Abstract
Emergency medical service (EMS) systems aim to respond to emergency calls and provide life-saving care to patients. The location of EMS resources is critical to providing this care in a timely manner, and as a result, EMS facility location problems have received a tremendous amount of attention since the 1960s, and their advancement is directly tied to a wide range of facility location problems. This chapter reviews uncertainty in facility location problems applied to EMS systems and provides an intuition for and understanding of EMS problem settings. The chapter begins by explaining EMS response processes and the goals of the early deterministic models. Next, it introduces probabilistic formulations that account for uncertainty in ambulance availability, response time, and demand. Then, it highlights directions within the field and the role of uncertainty in these problem settings. This includes EMS systems with tiered units, systems that consider resource relocation, EMS systems in developing countries, and several other areas. Lastly, it concludes by providing insights into how these models are used in practice.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Emergency medical service (EMS) systems aim to quickly respond to emergency calls and provide life-saving care to patients. The location of the responding EMS unit is critical to providing this care in a timely manner. As a result, EMS facility location problems have received a tremendous amount of attention since the 1960s, and their advancement is directly tied to a wide range of facility location problems. EMS facility location problems are similar to many other facility location problems: requests for emergency aid (EMS calls) are demand points at geographic locations that must be serviced by EMS units (ambulances, aircraft, etc.) positioned at strategically located facilities. Optimization models determine the optimal location of EMS stations and/or the optimal allocation of vehicles to a set of candidate locations to best meet this demand.
The early EMS facility location models were adapted from simple deterministic location models such as the Maximal Coverage Location Problem (MCLP) and P-Median Problem (PMP). These models provided high-level insight; however, they did not account for the inherent uncertainty of EMS systems and created a need for more advanced techniques. To address this need, probabilistic models were created specifically for EMS response. Initially, these models were simple extensions of deterministic models and addressed a single stochastic element associated with EMS response, such as uncertainty in ambulance availability, response time, or demand. Over time, improved computing power, new algorithms, and increased data availability allowed more advanced models to emerge. Today, the problem of locating EMS facilities with uncertainty is still a growing area of research, where researchers continue to refine existing models and investigate settings with new sources of uncertainty.
This chapter reviews uncertainty in facility location problems applied to EMS systems. The goal is to provide the reader with an intuition for and understanding of the EMS problem setting. This chapter does not provide formulations for the discussed models and is not a comprehensive literature review. Instead, it focuses on the main themes and approaches found in facility location research applied to EMS. The remainder of the chapter is structured as follows. Section 2 reviews the EMS response process in greater detail. Section 3 briefly presents deterministic EMS facility location models that serve as the basis for more advanced models. Section 4 introduces probabilistic formulations that account for uncertainty in ambulance availability, response time, and demand. Section 5 highlights interesting directions and applications of EMS facility location problems. Section 6 discusses common themes in the successful implementations of EMS facility location models. Lastly, Sect. 7 provides references to formal literature reviews that discuss EMS facility location problems.
2 EMS Background
2.1 The EMS Response Process
Most EMS systems emphasize the importance of timely care; however, there are two primary classifications of modern EMS systems. The scoop and run method is practiced in countries such as the United States, Canada, the United Kingdom, New Zealand, and Australia. Under this model, the EMS system seeks to quickly reach a patient, provide minimal pre-hospital care, and then deliver the patient to a care facility for further treatment (e.g., hospital emergency department). The alternative approach is the stay and stabilize method, which is practiced in countries such as Germany, France, Greece, Malta, and Austria. In these systems, fewer patients are delivered to care facilities. Although many studies have compared the outcomes and cost-effectiveness of both methods, differences in operational standards and context make it nearly impossible to determine if one approach is better than the other (Al-Shaqsi, 2010a). However, these differences may influence the way one would model the system and the response time threshold chosen. Furthermore, EMS agencies may be a public service, operated or funded by a government, or a private for-profit business. Once again, there is no clear answer to which approach is better in general; rather, this discrepancy is primarily driven by national and cultural approaches to healthcare (Narad & Gillespie, 1998). With this in mind, no two EMS systems are exactly the same, and every EMS system must adapt to differences in available resources, geographic challenges, EMS infrastructure, legal requirements, and cultural dynamics. We initially present models for an EMS system with a centralized dispatching system under the scoop and run method with a single type of ambulance. This distinction is made since these are the assumptions that many of the early EMS facility location models used. In Sect. 5, we explore settings where these assumptions are relaxed.
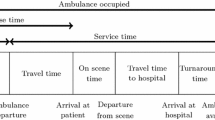
The EMS response process under the scoop and run model is as follows. (1) A medical emergency occurs and someone calls an emergency telephone line. On the phone, an EMS call taker asks the caller a series of questions to determine where the patient is located and estimate their condition. Typically, these questions are scripted by a computer system. (2) One or more EMS vehicles are dispatched to the patient’s location. In many areas, police or fire vehicles may also be dispatched to provide basic care, if they can reach the patient sooner. (3) The EMS vehicle arrives at the scene of the patient. (4) The EMS personnel treat the patient. (5) The patient is loaded into the vehicle and transported to a care facility. (6) Finally, the EMS vehicle reaches the care facility and transfers the patient. (7) After serving the patient, the EMS vehicle prepares for the next patient by returning to a station or another location. Figure 1 summarizes this process using the standard names for each time interval.
2.2 Response Time, Response Time Threshold, and Coverage
Improving patient outcomes following an emergency is the primary objective of any EMS system. Despite this simple goal, patient outcomes are difficult to quantify due to their qualitative nature. Response time is defined as the time interval between the moment an EMS vehicle is dispatched and an EMS vehicle arrives at the scene of a patient (see Fig. 1). In cardiac arrest patients, a 1-minute reduction in response time increases the odds of survival by 1–10% in a nonlinear, decaying, relationship (Stoesser et al., 2021; Holmén et al., 2020). Therefore, most EMS agencies use response time as the primary performance metric and as a proxy for outcomes since it is easy to measure and understand. Consequentially, nearly all EMS facility location problems have an objective function that evaluates response time.
The response time threshold (RTT) is a response time standard that many EMS agencies are held to. An EMS response time within the RTT is usually considered acceptable, and a response time above this threshold is usually considered to be too slow. In North America, the most widely used RTT in urban areas is 9 minutes for 90% of EMS responses (Fitch, 2005).
This standard is often traced back to several studies from the late 1970s and 1980s that concluded that a patient’s odds of survival following an out-of-hospital cardiac arrest (OHCA) decrease rapidly after this window (Mullie et al., 1989). In non-urban areas, this standard may be extended to account for longer travel distances and hard-to-reach areas. For example, the US state of California recommends that EMS agencies should respond within 20 minutes to patients in rural areas 90% of the time (Narad & Driesbock, 1999). Figure 2 presents the response time distribution by urbanicity in the United States. Globally, RTT standards vary due to the available resources, the type of EMS system used, and the national and cultural approaches to healthcare (see Table 1). In any setting, the RTT is extensively used in EMS facility location problems because it provides a simple classification for coverage. A request for EMS service that can be reached by an ambulance within the RTT is considered covered, whereas one that is beyond the RTT is not. Coverage is then implemented as a constraint or objective in EMS facility location problems.
Response time distribution by urban and rural areas in the United States (Jan-Feb 2020). The 90th percentile of response times is indicated by the dashed red line. As shown, the 90th percentile for urban and rural patients is outside the RTT standard of 9 and 20 minutes, respectively (data provided by NEMSIS)
We note that although intuitive and easy to measure, RTT coverage is a binary metric. Consider an urban system with an RTT of 9 minutes. From a modeling standpoint, a patient that is 30 seconds from a station has the same coverage as a patient that is 8:59 minutes from a station. Alternatively, if a patient is uncovered, the model does not distinguish if the patient is 9:00 minutes from a station or 30 minutes from a station. Therefore, throughout this chapter, we also highlight several approaches to encourage timely response without using the RTT. This includes minimizing average response time (Sect. 3), acknowledging the inherent uncertainty in response time (Sect. 4.3.1), and using the objective function to encourage favorable patient outcomes (Sect. 4.3.3).
3 Deterministic EMS Facility Location
3.1 Deterministic Single Coverage Models
We start by introducing deterministic models, inspired by or directly pulled from pioneering research on EMS facility location problems. We note that the term station is used loosely within this section (and throughout EMS research). A station could be any location where ambulances are positioned before being dispatched. Common locations include EMS bases, hospitals, and public parking lots.
-
The Location Set Covering Model (LSCM) positions the fewest number of stations at a set of predefined locations, such that all demand nodes are within the RTT from at least one station (Toregas et al., 1971).
-
The Maximal Coverage Location Problem (MCLP) weighs each demand node by its generated demand and then positions a limited number of stations at a set of predefined locations to maximize demand within the RTT from at least one station (Church & ReVelle, 1974).
-
The P-Median Problem (PMP) positions p stations at a set of predefined locations to minimize the average response time to all demand nodes, weighted by generated demand (Hakimi, 1964).
-
The P-Center Problem (PCP) positions p stations at a set of predefined locations to minimize the maximum response time to a demand node (Hakimi, 1965).
These models are the building blocks for the models with uncertainty and demonstrate the varying goals of an EMS system. For example, the LSCM requires RTT coverage for all demand nodes; however, the resulting solutions may not be achievable in an EMS system with limited resources. The MCLP maximizes RTT coverage using a limited number of stations; however, it ignores the response time of demand nodes located outside the RTT, which may lead to inequity in response time. The PMP minimizes the average response time and considers the effect of station location on all demand nodes. However, it may reach fewer patients within the RTT, which may lead to worse patient outcomes. Lastly, while the MCLP and PMP are inherently biased to serve areas with higher demand, the PCP minimizes the longest response time of all the demand nodes to provide near-homogeneous and more equitable service. However, the resulting solution may be an inefficient use of EMS resources.
To illustrate the importance of these modeling decisions, Fig. 3 provides a comparison of the MCLP and PMP applied to a fictional problem instance with five stations. The MCLP maximizes the demand nodes located within the RTT of a station, depicted by the gray dashed line, by locating several stations near the area with the highest density of demand to achieve a maximal coverage of 85.7%. As shown, the solution provides excellent coverage to the areas of denser demand (this may be a more populated area, like a city). Given the importance of a 9-minute response time for survival following cardiac arrest, one could argue that the MCLP is preferred since it can serve the most patients within this threshold. However, the MCLP provides poor coverage to outlier demand nodes. As shown, the 90th percentile response time is 17.7 minutes, well beyond the RTT and the threshold for resuscitation following cardiac arrest.
Alternately, the PMP minimizes the average response time of all demand nodes. While the PMP must provide quick response to areas with many demand nodes, the response times of the outlier demand nodes are also included within the objective function. The stations in the PMP solution are slightly more dispersed to attain a minimum average response time of 6.1 minutes and a 90th percentile response time of 11.0 minutes. This solution is preferable for the areas with fewer demand nodes (these may be the more rural areas). However, only 82.7% of demand points are covered within 9 minutes, which could lead to overall worse outcomes. These are the trade-offs researchers must be aware of. The formulation of an EMS facility location model must align with the objectives of the EMS system, and the researcher should communicate potential unforeseen implications of their model with practitioners.
3.2 Deterministic Multi-coverage Models
The models mentioned above assume that a station is always available to serve demand. In practice, all the vehicles at a particular station may be busy serving other patients when a request for aid is received. To hedge against this likelihood, deterministic multi-coverage models aim to increase the number of stations that can cover each demand node. This recognition of uncertainty in station availability is a precursor to the probabilistic availability models discussed in Sect. 4.1. There are two primary approaches to model multiple coverage: models that encourage multiple coverage through the objective function and models that enforce multiple coverage through constraints. Models that encourage multiple coverage reward demand nodes covered multiple times within their objective function. For example, the Hierarchical Objective Set Covering (HOSC) model is an extension of the LSCM that positions the fewest number of stations to cover each demand node once and maximizes the demand nodes covered multiple times (Daskin & Stern, 1981). Similarly, the Double Standard Model (DSM) combines the MCLP and LSCM to introduce the idea of multiple coverage radii. The model requires that a specified proportion of the demand be located within a distance \(r_1\) of a station, all demand be located within a distance \(r_2\) such that \(r_2 > r_1\), and maximizes the demand covered twice within \(r_1\) (Gendreau et al., 1997).
Models that use the second approach, enforcing multiple coverage via constraints, require a demand node to be located within the RTT from a predefined number of stations to be considered covered. This is the approach used in the Tandem Equipment Allocation Model (TEAM), a model that was initially constructed for fire systems with multiple types of vehicles (Schilling et al., 1979). Although this approach may make sense for fire systems, this method is unrealistic in EMS as covering more demand nodes with a single station is often preferable to covering just a few demand nodes with multiple stations. The Backup Coverage Problem II (BACOP II) is an MCLP-type model that combines both approaches. BACOP II rewards demand nodes that are covered by a single station with weight w and demand nodes that are covered twice with weight \((1-w)\), allowing the decision-maker to control the trade-off between single and double coverage by adjusting \(w \in [0,1]\) (Hogan & Revelle, 1986). This idea of encouraged and enforced reliability is similar to the trade-off of expected coverage models and chance-constrained models, which we discuss in Sects. 4.1.1 and 4.1.2, respectively.
4 Probabilistic EMS Facility Location
The models presented in Sect. 3 are the fundamental facility location models as applied to EMS systems. However, they rely on several unrealistic assumptions. The single coverage models assume that a station is always available to serve incoming demand within a known response time. The multi-coverage models hedge against station unavailability, but do not quantify this reliability. In this section, we present EMS facility location models that address the uncertainty in EMS systems to provide more accurate and dependable results. Section 4.1 reviews approaches to model the uncertainty in ambulance availability. Section 4.2 focuses specifically on the uncertainty in the arrival of EMS requests. Finally, Sect. 4.3 reviews methods to model the uncertainty in EMS response time.
4.1 Uncertainty in Vehicle Availability
Ambulance availability is (typically) defined as the probability that an ambulance will be available when one is needed to respond to an EMS request. In practice, availability is a high-level metric that depends on congestion in the system and is influenced by demand and service time. However, from a modeling perspective, it provides a convenient way to assess how well EMS requests are fulfilled. In Sect. 4.1.1, we review expected coverage models, which account for this uncertainty within the objective function, and in Sect. 4.1.2, we present models that guarantee a level of reliability through chance constraints.
4.1.1 Expected Coverage Facility Location Models
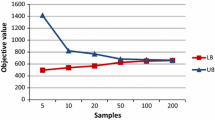
An expected coverage model optimizes the long-run probability that a request for EMS service is appropriately covered. These models often embed probability formulations within their objective functions as an extension to the MCLP. The Maximum Expected Covering Location Problem (MEXCLP) is often credited as the first EMS facility location problem to incorporate uncertainty in its formulation and is the seminal contributor of expected coverage models applied to EMS (Daskin, 1983). MEXCLP uses an objective function similar to the MCLP; however, it adjusts the value of covering a demand node by the long-run probability that an ambulance is available within its RTT. This probability is derived using a binomial probability distribution and a system-wide busy fraction, an input of the model that represents the long-run fraction of time an ambulance is unavailable to be assigned to arriving calls. We note that this busy fraction is believed to be the same for all ambulances in the system. Figure 4 shows how the objective function of MEXCLP is derived.
Several other expected coverage models are direct extensions of MEXCLP. The Multiple-coverage One-unit FLEET (MOFLEET) model extends this idea for a set number of ambulances and stations (Bianchi et al., 1988). The Generalized Maximum Expected Coverage (GMEXC) model provides a framework with varying time standards for each additional coverage of a node (Daskin et al., 1988). The Maximum Expected Covering Location with Time Variation (TIMEXCLP) is an extension that considers demand patterns over time (Repede & Bernardo, 1994). Although MEXCLP and its direct extensions are a tremendous step forward for the field, they rely on several limiting assumptions:
-
1.
All ambulances share the same system-wide busy fraction.
-
2.
Ambulances operate independently.
-
3.
The ambulance busy fraction is invariant to the locations and assignments of the ambulances and patients.
These assumptions are not true in practice. In any EMS system, certain ambulances may be utilized more than others depending on how many patients require care in a given area. Moreover, how these patients are assigned to a given ambulance also impacts the utilization of other vehicles. Lastly, the distance between an ambulance and its assigned patient impacts how long an ambulance must travel and consequentially its busy fraction. Therefore, it is unsurprising that researchers soon found methods to overcome these limitations.
The Hypercube Queuing Model (HQM) is a method that uses queuing theory to determine the steady-state behavior of servers in a multi-server system (Larson, 1974), can be approximated using correction factors for computational simplicity (Larson, 1975), and can distinguish service times dependent on unique server-patient assignments (Jarvis, 1985). This stream of research led to the Approximate MEXCLP (AMEXCLP), a direct extension of MEXCLP that uses correction factors to account for ambulance interdependencies. In this work, the authors provide an application of the HQM to waive all three assumptions noted above (Batta et al., 1989). Other models to directly use the HQM approximation in expected coverage models include an extension of MEXCLP to allow for two vehicle types (McLay, 2009) and a model to locate facilities in a system with a cut-off priority queue (Yoon & Albert, 2018). We note that these HQM approaches assume that EMS requests arrive according to a Poisson process and ambulance service times follow an exponential service time. The Poisson arrival assumption is consistent with real-world data (Kim & Whitt, 2014), and we elaborate on this in Sect. 4.2. The exponential service time assumption may deviate from reality, but several papers have shown that the performance of models does not critically depend on the choice of service time distribution (Ansari et al., 2017; Jagtenberg et al., 2017). Another expected coverage approach addresses the assumptions of MEXCLP without the HQM approximation using two models. The first model assumes that there is no interaction between stations to screen many solutions, and then this assumption is lifted in the second model for a given ambulance allocation. These models utilize an Erlang loss queue, which does not assume that EMS service follows an exponential distribution; however, they assume that all calls that arrive while all servers are busy are unable to be served (Restrepo et al., 2009).
4.1.2 Chance-Constrained Facility Location Models
All of the models mentioned in the previous section maximize expected coverage. A shortcoming of this approach is that it does not provide a guarantee on the reliability of coverage (probability a call arrives and can be served by an ambulance within its RTT) for a particular demand node. Presumably, an EMS agency would like to cover demand nodes with a given level of reliability. An alternative method is to use a chance-constrained model that requires a demand node to be covered with a specified level of reliability. For example, in the Maximum Availability Location Problem (MALP I and MALP II), a method is presented to determine how many ambulances must be positioned within the RTT of the demand nodes for a given reliability level. The authors present an MCLP variant in which a demand node is considered covered only if there are enough ambulances within its RTT to meet the reliability level (ReVelle & Hogan, 1989). The Probabilistic Location Set Covering Problem (PLSCP) is a similar approach applied to the LSCM (ReVelle & Hogan, 1988). However, these models are limited by the same three assumptions described above.
To address these assumptions, queuing theory is used to determine station-specific busy fractions, and refinements of these models include the QPLSCP and QMALP (Marianov & ReVelle, 1994). The use of queuing theory is then extended in the Probabilistic Location-Allocation Set Covering Model with a variable number of servers (PLASC\(\eta \)). PLASC\(\eta \) positions the minimum number of servers and allocates the demand nodes such that a patient will be served within a given time limit with pre-specified reliability (Marianov & Serra, 2002). The Extended Maximum Availability Location Problem (EMALP) uses the hypercube correction factor to adjust MALP to account for server interdependence (Galvão et al., 2005). Once again, using queuing theory, these models assume that ambulances arrive according to a Poisson process and assume an exponential service time or general service time with a loss (zero-length) queue.
4.2 Uncertainty in Arrival Rate
The models presented in Sect. 4.1 explore the likelihood that ambulances are busy and unable to serve a request for help. In an EMS system, the arrival rate (the number and distribution of requests for EMS service) is a factor that significantly affects availability. As shown in Fig. 5, demand for EMS requests is highly variable. Additionally, disasters and other events can cause EMS demand to spike well-beyond standard levels and prevent an EMS system from providing timely and reliable care to all patients. In this section, we explore models that explicitly model arrival rates and are better equipped to examine how this variability in demand affects the optimal locations of EMS resources.
Histogram of daily EMS demand in Mecklenburg County, North Carolina (2004), which includes the city of Charlotte and the surrounding area. The 10th percentile in demand is 151 requests per day and the 90th percentile is 194 requests per day. An unusual blizzard caused demand to spike to 264 requests in a single day (data provided by MEDIC)
4.2.1 Facility Location Models with Probabilistic Arrivals
A method to capture uncertainty in the arrival of EMS requests is to incorporate the underlying arrival distribution into the constraints of EMS facility location problems. One of the first models to do so is Rel-P, a model that considers the arrival distribution in a reliability constraint, under the assumption that a station serves all demand within its RTT as an upper bound (Ball et al., 1993). In many ways, Rel-P is a variation of the chance-constrained models presented in Sect. 4.1.2, since it constrains the likelihood of a request arriving while all servers are busy. However, this likelihood is derived assuming calls arrive according to a Poisson process. Due to the discrete nature, independence, and time invariance (at a high level) of EMS requests, using the Poisson distribution is a safe assumption used in most models and is consistent with real-world data (Kim & Whitt, 2014). A more explicit formulation was later proposed using a stochastic integer program in which the marginal probability distribution for the number of arrivals within each region is captured within a constraint (Beraldi et al., 2004). To adjust for server dependence, this idea is extended to a two-stage model, where the first level locates the EMS facilities and the second level determines how the demand is allocated between them (Beraldi & Bruni, 2009).
Robust and scenario optimization are other methods to model uncertainty in call arrivals. Rather than embedding the arrival distribution into the model, these approaches consider a finite set of demand realizations, called an uncertainty set. An element of this set may represent the number of EMS calls in each area of a city on a particular day, and the set contains different historical or expected demand patterns across multiple days. In robust optimization, the model finds the best EMS allocation that satisfies the given constraints across all demand realizations in the uncertainty set (Zhang, 2014; Boutilier & Chan, 2020). Scenario optimization is similar; however, each element in the uncertainty set is associated with a probability. These probabilities are used within the model to constrain the likelihood that some condition is violated across all scenarios (Noyan, 2010; Nickel et al., 2016). The validity of robust and scenario optimization models depends heavily on the variation captured within the uncertainty set. However, robust and scenario optimization offer several advantages; these approaches avoid using complicated constraints derived from probability distributions, they provide more tractable approaches for larger problem instances, and they rely on fewer assumptions regarding the underlying probability distributions than stochastic modeling approaches (Zhang, 2014).
4.2.2 Predicting Arrival Rates
Traditionally, demand is estimated for EMS facility location models by summarizing historical data, under the assumption that future demand will behave similarly. However, there is a growing stream of research that uses advanced machine learning and analytical models to predict demand. These methods are especially useful when planning for population growth or in areas without reliable historic data.
Early approaches that explore population, demographic, and spatial information associated with EMS demand found that the demand for ambulances is highly predictable using socioeconomic and land-use factors (Kamenetzky et al., 1982). For example, ambulance use is often higher in low-income, non-white, and elderly populations. Other approaches have focused on the daily, weekly, or seasonal cycles of EMS demand using a variety of methods (Channouf et al., 2007; Matteson et al., 2011). Lastly, there are even more granular models that combine spatial and temporal aspects in their forecasts (Zhou et al., 2015; Sariyer et al., 2017). Figure 6 demonstrates the daily temporal trend of EMS requests. Emergency demand is known to follow a circadian rhythm and is highest midday (Bagai et al., 2013). We discuss models that alter their deployment throughout the day in Sect. 5.2.1. We note these prediction models were developed using methods that require accurate historical data. In settings without historical EMS records, such as low- and middle-income countries (LMICs), methods have been developed to heavily rely on population estimates and other high-level features (Fujiwara et al., 1987; Boutilier & Chan, 2020).
4.3 Uncertainty in Response Time
As described in Sect. 2, response time is defined as the time interval between the moment an EMS vehicle is dispatched and an EMS vehicle arrives at the scene of a patient. The majority of the models presented so far assume that response time and an ambulance’s ability to respond within the RTT is known with certainty. In practice, traffic, weather, and other delays can cause uncertainty in the response time of EMS services and can severely affect patient outcomes (Kunkel & McLay, 2013). In this section, we review models that explicitly consider uncertainty in response time.
4.3.1 Facility Location Models with Probabilistic Response Time
The MCLP with Probabilistic Response (MCLP+PR) and MEXCLP with Probabilistic Response (MEXCLP + PR) are simple extensions of the MCLP and MEXCLP, respectively, which use a parameter in the objective function that represents the likelihood a station can reach a demand node within the time limit (Daskin, 1987; Erkut et al., 2009). A similar idea uses gradual covering to reflect coverage uncertainty (Berman et al., 2010; Eiselt & Marianov, 2009). Probabilistic response times are also considered in other models that account for server interdependencies (Goldberg & Paz, 1991), service level constraints (Alsalloum & Rand, 2006), and pre-trip (chute time) delays (Ingolfsson et al., 2008). Robust optimization (as described in Sect. 4.2.1) has also been used to model uncertainty in response times (Boutilier & Chan, 2020). Lastly, while the models discussed thus far focus on the RTT or the average response time, some researchers specifically constrain the tail of EMS response times, such as the 90th percentile of response time, using a value at risk (VaR) approach (Krishnan et al., 2016; Chan et al, 2017; Boutilier & Chan, 2022).
A closely related source of uncertainty is uncertainty in the total service time: the time interval from the moment an EMS unit is dispatched until it is available to respond to another call (see Fig. 1). While uncertainty in response time affects an ambulance’s ability to respond to a call within the RTT, service time affects an ambulance’s availability to serve future calls. For this reason, many of the queuing methods presented in Sect. 4.1 may be used to represent the distribution of service time.
4.3.2 Predicting Response Time
Many EMS models use distance from an EMS unit to a demand node as an approximation for response time. However, it is important to recognize that distance and response time have a nonlinear relationship (Budge et al., 2010). The earliest to explore this relationship modeled EMS response time using a variety of factors such as distance, acceleration (Ingolfsson et al., 2003), road type (Goldberg et al., 1990), and time of day (Hausner, 1975). Modern approaches continue to use similar inputs with more refined techniques (Do et al., 2013; Fleischman et al., 2013; Westgate et al., 2016). In the last decade, data availability has allowed for more accurate traffic pattern predictions and routing (Kok et al., 2012), which, in tandem with machine learning techniques, continues to allow for more precise response time predictions (Vlahogianni et al., 2014; Woodard et al., 2017; Boutilier & Chan, 2020).
4.3.3 Response Time and Patient Outcomes
The models explored so far emphasize timely response. However, improving patient outcomes is the ultimate goal of an EMS system. Some researchers in this area question whether EMS systems overvalue response time and the response time threshold at the expense of other factors important to effective care (Al-Shaqsi, 2010b). One method to ensure optimal outcomes is to replace the objective function based on response time with one that directly measures the survival likelihood of cardiac arrest patients (Erkut et al., 2008) or multiple patient types (Knight et al., 2012). Another approach is to carefully select response time thresholds that maximize survival (McLay & Mayorga, 2010). However, these approaches do not transfer well to patients with conditions that are non-life-threatening. Furthermore, predicting how EMS response affects outcomes is difficult; patient outcomes and response time do not have a linear relationship (Holmén et al., 2020), and there are many other factors that influence outcomes (Boutilier & Chan, 2022). For example, the odds of survival for a cardiac arrest incident observed by a bystander are 2.31 times higher than for an unobserved incident (Stoesser et al., 2021).
5 Notable Directions in EMS Facility Location
The methods and models described in Sect. 4 are a broad sampling of the techniques used to solve EMS facility location problems with uncertainty. These techniques account for many of the unknown elements of EMS systems and more accurately represent the underlying dynamics of a traditional EMS system than deterministic models. However, as mentioned in Sect. 2, it is difficult to generalize EMS systems. The methods presented in Sect. 4 may fail to capture the critical dynamics of more complicated or less studied settings. In this section, we explore a few of the many directions of EMS facility location problems and the advanced modeling techniques developed to capture their unique features. Section 5.1 reviews methods to model EMS systems with multiple vehicle types. Section 5.2 explores EMS facility location models that allow ambulance relocation. Section 5.3 discusses the unique challenges of EMS in low- and middle-income countries. Lastly, Sect. 5.4 briefly highlights a few other new applications and directions of EMS facility location research.
5.1 EMS Vehicle Types and Tiered EMS Systems
In the United States, it is estimated that over 65% of EMS responses are for patients with conditions that are non-life-threatening and unlikely to progress (data provided by NEMSIS). To avoid unnecessary utilization of expensive and resource-intensive ambulances for these non-urgent patients, many EMS systems implement a tiered EMS system in which EMS vehicles with different levels of training and resources are matched to the needs of a patient. Some advantages of a tiered EMS system are that lower-acuity ambulances are less resource-intensive, they typically allow for larger EMS fleets, and they can enable shorter response times for critical patients (Stout et al., 2000). However, patient misclassification and under-triage are risks that must be carefully managed in such a system (Wilson et al., 1992). In Sect. 5.1.1, we review the types of vehicles that may be available in a tiered EMS system, and in Sect. 5.1.2, we describe the facility location models that explore the unique dynamics and uncertainties of tiered EMS systems.
5.1.1 Tiered EMS Vehicle Types
In North America, transport-equipped EMS vehicles are traditionally categorized by the level of care they may provide a patient. An advanced life support (ALS) unit is a larger and more resource-intensive ambulance, usually with a truck chassis-cab and a large box-like rear compartment (see Fig. 7a). An ALS ambulance is staffed by highly trained paramedics equipped to provide advanced care such as administering intravenous fluids, providing controlled medication, using advanced airway techniques, and monitoring cardiac conditions in addition to providing basic noninvasive care. Regions that do not use a tiered EMS system often use an all-ALS ambulance system. Alternatively, a basic life support (BLS) unit is a less resource-intensive ambulance usually staffed by emergency medical technicians who are only equipped to provide noninvasive care such as performing cardiopulmonary resuscitation (CPR), immobilizing broken bones, administering oral medications, and providing oxygen (see Fig. 7b) (Al-Shaqsi, 2010a). Studies have found that 85% of calls in the United States are within the scope of BLS ambulances (Pozner et al., 2004), but despite their ability to serve the majority of patients, 5 of the 50 US states (Georgia, Hawaii, Missouri, South Dakota, Washington) do not license BLS agencies as of 2011 (National Highway Traffic Safety Administration, 2014).
Different types of vehicles in a tiered EMS system. (a) ALS ambulances are equipped to perform invasive care, and are preferred for time-sensitive patients in a tiered system. Photo by Eric Stratman. (b) BLS ambulances are equipped to perform non-invasive care, and are preferred for lower acuity patients in a tiered system. https://unsplash.com/photos/T5TojXFNnjk (See: https://unsplash.com/license). (c) EMS NTVs may be the sole respondent under the stay and stabilize EMS model or they may support transport vehicles under the scoop and run model. https://pixabay.com/photos/car-city-medicine-automobile-4368213/ (See: https://pixabay.com/service/license/). (d) Fire and Police units, which may act as NTVs, are playing an increasingly important role in many EMS systems. https://pixabay.com/photos/fire-in-houston-houston-texas-texas-3252193/ (See: https://pixabay.com/service/license/)
A non-transport vehicle (NTV) is another common component of an EMS system and is defined as any vehicle equipped to respond to an EMS request and provide on-scene care, but not intended to transport the patient (Crawford & Wilson, 2019). NTV is a very broad definition. A traditional NTV is often a sports utility vehicle (SUV) staffed by medical personnel (see Fig. 7c). This is the type of vehicle used in European-style stay and stabilize systems where an NTV staffed by a medical doctor is the sole respondent to the majority of patients. In a North American scoop and run system, an NTV may also be a medically trained fire or police unit. From 1977 to 2015, the number of fire incidents has decreased by 59% (Ahrens, 2017). Due to this extra capacity and the strategic positioning of fire companies, researchers and practitioners are exploring ways to use these resources in EMS systems (Swersey et al., 1993; McLay & Moore, 2012).
5.1.2 Facility Location with Tiered EMS
Tiered EMS systems bring new dynamics and modeling challenges to EMS facility location problems. In addition to providing reliable and timely EMS response, a tiered EMS system must ensure that the types of resources responding to a patient are appropriate for their need. Modeling this dynamic is often the central challenge of tiered EMS facility location models. There are three general approaches to tiered EMS models: (1) models that assume all patients are of equal priority, (2) models that differentiate between patient priority and assume priority is known with certainty at the time of dispatch, and (3) models that differentiate between patient priority and acknowledge the inherent uncertainty in patient classification. We explore all three of these approaches within this section.
Tiered EMS Without Patient Prioritization
Many of the early tiered EMS facility location models are extensions of the models reviewed in Sect. 4. They provide insights into EMS strategy; however, they do not explicitly consider how a tiered EMS unit will respond to individual patients or patient priority classes. Rather, the tiered units are used to redefine coverage. For example, the simplest approach to model a tiered system is to require a covered demand node to be within the RTT of all vehicle types. This is the approach of the early models that position resources for fire systems with multiple vehicle types (Marianov & ReVelle, 1992). However, unlike fire emergencies that often require multiple types of vehicles, EMS emergencies offer more flexibility because they usually only need one appropriate ambulance. Another approach is to use lower-acuity vehicle types to fill the coverage gaps of the higher-acuity ambulances. For example, a covered demand node must be within an RTT from an ALS ambulance; however, this RTT is more lenient (longer) for demand nodes that can be quickly reached by a BLS ambulance (Mandell, 1998). A slightly different tiered approach allows BLS ambulances to be the sole respondent to patients believed to meet their criteria for response; however, there is a chance that these patients need advanced care and trigger an ALS unit to also be dispatched (Marianov & Serra, 2001). While these methods utilize ALS and BLS units in a variety of ways, none of these approaches prioritize the need of patients with truly life-threatening emergencies.
Tiered EMS with Known Patient Prioritization
The manner in which tiered vehicles are used for patients with varying conditions and levels of urgency is an important dynamic of tiered EMS systems with many practical implications. One approach is to use higher-acuity ambulances for high-priority patients and use lower-acuity ambulances as the sole respondent to lower-acuity patients. Only when all higher-acuity ambulances are busy will a lower-acuity ambulance be used as the sole respondent for a high-priority patient. The previously mentioned MEXCLP2 uses such an approach (McLay, 2009) as do recent papers that explore more complicated vehicle substitutions (Nelas & Dias, 2021). However, in practice, these types of vehicle substitutions are likely unfavorable, and some models adjust the reward of responding to a call depending on if the patient-vehicle type match. In other words, they provide a full reward when the responding ambulance meets or exceeds the patient need and a partial reward when the assigned vehicle is lower than a patient’s need (Chong et al., 2016; Yoon et al., 2021) or do not allow any coverage when the vehicle does not meet a patient’s need (Boujemaa et al., 2018). While these models may account for the uncertainty in demand, service time, and ambulance availability, they assume that the information used to prioritize patient response and inform ambulance type decisions is known with certainty. In practice, EMS dispatchers must predict this information using the limited information provided during the initial EMS request, which may be inaccurate.
Tiered EMS with Patient Prioritization Under Uncertainty
Following a request for emergency care, an EMS dispatcher must use the limited information provided during the phone screening to decide which EMS unit should respond to the patient. Often EMS personnel act conservatively and assume a higher level of urgency (over-triage) to avoid delaying the patient from potentially life-saving care. Although there is no standard for appropriate rates of over- and under-triage, previous studies have estimated that over- and under-triage rates are as high as 78% and 4%, respectively (Dami et al., 2015). Optimal dispatching models have demonstrated that high uncertainty in patient classification leads to more urgent responses to mid-priority patients (McLay & Mayorga, 2013), and many researchers continue to investigate methods to assess and improve EMS triage accuracy (Bohm & Kurland, 2018; Alotaibi et al., 2021). However, it is unlikely that an EMS system will ever be perfectly accurate, and one method to hedge against this risk is through multiple response: the EMS practice in which multiple units are sent to the same patient. This approach ensures that the vehicle that best meets a patient’s need responds to the patient while allowing the unneeded vehicle to serve another patient sooner and, hence, influences the optimal location of EMS resources (Yoon & Albert, 2020). Surprisingly, misclassification in patient priority and the subsequent mitigating actions is not well explored in EMS facility location model literature and is certainly an area of opportunity for the field.
5.2 EMS Systems with Relocation
Thus far, we have presented the location of EMS units as static and implicitly assumed that whenever an EMS unit is not in use, it is waiting at a specific location. However, given the cyclic trends in EMS demand and the mobility of EMS units, ambulance relocation, defined as strategically moving EMS vehicles to improve EMS coverage, is a topic that has received much attention in EMS research. This is also commonly called System Status Management (SSM) in practice. There are two primary classifications for EMS relocation models: multi-period relocation and dynamic relocation. A multi-period relocation model relocates EMS units to account for the spatial-temporal trends in EMS demand, such as those described in Sect. 4.2.2. A dynamic relocation model relocates EMS units to account for gaps in coverage that form as EMS units become busy. In this section, we review both approaches.
5.2.1 Multi-period Relocation Models
Multi-period relocation models account for the cyclic spatial-temporal changes in demand for EMS service. For example, during the day, many people are at an office, school, or another commercial location. A strategic EMS system may increase the number of units located near commercial areas during these times. Then, during the evening, most people return home; therefore, it may be advantageous to shift EMS units to residential areas during these times (see Fig. 8). This is the basic idea of multi-period relocation models.
The Maximal Expected Coverage Location Model with Time Variation (TIMEXCLP) is often credited as the first EMS relocation model (Repede & Bernardo, 1994). TIMEXCLP is an adaptation of MEXCLP developed in partnership with an EMS system in Louisville, Kentucky, and accounts for changes in the EMS fleet size and spatial-temporal demand patterns. This application demonstrates the importance of relocation by showing that 95% coverage, which required nine ambulances under the MEXCLP solution, is achievable with eight ambulances if relocation is used. This model does not utilize the advancements of the HQM approach and is therefore subject to the limiting assumptions described in Sect. 4.1.1. Nearly 15 years later, the Dynamic Available Coverage Location Model (DACL), a multi-period LSCM model, was suggested as an extension of the QPLCP (mentioned in Sect. 4.1.2) with a correction factor to account for server dependence (Rajagopalan et al., 2008). However, a possible shortcoming of both of these models is they do not limit ambulance relocations. In practice, a system that relocates ambulances too often could be difficult to implement, increase the workload for EMS personnel, and cause fatigue (Bledsoe, 2003). To minimize relocations, TIMEXCLP was later extended to include relocation and facility costs (van den Berg & Aardal, 2015), and DACL was extended to minimize relocations (Saydam et al., 2013). Some additional multi-period relocation models include extensions that account for time-dependent travel times (Schmid & Doerner, 2010; Degel et al., 2015), a multi-period extension of the DSM (Başsar et al., 2011), a model that considers personnel workloads (Enayati et al., 2018), and a model tailored for tiered EMS systems (Boujemaa et al., 2020).
5.2.2 Dynamic Relocation Models
Whereas multi-period relocation models account for predictable changes in EMS demand, dynamic relocation models actively adjust ambulance deployment based on the state of the system. As ambulances become busy, dynamic relocation models shift other EMS units to fill coverage gaps. The first models in this area were real-time dynamic models, which were intended to be solved every time an ambulance was dispatched. However, due to computational challenges and complexity, implementing these models in practice is difficult. Alternatively, offline dynamic models provide pre-computed strategies that can be implemented by following a table or other tools. Lastly, we separate relocation models that use approximate dynamic programming to generate admissible solutions to larger problems while accounting for additional levels of information (e.g., ongoing trip duration, travel destination, attributes of queued demand, etc.).
Real-Time Dynamic Relocation Models
The first dynamic model, named \(RP^t\), is an extension of the DSM (Gendreau et al., 2001). At its simplest, \(RP^t\) can be viewed as an extension of the DSM that is solved whenever an ambulance is dispatched. However, to limit ambulance relocation and undesirable actions such as a round-trip, \(RP^t\) includes a penalty term in its objective function that is dependent on the history of the system. To allow for the model to be implemented in real time despite the computational complexity, the authors offer a method to solve for the future dispatching possibilities following each decision. There are several other real-time relocation models similar to \(RP^t\). Some of these extensions include approaches that replace coverage with a preparedness measure (Andersson & Väarbrand, 2007; van Barneveld et al., 2017a), a model that allows for multiple vehicle types (Mason, 2013), a dynamic extension of MEXCLP (Jagtenberg et al., 2015), a model that considers ambulance shift schedules (Naoum-Sawaya & Elhedhli, 2013), an extension that allows for the relaxation of the double-coverage constraint (Moeini et al., 2015), and a model tailored for rural areas (van Barneveld et al., 2017a).
Offline Dynamic Relocation Models
Real-time relocation models are difficult to implement in practice due to computational complexity, technology limitations, and workflow burdens. EMS relocation models that focus on developing strategies that can be used offline or read from a compliance table—a simple tool that tells EMS managers where they should locate ambulances given high-level metrics (number of available ambulances, time of day)—are preferred in many settings. For example, as mentioned previously, the \(RP^t\) computes future dispatching possibilities following each EMS unit dispatch. However, in the event of two EMS requests in a short period, the model may not have been solved to completion. To address this, the authors later proposed the Maximal Expected Coverage Relocation Problem (MECRP), one of the earliest offline models (Gendreau et al., 2006). MECRP pre-computes the optimal ambulance location given the number of ambulances while limiting the number of ambulance moves. Other models similar to MECRP that generate offline compliance tables include a Markov-chain model that can quickly assess the performance of many compliance tables (Alanis et al., 2013), an extension that allows for two types of vehicles (van Barneveld et al., 2017b), an approach to consider the variation of demand patterns over time and changes in response times (Nair & Miller-Hooks, 2009), and a model that considers call priorities (Sudtachat et al., 2014).
ADP Dynamic Relocation Models
Dynamic Programming (DP) is well-suited to optimize processes with sequential decisions, such as ambulance relocation. However, due to the high level of detail needed to accurately represent an EMS system, DP models quickly become intractable (due to large state spaces). Approximate Dynamic Programming (ADP) is a powerful tool that can be used to overcome this limitation and generate admissible solutions to complex stochastic and dynamic problems. For ADP applied to EMS relocation, the research by Maxwell et al. (2010) is often cited as the seminal work in this field. In their paper, the authors determine where an EMS unit should be positioned after it transfers a patient to the hospital. To inform these decisions, the ADP model uses a basis function, a linear function that encodes many details about the state of the EMS system to predict the cost of a relocation decision. The inputs of this basis function are inspired by queuing theory and an EMS location model. The weights of these inputs are tuned using least squares regression to minimize the error between the basis function and a cost found via simulation. It is important to note that in any ADP model, the final relocation strategy may not be the optimal solution because model convergence is highly dependent on the basis function and how the parameters are tuned. However, an admissible solution generated by an ADP can inform relocation decisions much faster than other real-time models, offers greater flexibility than the offline compliance tables since the user can deviate from the suggested solution, and allows for solving higher-dimensional problems. Two other refinements to EMS relocation using ADP include an approach that considers time-dependent travel times and demand (Schmid, 2012) and an approach that allows for the relocation of any idle EMS unit (Nasrollahzadeh et al., 2018). We note that since ADPs do not guarantee an optimal solution, methods can be used to develop bounds on the optimal solution (Maxwell et al., 2014; Nasrollahzadeh et al., 2018).
5.3 EMS in Low- and Middle-Income Countries
Time-sensitive medical emergencies, like cardiac arrests, motor vehicle accidents, and child or maternal health issues, are a major health concern in low- and middle-income countries (LMICs), comprising over 50% of all deaths (Moresky et al., 2019). Globally, LMICs are home to approximately 85% of the world’s population and 90% of all healthcare emergencies (Lecky et al., 2020; Prydz & Wadhwa, 2019). As a consequence, researchers and international organizations have stressed the need for increased focus on emergency medical care in LMICs with several calls to action (United Nations, 2010). Despite these calls and the widespread evidence that emergency medical care in LMICs saves lives, poor access and availability continues to be a major problem, with the lack of EMS as one of the main barriers (Moresky et al., 2019; Lecky et al., 2020). Many of the high-level challenges associated with EMS in LMICs are well-suited to operations research and management science tools. For example, recent surveys indicate that poor performance is a major barrier for patients attempting to access EMS services, with 20–30% of those surveyed indicating they wanted to take an ambulance, but response times were too slow or that an ambulance was not available (i.e., busy at another call) (Boutilier & Chan, 2020). Moreover, most LMICs are resource-constrained, presenting an opportunity to optimize the use of EMS resources to improve effectiveness and efficiency.
Early research on EMS in LMICs was primarily focused on rural areas, including a variant of the MLCP to determine the optimal location of rural health clinics in Colombia (Bennett et al., 1982). A few years later, motivated by the lack of an existing EMS system in the Dominican Republic, the HOSC formulation (see Sect. 3.2) was extended to include two objectives: one to minimize the number of resources and one to maximize demand covered multiple times (Eaton et al., 1986). At the time, existing models that accounted for ambulance availability required a pre-determined “busy fraction” for each ambulance base, which did not exist for the problem of designing a new EMS system, and motivated the authors to develop a multiple coverage formulation. More recently, researchers have shifted their focus to urban areas in LMICs. The first paper to explore EMS response optimization in a developing urban center leveraged MEXCLP to determine ambulance locations and conduct a case study in Bangkok, Thailand (Fujiwara et al., 1987). Since then, there have been several papers that optimize EMS response in urban centers around the world (Boutilier & Chan, 2020).
In general, EMS network design and response optimization in LMICs presents several unique challenges that are not typically found in high-income settings, which we highlight below:
-
Traffic can be extremely heavy (especially in urban areas), and it is often not the cultural norm to yield for ambulances, implying that ambulances must face the same traffic as regular road users. In contrast, ambulances are typically able to drive “fast” in high-income countries where it is the cultural norm to yield and where infrastructure is designed with EMS in mind (e.g., extra wide shoulders on freeways). The difference in road speed and consequential uncertainty in response time must be accounted for in models designing EMS systems for LMICs (Boutilier & Chan, 2020).
-
Many LMICs do not have a centralized EMS system, instead relying on decentralized ambulance services comprised of private and hospital-owned fleets. The lack of a centralized EMS system (or even a coordinated public health system) presents significant challenges associated with data collection, including data that may be required for many facility location models (Eaton et al., 1986). In addition, the decentralized nature of these services can lead to a phenomenon known as “ambulance abandonment,” where patients simultaneously request service from multiple ambulance providers and take the first one to arrive (Marla et al., 2021). Future work is needed to explore the competitive nature of these decentralized EMS systems.
-
Road infrastructure in LMICs is typically not designed for modern EMS resources, especially in dense urban areas and “old towns.” For example, many areas in urban slums cannot be accessed by four-wheeled vehicles (like ALS or BLS ambulances) and require non-traditional ambulance designs, such as motorcycles and three-wheeled vehicles (see Fig. 9a). Moreover, current ambulance designs and staff certifications in many LMICs are akin to the early EMS systems in high-income settings, where ambulances were staffed by “ambulance drivers” with limited first-aid training (rather than certified paramedics or physicians) and focused on patient transport, rather than treatment. These differences require innovative solutions and models designed to account for multiple vehicle types, restricted road access, limited transportation options, and lack of treatment in place.
Fig. 9 EMS facility location models can be adapted for settings that present unique modeling challenges. (a) Non-traditional ambulance designs, such a motorcycles, are common in LMIC settings. Photo by Justin Boutilier. (b) EMS helicopters offer increased speed and maneuverability for remote patients. https://pixabay.com/photos/helicopter-rescue-6392253/ (https://pixabay.com/service/license/). (c) UH-60M Blackhawk helicopters provide urgent care and evacuation to military casualties. Photo by Nolan Donahue, Given to and edited by Eric Stratman. (d) Search and rescue applications utilize sea and air units with various capabilities. https://pixabay.com/photos/coast-guard-sea-maritime-rescue-6718306/ (https://pixabay.com/service/license/)
5.4 Other Unique Settings in EMS Facility Location
The directions discussed in this section are a sampling of the unique areas in EMS facility location research. There are numerous directions for applications of EMS facility location (aircraft, military, following natural disasters, wilderness applications, etc.), and in this section, we provide a summary of a couple of these areas to demonstrate how EMS facility location models may be adapted to unique settings.
AED Location Models
Automatic electronic defibrillators (AEDs) are portable devices designed to deliver life-saving electric shocks to a patient experiencing an out-of-hospital cardiac arrest (OHCA). AEDs are safe and easy to use by untrained bystanders and significantly improve an OHCA patient’s chances of survival. An OHCA patient that receives an AED shock administered by a bystander is 2.36 times more likely to survive than a patient without AED shock, and the impact of EMS delays is significantly reduced following AED treatment (Stoesser et al., 2021). To improve accessibility, location models similar to those in EMS are used to located AEDs and have performed better than the traditional population-based AED location methods (Chan et al., 2013). In these models, predicting the location and timing of OHCA events is especially important since AEDs are often retrieved by bystanders that only travel a short distance from the patient (approximately 100 meters) and may face barriers to AED access (Sun et al., 2016). AED location research builds upon the EMS facility location models and explores dynamics unique to the AED application including uncertainty in the time before an OHCA is detected (Dao et al., 2012), the dimensionality of locating AEDs in multi-story buildings (Dao et al., 2012; Chan, 2017), and emphasise on the spatial probability distribution of demand (Chan et al, 2017).
Aircraft Location Models in EMS Systems
Aircraft are an important feature of some EMS systems. Although more expensive and dangerous than ground units, transportation aircraft may be advantageous in some settings due to their increased speed and maneuverability (Steenhoff et al., 2022). Generally, it is only recommended that helicopters be used for urgent patients that cannot be reached by ground-based units in 30 minutes (Godfrey & Loyd, 2021), and airplanes are only used for missions that require over 120 miles (193 km) of travel (Urdaneta et al., 1987). Historical records indicate that 64% of all patients served by aircraft suffered a traumatic injury (data provided by NEMSIS). Given the number of trauma patients served by EMS aircraft, many of the aircraft location models consider the optimal allocation of both trauma centers and EMS aircraft (Branas et al., 2001); however, this leads to added complexity when computing system busy fractions (Cho et al., 2014). Another approach is to exploit the added range of the aircraft for backup coverage in a tiered system with ground-based units (Erdemir et al., 2010).
In addition to airplanes and helicopters, unmanned aerial vehicles such as drones are becoming more common in healthcare applications (Scott & Scott, 2017). Several studies explore how drones can be used to transport medical supplies to rural areas (Kim et al., 2017; Knoblauch et al., 2019). In EMS systems, drones perform a variety of functions including delivering AEDs, critical blood products, and medication before EMS arrives to enable timely care to patients (Johnson et al., 2021). This is especially true in areas with limited EMS coverage. In a drone AED delivery system in Toronto, the optimal deployment of drone bases allows for a nearly 7-minute reduction in the 90th percentile of urban response time (Boutilier et al., 2017). In Sweden, a similar system using drones has already saved the life of a cardiac arrest patient (Schierbeck et al., 2021; BBC, 2022). This demonstrates the value of emerging technology in EMS and how EMS facility location research can be used to influence the deployment of these advanced technologies.
Military Medical Evacuation Location Models
Military medical evacuation (MEDEVAC) systems provide urgent care and evacuation to military casualties. Unlike EMS systems in which the primary time-sensitive medical emergency is often cardiac arrest, loss of blood is the direct cause of 85% of soldiers killed in action (Garrett, 2013). To account for the treatment of battlefield injuries, MEDEVAC coverage models generally allow for longer RTT thresholds of 60 minutes for high-priority patients (Bastian et al., 2012; Grannan et al., 2015) or prioritize patients by their condition (Fulton et al., 2010). Other works specify that MEDEVAC systems need to focus on the time interval from when a soldier is injured until the time that they are delivered to a facility equipped to safely perform blood transfusion, with a focus on the inherent stochasticity of this process (Lejeune & Margot, 2018). Another key difference is in the arrivals; while traditional EMS setting requests can be viewed as independent events, battlefield injuries generally occur in batches following an attack. Therefore, some of the MEDEVAC models try to avoid queuing assumptions that rely on a Poisson process. These models generally account for non-Poisson arrivals through either empirical or simulated data with some form of robust or scenario optimization (Fulton et al., 2010; Bastian, 2010; Bastian et al., 2012). We also note that the objectives of MEDEVAC facility location may balance facility vulnerability to adverse attacks (Bastian, 2010) and the required capabilities of MEDEVAC units (Bastian et al., 2012). Lastly, models that inform MEDEVAC dispatching policies are also influential within this stream of research (Rettke et al., 2016; Keneally et al., 2016).
Search and Rescue Location Models
Search and rescue (SAR) resource allocation is a field with many connections to EMS facility location problems. SAR systems, such as those deployed by national coast guard units, provide potentially life-saving aid to people in danger, and the location of resources is critical to providing this care in a timely manner. However, unlike EMS, the exact location of the person in need may be unknown in SAR missions, and conditions (weather, time of day) may dramatically impact the search effort, which is reflected in modeling approaches (Başsdemir & Melih, 2000; Abi-Zeid & Frost, 2005). Furthermore, unlike EMS systems where there is ample data to predict where an EMS request might be generated, the vastness of the areas patrolled by SAR makes it difficult to predict where future requests will occur, especially in maritime settings. Models have used a variety of methods to predict future demand (Azofra et al., 2007; Akbari et al., 2018). Additionally, SAR units must balance scheduled duties, operational and political rules, and fleet capabilities for a variety of watercraft and aircraft (Wagner et al., 2012; Karatas et al., 2017). We refer the reader to the chapter of Karatas et al. (2019) for a detailed review of SAR models.
6 Implementation of EMS Facility Location Models
The goal of EMS facility location problems is to develop strategies to better serve patients. Despite all of the academic contributions cited within this chapter, not all papers directly contribute to the development of an actual EMS implementation. As stated by Chaiken (1978), “careful studies of the actual use of models by decision-makers have drawn sobering conclusions about the chances that such models will actually be applied as intended.” Although many models indirectly bolster the field by developing newer and more elegant approaches, this field needs to keep the ultimate goal in mind and avoid turning into an academic exercise. From our review, we summarize the lessons learned and the important themes from several implementation-based papers.
Design for the User
Successful implementations of EMS facility location models need to be designed with the decision-maker in mind. While we found numerous implementations of deterministic and simple probabilistic models, we found very few implementations of the more complicated probabilistic models. This is likely because these simpler models are easier to explain and be accepted by an EMS agency. This is the same rationale that made offline relocation models more preferable in our discussion in Sect. 5.2.2. Similarly, in an implementation of the probabilistic MEXCLP in Lexington, Kentucky, that project was largely successful because the authors worked closely with the decision-makers, utilized a graphical interface to explain their ideas (Repede et al., 1993), and gained the EMS agency’s trust by modifying their model with their feedback (Repede & Bernardo, 1994). Similar collaborations and validations are noted in other implementations (Brandeau & Larson, 1986; Goldberg et al., 1990).
Guide EMS Practice
EMS facility location models must be timely and ahead of EMS practice. Following the implementation of an EMS facility location design in Morgantown, West Virginia, the researchers suggested that sophisticated models are only appropriate when given sufficient time for careful model formulation (Baker et al., 1980). This is perhaps why many of the most documented EMS facility location model implementations are in LMICs with emerging EMS infrastructures, as discussed in Sect. 5.3. Unlike areas with well-established EMS operations that are unlikely to change their existing strategy or facility locations, these emerging infrastructures are less committed and often open to change. The recent implementations of EMS facility location models to drone AED delivery systems is another example of research being timely and accessible to strategic planning efforts (Boutilier et al., 2017; Schierbeck et al., 2021; Boutilier & Chan, 2022).
Acknowledge EMS Legal Limitations
Any implementation will be subject to many legislative barriers. According to the General Data Protection Regulation (GDPR) law of the European Union, human intervention can be requested, and an adequate explanation must be provided for any automated decision (Olhede & Wolfe, 2018). Therefore, EMS location models must be robust enough that they still perform well should they be overridden by a human decision-maker and intuitive enough should an explanation be requested. Once again, these requirements limit the complexity of EMS location models. Similarly, EMS agencies are required to respond to calls in a reasonable manner. An EMS agency may prefer to always send the closest or most highly trained EMS unit to patients to avoid potential legal pitfalls. Within the next decade, we hope that EMS researchers expand the visibility of their work to lawmakers to demonstrate the benefit of more progressive EMS strategies and allow for more cost-effective, efficient, and patient-centered EMS care.
Focus on Accessibility
Although not every EMS facility location model is designed with a specific implementation in mind, there are many ways in which EMS facility location research can make an impact. Many EMS implementations use commercial tools, such as ESRI’s Geographic Information System (GIS) software, to inform their location problem (Foo et al., 2010). Perhaps the best way for EMS facility location modelers to have a direct impact in the field is through closer collaboration with these accessible tools. As another example, the relocation model developed by Mason (2013) has been implemented by multiple ambulance operators through an associated software package.
We conclude by acknowledging that it was difficult to find clear summaries of EMS systems that implement the results of facility location models. As a field dedicated to continuous improvement, we believe EMS models in action should receive greater attention (even when unsuccessful) to guide future directions and modeling efforts.
7 Additional Resources
In this chapter, we reviewed the models and methods of EMS facility location problems under uncertainty. We focused on the overall themes within this field and aimed to provide the reader with an understanding of these models and their evolution. In this section, we summarize resources that present more in-depth technical reviews of this field for a comprehensive literature review. Since there is no shortage of facility location review papers, we limit the cited works to those that focus on EMS or address another focus of this chapter.
-
The work of ReVelle et al. (1977) is the earliest literature review of EMS facility location problems. They present the deterministic LSCM, MCLP, and PMP models context-free and discuss the application of facility location problems to EMS and other emergency services.
-
The review by Brotcorne et al. (2003) summarizes the formulation of deterministic single and multi-coverage models as well as the early probabilistic models. They conclude with a summary of an early dynamic model and predicted their continued rise within the field.
-
Goldberg (2004) provides a review of the methods that support EMS facility location models, such as travel time modeling, demand prediction, testing model validity, and queuing. They classify existing models using a different method than the previous reviews and cite models that were directly implemented.
-
The chapter by Henderson (2011) provides a specific focus on EMS models with relocation, such as those discussed in Sect. 5.2, and provides additional discussion of this practice.
-
The summary by Başsar et al. (2012) provides a helpful taxonomy of facility location problems as applied to emergency services. They classify models based on their solution methodology, application, objective function, and parameters in a concise table.
-
Aringhieri et al. (2017) offer a slightly different perspective than the other review papers. In the first part of their paper, they address EMS facility location problems with sections related to probability, stochastic, relocation, and equity. Then, they discuss EMS dispatching and routing policies and the important connection with other components of the healthcare system.
-
The chapter by Karatas et al. (2019) provides a review of military facility location problems and provides greater details about the MEDEVAC and SAR settings discussed in Sect. 5.4.
-
The review paper by Bélanger et al. (2019) provides an in-depth review of deterministic and probabilistic models, providing more details on the model formulations. They also offer a thorough discussion on equity, relocation, and dispatching decisions in EMS systems.
References
Abi-Zeid, I., & Frost, J. R. (2005). SARPlan: a decision support system for Canadian Search and Rescue operations. European Journal of Operational Research, 162(3), 630–653.
Ahrens, M. (2017). Trends and patterns of U.S. fire loss. Quincy, MA: National Fire Protection Association.
Akbari, A., Pelot, R., & Eiselt, H. A. (2018). A modular capacitated multiobjective model for locating maritime search and rescue vessels. Annals of Operations Research, 267(1), 3–28.
Al-Shaqsi, S. (2010a). Models of international emergency medical service (EMS) systems. Oman Medical Journal, 25(4), 320–323.
Al-Shaqsi, S. (2010b). Response time as a sole performance indicator in EMS: Pitfalls and solutions. Open Access Emergency Medicine, 2, 1–6.
Alanis, R., Ingolfsson, A., & Kolfal, B. (2013). A Markov chain model for an EMS system with repositioning. Production and Operations Management, 22(1), 216–231.
Alotaibi, A., Alghamdi, A., Reynard, C., & Body, R. (2021). Accuracy of emergency medical services (EMS) telephone triage in identifying acute coronary syndrome (ACS) for patients with chest pain: a systematic literature review. BMJ Open, 11(8), e045815.
Alsalloum, O. I., & Rand, G. K. (2006). Extensions to emergency vehicle location models. Computers & Operations Research, 33(9), 2725–2743.
Andersson, T., & Väarbrand, P. (2007). Decision support tools for ambulance dispatch and relocation. The Journal of the Operational Research Society, 58(2), 195–201.
Ansari, S., Yoon, S., & Albert, L. A. (2017). An approximate hypercube model for public service systems with co-located servers and multiple response. Transportation Research Part E: Logistics and Transportation Review, 103, 143–157.
Aringhieri, R., Bruni, M. E., Khodaparasti, S., & van Essen, J. T. (2017). Emergency medical services and beyond: addressing new challenges through a wide literature review. Computers & Operations Research, 78, 349–368.
Azofra, M., Péerez-Labajos, C. A., Blanco, B., & Achúutegui, J. J. (2007). Optimum placement of sea rescue resources. Safety Science, 45(9), 941–951.
Bélanger, V., Ruiz, A., & Soriano, P. (2019). Recent optimization models and trends in location, relocation, and dispatching of emergency medical vehicles. European Journal of Operational Research, 272(1), 1–23.
Başsar, A., Çatay, B., & Ünlüyurt, T. (2011). A multi-period double coverage approach for locating the emergency medical service stations in Istanbul. The Journal of the Operational Research Society, 62(4), 627–637.
Başsar, A., Çatay, B., & Ünlüyurt, T. (2012). A taxonomy for emergency service station location problem. Optimization Letters, 6(6), 1147–1160.
Başsdemir, M. M. (2000). Locating search and rescue stations in the Aegean and western Mediterranean regions of Turkey. Journal of Aeronautics and Space Technologies, 1(3), 63–76.
Bagai, A., McNally, B. F., Al-Khatib, S. M., Brent Myers, J., Kim, S., Karlsson, L., Torp-Pedersen, C., Wissenberg, M., van Diepen, S., Fosbol, E. L., Monk, L., Abella, B. S., Granger, C. B., & Jollis, J. G. (2013). Temporal differences in out-of-hospital cardiac arrest incidence and survival. Circulation, 128(24), 2595–2602.
Baker, D. W. & Byrd, J. (1980). A lesson in timing: a nonemergency solution to an emergency service decision. Interfaces, 10(3), 30–33.
Ball, M. O. & Lin, F. L. (1993). A reliability model applied to emergency service vehicle location. Operations Research, 41(1), 18–36.
Bastian, N. D. (2010). A robust, multi-criteria modeling approach for optimizing aeromedical evacuation asset emplacement. The Journal of Defense Modeling and Simulation, 7(1), 5–23.
Bastian, N. D., Fulton, L. V., Mitchell, R., Pollard, W., Wierschem, D., & Wilson, R. (2012). The future of vertical lift: initial insights for aircraft capability and medical planning. Military Medicine, 177(7), 863–869.
Batta, R., Dolan, J. M., & Krishnamuthy, N. N. (1989). The maximal expected covering location problem: revisited. Transportation Science, 23(4), 277–287.
BBC. (2022). Drone helps save cardiac arrest patient in Sweden. BBC News.
Bennett, V. L., Eaton, D. J., & Church, R. L. (1982). Selecting sites for rural health workers. Social Science & Medicine, 16(1), 63–72.
Beraldi, P., & Bruni, M. E. (2009). A probabilistic model applied to emergency service vehicle location. European Journal of Operational Research, 196(1), 323–331.
Beraldi, P., Bruni, M. E., & Conforti, D. (2004). Designing robust emergency medical service via stochastic programming. European Journal of Operational Research, 158(1), 183–193.
Berman, O., Drezner, Z., & Krass, D. (2010). Generalized coverage: new developments in covering location models. Computers & Operations Research, 37(10), 1675–1687.
Bianchi, G., & Church, R. L. (1988). A hybrid fleet model for emergency medical service system design. Social Science & Medicine, 26(1), 163–171.
Bledsoe, B. (2003). EMS myth #7: system status management lowers response times and enhances patient care. EMSWorld, 32(9), 158–159.
Bohm, K., & Kurland, L. (2018). The accuracy of medical dispatch - a systematic review. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 26, 94.
Boujemaa, R., Jebali, A., Hammami, S., Ruiz, A., & Bouchriha, H. (2018). A stochastic approach for designing two-tiered emergency medical service systems. Flexible Services and Manufacturing Journal, 30(1), 123–152.
Boujemaa, R., Jebali, A., Hammami, S., & Ruiz, A. (2020). Multi-period stochastic programming models for two-tiered emergency medical service system. Computers & Operations Research, 123, 104974.
Boutilier, J. J., & Chan, T. C. Y. (2020). Ambulance emergency response optimization in developing countries. Operations Research, 68(5), 1315–1334.
Boutilier, J. J., & Chan, T. C. Y. (2022). Drone network design for cardiac arrest response. Manufacturing & Service Operations Management, 24(5), 2387–2796.
Boutilier, J. J., Brooks, S. C., Janmohamed, A., Byers, A., Buick, J. E., Zhan, C., Schoellig, A. P., Cheskes, S., Morrison, L. J., Chan, T. C. Y., & Rescu Epistry Investigators. (2017). Optimizing a drone network to deliver automated external defibrillators. Circulation, 135(25), 2454–2465.
Branas, C. C., & Revelle, C. S. (2001). An iterative switching heuristic to locate hospitals and helicopters. Socio-Economic Planning Sciences, 35(1), 11–30.
Brandeau, M., & Larson, R. C. (1986). Extending and applying the hypercube queueing model to deploy ambulances in Boston. National Emergency Training Center, 22, 121–153.
Brotcorne, L., Laporte, G., & Semet, F. (2003). Ambulance location and relocation models. European Journal of Operational Research, 147(3), 451–463.
Budge, S., Ingolfsson, A., & Zerom, D. (2010). Empirical analysis of ambulance travel times: the case of Calgary emergency medical services. Management Science, 56(4), 716–723.
Chaiken, J. M. (1978). Transfer of emergency service deployment models to operating agencies. Management Science, 24(7), 719–731.
Chan, T. C. Y. (2017). Rise and shock: optimal defibrillator placement in a high-rise building. Prehospital Emergency Care, 21(3), 309–314.
Chan, T. C. Y., Shen, Z.-J. M., & Siddiq, A. (2017). Robust defibrillator deployment under cardiac arrest location uncertainty via row-and-column generation. Operations Research, 66(2), 358–379.
Chan, T. C. Y., Li, H., Lebovic, G., Tang, S. K., Chan, J. Y. T., Cheng, H. C. K., Morrison, L. J., & Brooks, S. C. (2013). Identifying locations for public access defibrillators using mathematical optimization. Circulation, 127(17), 1801–1809.
Channouf, N., L’Ecuyer, P., Ingolfsson, A., & Avramidis, A. (2007). The application of forecasting techniques to modeling emergency medical system calls in Calgary, Alberta. Health Care Management Science, 10, 25–45.
Cho, S.-H., Jang, H., Lee, T., & Turner, J. (2014). Simultaneous location of trauma centers and helicopters for emergency medical service planning. Operations Research, 62(4), 751–771.
Chong, K. C., Henderson, S. G., & Lewis, M. E. (2016). The vehicle mix decision in emergency medical service systems. Manufacturing & Service Operations Management, 18(3), 347–360.
Church, R., & ReVelle, C. (1974). The maximal covering location problem. Papers of the Regional Science Association, 32(1), 101–118.
Crawford, W., & Wilson, S. (2019). Emergency medical services. Alabama Department of Public Health Administrative Code (p. 6). Alabama State Board of Health.
Dami, F., Golay, C., Pasquier, M., Fuchs, V., Carron, P.-N., & Hugli, O. (2015). Prehospital triage accuracy in a criteria based dispatch centre. BMC Emergency Medicine, 15, 32.
Dao, T. H. D., Zhou, Y., Thill, J.-C., & Delmelle, E. (2012). Spatiotemporal location modeling in a 3D indoor environment: the case of AEDs as emergency medical devices. International Journal of Geographical Information Science, 26(3), 469–494.
Daskin, M. S. (1983). A maximum expected covering location model: formulation, properties and heuristic solution. Transportation Science, 17(1), 48–70.
Daskin, M. S. (1987). Location, dispatching and routing models for emergency services with stochastic travel times. In A. Ghosh, & G. Rushton (Eds.), Spatial analysis and location-allocation models (pp. 224–265). Van Nostrand Reinhold Co.
Daskin, M. S. & Stern, E. H. (1981). A hierarchical objective set covering model for emergency medical service vehicle deployment. Transportation Science, 15(2), 137.
Daskin, M. S., Hogan, K., & ReVelle, C. (1988). Integration of multiple, excess, backup, and expected covering models. Environment and Planning B: Planning and Design, 15, 15–35.
Degel, D., Wiesche, L., Rachuba, S., & Werners, B. (2015). Time-dependent ambulance allocation considering data-driven empirically required coverage. Health Care Management Science, 18(4), 444–458.
Do, Y. K., Foo, K., Ng, Y. Y., & Ong, M. E. H. (2013). A quantile regression analysis of ambulance response time. Prehospital Emergency Care, 17(2), 170–176.
Eaton, D. J., Sánchez, U. H. MI., Lantigua, R. R., & Morgan, J. (1986). Determining ambulance deployment in Santo Domingo, Dominican Republic. The Journal of the Operational Research Society, 37(2), 113–126.
Eiselt, H. A. & Marianov, V. (2009). Gradual location set covering with service quality. Socio-Economic Planning Sciences, 43(2), 121–130.
Enayati, S., Mayorga, M. E., Rajagopalan, H. K., & Saydam, C. (2018). Real-time ambulance redeployment approach to improve service coverage with fair and restricted workload for EMS providers. Omega, 79, 67–80.
Erdemir, E. T., Batta, R., Rogerson, P. A., Blatt, A., & Flanigan, M. (2010). Joint ground and air emergency medical services coverage models: A greedy heuristic solution approach. European Journal of Operational Research, 207(2), 736–749.
Erkut, E., Ingolfsson, A., & Erdoğan, G. (2008). Ambulance location for maximum survival. Naval Research Logistics, 55(1), 42–58.
Erkut, E., Ingolfsson, A., Sim, T., & Erdoğan, G. (2009). Computational comparison of five maximal covering models for locating ambulances. Geographical Analysis, 41(1), 43–65.
Fitch, J. (2005). Response times: myths, measurement and management. The Journal of Emergency Medicine, 30(9), 47.
Fleischman, R. J., Lundquist, M., Jui, J., Newgard, C. D., & Warden, C. (2013). Predicting ambulance time of arrival to the emergency department using global positioning system and Google Maps. Prehospital Emergency Care: Official Journal of the National Association of EMS Physicians and the National Association of State EMS Directors, 17(4), 458–465.
Foo, C. P. Z., Ahghari, M., & MacDonald, R. D. (2010). Use of Geographic Information Systems to determine new helipad locations and improve timely response while mitigating risk of helicopter emergency medical services operations. Prehospital Emergency Care, 14(4), 461–468.
Fujiwara, O., Makjamroen, T., & Gupta, K. K. (1987). Ambulance deployment analysis: a case study of Bangkok. European Journal of Operational Research, 31(1), 9–18.
Fulton, L. V., Lasdon, L. S., McDaniel, R. R., & Nicholas Coppola, M. (2010). Two-stage stochastic optimization for the allocation of medical assets in steady-state combat operations. The Journal of Defense Modeling and Simulation, 7(2), 89–102.
Galvão, R. D., Chiyoshi, F. Y., & Morabito, R. (2005). Towards unified formulations and extensions of two classical probabilistic location models. Computers & Operations Research, 32(1), 15–33.
Garrett, M. X. (2013). USCENTCOM review of MEDEVAC procedures in Afghanistan. Technical Report. United States Central Command.
Gendreau, M., Laporte, G., & Semet, F. (1997). Solving an ambulance location model by Tabu search. Location Science, 5(2), 75–88.
Gendreau, M., Laporte, G., & Semet, F. (2001). A dynamic model and parallel Tabu search heuristic for real-time ambulance relocation. Parallel Computing, 27(12), 1641–1653.
Gendreau, M., Laporte, G., & Semet, F. (2006). The maximal expected coverage relocation problem for emergency vehicles. The Journal of the Operational Research Society, 57(1), 22–28.
Godfrey, A., & Loyd, J. W. (2021). EMS helicopter activation. StatPearls. Treasure Island (FL): StatPearls Publishing.
Goldberg, J. (2004). Operations research models for the deployment of emergency services vehicles. EMS Management Journal, 1(1), 20.
Goldberg, J., & Paz, L. (1991). Locating emergency vehicle bases when service time depends on call location. Transportation Science, 25(4), 264–280.
Goldberg, J., Dietrich, R., Chen, J. M., George Mitwasi, M., Valenzuela, T., & Criss, E. (1990). Validating and applying a model for locating emergency medical vehicles in Tuczon, AZ. European Journal of Operational Research, 49(3), 308–324.
Grannan, B. C., Bastian, N. D., & McLay, L. A. (2015). A maximum expected covering problem for locating and dispatching two classes of military medical evacuation air assets. Optimization Letters, 9(8), 1511–1531.
Hakimi, S. L. (1964). Optimum locations of switching centers and the absolute centers and medians of a graph. Operations Research, 12(3), 450–459.
Hakimi, S. L. (1965). Optimum distribution of switching centers in a communication network and some related graph theoretic problems. Operations Research, 13(3), 462–475.
Hausner, J. (1975). Determining the travel characteristics of emergency service vehicles. New York: RAND Corporation.
Henderson, S. G. (2011). Operations research tools for addressing current challenges in emergency medical services. In J. J. Cochran, L. A. Cox, P. Keskinocak, J. P. Kharoufeh, & J. Cole Smith (Eds.), Wiley encyclopedia of operations research and management science. Hoboken, NJ, USA: John Wiley & Sons, Inc. isbn: 978-0-470-40053-1.
Hogan, K., & Revelle, C. (1986). Concepts and applications of backup coverage. Management Science, 32(11), 1434–1444.
Holmén, J., Herlitz, J., Ricksten, S.-E., Strömsöe, A., Hagberg, E., Axelsson, C., & Rawshani, A. (2020). Shortening ambulance response time increases survival in out-of-hospital cardiac arrest. Journal of the American Heart Association, 9(21), e017048.
Ingolfsson, A., Erkut, E., & Budge, S. (2003). Simulation of single start station for Edmonton EMS. Journal of the Operational Research Society, 54(7), 736–746.
Ingolfsson, A., Budge, S., & Erkut, E. (2008). Optimal ambulance location with random delays and travel times. Health Care Management Science, 11(3), 262–274.
Jagtenberg, C. J., Bhulai, S., & van der Mei, R. D. (2015). An efficient heuristic for real-time ambulance redeployment. Operations Research for Health Care, 4, 27–35.
Jagtenberg, C. J., Bhulai, S., & van der Mei, R. D. (2017). Dynamic ambulance dispatching: is the closest-idle policy always optimal? Health Care Management Science, 20(4), 517–531.
Jarvis, J. P. (1985). Approximating the equilibrium behavior of multi-server loss systems. Management Science, 31(2), 235–239.
Johnson, A. M., Cunningham, C. J., Arnold, E., Rosamond, W. D., & Zégre-Hemsey, J. K. (2021). Impact of using drones in emergency medicine: what does the future hold? Open Access Emergency Medicine, 13, 487–498.
Kamenetzky, R. D., Shuman, L. J., & Wolfe, H. (1982). Estimating need and demand for prehospital care. Operations Research, 30(6), 1148–1167.
Karatas, M., Razi, N., & Gunal, M. M. (2017). An ILP and simulation model to optimize search and rescue helicopter operations. Journal of the Operational Research Society, 68(11), 1335–1351.
Karatas, M., Yakıcı, E., & Razi, N. (2019). Military facility location problems: a brief survey. Operations Research for Military Organizations, 1–27. isbn: 978-1-5225-5513-1.
Keneally, S. K., Robbins, M. J., & Lunday, B. J. (2016). A Markov decision process model for the optimal dispatch of military medical evacuation assets. Health Care Management Science, 19(2), 111–129.
Kim, S.-H., & Whitt, W. (2014). Are call center and hospital arrivals well modeled by nonhomogeneous Poisson processes? Manufacturing & Service Operations Management, 16(3), 464–480.
Kim, S. J., Lim, G. J., Cho, J., & Côté, M. J. (2017). Drone-aided healthcare services for patients with chronic diseases in rural areas. Journal of Intelligent & Robotic Systems, 88(1), 163–180.
Knight, V. A., Harper, P. R., & Smith, L. (2012). Ambulance allocation for maximal survival with heterogeneous outcome measures. Omega, 40(6), 918–926. Special Issue on Forecasting in Management Science.
Knoblauch, A. M., de la Rosa, S., Sherman, J., Blauvelt, C., Matemba, C., Maxim, L., Defawe, O. D., Gueye, A., Robertson, J., McKinney, J., Brew, J., Paz, E., Small, P. M., Tanner, M., Rakotosamimanana, N., & Lapierre, S. G. (2019). Bi-directional drones to strengthen healthcare provision: experiences and lessons from Madagascar, Malawi and Senegal. BMJ Global Health, 4(4), e001541.
Kok, A. L., Hans, E. W., & Schutten, J. M. J. (2012). Vehicle routing under time-dependent travel times: the impact of congestion avoidance. Computers & Operations Research, 39(5), 910–918.
Krafft, T., García-Castrillo Riesgo, L., Fischer, M., Lippert, F., Overton, J., & Robertson-Steel, I. (2003). EMS data-based health surveillance system project report (p. 79). Munich: European Emergency Data Project.
Krishnan, K., Marla, L., & Yue, Y. (2016). Robust ambulance allocation using risk-based metrics. In 2016 8th International Conference on Communication Systems and Networks, 1–6.
Kunkel, A., & McLay, L. A. (2013). Determining minimum staffing levels during snowstorms using an integrated simulation, regression, and reliability model. Health Care Management Science, 16(1), 14–26.
Larson, R. C. (1974). A hypercube queuing model for facility location and redistricting in urban emergency services. Computers & Operations Research, 1(1), 67–95.
Larson, R. C. (1975). Approximating the performance of urban emergency service systems. Operations Research, 23, 845–868.
Lecky, F. E., Reynolds, T., Otesile, O., Hollis, S., Turner, J., Fuller, G., Sammy, I., Williams-Johnson, J., Geduld, H., Tenner, A. G., French, S., Govia, I., Balen, J., Goodacre, S., Marahatta, S. B., De-Vries, S., Sawe, H. R., El-Shinawi, M., Mfinanga, J., Rubiano, A. M., Chebbi, H., Do Shin, S., Ferrer, J. M. E., Haddadi, M., Firew, T., Taubert, K., Lee, A., Convocar, P., Jamaluddin, S., Kotecha, S., Abu Yaqeen, E., Wells, K., & Wallis, L. (2020). Harnessing interdisciplinary collaboration to improve emergency care in low- and middle-income countries (LMICs): results of research prioritisation setting exercise. BMC Emergency Medicine, 20(1), 68.
Lejeune, M. A., & Margot, F. (2018). Aeromedical battlefield evacuation under endogenous uncertainty in casualty delivery times. Management Science, 64(12), 5481–5496.
Mandell, M. B. (1998). Covering models for two-tiered emergency medical services systems. Location Science, 6(1), 355–368.
Marianov, V., & ReVelle, C. (1992). A probabilistic fire-protection siting model with joint vehicle reliability requirements. Papers in Regional Science, 71(3), 217–241.
Marianov, V., & Revelle, C. (1994). The queuing probabilistic location set covering problem and some extensions. Socio-Economic Planning Sciences, 28(3), 167–178.
Marianov, V., & Serra, D. (2001). Hierarchical location-allocation models for congested systems. European Journal of Operational Research, 135(1), 195–208.
Marianov, V., & Serra, D. (2002). Location–allocation of multiple-server service centers with constrained queues or waiting times. Annals of Operations Research, 111(1), 35–50.
Marla, L., Krishnan, K., & Deo, S. (2021). Managing EMS systems with user abandonment in emerging economies. IISE Transactions, 53(4), 389–406.
Mason, A. J. (2013). Simulation and real-time optimised relocation for improving ambulance operations. In B. T. Denton (Ed.), Handbook of healthcare operations management (vol. 184, pp. 289–317). New York, NY: Springer New York. isbn: 978-1-4614-5885-2.
Matteson, D. S., McLean, M. W., Woodard, D. B., & Henderson, S. G. (2011). Forecasting emergency medical service call arrival rates. The Annals of Applied Statistics, 5(2), 1379–1406.
Maxwell, M. S., Restrepo, M., Henderson, S. G., & Topaloglu, H. (2010). Approximate dynamic programming for ambulance redeployment. INFORMS Journal on Computing, 22(2), 266–281.
Maxwell, M. S., Cao Ni, E., Tong, C., Henderson, S. G., Topaloglu, H., & Hunter, S. R. (2014). A bound on the performance of an optimal ambulance redeployment policy. Operations Research, 62(5), 1014–1027.
McLay, L. A. (2009). A maximum expected covering location model with two types of servers. IIE Transactions, 41(8), 730–741.
McLay, L. A. & Mayorga, M. E. (2010). Evaluating emergency medical service performance measures. Health Care Management Science, 13(2), 124–136.
McLay, L. A. & Mayorga, M. E. (2013). A model for optimally dispatching ambulances to emergency calls with classification errors in patient priorities. IIE Transactions, 45(1), 1–24.
McLay, L. A. & Moore, H. (2012). Hanover county improves its response to emergency medical 911 patients. Interfaces, 42(4), 380–394.
Moeini, M., Jemai, Z., & Sahin, E. (2015). Location and relocation problems in the context of the emergency medical service systems: a case study. Central European Journal of Operations Research, 23(3), 641–658.
Moresky, R. T., Razzak, J., Reynolds, T., Wallis, L. A., Wachira, B. W., Nyirenda, M., Carlo, W. A., Lin, J., Patel, S., Bhoi, S., Risko, N., Wendle, L. A., & Calvello Hynes, E. J. (2019). Advancing research on emergency care systems in low-income and middle-income countries: ensuring high-quality care delivery systems. BMJ Global Health, 4(Suppl 6), e001265.
Mullie, A., Van Hoeyweghen, R., & Quets, A. (1989). Influence of time intervals on outcome of CPR. Resuscitation, 17, S23–S33.
Nair, R., & Miller-Hooks, E. (2009). Evaluation of relocation strategies for emergency medical service vehicles. Transportation Research Record, 2137(1), 63–73.
Naoum-Sawaya, J., & Elhedhli, S. (2013). A stochastic optimization model for real-time ambulance redeployment. Computers & Operations Research, 40(8), 1972–1978.
Narad, R. A., & Driesbock, K. R. (1999). Regulation of ambulance response times in California. Prehospital Emergency Care, 3(2), 131–135.
Narad, R. A., & Gillespie, W. (1998). The public vs private debate: Separating facts from values. Prehospital Emergency Care, 2(3), 196–202.
Nasrollahzadeh, A. A., Khademi, A., & Mayorga, M. E. (2018). Real-time ambulance dispatching and relocation. Manufacturing & Service Operations Management, 20(3), 467–480.
National Highway Traffic Safety Administration. (2014). Traffic safety facts: EMS research note: EMS system demographics. Department of Transportation Highway Safety 812 041; DOT HS 812 041. United States National Highway Traffic Safety Administration.
Nelas, J., & Dias, J. (2021). Locating emergency vehicles: modelling the substitutability of resources and the impact of delays in the arrival of assistance. Operations Research Perspectives, 8, 100202.
Nickel, S., Reuter-Oppermann, M., & Saldanha-da-Gama, F. (2016). Ambulance location under stochastic demand: a sampling approach. Operations Research for Health Care, 8, 24–32.
Noyan, N. (2010). Alternate risk measures for emergency medical service system design. Annals of Operations Research, 181(1), 559–589.
Olhede, S. C. & Wolfe, P. J. (2018). The growing ubiquity of algorithms in society: implications, impacts and innovations. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 376(2128), 20170364.
Pozner, C. N., Zane, R., Nelson, S. J., & Levine, M. (2004). International EMS systems: The United States: past, present, and future. Resuscitation, 60(3), 239–244.
Prydz, E. B., & Wadhwa, D. (2019). Classifying countries by income. The World Bank.
Rajagopalan, H. K., Saydam, C., & Xiao, J. (2008). A multiperiod set covering location model for dynamic redeployment of ambulances. Computers & Operations Research, 35(3), 814–826.
Repede, J. F., & Bernardo, J. J. (1994). Developing and validating a decision support system for locating emergency medical vehicles in Louisville, Kentucky. European Journal of Operational Research, 75(3), 567–581.
Repede, J. F., Jeffries, C. J., & Hubbard, E. (1993). ALIAS: a graphical user interface for an ambulance location model. International Journal of Operations & Production Management, 13(12), 36–46.
Restrepo, M., Henderson, S. G., & Topaloglu, H. (2009). Erlang loss models for the static deployment of ambulances. Health Care Management Science, 12(1), 67–79.
Rettke, A., Robbins, M., & Lunday, B. (2016). Approximate dynamic programming for the dispatch of military medical evacuation assets. European Journal of Operational Research, 254, 824–839.
ReVelle, C., & Hogan, K. (1988). A reliability-constrained siting model with local estimates of busy fractions. Environment and Planning B: Planning and Design, 15(2), 143–152.
ReVelle, C., & Hogan, K. (1989). The maximum availability location problem. Transportation Science, 23(3), 192–200.
ReVelle, C., Bigman, D., Schilling, D., Cohon, J., & Church, R. (1977). Facility location: a review of context-free and EMS models. Health Services Research, 12(2), 129–146.
Sariyer, G., Ataman, M. G., Akay, S., Sofuoglu, T., & Sofuoglu, Z. (2017). An analysis of emergency medical services demand: Time of day, day of the week, and location in the city. Turkish Journal of Emergency Medicine, 17(2), 42–47.
Saydam, C., Rajagopalan, H. K., Sharer, E., & Lawrimore-Belanger, K. (2013). The dynamic redeployment coverage location model. Health Systems, 2(2), 103–119.
Schierbeck, S., Hollenberg, J., Nord, A., Svensson, L., Nordberg, P., Ringh, M., Forsberg, S., Lundgren, P., Axelsson, C., & Claesson, A. (2021). Automated external defibrillators delivered by drones to patients with suspected out-of-hospital cardiac arrest. European Heart Journal, 42, 1478–1487.
Schilling, D., Jack Elzinga, D., Cohon, J., Church, R. L., & ReVelle, C. (1979). The TEAM/FLEET models for simultaneous facility and equipment siting. Transportation Science, 13(2), 163–175.
Schmid, V. (2012). Solving the dynamic ambulance relocation and dispatching problem using approximate dynamic programming. European Journal of Operational Research, 219(3), 611–621.
Schmid, V., & Doerner, K. F. (2010). Ambulance location and relocation problems with time-dependent travel times. European Journal of Operational Research, 207(3), 1293–1303.
Scott, J., & Scott, C. (2017). Drone delivery models for healthcare. In: Hawaii International Conference on System Sciences.
Steenhoff, T. C., Siddiqui, D. I., & Zohn, S. F. (2022). EMS air medical transport. StatPearls. Treasure Island (FL): StatPearls Publishing.
Stoesser, C. E., Boutilier, J. J., Sun, C. L. F., Brooks, S. C., Cheskes, S., Dainty, K. N., Feldman, M., Ko, D. T., Lin, S., Morrison, L. J., Scales, D. C., & Chan, T. C. Y. (2021). Moderating effects of out-of-hospital cardiac arrest characteristics on the association between EMS response time and survival. Resuscitation, 169, 31–38.
Stout, J., Pepe, P. E., & Mosesso, V. N. (2000). All–advanced life support vs tiered-response ambulance systems. Prehospital Emergency Care, 4(1), 1–6.
Sudtachat, K., Mayorga, M. E., & McLay, L. A. (2014). Recommendations for dispatching emergency vehicles under multitiered response via simulation. International Transactions in Operational Research, 21(4), 581–617.
Sun, C. L. F., Demirtas, D., Brooks, S. C., Morrison, L. J., & Chan, T. C. Y. (2016). Overcoming spatial and temporal barriers to public access defibrillators via optimization. Journal of the American College of Cardiology, 68(8), 836–845.
Swersey, A. J., Goldring, L., & Geyer, E. D. (1993). Improving fire department productivity: merging fire and emergency medical units in New Haven. Interfaces, 23(1), 109–129.
Toregas, C., Swain, R., ReVelle, C., & Bergman, L. (1971). The location of emergency service facilities. Operations Research, 19(6), 1363–1373.
United Nations. (2010). The millennium development goals report. Technical Report. New York, NY.
Urdaneta, L. F., Miller, B. K., Ringenberg, B. J., Cram, A. E., & Scott, D. H. (1987). Role of an emergency helicopter transport service in rural trauma. Archives of Surgery, 122(9), 992–996.
van Barneveld, T. C., Bhulai, S., & van der Mei, R. D. (2017a). A dynamic ambulance management model for rural areas: computing redeployment actions for relevant performance measures. Health Care Management Science, 20(2), 165–186.
van Barneveld, T. C., van der Mei, R. D., & Bhulai, S. (2017b). Compliance tables for an EMS system with two types of medical response units. Computers & Operations Research, 80, 68—81.
van den Berg, P. L. & Aardal, K. (2015). Time-dependent MEXCLP with startup and relocation cost. European Journal of Operational Research, 242(2), 383–389.
Vlahogianni, E. I., Karlaftis, M. G., & Golias, J. C. (2014). Short-term traffic forecasting: where we are and where we’re going. Transportation Research Part C: Emerging Technologies, 43, 3–19.
Wagner, M. R., & Radovilsky, Z. (2012). Optimizing boat resources at the U.S. Coast Guard: deterministic and stochastic models. Operations Research, 60(5), 1035–1049.
Westgate, B. S., Woodard, D. B., Matteson, D. S., & Henderson, S. G. (2016). Large-network travel time distribution estimation for ambulances. European Journal of Operational Research, 252(1), 322–333.
Wilson, B., Gratton, M. C., Overton, J., & Watson, W. A. (1992). Unexpected ALS procedures on non-emergency ambulance calls: The value of a single-tier system. Prehospital and Disaster Medicine, 7(4), 380–382.
Woodard, D., Nogin, G., Koch, P., Racz, D., Goldszmidt, M., & Horvitz, E. (2017). Predicting travel time reliability using mobile phone GPS data. Transportation Research Part C: Emerging Technologies, 75, 30–44.
Yoon, S., & Albert, L. A. (2018). An expected coverage model with a cutoff priority queue. Health Care Management Science, 21(4), 517–533.
Yoon, S., & Albert, L. A. (2020). A dynamic ambulance routing model with multiple response. Transportation Research Part E: Logistics and Transportation Review, 133, 101807.
Yoon, S., Albert, L. A., & White, V. M. (2021). A stochastic programming approach for locating and dispatching two types of ambulances. Transportation Science, 55(2), 275–296.
Zhang, Z.-H., & Jiang, H. (2014). A robust counterpart approach to the bi-objective emergency medical service design problem. Applied Mathematical Modelling, 38(3), 1033–1040.
Zhou, Z., Matteson, D. S., Woodard, D. B., Henderson, S. G., & Micheas, A. C. (2015). A spatio-temporal point process model for ambulance demand. Journal of the American Statistical Association, 110(509), 6–15.
Acknowledgements
The authors acknowledge the Mecklenburg EMS Agency and NEMSIS for data used in this chapter. The content reproduced from the NEMSIS Database remains the property of the National Highway Traffic Safety Administration. The National Highway Traffic Safety Administration is not responsible for any claims arising from works based on the original data, text, tables, or figures. The third author was in part supported by the National Science Foundation Award 2000986. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the US Government or the National Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stratman, E.G., Boutilier, J.J., Albert, L.A. (2023). Uncertainty in Facility Location Models for Emergency Medical Services. In: Eiselt, H.A., Marianov, V. (eds) Uncertainty in Facility Location Problems. International Series in Operations Research & Management Science, vol 347. Springer, Cham. https://doi.org/10.1007/978-3-031-32338-6_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-32338-6_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-32337-9
Online ISBN: 978-3-031-32338-6
eBook Packages: Business and ManagementBusiness and Management (R0)