Abstract
Post-traumatic ankle arthritis is a common cause of pain and disability in patients who have sustained fractures or instability events. Unlike hip and knee arthritis, the biology of ankle arthritis is less commonly purely degenerative. The treatment of this condition varies based on patient presentation, etiology, and surgeon experience. Arthrodesis is the gold standard treatment for this condition, and multiple options are available to the treating surgeon regarding approach, implant selection, and concomitant procedures. There are some basic techniques that should be known to all foot and ankle surgeons, as well as some special considerations for particularly challenging cases and revision options.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Ankle arthritis occurs much less commonly than arthritis of the hip and knee. Autopsy and cadaveric studies find advanced degenerative changes at the ankle three times less prevalent than the larger joints [1, 2]. While the ankle cartilage is generally thinner and sees greater stress than these other joints, the tensile properties of talar cartilage degrade more slowly over time during aging [3, 4]. Due to these physiologic differences, the development of primary ankle arthritis is fairly uncommon, less than 10% in several longitudinal studies. These cohorts demonstrated 70% or greater of patients presenting with clinical ankle arthritis were secondary to trauma [5, 6]. Within this post-traumatic subset, the most common etiology was rotational malleolar fractures, followed by chronic ankle instability, pilon/tibial shaft/talar fractures, and osteochondral lesions. Despite variable mechanisms of trauma between fracture and instability, there are similar kinematic changes with loss of plantar/dorsiflexion of the tibiotalar joint but also restrictions in surrounding midfoot mobility [7].
End-stage ankle arthritis has been shown to compromise quality of life much like other lower extremity arthritis, and many patients will fail conservative measures. Due to the relationship with trauma, there is also a need to have durable management for younger patients that have developed this debilitating condition. While the use of ankle arthroplasty is gradually increasing, and outcomes are improving, ankle arthrodesis is still the gold standard for end-stage ankle arthritis [8].
Ankle arthrodesis offers a durable answer for the painful arthritic ankle, while allowing for correction of deformity and instability. Like all surgical options, there are known complications associated with this procedure, even when successful fusion occurs. The most problematic outcome of ankle arthrodesis is the alteration in gait mechanics. The fused ankle often demonstrates a shorter stride length, with increased motion of the nearby subtalar and talonavicular articulations [9]. This is felt to be related to the high incidence of adjacent joint arthritis, with some studies identifying up to 100% prevalence of subtalar arthrosis at 10 years post-ankle arthrodesis [10]. Nonetheless, ankle arthrodesis remains an important tool in the armamentarium of the orthopaedic foot and ankle surgeon or traumatologist in the setting of post-traumatic arthritis.
2 Post-traumatic Biochemical Environment
Due to its unique relationship with trauma, the biochemical profile of the arthritic ankle has received research attention. From a composition standpoint, the ankle demonstrates a higher percentage sulfated glycosaminoglycans (GAGs) with a lower water content than the knee, despite a similar collagen content [11]. This leads to a stiffer, more compression-resistant cartilage at the ankle. Baseline levels of protein and proteoglycan synthesis are higher in the ankle as well, suggesting a higher metabolic activity in this joint, which seems to be related to the extracellular environment rather than differences in cell programming. Additionally, the ankle cartilage is more resistant to catabolism in the presence of pro-inflammatory IL-1 [11].
The biochemical environment surrounding intra-articular fracture has also been the focus of investigation. Synovial fluid studies have been performed at the time of fracture demonstrating significant increases in pro-inflammatory markers including TNF-α, IFN-γ, multiple interleukins and matrix metalloproteinases, and hemarthrosis markers in comparison to the uninjured ankle [12]. The same group was able to perform a 6 month follow-up on several of these patients at the time of syndesmotic screw removal, with repeat analysis of injured and control ankle synovial fluid. The authors demonstrated continued elevation of inflammatory markers, even in the setting of complete bone healing [13]. Similar findings occurred when examining the synovium of fractures histologically, suggesting that the tissue of the ankle is also altered and may play a role in the degenerative environment postfracture [14]. These inflammatory changes have not been found to correlate to fracture treatment or quality of reduction, so are likely the natural history of the injury itself rather than a sequela of altered mechanics [15].
Overall, the basic science aspect of post-traumatic arthritis is a growing field and potential target for therapeutics in the future. While fracture reduction and treatment is key for the surgeon, management of the biological milieu within the joint may play an important role in mitigating cartilage damage in the future.
3 Preoperative Evaluation and Surgical Indications
Prior to indicating a patient for ankle arthrodesis, a thorough history and physical examination should be performed. Patient history should include prior fracture or instability events, medical history of inflammatory or other arthropathies, prior surgeries to the ankle, and any pain or dysfunction of other joints, including other joints in the foot, the knee/hip, or upper extremities, that may affect the patient’s ability to rehabilitate postoperatively or accommodate the change in biomechanics. Other important aspects of social history include use of cigarettes or other nicotine sources, drug usage, and functional requirements/expectations, both recreational and vocational. A history of prior attempts at conservative management can also be beneficial. Recent studies have found a relative risk of nonunion of 5.8 in active smokers, so discussions about nicotine cessation are an important consideration, as these risks decline to normal in ex-smokers [16].
Physical examination should include the foot and continue upwards. Alignment of the foot itself, deformity at the hindfoot and ankle, and the entire limb alignment are important to evaluate. The skin should be evaluated for prior incisions, including prior soft tissue flap coverage. Vascular exam should be performed, and doppler pulse exam is necessary if pulses are not palpable. Neurologic exam can include Semmes-Weinstein monofilament testing if there is any concern for neuropathy, which may be present in a traumatized foot. Ankle stability and range of motion are important in surgical planning and patient expectations. Manually stabilizing the ankle demonstrating residual motion through the foot can be helpful for patients to understand the biomechanical changes of the arthrodesis and also help alleviate some of the anxiety associated with the term “fusion.” Additionally, special attention on assessment of subtalar motion is critical, as limitations of subtalar mobility can significantly compromise gait mechanics and clinical outcomes. Ability to correct any deformity at the ankle should be evaluated, as well as any compensatory deformity at the foot from longstanding ankle malalignment.
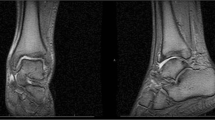
Radiographic evaluation should consist, at a minimum, of weightbearing X-rays of the foot and ankle. Hindfoot alignment films and calibrated full length standing films can be helpful when assessing deformity and associated limb length discrepancy. Computed tomography (CT) scans can be helpful to assess bone quality, bone loss, and surrounding joint arthrosis. With the increasing availability of weightbearing CT (WBCT) in many practices, there is growing evidence that this modality provides increased information on hindfoot alignment, as well as compensatory deformity, that could be beneficial to the surgeon in operative planning [17, 18]. Magnetic resonance imaging (MRI) plays less of a role in routine workup of ankle arthritis but may be beneficial in select settings, such as evaluating for osteochondral lesions, or avascular necrosis (AVN) of the talus which may increase nonunion risk.
Based on the data obtained from the surgeon’s evaluation, one can then synthesize an appropriate reconstructive plan for the patient. Once the plan for arthrodesis has been confirmed, there are multiple approaches and techniques the surgeon should be aware of to tailor to the specific patient presentation.
4 Surgical Techniques
Regardless of technique, the standard surgical principles of arthrodesis apply. There should be respect of the soft tissues and blood supply, as well as neurologic structures. Joint preparation is paramount, and all cartilage should be removed with feathering and/ or drilling of the subchondral surface of both the tibia and talus to access healthy bleeding bone. Alignment of the hindfoot should be performed with the ankle in neutral dorsiflexion/plantarflexion, five degrees of valgus, similar or slight external rotation to contralateral foot, and centralizing or slight posterior shift of the talus under the tibia to maximize biomechanical function. To achieve these goals, there are multiple approaches, which can be selected based on surgeon experience and patient presentation.
4.1 Open (and Mini-Open)
Open preparation of the joint is the gold standard procedure. Direct visualization of the joint for debridement and removal of cartilage, removal of prior implants, application of biologics if indicated, and fixation can be performed through various approaches. Each approach is associated with its own risks and benefits. Overall, open ankle arthrodesis has a fusion rate reported in the 90–95% across multiple approaches [19, 20].
4.1.1 Anterior
This has become a workhorse approach for many surgeons. It has benefit of excellent visualization of the entire ankle joint, allows correction of deformity, and supplemental plate fixation can be directly applied through this approach. Anterior plate fixation in addition to crossed screws has demonstrated improvement in rigidity of the fixation construct, and many manufacturers have begun developing arthrodesis specific instrumentation for this approach [21,22,23]. Usage of an anterior plate has been shown to lead to an increased fusion rate and decreased complication rate in open arthrodesis [19]. Additionally, the same approach can be used for pilon fracture reduction or ankle joint debridement in earlier arthrosis. This approach can be reused for later conversion to arthroplasty if indicated. The anterior approach is also extensile distally if further work such as talonavicular or naviculocuneiform work is planned for hindfoot and/or midfoot stabilization.
Complications associated with this approach are usually soft tissue related. In nearly all cases, the superficial peroneal nerve and its branches will cross the incision. These must be managed carefully to prevent nerve pain or sensory loss, particularly in revision cases. More catastrophic is wound breakdown. There is a limited soft tissue envelope in this region. The tissue experiences significant tension during sagittal plane motion and has the risk of incisional breakdown due to bowstringing of the tibialis anterior and/or extensor hallucis longus tendons. Contraindications to the approach are prior trauma and incisions, prior flap reconstruction, other indications for fibular excision/osteotomy (osteomyelitis/deformity), or the need to access posterior implants.
This technique continues to evolve with surgeon understanding, technique, and implant design. As pre-contoured plates have become more common, so have lower-profile implants with greater rigidity. In uncomplicated cases, this allows for smaller “mini-open” approaches. Studies have demonstrated good access for joint preparation with these smaller incisions, with the benefit of decreased wound size for healing [24, 25]. Early anterior plating techniques included manual contouring of reconstruction plates, often with nonlocking fixation [21]. This progressed to pre-contoured locking plates, which were often thick and placed the at-risk anterior soft tissue envelope under further tension. Newer implants are smaller, using locking technology and larger screws (often 4.5 mm) to increase stability with a smaller footprint (Fig. 1). When placing an anterior plate, the risk of impingement on the talonavicular joint should be noted on lateral fluoroscopy.
Mini-open techniques are attempts at a less invasive modification of open techniques, and are anterior-based. These can include either a single small anterior approach or multiple smaller incisions [25]. The benefit being that smaller incisions disrupt less blood supply and reduce soft tissue complications. Joint preparation techniques often include burrs in addition to the usual curettes/elevators/osteotomes to help denude cartilage and subchondral bone with less direct visualization. Fixation usually includes cannulated compression screws alone.
4.1.1.1 Authors’ Technique: Tips and Tricks
The anterior approach is our workhorse approach for ankle arthrodesis. The authors prefer to perform the retinacular incision just lateral to the EHL tendon during the approach to maintain the sheath of the tibialis anterior and increase likelihood of a durable repair during closure. The deep approach remains the same, between the TA and EHL tendons, with care to protect the neurovascular bundle. One or two small crossing vessels often delineate the deep approach; these can be coagulated to mobilize the bundle. The retinacular layer should be repaired meticulously during closure with interrupted sutures.
Once the joint capsule is encountered, it is incised, and some tissue redundancy or synovitis can be excised. Anterior osteophytes and loose bodies are excised for visualization. A Gelpi retractor works well for tissue retraction while protecting neurovascular structures. Restoration of alignment may require preferential bone removal from medial or lateral joint. Lamina spreaders of pin distractors can be used to better access the joint surfaces. Curved curettes are helpful in the posterior joint for preparation.
After joint preparation and deformity correction, guide wires for compression screws are placed percutaneously, both medial and lateral, to stabilize the ankle. Additional screws can be place anterior-posterior or posterior-anterior (“home run”) as indicated by deformity and bone quality. The wires are drilled and replaced by screws one at a time, to avoid losing fixation during the fixation process. We strive to obtain cannulated screw fixation and compression in the mid-talar body region, both medial and lateral to midline (Fig. 1). If bone quality is poor, or the bone blows out laterally, transfibular fixation is an option as well. We prefer headless compression screws to avoid implant prominence. The anterior plate will help obtain central compression and stability. Depending on anterior tibial anatomy, an osteotome, or burr may be required to smooth out distal tibial prominence and allow for the plate to seat flush. This also helps reduce anterior soft tissue tension and the chance of talonavicular impingement.
4.1.2 Lateral
The lateral, or transfibular, approach to ankle arthrodesis was initially popularized by Mann [26]. He described an ankle fusion technique that uses a transfibular approach that affords good visualization, avoidance of nerve complications, and rigid fixation without the need for additional bone graft. While an effective technique, there are downfalls to sacrificing the fibula. An intact fibula provides another surface for bony union, a strut against valgus tilt in delayed/nonunion, and importantly, the ability to convert to ankle arthroplasty in the future. Some attempts at modifying the lateral approach have also been used with good success, with attempts to preserve the fibula using this approach [27]. Additionally, it can be challenging to prepare the medial aspect of the joint without a second incision [24].
The early approach described by Mann was a fibular sacrificing approach. This involved a sizeable incision of 15–20 cm along the fibula and aiming distally in the internervous plane between superficial peroneal and sural nerves. Full thickness flaps are developed, and the fibula excised for visualization of the tibiotalar joint. The fibula is osteotomized 3–4 cm proximal to the joint and beveled lateral-medial to avoid soft tissue irritation. This was combined with a 4 cm anteromedial approach to access this portion of the joint. He prepared the joints with flat cuts of the tibia and talus and transfixed the joint with two or three 6.5 mm screws from the lateral talus to the medial tibia for compression. Of note, much like the anterior approach, lateral plate supplementation has also become more common over time. This lateral fibular sacrificing approach is also useful in TTC preparation, as is gives access to both the tibiotalar and subtalar joints, and allows plate fixation across both joints in conjunction with, or substitution for, a TTC nail.
An alternate fibular sparing technique is also available. A similar initial approach is used, but the fibula is left on a posterior soft tissue hinge to maintain vascularity. After ankle or TTC arthrodesis, the inner surface of the fibula can be prepared with a sagittal flat cut, or standard arthrodesis preparation, and fixed back against the tibia at the syndesmosis, and against the talus as well. The lateral aspect of the tibia and talus should be prepared as well. This ideally provides another bony surface for union and maintains a lateral strut which allows later takedown conversion to ankle arthroplasty if indicated. Standard screw placement can still be used, or compression screws from the lateral-medial trajectory afforded by the surgical approach are acceptable. The fibula is fixed with transverse screws (Fig. 2). This can be combined with a mini-open anterior approach if needed for joint preparation, and there has been case series including a combined lateral and anterior approach with plating for TTC arthrodesis [28].
Lateral approach radiographs and preparation. (a, b) Mortise preoperative and postoperative films. (c) Intra-operative photo of fibular osteotomy (proximal to right). (d) Sagittal cut to prepare internal (medial) surface of fibula. (e) Intra-operative view of lateral talus/tibiotalar joint with fibula retracted posteriorly
Wound healing is a risk factor, due to the less vascularized nature of the lateral tissues. Additionally, care must be taken to avoid aggressive soft tissue dissection over the talar neck, which may damage the tenuous blood supply to this bone. Peroneal tendons must be identified and protected to maintain function of the subtalar joint as well.
The lateral approach maintains a useful place in the surgeon’s toolbox. In the authors’ experience, it is more commonly used as a salvage approach at this time, when soft tissue or deformity are limiting factors preventing the anterior approach. In general, outcomes are similar to use of an anterior approach, therefore selection of the correct method falls on the surgeon and the patient presentation [29]. It benefits from avoiding the tenuous anterior skin in the setting of prior trauma, flap coverage, or other soft tissue concerns. This often allows usage of a prior incision in the setting of post-traumatic arthritis, as prior fibular fracture fixation is common in this cohort. Removal of the fibula decompresses the lateral ankle and often aids in a tension free closure, which can be beneficial in soft tissue compromise or severe deformity. There is greater access to the distal tibia and talar body if bony resection/shortening must be performed for deformity correction. Additionally, the ability to fully access the talar body can be helpful if bulk allograft such as femoral head is needed due to talar collapse or bone loss.
4.1.3 Posterior
A third approach that the surgeon should be aware of is posterior. This can be direct posterior, or through a previously used posterolateral or posteromedial incision that was used in prior fracture fixation. While this approach is less commonly used that the traditional anterior or lateral approaches, it has several valuable indications. As mentioned, if there is failure of posterior implants from prior trauma, this approach can be used to remove these and perform the arthrodesis simultaneously (Fig. 3). In the setting of prior soft tissue reconstruction, or threatened anterior/lateral soft tissue, the posterior approach provides an option with robust soft tissue coverage distant to prior incisions or tissue flaps. Third, the approach can be used to perform a simultaneous tibiotalar and subtalar fusion, while preserving the fibula, in the setting of severe hindfoot post-traumatic arthritis or in the neuropathic patient.
Patient with BMI of 50, 1 pack per day smoker referred to Foot & Ankle for salvage after failed ORIF and revision ORIF. (a, b) AP and Lateral injury films. (c, d) Intraoperative AP and lateral views. (e, f) Early failure at 6 week follow-up. (g–i) Continued loss of reduction after syndesmotic revision. (j, k) Successful fusion 3 months after posterior approach implant removal and TTC arthrodesis
There is limited literature on the isolated posterior tibiotalar arthrodesis, but the approach has been investigated thoroughly in the setting of TTC fusions. It has been described for use in severe deformity, with locked plating or intramedullary nailing. The posterior approach has been compared to the lateral approach and found to be safe and effective [30,31,32,33,34]. These patients are often positioned prone, which also adds some surgical and anesthetic challenges in longer, more complex cases.
4.2 Arthroscopic
As interest in minimally invasive techniques and instrumentation have grown, there has been increasing interest in arthroscopic ankle arthrodesis. The technique was first described in the 1980s, with increasing literature to support it. Smaller incisions and percutaneous fixation offer the benefits of decreased wound healing complications and soft tissue stripping and potentially less disruption of the blood supply to the tibia and talus. This technique can be particularly useful in patients with peripheral vascular disease or soft tissue trauma who have been optimized but remain at increased risk for wound healing complications. Barriers to the technique are the need for arthroscopic equipment and surgeon familiarity with ankle arthroscopy. It can also be more challenging to correct deformity with this approach, but deformity alone is not a contraindication to arthroscopic joint preparation. This is becoming more routine for foot and ankle trained orthopedists, but still not a common skill for traumatologists caring for their own post-traumatic patients. Additionally, no supplemental plating can be performed with this approach.
Longitudinal and comparative studies have demonstrated excellent fusions rates, generally exceeding 90% and approaching 100% in some studies with this technique [35, 36].Some comparative studies have even demonstrated higher fusion success rates with arthroscopic joint preparation compared to open techniques, with shorter time to union [35, 37]. It has also demonstrated some success in AVN of the talus, and this may be a benefit of soft tissue preservation [38]. Deformity correction can be challenging when using arthroscopic techniques. There have, however, been isolated reports of successful arthrodesis despite some larger defomities [39]. The principles of arthrodesis remain the same, and the joint must be fully denuded of all cartilage and sufficient perforation of the subchondral bone performed. Fixation is usually performed with 2–3 cannulated compression screws.
4.3 External Fixation
External fixation is not a standalone “technique,” per se, but an important adjunct to hindfoot salvage and arthrodesis. It plays a particularly important role in the post-traumatic arthritic ankle, especially in the circumstances of infection, poor soft tissue status, and significant tibial axis deformity or malalignment. It has been shown to provide good fusion rates with good maintenance of alignment as well [40]. Like previously discussed techniques, the ankle joint must be prepared (open or arthroscopically) for arthrodesis prior to application of the external ring fixator. Definitive fusion with external fixation is generally performed with a thin wire ring fixator, which provides the greatest stability and options for deformity correction and compression.
Fusion via external fixation provides an excellent salvage opportunity, and the technique fits particularly well with the challenges of the post-traumatic ankle. The simplest of uses can be in a patient with poor soft tissues. By minimizing incisions for implant placement, the soft tissue envelope can be preserved. Additionally, a fixator with adjustable struts can be used in the setting of severe post-traumatic deformity with skin contracture to gradually correct the deformity prior to final arthrodesis, limiting soft tissue complications with acute correction [42,43,44]. This can be performed entirely with the ring fixator, or a transition to internal fixation after deformity correction, to limit time in the frame. Another valuable, and likely most common, case for ring fixation is the setting of infection. An example may be a pilon fracture that has become infected and failed internal fixation. In such a case, the implants could be removed, the joint prepared for arthrodesis, and the fixator used to stabilize the fusion site, and soft tissues, primarily while avoiding local instrumentation and allowing antibiotic treatment. These principles carry over from the Charcot literature, demonstrating the benefits of external versus internal fixation in the setting of active infection [45, 46].
Ring fixation is also helpful in the most complex of cases. This is an excellent salvage option in the setting of significant bone loss, or in the need for extensive bony resection for clearance of osteomyelitis [47]. Use of external fixation can allow for simultaneous bony resection and fracture site debridement, excision of necrotic bone, shortening of the tibiotalar region if necessary for soft tissue coverage, and proximal bone transport to salvage the functional length of the limb. While increasingly complex and requiring an experienced surgeon, this option provides for the salvage of a post-traumatic limb in a setting where below-knee amputation may be the only other valid option. Additionally, a fixator can be used to stabilize bone and soft tissue in the setting of multiple debridements or soft tissue reconstruction by the plastic surgery team (Fig. 4).
Reconstruction of infected malunion with bone transport. (a) Clinical photo of alignment. (b, c) AP and lateral views of malunion. (d) Limb length view demonstrating loss of length and alignment. (e, f) AP and lateral in thin-wire frame with proximal osteotomy (red dotted line) and distal excision of necrotic bone and antibiotic spacer. (g, h) Successful docking and fusion with supplemental hardware distal and well-healed regenerate bone proximal
Ring fixation is a complex task, and both static and dynamic frames have risks to the patient. These devices require expertise not only for application, but for long-term management. It is common to require pin changes for infection and strut changes for dynamic frames. Patients may not tolerate the bulky device for extended periods of time, and it can lead to issues with clothing and ambulation. A severe complication is the potential for fracture through half-pin sites in the tibia [41]. Despite this, this method of fixation confers important and valuable benefits and the option for limb salvage, in select patients.
5 Special Considerations
5.1 The Varus Ankle
Every ankle fusion should involve preoperative planning and consideration of multiple patient specific factors, particularly in the post-traumatic setting. One common deformity requiring special attention is the varus arthritic ankle. Varus deformity can be intra-articular or extra-articular. It can be secondary to the trauma or due to the patient’s native anatomy. It can develop from varus malunion of the tibia and or talus, talar neck malunion, compartment syndrome sequelae, or from chronic lateral ankle instability in post-traumatic cases. Varus alignment has been identified as an independent predictor of nonunion in large studies, with greater than double the nonunion rate of a neutral preoperative alignment [20].
The subtalar joint often compensates for malalignment of the ankle, and its flexibility must be evaluated preoperatively, as well as associated foot alignment and compensatory deformity [48]. The compensatory deformities of the foot in general must also be studied during preoperative planning. A host of other foot deformities must be considered when correcting the varus ankle, depending on the associated foot alignment. Most of the concomitant surgical options are those associated with the cavovarus foot in general, including a lateral calcaneal closing wedge/slide, first metatarsal dorsiflexion, claw toe corrections, gastrocnemius recession or Achilles lengthening, plantar fascia release, peroneus longus to brevis transfer, or talonavicular arthrodesis [49, 50]. Of paramount importance is the posteromedial release of the hindfoot. In the setting of significant cavovarus deformity, the soft tissue structures must be aggressively released to allow for deformity correction. This must be patient specific but generally includes the posterior tibial and flexor digitorum longus tendon, talonavicular and subtalar joint capsule, spring and deltoid ligament, plantar fascia, and tarsal tunnel [50]. This will allow for a more balanced plantigrade foot after deformity correction and arthrodesis of the ankle. Many of these soft tissue structures also may contract subsequent to a lower extremity compartment syndrome and can be seen commonly in post-traumatic foot/ankle deformity. Providing a well-balanced foot for the patient is important to maximize function beneath an ankle arthrodesis.
5.2 Tibial Osteotomy
In the setting of extra-articular fractures, or prior fracture malreduction, the development of post-traumatic arthritis may come from malalignment rather than cartilage and joint trauma. In these unique cases, the ankle joint may be able to be salvaged, at least temporarily, with a corrective osteotomy. In response to injury, ankle cartilage has been shown to produce proteoglycans at an accelerated rate compared to other joints [11]. Therefore, the ankle may be more amenable to joint salvage techniques. At the least, appropriate realignment of the lower extremity axis can improve the outcomes of future ankle arthrodesis or fusion, as well as alignment at the hip and knee. Additionally, these procedures may occur concurrently with the ankle arthrodesis. Attempts at joint preservation with standard supramalleolar osteotomy have been shown to be successful and are worth consideration in patients that are symptomatic with milder radiographic changes and any residual malalignment [51, 52]. Additionally, osteotomies or malunion corrections at other levels along the tibial axis may be required in advance of, or simultaneous with, the planned ankle arthrodesis. These osteotomies can be either intra-articular (Fig. 5) or remote from the tibiotalar joint (Fig. 6), depending on the deformity location. Osteotomy for deformity correction can be accomplished with multiple techniques including open or percutaneous methods and can be stabilized with internal or external fixation [42, 53].
Joint sparing osteotomy for post-traumatic malunion with early arthrosis. (a) AP view demonstrating shortening and varus malalignment. (b) Proposed osteotomy site and translation. (c) AP image after osteotomy and frame placement. (d, e) Intraoperative view of osteotomy using multiple drill holes. F: Healed osteotomy with improved alignment
5.3 Tibiotalocalcaneal Arthrodesis
Tibiotalocalcaneal (TTC) arthrodesis is a technique useful for revision arthrodesis, severe trauma with concomitant tibiotalar and subtalar arthritis, or for increased stability and fixation in poor bone quality or patients with severe neuropathy. Fusion rates are less favorable than ankle arthrodesis alone, often in the 85–90% range, with complication rates approaching 30%, but this technique should be reserved for complex and salvage situations [54]. This can be performed through multiple approaches, similar to tibiotalar arthrodesis mentioned above. This should be tailored based on soft tissue considerations, prior incisions, direction of deformity and the need for removal of any implants present. In the setting of minimal deformity, a combination of standard anterior tibiotalar and separate sinus tarsi approaches is possible. A single transfibular incision can be used to address both joints simultaneously, as can the posterior approach (Achilles splitting or posterolateral/posteromedial). Fixation options include TTC nails, plate fixation, external fixation, or some hybrid of these options, as seen in Figs. 3 and 4 [28, 31].
The same techniques of arthrodesis apply, with careful soft tissue handling and respect for the blood supply, meticulous joint preparation, deformity correction, and rigid fixation. This technique can also be beneficial in the setting of talus AVN or significant bone loss, in order to salvage limb length. The classic technique is to use a femoral head allograft to replace excised bone, but this has been shown to have poor arthrodesis rates in some populations [55]. There is developing interest in custom implants to fill a post-traumatic void, with three-dimensional printing of custom mesh implants to incorporate into fusion constructs as a limb salvage option, though long term studies are lacking at this time [56, 57].
5.4 Conclusion
In summary, post-traumatic ankle arthrosis is one of the most common presentations of symptomatic arthritis in the orthopaedic surgeon’s patient population. This is a multifactorial process, with many treatment options available in the surgeon’s armamentarium, from approach to fixation techniques. The biological basis of these changes remain under investigation, but maintaining appropriate anatomic alignment is key for the surgeon. Techniques for treatment will likely continue to evolve, but arthrodesis currently remains the gold standard for management of post-traumatic tibiotalar arthritis.
References
Huch K, Kuettner KE, Dieppe P. Osteoarthritis in ankle and knee joints. Semin Arthritis Rheum. 1997;26:667–74.
Muehleman C, Bareither D, Huch K, Cole AA, Kuettner KE. Prevalence of degenerative morphological changes in the joints of the lower extremity. Osteoarthr Cartil. 1997;5:23–37.
Kempson GE. Age-related changes in the tensile properties of human articular cartilage: a comparative study between the femoral head of the hip joint and the talus of the ankle joint. Biochim Biophys Acta. 1991;1075:223–30.
Athanasiou KA, Niederauer GG, Schenck RC. Biomechanical topography of human ankle cartilage. Ann Biomed Eng. 1995;23:697–704.
Saltzman CL, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–6.
Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467:1800–6.
Deleu PA, et al. Post-sprain versus post-fracture post-traumatic ankle osteoarthritis: impact on foot and ankle kinematics and kinetics. Gait Posture. 2021;86:278–86.
Seaworth CM, et al. Epidemiology of total ankle arthroplasty: trends in New York State. Orthopedics. 2016;39:170–6.
Sturnick DR, et al. Adjacent joint kinematics after ankle arthrodesis during cadaveric gait simulation. Foot Ankle Int. 2017;38:1249–59.
Ling JS, et al. Investigating the relationship between ankle arthrodesis and adjacent-joint arthritis in the hindfoot: a systematic review. J Bone Joint Surg Am. 2015;97:513–9.
Kuettner KE, Cole AA. Cartilage degeneration in different human joints. Osteoarthr Cartil. 2005;13:93–103.
Adams SB, et al. Inflammatory cytokines and matrix metalloproteinases in the synovial fluid after intra-articular ankle fracture. Foot Ankle Int. 2015;36:1264–71.
Adams SB, et al. Inflammatory microenvironment persists after bone healing in intra-articular ankle fractures. Foot Ankle Int. 2017;38:479–84.
Furman BD, et al. Articular ankle fracture results in increased synovitis, synovial macrophage infiltration, and synovial fluid concentrations of inflammatory cytokines and chemokines. Arthritis Rheumatol. 2015;67:1234–9.
Pham TM, et al. Association of acute inflammatory cytokines, fracture malreduction, and functional outcome 12 months after intra-articular ankle fracture-a prospective cohort study of 46 patients with ankle fractures. J Orthop Surg Res. 2021;16:338.
Allport J, Ramaskandhan J, Siddique MS. Nonunion rates in hind- and midfoot arthrodesis in current, ex-, and nonsmokers. Foot Ankle Int. 2021;42:582–8.
Barg A, et al. Weightbearing computed tomography of the foot and ankle: emerging technology topical review. Foot Ankle Int. 2018;39:376–86.
Richter M, Seidl B, Zech S, Hahn S. PedCAT for 3D-imaging in standing position allows for more accurate bone position (angle) measurement than radiographs or CT. Foot Ankle Surg. 2014;20:201–7.
van den Heuvel SBM, Doorgakant A, Birnie MFN, Blundell CM, Schepers T. Open ankle arthrodesis: a systematic review of approaches and fixation methods. Foot Ankle Surg. 2021;27:339–47.
Chalayon O, et al. Factors affecting the outcomes of uncomplicated primary open ankle arthrodesis. Foot Ankle Int. 2015;36:1170–9.
Tarkin IS, et al. Anterior plate supplementation increases ankle arthrodesis construct rigidity. Foot Ankle Int. 2007;28:219–23.
Kestner CJ, Glisson RR, Nunley JA. A biomechanical analysis of two anterior ankle arthrodesis systems. Foot Ankle Int. 2013;34:1006–11.
Plaass C, Knupp M, Barg A, Hintermann B. Anterior double plating for rigid fixation of isolated tibiotalar arthrodesis. Foot Ankle Int. 2009;30:631–9.
Chinnakkannu K, et al. Mini-open vs. transfibular approach for ankle arthrodesis, which approach is superior in joint preparation: a cadaver study. Indian J Orthop. 2020;55:135–41.
Paremain GD, Miller SD, Myerson MS. Ankle arthrodesis: results after the miniarthrotomy technique. Foot Ankle Int. 1996;17:247–52.
Mann RA, Van Manen JW, Wapner K, Martin J. Ankle fusion. Clin Orthop Relat Res. 1991;(268):49–55.
Smith JT, Chiodo CP, Singh SK, Wilson MG. Open ankle arthrodesis with a fibular-sparing technique. Foot Ankle Int. 2013;34:557–62.
Ciufo DJ, Grant AM. Orthogonal locked plating for tibiotalocalcaneal arthrodesis. Tech Foot Ankle Surg. 2022;21(1):40–7. https://doi.org/10.1097/BTF.0000000000000295.
Kim JG, et al. Ankle arthrodesis: a comparison of anterior approach and transfibular approach. Clin Orthop Surg. 2018;10:368–73.
Mulligan RP, Adams SB, Easley ME, DeOrio JK, Nunley JA. Comparison of posterior approach with intramedullary nailing versus lateral transfibular approach with fixed-angle plating for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2017;38:1343–51.
Kile TA, Donnelly RE, Gehrke JC, Werner ME, Johnson KA. Tibiotalocalcaneal arthrodesis with an intramedullary device. Foot Ankle Int. 1994;15:669–73.
Nickisch F, Avilucea FR, Beals T, Saltzman C. Open posterior approach for tibiotalar arthrodesis. Foot Ankle Clin. 2011;16:103–14.
Pellegrini MJ, et al. Outcomes of tibiotalocalcaneal arthrodesis through a posterior achilles tendon-splitting approach. Foot Ankle Int. 2016;37:312–9.
Fetter NL, DeOrio JK. Posterior approach with fibular preservation for tibiotalocalcaneal arthrodesis with an intramedullary nail. Foot Ankle Int. 2012;33:746–9.
Quayle J, et al. Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg. 2018;24:137–42.
Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot Ankle Int. 2005;26:275–80.
Myerson MS, Quill G. Ankle arthrodesis: a comparison of an arthroscopic and an open method of treatment. Clin Orthop Relat Res. 1991;(268):84–95.
Kendal AR, Cooke P, Sharp R. Arthroscopic ankle fusion for avascular necrosis of the talus. Foot Ankle Int. 2015;36:591–7.
Dannawi Z, Nawabi DH, Patel A, Leong JJH, Moore DJ. Arthroscopic ankle arthrodesis: are results reproducible irrespective of pre-operative deformity? Foot Ankle Surg. 2011;17:294–9.
Morasiewicz P, et al. Radiological evaluation of ankle arthrodesis with Ilizarov fixation compared to internal fixation. Injury. 2017;48:1678–83.
Jones CP, Youngblood SA, Waldrop N, Davis WH, Pinzur MS. Tibial stress fracture secondary to half-pins in circular ring external fixation for charcot foot. Foot Ankle Int. 2014;35:572–7.
Paley D, Lamm BM, Katsenis D, Bhave A, Herzenberg JE. Treatment of malunion and nonunion at the site of an ankle fusion with the Ilizarov apparatus. J Bone Joint Surg. 2006;88:119–34.
Paley D. Principles of deformity correction. Berlin: Springer; 2002. https://doi.org/10.1007/978-3-642-59,373-4.
Paley D, Chaudray M, Pirone AM, Lentz P, Kautz D. Treatment of malunions and mal-nonunions of the femur and tibia by detailed preoperative planning and the Ilizarov techniques. Orthop Clin North Am. 1990;21:667–91.
Conway JD. Charcot salvage of the foot and ankle using external fixation. Foot Ankle Clin. 2008;13:157–73.
Lee DJ, Schaffer J, Chen T, Oh I. Internal versus external fixation of charcot midfoot deformity realignment. Orthopedics. 2016;39:e595–601.
Lovisetti G, Kirienko A, Myerson C, Vulcano E. Ankle salvage following nonunion of distal tibia fractures. Foot Ankle Int. 2018;39:1210–8.
Wang B, Saltzman CL, Chalayon O, Barg A. Does the subtalar joint compensate for ankle malalignment in end-stage ankle arthritis? Clin Orthop Relat Res. 2015;473:318–25.
AlSayel F, Valderrabano V. Arthrodesis of a varus ankle. Foot Ankle Clin. 2019;24:265–80.
Fortin P, Guettler J, Manoli AR, Oak MI. Idiopathic cavovarus and lateral ankle instability: recognition and treatment implications relating to ankle arthritis. Foot Ankle Int. 2002.
Krähenbühl N, Susdorf R, Barg A, Hintermann B. Supramalleolar osteotomy in post-traumatic valgus ankle osteoarthritis. Int Orthop. 2020;44:535–43.
Choi JY, Kim KW, Suh JS. Low tibial valgization osteotomy for more severe varus ankle arthritis. Foot Ankle Int. 2020;41:1122–32.
Goodier WD, Calder PR. External fixation for the correction of adult post-traumatic deformities. Injury. 2019;50:S36–44.
Hegeman E, Dowd TC, Huh J. Outcomes following intramedullary nail vs plate fixation for tibiotalocalcaneal arthrodesis: a systematic review. Foot Ankle Orthop. 2022;7:2473011421S00230.
Jeng CL, Campbell JT, Tang EY, Cerrato RA, Myerson MS. Tibiotalocalcaneal arthrodesis with bulk femoral head allograft for salvage of large defects in the ankle. Foot Ankle Int. 2013;34:1256–66.
Heidari KS, Lalli T. Case report: tibiotalocalcaneal arthrodesis utilizing a titanium mesh implant for limb salvage after failed charcot reconstruction. Foot Ankle Orthop. 2022;7:2473011421S00231.
Steele JR, et al. Comparison of 3D printed spherical implants versus femoral head allografts for tibiotalocalcaneal arthrodesis. J Foot Ankle Surg. 2020;59:1167–70.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ciufo, D.J., Fortin, P.T. (2023). Post-traumatic Ankle Arthritis: Fusions. In: Herscovici Jr., D., Anglen, J.O., Early, J.S. (eds) Evaluation and Surgical Management of the Ankle. Springer, Cham. https://doi.org/10.1007/978-3-031-33537-2_21
Download citation
DOI: https://doi.org/10.1007/978-3-031-33537-2_21
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33536-5
Online ISBN: 978-3-031-33537-2
eBook Packages: MedicineMedicine (R0)