scores. Regression analysis was performed to investigate a possible correlation between score and BMI. p values below 0.05 were considered statistically significant.
Results
The present study included 250 patients who had TLH for benign, malignant or pre-malignant pathology. The mean age of our patient group was 52.7 and the mean BMI was 30.6. Table 3 shows the distribution of patients according to WHO BMI categories. Table 4 shows the indications for surgery.
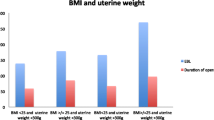
The mean operating time was 135 min (range, 58–342 min) and mean theatre time was 154 min (range, 81–362 min). The mean estimated blood loss (EBL) was 73 ml (range, 50–800 ml). The mean length of stay (LOS) was 1.3 nights (range, 1–4 nights). The breakdown of these data according to BMI category is shown in Fig. 1.
The overall complication in our case series was 2 % (Table 5). There was one conversion to laparotomy (0.4 % rate of conversion), due to difficulty in maintaining pneumoperitoneum. There was no haemorrhage large enough to require blood transfusion and no visceral injuries.
The mean index score for the 250 patients was 6.1 (range, 2–15). The mean scores for each BMI group and their standard deviations are shown in Fig. 2. The class III obesity group had the highest score and the differences between the score of this group and the scores of each of the other BMI groups were statistically significant. There were no statistically significant differences observed between the scores of the other four BMI groups. Regression analysis showed no significant correlation between the two variables, BMI and score (sig. >0.05, data not shown).
Discussion
Here, we present the outcomes of a case series of 250 TLHs performed in our unit for benign indications, gynaecological cancer and pre-malignant disease and we investigate the relationship between the surgical outcomes and the BMI of the patients operated on. To compare surgical outcomes, we used a composite score index to offset the relatively low number of patients and rarity of complications [5, 8, 9]. The highest mean composite score was observed in morbidly obese patients (BMI > 40).
Several studies have reported on outcomes of laparoscopic hysterectomies, including, in the same cohort of patients, total, subtotal and laparoscopically assisted vaginal hysterectomies. Such a large study was published by Donnez et al. in 2008 [10]. This was a retrospective review of 3190 laparoscopic hysterectomies, suggesting that the laparoscopic route is safe and beneficial to the patient when compared with abdominal hysterectomy. There are very few published case series of TLHs alone, which are large enough to be able to assess rates of rare complications. One of the largest such studies was published by Chopin et al. and included a cohort of 1460 TLHs [6]. Our outcomes were largely comparable with the outcomes of these authors. Our mean operating time was 139 min (compared to 132 min by Chopin et al.) and complication rates were either similar or lower. We noted a striking difference in length of stay with 1.4 days in our study compared to 3.5 for Chopin et al., which is probably evidence of the differences seen among surgical teams in managing their patients at the post-operative period. Elsewhere, Bonilla et al. reported their 5-year experience of 511 TLHs [11]. Again, complication rates were comparable with our study.
When attempting to compare surgical outcomes, large numbers of patients are required in order to reach statistical significance for complications such as visceral injuries, which usually have rates less than 1 %. To deal with this problem, Siedhof et al. suggested a composite index which compounds surgical outcomes into a single, easily interpretable score [5]. We observed the highest mean composite score in the morbidly obese patients group, mainly due to higher operating and theatre times. Despite the fact that this observation reached statistical significance, the clinical significance may be doubtful. In fact, our results indicate that the clinical perception, which suggests that laparoscopic surgery in the obese patient is more challenging and hence the outcome is likely to be worse with increasing BMI, may not be valid. The financial implications on the other hand may be more important. Longer theatre times translate to higher costs. In the UK, the average National Health Service (NHS) theatre cost is UK£20 per minute [12]. Therefore, the difference in mean theatre time of 35 min observed between normal-weight and morbidly obese patients in our series translates to significant differences in theatre operating costs.
Our observations are in agreement with those of Chopin et al. who suggested that when the operative technique is meticulous, surgical outcomes of laparoscopic hysterectomies are similar in normal, overweight and obese patients, although the operating time is longer for the latter group [6]. Another group of authors observed similar complication rates between obese and non-obese patients undergoing TLH [13]. The above studies grouped all their patients with BMI > 30 into one group, thus missing the opportunity to compare outcomes by various classes of obesity. In particular, Chopin et al., the largest series of TLHs alone investigating the correlation between complications and BMI, had a very uneven distribution of BMIs with only 7 % of their cases with BMI > 30 versus 53 % in our case series [6]. Other studies have examined the outcomes of a mixture of laparoscopic or robot-assisted gynaecological procedures in relation to patient BMI and found that obesity was not a risk factor for poor surgical outcome in their case series [14–17]. On the other hand, such findings are in contrast with Siedhof et al. This group reported their results from a cohort of 834 laparoscopic hysterectomies. As BMI increased, they observed an exponential increase in the composite index, an increase in operating and theatre time and a linear increase in EBL [5].
Our study carries a number of limitations. It is an observational retrospective study with the relevant inherent bias. It includes a relatively low number of patients and there is an imbalance in numbers of patients in the various BMI groups, in particular, a lower number of morbidly obese patients. Patients were operated on by three laparoscopic surgeons with different levels of experience. Due to the retrospective nature of the study, certain groups of data were incomplete. As a result, we were not able to examine the effect of confounding factors such as uterine weight and presence of dense adhesions to the surgical outcome, and thus single out BMI as the only likely risk factor. Finally, we grouped cancer patients and patients with benign conditions together, a selection that has been avoided by other similar studies.
Conclusions
In conclusion, we suggest that diligent and consistent surgical technique produces similar outcomes in normal-weight, obese and morbidly obese women requiring TLH. Differences in duration of surgery and theatre time may translate into higher operational costs for morbidly obese women. While this retrospective study carries a number of limitations, our results advocate the safety of major laparoscopic pelvic surgery in morbidly obese women. Certainly, this should not discourage clinicians from counselling their patients appropriately in relation to weight loss.
References
Health Survey for England (2013) http://www.hscic.gov.uk/catalogue/PUB16076
Butland B, Jebb S, Kopelman P, et al (2007) Tackling obesities: future choices – project report (2nd). London: Foresight Programme of the Government Office for Science. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07-1184x-tackling-obesities-future-choices-report.pdf
Bamgbade OA, Rutter TW, Nafiu OO, Dorje P (2007) Postoperative complications in obese and non-obese patients. World J Surg 31:556–561
Lamvu G, Zolnoun D, Boggess J, Steege JF (2004) Obesity: physiologic changes and challenges during laparoscopy. Am J Obstet Gynecol 191:669–674
Siedhoff MT, Carey ET, Findley AD, et al. (2012) Effect of extreme obesity on outcomes in laparoscopic hysterectomy. J Minim Invasive Gynecol 19:701–707
Chopin N, Malaret JM, Lafay-Pillet MC, et al. (2009) Total laparoscopic hysterectomy for benign uterine pathologies: obesity does not increase the risk of complications. Hum Reprod 24:3057–3062
Osler M, Daugbjerg S, Frederiksen BL, Ottesen B (2011) Body mass and risk of complications after hysterectomy on benign indications. Hum Reprod 26:1512–1518
Clavien PA, Barkun J, de Oliveira ML, et al. (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Erekson EA, Yip SO, Ciarleglio MM, Fried TR (2011) Postoperative complications after gynecologic surgery. Obstet Gynecol 118:785–793
Donnez O, Jadoul P, Squifflet J, Donnez J (2009) A series of 3190 laparoscopic hysterectomies for benign disease from 1990 to 2006: evaluation of complications compared with vaginal and abdominal procedures. BJOG 116:492–500
Bonilla DJ, Mains L, Rice J, Crawford B 3rd (2010) Total laparoscopic hysterectomy: our 5-year experience (1998-2002). Ochsner J 10:8–12
NHS Institute for Innovation and Improvement (2013) Evaluation of the Productive Operating Theatre Programme http://www.institute.nhs.uk/quality_and_value/productivity_series/the_productive_operating_theatre.html
Heinberg EM, Crawford BL 3rd, Weitzen SH, Bonilla DJ (2004) Total laparoscopic hysterectomy in obese versus nonobese patients. Obstet Gynecol 103:674–680
Camanni M, Bonino L, Delpiano EM, et al. (2010) Laparoscopy and body mass index: feasibility and outcome in obese patients treated for gynecologic diseases. J Minim Invasive Gynecol 17:576–582
George A, Eisenstein D, Wegienka G (2009) Analysis of the impact of body mass index on the surgical outcomes after robot-assisted laparoscopic myomectomy. J Minim Invasive Gynecol 16:730–733
Ghezzi F, Cromi A, Bergamini V, et al. (2006) Laparoscopic management of endometrial cancer in nonobese and obese women: a consecutive series. J Minim Invasive Gynecol 13:269–275
Bai SW, Lim JH, Kim JY, et al. (2002) Relationship between obesity and the risk of gynecologic laparoscopy in Korean women. J Am Assoc Gynecol Laparosc 9:165–169
Acknowledgments
This project was supported by a grant (“Inspire” grant) from the University of Liverpool.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Minas, V., Ventii, C., Murray, N. et al. Total laparoscopic hysterectomy for benign, malignant and pre-malignant gynaecological pathology: relation between surgical outcome and body mass index. Gynecol Surg 13, 493–497 (2016). https://doi.org/10.1007/s10397-016-0968-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-016-0968-y