Abstract
Globally, lung cancer represents the leading cause of cancer death in males, and is the second leading cause in females. Two current developments will result in substantially higher numbers of non-small cell lung cancer (NSCLC) patients and especially elderly patients with stage I NSCLC. An aging population will increase the number of NSCLC patients by 50 % in the US and the majority of these patients will be older than 65 years. CT based screening of patients at high risk for lung cancer has recently been approved in the US and is expected to increase the number stage IA by a factor of two. Treatment of this increasing number of elderly patients and patients with comorbidities will pose a challenge to all disciplines involved in lung cancer treatment, because surgical lobectomy as standard of care cannot be performed in relevant proportions of the patients. In this chapter, the principles and practice of stereotactic body radiotherapy (SBRT) for treatment of stage I NSCLC are summarized. This radiotherapy concept, where millimeter accuracy of radiotherapy allowed irradiation with very high irradiation doses, consistently achieves local tumor control in >90 % of the patients. Simultaneously, accurate restriction of high irradiation doses to the tumor minimizes toxicity. This effective local treatment translates into improved overall survival compared to traditional radiotherapy or watchful waiting. Consequently, SBRT is considered as treatment of choice for medically inoperable patients, appears equivalent to sublobar resection and is the standard of care for patients refusing lobectomy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Propensity Score Match
- Cancer Specific Survival
- Stereotactic Body Radiotherapy
- Local Tumor Control
- Early Stage NSCLC
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Rational for Stereotactic Body Radiotherapy
Globally, lung cancer represents the leading cause of cancer death in males, and is the second leading cause in females. High rates of cure are only achieved if the diagnosis of non-small cell lung cancer (NSCLC) is made at an early stage of disease; however, this is accomplished only in about one quarter of the patients due to the indolent nature of early stage NSCLC. Two current developments will result in substantially higher numbers of NSCLC patients and especially elderly patients with stage I NSCLC. (1) An aging population will increase the number of NSCLC patients by 50 % in the US and the majority of these patients will be older than 65 years [1]. (2) CT based screening of patients at high risk for lung cancer has recently been approved in the US and is expected to increase the number of stage IA by a factor of two [2].
Treatment of this increasing number of elderly patients with early stage NSCLC will pose a challenge to all disciplines involved in lung cancer treatment. Despite surgical resection – lobectomy and systematic lymph node dissection – is the standard of care, its use is declining. Of all patients with stage I disease, >80 % are treated with surgical resection [3], but resection rates drop in the elderly Western population due to comorbidities and the associated risk of increased operative mortality and morbidity [4]. In the US population older than 65 years, the proportion of patients treated with open or laparoscopic surgery decreased from 75.2 to 67.3 % between 1998 and 2007 [5] and this proportion drops to <40 % in patients older than 75 years based on data from the Netherlands [6].
These numbers illustrate the need for non-surgical options offering safe and effective treatment for elderly comorbid patients with stage I NSCLC. Best supportive care without any curative treatment is practiced with increasing frequency: life expectancy of elderly patients with (severe) comorbidities is assumed being too short to justify a potentially toxic and cumbersome curative treatment. Based on the California Cancer Center registry, 7 % of all stage I NSCLC patients remain treated with best supportive care [3] and this proportion of untreated patients increases to 30 % in the elderly population >75 years old [6, 7]. However, lung cancer specific survival (CSS) is <20 % after 5 years in these untreated patients indicating the need for a curative treatment option.
Conventionally fractionated radiotherapy is an established curative treatment option for medically inoperable patients with stage I NSCLC. The term “conventional” radiotherapy refers to the technique and fractionation of radiotherapy: uncertainties in tumor extension and tumor targeting require large safety margins and result in large volumes of normal tissue irradiated. Therefore, radiotherapy is delivered in multiple small irradiation fractions of usually 2 Gy per day (conventional fractionation) to total doses of 60–66 Gy, delivered over a period of 6–7 weeks. This treatment has been the standard of care for medically inoperable patients and achieved 3-years OS rates of about 30 % and 3-years CSS of about 50 %, better than best supportive care [8]. However, local tumor relapse is the most frequent site of treatment failure after irradiation with conventional radiotherapy and retrospective studies have demonstrated a dose-response relationship for local tumor control and disease specific survival [9–11]: higher irradiation doses are associated with better local tumor control, which improves OS [8, 12]. These data indicate the need for a methodology making safe intensification of radiotherapy possible.
SBRT Background and Definitions
Principles and practice of Stereotactic Body Radiotherapy (SBRT) were transferred from cranial stereotactic radiotherapy/radiosurgery in the mid-90s by pioneering work at the Karolinska Hospital in Sweden and this concept was quickly adopted and further developed in Japan [13] and Germany [14, 15]. Several national and international bodies [16–19] have defined stereotactic Body Radiotherapy (SBRT) as a method of external beam radiotherapy (EBRT) to accurately deliver a high dose of irradiation in one or few treatment fractions to an extra-cranial target.
SBRT can be adequately performed with either traditional linear accelerators equipped with suitable image-guidance technology, accelerators specifically adapted for SBRT and dedicated delivery systems. Additionally, the principles of SBRT apply for both photon and particle therapy. It is of fundamental importance that the whole work-flow of SBRT – the medial and technical parts – are systematically optimized and appropriate quality assurance procedures are implemented. SBRT is therefore a multi-professional teamwork involving the Radiation Oncologists, Medical Physicists and Radiation Technologists. Targeting the tumor with daily image guidance is most important to avoid its missing and to avoid delivery of high irradiation doses to critical normal structures. This high accuracy allows safe treatment with irradiation doses, which are at least equivalent to radical doses in conventional fractionation. The full SBRT irradiation dose is delivered in few fractions, usually but not necessarily in maximum 3–10. Adjustment of single-fraction dose and total dose to size and location of the target is essential.
Outcome After SBRT for Early Stage NSCLC
SBRT in the Elderly Population Compared to Best Supportive Care
Two population-based analyses from the Netherlands [6, 7] and the US [20] demonstrated an improvement in OS for stage I NSCLC by the introduction of SBRT into the elderly patient population. SBRT represents an attractive treatment option for this elderly patient population because of its non-invasive nature, practice on an outpatient basis and short overall treatment time of 1–2 weeks: these factors might improve patient referral to a curative treatment and improve patient compliance.
In the Dutch study of patients older than 75 years, OS survival was improved in the total patient population from median 16 months to median 21 months by the introduction of SBRT between 1999 and 2007 [7]. Availability of SBRT reduced the proportion of patients treated with (non-curative) best supportive care from 38 to 28 % and increased the proportion of patents treated with (curative) radiotherapy from 26 to 42 %. The proportion of patients treated with surgery remained constant during the analyzed time periods.
The US study is based on the SEER database of patients older than 65 years and compared five different treatment options for patients with stage I NSCLC [20]: best supportive care, conventional radiotherapy, SBRT, sublobar resection and lobectomy. Propensity score matching between SBRT and non-SBRT treatment was performed to correct for imbalances of race, sex, education level, median income, comorbidity score, histology, tumor grade, tumor size, and receipt of lymph node sampling. SBRT achieved improved OS compared to best supportive care and conventional radiotherapy and differences were not significant compared to sublobar resection and lobectomy. Safety of SBRT in this elderly population is expressed in 30- and 90-days mortality rates of 0 and 0.8 %, respectively; 90-day mortality rates were 4.1 % for sublobar resection and lobectomy.
Two studies focused on safety and efficacy of SBRT in patients older than 80 years. A Japanese study about 109 patients with a median age of 83 years (maximum 91) reported 3-years OS of 53.7 % [21]. One patient suffered from a grade 5 radiation induced pneumonitis: this patients was medically inoperable because of interstitial pneumonia associated with antineutrophil cytoplasmic antibody-related vasculitis. Sandhu et al. described treatment of 24 patients with a median age of 85 years and 2-years OS was 74 % after SBRT with a median dose of 48 Gy delivered in 4–5 fractions. No patient developed early or late grade 3+ toxicity. A Dutch study reported SBRT in 193 patients older than 75 years, median 79 years [22]: all patients but one finished their treatment resulting in 3-years OS of 45 %. No grade 4+ toxicity was observed. Summarizing these data, SBRT was safe with only one treatment related death in 326 patients and with small numbers of grade 3 and 4 toxicity despite median age ranged between 79 and 85 years. SBRT data appear favorable compared to surgical series, where mortality in octogenarians approaches 10–15 % in some series and postoperative morbidity is consistently reported in >20 % of the patients [23].
Another concern is safety of SBRT in patients with very poor pre-treatment pulmonary function. Palma et al. analyzed SBRT in 176 patients with chronic obstructive pulmonary disease (COPD) at stage Global Initiative for Chronic Obstructive Lung Disease (GOLD) III/IV [24]. Patients were treated with a risk-adapted fractionation of 60 Gy delivered in 3–8 fractions. Three-year OS was 47 % and no patient developed any grade IV or V toxicity. Guckenberger et al. analyzed post-SBRT pulmonary function changes in 270 patients treated at five international centers [25]. In the patient cohort with worst pre-SBRT values (FEV1 <40 %), pulmonary function was stable over a 24 months period indicating safety of SBRT in this high-risk cohort of patients with severe pulmonary comorbidities. Stable or only small loss of pulmonary function after SBRT has been reported by other groups as well [26–29] and is explained by the parallel structure of the lung and restriction of high SBRT doses to small volumes.
There certainly exists a cohort of patients with severe comorbidities and very limited OS, which will not benefit from curative SBRT. However, such patient selection criteria are not available. Consequently, SBRT should be offered to all patients irrespective of old age and pre-existing pulmonary comorbidities unless they will not tolerate the procedure of SBRT planning and delivery.
SBRT in Medically Inoperable Patients Compared to Conventionally Fractionated Radiotherapy
Local tumor control rates of 84–98 % are reported by several prospective phase II trials of SBRT in medically inoperable stage I NSCLC patients [30–35]. This improved local tumor control compared to conventional radiotherapy [8] transfers into an improved OS as demonstrated in a meta-analysis [36] and a population based analysis [20]: 3-years OS is approximately 50 % after SBRT with pre-treatment comorbidities being a strong predictor for OS [37].
Large single- and multi-institutional studies confirm results from the prospective studies described above, highly consistent results despite differences in the methodology of SBRT (Table 4.1). A patterns-of-care and outcome study analyzed SBRT in 582 patients treated at 13 German and Austrian academic centers [38]: local tumor control and OS was independent from the SBRT technologies used at different time periods and used at different centers and no learning curve or procedure volume effect was observed. This again confirms the robustness of SBRT.
Based on these findings, the 1.2013 version of the NCCN Guidelines [39] as well as the ESMO Clinical Practice Guidelines [40] consider SBRT as superior to conventionally fractionated radiotherapy and as the standard of care for medically inoperable patients.
SBRT in Medically Inoperable Patients Compared to Radiofrequency Ablation
Radiofrequency ablation (RFA) has been introduced as a minimally invasive option into the treatment of stage I NSCLC. No study performed a direct comparison between SBRT and RFA but a recent literature review reported improved local tumor control, cancer specific survival and overall survival after SBRT compared to RFA [41]. Additionally, toxicity and 30-day mortality [42] were lower after SBRT resulting in the conclusion, that SBRT should be proposed as the first non-surgical treatment to high-risk patients.
SBRT in Medically Operable Patients Compared to Surgery
Lobectomy is the evidence-based standard of care for operable stage I NSCLC patients: a randomized trial described improved local tumor control and OS after lobectomy compared to wedge resection [43]. Whether sublobar anatomical resection (segmentectomy) is equivalent to lobectomy is discussed controversially [44] but results of segmentectomy appear comparable especially in stage IA patients [45].
Based on the promising outcome of SBRT in medically inoperable patients, three randomized trials comparing SBRT with lobectomy (ROSEL, STAR) or sublobar resection (ACOSOG Z4099/RTOG 1021) have been started but all three studies closed early due to poor accrual: only 68/2,410 (2.8 %) patients were enrolled leaving us without level I evidence.
Because of this lack of level I evidence, several studies used statistical methods like matched pair analyses and propensity score matching were performed to correct for imbalances in patient characteristics between SBRT and surgery. Grills et al. performed a single-institution comparison between SBRT and wedge resection and reported improved local tumor control after SBRT with no differences in cancer specific survival; OS was better in the surgical cohort, which was explained by older age and increased comorbidities in the SBRT patients [46]. The previously cited US population based analysis showed no difference in OS and cancer specific survival for SBRT versus sublobar resection and SBRT versus lobectomy [20]. Puri et al. reported identical cancer specific survival between SBRT and surgery (lobectomy in 80 % of the patients) [47]. OS appeared better after surgery compared to SBRT but was not statistically significant and this potential difference was explained by increased pulmonary comorbidities in the SBRT cohort, which was not corrected in the propensity score matching. Verstegen et al. compared SBRT and VATS lobectomy in 128 patients after propensity score matching of gender, age, clinical tumor stage, tumor diameter, location of the tumor, pretreatment tumor histology, lung function (FEV1%), Charlson comorbidity score and WHO performance score [48]. Locoregional control was better after SBRT with no differences in freedom from progression and OS.
Few studies reported outcome after SBRT when patients were considered as suitable for surgical resection but surgery was refused. Two Japanese and Dutch studies described excellent OS of 70 % after 5 years (n = 87) [49] and 85 % at 3 years (n = 177) [50], respectively, results which compare well to OS after lobectomy.
Consequently, SBRT is a viable treatment option in the situation, when lobectomy is refused by the patients. Additionally, SBRT appears equivalent to sublobar resection and both options with their specific pros and cons should be discussed with the patient.
Toxicity and Quality of Live After Lung SBRT
The majority of patients are referred for SBRT because of severe pulmonary comorbidities and their poor pulmonary function does not allow surgical resection. Consequently, pulmonary toxicity is a concern in lung SBRT. The incidence of symptomatic radiation induced pneumonitis is consistently below 10 % in SBRT of lung tumors <5 cm in diameter and peripherally located. Higher mean lung doses and a larger low-dose spread have been reported to be correlated with the risk of radiation-induced pneumonitis [51, 52]. Additionally, pulmonary function is stable after SBRT with a loss of <10 % (FEV1, DLCO) within 24 months after treatment [25]. Pulmonary toxicity was not increased even in patients with very poor pre-SBRT pulmonary function [25] and with severe COPD GOLD III-IV [53]. Patients with pre-existent pulmonary fibrosis might be at increased risk for radiation induced pneumonitis
Chest wall toxicity (myositis, neuralgia, rip fracture, subcutaneous fibrosis, skin ulceration) has been reported when tumor are located close to the respective normal tissue structures. Doses >30 Gy to the chest wall haven been correlated with these toxicities and the volume of the chest wall exposed to these doses should be minimized by conformal treatment planning [54–56].
Severe toxicity to the brachial plexus (neuropathic pain, motor weakness, or sensory alteration), large bronchi (stenosis with pulmonary atelectasis) and esophagus (ulceration, perforation, fistula) has been reported but these toxicities are rare. Limiting the total dose to the plexus to <26 Gy in 3–4 fractions can minimize the risk of toxicity [57]. The issue of SBRT for centrally located tumors close to the esophagus and large bronchi is discussed below.
Studies consistently reported that SBRT has no detrimental or negative on quality-of-life (QoL) [58–60]. Overall QoL as well as subdomains of dyspnea and cough were stable after SBRT in all studies and one study described significantly improved emotional functioning [58].
Clinical Practice of SBRT for Early Stage NSCLC
Lung SBRT is a multi-disciplinary task, involving all disciplines dealing with the diagnosis and treatment of lung cancer. Within the radiotherapy department, SBRT needs to be implemented and practiced by a multi-professional team consisting of the Radiation Oncologists, Medical Physicists and Radiation Technologists: all members of the team should have undergone dedicated training in SBRT. The development of written protocols is an essential component of the quality assurance.
Any treatment of NSCLC should be discussed within an interdisciplinary tumor board and this applies to SBRT as well. A careful assessment of the performance status is important to provide a sensible therapy concept. Perioperative morbidity is associated with older age and the presence of co-morbidities [4, 61]. Therefore, pulmonary function tests, cardiac assessment and performance status are recommended clinical assessments before estimating the operative risk and adjusting the treatment to the patient individual medical and personal situation.
In the following part, some clinical and technical issues of SBRT for stage I NSCLC will be discussed
SBRT Without Histopathological Confirmation of Disease
Histological confirmation of disease is recommended prior to any treatment for NSCLC. Transbronchial biopsy or transthoracic needle aspiration are primary methods. Nevertheless sometimes it is impossible or at high risk to prove malignancy because of the medical and/or pulmonary co-morbidities. In such cases radiological criteria of malignancy should be consulted. Swensen et al. [62] described a prediction model to estimate the probability of malignancy in solitary pulmonary nodules: clinical and radiographic characteristics are used to estimate the likelihood of malignant disease. Inclusion of FDG-PET imaging might further improve the accuracy of the prediction model [63, 64]. If malignancy is highly likely based on the described criteria, immediate SBRT without histopathological proof is justified [65], which is also standard practice in thoracic surgery [66]. Repeated imaging to evaluate the growth pattern is an option in boarderline risk-of-malignancy patients but might put the patient at risk for disease progression in the time interval [67].
Staging of Disease
In SBRT, only the primary tumor is treated with high irradiation doses and no elective nodal irradiation is performed. Consequently, a whole body FDG PET scan should be performed in all cases for exclusion of nodal metastases. The added value of FDG PET lies in the higher diagnostic accuracy for the detection of nodal metastases compared to CT-based staging (negative predictive value 90 %) [68, 69]. The FDG PET scan should be not older than 6 weeks to avoid disease progression in the interval between staging and treatment. In case of pathologic FDG uptake in mediastinal lymph nodes, further evaluation, e.g. by EBUS/EUS are mandatory. If the situation is still unclear, a mediastinoscopy may be necessary. After FDG PET based staging and exclusion of nodal disease, lymph node metastases are observed in about 10 % of the patients [70].
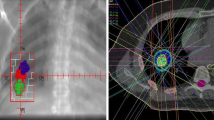
Technology of SBRT Planning and Delivery
Because lung tumors can move by several centimeters due to breathing of the patient, a motion management strategy is required for all patients [71]. This starts at treatment planning, where patient individual tumor motion is assessed by 4-dimensional CT (4D-CT), also known as respiration-correlated CT [72, 73]. Additionally, 4D-CT reduces motion artifacts and systematic errors introduced due to the non-representativeness of the captured breathing position [74, 75]. Various motion compensation techniques have been developed and are available in clinical practice – gating, tracking, breath-hold irradiation mid-ventilation concept, internal target volume concept – all with specific pros and cons [76]. It is of utmost importance, that breathing motion is consistently integrated into all steps of SBRT planning and delivery, especially into the image-guidance procedure. Though patient-specific motion management is strongly recommended, no benefit for advanced motion management strategies like gating or tracking has been found for patients with tumors moving <10–15 mm in amplitude, the majority of the patients [76, 77].
Treatment planning can be performed using 3D-conformal radiotherapy (3D-CRT), Intensity-modulated radiotherapy (IMRT) or volumetric modulated arc therapy (VMAT). All published prospective trials have used 3D-CRT but IMRT and VMAT have the potential to increase dose conformity and homogeneity and reduce treatment delivery times [78]. Type B algorithms achieve accurate dose calculation especially at the interface of lung tissue and soft tissue and their use is highly recommended [79]. Monte Carlo dose calculation algorithms achieve most accurate results but differences to collapsed cone algorithms appear small.
The position of lung tumors within the patient varies from day to day and is different between the time of treatment planning and treatment delivery. This variation of the tumor position is not caused by patient misalignment but is rather a relative motion of the pulmonary tumor within the lung. The magnitude of this variability is 5–7 mm on average and up to several centimeters in individual patients [80, 81]. To avoid missing the tumor at the time of treatment delivery with the consequence of decreased local tumor control, daily pre-treatment image-guidance (IGRT) is mandatory [77]. Various IGRT technologies are available, which can be broadly categorized into planar and volumetric imaging. Major advantage of planar imaging is the possibility to perform repetitive verification during treatment delivery; however, implanted fiducial markers are required for visualization of the soft-tissue tumor with the associated risk of pneumothorax. Major advantage of volumetric imaging is the possibility not only to verify the tumor position but also the position of critical organs at risk close to the tumor, e.g. the spinal cord.
SBRT Irradiation Dose and Fractionation
Because of large differences in single-fraction doses between studies, comparison of physical doses is less meaningful but doses are converted to biological effective doses (BED) to account fractionation effects [82]. Independently, several groups demonstrated a clear dose-effect relationship for local tumor control [83–86]: a minimum PTV dose of >100 Gy BED (biological effective dose; α/β ratio 10 Gy) achieved local tumor control >90 %. It could be demonstrated that this dose-dependent increase in local control translates into improved OS [83, 87]. A recent meta-analysis reported best OS for medium-to-high SBRT doses of 83.2–146 Gy BED; OS was worse after SBRT with >146 Gy BED indicating a detrimental effect of excessively high SBRT doses [88].
This dose of minimum 100 Gy BED is usually delivered in 1–10 fractions but reimbursement rules have resulted in a widespread use of 5 or fewer fractions in the United States. The most frequently used fractionation scheme is 3 fractions of 18 Gy as PTV encompassing dose [89]. Whereas safety of such high single and total doses has been demonstrated for peripheral lung tumors of usually <5 cm size, high rates of severe toxicity have been reported in centrally located tumors with critical organs like the esophagus and large bronchi close by [90, 91]. In contrast, safety of SBRT for centrally located tumors has been reported if the total dose is delivered using a larger number (5–10) of treatment fractions of a lower single-fraction doses [92], a concept which is called risk adapted fractionation. Eight fractions of 7.5 Gy as PTV encompassing dose is the most frequently used and best-evaluated fractionation scheme for centrally located tumors [93].
Response Assessment and Follow-Up
Regular chest CT follow-up every 3–6 months for 2–3 years and annually thereafter is recommended for early detection of secondary primary lung tumors and local recurrences amendable for salvage therapy. Localized acute (asymptomatic) pneumonitis and late pulmonary fibrotic changes are regularly observed in the follow-up CT images and the radiological appearance of the fibrotic changes may remain dynamic for several years [94]. Anyone involved in the response assessment should be aware of these normal tissue reactions to SBRT doses to avoid misinterpretation as local recurrence. An algorithm for follow-up has been proposed, which identified high-risk CT morphological features of local recurrence: enlarging opacity at primary site, sequential enlarging opacity, enlarging opacity after 12-months, bulging margins of the opacity, loss of a linear margin, and loss of air bronchograms [95]. In the presence of such high-risk CT features, an FDG-PET should be acquired and a SUVmax ⩾5 is predictive for local recurrence.
Salvage treatment of isolated local recurrences has been performed very rarely and both salvage surgery and SBRT have been described. Salvage surgery was reported as safe in two studies with 5 [96] and 7 [97], where significant SBRT-related adhesions were found in none of the patients; re-SBRT should be restricted to peripherally located tumors [98].
Summary
SBRT is an evidence-based treatment option for patients with stage I NSLCLC. Prospective and retrospective studies reported consistent results of SBRT for stage I NSCLC: local tumor control exceeding 90 % and overall survival mainly limited by the comorbidities of the patients. Safe practice of SBRT requires, that it is performed by a multi-professional team experienced and trained in SBRT and image-guided radiotherapy. It is essential that patient selection to SBRT treatment is discussed in multi-disciplinary tumor boards considering the perioperative risk of the patient and patient preference.
References
Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27(17):2758–65.
National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409.
Raz DJ, Zell JA, Ou SH, Gandara DR, Anton-Culver H, Jablons DM. Natural history of stage I non-small cell lung cancer: implications for early detection. Chest. 2007;132(1):193–9.
de Perrot M, Licker M, Reymond MA, Robert J, Spiliopoulos A. Influence of age on operative mortality and long-term survival after lung resection for bronchogenic carcinoma. Eur Respir J. 1999;14(2):419–22.
Vest MT, Herrin J, Soulos PR, Decker RH, Tanoue L, Michaud G, Kim AW, Detterbeck F, Morgensztern D, Gross CP. Use of new treatment modalities for non-small cell lung cancer care in the Medicare population. Chest. 2013;143(2):429–35.
Haasbeek CJ, Palma D, Visser O, Lagerwaard FJ, Slotman B, Senan S. Early-stage lung cancer in elderly patients: a population-based study of changes in treatment patterns and survival in the Netherlands. Ann Oncol. 2012;23(10):2743–7.
Palma D, Visser O, Lagerwaard FJ, Belderbos J, Slotman BJ, Senan S. Impact of introducing stereotactic lung radiotherapy for elderly patients with stage I non-small-cell lung cancer: a population-based time-trend analysis. J Clin Oncol. 2010;28(35):5153–9.
Rowell NP, Williams CJ. Radical radiotherapy for stage I/II non-small cell lung cancer in patients not sufficiently fit for or declining surgery (medically inoperable). Cochrane Database Syst Rev. 2001;(2):CD002935.
Martel MK, Ten Haken RK, Hazuka MB, Kessler ML, Strawderman M, Turrisi AT, Lawrence TS, Fraass BA, Lichter AS. Estimation of tumor control probability model parameters from 3-D dose distributions of non-small cell lung cancer patients. Lung Cancer. 1999;24(1):31–7.
Willner J, Baier K, Caragiani E, Tschammler A, Flentje M. Dose, volume, and tumor control prediction in primary radiotherapy of non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2002;52(2):382–9.
Partridge M, Ramos M, Sardaro A, Brada M. Dose escalation for non-small cell lung cancer: analysis and modelling of published literature. Radiother Oncol. 2011;99(1):6–11.
Sibley GS, Jamieson TA, Marks LB, Anscher MS, Prosnitz LR. Radiotherapy alone for medically inoperable stage I non-small-cell lung cancer: the Duke experience. Int J Radiat Oncol Biol Phys. 1998;40(1):149–54.
Uematsu M, Shioda A, Tahara K, Fukui T, Yamamoto F, Tsumatori G, Ozeki Y, Aoki T, Watanabe M, Kusano S. Focal, high dose, and fractionated modified stereotactic radiation therapy for lung carcinoma patients: a preliminary experience. Cancer. 1998;82(6):1062–70.
Wulf J, Hadinger U, Oppitz U, Olshausen B, Flentje M. Stereotactic radiotherapy of extracranial targets: CT-simulation and accuracy of treatment in the stereotactic body frame. Radiother Oncol. 2000;57(2):225–36.
Herfarth KK, Debus J, Lohr F, Bahner ML, Fritz P, Hoss A, Schlegel W, Wannenmacher MF. Extracranial stereotactic radiation therapy: set-up accuracy of patients treated for liver metastases. Int J Radiat Oncol Biol Phys. 2000;46(2):329–35.
Benedict SH, Yenice KM, Followill D, Galvin JM, Hinson W, Kavanagh B, Keall P, Lovelock M, Meeks S, Papiez L, et al. Stereotactic body radiation therapy: the report of AAPM Task Group 101. Med Phys. 2010;37(8):4078–101.
Potters L, Kavanagh B, Galvin JM, Hevezi JM, Janjan NA, Larson DA, Mehta MP, Ryu S, Steinberg M, Timmerman R, et al. American Society for Therapeutic Radiology and Oncology (ASTRO) and American College of Radiology (ACR) practice guideline for the performance of stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2010;76(2):326–32.
Kirkbride P, Cooper T. Stereotactic body radiotherapy. Guidelines for commissioners, providers and clinicians: a national report. Clin Oncol. 2011;23(3):163–4.
Sahgal A, Roberge D, Schellenberg D, Purdie TG, Swaminath A, Pantarotto J, Filion E, Gabos Z, Butler J, Letourneau D, et al. The Canadian Association of Radiation Oncology scope of practice guidelines for lung, liver and spine stereotactic body radiotherapy. Clin Oncol. 2012;24(9):629–39.
Shirvani SM, Jiang J, Chang JY, Welsh JW, Gomez DR, Swisher S, Buchholz TA, Smith BD. Comparative effectiveness of 5 treatment strategies for early-stage non-small cell lung cancer in the elderly. Int J Radiat Oncol Biol Phys. 2012;84(5):1060–70.
Takeda A, Sanuki N, Eriguchi T, Kaneko T, Morita S, Handa H, Aoki Y, Oku Y, Kunieda E. Stereotactic ablative body radiation therapy for octogenarians with non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2013;86(2):257–63.
Haasbeek CJ, Lagerwaard FJ, Antonisse ME, Slotman BJ, Senan S. Stage I nonsmall cell lung cancer in patients aged > or =75 years: outcomes after stereotactic radiotherapy. Cancer. 2010;116(2):406–14.
Saha SP, Bender M, Ferraris VA, Davenport DL. Surgical treatment of lung cancer in octogenarians. South Med J. 2013;106(6):356–61.
Palma D, Lagerwaard F, Rodrigues G, Haasbeek C, Senan S. Curative treatment of stage I non-small-cell lung cancer in patients with severe COPD: stereotactic radiotherapy outcomes and systematic review. Int J Radiat Oncol Biol Phys. 2012;82(3):1149–56.
Guckenberger M, Kestin LL, Hope AJ, Belderbos J, Werner-Wasik M, Yan D, Sonke JJ, Bissonnette JP, Wilbert J, Xiao Y, et al. Is there a lower limit of pretreatment pulmonary function for safe and effective stereotactic body radiotherapy for early-stage non-small cell lung cancer? J Thorac Oncol. 2012;7(3):542–51.
Stephans KL, Djemil T, Reddy CA, Gajdos SM, Kolar M, Machuzak M, Mazzone P, Videtic GM. Comprehensive analysis of pulmonary function Test (PFT) changes after stereotactic body radiotherapy (SBRT) for stage I lung cancer in medically inoperable patients. J Thorac Oncol. 2009;4(7):838–44.
Takeda A, Enomoto T, Sanuki N, Handa H, Aoki Y, Oku Y, Kunieda E. Reassessment of declines in pulmonary function >/=1 year after stereotactic body radiotherapy. Chest. 2013;143(1):130–7.
Bishawi M, Kim B, Moore WH, Bilfinger TV. Pulmonary function testing after stereotactic body radiotherapy to the lung. Int J Radiat Oncol Biol Phys. 2012;82(1):e107–10.
Henderson M, McGarry R, Yiannoutsos C, Fakiris A, Hoopes D, Williams M, Timmerman R. Baseline pulmonary function as a predictor for survival and decline in pulmonary function over time in patients undergoing stereotactic body radiotherapy for the treatment of stage I non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2008;72(2):404–9.
Nagata Y, Takayama K, Matsuo Y, Norihisa Y, Mizowaki T, Sakamoto T, Sakamoto M, Mitsumori M, Shibuya K, Araki N, et al. Clinical outcomes of a phase I/II study of 48 Gy of stereotactic body radiotherapy in 4 fractions for primary lung cancer using a stereotactic body frame. Int J Radiat Oncol Biol Phys. 2005;63(5):1427–31.
Baumann P, Nyman J, Hoyer M, Wennberg B, Gagliardi G, Lax I, Drugge N, Ekberg L, Friesland S, Johansson KA, et al. Outcome in a prospective phase II trial of medically inoperable stage I non-small-cell lung cancer patients treated with stereotactic body radiotherapy. J Clin Oncol. 2009;27(20):3290–6.
Fakiris AJ, McGarry RC, Yiannoutsos CT, Papiez L, Williams M, Henderson MA, Timmerman R. Stereotactic body radiation therapy for early-stage non-small-cell lung carcinoma: four-year results of a prospective phase II study. Int J Radiat Oncol Biol Phys. 2009;75(3):677–82.
Ricardi U, Filippi AR, Guarneri A, Giglioli FR, Ciammella P, Franco P, Mantovani C, Borasio P, Scagliotti GV, Ragona R. Stereotactic body radiation therapy for early stage non-small cell lung cancer: results of a prospective trial. Lung Cancer. 2010;68(1):72–7.
Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, Fakiris A, Bezjak A, Videtic G, Johnstone D, et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303(11):1070–6.
Bral S, Gevaert T, Linthout N, Versmessen H, Collen C, Engels B, Verdries D, Everaert H, Christian N, De Ridder M, et al. Prospective, risk-adapted strategy of stereotactic body radiotherapy for early-stage non-small-cell lung cancer: results of a Phase II trial. Int J Radiat Oncol Biol Phys. 2011;80(5):1343–9.
Grutters JP, Kessels AG, Pijls-Johannesma M, De Ruysscher D, Joore MA, Lambin P. Comparison of the effectiveness of radiotherapy with photons, protons and carbon-ions for non-small cell lung cancer: a meta-analysis. Radiother Oncol. 2010;95(1):32–40.
Kopek N, Paludan M, Petersen J, Hansen AT, Grau C, Hoyer M. Co-morbidity index predicts for mortality after stereotactic body radiotherapy for medically inoperable early-stage non-small cell lung cancer. Radiother Oncol. 2009;93(3):402–7.
Guckenberger M, Allgauer M, Appold S, Dieckmann K, Ernst I, Ganswindt U, Holy R, Nestle U, Nevinny-Stickel M, Semrau S, et al. Safety and efficacy of stereotactic body radiotherapy for stage i non-small-cell lung cancer in routine clinical practice: a patterns-of-care and outcome analysis. J Thorac Oncol. 2013;8(8):1050–8.
NCCN Clinical Practice Guidelines in Oncology: non-small cell lung cancer Version 1.2013. http://www.nccn.org/.
Vansteenkiste J, De Ruysscher D, Eberhardt WEE, Lim E, Senan S, Felip E, Peters S. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi89–98.
Renaud S, Falcoz PE, Olland A, Massard G. Is radiofrequency ablation or stereotactic ablative radiotherapy the best treatment for radically treatable primary lung cancer unfit for surgery? Interact Cardiovasc Thorac Surg. 2013;16(1):68–73.
Crabtree T, Puri V, Timmerman R, Fernando H, Bradley J, Decker PA, Paulus R, Putnum Jr JB, Dupuy DE, Meyers B. Treatment of stage I lung cancer in high-risk and inoperable patients: comparison of prospective clinical trials using stereotactic body radiotherapy (RTOG 0236), sublobar resection (ACOSOG Z4032), and radiofrequency ablation (ACOSOG Z4033). J Thorac Cardiovasc Surg. 2013;145(3):692–9.
Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60(3):615–22; discussion 622–3.
Whitson BA, Groth SS, Andrade RS, Maddaus MA, Habermann EB, D’Cunha J. Survival after lobectomy versus segmentectomy for stage I non-small cell lung cancer: a population-based analysis. Ann Thorac Surg. 2011;92(6):1943–50.
Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, Okada M. Oncologic outcomes of segmentectomy compared with lobectomy for clinical stage IA lung adenocarcinoma: propensity score-matched analysis in a multicenter study. J Thorac Cardiovasc Surg. 2013;146(2):358–64.
Grills IS, Mangona VS, Welsh R, Chmielewski G, McInerney E, Martin S, Wloch J, Ye H, Kestin LL. Outcomes after stereotactic lung radiotherapy or wedge resection for stage I non-small-cell lung cancer. J Clin Oncol. 2010;28(6):928–35.
Puri V, Crabtree TD, Kymes S, Gregory M, Bell J, Bradley JD, Robinson C, Patterson GA, Kreisel D, Krupnick AS, et al. A comparison of surgical intervention and stereotactic body radiation therapy for stage I lung cancer in high-risk patients: a decision analysis. J Thorac Cardiovasc Surg. 2012;143(2):428–36.
Verstegen NE, Oosterhuis JW, Palma DA, Rodrigues G, Lagerwaard FJ, van der Elst A, Mollema R, van Tets WF, Warner A, Joosten JJ, et al. Stage I-II non-small-cell lung cancer treated using either stereotactic ablative radiotherapy (SABR) or lobectomy by video-assisted thoracoscopic surgery (VATS): outcomes of a propensity score-matched analysis. Ann Oncol. 2013;24(6):1543–8.
Oshiro Y, Aruga T, Tsuboi K, Marino K, Hara R, Sanayama Y, Itami J. Stereotactic body radiotherapy for lung tumors at the pulmonary hilum. Strahlenther Onkol. 2010;186(5):274–9.
Lagerwaard FJ, Verstegen NE, Haasbeek CJ, Slotman BJ, Paul MA, Smit EF, Senan S. Outcomes of stereotactic ablative radiotherapy in patients with potentially operable stage I non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2012;83(1):348–53.
Guckenberger M, Baier K, Polat B, Richter A, Krieger T, Wilbert J, Mueller G, Flentje M. Dose-response relationship for radiation-induced pneumonitis after pulmonary stereotactic body radiotherapy. Radiother Oncol. 2010;97(1):65–70.
Ong CL, Palma D, Verbakel WF, Slotman BJ, Senan S. Treatment of large stage I-II lung tumors using stereotactic body radiotherapy (SBRT): planning considerations and early toxicity. Radiother Oncol. 2010;97(3):431–6.
Haasbeek C, Palma D, Lagerwaard FJ, Slotman BJ, Senan S. Stereotactic Body Radiotherapy (SBRT) outcomes in stage I lung cancer patients with severe chronic obstructive pulmonary disease (GOLD III-IV). Int J Radiat Oncol Biol Phys. 2010;78(3):S183.
Dunlap NE, Cai J, Biedermann GB, Yang W, Benedict SH, Sheng K, Schefter TE, Kavanagh BD, Larner JM. Chest wall volume receiving >30 Gy predicts risk of severe pain and/or rib fracture after lung stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys. 2010;76(3):796–801.
Stephans KL, Djemil T, Tendulkar RD, Robinson CG, Reddy CA, Videtic GM. Prediction of chest wall toxicity from lung stereotactic body radiotherapy (SBRT). Int J Radiat Oncol Biol Phys. 2012;82(2):974–80.
Woody NM, Videtic GM, Stephans KL, Djemil T, Kim Y, Xia P. Predicting chest wall pain from lung stereotactic body radiotherapy for different fractionation schemes. Int J Radiat Oncol Biol Phys. 2012;83(1):427–34.
Forquer JA, Fakiris AJ, Timmerman RD, Lo SS, Perkins SM, McGarry RC, Johnstone PA. Brachial plexopathy from stereotactic body radiotherapy in early-stage NSCLC: dose-limiting toxicity in apical tumor sites. Radiother Oncol. 2009;93(3):408–13.
van der Voort van Zyp NC, Prevost JB, van der Holt B, Braat C, van Klaveren RJ, Pattynama PM, Levendag PC, Nuyttens JJ. Quality of life after stereotactic radiotherapy for stage I non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2010;77(1):31–7.
Widder J, Postmus D, Ubbels JF, Wiegman EM, Langendijk JA. Survival and quality of life after stereotactic or 3D-conformal radiotherapy for inoperable early-stage lung cancer. Int J Radiat Oncol Biol Phys. 2011;81(4):e291–7.
Lagerwaard FJ, Aaronson NK, Gundy CM, Haasbeek CJ, Slotman BJ, Senan S. Patient-reported quality of life after stereotactic ablative radiotherapy for early-stage lung cancer. J Thorac Oncol. 2012;7(7):1148–54.
Bolliger CT, Wyser C, Roser H, Soler M, Perruchoud AP. Lung scanning and exercise testing for the prediction of postoperative performance in lung resection candidates at increased risk for complications. Chest. 1995;108(2):341–8.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8):849–55.
Patel VK, Naik SK, Naidich DP, Travis WD, Weingarten JA, Lazzaro R, Gutterman DD, Wentowski C, Grosu HB, Raoof S. A practical algorithmic approach to the diagnosis and management of solitary pulmonary nodules: part 2: pretest probability and algorithm. Chest. 2013;143(3):840–6.
Patel VK, Naik SK, Naidich DP, Travis WD, Weingarten JA, Lazzaro R, Gutterman DD, Wentowski C, Grosu HB, Raoof S. A practical algorithmic approach to the diagnosis and management of solitary pulmonary nodules: part 1: radiologic characteristics and imaging modalities. Chest. 2013;143(3):825–39.
Verstegen NE, Lagerwaard FJ, Haasbeek CJ, Slotman BJ, Senan S. Outcomes of stereotactic ablative radiotherapy following a clinical diagnosis of stage I NSCLC: comparison with a contemporaneous cohort with pathologically proven disease. Radiother Oncol. 2011;101(2):250–4.
Sawada S, Yamashita MK, Eisaku N, Naoyuki O, Isao S, Yoshihiko ST. Evaluation of resected tumors that were not diagnosed histologically but were suspected of lung cancer preoperatively. J Thorac Oncol. 2007;2(8):S422.
Murai T, Shibamoto Y, Baba F, Hashizume C, Mori Y, Ayakawa S, Kawai T, Takemoto S, Sugie C, Ogino H. Progression of non-small-cell lung cancer during the interval before stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys. 2012;82(1):463–7.
Stiles BM, Servais EL, Lee PC, Port JL, Paul S, Altorki NK. Point: clinical stage IA non-small cell lung cancer determined by computed tomography and positron emission tomography is frequently not pathologic IA non-small cell lung cancer: the problem of understaging. J Thorac Cardiovasc Surg. 2009;137(1):13–9.
Park HK, Jeon K, Koh WJ, Suh GY, Kim H, Kwon OJ, Chung MP, Lee KS, Shim YM, Han J, et al. Occult nodal metastasis in patients with non-small cell lung cancer at clinical stage IA by PET/CT. Respirology. 2010;15(8):1179–84.
Senthi S, Lagerwaard FJ, Haasbeek CJ, Slotman BJ, Senan S. Patterns of disease recurrence after stereotactic ablative radiotherapy for early stage non-small-cell lung cancer: a retrospective analysis. Lancet Oncol. 2012;13(8):802–9.
Seppenwoolde Y, Shirato H, Kitamura K, Shimizu S, van Herk M, Lebesque JV, Miyasaka K. Precise and real-time measurement of 3D tumor motion in lung due to breathing and heartbeat, measured during radiotherapy. Int J Radiat Oncol Biol Phys. 2002;53(4):822–34.
Ford EC, Mageras GS, Yorke E, Ling CC. Respiration-correlated spiral CT: a method of measuring respiratory-induced anatomic motion for radiation treatment planning. Med Phys. 2003;30(1):88–97.
Low DA, Nystrom M, Kalinin E, Parikh P, Dempsey JF, Bradley JD, Mutic S, Wahab SH, Islam T, Christensen G, et al. A method for the reconstruction of four-dimensional synchronized CT scans acquired during free breathing. Med Phys. 2003;30(6):1254–63.
Fredberg Persson G, Eklund Nygaard D, Munck Af Rosenschold P, Richter Vogelius I, Josipovic M, Specht L, Korreman SS. Artifacts in conventional computed tomography (CT) and free breathing four-dimensional CT induce uncertainty in gross tumor volume determination. Int J Radiat Oncol Biol Phys. 2011;80(5):1573–80.
Hurkmans CW, van Lieshout M, Schuring D, van Heumen MJ, Cuijpers JP, Lagerwaard FJ, Widder J, van der Heide UA, Senan S. Quality assurance of 4D-CT scan techniques in multicenter phase III trial of surgery versus stereotactic radiotherapy (radiosurgery or surgery for operable early stage (stage 1A) non-small-cell lung cancer [ROSEL] study). Int J Radiat Oncol Biol Phys. 2010;80(3):918–27.
Wolthaus JW, Sonke JJ, van Herk M, Belderbos JS, Rossi MM, Lebesque JV, Damen EM. Comparison of different strategies to use four-dimensional computed tomography in treatment planning for lung cancer patients. Int J Radiat Oncol Biol Phys. 2008;70(4):1229–38.
Guckenberger M, Krieger T, Richter A, Baier K, Wilbert J, Sweeney RA, Flentje M. Potential of image-guidance, gating and real-time tracking to improve accuracy in pulmonary stereotactic body radiotherapy. Radiother Oncol. 2009;91(3):288–95.
Ong CL, Verbakel WF, Cuijpers JP, Slotman BJ, Lagerwaard FJ, Senan S. Stereotactic radiotherapy for peripheral lung tumors: a comparison of volumetric modulated arc therapy with 3 other delivery techniques. Radiother Oncol. 2010;97(3):437–42.
Hurkmans CW, Cuijpers JP, Lagerwaard FJ, Widder J, van der Heide UA, Schuring D, Senan S. Recommendations for implementing stereotactic radiotherapy in peripheral stage IA non-small cell lung cancer: report from the Quality Assurance Working Party of the randomised phase III ROSEL study. Radiat Oncol. 2009;4:1.
Guckenberger M, Baier K, Guenther I, Richter A, Wilbert J, Sauer O, Vordermark D, Flentje M. Reliability of the bony anatomy in image-guided stereotactic radiotherapy of brain metastases. Int J Radiat Oncol Biol Phys. 2007;69(1):294–301.
Purdie TG, Bissonnette JP, Franks K, Bezjak A, Payne D, Sie F, Sharpe MB, Jaffray DA. Cone-beam computed tomography for on-line image guidance of lung stereotactic radiotherapy: localization, verification, and intrafraction tumor position. Int J Radiat Oncol Biol Phys. 2007;68(1):243–52.
Guckenberger M, Klement RJ, Allgauer M, Appold S, Dieckmann K, Ernst I, Ganswindt U, Holy R, Nestle U, Nevinny-Stickel M, et al. Applicability of the linear-quadratic formalism for modeling local tumor control probability in high dose per fraction stereotactic body radiotherapy for early stage non-small cell lung cancer. Radiother Oncol. 2013;109(1):13–20.
Onishi H, Araki T, Shirato H, Nagata Y, Hiraoka M, Gomi K, Yamashita T, Niibe Y, Karasawa K, Hayakawa K, et al. Stereotactic hypofractionated high-dose irradiation for stage I nonsmall cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multiinstitutional study. Cancer. 2004;101(7):1623–31.
Wulf J, Baier K, Mueller G, Flentje MP. Dose-response in stereotactic irradiation of lung tumors. Radiother Oncol. 2005;77(1):83–7.
Guckenberger M, Wulf J, Mueller G, Krieger T, Baier K, Gabor M, Richter A, Wilbert J, Flentje M. Dose-response relationship for image-guided stereotactic body radiotherapy of pulmonary tumors: relevance of 4D dose calculation. Int J Radiat Oncol Biol Phys. 2009;74(1):47–54.
Grills IS, Hope AJ, Guckenberger M, Kestin LL, Werner-Wasik M, Yan D, Sonke JJ, Bissonnette JP, Wilbert J, Xiao Y, et al. A collaborative analysis of stereotactic lung radiotherapy outcomes for early-stage non-small-cell lung cancer using daily online cone-beam computed tomography image-guided radiotherapy. J Thorac Oncol. 2012;7(9):1382–93.
Onimaru R, Fujino M, Yamazaki K, Onodera Y, Taguchi H, Katoh N, Hommura F, Oizumi S, Nishimura M, Shirato H. Steep dose-response relationship for stage I non-small-cell lung cancer using hypofractionated high-dose irradiation by real-time tumor-tracking radiotherapy. Int J Radiat Oncol Biol Phys. 2008;70(2):374–81.
Zhang J, Yang F, Li B, Li H, Liu J, Huang W, Wang D, Yi Y, Wang J. Which is the optimal biologically effective dose of stereotactic body radiotherapy for Stage I non-small-cell lung cancer? A meta-analysis. Int J Radiat Oncol Biol Phys. 2011;81(4):e305–16.
McGarry RC, Papiez L, Williams M, Whitford T, Timmerman RD. Stereotactic body radiation therapy of early-stage non-small-cell lung carcinoma: phase I study. Int J Radiat Oncol Biol Phys. 2005;63(4):1010–5.
Timmerman R, McGarry R, Yiannoutsos C, Papiez L, Tudor K, DeLuca J, Ewing M, Abdulrahman R, DesRosiers C, Williams M, et al. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. J Clin Oncol. 2006;24(30):4833–9.
Song SY, Choi W, Shin SS, Lee SW, Ahn SD, Kim JH, Je HU, Park CI, Lee JS, Choi EK. Fractionated stereotactic body radiation therapy for medically inoperable stage I lung cancer adjacent to central large bronchus. Lung Cancer. 2009;66(1):89–93.
Senthi S, Haasbeek CJ, Slotman BJ, Senan S. Outcomes of stereotactic ablative radiotherapy for central lung tumours: a systematic review. Radiother Oncol. 2013;106(3):276–82.
Haasbeek CJ, Lagerwaard FJ, Slotman BJ, Senan S. Outcomes of stereotactic ablative radiotherapy for centrally located early-stage lung cancer. J Thorac Oncol. 2011;6(12):2036–43.
Guckenberger M, Heilman K, Wulf J, Mueller G, Beckmann G, Flentje M. Pulmonary injury and tumor response after stereotactic body radiotherapy (SBRT): results of a serial follow-up CT study. Radiother Oncol. 2007;85(3):435–42.
Huang K, Dahele M, Senan S, Guckenberger M, Rodrigues GB, Ward A, Boldt RG, Palma DA. Radiographic changes after lung stereotactic ablative radiotherapy (SABR) – Can we distinguish recurrence from fibrosis? A systematic review of the literature. Radiother Oncol. 2012;102(3):335–42.
Chen F, Matsuo Y, Yoshizawa A, Sato T, Sakai H, Bando T, Okubo K, Shibuya K, Date H. Salvage lung resection for non-small cell lung cancer after stereotactic body radiotherapy in initially operable patients. J Thorac Oncol. 2010;5(12):1999–2002.
Neri S, Takahashi Y, Terashi T, Hamakawa H, Tomii K, Katakami N, Kokubo M. Surgical treatment of local recurrence after stereotactic body radiotherapy for primary and metastatic lung cancers. J Thorac Oncol. 2010;5(12):2003–7.
Peulen H, Karlsson K, Lindberg K, Tullgren O, Baumann P, Lax I, Lewensohn R, Wersall P. Toxicity after reirradiation of pulmonary tumours with stereotactic body radiotherapy. Radiother Oncol. 2011;101(2):260–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Guckenberger, M. (2015). Stereotaxic Body Radiotherapy for Stage I NSCLC. In: Peters, S., Besse, B. (eds) New Therapeutic Strategies in Lung Cancers. Springer, Cham. https://doi.org/10.1007/978-3-319-06062-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-06062-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06061-3
Online ISBN: 978-3-319-06062-0
eBook Packages: MedicineMedicine (R0)