Abstract
Background
Arthrodesis is considered the gold standard for end-stage ankle arthritis in patients who fail conservative management. Achieving union is paramount while minimizing complications. An essential item for successful union is preparation of the articular surface. Our study aims to evaluate the difference in joint preparation between direct lateral and dual mini-open approaches.
Materials and Methods
Ten below knee fresh-frozen specimens were used for this study. Five were prepared through lateral approach, and five using dual mini-incisions. After preparation, all ankles were dissected and images of tibial plafond and talar articular surfaces were taken. Surface areas of articulating facets and unprepared cartilage of talus, distal tibia, and distal fibula were measured and analyzed.
Results
A greater amount of total surface area was prepared with the mini-open approach in comparison to the transfibular approach. Percentage of prepared surface area of total articulating surface (including talus and tibia/fibula), talus, tibia, and fibula with the transfibular approach were 76.9%, 77.7%, and 75%, respectively. Percentages were 90.9%, 92.9%, and 88.6% with the mini-open approach. When excluding medial gutter, there was no significant difference between techniques (83.94% vs. 90.85%, p = 0.1412).
Conclusion
Joint preparation with the mini-open approach is equally efficacious as the transfibular approach for the tibiotalar joint. The mini-open approach does provide superior preparation of the medial gutter and inferior tibial surface which may help to increase union rates and decreased complications.
Level of Evidence
V.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle arthrodesis is a common procedure that can be indicated for symptoms such as pain, instability, or deformity. These issues commonly arise from conditions including but not limited to malunion, nonunion, arthritic pain, failed total ankle arthroplasty, posttraumatic injury, osteoarthritis, rheumatoid arthritis, congenital anomalies, and neurotraumatic injury [1,2,3,4]. Outcomes are dependent upon successful union, which may be impacted by a multitude of patient-related factors including comorbidities, smoking status, and surgical technique.
Many approaches for open ankle arthrodesis have been described in the literature, including the transfibular, anterior, and mini-open techniques [5, 6]. Choice of technique is largely dependent upon the type of injury as well as preference and training of each surgeon but may also be dictated by existing hardware or prior incisions [2]. Additionally, the use of the mini-open technique is limited in patients with severe deformity [6]. The transfibular (lateral) approach utilizes a 10–12 cm incision over the distal fibula, followed by removal of approximately the distal 6 cm of the fibula [2, 4]. This approach is designed to advance between the peroneal nerve anteriorly and sural nerve posteriorly, and care must, therefore, be taken to avoid these structures [2].
Despite their efficacy, open approaches have been previously associated with wound complications and difficulty in conversion to arthroplasty if the distal fibula is excised. To address these pitfalls, the mini-open (extended arthroscopic portals) approach was introduced. In this technique, two incisions of approximately two centimeters each are made in the medial and lateral gutters of the ankle joint, which are subsequently used to visualize and access the articular surfaces. The fibula is preserved in this approach aside from denudation of the medial portion of the lateral malleolus for joint preparation [4, 7, 8]
Appropriate joint preparation is a key component to successful ankle arthrodesis regardless of surgical technique. Inadequate denudation of articular surfaces involved in the arthrodesis can lead to increased nonunion rates in ankle arthrodesis [3]. Proper preparation of the arthrodesis site includes removing articular cartilage so that underlying cancellous bone can be maximally exposed [4].
Both the transfibular and mini-open approach serve the same primary purpose of facilitating ankle arthrodesis. The goal of this study was to compare how much cartilage denudation and joint preparation could be accomplished using the mini-open approach versus the transfibular approach in fusion of the tibiotalar joint.
Materials and Methods
We used ten below knee fresh-frozen cadaver legs for this cadaveric study. All were stored at −20 °C and thawed at room temperature for 24 h prior to use. Demographic variables for the corresponding deceased patients were recorded, including age, gender, height, and weight (Table 1).
Each specimen was arbitrarily assigned to undergo either the transfibular approach or mini-open approach with dual incisions for the ankle. Ankle joints of five specimens were prepared through the transfibular approach, while the remaining five ankles were prepared using dual mini-incisions.
For the transfibular approach, a skin incision was made over the fibula shaft starting 10 cm proximal to the tip, and then curving distally towards the base of the fourth metatarsal. Full thickness skin flaps were developed in the plane. Detailed preparation of the bony surface of the fibula, including denudating the cartilage and removing soft tissue, was conducted. The dissection was carried across the anterior aspect of the tibia and ankle joint with the help of a periosteal elevator, by stripping soft tissue from the distal end of the tibia, ankle joint, and proximal talar neck medially towards the medial malleolus. The fibula was subsequently osteotomized with beveling approximately 1–2 cm proximal to the level of the ankle joint (Fig. 1). The anterior tibiofibular ligament (AITFL) and anterior talofibular ligament (ATFL) were released and the distal fibula fragment was flipped or retracted posteriorly utilizing the intact calcaneofibular ligament (CFL) as a soft tissue hinge. The joint surface was distracted with a lamina spreader and prepared using osteotomes and curettes.
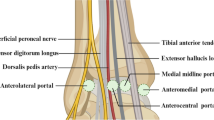
The mini-open approach was executed beginning with two incisions made over standard arthroscopic portal sites centering over the ankle. Each incision measured approximately 2 cm in length. The medial incision was placed immediately medial to the anterior tibial tendon and lateral to the medial notch. The lateral incision was made between the peroneus tertius and fibula (Fig. 2). After careful blunt dissection, the joint capsule was incised longitudinally through both incisions. Soft tissues were elevated subperiosteally from the anterior tibia through both incisions. Osteophytes were removed if present. Joint surfaces were distracted through one incision while working through the other incision. Joint surfaces were denuded with osteotomes and curettes. Joint preparation was completed and checked by a fellowship-trained foot and ankle surgeon.
After articular preparation was complete, all ankles were completely dissected, and unprepared surfaces were demarcated with a marking pen. Photographic images of the tibial plafond and talar articular surfaces were taken (Fig. 3).
Measurement and Statistical Analysis
Surface areas of each articular facet and unprepared cartilage of the talus, distal tibia, and distal fibula were measured using image-analysis software, ImageJ (Wayne Rasband, National Institutes of Health, Bethesda, MD) [9,10,11]. These measurements were used to calculate percentages of prepared and unprepared cartilage of each articular surface for each specimen. Statistical comparisons were performed using SPSS software.
Results
Table 1 shows characteristics of cadaver specimens used. Ten below-knee fresh-frozen cadaver specimens were used for this study, including three females and seven males. The average age at death was 62.4 (± 15.5) years, average height was 68.9 (± 6.5) in., and average weight was 177.4 (± 51.5) lbs.
The tibiotalar articular surface (inferior surface of tibia plus dome of talus) was more prepared using the mini-open approach (p = 0.0146). When assessing the inferior tibial and talar dome surfaces individually, the inferior tibial surface had a higher percent of preparation using the mini-open approach (Fig. 4). There was no significant difference in the amount of preparation of the lateral gutter (lateral malleolus of fibula plus lateral facet of talus) using either approach; however, the lateral malleolus was significantly more prepared using the transfibular approach (92.9%) than the mini-open approach (79.1%) (p = 0.0419) (Fig. 5).
Total prepared surface area was analyzed by ankle gutter (Table 2). The medial gutter (medial malleolus of tibia plus medial facet of talus) was significantly more denuded of cartilage in the mini-open approach (91.1%) compared to the transfibular approach (44.7%) (p = 0.0087). Of the surfaces in the medial gutter, the medial facet of the talus was significantly more prepared using the mini-open approach (100%) in comparison to the transfibular approach (31.2%) (p = 0.0006). No significant difference was found between the two approaches for the medial malleolus (p = 0.1156) (Table 3). However, the mini-open approach did allow for greater preparation of the inferior tibia (articular surface of the talar dome) as compared to the transfibular approach (94.2% vs. 76.4%, p = 0.0141).
When comparing total surface area of the ankle joint excluding the lateral gutter (Table 2), the mini-open approach provided greater average percent preparation (94.2%) compared to the transfibular approach (72.4%) (p = 0.0021). When excluding the medial gutter from analysis, neither approach provided significantly more preparation. Overall, a higher percentage of surface area of the talus, tibia/fibula, and entire ankle joint (articular surfaces of talus, tibia, and fibula combined) was prepared using the mini-open approach compared to the transfibular approach (Table 4).
Discussion
Ankle arthrodesis has been considered a gold-standard procedure for end-stage ankle arthritis in patients who fail conservative management. It may be performed through direct anterior, transfibular, arthroscopic, or mini-open approaches. Regardless of approach, important aspects of fusion are joint preparation, apposition of the joint surfaces, and stable fixation. Although total ankle replacement has increased in popularity for treatment of end-stage arthritis among older patients, ankle arthrodesis is commonly performed among younger patients, as well as patients with significant comorbidities. Arthrodesis may be associated with complications such as infection, chronic pain, and nonunion. Of these, nonunion is the most common complication reported in the literature [12]. Therefore, achieving union while minimizing complications associated with the procedure is of utmost importance.
The transfibular approach allows for excellent deformity correction, visualization of the joint, and has a smaller learning curve when compared to the mini-open approach [13]. These benefits come at the risk of possible blood supply compromise during this approach [6, 13]. Reproducible results can be achieved with the mini-open approach, in patients with lesser deformity, while preserving the soft tissue envelope and blood supply especially in settings where arthroscopic ankle fusion cannot be performed [14].
Although arthroscopic ankle arthrodesis overcomes many disadvantages of open ankle arthrodesis, there is a challenging learning curve and a high level of expertise is required. Additionally, arthroscopic ankle procedures may lead to longer surgical times [15]. It can also only be used if there is minimal deformity [16]. The mini-open anterior (extended arthroscopic portal) approach retains much of the advantages of arthroscopic arthrodesis using the same planes with minimally-increased exposure. Nonetheless, the less invasive nature of the approach has been proposed to theoretically prevent adequate preparation of the joint.
This anatomic study demonstrated that use of the mini-open approach resulted in significantly greater preparation of the tibiotalar articular surface as well as the medial gutter. Additionally, when excluding the lateral gutter, the mini-open approach performed equally or superiorly to the transfibular approach while preparing the remaining surface areas of the ankle joint. These results support the use of the mini-open approach as an equally efficacious approach in comparison to the commonly used transfibular approach. Clinically, the anterior mini-open approach is advantageous in that it optimizes surgical exposure, and the patient can be in the supine position. This preserves the mortise on both sides. It is important to note that this approach does involve dissection through the neurovascular plane, increased wound complication rates, and there is a high level of unfamiliarity with the approach amongst general orthopedic surgeons. Nonetheless, the mini-open approach preserves the fibula, providing the option to perform conversion into arthroplasty in the future if necessary. Paremain et al. [14] and Ahmad et al. [17] reported 100% union using the mini-open technique. In the study by Paremain et al. the mean time to union was 6 weeks (3–15 weeks) [14] and Ahmad et al. reported a mean time of 14.1 weeks (10–16 weeks) to union [17]. This high rate of union may be attributed to the increased amount of prepared surface area which was available for union. However, further clinical studies are needed for validation.
The transfibular approach demonstrated significantly greater efficacy for preparation of the lateral malleolus of the lateral ankle gutter in comparison to the mini-open approach. This technique has the advantages of being used for ankle fractures, avoiding neurovascular structures, and helping to correct deformities with fibular sparing. The transfibular approach for ankle arthrodesis using the fibula as an onlay graft is associated with high union rates [18,19,20,21], with a mean time to union reported to be 14 weeks in the literature [22]. One disadvantage of this approach is that it may lead to inadequate preparation of the medial gutter, which was demonstrated in our study with an average of only 44.7% preparation. Additionally, the transfibular approach using fibular osteotomy may result in compromise of venous and nervous structures [23]. The transfibular approach also entails sacrifice of the integrity of the distal fibula. In cases in which conversion, total ankle arthroplasty may be warranted, preservation of the distal fibula is critical [24, 25].
In our study, there was a significant difference in the amount of area prepared, especially on the medial malleolus, lateral malleolus, and inferior surface of the tibia. While the medial malleolus and tibia had a greater percentage of preparation with the mini-open approach, the lateral malleolus was better prepared with the lateral approach. Overall, our results demonstrated that the mini-open approach has efficacy comparable to that of the transfibular approach. Clinically, this is important, because preparation of more surface area may result in faster union rates. The mini-open approach may be advantageous in comparison to the arthroscopic approach as well, as there is less technical skill required and, therefore, less of a learning curve.
The results of our study demonstrated that the medial gutter was poorly prepared in the transfibular approach as compared to mini-open technique. Therefore, to overcome this, a medial/anteromedial incision may be required for the preparation of the medial gutter when using the transfibular approach. Some literature reports use of a medial osteotomy to approach the medial side of the joint [26]. When excluding the medial gutter, there was no significant difference in preparation between the two techniques. However, it should be noted that many surgeons excise the medial malleolus or will not prepare the medial gutter. When assessing overall preparation, specimens that underwent dissection with the mini-open approach had significantly greater preparation including a greater amount of preparation of the articular surface for the talar dome. Our results validate the mini-open approach as an efficacious approach comparable to that of the transfibular approach for ankle arthrodesis.
Limitations
This study has several limitations. First, the cadaver specimens available were limited to ten, restricting the power of the study and none of the specimens used had a deformity or arthritis of the joint. Also, freezing and thawing of the specimens could have affected the results by limiting the exposure depending on thawing. We are not able to comment on the impact of preparation on non-union due to the nature of study. Actual results in living persons depend on multiple factors including comorbidities and smoking status apart from surgical techniques. The type of fixation may also have an impact on union. However, both of these techniques typically use cross compression screws (3–5 screws depending on the surgeon’s preference). It should be noted that the transfibular approach does need additional screws to fix the fibula to the tibia and talus. Although both these techniques use compression screws only the transfibular technique provides an additional onlny graft.
This is the first study which demonstrates the efficacy of joint preparation with the mini-open approach in comparison to the transfibular approach. The mini-open approach may, therefore, provide equivalent if not superior clinical outcomes in that it allows for adequate joint preparation, preserves vascularity, minimizes soft tissue damage, and enables possible future total ankle arthroplasty.
Conclusion
The mini-open approach using dual incisions results in overall equal if not superior joint preparation when compared to the transfibular approach. There was no significant difference in tibiotalar articular surface area preparation when excluding the medial gutter. Both of these techniques provide adequate joint preparation. Therefore, the mini-open technique can be considered in patients with high risk for complications and when arthroscopic surgery is not possible. The impact of these results needs to be evaluated with further clinical studies.
Brief Summary
-
Arthrodesis is considered the gold standard for end-stage ankle arthritis in patients who fail conservative management. It may be done through anterior, lateral, arthroscopic, or mini-open approach.
-
Despite their efficacy, open approaches have been previously associated with wound complications and difficulty in conversion to arthroplasty if the distal fibula is excised.
-
Nonunion is the most common complication reported. An essential item for successful union is preparation of the articular surface which may be limited by the approach used.
-
Joint preparation with mini-open approach is equally efficacious as transfibular approach for the tibiotalar joint. When excluding medial gutter, there was no significant difference between techniques (83.94% vs. 90.85%, p = 0.1412).
-
Percentage of prepared surface area of total articulating surface (including talus and tibia/fibula), talus, tibia, and fibula with the transfibular approach were 76.9%, 77.7%, and 75%, respectively. Percentages were 90.9%, 92.9%, and 88.6% with the mini-open approach.
-
Mini-open technique can be considered in patients with high risk for complications and when arthroscopic surgery is not possible.
References
Gharehdaghi, M., Rahimi, H., & Mousavian, A. (2014). Anterior ankle arthrodesis with molded plate: technique and outcomes. Arch Bone Joint Surg, 2(3), 203.
Nihal, A., Gellman, R. E., Embil, J. M., & Trepman, E. (2008). Ankle arthrodesis. Foot Ankle Surg, 14(1), 1.
Muscarella, V., Sadri, S., & Pusateri, J. (2012). Indications and considerations of foot and ankle arthrodesis clinics in podiatric. Med Surg, 20, 59.
Bluman, E. M., & Chiodo, C. P. (2010). Tibiotalar arthrodesis. Sem Arthro, 29(1), 1–9.
Kim, J. G., Ha, D. J., Gwak, H. C., Kim, C. W., Kim, J. H., Lee, S. J., et al. (2018). Ankle arthrodesis: A comparison of anterior approach and transfibular approach. CiOS Clin Ortho Surg, 10(3), 368–373.
Raikin, S. M. (2003). Arthrodesis of the ankle: arthroscopic, mini-open, and open techniques. Foot Ankle Clin, 8(2), 347.
Wrotslavsky, P., Giorgini, R., Japour, C., & Emmanuel, J. (2006). The mini-arthrotomy ankle arthrodesis: a review of nine cases. J Foot and Ankle Surg, 45(6), 424–430.
Peterson, K. S., Lee, M. S., & Buddecke, D. E. (2010). Arthroscopic versus open ankle arthrodesis: a retrospective cost analysis. J Am Col Foot Ankle Surg, 49(3), 242–247.
Hartig, S. M. (2013). Basic image analysis and manipulation in image. J Curr Pro Mole Biol, 102(1), 14–15.
Schindelin, J., Arganda-Carreras, I., Frise, E., Kaynig, V., Longair, M., Pietzsch, T., et al. (2012). Fiji: an open-source platform for biological-image analysis. Nature Methods, 9(7), 676–678.
Abyar, E., McKissack, H. M., Pinto, M. C., Littlefield, Z. L., Moraes, L. V., Stefani, K., et al. (2019). Subtalar fusion preparation: what are we really doing? Cadaver Study Foot Ankle Spec, 8, 1938640019846970.
Haddad, S. L., Coetzee, J. C., Estok, R., Fahrbach, K., Banel, D., & Nalysnyk, L. (2007). Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis: a systematic review of the literature. The Journal of Bone and Joint Surgery, 89(9), 1899–1905.
Hess, M. C., Abyar, E., McKissack, H. M., Strom, S., & Johnson, M. D. (2020). Applications of the transfibular approach to the hindfoot: a systematic review and description of a preferred technique. Foot Ankle Surg, 1, 60–139.
Paremain, G. D., Miller, S. D., & Myerson, M. S. (1996). Ankle arthrodesis: results after the miniarthrotomy technique. Foot Ankle Internat, 17(5), 247–252.
Chiang, C. C., Tzeng, Y. H., Jeff Lin, C. F., Wang, C. S., Lin, C. C., & Chang, M. C. (2019). Arthroscopic reduction and minimally invasive surgery in supination-external rotation ankle fractures: a comparative study with open reduction. Arthro J Arthr Surg, 35(9), 2671–2683.
Duan, X., Yang, L., & Yin, L. (2016). Arthroscopic arthrodesis for ankle arthritis without bone graft. J Ortho Surg Res, 10, 190–478.
Ahmad, J., & Raikin, S. M. (2015). Minimally invasive ankle arthrodesis in: minimally invasive. Surg Ortho, 11(1), 1–8.
Colman, A. B., & Pomeroy, G. C. (2007). Transfibular ankle arthrodesis with rigid internal fixation: an assessment of outcome. Foot Ankle Internat, 28(3), 303–307.
Monroe, M. T., Beals, T. C., & Manoli, A. (1999). Clinical outcome of arthrodesis of the ankle using rigid internal fixation with cancellous screws. Foot Ankle Internat, 20(4), 227–231.
Napiontek, M., & Jaszczak, T. (2015). Ankle arthrodesis from lateral transfibular approach: analysis of treatment results of 23 feet treated by the modified Mann’s technique European. J Ortho Surg Traumatol, 25(7), 1195–1199.
Kennedy, J. G., Hodgkins, C. W., Brodsky, A., & Bohne, W. H. (2006). Outcomes after standardized screw fixation technique of ankle arthrodesis. Clin Ortho Relat Res, 447, 112–118.
Mann, R. A., Van Manen, J. W., Wapner, K., & Martin, J. (1991). Ankle fusion. Clin Ortho Relat Res, 268, 49–55.
Rausch, S., Loracher, C., Fröber, R., Gueorguiev, B., Wagner, A., Gras, F., et al. (2014). Anatomical evaluation of different approaches for tibiotalocalcaneal arthrodesis. Foot Ankle Internat, 35(2), 163–167.
Pellegrini, M. J., Schiff, A. P., Adams, S. B., Queen, R. M., DeOrio, J. K., Nunley, J. A., et al. (2014). Conversion of tibiotalar arthrodesis to total ankle arthroplasty. Jf B Joint Surg Am, 97(24), 2004–2013.
Huntington, W. P., Davis, W. H., & Anderson, R. (2016). Total ankle arthroplasty for the treatment of symptomatic nonunion following tibiotalar fusion. Foot Ankle Spec, 9(4), 330–335.
Hendrickx, R. P. M., Stufkens, S. A. S., De Bruijn, E. E., Sierevelt, I. N., Van Dijk, C. N., & Kerkhoffs, G. M. M. J. (2011). Medium- to long-term outcome of ankle arthrodesis. Foot Ankle Internat, 32(10), 940–947.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chinnakkannu, K., McKissack, H.M., He, J.K. et al. Mini-open vs. Transfibular Approach for Ankle Arthrodesis, Which Approach is Superior in Joint Preparation: A Cadaver Study. JOIO 55 (Suppl 1), 135–141 (2021). https://doi.org/10.1007/s43465-020-00244-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-020-00244-x