Abstract
Stereotactic body radiotherapy (SBRT) may be a potential alternative to surgical resection in high-risk operable patients with early-stage non-small cell lung cancer (NSCLC). A number of clinical studies have been undertaken to answer this question, although the conclusion has remained undetermined. Although three randomized clinical trials have failed, currently several prospective clinical trials are ongoing on SBRT versus surgery for early-stage NSCLC. This review article was designed to overview the previous and ongoing clinical trials and to discuss the future perspectives in the comparisons.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
While some researchers hypothesized equipoise between stereotactic body radiotherapy (SBRT) and surgery in low-risk or high-risk operable patients with early-stage non-small cell lung cancer (NSCLC), the definition of operability is ambiguous [1]. Given the ambiguous definition of the operability, it has been a challenge to investigate SBRT versus surgery (pulmonary resection) in operable patients. There is no high-level evidence available to address this topic, given the fact that there have been no completed randomized controlled trials on SBRT versus surgery for early-stage NSCLC.
Lobectomy with systematic lymph node dissection remains the accepted standard for low-risk patients with clinical stage I NSCLC. Specifically, the guidelines from the Japan Lung Cancer Society [2], European Society of Medical Oncology [3], and National Comprehensive Cancer Network (NCCN) [4] strongly recommend that operable patients with early-stage NSCLC should undergo lobectomy and mediastinal lymph node dissection.
In patients with early-stage NSCLC who are medically compromised but operable, treatment modalities are controversial because SBRT or stereotactic ablative radiotherapy (SABR) has been increasingly recognized as an alternative to surgical resection for early-stage NSCLC in those patients [5,6,7].
A majority of original studies that have sought to answer this important question are largely retrospective cohort studies [7,8,9] and single institutional reports [5, 10, 11]. Moreover, recently published meta-analyses performed quantitative syntheses of pooled data mostly from retrospective studies, therefore, were not free of a number of biases inherent to retrospective studies [12,13,14,15,16,17]. In terms of minimizing those biases, prospective (and ideally randomized) trials would provide fair comparisons between SBRT and surgery. In this article, we set out to review previous clinical trials, summarize ongoing ones, and discuss future perspectives.
Previous clinical trials
Before planning any well-designed clinical trials, we should learn from previous failed trials because the history of medicine may also repeat itself. Previously, three-phase 3 randomized studies have been initiated to compare SABR with surgery in patients with early-stage NSCLC (the STARS trial [NCT00840749], the ROSEL trial [NCT00687986], and the ACOSOG Z4099 trial [NCT01336894]), however, all were closed early because of slow accrual. In an unplanned and post hoc analysis of two randomized trials (the STARS trial and the ROSEL trial) that each closed early due to inadequate accrual, Joe Chang and colleagues compared stereotactic ablative radiotherapy (SABR) with lobectomy for stage I NSCLC in the article titled “Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomized trials.” in Lancet Oncology in 2015 [18]. Since the publication, there have been to date no supporting results from other prospective trials for 4 years.
What were the study design and major findings?
Definition of operability (for example, in terms of comorbidities and pulmonary function test) was not described in the Lancet Oncology manuscript. The 28 sites in the STARS trial randomized only 36 patients, and the ten sites in the ROSEL study randomized only 22 patients. In their analysis of two studies, only 4% (58 patients) of planned patients were enrolled. The primary outcome was overall survival and the median follow-up was 40.2 months (median survival was not reached in either group). There were 6 events (deaths) in the surgery arm and one event in SABR arm. The hazard ratio for overall survival was 0.14 (95% confidence interval: 0.017–1.19), although the p value from log-rank test to evaluate the difference in overall survival was 0.037. The hazard ratio for recurrence-free survival was 0.69 (95% 0.21–2.29). On the basis of these results, the authors concluded that SABR could be an option for operable clinical stage I NSCLC.
What were the responses to the article?
To my knowledge, one supportive comment to the above article and four critical comments were published in Lancet Oncology [19,20,21,22,23]. A majority of the comments on the publication were very critical of underpowered statistical analyses, poor surgical quality, and funding initiatives. Additionally, the issues of an unplanned publication of two underpowered clinical trials were discussed also in the Journal of Thoracic and Cardiovascular Surgery [24, 25]. The expert review and the comment on the review both raised the concerns for inadequate statistical power and follow-up, instability of the results, and the results not supporting the conclusion.
Ongoing clinical trials
In search of ongoing randomized trials that compare surgery and SBRT for early-stage NSCLC, the website “ClinicalTrials.gov”, which is run by the United States National Library of Medicine at the National Institutes of Health, was queried with the following key words: “non-small cell lung cancer”, “surgery”, and “radiotherapy”. In total, 244 study titles were identified with the search. After reviewing the study details, five prospective clinical trials in comparison of surgery and stereotactic body radiotherapy for patients with early-stage NSCLC were selected for review (Tables 1, 2).
Study characteristics
All the studies required the stage of the disease (stage I non-small cell lung cancer) and an eligibility (mediastinal staging) for enrollment. Among the studies varied the primary country, specialty of the principal investigator, age limit, study design, extent of pulmonary resection, primary outcome, sample size, description of cardiopulmonary function for enrollment, and follow-up periods. Among the five clinical trials, four studies (80%) required being biopsy-proven for enrollment. The primary country was United States of America in three studies and the primary investigator was a thoracic surgeon in one study (20%). Regarding the study design, three studies (60%) were randomized controlled studies, all of which are still recruiting patients. The estimated sample size of the studies ranged from 76 to 670 patients. Study results were not available in any study.
Future perspectives
In general, the study designs of ongoing prospective clinical trials still leave room to be improved. Each of PICO (patient, intervention, comparison, and outcome) that are fundamental in clinical research should be reviewed.
Eligible patients should be high-risk operable patients. It does not appear a good idea to include both low-risk operable patients and high-risk operable patients in the same “surgery” group, and I would suggest they should first focus on high-risk patients because there is no high-level evidence for such a patient group. Clinical equipoise will be of utmost importance for patient accrual. For that purpose, criteria for patient enrollment should include comorbidity information and pulmonary function test. The control group is ideally made from randomization. Given the nature of randomization, selection bias, information bias, evaluation bias, and confounding factors are presumably minimized. A sufficient sample size is a prerequisite for significant statistical analysis in randomized controlled trials. On the other hand, a small number of patients from a large number of institutions will be associated with difficult quality control.
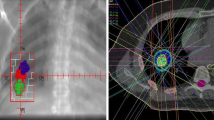
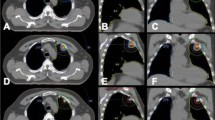
The issues of Intervention and Comparison will be, as pointed out previously, mainly related to surgery. First, quality of surgery appears more difficult to control than that of SBRT, therefore, should be evaluated using quality indicators of pulmonary resection [26]. Another issue in this setting would be a more complex post-treatment management in surgical patients. Thoracic surgical patients require inpatient and outpatient managements following pulmonary resection, whereas healthy SBRT patients will probably be managed on an outpatient basis. Third, advantages of minimally invasive approaches such as (uniport or multi-port) video-assisted thoracoscopic surgery and robotic-assisted thoracoscopic surgery should be recognized in contrast to conventional open thoracotomy. The extent of pulmonary resection also varied between lobectomy, segmentectomy, and wedge resection and should be specified in each clinical trial. Ideally, surgical patients in randomized controlled studies should be operated on by certified thoracic surgeons if SBRT patients are treated using qualified SBRT devices.
In conclusion, we should strive to develop and perform a well-designed prospective clinical trial. High-risk operable patients should first be focused on. Patients, intervention, comparison, and outcomes should be carefully discussed in developing research protocols.
References
Onishi H, Shirato H, Nagata Y, Hiraoka M, Fujino M, Gomi K, et al. Stereotactic body radiotherapy (SBRT) for operable stage I non-small-cell lung cancer: can SBRT be comparable to surgery? Int J Radiat Oncol Biol Phys. 2011;81:1352–8.
The Japan Lung Cancer Society’s guidelines for treatments of Lung Cancer. https://www.haigan.gr.jp/guideline/2018/1/2/180102010100.html#cq2. Accessed 12 Oct 2019
NCCN Clinical Practice Guidelines in Oncology. Non-small cell lung cancer. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 12 Oct 2019
ESMO Clinical Practice Guidelines: lung and chest tumours. https://www.esmo.org/Guidelines/Lung-and-Chest-Tumours. Accessed 12 Oct 2019
Matsuo Y, Chen F, Hamaji M, Kawaguchi A, Ueki N, Nagata Y, et al. Comparison of long-term survival outcomes between stereotactic body radiotherapy and sublobar resection for stage I non-small-cell lung cancer in patients at high risk for lobectomy: a propensity score matching analysis. Eur J Cancer. 2014;50:2932–8.
Verstegen NE, Oosterhuis JW, Palma DA, Rodrigues G, Lagerwaard FJ, van der Elst A, et al. Stage I-II non-small-cell lung cancer treated using either stereotactic ablative radiotherapy (SABR) or lobectomy by video-assisted thoracoscopic surgery (VATS): outcomes of a propensity score-matched analysis. Ann Oncol. 2013;24:1543–8.
Grills IS, Mangona VS, Welsh R, Chmielewski G, McInerney E, Martin S, et al. Outcomes after stereotactic lung radiotherapy 411 or wedge resection for stage I non-small-cell lung cancer. J Clin Oncol. 2010;28:928–35.
Nakagawa T, Negoro Y, Matsuoka T, Okumura N, Dodo Y. Comparison of the outcomes of stereotactic body radiotherapy and surgery in elderly patients with cT1-2N0M0 non-small cell lung cancer. Respir Investig. 2014;52:221–6.
Paul S, Lee PC, Mao J, Isaacs AJ, Sedrakyan A. Long term survival with stereotactic ablative radiotherapy (SABR) versus thoracoscopic sublobar lung resection in elderly people: national population based study with propensity matched comparative analysis. BMJ. 2016;8(354):i3570.
Hamaji M, Chen F, Matsuo Y, Kawaguchi A, Morita S, Ueki N, Sonobe M, Nagata Y, Hiraoka M, Date H. Video-assisted thoracoscopic lobectomy versus stereotactic radiotherapy for stage I lung cancer. Ann Thorac Surg. 2015;99:1122–9.
Port JL, Parashar B, Osakwe N, Nasar A, Lee PC, Paul S, et al. A propensity-matched analysis of wedge resection and stereotactic body radiotherapy for early stage lung cancer. Ann Thorac Surg. 2014;98:1152–9.
Wang HH, Zhang CZ, Zhang BL, Chen J, Zeng XL, Deng L, et al. Sublobar resection is associated with improved outcomes over radiotherapy in the management of high-risk elderly patients with Stage I non-small cell lung cancer: a systematic review and meta-analysis. Oncotarget. 2017;8:6033–42.
Ma L, Xiang J. Clinical outcomes of video-assisted thoracic surgery and stereotactic body radiation therapy for early-stage non-small cell lung cancer: a meta-analysis. Thorac Cancer. 2016;7:442–51.
Zheng X, Schipper M, Kidwell K, Lin J, Reddy R, Ren Y, Chang A, Lv F, Orringer M, Spring Kong FM. Survival outcome after stereotactic body radiation therapy and surgery for stage I non-small cell lung cancer: a meta-analysis. Int J Radiat Oncol Biol Phys. 2014;90:603–11.
Zhang B, Zhu F, Ma X, Tian Y, Cao D, Luo S, Xuan Y, Liu L, Wei Y. Matched-pair comparisons of stereotactic body radiotherapy (SBRT) versus surgery for the treatment of early stage non-small cell lung cancer: a systematic review and meta-analysis. Radiother Oncol. 2014;112:250–5.
Li M, Yang X, Chen Y, Yang X, Dai X, Sun F, et al. Stereotactic body radiotherapy or stereotactic ablative radiotherapy versus surgery for patients with T1-3N0M0 non-small cell lung cancer: a systematic review and meta-analysis. Onco Targets Ther. 2017;10:2885–922.
Chen H, Laba JM, Boldt RG, Goodman CD, Palma DA, Senan S, et al. Stereotactic ablative radiation therapy versus surgery in early lung cancer: a meta-analysis of propensity score studies. Int J Radiat Oncol Biol Phys. 2018;101:186–94.
Chang JY, Senan S, Paul MA, Mehran RJ, Louie AV, Balter P, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol. 2015;16:630–7.
Treasure T, Rintoul RC, Macbeth F. SABR in early operable lung cancer: time for evidence. Lancet Oncol. 2015;16:597–8.
Hamaji M, Groth SS, Sugarbaker DJ, Burt BM. Surgery versus SABR for resectable non-small-cell lung cancer. Lancet Oncol. 2015;16:e372.
Dearman C, van As N, Crellin A, Slevin N, Sharma RA. Surgery versus SABR for resectable non-small-cell lung cancer. Lancet Oncol. 2015;16:e373–e374374.
Opitz I, Rocco G, Brunelli A, Varela G, Massard G, Weder W, European Society of Thoracic Surgeons. Surgery versus SABR for resectable non-small-cell lung cancer. Lancet Oncol. 2015;16:e372–e373373.
Zhang L, Tian J, Wang C. Surgery versus SABR for resectable non-small-cell lung cancer. Lancet Oncol. 2015;16:e371–e372372.
Meyers BF, Puri V, Broderick SR, Samson P, Keogan K, Crabtree TD. Lobectomy versus stereotactic body radiotherapy for stage I non-small cell lung cancer: post hoc analysis dressed up as level-1 evidence? J. Thorac. Cardiovasc. Surg. 2015;150:468–71.
Jones DR. Do we know bad science when we see it? J Thorac Cardiovasc Surg. 2015;150:472–3.
Cassivi SD, Allen MS, Vanderwaerdt GD, Ewoldt LL, Cordes ME, Wigle DA, Nichols FC, Pairolero PC, Deschamps C. Patient-centered quality indicators for pulmonary resection. Ann Thorac Surg. 2008;86:927–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Masatsugu Hamaji declares that he has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hamaji, M. Surgery and stereotactic body radiotherapy for early-stage non-small cell lung cancer: prospective clinical trials of the past, the present, and the future. Gen Thorac Cardiovasc Surg 68, 692–696 (2020). https://doi.org/10.1007/s11748-019-01239-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01239-8