Abstract
Biofilms, defined as a surface attached community of bacteria embedded in a matrix of extracellular polymeric substances, are a significant global health problem, causing considerable patient morbidity and mortality and contributing to the economic burden of infectious disease. Conventional antibiotics are largely ineffective against bacteria residing with a biofilm, necessitating alternative strategies to combat biofilms. Such strategies, which either inhibit biofilm formation or disperse existing biofilms, are ideally based upon a non-microbicidal approach, which avoids placing direct evolutionary pressure on the bacteria to develop resistance. Several such approaches are discussed in this chapter and range from the design of small molecules to interfere with the bacterial communication and signaling pathways that control biofilm formation and maintenance, such as quorum sensing and two-component signal transduction systems, to macromolecular approaches to biofilm eradication such as enzymatic degradation of the biofilm matrix and the development of biofilm-specific antibodies. When combined with conventional antibiotics that are effective against planktonic bacteria, the strategies discussed here have the potential to eradicate biofilm based bacterial infections and have a significant impact upon human health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Extracellular Polymeric Substance
- Quorum Sense
- Planktonic Bacterium
- Ferric Ammonium Citrate
- Conventional Antibiotic
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The identification of novel targets and compound-scaffolds to combat biofilms is a valuable tool in the fight against infectious diseases, many of which are now known to be biofilm-mediated. Continuing research into the environmental cues and genetic elements that play a part in the regulation of biofilms, such as quorum sensing, two-component signal transduction systems, cyclic-di-GMP signaling, and indole-signaling, along with an evolving knowledge of the composition of biofilms, has led to numerous innovative strategies for combating biofilms.
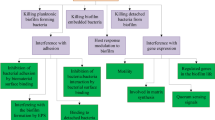
Strategies to inhibit biofilm formation, and/or eradicate established biofilms, have the potential to have a profound impact on human medicine by enhancing the efficacy of antibiotics that are otherwise ineffective against biofilm bacteria. Controlling biofilm development via non-microbicidal mechanisms should limit the pressure on bacteria to evolve resistance as compared to the selective pressures exerted by conventional bactericidal entities. Here, we aim to provide an overview of the various strategies that have been explored for the inhibition or eradication of bacterial biofilms, focusing on strategies that operate via non-microbicidal mechanisms. These approaches range from: effecting phenotype shifts through controlling cell-signaling pathways with small molecules, to enzymatic approaches to biofilm eradication by matrix degradation. Such strategies have the potential, when paired with conventional antibiotics that will kill planktonic bacteria, to eliminate established biofilm infections.
1.1 Biofilms
Biofilms, defined as highly organized surface-associated communities of bacteria encased within an extracellular matrix, play a significant role in infectious disease. Biofilms contribute to both pathogenesis and antibiotic/host immune resistance, and have a considerable impact on many fields, including medicine, food, environment, and industry. The impact of biofilms upon infectious disease is a particular cause for concern given the fact that The National Institutes of Health (NIH) estimates that 80 % of all bacterial infections occurring in the human body are biofilm related, and it is estimated that 17 million new biofilm infections arise each year in the U.S., resulting in up to 550,000 fatalities (Quave et al. 2012). Biofilms play a role in lung infections of cystic fibrosis (CF) patients, burn wound infections, ear infections, bacterial endocarditis, chronic wound infections, and tooth decay (Musk and Hergenrother 2006). In addition to increased mortality rates, biofilm mediated infections impart a considerable economic burden; with device related biofilm infections adding over one billion dollars to US hospitalization costs annually (Shirtliff and Leid 2009). The total economic impact of biofilms to the agricultural, engineering, and medical sectors of society has been estimated at billions of dollars annually (Davies 2003).
Bacteria within a biofilm present a number of characteristics that lead to difficulties in their eradication. They are phenotypically distinct from their planktonic counterparts, particularly in regard to growth rates and gene expression (Donlan and Costerton 2002). Biofilms are inherently insensitive to antibiotics, exhibiting upwards of 1000-fold higher resistance than planktonic bacteria (Rasmussen and Givskov 2006). Furthermore, the higher cell densities found within a biofilm (1011 CFU/mL compared to 108 CFU/mL for bacteria in the planktonic state) vastly increase the opportunity for horizontal gene transfer, with transfer rates of up to 1,000-fold higher than for planktonic cells (Hausner and Wuertz 1999), leading to an increased likelihood of the emergence of strains with increased resistance or altered virulence profiles (Quave et al. 2012).
1.2 Effectiveness of Conventional Antibiotics in Eradicating Biofilms
There are many factors that lead to the increased resistance bacteria exhibit towards antibiotics while in a biofilm state. These include changes in gene expression related to antibiotic resistance, such as upregulation of genes responsible for efflux pumps (Davey and O’Toole 2000). The biofilm matrix, which is predominantly comprised of self-produced extracellular polymeric substances (EPS) including carbohydrates, proteins, lipids and extracellular DNA, affects penetration of certain antibiotic classes into the biofilm (Mah and O’Toole 2001; Flemming et al. 2007). The reduced growth rate exhibited by cells embedded deep within the biofilm that experience a lack of nutrients and oxygen also likely plays a role in resistance to antibiotics (Mah and O’Toole 2001), as bacterial cells with reduced metabolic activity are inherently more recalcitrant to antimicrobial therapies (Spoering and Lewis 2001). This reduced efficacy is due to the fact that almost all conventional antibiotics target one of five biosynthetic processes occurring in actively growing bacteria: the biosynthesis of proteins, RNA, DNA, peptidoglycan and folic acid (Hurdle et al. 2011). In the absence of genetic resistance mechanisms, conventional antibiotics efficiently kill growing and dividing bacterial cells, but are very inefficient at killing non-multiplying bacteria (Coates and Hu 2008), leading to minimal inhibitory concentrations (MICs) of conventional antibiotics against biofilm-residing bacteria being 100-1,000-fold higher than against planktonic bacteria (Hoiby et al. 2010a).
Despite this recalcitrance, certain conventional antibiotics have demonstrated activity against bacterial cells growing in the biofilm state. For example, rifampin has activity against staphylococcal biofilm cells, particularly when used in combination with one or more additional antibiotic including: fusidic acid, vancomycin and ciprofloxacin (Saginur et al. 2006). Colistin has demonstrated activity against non-dividing Pseudomonas aeruginosa biofilm cells that reside at the center of a biofilm; however metabolically active cells can acquire resistance to polymyxins and other cationic peptides rapidly due to modification of their outer membrane. Therefore, colistin appears to only be a viable option for treating P. aeruginosa biofilm infections when used in combination with another antibiotic such as ciprofloxacin (Hoiby et al. 2010a). Even more problematic is the fact that several studies have shown that the presence of sub-MIC levels of some antibiotics, as experienced at the beginning or end of a dosing regimen, or by cells deep within the biofilm throughout the regimen, can induce in vitro biofilm formation in a range of bacteria. Almost all the most commonly used antibiotic classes including: aminoglycosides, ß-lactams, fluoroquinolones, glycopeptides, rifamycins, tetracyclines exhibit this phenomenon. This has prompted a need to develop alternative strategies to combat biofilms (Kaplan 2011).
2 Small Molecule Strategies for Combating Biofilms
Several approaches to the design of small molecules that either inhibit the formation of biofilms, or cause established biofilms to disperse, have been investigated. Many of these approaches involve designing small molecules to interfere with the bacterial communication pathways that control the formation and maintenance of biofilms. Additionally, many natural products possess anti-biofilm activity and have been used as structural inspiration in medicinal chemistry programs to identify anti-biofilm compounds. These strategies are detailed below.
2.1 Disruption of Quorum Sensing Pathways
Quorum sensing (QS) involves intercellular communication between bacteria via the production of diffusible small molecules, and allows the community to make coordinated alterations in gene expression based upon population density (Camilli and Bassler 2006). There exist a number of different quorum sensing molecules that have been shown to play a role in the formation of biofilms in numerous species of bacteria. These include: acyl homoserine lactones (AHLs) in Gram-negative bacteria, autoinducer peptides (AIPs) employed by Gram positive bacteria, and autoinducer-2 (AI-2) molecules derived from 4,5-dihydroxy-2,3-pentanedione (DPD), which are interspecies signals employed by both Gram-negative and Gram-positive bacteria (Irie and Parsek 2008). The approach of interfering with QS pathways to modulate biofilm formation has been one of the most popular approaches to combating biofilms and a number of small molecules that modulate QS pathways have been developed.
Acyl Homoserine Lactones (AHLs)
AHLs are the predominant QS signal employed by Gram-negative bacteria, and more than 70 species of bacteria are known to communicate via AHL-mediated QS, with specificity mediated via variation in the length and oxidation state of the acyl side chain (for example, compounds 1–3) (Fig. 6.1) (Amara et al. 2009). In the well-studied QS system of Vibrio fisheri, AHL synthesis occurs when the luxI gene is activated, producing the AHL synthase enzyme LuxI. When the AHL reaches a threshold intracellular concentration, it binds to the transcriptional activator LuxR, leading to activation of the luxR operon. AHLs freely diffuse in and out of bacterial cells allowing the AHL concentration to correlate to the bacterial concentration, which enables population density-based control of gene expression and therefore control of various processes such as biofilm formation and maintenance (Finch et al. 1998). Homologous systems to the LuxI and LuxR proteins exist in several Gram-negative bacteria, including LasI and LasR in the medically important biofilm-forming bacterium P. aeruginosa (Parsek and Greenberg 2000). The role of AHL based QS in biofilm development was first demonstrated by the discovery that a P. aeruginosa lasI mutant forms biofilms with altered morphology and reduced thickness compared to the wild type strain, and that the mutant biofilms are sensitive to biocides. Exogenous addition of the synthetic QS ligand to the mutant strain resulted in biofilms that resembled the wild-type and restoration of biocide resistance (Davies et al. 1998).
AHLs are prone to hydrolysis at physiological pH and the ring-opened product is QS inactive, and they have also been reported to possess immunomodulatory activity (Yates et al. 2002). This has led to the design of several synthetic AHL analogues with the aim of improving stability and in vivo properties. Recently, the Blackwell group have documented the synthesis and identification of a number of natural and unnatural AHLs with the ability to modulate QS in P. aeruginosa and Agrobacterium tumefaciens, and demonstrated that two of the most active AHL analogues inhibit biofilm formation in P. aeruginosa PAO1. Significant inhibition of biofilm formation was observed for a green fluorescent protein (GFP) producing PAO1 strain in the presence of synthetic AHLs 4 and 5 (Fig. 6.1) at 50 μM (Geske et al. 2005). The N-acyl cyclopentylamide analogue, C10-CPA 6, completely prevents biofilm formation by GFP labeled P. aeruginosa PAO1 at 250 μM under flow conditions (Ishida et al. 2007).
A series of inhibitors of the P. aeruginosa transcriptional regulator LasR bearing electrophilic functional groups, including isothiocyanates, bromoacetamides, and chloroacetamides, were designed to react with Cys79 in the LasR binding pocket. Isothiocyanate containing ligands were able to covalently and selectively bind Cys79 and inhibit quorum sensing, with compound, 7 (Fig. 6.1), inhibiting PAO1 biofilm formation by almost 50 % at a concentration of 50 μM (Amara et al. 2009). More recently, the thiolactone 8 was reported by the Bassler group and reduces P. aeruginosa biofilm height by almost threefold at 100 μM, and brings about a reduction in nematode death in a Caenorhabditis elegans P. aeruginosa infection assay at 50 μM (O’Loughlin et al. 2013).
Autoinducing Peptides (AIPs)
QS in Gram-positive bacteria is predominantly mediated by autoinducing peptides (AIPs) (Lyon and Novick 2004). The accessory gene regulator (agr) operon, which plays an important role in biofilm formation in Staphylococcus aureus, contains the agrD gene, which encodes AgrD, the precursor of the S. aureus AIP 9 (Fig. 6.2). The S. aureus AIP binds AgrC, a histidine kinase, leading to the expression of a small non-coding RNA known as RNA-III, which subsequently down-regulates genes that encode adhesins required for biofilm formation (Bordi and de Bentzmann 2011). The RNA-III activating protein (RAP) activates TRAP (target of RNA-III activating peptide) via phosphorylation, leading to increased cell adhesion and biofilm formation (Fux et al. 2003). The RNA-III inhibiting peptide (RIP) 10 inhibits phosphorylation of TRAP leading to reduced biofilm formation, and RIP has been investigated as an anti-biofilm agent, successfully preventing infections in multiple animal models (Giacometti et al. 2003). AIP analogues have also been investigated as anti-biofilm agents; the truncated peptide 11 is a potent AgrC QS antagonist (Chan et al. 2004), while the peptidomimetic 12 promotes biofilm formation in S. aureus (Fowler et al. 2008), and the synthetic RIP derivative FS3 13 (Fig. 6.2) enhances the efficacy of tigecycline in a rat model of staphylococcal vascular graft infection (Simonetti et al. 2013).
Autoinducer-2 (AI-2)
Autoinducer-2 (AI-2) is the collective term for a number of autoinducing signals derived from DPD 14 (Fig. 6.3). The synthase that drives DPD production is conserved in over 55 bacterial species (Waters and Bassler 2005) and AI-2 has been proposed as a putative universal quorum sensing mechanism shared by both Gram-negative and Gram-positive bacteria. The structures of AI-2 from Vibrio harveyi (S-THMF borate 15) and Salmonella typhimurium (R-THMF 16) are depicted in Fig. 6.3 (Miller et al. 2004).
Several AI-2 analogues have been developed, including the C4-alkoxy-5-hydroxy-2,3-pentanediones 17 and 18 (Fig. 6.3), which activate the AI-2 pathway more potently than DPD, exhibiting submicromolar EC50 values in a V. harveyi reporter strain (Tsuchikama et al. 2012). Several C1-substituted DPD analogues act as antagonists of AI-2-based QS, with propyl-DPD 19 and butyl-DPD 20 exhibiting IC50 values tenfold below that of DPD (Lowery et al. 2008). Another C1-substituted analogue, isobutyl-DPD 21 significantly inhibits maturation of Escherichia coli biofilms and also brings about near complete clearance of pre-formed E. coli biofilms when administered in combination with gentamicin (Roy et al. 2013).
Another approach to interfering with AI-2 signaling is to design compounds that inhibit synthesis of the signal itself. The biosynthesis of DPD begins from S-adenosyl methionine (SAM), therefore a number of nucleoside analogues have been evaluated as potential inhibitors, with the finding that the adenosine analogue 22 (Fig. 6.3) blocks AI-2-based QS without affecting bacterial growth. This compound was subsequently shown to affect biofilm formation in several Vibrio species (Brackman et al. 2009). Another enzyme involved in the biosynthesis of both AI-2 and AHLs is 5′-methylthioadenosine nucleosidase (MTAN), which catalyzes the N-glycosyl hydrolysis of SAM and other adenosyl derivatives (Ronning et al. 2010; Gutierrez et al. 2009). Transition state analogues 23, 24, and 25 (Fig. 6.3) inhibit MTAN activity in cell lysates of a virulent Vibrio cholerae strain with nanomolar IC50 values, and inhibit QS induction in V. harveyi reporter strains. Analogues 23 and 25 also inhibit MTAN in E. coli, resulting in inhibition of AI-2 production, while compound 25 reduces biofilm formation in E. coli and V. cholerae by 18 and 71 % respectively at a concentration of 1 μM without inhibiting planktonic growth (Gutierrez et al. 2009).
2.2 Small Molecule Disruption of Other Signaling Pathways
c-di-GMP
Bis-(3′5′)-cyclic di-guanylic acid (c-di-GMP) 26 (Fig. 6.4) is a ubiquitous second messenger bacterial signaling molecule. Diguanylate cyclases (DGCs) and phosphodiesterases (PDEs), which are responsible for the synthesis and breakdown of c-di-GMP, respectively (Yan and Chen 2010) are regulated by various environmental and intracellular signals such as oxygen, light, and small molecules, and play a role in the transition between the planktonic and biofilm lifestyle in P. aeruginosa (Tamayo et al. 2007). It has been observed that exopolysaccharide (a component of the biofilm matrix) synthesis is regulated by c-di-GMP in various proteobacterial species including V. cholera, P. aeruginosa, Pseudomonas fluorescens, A. tumefaciens, E. coli, and Salmonella enterica (Ryjenkov et al. 2005), while dispersion of bacteria from a mature biofilm is also thought to be regulated by c-di-GMP (Tamayo et al. 2007).
Interfering with c-di-GMP signaling is therefore another attractive target for the control of biofilm formation. Modification of the 2′ position of c-di-GMP generates analogues with selectivities for different classes of c-di-GMP binding proteins, and the 2′-fluoro analogue 27 exhibits higher affinity for DGCs than does the native ligand (Zhou et al. 2013). Screening of a 1,120 compound library with known biological activities identified sulfathiazole 28 (Fig. 6.4), which inhibits DGC activity and inhibits E. coli biofilm formation with an IC50 value of 5.8 μM without significantly inhibiting bacterial growth (Antoniani et al. 2010). The benzimidazole 29 was identified from a high-throughput screen (HTS) of approximately 66,000 compounds and natural-product extracts from the Center for Chemical Genomics at the University of Michigan for compounds that affect induction of a V. cholerae c-di-GMP-inducible transcriptional fusion. Compound 29 is a broad-spectrum inhibitor of biofilm formation, significantly inhibiting biofilm formation by P. aeruginosa (CF-145), Klebsiella pneumoniae, Erwinia amylovora, and Shigella boydii, at 100 μM and by MRSA USA300, and S. aureus Newman at 25 μM, without affecting bacterial growth. IC50 values for inhibition of biofilm formation by P. aeruginosa and V. cholerae were reported to be 45.9 and 32.3 nM, respectively, however compound 29 did not disperse pre-formed biofilms (Sambanthamoorthy et al. 2011).
Another small molecule, compound 30, was identified from a high-throughput screen for inhibitors of DGCs and shown to significantly reduce c-di-GMP levels in V. cholerae and inhibit biofilm formation by V. cholerae and P. aeruginosa (Sambanthamoorthy et al. 2012). In other studies, ebselen 31 and ebselen oxide 32 were shown to reduce DGC activity by covalently modifying cysteine residues, leading to inhibition of c-di-GMP-receptor binding and subsequent inhibition of biofilm formation in P. aeruginosa (Lieberman et al. 2014).
Indole Signaling
Indole is another putative universal intercellular signal molecule (Lee and Lee 2010) that plays a role in the control of many behaviors including biofilm formation (Lee et al. 2007b). Eighty-five species of bacteria have been documented to produce indole, with both indole-positive and indole-negative strains of bacteria altering various behaviors upon the extracellular presence of indole (Lee and Lee 2010). E. coli produces high concentrations (>600 μM) of extracellular indole when cultured in rich medium and indole has been shown to decrease biofilm formation in E. coli in a non-toxic manner (Lee et al. 2007a). Indole is readily converted by oxygenases found in several bacterial species to a number of oxidized indole derivatives, such as hydroxyindoles 33–35, isatin 36, and isoindigo 37 (Fig. 6.5), which have been investigated for their effects on biofilm formation. 5-Hydroxyindole 33 and 7-hydroxyindole 34 inhibit biofilm formation by enterohemorrhagic E. coli (EHEC) by 11-fold and 27-fold respectively at a concentration of 1 mM, compared to 18-fold inhibition by indole at the same concentration (Lee et al. 2007a). Indole-3-acetaldehyde, 38, which is produced by the plant pathogen Rhodococcus sp. BFI 332, inhibits biofilm formation by EHEC without affecting planktonic growth, while the spent medium of Rhodococcus sp. BFI 332, from which 38 was identified, was shown to have an inhibitory effect on biofilm formation by two Staphylococcal species, S. aureus and Staphylococcus epidermidis (Wood et al. 2008).
The plant secondary metabolites 3-indolylacetonitrile (IAN) 39 and indole-3-carboxyaldehyde (I3CA) 40 (Fig. 6.5) reduce biofilm formation by E. coli O157:H7 by 11-fold and 24-fold respectively at 100 μg/mL, compared to a threefold reduction brought about by indole. In contrast to indole and the hydroxyindoles, which promote biofilm formation by P. aeruginosa PAO1, 39 and 40 weakly inhibit biofilm formation by this bacterium, effecting a 1.9-fold and 2.3-fold reduction in respectively (Lee et al. 2011a). A follow up study to identify indole derivatives with increased anti-virulence activity compared to IAN 39, identified the simple synthetic indole derivatives, 7-fluoroindole (7FI) 41, and 7-formylindole 42, which reduce P. aeruginosa biofilm formation by fourfold and fivefold respectively at concentrations of 1 mM (Lee et al. 2012).
The pyrroloindoline and indole containing monobrominated secondary metabolites from the bryozoan Flustra foliacea (Peters et al. 2003) have been used as scaffolds for the design of compounds to interfere with indole signaling. One metabolite, desformylflustrabromine (dFBr) 43 (Fig. 6.5) inhibits biofilm formation by E. coli and S. aureus with IC50 values of 70 μM and 174 μM respectively, however this compound exhibits microbicidal effects on planktonic growth at these concentrations (Bunders et al. 2011b). Synthetic manipulation of various regions of the dFBr scaffold led to the identification of 44, which inhibits biofilm formation by S. aureus and E. coli with IC50 values of 5.9 μM and 53 μM respectively, and compound 45, which inhibits biofilm formation by S. aureus and E. coli with IC50 values of 7.7 μM and 15.6 μM respectively. Both compounds elicit their effects through a non-microbicidal mechanism. Mechanistic studies with both compounds in wild-type and knockout E. coli strains revealed that the activity of these indole derivatives is dependent on the same factors as the activity of indole itself, namely temperature, the transcriptional regulator SdiA, and tryptophanase, suggesting that the observed anti-biofilm activity may be occurring through modulation of indole-based signaling pathways (Bunders et al. 2011b; Minvielle et al. 2013b). Other flustramine derived small molecules with non-microbicidal anti-biofilm activity include compound 46, which inhibits biofilm formation by Acinetobacter baumannii with an IC50 value of 193 μM, compound 47, which inhibits biofilm formation by E. coli with an IC50 value of 36 μM, and compounds 48 and 49, which exhibit Gram-positive anti-biofilm activity, inhibiting biofilm formation by S. aureus (Bunders et al. 2011a; Minvielle et al. 2013a).
Two-Component Systems
Two component signal transduction systems (TCS) are a class of regulatory systems found mainly in prokaryotes that allow the organism to sense and respond to changes in their environment. The prototypical TCS consist of a histidine kinase and a response regulator. In response to an extracellular signal, the histidine kinase undergoes autophosphorylation at a conserved histidine residue. The phosphorylated histidine kinase subsequently transfers the phosphate group to a conserved aspartate residue on the response regulator that results in activation of an effector domain and ultimately leads to the response, which typically involves altered gene expression (Stock et al. 2000). TCS regulate the expression of genes that control numerous behaviors including biofilm formation and maintenance (Gotoh et al. 2010). Examples of TCS involved in biofilm regulation include, AgrAC (S. aureus) (Gotoh et al. 2010) LytSR (S. aureus) (Sharma-Kuinkel et al. 2009), BfmRS (A. baumannii) (Tomaras et al. 2008) BfmRS (P. aeruginosa) (Petrova et al. 2011), GacAS (P. aeruginosa) (Parkins et al. 2001) and VicRK (S. mutans) (Reck et al. 2011).
The role of TCS in the control of biofilm formation and maintenance, and the fact that it has been demonstrated that both the histidine kinase and response regulator are targetable by small molecules makes them attractive targets for the development of anti-biofilm compounds (Worthington et al. 2013). Walkmycin C 50 (Fig. 6.6), a member of the walkmycin family of natural products produced by Streptomyces sp. strain MK632-100 F11, inhibits autophosphorylation of the histidine kinase WalK (YycG) from both B. subtilis and S. aureus, and was subsequently shown to inhibit the in vitro autophosphorylation activity of purified VicK (an orthologue of WalK that is involved in sucrose dependant biofilm formation) from Streptococcus mutans with an IC50 of 2.87 μM. At sub-MIC levels, walkmycin C causes the formation of abnormal biofilms and a reduction in biofilm mass (37.6 % of the control at 0.63 μg/mL) in S. aureus (Eguchi et al. 2011). Walkmycin C also inhibits the histidine kinase CiaH in S. mutans, which plays a role in sucrose-dependent biofilm formation, with an IC50 of 4.87 μM (Qi et al. 2004). The bacterial secondary metabolite carolacton 51, affects the viability of S. mutans biofilms at nanomolar concentrations, killing bacterial cells that are within a biofilm state while exhibiting only minor effects on the growth of planktonic bacteria. Carolacton was subsequently shown to affect the expression of several TCS in S. mutans biofilm cells, two of which (VicKRX and ComDE) were shown to play essential roles in the response to carolacton. It was shown that this response is mediated through the serine/threonine protein kinase PknB, which the authors posited could be due to phosphorylation of VicR by PknB Although the effect of carolacton upon S. mutans biofilms is microbicidal, the selectivity toward biofilm bacteria over planktonic bacteria represents an alternative strategy for the small molecule control of biofilms and validates targeting of TCS as a means of controlling bacterial biofilms (Reck et al. 2011; Kunze et al. 2010).
Other Signaling Molecules
The fatty acid signaling molecule, cis-2-decenoic acid 52 (Fig. 6.6), which is produced by P. aeruginosa, has been shown to induce the dispersion of established biofilms of several bacterial species when assayed using microcolony disaggregation and measurement of the number of cells released into the bulk culture medium as the readout of biofilm dispersion (Davies and Marques 2009). The ability of cis-2-decenoic acid 52 to disperse pre-formed biofilms of A. baumannii and S. aureus has also been assayed with a crystal violet reporter assay, which measures the biofilm mass remaining as a function of compound concentration. However, under these conditions less than 10 % dispersion was observed at a concentration of 400 μM (Su et al. 2011). Another fatty acid, cis-11-methyl-2-dodecenoic acid 53, known as diffusible signal factor (DSF), produced by Xanthomonas campestris, is able to disaggregate cell flocs formed by X. campestris (Dow et al. 2003). The fatty acid-derived molecule palmitoyl-DL-carnitine 54 (Fig. 6.6) inhibits biofilm formation by P. aeruginosa PAO1, E. coli, and Listeria monocytogenes with IC50 values of 13.2, 3.00 and 5.85 μM respectively, but does not disperse pre-formed biofilms (Wenderska et al. 2011; Nguyen et al. 2012).
Certain D-amino acids produced by bacteria in the stationary phase are thought to be a native signal for biofilm disassembly in B. subtilis, and exhibit inhibitory effects upon biofilm formation by several bacteria including B. subtilis, S. aureus and P. aeruginosa. This activity is thought to be a result of disruption of the connection between an extracellular matrix protein and the bacterial cell, which is posited to prevent growth of initial foci into larger assemblies of cells. D-Tyrosine, D-leucine, D-tryptophan, and D-methionine synergistically inhibit biofilm formation by B. subtilis, exhibiting activity at 10 nM in combination, while only displaying activity at micromolar to millimolar concentrations when administered alone. The analogous L-amino acids, and other D-amino acids including D-alanine and D-phenylalanine were inactive. Against S. aureus, the combination of D-phenylalanine, D-proline, and D-tyrosine exhibit greater biofilm inhibitory activity than the combination of D-tyrosine, D-leucine, D-tryptophan, and D-methionine (Kolodkin-Gal et al. 2010; Hochbaum et al. 2011).
2.3 Metal Ions and Chelation
Some metal ions play an important role in biofilm formation, stimulating cell–cell adhesion and aggregation (Abraham et al. 2012), and the effect of metal ion chelation upon biofilm formation has been investigated as a strategy to combat biofilms. Ethylenediaminetetraacetic acid (EDTA) was shown to disperse P. aeruginosa biofilms and result in 1,000-fold enhanced killing by gentamicin (Banin et al. 2006), while a combination of EDTA and minocycline effectively reduced in vitro and ex vivo staphylococcal catheter colonization (Raad et al. 2003).
A screen of 4,500 compounds belonging to the University of Illinois Marvel Library Compound Collection (MLCC) led to the identification of ferric ammonium citrate (FAC) 55 (Fig. 6.7) as a non-toxic inhibitor of P. aeruginosa PA14 biofilms, exhibiting an IC50 value of approximately 60 μM. No toxicity was observed even upwards of 500 μM and it was shown that neither the ammonium nor citrate ions were responsible for the observed anti-biofilm activity. The subsequent analysis of other iron salts (ferric chloride, ferric sulfate, ferrous sulfate) revealed biofilm inhibitory profiles that were comparable to that of FAC and it was also demonstrated that upon switching to an iron-rich growth media established P. aeruginosa biofilms could be disrupted and cleared in continuous flow experiments (Musk et al. 2005). High iron levels have been shown to suppress extracellular DNA (eDNA) release and structural development of biofilms in P. aeruginosa, and it is thought that biofilm formation by P. aeruginosa can only occur in a narrow iron concentration range (1–100 μM) (Yang et al. 2007). Iron chelated by either picolinic acid or acetohydroxamic acid prevents biofilm formation by P. aeruginosa PA14 and also by 20 clinical isolates of P. aeruginosa (Musk and Hergenrother 2008). Additionally, at sub-MIC levels the antibiotic nitroxoline 56 inhibits de novo P. aeruginosa biofilm synthesis with little microbicidal activity toward planktonic bacteria. The thickness of preformed biofilms was also reduced by 40 % by nitroxoline at 8 μg/mL, and iron and zinc complexation was shown to underlie the activity of nitroxoline (Sobke et al. 2012).
A high-throughput screen of 66,095 small molecules by Junker and Clardy identified several compounds that inhibit PAO1 biofilms with IC50 values below 20 μM, the structures of some of which lead the authors to posit that they act via metal chelation. The most active compound identified, 57 (Fig. 6.7), exhibits an IC50 value of 530 nM in minimal media, making it one of the most potent biofilm inhibitors reported to date (Junker and Clardy 2007).
The plant derived sugar 1,2,3,4,6-penta-O-galloyl-b-n-glucopyranose (PGG) 58, which inhibits biofilm formation by S. aureus by preventing surface attachment of cells and reducing the production of the important matrix component polysaccharide intercellular adhesin (PIA), is a strong iron chelator and it has been shown that addition of FeSO4 restores biofilm formation and PIA production, indicating that metal ion chelation is the mechanism of biofilm inhibition by PGG (Lin et al. 2012).
2.4 Natural Products and Natural Product Analogues
Natural products provide a diverse array of chemical structures and possess a plethora of biological activities. Natural products that inhibit or disperse bacterial biofilms provide a starting point for medicinal chemistry programs from which more efficacious compounds can be developed, and may even lead to the identification of new anti-biofilm targets. Much of the natural product inspiration for these programs has come from compounds isolated from plants and marine organisms.
2.4.1 Plant Natural Products
Interest in studying natural products derived from plant sources for the discovery of new biologically active compounds is not uncommon, and many traditional medicines have been rooted heavily in the use of plant extracts (Lai and Roy 2004). The antibiotic properties of garlic have long been known and can be attributed to the disulfide allicin 59 (Fig. 6.8) (Slusarenko et al. 2008). P. aeruginosa biofilms treated with garlic extracts in vitro exhibit enhanced susceptibility to treatment with tobramycin and to grazing by polymorphonuclear (PMN) leukocytes, and garlic extracts have also been shown to clear pulmonary P. aeruginosa infections in mouse models when dosed prophylactically (Bjarnsholt et al. 2005). Compounds identified as being responsible for these activities include the dithianes 60 and 61, which have been shown to modulate QS in LuxR systems and do not display microbicidal activity (Persson et al. 2005).
Extracts from Rubus ulmifolius (Elmleaf blackberry), which are rich in the polyphenol ellagic acid 62 and its glycosylated derivatives, inhibit biofilm formation by S. aureus at concentrations of 50–200 μg/mL, and ellagic acid alone also possesses anti-biofilm properties (Quave et al. 2012). The resin acid 4-epi-pimaric acid 63, which was isolated from Aralia cachemirica L. (Araliaceae), inhibits biofilm formation by S. mutans on a saliva-coated surface at sub-MIC concentrations (4 μg/mL) (Ali et al. 2012). Resveratrol, which is found in the skin of grapes and berries, inhibits biofilm formation by V. cholerae (Augustine et al. 2014). Several flavonoids from citrus species, including naringenin 64, and quercetin 65, are antagonists of AHL and AI-2-mediated cell–cell signaling in V. harveyi, and also inhibit biofilm formation by V. harveyi and E. coli by over 80 % at 50 μM (Vikram et al. 2010). The antioxidant phloretin 66 (found in apple tree leaves) reduces biofilm formation by EHEC O157:H7 by 89 % at 25 μg/mL without affecting the growth of planktonic cells and also without affecting commensal E. coli K-12 biofilms. This is significant as the eradication of commensal bacteria by conventional antibiotics is a major problem and can result in increased susceptibility to infection by opportunistic pathogens, making antibacterial strategies that selectively eliminate pathogenic bacteria a potential future therapeutic avenue for human medicine. Phloretin represses several genes including those encoding toxins, AI-2 importer genes, and curli genes, and reduces fimbria production in EHEC biofilm cells (Lee et al. 2011b). The triterpene ursolic acid 67 (Fig. 6.8), which was identified from a screen of 13,000 compounds, inhibits E. coli biofilm formation at 22 μM without affecting growth, upregulating genes responsible for several processes tied to biofilm formation including: chemotaxis, motility, and heat shock (Ren et al. 2005).
2.4.2 Marine Natural Products
Halogenated Furanones
Much research has centered on the biological activities and effects that halogenated furanones (HFs) have on bacterial QS (Hentzer et al. 2002; Manefield et al. 2002; Ren et al. 2001). HFs were isolated from the marine red algae Delisea pulchra and exhibit structural similarities to AHLs, possessing a non-polar aliphatic carbon “tail” of varying lengths attached to a relatively polar “head”. Naturally occurring HFs inhibit biofilm formation and swarming in E. coli and B. subtilis at 20–60 μg/mL (Ren et al. 2001, 2002), Synthetic manipulation of the furanone scaffold has resulted in a number of HF analogues anti-biofilm activity. HFs have been shown to inhibit luminescence in V. fischeri, to affect the expression of numerous genes involved in virulence factor production and biofilm formation in P. aeruginosa (Hentzer et al. 2003; Rasmussen et al. 2000) and to penetrate P. aeruginosa biofilm matrices and interfere with bacterial QS, without any associated microbicidal properties (Hentzer et al. 2002). HF 68, which lacks a side chain and possesses a vinyl bromide, is one analogue that exhibits such activity. Biofilms grown in the presence of HF 68, display noticeable changes in biofilm maturation and structure, similar to those observed in P. aeruginosa mutants lacking the lasI system. The furanone causes rapid bacterial detachment, resulting in a loss of biomass in comparison to untreated biofilms, while other experiments have shown that furanone treated biofilms are sensitized to tobramycin (Hentzer et al. 2003). HF 68 also exhibits activity against Gram-positive biofilms, effecting a 63 and 76 % reduction in growth of S. mutans and Streptococcus intermedius biofilms respectively at a concentration of 60 μM (Lonn-Stensrud et al. 2007). HFs 69, 70, and 71 inhibit E. coli biofilm formation by up to 80 % at concentrations of 224 μM (69 and 70) and 141 μM (71) (Han et al. 2008), while furanones 72–76, which contain an exocyclic ester functionality and are non-brominated, are effective inhibitors of P. aeruginosa biofilm formation (Kim et al. 2008) (Fig. 6.9).
Despite this promising activity, there are some issues with halogenated furanones that currently limit their therapeutic application, including toxicity, carcinogenic properties, and instability under aqueous conditions (Hentzer and Givskov 2003) Future medicinal chemistry efforts will be necessary to overcome some of these limitations.
2-Aminoimidazoles
The marine alkaloids oroidin 77 and bromoageliferin 78 (Fig. 6.10) are nitrogen-dense small molecules characterized by the incorporation of one or more 2-aminoimidazole (2-AI) sub-units that are produced by marine sponges of the family Agelasidae (Braekman et al. 1992). They are believed to a play a role as a chemical anti-feeding defense mechanism against predators, and were first reported to inhibit biofilm formation by the Gram-negative marine α-proteobacterium Rhodospirillum salexigens in 1997, exhibiting IC50 values of 169 μM and 2.43 nM respectively (Yamada et al. 1997).
These alkaloids have been used as structural inspiration for the development of simplified, synthetically accessible small molecules with anti-biofilm activity. Two simplified analogues of bromoageliferin: TAGE (trans-bromoageliferin) 79 and CAGE (cis-bromoageliferin) 80 (Fig. 6.10) inhibit biofilm formation by P. aeruginosa via a non-microbicidal mechanism, while TAGE also disperses established P. aeruginosa biofilms (Huigens et al. 2007). Installation of di-brominated acylpyrrole moieties similar to those present in bromoageliferin onto the TAGE scaffold results in compound 81, which exhibits increased biofilm inhibitory activity against P. aeruginosa, with low micromolar IC50 values; however 81 does not disperse pre-formed biofilms with the same efficiency as TAGE (Huigens et al. 2008).
Oroidin 77 exhibits a similar level of activity to TAGE and CAGE for inhibition of biofilm formation by P. aeruginosa (Richards et al. 2008a), and a structure-activity-relationship (SAR) study of the oroidin scaffold was subsequently conducted thorough the construction of a 50-member library of analogues. Any modifications to the 2-AI head of the molecule completely abolished activity establishing the importance of this moiety for anti-biofilm activity. The most active molecule discovered was dihydrosventrin (DHS) 82 (Fig. 6.10), a reduced analogue of the oroidin family alkaloid sventrin, which has also been isolated from marine sponges. DHS inhibits the formation of biofilms by P. aeruginosa, A. baumannii, and Bordatella bronchiseptica with mid-micromolar IC50 values, and also disperses preformed biofilms of the same three species (Richards et al. 2008c). The construction of a library of second-generation analogues led to the identification of the para-bromo phenyl derivative 83, which exhibits more potent non-microbicidal anti-biofilm activity against A. baumannii than DHS (IC50 = 27 μM, EC50 = 41 μM) (Richards et al. 2008d).
Other oroidin analogues with potent anti-biofilm activity include those in which the native amide bond directionality is reversed (Richards et al. 2008b). Several such analogues that possess an aliphatic tail group (84–86), are low micromolar inhibitors of P. aeruginosa biofilm development, exhibiting at least four times more potent activity than oroidin. The most active reverse amide 2-AI (85) is also an extremely effective dispersion agent, eradicating pre-formed P. aeruginosa biofilms with mid-micromolar EC50 values. Several of the reverse amide class of 2-AIs, including compound 86, also inhibit biofilm formation by A. baumannii and a biotinylated analogue of compound 86 was used to identify the molecular target of this class of molecules in A. baumannii as BfmR (Thompson et al. 2012), the response regulator component of the BfmRS TCS. BfmR plays an important role in a biofilm formation and bfmR mutants exhibit significantly reduced biofilm-forming ability and altered planktonic cellular morphology (Tomaras et al. 2008), thus making BfmR an attractive anti-biofilm target.
The incorporation of a triazole moiety into the oroidin analogues has resulted in a number of highly active compounds (Rogers and Melander 2008), with the most active compounds possessing a substituted unsaturated aryl pendant group. Compound 87 (Fig. 6.10), which possesses broad-spectrum biofilm inhibition and dispersion properties, exhibiting low micromolar-high nanomolar IC50 values against P. aeruginosa, A. baumannii, and S. aureus, also exhibits synergism with several antibiotics for the dispersion of biofilms of several bacterial strains, and re-sensitizes planktonic bacteria of drug-resistant strains of S. aureus and A. baumannii to the effects of conventional antibiotics (Rogers et al. 2010a).
Aryl-2-AI derivatives (Fig. 6.10) have also proven to be active anti-biofilm compounds, with compound 88 effectively inhibiting E. coli biofilm formation (Bunders et al. 2010). Steenackers and co-workers subsequently reported a related series of aryl 2-AI compounds, the parent compound of which, compound 89, displays moderate biofilm inhibitory activity against S. typhimurium and P. aeruginosa. Incorporating substituents on the phenyl ring of 89 resulted in increased biofilm inhibition activity, and introduction of substituents at the 5-position of the 2-AI ring resulted in a further slight increase in activity, with the most active analogues 90–96 exhibiting low micromolar IC50 values for the inhibition of biofilm formation by S. typhimurium and P. aeruginosa (Steenackers et al. 2011a, b). A related series of 1,4,5-trisubstituted naamine alkaloids, including compounds 97 and 98, also inhibit biofilm formation by S. typhimurium and P. aeruginosa with micromolar IC50 values (Ermolat’ev et al. 2010).
Scaffolds related to the 2-AI heterocycle that have been investigated for anti-biofilm properties include the 2-aminobenzimidazole (2-ABI) and 2-aminopyrimidine scaffolds (2-AP) (Fig. 6.10). The 2-ABI 99 is highly active against Gram-positive bacteria, both inhibiting and dispersing biofilms via a mechanism that was inhibited by the presence of Zn (II), and the compound was subsequently shown to bind Zn (II) (Rogers et al. 2009). A series of related 2-ABIs was later studied against P. aeruginosa, leading to the identification of compound 100, which inhibits biofilm formation with an IC50 value of 4 μM and disperses pre-formed biofilms with an EC50 value of 92 μM (Frei et al. 2012). 2-APs are less active inhibitors of biofilm formation than their 2-AI counterparts, particularly against Gram-negative bacteria and none reported thus far disperse pre-formed biofilms. However compounds 101 and 102 do inhibit biofilm formation by S. aureus (Lindsey et al. 2012).
Other Marine Natural Products
Other natural product scaffolds of marine origin that possess anti-biofilm activity include: the diterpene alkaloid (−)-ageloxime D 103 (Fig. 6.11), which was isolated from the marine sponge Agelas nakamurai, and inhibits biofilm formation by S. epidermidis without affecting bacterial growth (Hertiani et al. 2010), and the structurally simple bacterial metabolite ethyl N-(2-phenethyl) carbamate 104 (Fig. 6.11), which was isolated from the culture medium of the marine bacterium SCRC3P79 (Cytophaga sp.), and possesses moderate anti-biofilm activity against R. salexigens (Yamada et al. 1997). Compound 104 was subsequently shown to be moderately active in inhibiting biofilm formation by several medically relevant strains of bacteria, and construction of a library of readily accessible analogues based upon compound 104 led to the identification of a number of compounds with increased activity, including the menthyl derived compounds 105–107, which inhibit biofilm formation by several strains of S. aureus with IC50 values in the mid to low micromolar range (Rogers et al. 2010b).
3 Macromolecule Approaches
3.1 Enzymatic Degradation of Matrix Components
Given that the matrix typically accounts for over 90 % of the dry mass of a biofilm and forms the basis of the three-dimensional structure of the biofilm, immobilizing the cells and allowing for cell-cell communication, degradation of the matrix is an attractive approach to eradicating biofilms. As mentioned earlier, bacteria within a biofilm produce EPS that constitute the matrix. Enzymatic degradation of the biomolecules that constitute the EPS is an innate phenomenon employed by several diverse bacterial species, and involves the secretion of enzymes such as glycosidases, proteases, and DNases that degrade various components of the EPS (Kaplan 2010). Examples of endogenously produced matrix degrading enzymes include the S. aureus DNase thermonuclease, the glycoside hydrolase dispersin B, and alginate lyase, which is produced by P. aeruginosa. These enzymes, and many others, are used by the bacteria to initiate dispersion of the biofilm, which contributes to bacterial survival and disease transmission (Kaplan 2010), and several of these enzymes have been investigated as potential therapeutic agents.
Dispersin B inhibits the formation of biofilms by several medically relevant bacterial species including S. aureus, S. epidermidis, and E. coli, and disperses S. epidermidis and E. coli biofilms (Izano et al. 2008; Kaplan et al. 2004; Itoh et al. 2005). Dispersin B also sensitizes S. epidermidis biofilm cells to the action of antimicrobials (Izano et al. 2008; Donelli et al. 2007) and is active in vivo, lowering the rate of catheter colonization by S. aureus in combination with triclosan in a rabbit model of infection (Darouiche et al. 2009). Alginate lyase degrades the polysaccharide alginate and enhances the microbicidal activity of aminoglycosides against P. aeruginosa biofilms in vitro (Alkawash et al. 2006; Alipour et al. 2009; Lamppa and Griswold 2013). Alginate lyase has demonstrated in vivo efficacy, enhancing the clearance of mucoid P. aeruginosa when coadministered with amikacin in a rabbit model of endocarditis (Bayer et al. 1992).
Biofilms formed in the presence of DNase exhibit reduced biomass and decreased antibiotic tolerance (Tetz and Tetz 2010), and the use of nucleases to combat biofilms has been explored against a number of bacterial strains. An extracellular DNase (NucB), produced by Bacillus licheniformis, induces rapid biofilm dispersal against several species of bacteria including B. subtilis, E. coli, and Micrococcus luteus (Bayer et al. 1992), while S. aureus also produces a nuclease, known as Nuc, that exhibits biofilm inhibitory activity (Kiedrowski et al. 2011) Recombinant human DNase I (rhDNase) inhibits biofilm formation by both S. aureus and S. epidermidis, disperses S. aureus biofilms, and increases the susceptibility of both S. aureus biofilm cells to chlorhexidine gluconate and povidone iodine, and P. aeruginosa biofilm cells to aminoglycosides in vitro (Alipour et al. 2009; Kaplan et al. 2012). rhDNase also displays activity in vivo, increasing the survival of S. aureus-infected C. elegans when administered in combination with tobramycin (Kaplan et al. 2012). rhDNase I (also known as dornase alfa and marketed as Pulmozyme by Genentech) is used in the clinic for the treatment of pulmonary disease in cystic fibrosis (CF) patients (Parsiegla et al. 2012), in which biofilm mediated P. aeruginosa infections are a major contributing factor to lung tissue damage (Hoiby et al. 2010b). Administration of Pulmozyme leads to reduced demand for antibiotics and improved lung function in CF patients (Frederiksen et al. 2006).
Endogenous proteases also play a role in biofilm dispersal (Boles and Horswill 2008) and exogenous addition has been investigated for the dispersal of established biofilms. For example, the S. epidermidis serine protease Esp inhibits S. aureus biofilm formation and eradicates preformed S. aureus biofilms. Esp also enhances the susceptibility of S. aureus biofilms to the antimicrobial peptide human beta-defensin 2 (hBD2), and exhibits activity in vivo, eliminating human nasal colonization by S. aureus (Iwase et al. 2010). Proteinase K exhibits anti-biofilm activity against S. aureus, believed to be by effecting an increase in proteolytic activity (Park et al. 2012). Finally, the metalloprotease serratopeptidase (SPEP) from Serratia marcescens, a widely used an anti-inflammatory therapeutic, inhibits biofilm formation by P. aeruginosa and S. epidermidis, enhances the activity of ofloxacin against biofilms of these bacteria (Selan et al. 1993), and inhibits biofilm formation by L. monocytogenes (Longhi et al. 2008).
3.2 The Use of Antibodies to Combat Biofilms
Another non-small molecule approach to eradicating biofilms is the use of antibodies. Monoclonal antibodies (mAbs) that bind the P. aeruginosa cell surface anchored exopolysaccharide Psl, which plays a role in the formation and maintenance of biofilms by acting as a scaffold for other biofilm initiating components (Jackson et al. 2004; Digiandomenico et al. 2012), were identified from a screen of an M13 phage-based human antibody library. Lead mAbs inhibit host cell attachment by P. aeruginosa and impart significant protection in multiple animal models of P. aeruginosa infection including a mouse acute lethal pneumonia model and a thermal injury model (Digiandomenico et al. 2012). Antibodies to the partially de-N-acetylated form of the staphylococcal surface polymer poly-N-acetylglucosamine (PNAG), which promotes biofilm formation, increase killing of S. aureus by human neutrophils, while passive immunization of mice with anti-dPNAG-DT rabbit sera results in increased clearance of S. aureus from the blood compared to mice treated with normal rabbit sera (Maira-Litran et al. 2005).
4 Conclusion
The contribution of the biofilm phenotype to the pathogenesis and host/antibiotic resistance of numerous bacterial infections, combined with the ineffectiveness of conventional antibiotics in eradicating such infections, has led to a serious need for alternative strategies to target bacteria residing within a biofilm. Numerous different approaches to this problem have been investigated, including the design or identification of small molecules that interfere with bacterial communication and signaling pathways and inhibit biofilm formation or cause biofilm dispersion, and the use of enzymes to degrade specific components of the matrix thereby causing the biofilm to disperse. In combination with conventional antibiotics these strategies have the potential to treat biofilm-based infections and have a significant impact in the fight against infectious disease.
References
Abraham NM, Lamlertthon S, Fowler VG, Jefferson KK (2012) Chelating agents exert distinct effects on biofilm formation in Staphylococcus aureus depending on strain background: role for clumping factor B. J Med Microbiol 61(Pt 8):1062–1070
Ali F, Sangwan PL, Koul S, Pandey A, Bani S, Abdullah ST, Sharma PR, Kitchlu S, Khan IA (2012) 4-epi-pimaric acid: a phytomolecule as a potent antibacterial and anti-biofilm agent for oral cavity pathogens. Eur J Clin Microbiol 31(2):149–159
Alipour M, Suntres ZE, Omri A (2009) Importance of DNase and alginate lyase for enhancing free and liposome encapsulated aminoglycoside activity against Pseudomonas aeruginosa. J Antimicrob Chemother 64(2):317–325
Alkawash MA, Soothill JS, Schiller NL (2006) Alginate lyase enhances antibiotic killing of mucoid Pseudomonas aeruginosa in biofilms. APMIS 114(2):131–138
Amara N, Mashiach R, Amar D, Krief P, Spieser SA, Bottomley MJ, Aharoni A, Meijler MM (2009) Covalent inhibition of bacterial quorum sensing. J Am Chem Soc 131(30):10610–10619
Antoniani D, Bocci P, Maciag A, Raffaelli N, Landini P (2010) Monitoring of diguanylate cyclase activity and of cyclic-di-GMP biosynthesis by whole-cell assays suitable for high-throughput screening of biofilm inhibitors. Appl Microbiol Biotechnol 85(4):1095–1104
Augustine N, Goel AK, Sivakumar KC, Ajay Kumar R, Thomas S (2014) Resveratrol – a potential inhibitor of biofilm formation in Vibrio cholerae. Phytomedicine 21(3):286–289
Banin E, Brady KM, Greenberg EP (2006) Chelator-induced dispersal and killing of Pseudomonas aeruginosa cells in a biofilm. Appl Environ Microbiol 72(3):2064–2069
Bayer AS, Park S, Ramos MC, Nast CC, Eftekhar F, Schiller NL (1992) Effects of alginase on the natural history and antibiotic therapy of experimental endocarditis caused by mucoid Pseudomonas aeruginosa. Infect Immun 60(10):3979–3985
Bjarnsholt T, Jensen PO, Rasmussen TB, Christophersen L, Calum H, Hentzer M, Hougen HP, Rygaard J, Moser C, Eberl L, Hoiby N, Givskov K (2005) Garlic blocks quorum sensing and promotes rapid clearing of pulmonary Pseudomonas aeruginosa infections. Microbiology 151:3873–3880
Boles BR, Horswill AR (2008) Agr-mediated dispersal of Staphylococcus aureus biofilms. PLoS Pathog 4(4):e1000052. doi:10.1371/journal.ppat.1000052
Bordi C, de Bentzmann S (2011) Hacking into bacterial biofilms: a new therapeutic challenge. Ann Intensive Care 1(1):19
Brackman G, Celen S, Baruah K, Bossier P, Van Calenbergh S, Nelis HJ, Coenye T (2009) AI-2 quorum-sensing inhibitors affect the starvation response and reduce virulence in several Vibrio species, most likely by interfering with LuxPQ. Microbiology 155(Pt 12):4114–4122
Braekman JC, Daloze D, Stoller C, Vansoest RWM (1992) Chemotaxonomy of Agelas (Porifera, Demospongiae). Biochem Syst Ecol 20(5):417–431. doi:10.1016/0305-1978(92)90082-O
Bunders CA, Richards JJ, Melander C (2010) Identification of aryl 2-aminoimidazoles as biofilm inhibitors in Gram-negative bacteria. Bioorg Med Chem Lett 20(12):3797–3800
Bunders C, Cavanagh J, Melander C (2011a) Flustramine inspired synthesis and biological evaluation of pyrroloindoline triazole amides as novel inhibitors of bacterial biofilms. Org Biomol Chem 9(15):5476–5481
Bunders CA, Minvielle MJ, Worthington RJ, Ortiz M, Cavanagh J, Melander C (2011b) Intercepting bacterial indole signaling with flustramine derivatives. J Am Chem Soc 133(50):20160–20163
Camilli A, Bassler BL (2006) Bacterial small-molecule signaling pathways. Science 311(5764):1113–1116
Chan WC, Coyle BJ, Williams P (2004) Virulence regulation and quorum sensing in staphylococcal infections: competitive AgrC antagonists as quorum sensing inhibitors. J Med Chem 47(19):4633–4641
Coates AR, Hu Y (2008) Targeting non-multiplying organisms as a way to develop novel antimicrobials. Trends Pharmacol Sci 29(3):143–150
Darouiche RO, Mansouri MD, Gawande PV, Madhyastha S (2009) Antimicrobial and antibiofilm efficacy of triclosan and DispersinB combination. J Antimicrob Chemother 64(1):88–93
Davey ME, O’Toole GA (2000) Microbial biofilms: from ecology to molecular genetics. Microbiol Mol Biol Rev 64(4):847–867
Davies D (2003) Understanding biofilm resistance to antibacterial agents. Nat Rev Drug Discov 2(2):114–122
Davies DG, Marques CNH (2009) A fatty acid messenger is responsible for inducing dispersion in microbial biofilms. J Bacteriol 191(5):1393–1403
Davies DG, Parsek MR, Pearson JP, Iglewski BH, Costerton JW, Greenberg EP (1998) The involvement of cell-to-cell signals in the development of a bacterial biofilm. Science 280(5361):295–298
Digiandomenico A, Warrener P, Hamilton M, Guillard S, Ravn P, Minter R, Camara MM, Venkatraman V, Macgill RS, Lin J, Wang Q, Keller AE, Bonnell JC, Tomich M, Jermutus L, McCarthy MP, Melnick DA, Suzich JA, Stover CK (2012) Identification of broadly protective human antibodies to Pseudomonas aeruginosa exopolysaccharide Psl by phenotypic screening. J Exp Med 209(7):1273–1287
Donelli G, Francolini I, Romoli D, Guaglianone E, Piozzi A, Ragunath C, Kaplan JB (2007) Synergistic activity of dispersin B and cefamandole nafate in inhibition of staphylococcal biofilm growth on polyurethanes. Antimicrob Agents Chemother 51(8):2733–2740
Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15(2):167–193
Dow JM, Crossman L, Findlay K, He YQ, Feng JX, Tang JL (2003) Biofilm dispersal in Xanthomonas campestris is controlled by cell-cell signaling and is required for full virulence to plants. Proc Natl Acad Sci U S A 100(19):10995–11000
Eguchi Y, Kubo N, Matsunaga H, Igarashi M, Utsumi R (2011) Development of an antivirulence drug against Streptococcus mutans: repression of biofilm formation, acid tolerance, and competence by a histidine kinase inhibitor, walkmycin C. Antimicrob Agents Chemother 55(4):1475–1484
Ermolat’ev DS, Bariwal JB, Steenackers HP, De Keersmaecker SC, Van der Eycken EV (2010) Concise and diversity-oriented route toward polysubstituted 2-aminoimidazole alkaloids and their analogues. Angew Chem Int Ed Engl 49(49):9465–9468. doi:10.1002/anie.201004256
Finch RG, Pritchard DI, Bycroft BW, Williams P, Stewart GS (1998) Quorum sensing: a novel target for anti-infective therapy. J Antimicrob Chemother 42(5):569–571
Flemming HC, Neu TR, Wozniak DJ (2007) The EPS matrix: the “house of biofilm cells”. J Bacteriol 189(22):7945–7947. doi:10.1128/JB.00858-07
Fowler SA, Stacy DM, Blackwell HE (2008) Design and synthesis of macrocyclic peptomers as mimics of a quorum sensing signal from Staphylococcus aureus. Org Lett 10(12):2329–2332
Frederiksen B, Pressler T, Hansen A, Koch C, Hoiby N (2006) Effect of aerosolized rhDNase (Pulmozyme) on pulmonary colonization in patients with cystic fibrosis. Acta Paediatr 95(9):1070–1074
Frei R, Breitbach AS, Blackwell HE (2012) 2-Aminobenzimidazole derivatives strongly inhibit and disperse Pseudomonas aeruginosa biofilms. Angew Chem Int Ed Engl 51(21):5226–5229
Fux CA, Stoodley P, Hall-Stoodley L, Costerton JW (2003) Bacterial biofilms: a diagnostic and therapeutic challenge. Expert Rev Anti Infect Ther 1(4):667–683
Geske GD, Wezeman RJ, Siegel AP, Blackwell HE (2005) Small molecule inhibitors of bacterial quorum sensing and biofilm formation. J Am Chem Soc 127(37):12762–12763
Giacometti A, Cirioni O, Gov Y, Ghiselli R, Del Prete MS, Mocchegiani F, Saba V, Orlando F, Scalise G, Balaban N, Dell’Acqua G (2003) RNA III inhibiting peptide inhibits in vivo biofilm formation by drug-resistant Staphylococcus aureus. Antimicrob Agents Chemother 47(6):1979–1983
Gotoh Y, Eguchi Y, Watanabe T, Okamoto S, Doi A, Utsumi R (2010) Two-component signal transduction as potential drug targets in pathogenic bacteria. Curr Opin Microbiol 13(2):232–239
Gutierrez JA, Crowder T, Rinaldo-Matthis A, Ho MC, Almo SC, Schramm VL (2009) Transition state analogs of 5′-methylthioadenosine nucleosidase disrupt quorum sensing. Nat Chem Biol 5(4):251–257
Han Y, Hou S, Simon KA, Ren D, Luk YY (2008) Identifying the important structural elements of brominated furanones for inhibiting biofilm formation by Escherichia coli. Bioorg Med Chem Lett 18(3):1006–1010
Hausner M, Wuertz S (1999) High rates of conjugation in bacterial biofilms as determined by quantitative in situ analysis. Appl Environ Microbiol 65(8):3710–3713
Hentzer M, Givskov M (2003) Pharmacological inhibition of quorum sensing for the treatment of chronic bacterial infections. J Clin Invest 112(9):1300–1307
Hentzer M, Riedel K, Rasmussen TB, Heydorn A, Andersen JB, Parsek MR, Rice SA, Eberl L, Molin S, Hoiby N, Kjelleberg S, Givskov M (2002) Inhibition of quorum sensing in Pseudomonas aeruginosa biofilm bacteria by a halogenated furanone compound. Microbiology 148:87–102
Hentzer M, Wu H, Andersen JB, Riedel K, Rasmussen TB, Bagge N, Kumar N, Schembri MA, Song ZJ, Kristoffersen P, Manefield M, Costerton JW, Molin S, Eberl L, Steinberg P, Kjelleberg S, Hoiby N, Givskov M (2003) Attenuation of Pseudomonas aeruginosa virulence by quorum sensing inhibitors. Embo J 22(15):3803–3815
Hertiani T, Edrada-Ebel R, Ortlepp S, van Soest RW, de Voogd NJ, Wray V, Hentschel U, Kozytska S, Muller WE, Proksch P (2010) From anti-fouling to biofilm inhibition: new cytotoxic secondary metabolites from two Indonesian Agelas sponges. Bioorg Med Chem 18(3):1297–1311
Hochbaum AI, Kolodkin-Gal I, Foulston L, Kolter R, Aizenberg J, Losick R (2011) Inhibitory effects of D-amino acids on Staphylococcus aureus biofilm development. J Bacteriol 193(20):5616–5622
Hoiby N, Bjarnsholt T, Givskov M, Molin S, Ciofu O (2010a) Antibiotic resistance of bacterial biofilms. Int J Antimicrob Agents 35(4):322–332. doi:10.1016/j.ijantimicag.2009.12.011
Hoiby N, Ciofu O, Bjarnsholt T (2010b) Pseudomonas aeruginosa biofilms in cystic fibrosis. Future Microbiol 5(11):1663–1674
Huigens RW, Richards JJ, Parise G, Ballard TE, Zeng W, Deora R, Melander C (2007) Inhibition of Pseudomonas aeruginosa biofilm formation with bromoageliferin analogues. J Am Chem Soc 129(22):6966–6967
Huigens RW, Ma L, Gambino C, Basso A, Moeller PDR, Cavanagh J, Wozniak DJ, Melander C (2008) Control of bacterial biofilms with marine alkaloid derivatives. Mol Biosyst 4(6):614–621
Hurdle JG, O’Neill AJ, Chopra I, Lee RE (2011) Targeting bacterial membrane function: an underexploited mechanism for treating persistent infections. Nat Rev Microbiol 9(1):62–75
Irie Y, Parsek MR (2008) Quorum sensing and microbial biofilms. Curr Top Microbiol Immunol 322:67–84
Ishida T, Ikeda T, Takiguchi N, Kuroda A, Ohtake H, Kato J (2007) Inhibition of quorum sensing in Pseudomonas aeruginosa by N-acyl cyclopentylamides. Appl Environ Microbiol 73(10):3183–3188
Itoh Y, Wang X, Hinnebusch BJ, Preston JF 3rd, Romeo T (2005) Depolymerization of beta-1,6-N-acetyl-D-glucosamine disrupts the integrity of diverse bacterial biofilms. J Bacteriol 187(1):382–387
Iwase T, Uehara Y, Shinji H, Tajima A, Seo H, Takada K, Agata T, Mizunoe Y (2010) Staphylococcus epidermidis Esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Nature 465(7296):346–349
Izano EA, Amarante MA, Kher WB, Kaplan JB (2008) Differential roles of poly-N-acetylglucosamine surface polysaccharide and extracellular DNA in Staphylococcus aureus and Staphylococcus epidermidis biofilms. Appl Environ Microbiol 74(2):470–476
Jackson KD, Starkey M, Kremer S, Parsek MR, Wozniak DJ (2004) Identification of psl, a locus encoding a potential exopolysaccharide that is essential for Pseudomonas aeruginosa PAO1 biofilm formation. J Bacteriol 186(14):4466–4475
Junker LM, Clardy J (2007) High-throughput screens for small-molecule inhibitors of Pseudomonas aeruginosa biofilm development. Antimicrob Agents Chemother 51(10):3582–3590
Kaplan JB (2010) Biofilm dispersal: mechanisms, clinical implications, and potential therapeutic uses. J Dent Res 89(3):205–218
Kaplan JB (2011) Antibiotic-induced biofilm formation. Int J Artif Organs 34(9):737–751
Kaplan JB, Ragunath C, Velliyagounder K, Fine DH, Ramasubbu N (2004) Enzymatic detachment of Staphylococcus epidermidis biofilms. Antimicrob Agents Chemother 48(7):2633–2636
Kaplan JB, LoVetri K, Cardona ST, Madhyastha S, Sadovskaya I, Jabbouri S, Izano EA (2012) Recombinant human DNase I decreases biofilm and increases antimicrobial susceptibility in staphylococci. J Antibiot (Tokyo) 65(2):73–77
Kiedrowski MR, Kavanaugh JS, Malone CL, Mootz JM, Voyich JM, Smeltzer MS, Bayles KW, Horswill AR (2011) Nuclease modulates biofilm formation in community-associated methicillin-resistant Staphylococcus aureus. PLoS One 6(11):e26714
Kim C, Kim J, Park HY, Park HJ, Lee JH, Kim CK, Yoon J (2008) Furanone derivatives as quorum-sensing antagonists of Pseudomonas aeruginosa. Appl Microbiol Biotechnol 80(1):37–47
Kolodkin-Gal I, Romero D, Cao S, Clardy J, Kolter R, Losick R (2010) D-amino acids trigger biofilm disassembly. Science 328(5978):627–629
Kunze B, Reck M, Dotsch A, Lemme A, Schummer D, Irschik H, Steinmetz H, Wagner-Dobler I (2010) Damage of Streptococcus mutans biofilms by carolacton, a secondary metabolite from the mycobacterium Sorangium cellulosum. BMC Microbiol 10:199
Lai PK, Roy J (2004) Antimicrobial and chemopreventive properties of herbs and spices. Curr Med Chem 11(11):1451–1460
Lamppa JW, Griswold KE (2013) Alginate lyase exhibits catalysis-independent biofilm dispersion and antibiotic synergy. Antimicrob Agents Chemother 57(1):137–145
Lee J, Lee JH (2010) Indole as an intercellular signal in microbial communities. Fems Microbiol Rev 34(4):426–444
Lee J, Bansal T, Jayaraman A, Bentley WE, Wood TK (2007a) Enterohemorrhagic Escherichia coli biofilms are inhibited by 7-hydroxyindole and stimulated by isatin. Appl Environ Microbiol 73(13):4100–4109
Lee J, Jayaraman A, Wood TK (2007b) Indole is an inter-species biofilm signal mediated by SdiA. BMC Microbiol 7:42
Lee JH, Cho MH, Lee J (2011a) 3-indolylacetonitrile decreases Escherichia coli O157:H7 biofilm formation and Pseudomonas aeruginosa virulence. Environ Microbiol 13(1):62–73
Lee JH, Regmi SC, Kim JA, Cho MH, Yun H, Lee CS, Lee J (2011b) Apple flavonoid phloretin inhibits Escherichia coli O157:H7 biofilm formation and ameliorates colon inflammation in rats. Infect Immun 79(12):4819–4827
Lee JH, Kim YG, Cho MH, Kim JA, Lee J (2012) 7-fluoroindole as an antivirulence compound against Pseudomonas aeruginosa. FEMS Microbiol Lett 329(1):36–44
Lieberman OJ, Orr MW, Wang Y, Lee VT (2014) High-throughput screening using the differential radial capillary action of ligand assay identifies ebselen as an inhibitor of diguanylate cyclases. ACS Chem Biol 9(1):183–192
Lin MH, Shu JC, Huang HY, Cheng YC (2012) Involvement of iron in biofilm formation by Staphylococcus aureus. PLoS One 7(3):e34388
Lindsey EA, Worthington RJ, Alcaraz C, Melander C (2012) 2-Aminopyrimidine as a novel scaffold for biofilm modulation. Org Biomol Chem 10(13):2552–2561
Longhi C, Scoarughi GL, Poggiali F, Cellini A, Carpentieri A, Seganti L, Pucci P, Amoresano A, Cocconcelli PS, Artini M, Costerton JW, Selan L (2008) Protease treatment affects both invasion ability and biofilm formation in Listeria monocytogenes. Microb Pathog 45(1):45–52
Lonn-Stensrud J, Petersen FC, Benneche T, Scheie AA (2007) Synthetic bromated furanone inhibits autoinducer-2-mediated communication and biofilm formation in oral streptococci. Oral Microbiol Immunol 22(5):340–346
Lowery CA, Park J, Kaufmann GF, Janda KD (2008) An unexpected switch in the modulation of AI-2-based quorum sensing discovered through synthetic 4,5-dihydroxy-2,3-pentanedione analogues. J Am Chem Soc 130(29):9200–9201
Lyon GJ, Novick RP (2004) Peptide signaling in Staphylococcus aureus and other Gram-positive bacteria. Peptides 25(9):1389–1403
Mah TFC, O’Toole GA (2001) Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol 9(1):34–39
Maira-Litran T, Kropec A, Goldmann DA, Pier GB (2005) Comparative opsonic and protective activities of Staphylococcus aureus conjugate vaccines containing native or deacetylated Staphylococcal Poly-N-acetyl-beta-(1–6)-glucosamine. Infect Immun 73(10):6752–6762
Manefield M, Rasmussen TB, Henzter M, Andersen JB, Steinberg P, Kjelleberg S, Givskov M (2002) Halogenated furanones inhibit quorum sensing through accelerated LuxR turnover. Microbiology 148:1119–1127
Miller ST, Xavier KB, Campagna SR, Taga ME, Semmelhack MF, Bassler BL, Hughson FM (2004) Salmonella typhimurium recognizes a chemically distinct form of the bacterial quorum-sensing signal AI-2. Mol Cell 15(5):677–687
Minvielle MJ, Bunders CA, Melander C (2013a) Indole/triazole conjugates are selective inhibitors and inducers of bacterial biofilms. Medchemcomm 4(6):916–919
Minvielle MJ, Eguren K, Melander C (2013b) Highly active modulators of indole signaling alter pathogenic behaviors in gram-negative and gram-positive bacteria. Chemistry 19(51):17595–17602
Musk DJ, Hergenrother PJ (2006) Chemical countermeasures for the control of bacterial biofilms: effective compounds and promising targets. Curr Med Chem 13(18):2163–2177
Musk DJ Jr, Hergenrother PJ (2008) Chelated iron sources are inhibitors of Pseudomonas aeruginosa biofilms and distribute efficiently in an in vitro model of drug delivery to the human lung. J Appl Microbiol 105(2):380–388
Musk DJ, Banko DA, Hergenrother PJ (2005) Iron salts perturb biofilm formation and disrupt existing biofilms of Pseudomonas aeruginosa. Chem Biol 12(7):789–796
Nguyen UT, Wenderska IB, Chong MA, Koteva K, Wright GD, Burrows LL (2012) Small-molecule modulators of Listeria monocytogenes biofilm development. Appl Environ Microbiol 78(5):1454–1465
O’Loughlin CT, Miller LC, Siryaporn A, Drescher K, Semmelhack MF, Bassler BL (2013) A quorum-sensing inhibitor blocks Pseudomonas aeruginosa virulence and biofilm formation. Proc Natl Acad Sci U S A 110(44):17981–17986
Park JH, Lee JH, Cho MH, Herzberg M, Lee J (2012) Acceleration of protease effect on Staphylococcus aureus biofilm dispersal. FEMS Microbiol Lett 335(1):31–38
Parkins MD, Ceri H, Storey DG (2001) Pseudomonas aeruginosa GacA, a factor in multihost virulence, is also essential for biofilm formation. Mol Microbiol 40(5):1215–1226, doi: mmi2469 [pii]
Parsek MR, Greenberg EP (2000) Acyl-homoserine lactone quorum sensing in gram-negative bacteria: a signaling mechanism involved in associations with higher organisms. Proc Natl Acad Sci U S A 97(16):8789–8793
Parsiegla G, Noguere C, Santell L, Lazarus RA, Bourne Y (2012) The structure of human DNase I bound to magnesium and phosphate ions points to a catalytic mechanism common to members of the DNase I-like superfamily. Biochemistry 51(51):10250–10258
Persson T, Hansen TH, Rasmussen TB, Skinderso ME, Givskov M, Nielsen J (2005) Rational design and synthesis of new quorum-sensing inhibitors derived from acylated homoserine lactones and natural products from garlic. Org Biomol Chem 3(2):253–262
Peters L, Konig GM, Wright AD, Pukall R, Stackebrandt E, Eberl L, Riedel K (2003) Secondary metabolites of Flustra foliacea and their influence on bacteria. Appl Environ Microbiol 69(6):3469–3475
Petrova OE, Schurr JR, Schurr MJ, Sauer K (2011) The novel Pseudomonas aeruginosa two-component regulator BfmR controls bacteriophage-mediated lysis and DNA release during biofilm development through PhdA. Mol Microbiol 81(3):767–783
Qi F, Merritt J, Lux R, Shi W (2004) Inactivation of the ciaH Gene in Streptococcus mutans diminishes mutacin production and competence development, alters sucrose-dependent biofilm formation, and reduces stress tolerance. Infect Immun 72(8):4895–4899
Quave CL, Estevez-Carmona M, Compadre CM, Hobby G, Hendrickson H, Beenken KE, Smeltzer MS (2012) Ellagic acid derivatives from Rubus ulmifolius inhibit Staphylococcus aureus biofilm formation and improve response to antibiotics. PLoS One 7(1):e28737
Raad I, Chatzinikolaou I, Chaiban G, Hanna H, Hachem R, Dvorak T, Cook G, Costerton W (2003) In vitro and ex vivo activities of minocycline and EDTA against microorganisms embedded in biofilm on catheter surfaces. Antimicrob Agents Chemother 47(11):3580–3585
Rasmussen TB, Givskov M (2006) Quorum-sensing inhibitors as anti-pathogenic drugs. Int J Med Microbiol 296(2–3):149–161
Rasmussen TB, Manefield M, Andersen JB, Eberl L, Anthoni U, Christophersen C, Steinberg P, Kjelleberg S, Givskov M (2000) How Delisea pulchra furanones affect quorum sensing and swarming motility in Serratia liquefaciens MG1. Microbiology 146(Pt 12):3237–3244
Reck M, Rutz K, Kunze B, Tomasch J, Surapaneni SK, Schulz S, Wagner-Dobler I (2011) The biofilm inhibitor carolacton disturbs membrane integrity and cell division of Streptococcus mutans through the serine/threonine protein kinase PknB. J Bacteriol 193(20):5692–5706
Ren D, Sims JJ, Wood TK (2001) Inhibition of biofilm formation and swarming of Escherichia coli by (5Z)-4-bromo-5-(bromomethylene)-3-butyl-2(5H)-furanone. Environ Microbiol 3(11):731–736
Ren D, Sims JJ, Wood TK (2002) Inhibition of biofilm formation and swarming of Bacillus subtilis by (5Z)-4-bromo-5-(bromomethylene)-3-butyl-2(5H)-furanone. Lett Appl Microbiol 34(4):293–299
Ren DC, Zuo RJ, Barrios AFG, Bedzyk LA, Eldridge GR, Pasmore ME, Wood TK (2005) Differential gene expression for investigation of Escherichia coli biofilm inhibition by plant extract ursolic acid. Appl Environ Microbiol 71(7):4022–4034
Richards JJ, Ballard TE, Huigens RW, Melander C (2008a) Synthesis and screening of an oroidin library against Pseudomonas aeruginosa biofilms. Chembiochem: Eur J Chem Biol 9(8):1267–1279
Richards JJ, Ballard TE, Melander C (2008b) Inhibition and dispersion of Pseudomonas aeruginosa biofilms with reverse amide 2-aminoimidazole oroidin analogues. Org Biomol Chem 6(8):1356–1363
Richards JJ, Huigens RW, Ballard TE, Basso A, Cavanagh J, Melander C (2008c) Inhibition and dispersion of proteobacterial biofilms. Chem Commun 14:1698–1700
Richards JJ, Reed CS, Melander C (2008d) Effects of N-pyrrole substitution on the anti-biofilm activities of oroidin derivatives against Acinetobacter baumannii. Bioorg Med Chem Lett 18(15):4325–4327
Rogers SA, Melander C (2008) Construction and screening of a 2-aminoimidazole library identifies a small molecule capable of inhibiting and dispersing biofilms across bacterial order, class, and phylum. Angew Chem Int Ed 47(28):5229–5231
Rogers SA, Huigens RW, Melander C (2009) A 2-aminobenzimidazole that inhibits and disperses gram-positive biofilms through a zinc-dependent mechanism. J Am Chem Soc 131(29):9868–9869
Rogers SA, Huigens RW 3rd, Cavanagh J, Melander C (2010a) Synergistic effects between conventional antibiotics and 2-aminoimidazole-derived antibiofilm agents. Antimicrob Agents Chemother 54(5):2112–2118
Rogers SA, Whitehead DC, Mullikin T, Melander C (2010b) Synthesis and bacterial biofilm inhibition studies of ethyl N-(2-phenethyl) carbamate derivatives. Org Biomol Chem 8(17):3857–3859
Ronning DR, Iacopelli NM, Mishra V (2010) Enzyme-ligand interactions that drive active site rearrangements in the Helicobacter pylori 5′-methylthioadenosine/S-adenosylhomocysteine nucleosidase. Protein Sci 19(12):2498–2510
Roy V, Meyer MT, Smith JA, Gamby S, Sintim HO, Ghodssi R, Bentley WE (2013) AI-2 analogs and antibiotics: a synergistic approach to reduce bacterial biofilms. Appl Microbiol Biotechnol 97(6):2627–2638
Ryjenkov DA, Tarutina M, Moskvin OV, Gomelsky M (2005) Cyclic diguanylate is a ubiquitous signaling molecule in bacteria: insights into biochemistry of the GGDEF protein domain. J Bacteriol 187(5):1792–1798
Saginur R, Stdenis M, Ferris W, Aaron SD, Chan F, Lee C, Ramotar K (2006) Multiple combination bactericidal testing of staphylococcal biofilms from implant-associated infections. Antimicrob Agents Chemother 50(1):55–61
Sambanthamoorthy K, Gokhale AA, Lao W, Parashar V, Neiditch MB, Semmelhack MF, Lee I, Waters CM (2011) Identification of a novel benzimidazole that inhibits bacterial biofilm formation in a broad-spectrum manner. Antimicrob Agents Chemother 55(9):4369–4378
Sambanthamoorthy K, Sloup RE, Parashar V, Smith JM, Kim EE, Semmelhack MF, Neiditch MB, Waters CM (2012) Identification of small molecules that antagonize diguanylate cyclase enzymes to inhibit biofilm formation. Antimicrob Agents Chemother 56(10):5202–5211
Selan L, Berlutti F, Passariello C, Comodi-Ballanti MR, Thaller MC (1993) Proteolytic enzymes: a new treatment strategy for prosthetic infections? Antimicrob Agents Chemother 37(12):2618–2621
Sharma-Kuinkel BK, Mann EE, Ahn JS, Kuechenmeister LJ, Dunman PM, Bayles KW (2009) The Staphylococcus aureus LytSR two-component regulatory system affects biofilm formation. J Bacteriol 191(15):4767–4775
Shirtliff ME, Leid JG (ed) (2009) Biofilms and device-related infections. In: Costerton JW (ed) Springer series on biofilms. Springer, New York. doi:10.1007/978-3-540-68119-9
Simonetti O, Cirioni O, Mocchegiani F, Cacciatore I, Silvestri C, Baldassarre L, Orlando F, Castelli P, Provinciali M, Vivarelli M, Fornasari E, Giacometti A, Offidani A (2013) The efficacy of the quorum sensing inhibitor FS8 and tigecycline in preventing prosthesis biofilm in an animal model of staphylococcal infection. Int J Mol Sci 14(8):16321–16332
Slusarenko AJ, Patel A, Portz D (2008) Control of plant diseases by natural products: allicin from garlic as a case study. Eur J Plant Pathol 121(3):313–322
Sobke A, Klinger M, Hermann B, Sachse S, Nietzsche S, Makarewicz O, Keller PM, Pfister W, Straube E (2012) The urinary antibiotic 5-nitro-8-hydroxyquinoline (Nitroxoline) reduces the formation and induces the dispersal of Pseudomonas aeruginosa biofilms by chelation of iron and zinc. Antimicrob Agents Chemother 56(11):6021–6025
Spoering AL, Lewis K (2001) Biofilms and planktonic cells of Pseudomonas aeruginosa have similar resistance to killing by antimicrobials. J Bacteriol 183(23):6746–6751
Steenackers HP, Ermolat’ev DS, Savaliya B, De Weerdt A, De Coster D, Shah A, Van der Eycken EV, De Vos DE, Vanderleyden J, De Keersmaecker SC (2011a) Structure-activity relationship of 4(5)-aryl-2-amino-1H-imidazoles, N1-substituted 2-aminoimidazoles and imidazo[1,2-a]pyrimidinium salts as inhibitors of biofilm formation by Salmonella typhimurium and Pseudomonas aeruginosa. J Med Chem 54(2):472–484
Steenackers HP, Ermolat’ev DS, Savaliya B, Weerdt AD, Coster DD, Shah A, Van der Eycken EV, De Vos DE, Vanderleyden J, De Keersmaecker SC (2011b) Structure-activity relationship of 2-hydroxy-2-aryl-2,3-dihydro-imidazo[1,2-a]pyrimidinium salts and 2 N-substituted 4(5)-aryl-2-amino-1H-imidazoles as inhibitors of biofilm formation by Salmonella Typhimurium and Pseudomonas aeruginosa. Bioorg Med Chem 19(11):3462–3473
Stock AM, Robinson VL, Goudreau PN (2000) Two-component signal transduction. Annu Rev Biochem 69:183–215
Su Z, Peng L, Worthington RJ, Melander C (2011) Evaluation of 4,5-disubstituted-2-aminoimidazole-triazole conjugates for antibiofilm/antibiotic resensitization activity against MRSA and Acinetobacter baumannii. ChemMedChem 6(12):2243–2251
Tamayo R, Pratt JT, Camilli A (2007) Roles of cyclic diguanylate in the regulation of bacterial pathogenesis. Annu Rev Microbiol 61:131–148
Tetz VV, Tetz GV (2010) Effect of extracellular DNA destruction by DNase I on characteristics of forming biofilms. DNA Cell Biol 29(8):399–405
Thompson RJ, Bobay BG, Stowe SD, Olson AL, Peng L, Su Z, Actis LA, Melander C, Cavanagh J (2012) Identification of BfmR, a response regulator involved in biofilm development, as a target for a 2-aminoimidazole-based antibiofilm agent. Biochemistry 51(49):9776–9778
Tomaras AP, Flagler MJ, Dorsey CW, Gaddy JA, Actis LA (2008) Characterization of a two-component regulatory system from Acinetobacter baumannii that controls biofilm formation and cellular morphology. Microbiology 154:3398–3409
Tsuchikama K, Zhu J, Lowery CA, Kaufmann GF, Janda KD (2012) C4-alkoxy-HPD: a potent class of synthetic modulators surpassing nature in AI-2 quorum sensing. J Am Chem Soc 134(33):13562–13564
Vikram A, Jayaprakasha GK, Jesudhasan PR, Pillai SD, Patil BS (2010) Suppression of bacterial cell-cell signalling, biofilm formation and type III secretion system by citrus flavonoids. J Appl Microbiol 109(2):515–527
Waters CM, Bassler BL (2005) Quorum sensing: cell-to-cell communication in bacteria. Annu Rev Cell Dev Biol 21:319–346
Wenderska IB, Chong M, McNulty J, Wright GD, Burrows LL (2011) Palmitoyl-DL-carnitine is a multitarget inhibitor of Pseudomonas aeruginosa biofilm development. Chembiochem: Eur J Chem Biol 12(18):2759–2766
Wood TK, Lee J, Zhang XS, Hegde M, Bentley WE, Jayaraman A (2008) Indole cell signaling occurs primarily at low temperatures in Escherichia coli. Isme J 2(10):1007–1023
Worthington RJ, Blackledge MS, Melander C (2013) Small molecule inhibition of bacterial two-component systems to combat antibiotic resistance and virulence. Future Med Chem 5(11):1265–1284
Yamada A, Kitamura H, Yamaguchi K, Fukuzawa S, Kamijima C, Yazawa K, Kuramoto M, Wang GYS, Fujitani Y, Uemura D (1997) Development of chemical substances regulating biofilm formation. Bull Chem Soc Jpn 70(12):3061–3069
Yan H, Chen W (2010) 3′,5′-Cyclic diguanylic acid: a small nucleotide that makes big impacts. Chem Soc Rev 39(8):2914–2924
Yang L, Barken KB, Skindersoe ME, Christensen AB, Givskov M, Tolker-Nielsen T (2007) Effects of iron on DNA release and biofilm development by Pseudomonas aeruginosa. Microbiology 153(Pt 5):1318–1328
Yates EA, Philipp B, Buckley C, Atkinson S, Chhabra SR, Sockett RE, Goldner M, Dessaux Y, Camara M, Smith H, Williams P (2002) N-acylhomoserine lactones undergo lactonolysis in a pH-, temperature-, and acyl chain length-dependent manner during growth of Yersinia pseudotuberculosis and Pseudomonas aeruginosa. Infect Immun 70(10):5635–5646
Zhou J, Watt S, Wang J, Nakayama S, Sayre DA, Lam YF, Lee VT, Sintim HO (2013) Potent suppression of c-di-GMP synthesis via I-site allosteric inhibition of diguanylate cyclases with 2′-F-c-di-GMP. Bioorg Med Chem 21(14):4396–4404
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Melander, R.J., Melander, C. (2015). Innovative Strategies for Combating Biofilm-Based Infections. In: Donelli, G. (eds) Biofilm-based Healthcare-associated Infections. Advances in Experimental Medicine and Biology, vol 831. Springer, Cham. https://doi.org/10.1007/978-3-319-09782-4_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-09782-4_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09781-7
Online ISBN: 978-3-319-09782-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)